Infectious Arthritis: Suppurative, TB, Reactive, Osteoarthritis
advertisement
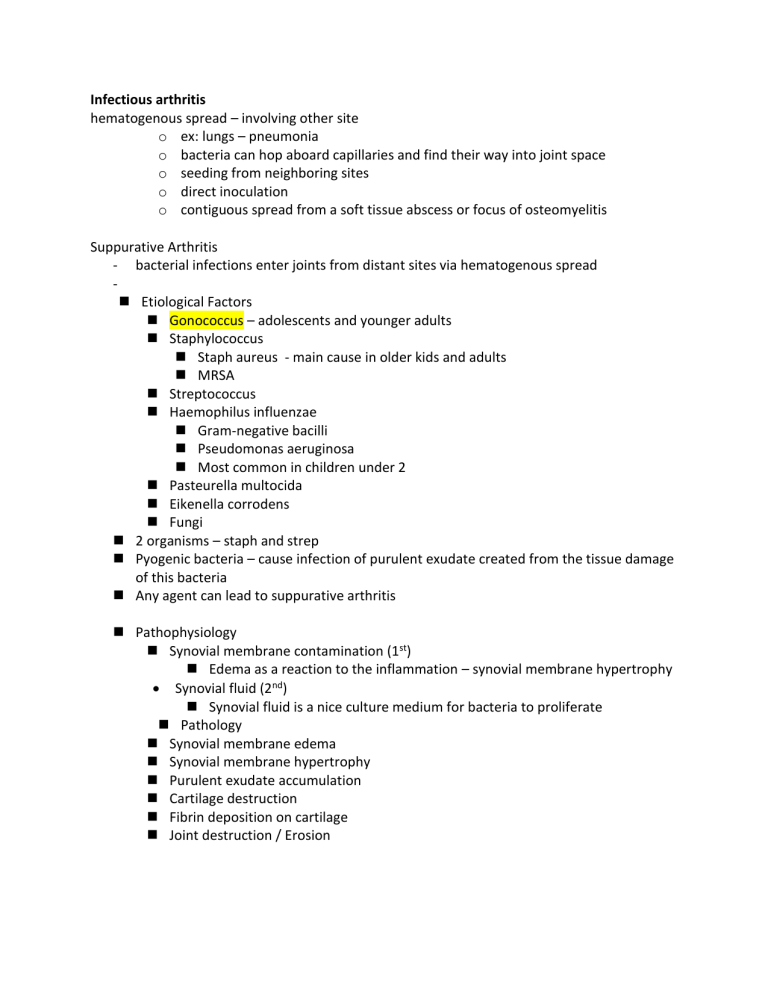
Infectious arthritis hematogenous spread – involving other site o ex: lungs – pneumonia o bacteria can hop aboard capillaries and find their way into joint space o seeding from neighboring sites o direct inoculation o contiguous spread from a soft tissue abscess or focus of osteomyelitis Suppurative Arthritis - bacterial infections enter joints from distant sites via hematogenous spread Etiological Factors Gonococcus – adolescents and younger adults Staphylococcus Staph aureus - main cause in older kids and adults MRSA Streptococcus Haemophilus influenzae Gram-negative bacilli Pseudomonas aeruginosa Most common in children under 2 Pasteurella multocida Eikenella corrodens Fungi 2 organisms – staph and strep Pyogenic bacteria – cause infection of purulent exudate created from the tissue damage of this bacteria Any agent can lead to suppurative arthritis Pathophysiology Synovial membrane contamination (1st) Edema as a reaction to the inflammation – synovial membrane hypertrophy Synovial fluid (2nd) Synovial fluid is a nice culture medium for bacteria to proliferate Pathology Synovial membrane edema Synovial membrane hypertrophy Purulent exudate accumulation Cartilage destruction Fibrin deposition on cartilage Joint destruction / Erosion Suppurative Arthritis Classic presentation - Sudden development of a painful and swollen joint o Hip, knee, shoulder, elbow o Painful, hot, red, acute, swollen - Limited ROM - Fever, leukocytosis - Elevated sedimentation rate - Nongonococcal cases – infection involves only a single joint – most commonly the knee - Axial joints most commonly involved in drug users - Joint aspiration is diagnostic if it yields purulent fluid in which the agent can be identified o Purulent effusion extremely high WBC count o Inflammatory effusions Leukocytes o Hemorrhagic effusions Coagulation defect, hemophilia A or B - Do CBC and white count Aspiration and culture based on H and P Single or multi joint involvement Rapid joint destruction without treatment o Need to rule out joint infection quick or irrev joint damage can occur Differential: o Cellulitis, bursitis, acute osteo - Tissue damage – dead immune cells sequestered to that area – some cells die along with tissue debris accumulate in that joint secondary to infection These tissues will be compromised as well Fibrin depositions- found in infective – widespread joint destruction Total loss of cartilage involving erosion Pre disposing conditions: - Immune deficiency o Parts of the complement system membrane attack complex (C5,6,7) are more prone to gonococcal attacks - Illness, joint trauma, chronic arthritis, IV drug use Disseminated Gonococcal Infection - Subacute symptoms - Single joint o Oligoarthritic pattern o Knee, ankle, hip, shoulder, elbow, wrist, sternoclav - Migratory type of joint - Bacteremia infection stage o Migratory polyarthritis o Tenosynovitis o Dermatitis - Septic arthritis Joint localization stage o Myalgia, fever, chills, rash o Joint fluid Leukocytes Synovial culture negative Blood culture positive o Purulent exudate in urogenital region IV Drug Use - Axial spine - Sacroiliac - Sternoclav Tuberculosis Arthritis - Complication of adjoining osteo - Monoarticular pain and swelling - Systemic symptoms vary - After hematogenous spread from visceral (usually pulmonary) site of infection - Onset is insidious - Gradual progressive pain – Chronic progressive - Caseous necrosis - Granulomas o Langerhans giant cells on center of granuloma and on the periphery o Response of synovial membrane leads to pannus formation - Affected synovium grows as a pannus over the articular cartilage and erodes the bone along the joint margins o Fibrinous hypertrophic type of growth found on synovial membrane - Chronic disease results in fibrous ankylosis and obliteration of the joint space Hematogenous spread o Visceral, pulmonary, osteomyelitis Ghon complex o Primary infection site o Draining lymph nodes Large, weight bearing joints Synovial culture + Mycobacterium stain red Joint fluid o PCR fastest way to check for TB o Neutrophils o Acid fast stain 45 yr. old man with hx of cough now having trouble walking, weight bearing joints pain - - - Order of which pathology occurs: 1. Confluent granulomas 2. Central caseous necrosis 3. Pannus over articular cartilage 4. Bone erosions along joint margins 5. Fibrous ankylosis and obliteration of joint space 6. Severe destruction 7. Weight bearing joints Pott Disease - Similar to TB - Bone is eroded away - Granulomas form - Collapse of vertebral – pushing or impinging on nerve exiting - Annulofibrosis HLA – D27 association Disorganized bone formation – hyperthyroid, renal dx Anti ds – DNA + - lupus Bamboo spine - Buzz work for ankylosing spondylitis Joint infiltration with basophils - Associated with leukemia mild dysplastic symptoms Seronegative Spondyloarthropathies Unified by the following features: 1. Pathologic changes in ligamentous attachments rather than synovium 2. Involvement of the sacroiliac joints with or without other joints 3. Absence of rheumatoid factor 4. HLA B27 Manifestations are immune mediated and are triggered by a T-cell response against an identified antigen that may cross react with native molecules of the musculoskeletal system 1. Ankylosing Spondylitis 2. Reactive arthritis 3. Psoriatic arthritis 4. Ulcerative colitis 5. Chron Disease Ankylosing Spondylitis - Destruction of articular cartilage and bony ankylosis - Chronic inflammatory joint disease - Sacroiliac and apophyseal joints (between tuberosities and processes) o Prominent region of tendon and ligament insertions - 20s-30s - Lower back pain and spinal immobility - H:A-B27 positive - Enthesis – site o Point of tendon, ligament or muscle insertion into bone - Enthesis – inflammation at site o Erosion, osteitis, ossification o Mononuclear cell infiltrate o PMN - Sacroiliac infiltration o CD4 and CD8 o Macrophages and High TNF-a - No specific lab test Pathology 1. Chronis synovitis 2. Destruction of articular cartilage 3. Bony ankylosis 4. Tendinoligamentous inflammation and ossification 5. Bony outgrowths – severe spinal immobility a. Syndesmophytes – osseous excrescence attached to a ligament i. Bone on a ligament bro ii. Bamboo spine Clinical Features - Chronic progressive, low back pain, peripheral joint pain - Complications: spine fracture, uveitis, aortitis Reactive Arthritis - Triad of: arthritis, non-gonococcal urethritis or cervicitis, and conjunctivitis - Men in their 20s 30s - HLA -B27 - HIV - Autoimmune reaction caused by prior infection of the genitourinary system (Chlamydia) or GI (shigella, Salmonella, Yersinia, Campylobacter) - Arthritic symptoms develop within several weeks of initial bout of urethritis or diarrhea - Joint stiffness and low back pain - Ankles, knees, feet in an asymmetric pattern - Sausage fingers – synovitis of a digital tendon sheath - Calcaneal spurs DNA bony outgrowths – ossification of tendoligamentous insertion sites - Severe cases look just like ankylosing spondylitis – sacroiliac involvement - Extraarticular involvement: o Balanitis, o Cardiac conduction probs, aortic regurgitation o Keratoderma blennorrhagia – skin lesions on palms and soles o Plaques/ erosion of tongue o conjunctivitis - Immunologic responses against lipopolysaccharide components Macrophage infiltration of fibrocartilage - Self-limited 3-12 months 50% of patients get recurrent arthritis, tendonitis, fasciitis, lower back pain 25 you man had a UTI 7 weeks ago and resolved now his right ankle and knee hurt o Low fever, fatigue, superficial oral ulcers o Anemia, synovial fluid in knee o Chlamydia infection Osteoarthritis - Degenerative bone disease - Degeneration of cartilage - Structural and functional failure of synovial joints - Collagen 2 is degraded by matrix metalloproteases - Degradations exceeds synthesis - Environmental factors – age and biomechanical stress 3 phases: 1. Chondrocyte injury a. Genetic b. Biochemical factors 2. Early OA a. Chondrocytes proliferation b. Secrete inflammatory mediators i. Collagens, proteoglycans, and proteases ii. Remodel the cartilaginous matrix iii. Initiate inflammatory changes c. Remodeling of cartilage matrix d. Secondary inflammatory changes in the synovium and subchondral bone 3. Late OA a. Repetitive injury and chronic inflammation b. Chondrocyte drop out c. Marked loss of cartilage d. Extensive subchondral bone changes Morphology - Fissures and clefts at articular surface - Loss of articular cartilage - Full thickness portions of the cartilage are sloughed - Joint mice o Dislodged pieces of cartilage and subchondral bone tumble into the joint, forming loose bodies o Pieces of cartilage and subchondral bone break off - Exposed subchondral plate becomes new articular surface - There are some chondrocytes there trying to make new cartilage but not enough - Bone eburnation – loss of articular cartilage - Fracture gaps – force synovial fluid into the subchondral space causing micro fissures - Synovial fluid leaks in forming subchondral cysts - Fibrous-walled cysts develop fibrous tissue deposition bony outgrowths occur - Collagen 2 is cleaved causing fissures and clefts Granular soft articular surface Chondrocytes die and full thickness portions of cartilage are sloughed Dislodged pieces of cartilage and subchondral bone tumble into the joint – JOINT MICE - Exposed subchondral bone becomes new articular surface Friction with the opposing bone smooths the surface – ENUBRIATION Sclerosis of the underlying bone Small fractures through the articulating bone Fracture gaps allow synovial fluid into the subchondral regions o Forming fibrous walled cysts Osteophytes develop at the margins of the articular surface Deep achy pain that worsens with use, morning stiffness, ~20 mins Crepitus, limited ROM Asymmetrical, single joint or few Hips, knees, lumbar, cervical, proximal and distal IPJ, first mets Heberden nodes – prominent osteophytes at the DIPJ Impingement on Spinal Foramina by Osteophytes Results in cervical and lumbar nerve root compression Radicular pain Muscle spasms Muscle atrophy Neurologic deficits – immediate and through investigation Osteo – subchondral space, thin and fibrillated cartilage can be wiped out completely Rheumatoid – immune complex mediated – can have fibrous ankylosis, eroding cartilage pannus formation, and inflamm involving the joint and soft tissue surrounding the joint Rheumatoid Arthritis Chronic inflammatory disorder of autoimmune origin that may affect mani tissues and organs but primarily attacks the joints Non suppurative proliferative and inflammatory synovitis Progresses to destruction of the articular cartilage and ankylosis of the joints Extra articular lesions may involve the heart, skin, vessels, and lungs o May resemble other auto immune things like lupus or scleroderma HLA DRB-1 CANNOT tell diff btw endogenous and exogenous antigens Enzymatic modification – proteins that have largely in their makeup an enzyme modified __ and turns it into citrulline – citrulline combines with another macromolecule to form antigen This is what the body attacks T and b cells respond to self-antigens Fibroblast chondrocyte proliferation – synovial cells are proliferated release collagenase etc all contribute to formation of pannus leading to bony and cart destruction – what you have Is fibrosis and eventually ankylosis Pathogenesis - CD4+ Helper T cells may initiate autoimmune response in RA by reacting with an arthritogenic agent - Microbial or self antigen - T cells produce cytokines that stimulate with inflammatory cells to effect tissue injury o TH1 releases IFN-y to activate macrophages and resident synovial cells o TH17 releases IL-17 to recruit neutrophils and monocytes o TNF and IL-1 from macrophages stimulate protease release that destroy hyaline cartilage - The synovium of RA contains germinal centers with secondary follicles and plasma cells that produce autoantibodies against self-antigens Autoantibodies are specific for citrullinated peptides o arginine peptides are post-translationally converted to citrulline in RA, antigen-antibody complexes containing citrullinated fibrinogen, type 2 collagen, enolase, and vimentin deposit in the joints antibodies against these peptides are diagnostic markers Morphology Joints Symmetric arthritis Small joints of the hand and feet Synovium (Bulbous villi) Edematous Thickened Hyperplastic Dense inflammatory infiltrates Lymphoid follicles Increased vascularity Fibrinopurulent exudate on the synovial and joint surfaces Rheumatoid cutaneous nodules - most common cutaneous lesions - Areas of skin subjected to pressure - forearm, elbow, occiput, lumbosacral Blood Vessels - Severe erosive disease, rheumatoid nodules, and high titers of rheumatoid factor are at risk for developing vasculitis - Acute necrotizing vasculitis o Small and large arteries - Obliterating endarteritis o Affects segments of small arteries such as vasa vasorum, digital arteries o Results in peripheral neuropathy, ulcers, and gangrene - Leukocytoclastic vasculitis o Produces purpura, cutaneous ulcers, and nail bed infection - Uveitis and keratoconjunctivitis Diagnosis of RA (1) characteristic radiographic finding (2) sterile, turbid synovial fluid (3) combination of rheumatoid factor and anti-CCP antibody (80% of patients) - Manifests as a symmetric arthritis of small joints of the hand and feet Synovium becomes edematous, thickened, and hyperplastic Smooth contour turns into bulbous villi (A,B) Histo changes Pannus formation 1. Synovial hyperplasia and proliferation 2. Dense inflammatory infiltrate of CD4+ helper T cells, plasma cells, dendritic cells and macrophages 3. Increased vascularity due to angiogenesis 4. Fibrinopurulent exudate on the synovial and joint surfaces 5. Osteoclastic activity in underlying bone a. Allowing the synovium to penetrate into the bone and cause periarticular erosions and cysts i. Periarticular erosions and subchondral cysts WTF is a pannus? - Mass of edematous synovium, inflammatory cells, granulation tissue, and fibroblasts that grow over the articular cartilage and cause erosion - After cartilage has been destroyed, pannus bridges the opposing bones to form a fibrous ankylosis - Eventually ossifies and results in fusion of the bones bony ankylosis Osteoarthritis (degenerative joint disease), the most common disease of joints, is a degenerative process of articular cartilage in which matrix breakdown exceeds synthesis. Inflammation is minimal and typically secondary. Local production of inflammatory cytokines may contribute to the progression of joint degeneration. Rheumatoid arthritis (RA) is a chronic autoimmune inflammatory disease that affects mainly small joints, but can be systemic. RA is caused by a cellular and humoral immune response against self-antigens, particularly citrul- linated proteins. TNF plays a central role and antagonists against TNF are of clinical benefit. Seronegative spondyloarthropathies are a heterogeneous group of likely autoimmune arthritides that prefer- entially involve the sacroiliac and vertebral joints and are associated with HLA-B27. Suppurative arthritis describes direct infection of a joint space by bacterial organisms. Tumors and Tumor-Like Lesions Involving Joints and Tendons Reactive(?) Secondary Trauma or Degenerative Processes Neoplastic Cytogenetic Studies Reveal consistent Chromosomal Aberrations Benign neoplasms Tenosynovial Giant Cell Tumor - Several neoplasms that develop in the synovial lining of joints, tendon sheaths, and bursae - 20s-40s - Both types o are heavily infiltrated by macrophages o May contain hemosiderin or foamy lipid o Scattered multinucleated giant cells o Patchy fibrosis Diffuse type o Pigmented villonodular synovitis o Involved large joints o Normally smooth synovium is converted into a tangled mat by red-brown folds, finger-like projections and nodules o Spread along the surface and infiltrate the sub synovial tissue o Knee involved 80% o Symptoms: pain, locking, recurrent swelling, ROM limits o Palpable mass o Most common mesenchymal neoplasm of the hand o Surgical excision o Recurrence is common Localized Type o Giant cell tumor of the tendon sheath o Occurs at discrete nodules attached to a tendon sheath o Common in hand o Well circumscribed o Polygonal, moderately sized, resemble synoviocytes o Solitary, slow growing, painless o Tendon sheaths along wrists and fingers - PVNS – diffuse o Involves the synovium o One or more joints diffusely o 20s-40s o Synovial Hypertrophy Nodules Fronds o Finger-like projections o Microscopic Multinucleated giant cells Foamy macrophages o Clinical Monoarticular Arthritis ROM Limitation Aggressive Surgery Significant recurrence rate - GCTTS – localized o Discrete nodule on a tendon sheath o Wrist, Fingers o Arise in the 20s – 40s o Solitary, Slow-growing o Painless mass o Cortical erosion o Often recurs locally o Surgery o Localized o Well circumscribed (walnut shaped) o Microscopic o Tumor cells o Polyhedral o Histiocytes o Multinucleated Giant Cells o Resemble synoviocytes Synovial Sarcoma - Arise near joints, especially the knee - Lump painful or tender, slow-growing - Deep seated mass present for several years - Cell of origin unclear - Lower extremity - Lack synovium - Inconsistent with origin from synoiocytes - 20s-40s - Chromosomal translocation o X and 18 o Fusion genes - Morphology o Monophasic or biphasic o Spindle shaped o Uniform spindle cells with scant cytoplasm and dense chromatin in short tightly packed fascicles o May calcify o Biphasic type gland link structures composed of cuboidal to columnar epithelium positive for epithelial markers (keratin) – differ from other sarcomas o Monophasic type Misdiagnosed as fibro or adeno