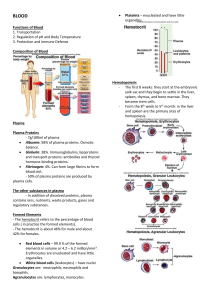
BLOOD Platelets – enucleated and have little organelles. Functions of Blood 1. Transportation 2. Regulation of pH and Body Temperature 3. Protection and Immune Defense Composition of Blood Hematopoiesis - The first 8 weeks: they start at the embryonic yolk sac and they begin to settle in the liver, spleen, thymus, and bone marrow. They become stem cells. - Form the 8th week to 5th month: in the liver and spleen are the primary sites of hemopoiesis. Plasma Plasma Proteins - 7g/100ml of plasma Albumin: 58% of plasma proteins. Osmotic balance. Globulin: 38%. Immunoglobulins, lipoproteins and transport proteins: antibodies and thyroid hormone-binding proteins. Fibrinogen: 4%. Can form large fibrins to form blood clot. - 50% of plasma proteins are produced by plasma cells. The other substances in plasma - In addition of dissolved proteins, plasma contains ions, nutrients, waste products, gases and regulatory substances. Formed Elements - The hematocrit refers to the percentage of blood cells ( in practice the formed elements). - The hematocrit is about 46% for male and about 42% for females. Red blood cells – 99.9 % of the formed elements in volume or 4.2 – 6.2 million/mm³. Erythrocytes are enucleated and have little organelles. White blood cells (leukocytes) – have nuclei Granulocytes are: neutrophils, eosinophils and basophils. Agranulocytes are: lymphocytes, monocytes. Recycling of RBC/hemoglobin Components Globular proteins are broken down to amino acids for resumption. Heme is separated from its iron and becomes biliverdin (green) then to bilirubin to be absorbed in the liver, there conjugated and then excreted in bile from the intestines. A build up of bilirubin in the circulation and intestinal spaces is known as jaundice. Erythrocytes 99.9% in volume of the formed elements. 5.4 million cells/ one microliter (ul or mm³) of blood for a man. 4.8 million cells/ one microliter (ul or mm³) for a woman. 260 million RBC/drop of blood. 25 trillion RBCs in the blood of an adult = 1/3 of all the cells in the human body. (75 trillion cells) The diameter is 7.5 microns and the thickness varies at the edge (thick, 1.5 -2.5 microns) and the center (thinner, 1 micron). Functions of Erythrocytes - 33% of RBC is hemoglobin, Hb, an oxygen and CO2 carrying protein. - Each Hb consist of two pairs of subunits (alpha and beta) and each subunit has an oxygen binding heme. Leukocytes Nucleus is present and hemoglobin is absent. Granulocytes: Neutrophils, eosinophils, basophils Agranulocytes: monocytes, lymphocytes There are as many as 6-8,000 leukocytes in 1 microliter of blood, but most of the leukocytes are found on peripheral tissues. Functions of Leukocytes General defense: 1. neutrophils, 2. eosinophils, 3. basophils and 4. monocytes Specific immunity: 1. lymphocytes Neutrophils: polymorphonuclear Live in the circulatory system for only 10-12 hours, then move into tissues, where they live up to 1-2 days. Phagocytic and secrete lysozymes to digest bacteria and others. Eosinophils: reduce inflammation and parasitic reaction Basophils: releases histamines, which promotes inflammation also release heparin, which inhibits blood clotting. Monocytes – live 2-3 days in circulation and migrate in the tissues as macrophages, which phagocytose foreign bodies. An increased number of monocytes is an indication of an infection. Lymphocytes They are about the size of an RBC and they contain a nucleus. There are three types: T-cells: attack foreign bodies. B-cells: differentiate into plasma cells, which secrete antibodies. Natural Killer cells (NK cells): destroys the bodies own abnormal cells. Thrombocytes Megakaryocytes in bone marrow, which release their fragments into circulation, then called platelets. Platelets have no nuclei. Participate in blood clotting. Platelets survive about 10-12 days in circulation and are about 150,000 – 300,000/ul Thrombocytopenia is a loss of platelets and is a sign of bleeding etc.. Thrombocytosis is excess platelets and is a sign of infection. Hemostatis Prevents loss of blood in three phases 1. The vascular phase: immediate temporary closure of a blood vessel by constriction of vascular smooth muscles. 2. The platelet phase: formation of a platelet plug by platelet adhesion and aggregation. Platelets bind to collagen in damaged tissues. Platelets are adhered and form a plug. 3. The coagulation phase: for a large blood clot formation by the network of fibrin from fibrinogen. A large number of steps involving many factors are required, some of which require thrombin and Ca++. Clotting Process Clotting is the phenomenon where blood cells are trapped in the framework of fibers. The clotting process requires Ca++ and 11 different plasma proteins, mostly enzymes The process goes through 3-stages: 1. Activation of prothrombinase by either the extrinsic or intrinsic pathway. 2. Prothormbinase converts prothrombin to thrombin. 3. Thrombin converts fibrinogen to fibrin. Extrinsic pathway: the process is triggered by a tissue factor of damaged endothelial cells, the other enzymes are successively activated to complete the clotting process- a cascade. The process is fast and takes only 15 seconds. Intrinsic pathway: starts with the activation of factor XII by contacting the damaged blood vessels and is a slower process. Blood Collection and Analysis • Collection of human blood is usually performed from a superficial vein via venipuncture or from the finger tip or sole. • Only when needed an arterial puncture may be performed. • The temperature of blood is about 38°C and is slightly higher than that of the body temperature. • Having a large quantity of proteins in plasma (7g/100ml) and corpuscles, bloods’ viscosity is more than five times higher than that of water. • The pH of blood is about 7.4. Blood Tests • Genetically determined RBC antigens (glycoproteins) rest on the surface of the membrane. • There are at least 50 different kinds of antigens on the surface of an RBC. • Their antibodies are found in plasma. • One set of important antigens are A and B, typed ABO. Although A/B antibodies are not found in the blood until about 2 months after birth. Blood Typing Hemolytic Disease of the Newborn