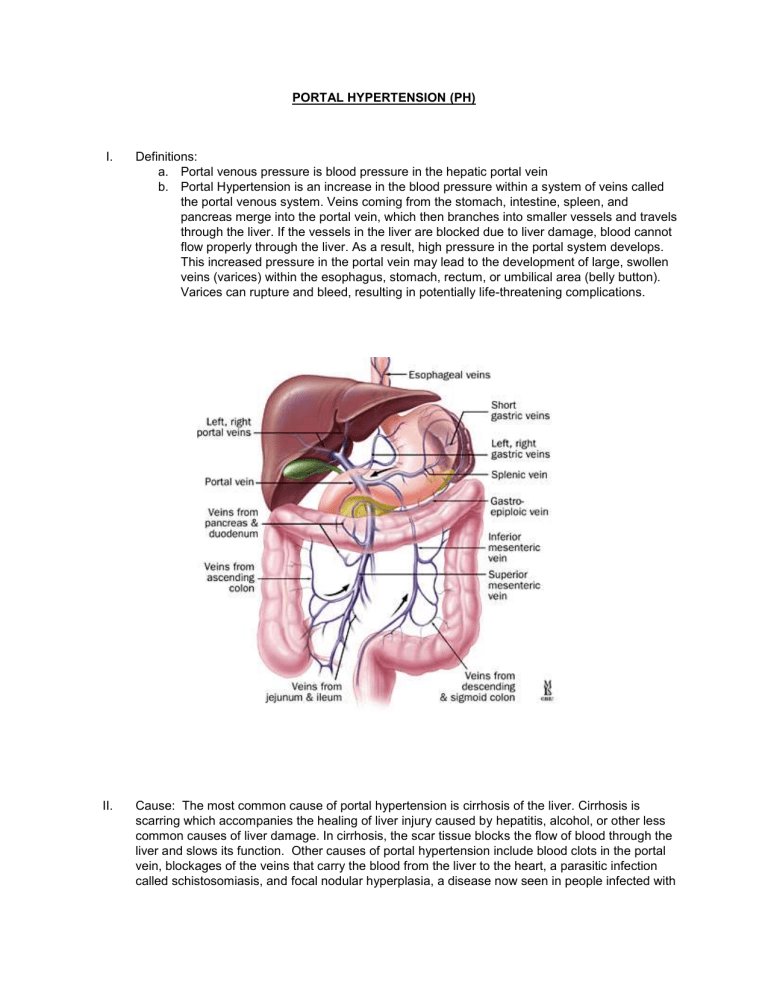
PORTAL HYPERTENSION (PH) I. Definitions: a. Portal venous pressure is blood pressure in the hepatic portal vein b. Portal Hypertension is an increase in the blood pressure within a system of veins called the portal venous system. Veins coming from the stomach, intestine, spleen, and pancreas merge into the portal vein, which then branches into smaller vessels and travels through the liver. If the vessels in the liver are blocked due to liver damage, blood cannot flow properly through the liver. As a result, high pressure in the portal system develops. This increased pressure in the portal vein may lead to the development of large, swollen veins (varices) within the esophagus, stomach, rectum, or umbilical area (belly button). Varices can rupture and bleed, resulting in potentially life-threatening complications. II. Cause: The most common cause of portal hypertension is cirrhosis of the liver. Cirrhosis is scarring which accompanies the healing of liver injury caused by hepatitis, alcohol, or other less common causes of liver damage. In cirrhosis, the scar tissue blocks the flow of blood through the liver and slows its function. Other causes of portal hypertension include blood clots in the portal vein, blockages of the veins that carry the blood from the liver to the heart, a parasitic infection called schistosomiasis, and focal nodular hyperplasia, a disease now seen in people infected with the AIDS virus and Budd-Chiari syndrome, an uncommon condition induced by thrombotic or non-thrombotic obstruction to hepatic venous outflow. Sometimes the cause is unknown. III. The main symptoms and complications of portal hypertension include: a. Gastrointestinal bleeding marked by black, tarry stools or blood in the stools, or vomiting of blood due to the spontaneous rupture and hemorrhage from varices. b. Ascites (an accumulation of fluid in the abdomen). c. Encephalopathy or confusion and forgetfulness caused by poor liver function. A condition in which it is believed that toxic products from the intestines (for example, ammonia) that are normally removed from the blood by the liver remain in the blood and are delivered to the brain. The effects on the brain can vary from minor alterations in thinking to full coma. d. Reduced levels of platelets, blood cells that help form blood clots, or white blood cells, the cells that fight infection IV. Diagnosis of problem: Transjugular Liver Biopsy a. Using a transvenous approach, the biopsy needle is inserted into the liver via the hepatic vein, avoiding the peritoneum and the liver capsule. Thus, if there is any bleeding related to the procedure, it will be back into the venous system. b. Catheter is threaded through the SVC through the IVC and into the RHV (Right Hepatic Vein). Wedging the cannula against the liver parenchyma and also directing the needle towards the region where there is more liver tissue and obtain biopsies through vein into liver tissue. c. Besides the biopsy, pressure measurements are taken. Free Right Hepatic pressure is the measurement in the RHV (It should be about the same as the IVC). Indirect measurement of Portal Venous Pressure is measured by the Wedge Hepatic Venous Pressure (WHVP). It is obtained by inflating the balloon in the RHV, thereby occluding the vein. d. HVPG (Hepatic Venous Pressure Gradient) is the difference between the wedged and free hepatic pressure and reflects the gradient between portal vein and vena caval pressures. An HPVG of ≥10 mmHg defines clinically significant portal hypertension, and if the measurement exceeds 12 mmHg, variceal hemorrhaging may occur.[4] Catheter in Right Hepatic Vein e. Portal Vein V. Normal/Abnormal Parameters a. Normal Pressures: i. Right Atrium: < 5 mm Hg ii. IVC: 3-8 mm Hg iii. Portal venous pressure: 7-12 mm Hg iv. Free Right Hepatic: 3-8 mm Hg v. Wedge Hepatic Venous Pressure: 7-12 mm Hg (indirect Portal Venous Pressure) vi. HVPG: 1-5 mm Hg (HVPG= Wedge pressure – free pressure) b. Abnormal indicating PH i. Right Atrium: >5 mm Hg ii. IVC: >8 mm Hg iii. Portal Pressure: > 12 iv. Free Right Hepatic: > 8 mm Hg v. Wedge Hepatic Venous pressure: >12 mm Hg (indirect Portal Venous Pressure) vi. HVPG: > 10mm Hg VI. Treatment for PH: TIPS (Transjugular Intrahepatic Portosystemic Shunt (TIPS): This procedure involves placing a stent (a tubular device) in the middle of the liver. Transjugular Intrahepatic Portosystemic Shunt or (TIPS) is a shunt (tube) placed between the portal vein which carries blood from the intestines and intraabdominal organs to the liver and the hepatic vein which carries blood from the liver back to the vena cava and the heart. VII. The stent connects the hepatic vein with the portal vein, which reroutes blood flow in the liver and helps relieve pressure in abnormal veins. a. During the TIPS procedure, a radiologist makes a tunnel through the liver with a needle, connecting the portal vein to one of the hepatic veins. A metal stent is placed in this tunnel to keep it open. b. The procedure reroutes blood flow in the liver and reduces pressure in all abnormal veins, not only in the stomach and esophagus, but also in the bowel and the liver. c. d. There are two important complications of the TIPS procedure. i. The first is hepatic encephalopathy, a condition in which it is believed that toxic products from the intestines (for example, ammonia) that are normally removed from the blood by the liver remain in the blood and are delivered to the brain. (The TIPS allows the toxin-containing blood to bypass the liver.) The effects on the brain can vary from minor alterations in thinking to full coma. ii. A second complication is heart failure due to the sudden increase in the amount of blood returning to the heart through the shunt. The heart is unable to pump the returning blood fast enough, resulting in heart failure. VIII. References a. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2747432/ b. http://www.webmd.com/digestive-disorders/digestive-diseases-portal c. http://www.medscape.com/viewarticle/704841_2 d. http://www.cmaj.ca/content/174/10/1433/F1.expansion.html e. http://radiographics.rsna.org/content/28/2/359/F3.expansion.html f. http://lane.stanford.edu/portals/cvicu/HCP_CV_Tab_1/Intracardiac_Pressures.pdf