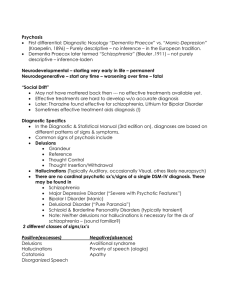
PSYCHIATRIC HISTORY
BIO-DATA OF THE PATIENT
NAME
:
Kiran
AGE
:
45 years
SEX
:
Female
REG. No.
:
F-9126
WARD
:
Female closed Ward
MARITAL STATUS
:
Unmarried
RELIGION
:
Hindu
EDUCATION
:
B.A
OCCUPATION
:
Unemployed
LANGUAGE
:
Hindi
D.O.A
:
06/08/19
DIAGNOSIS
:
Paranoid Schizophrenia
INFORMANT
:
Mr.Sanjay
RELATIONSHIP WITH PATIENT :
Brother
RELIABILITY OF INFORMANT
Reliable
:
PRESENTING COMPLAINTS
ACCORDING TO THE PATIENT:
I wanted to quit smoking, that is why I came here.
I am alright, I have no other complaints, now I have left even smoking.
ACCORDING TO RELATIVES:
Patient was presented to the hospital with C/O:
Suspiciousness
Withdrawn behaviour
Irregular sleep and appetite.
Increased smoking.
Misidentification
Grandeur behavior
HISTORY OF PRESENT ILLNESS
ONSET: Onset of illness is insidious
COURSE OF ILLNESS: Continuous.
Patient was apparently well and behaved quite normally and wishes to shop on asking
for her own account. When she was asked to sign, she refused acknowledging herself
as Kiran. Patient talks about being an IAS and would go to UPSC office , but at other
instances wishes to take up secretariat job and would take up a course of YMCA.
Patient wears bangles, signifies marriage and acknowledges herself as married. She
would change her name every time asked; she would also change her designation and
would tell her age as 3 days or few months. She suspects her aunt to be beating her up
and asking her to do household chores. Lately, she had started hearing few people
talking about her, abusing her in hindi, on asking about those people, she would
suspect her cousins. She has totally withdrawn herself from last a week. Her appetite
has reduced. She identifies everyone as 10 or 12 years of age.
PAST HISTORY OF ILLNESS
MEDICAL: Patient has diastolic dysfunction, for which she is taking medication, since
4 years. She is regularly getting her checkups in GTB Hospital, Shahdara, Delhi.
SURGICAL: Patient does not have any significant surgical history.
PSYCHIATRIC: Patient is under treatment since one year. She had same records
and history in 2003 for which, she got admitted in IHBAS. After treatment, she had on
and off symptoms. She followed up well but due to recurrence, she is continuing on
medications {Clozapine}
FAMILY HISTORY
Patient lives with her brother who is married and settled in Delhi. Patient has two sisters
and four brothers. Patient is unmarried. There is no significant family history of medical,
surgical or psychiatric illness.
FAMILY TREE:
Father
Mother
Sister
Sister
Brother
Patient
Brother
Brother
53 years
50 years
47 years
45 years
42 years
39 years
Brother
37 years
PERSONAL HISTORY
BIRTH AND EARLY DEVELOPMENT:
Patient was born by full term normal vaginal delivery in hospital with no pre natal; natal
and post natal complications. Patient gasped and cried soon after birth. She had normal
milestones and development.
CHILDHOOD:
Patient used to do thumb-sucking during childhood. Her relationship with her parents,
friends and teachers was good.
PHYSICAL ILLNESS DURING CHILDHOOD:
There is no significant history of physical illness during childhood.
SCHOOL:
Patient started her schooling at 3 years of age and continued her schooling till 17 years
of age. Her performance in school was average and patient had interest in studies.
Patient had good relationship with her peers as well as teachers.
OCCUPATION:
Patient was unemployed.
SEXUAL HISTORY:
Patient attained puberty at 12 years of age. She is heterosexual and is unmarried.
MARITAL HISTORY:
Patient is unmarried.
SUBSTANCE ABUSE:
Patient does smoking from past 5 years. There is no other history of any other type of
psychoactive substance use.
PRE MORBID PERSONALITY
SOCIAL RELATIONS:
Patient had developed suspicious nature towards her family members and relatives.
INTELLECTUAL ACTIVITIES:
Patient’s hobbies include reading novels, watching T.V.
MOOD:
Patient had stable mood and used to behave in normal pattern.
HABITS:
When patient was not involved in any bad habits like substance abuse, she was well
adjusted in the society.
INVESTIGATIONS
INVESTIGATIONS
RESULT
NORMAL VALUES
Sugar (Random)
94 mg/dl
70 – 120 mg/dl
Bilirubin (Total)
Bilirubin (Direct)
SGOT
SGPT
ALP
Sodium
0.4 mg/dl
0.1 mg/dl
22 U/L
28 U/L
163 U/L
141 mmol/L
0.2 -1.2 mg/dl
0.0 – 0.5 mg/dl
Upto 40 U/L
Upto 38 U/L
100 – 290 U/L
135 – 158 mmol/L
Potassium
Calcium
Phosphorus
4.7 mmol/L
9.2 mg/dl
4.3 mg/dl
3.8 – 5.6 mmol/L
8.1 – 10.4 mg/dl
2.5 – 5.0 mg/dl
Magnesium
0.88 mmol/L
0.66 – 1.07 mmol/L
Urine
Pale yellow,albumin-nil,
epithelial cells- 3to4mpb,
pus cells- 1to2.
MEDICATIONS
DRUG
Tab. Ramipril
DOSE
2.5 mg
ROUTE
Orally
TIME
BD
Tab.Trihexyphenidyl
2 mg
Orally
OD
Tab. BetalocTR
20 mg
Orally
BD
Tab. Risperidone
1 mg
Orally
BD
ACTION
Antipsychotic
Tab. Senorm LA
100 mg
Orally
BD
Tab. Sodium
Valproate
Tab. Amisulphride
600 mg
Orally
BD
1050 mg
Orally
OD
75 mg
Orally
OD
Tab. Aspirin
SUMMARY OF NURSING CARE
DAY 1
Rapport maintained with the patient.
Vital Signs checked.
Intake-Output chart recorded.
Medications given.
Psychiatric History taken.
DAY 2
Vital signs checked.
Intake-output chart recorded.
Medications given.
Mental status examination done.
DAY 3
Vital signs checked.
Intake-output chart recorded.
Medications given.
General conversation done with the patient.
DAY 4
Vital signs checked.
Intake-output chart recorded.
Medications given.
Patient encouraged to play carom.
Anti coagulant
DAY 5
Vital signs checked.
Intake-output chart recorded.
Medications given.
Patient asked to interact with other patients in the ward.
MENTAL STATUS EXAMINATION
PHYSICAL EXAMINATION
Vital signs
Temperature :
Pulse
:
Respiration :
B.P.
:
I.
98.20F
80/mt
26/mt
110/70 mmHg
APPEARANCE
1. GROOMING AND DRESS
Inference:
Patient is wearing appropriate dress which is according to the place and
season. Patient is wearing suit ,sweater and slippers.
2. HYGIENE
Inference:
Hygienic condition of the patient is good. Clothes of patient are clean. Nails of
the patient are clean and are cut properly. Hair are combed.
3. PHYSIQUE
Inference:
Patient is of average built and height.
4. POSTURE
Inference:
Patient is having an open posture. She is sitting upright on a chair.
5. FACIAL EXPRESSIONS
Inference:
Facial expressions of the patient are happy.
6. LEVEL OF EYE CONTACT
Inference:
Patient maintains eye-to-eye contact almost throughout the conversation.
7. RAPPORT
N: Goodmorning Kiran!
P: Goodmorning!
N: Main M.Sc Psychiatric Nursing ki student hoon. Aaj main aapse kuch
sawal karungi, jo aapke ilaj aur meri padai mein mujhe sahayeta karenge.
Kya aap mujhse baat karenge?
P: Haanji!
Inference:
A comfortable rapport is maintained with the patient. She took part in the
conversation well and responded to all the questions asked to her.
II.
MOTOR ACTIVITY
Inference:
Patient’s level of activity is normal.
III.
SPEECH
Inference:
Patient speaks in Hindi and English language. Rate of speech is normal and she
speaks in normal volume. Content of speech is appropriate.
IV.
EMOTIONS
1. MOOD
N: How are you feeling today?
P: I am good today.
Inference:
Patient feels much better. She is in a normal mood.
2. AFFECT
Inference:
Patient’s emotional response is congruent with the speech content.
V.
THOUGHT
1. FORMATION LEVEL
N: What is your name?
P: Chamkili.
N: Who is Kiran?
P: She is my aunt.
Inference:
Formation level of the patient is intact.
2. CONTENT LEVEL
N: Did you ever felt that people are talking about you and they want to harm
you?
P: I used to get this feeling before that some girls are abusing me in hindi and
English language, and my aunt wanted to harm me. But now, I don’t get this
feeling.
N: Are you afraid of anything?
P: No.
N: Where do you stay?
P: In America. I have taken admission here in college.
Inference:
Content level of thought is also impaired, as patient is having delusion of
persecution, delusion of grandiosity and delusion of reference.
3. PROGRESSION LEVEL
N: Is there any thought which you think over and again?
P: No.
Inference:
Progression level of thought is intact.
VI.
PERCEPTION
N: Do you hear any unusual voices which others don’t hear?
P: I told you, it used to happen before.
N: Okay, tell me what is kept near this wall?
P: Broom.
N: Do you see any unusual things or people which others don’t see?
P: No.
Inference:
Perception in patient is intact. Patient is not having any kind of hallucinations
or illusions at present. There is history of auditory hallucinations.
VII. SENSORIUM AND COGNITIVE ABILITY
1. LEVEL OF ALERTNESS/CONSCIOUSNESS
Inference:
Patient is alert as well as conscious. She is actively listening to all the
questions and giving answers.
2. ORIENTATION
N: Who is sitting at your right?
P: Patient Saroj.
N: Which place is this?
P: Mental hospital, IHBAS
N: What is the time right now?
P: 10:15.
Inference:
Patient is fully oriented to place, person and time.
3. MEMORY
a. Immediate memory
N: You have to repeat after me the following figures: 18, 5, 43,
59, 88.
P: 18, 5, 43, 88.
Inference:
Immediate memory of the patient is intact.
b. Recent memory
N: When did you first come to this place?
P: I don’t remember.
Inference:
Recent memory if patient is impaired.
c. Remote memory
N: What is your age?
P: I think 7 years.
Inference:
Patient’s remote memory is impaired.
4. CONCENTRATION AND ATTENTION
N: Solve: 64 + 21 =?
P: 85
Inference:
Patient is having good concentration and attention.
5. INFORMATION AND INTELLIGENCE
N: Who is Prime minister of India?
P: I don’t know
N: What is the capital of India?
P: Don’t know
Inference:
Patients’ information and intelligence is impaired.
6. ABSTRACT THINKING
N: “Pet mein chuhe daudna” what do you understand by this?
P: Bhookh lagna.
Inference:
Abstract thinking of the patient is good.
7. JUDGMENT
a. Social
N: What would you do if you find your neighbours’ house on fire?
P: Call fire extinguisher.
Inference:
Patient has logical social judgment.
b. Personal
N: If you find a 500 rupees note on road, what would you do?
P: I will leave it there.
Inference:
Patient has fair personal judgment.
VIII. INSIGHT
N: Do you think that you are here because you have mental problem?
P: No. I am alright.
Inference:
Insight is absent. Patient has grade I rating score.
IX.
GENERAL ATTITUDE
Inference:
Patient is in normal mood. She is communicating well. She is very co-operative.
X.
SPECIAL POINTS
N: Is your appetite good?
P: yes
N: Do you sleep appropriately?
P: Yes.
N: Do you have any bowel problems?
P: No.
Inference:
Patient’s appetite and sleep patterns are normal.
XI.
PSYCHOSOCIAL FACTORS
1. STRESSORS
N: What do you think, is the reason of your illness?
P: I am fine, I am not sick. (Frowning)
Inference:
Patient didn’t talked about stressors related to his symptoms and got angry
when asked about so.
2. COPING SKILLS
N: What do you do to divert your mind when you feel stressed?
P: I go off to sleep.
Inference:
Patient does not adapt any coping skills.
3. RELATIONSHIPS
N: Do you love your family?
P: Yes, very much.
N: Do you have friends?
P: No!
Inference
Patient does not have any friends but has good relationship with family
members.
4. SOCIO CULTURAL
N: Did you ever feel that society rules are strict?
P: No.
Inference
There are no socio-cultural factors related with the symptoms of the patient.
5. SPIRITUAL
N: Do you believe in God?
P: Yes. I used to go to temple and sit there long.
Inference:
Patient is religious and believes in God.
6. OCCUPATIONAL
N: Were you working anywhere before coming here?
P: Yes, I was working as a lecturer.
Inference:
Patient was unemployed as per file but according to her she was working as a
lecturer.
ABOUT THE DIAGNOSIS
SCHIZOPHRENIA
INTRODUCTION
Schizophrenia is a major mental disorder. It is the most common of the psychotic
disorders. It has been estimated that 50% of all mental hospital beds are occupied by
patients diagnosed as schizophrenic.
The word schizophrenic is derived from a Greek word “schizo” meaning split and
“phrenic” meaning mind.
The term schizophrenia was first coined by a Swiss psychiatrist “Eugen Bleuler”.
Schizophrenia indicates a group of disturbances which sometimes occur in different
combinations and intensities. Hence it is heterogeneous in nature. Schizophrenia has
generally been considered to be of ancient origin.
DEFINITION
Schizophrenia is defined as a functional psychosis characterized by disturbances in
thinking, emotion, violation and perception. The illness occurs in the state of clear
consciousness.
HISTORY AND EVOLUTION
Benedict Augustin Morel in his 1860 “Traite des Maladies Mentales (Treatise
on Mental Illness) first used the term dementia praecox.
Kahlbaum in 1868 characterized a pattern of abnormal motor tension which he
referred to as “Katatonia” or catatonia.
Emil Kraepelin (1896), a German psychiatrist grouped it to a single clinical
entity, which he named as dementia praecox. “Dementia” referred to as
progressive deterioration course of both emotional and cognitive processes,
while “praecox” indicates the early age of onset in previously healthy individuals.
Eugen Bleuler was the first to use the term “Schizophrenia” derived from the
Greek words for “split” and “mind”. He referred to a splitting of the psychic
functions where the personality loses its unity.
He viewed “ the schizophrenias” as being composed of several different entities
but characterized by four principal features: (a) Autism, (b) Ambivalence (c) Associative disturbance (d) Affective change.
Kurt Schineider outlined the first rank of symptoms as the core features which
are somewhat pathognomonic of the disorder.
Second – rank symptoms included other forms of hallucinations, depressive or
euphoric mood changes, emotional blunting, perplexity, sudden delusional ideas.
FIRST RANK SYMPTOMS OF SCHNEIDER
Totally there are 11 first rank symptoms:
1. Voices discussing or arguing: The patient hears voices which discuss or argue
about him, referring to him in their conversation as a third person. Hence also
termed as third person auditory hallucinations.
2. Voices commenting: The patient hears voices describing his activities as they
occur. Also called as running commentary auditory hallucinations.
3. Audible thoughts: Patient hears as if his thoughts are spoken aloud. Also called
as thought echo.
4. Thought broadcast: The experience that one’s thought is broadcast outside so
that others come to know what he/she is thinking.
5. Thought withdrawal: The experience that the thoughts are being withdrawn by
an outside agency or force against their will.
6. Thought insertion: The experience of strange and unwanted thoughts which are
inserted into a person’s mind.
7. Made volitional act: Patient feels that his actions are not his own but are in
response to some external influence.
8. Made impulse: Sudden strong impulses which are experienced as arising from
an alien source.
9. Made feelings: Feelings are experienced as if they are imposed from outside.
10. Somatic passivity: A somatic or physical experience which the patient feels is
the result of some external forces operating on his body, over which he is not
able to exercise any control.
11. Delusional perceptions: The attribution of abnormal significance to a normal
perception without any understandable justification.
EPIDEMIOLOGY
According to the World Mental Health Report 2001, 24 million people worldwide
suffer from schizophrenia.
The point prevalence of schizophrenia is about 0.5 – 1%. Schizophrenia is
prevalent across racial, socio – cultural and national boundaries with a few
exceptions in the prevalence rates in some isolated communities.
The incidence of schizophrenia is currently about 0.5 per 1000. The onset of
schizophrenia occurs usually later in females and often runs a more benign
course, as compared to males.
ETIOLOGY
How or why schizophrenia develops remains a puzzle despite extensive research.
Current views indicates that it is most likely to be a breakdown in the balance
between interacting sets of factors, namely, biological, psychological and social.
I. GENETIC FACTORS
The case for a genetic basis of schizophrenic disorders has been supported by a
variety of studies, including adoptional studies and twin studies. Such studies lend
support to the hypotheses that genetic factors play an important role in the causation
of schizophrenia which probably varies from person to person.
INCIDENCE OF SCHIZOPHRENIA IN SPECIAL POPULATIONS
POPULATION
INCIDENCE (%)
General population.
1.0
Sibling of schizophrenic patient.
8.0
Child with one schizophrenic parent.
12.0
Dizygotic twin of schizophrenic patient.
12.0
Child of two schizophrenic parents.
40.0
Monozygotic twin of schizophrenic patient.
47.0
II. NEUROCHEMICAL FACTORS
DOPAMINE
In its simplest form the dopamine theory proposes that schizophrenia is the
result of a hyperdopaminergic state.
The evidence rests on two major observations - drugs that cause dopamine
release like amphetamine produce schizophrenia like symptoms and
dopamine blocking agents are effective as antipsychotics.
Several dopamine receptors have been identified and post mortem studies
have reported an increased density of D1 and D2 receptor sites in
schizophrenic patients as compared to normal.
Emerging evidence suggests a complex interplay of many other neurotransmitter
systems in schizophrenia such as the following: -
Serotonin (antagonism of 5- HT2 receptor relieves psychiatric symptoms)
Nor – epinephrine (increase in levels)
Glutamate (hypofunction)
GABA (decreased activity)
III. NEURODEVELOPMENTAL FACTORS
Retrospective studies report more obstetric and birth complications
(prematurity, prolonged labour, hypoxia and foetal distress) especially in
early onset cases in males.
Hypoxic damage to the peri-ventricular vasculature may lead to
ventriculomegaly and some brain structures, especially the
hippocampus are highly susceptible to hypoxic injury.
Abnormal neuronal migration during the second trimester of foetal
development has also been reported.
Patient does not have any friends and neither has he had good
relationship with family members.
IV. NEURODEGENERATIVE HYPOTHESIS
Post – mortem and CT scan studies demonstrate diminished cerebral
size and enlargement of the lateral ventricle in schizophrenia. MRI and
PET have shown focal diminution of temporal lobes and possibly
hippocampus.
White matter abnormalities in the corpus callosum have also been
reported.
V. PSYCHOLOGICAL FACTORS
Persons who are withdrawn and have very few social contacts
(introverted personalities or schizoid personalities) are more prone to
develop schizophrenic illness.
Ego boundary disturbance is also considered to be a cause of
schizophrenia. Behaviorists assert that negative reinforcement and
extinction schedules cause schizophrenia.
Most psychoanalyst and behavioural theories suggest that a person’s
relationship to the environment can bring about schizophrenic.
VI. SOCIAL OR ENVIRONMENTAL FACTORS
Children and adults develop schizophrenia because their home environment
is not conducive to normal emotional growth. People who have developed
schizophrenia tend to come from families where there is considerable conflict.
Generally communication between parents and children in such families is
inadequate. There is communication deviance.
Some studies have shown that schizophrenia is more prevalent in areas of
high social mobility and disorganization, especially in members of very low
social class.
CLINICAL FEATURES
Schizophrenia can be grouped as:
1. Schizophrenia with positive symptoms.
2. Schizophrenia with negative symptoms.
Positive symptoms of schizophrenia are:
Delusions
Hallucinations
Bizarre behaviour
Aggression
Agitation
Suspiciousness
Hostility
Excitement
Grandiosity
Conceptual disorganization
Negative symptoms of schizophrenia are:
Apathy
Avolition
Social withdrawl
Diminished emotional responsiveness
Blunted affect
Stereotyped thinking
Artificial gestures / detachment
Lack of spontaneity
There are fundamental groups of signs and symptoms which may occur singly or
together in various clinical patterns. The groups of symptoms are:
1. THOUGHT AND SPEECH DISORDERS
AUTISTIVE THINKING is one of the most important features of schizophrenia.
Here the thinking is governed by private and illogical rules. The patient may
consider two things identical because they have identical predicates or properties
e.g. Lord Rama was a Hindu, I am a Hindu; so I am Lord Rama.
LOOSENING OR ASSOCIATIONS is a pattern of spontaneous speech in which
things said in juxtaposition lack a meaningful relationship or there is idiosyncratic
shifting from one frame of reference to another. The speech is often described as
being ‘disjointing’. If loosening becomes very severe speech becomes virtually
incomprehensible. This is known as incoherence.
THOUGHT BLOCKING is a characteristic feature of schizophrenia although it
can be seen in complex partial seizures (temporal lobe epilepsy0. There is a
sudden interruption of stream of speech before the thought is completed. After a
pause the subject cannot recall what he had meant to say. This may be
associated with thought withdrawal.
NEOLOGISMS are newly formed words or phrases whose derivation cannot be
understood. These are created to express a concept for which the subject has no
dictionary word. E.g. describing stomach as a “food vessel”.
DELUSIONS are false unshakable beliefs which are not in keeping with patient’s
socio – cultural and emotional background.
The commonly seen delusions in schizophrenia include: Delusions of persecution: - Being persecuted against e.g. people are
against me.
Delusions of reference: - being referred to by others e.g. people are
talking about me.
Delusions of grandeur: - exaggerated self importance.
Delusions of control: - being controlled by an external force, known or
unknown.
Somatic or hypochondrical delusions
A schizophrenia patient may show complete mutism (with no speech production),
poverty of speech (decreased speech production), poverty but content conveys
little information).
Echolalia (repetition or echo by patient of the words or phrases of examiner), preseveral (persistent repetition of words beyond their relevance) or vebigeration
(senseless repetitions of same words or phrases over and over again). These are
disorders of verbal behaviour or speech.
2. DISORDER OF PERCEPTION
HALLUCINATIONS are important perceptual disturbances occurring in
schizophrenia. A hallucination is a perception in the absence of an external
stimulus. Hallucinations may be auditory, visual, tactile, olfactory or gustatory.
Auditory hallucinations are the commonest form of hallucination in schizophrenia.
3. DISORDERS OF AFFECT
These include apathy emotional blunting, emotional shallowness, anhedonai
(incapability of experiencing pleasure) and inappropriate emotional response
(emotional response inappropriate to thought).
The incapability of schizophrenic patient to establish emotional contact with other
individuals leads to a lack of rapport with the physician.
4. DISORDERS OF MOTOR BEHAVIOR
There can be a decrease in psychomotor activity (decreased spontaneity, inertia
stupour). Or increase (excitement, aggressiveness, restlessness, agitation).
Mannerisms, grimacing, stereotypes (repetitive strange behavior) decreased self
care and poor grooming are commonly seen in catatonic schizophrenia.
5. NEGATIVE SYMPTOMS
The prominent negative symptoms of schizophrenia include:
- Affective flattering of blunting.
- Attentional impairment
- Avolition – apathy (lack of initiative)
- Annedonia (inability to experience pleasure)
- Asociality (social withdrawl)
- Alogia (lack of speech output)
6. OTHER FEATURES
Decreased functioning in work, social relations and self – care, as
compared to earlier levels.
Loss of ego boundaries (feeling of blurring of boundaries of self with the
environment; uncertainty and perplexity regarding own identity and
hearing of existence).
Multiple somatic symptoms, especially in the early stages.
Insight (into the illness) is absent and judgment is usually poor.
Suicide can occur in schizophrenia due to several reasons which include
the presence of associated depression, command hallucinations
(commanding the patient to commit suicide) impulsive behavior,
anhedonia or return of insight in the illness.
There is usually a marked ‘variability’ in symptomatology over time.
There is no underlying organic cause.
There is no prominent mood disorder of depressive or manic type.
DIAGNOSIS
According to ICD – 10 for the diagnosis of schizophrenia a minimum of 1 very clear
symptom (and usually 2 or more is less clear cut) belonging to any one of the groups
referred to as (a) to (d) below, or symptoms from at least 2 of the groups referred to as
(e) to (h) should have been clearly present for most of the time during a period of 1
month or more (DSM –IV-TR on the other hand requires a minimum period of 6
months). If the duration isles than 1 month then a diagnosis of acute schizophrenia like
psychotic disorder should be made.
a) Thought echo though insertion or withdrawal or thought broadcasting
b) Delusions of control influence of passivity clearly referred to body or limb
movement or specific thoughts actions or sensations; Delusional perception.
c) Hallucination voices giving a running commentary on the patient’s behavior or
discussing the patient among themselves or other types of hallucinatory voices
coming from some part of the body.
d) Persistent delusions of other kinds that are culturally inappropriate and
completely impossible (e.g. being able to control the weather, or being in
communication with client form another world.
e) Persistent hallucinations in any modality, when accompanied by fleeting or half
formed delusions without clear affective content or by persistent over valued ides
or when occurring every day for weeks or months on end.
f) Breaks or interpolations in the train of thought resulting in coherence or irrelevant
speech or neologisms.
g) Catatonic behavior such as excitement posturing or waxy flexibility negativism
mutism and stupor.
h) Negative symptoms such as marked apathy paricity of speech and blunting or
incognivity of emotional responses, usually resulting in social withdrawal and
lowering of social performance; it must be clear that these are not due to
depression or to neuroleptic medication.
i) A significant and consistent change in the overall quality of some aspects of
personal behavior manifest as loss of interest aimlessness idleness a self
absorbed attitude and social withdrawal.
If the patient also meets criteria for manic episode or depressive episode the guidelines
mentioned must have been met before the disturbance of mood developed. The
disorders not diagnosed in the presence of overt brain disease or alcohol or drug
related intoxication, dependence on withdrawal.
CLINICAL TYPES
Schizophrenia can be classified into the following subtypes: 1.
2.
3.
4.
5.
6.
7.
8.
Paranoid
Hebephrenic
Catatonic
Residual
Undifferentiated
Simple
Post schizophrenic depression
Other
PARANOID SCHIZOPHRENIA
It is characterized by the following features:
IN BOOK
Delusions of persecution,
reference, grandeur, control, or
infidelity. The delusions are
usually well systematized (i.e.
thematically well connected
with each other).
The hallucinations usually
have a persecutory or
grandiose content.
Disturbances of affect volition
speech and motor behavior.
IN PATIENT
Delusion of persecution and
reference
Persecutory hallucinations
Absent
The personality deterioration is much less than in other types of schizophrenias.
Patients may be apprehensive (due to delusions and hallucinations) Evasive and
guarded on mental status examination.
The onset of paranoid schizophrenia is usually insidious occurs later in life as compared
to the other types of schizophrenias. The course is usually progressive and complete
recovery usually does not occur.
II. DISORGANIZED OR HEBEPHRENIC SCHIZOPHRENIC
Disorganized schizophrenia is characterized by the following features:
Marked thought disorder, incoherence and severe loosening of associations.
Delusions and hallucinations are fragmentary and changeable.
Emotional disturbances (inappropriate affect blunted affect or senseless
giggling), mannerisms, mirror gazing disinhibited behavior, poor self care and
hygiene, markedly impaired social and occupational functioning, extreme social
withdrawal and other odditon of behavior.
The onset is insidious, usually in the early 2nd decade. The course is progressive
and downhill. Hebephrenic schizophrenia has one of the worst prognosis among
the subtypes of schizophrenia.
III. CATATONIC SCHIZOPHRENIA
It is characterized by marked disturbance of motor behavior. It can present in
three clinical forms
IV.
Excited catatonia
Stuporous catatonia
Catatonia alternating between excitement and stupor.
RESIDUAL SCHIZOPHRENIA
This category should be used when there has been at least one episode of
schizophrenia in the past but without prominent psychotic symptoms at present.
Emotional blunting social withdrawal eccentric behavior illogical thinking and loosening
the associations are common.
UNDIFFERENTIATED SCHIZOPHRENIA
V.
This is a very common type of schizophrenia and is diagnosed either when features of
no subtype are fully present or features of more than one subtype are exhibited though
general criteria for diagnosis of schizophrenia are met.
VI.
SIMPLE SCHIZOPHRENIA
An uncommon disorder, insidious in onset but with progressive development of odd
behavior. Wandering tendency self absorbed idle and aimless activity are present.
PROGNOSIS
GOOD PROGNOSTIC FACTORS
i.
ii.
iii.
iv.
v.
Acute or abrupt onset
Onset > 35 yrs of age
Presence of precipitating stressor
Good pre morbid adjustment
Catatonic subtype (paranoid
subtype has intermediate
prognosis)
vi. Short duration (< 6 months)
vii. Presence of depression
viii. Predominance of positive
symptoms
ix. Family history of mood disorder
x. First episode
xi. Pyknic physique
xii. Female sex
xiii. Good social support
xiv.
Presence of confusion,
perplexity or disorientation in
acute phase
xv. Proper treatment good treatment
compliance and good response
to treatment.
xvi.
Outpatient treatment
xvii. Normal cranial CT scan
POOR PROGNOSTIC FACTORS
i. Insidious onset
ii. Onset < 20 yrs of age
iii. Absence of stressor
iv. Poor pre morbid adjustment
v. Disorganized simple
undifferentiated or chronic
catatonic subtypes
vi. Chronic course (> 2 years)
vii. Absence of depression
viii. Predominance of negative
symptoms
ix. Family history of schizophrenia
x. Past history of schizophrenia
xi. Asthenic physique
xii. Male sex
xiii. Poor social support or unmarried
xiv.
Blurred affect
xv. Absence of treatment or proper
response to treatment
xvi.
xvii.
Institutionalization
Evidence of ventricular
enlargement on cranial CT scan
MANAGEMENT OF SCHIZOPHRENIA
The treatment of schizophrenia can be arduous process for patients, families and
clinicians alike. No cure exists for this tenacious disease. So therapeutic efforts are
aimed at management of symptoms and at social and psychological rehabilitations.
Nevertheless, carefully designed treatment programmes can help many schizophrenics
to regain lost functioning and a greater sense of psychological well being. Long term
supports necessary for most schizophrenics to maximize both their ability to function
and their quality of life.
TREATMENT METHODS OF SCHIZOPHRENIA
I. MEDICAL MANAGEMENT
SOMATIC (PHYSICAL) THERAPIES
1. Antipsychotic medications:
DRUG
(A) TYPICAL OR TRADITIONAL
ANTIPSYCHOTICS
(I) Chlorpromazine
(II) Thioridazine
(III)Trifluoperazine
(IV) Haloperidol
(V) Pimozide
(VI) Triflupromazine
(VII) Prochlorperazine
(VIII) Flupenthixol
(IX) Lolapine
(X) Zudopenthixol
(B) ATYPICAL OR NEWER ANTIPSY
CHOTICS
(I) Clozapine
(II) Resperidone
(III)Olanzapine
(IV) Ziprasidone
ORAL DOSE (mg/day)
300-1500
300-800
15-60
5-100
4-12
100-400
45-150
3-10
25-150
50-150
25-450
2-8
5-20
40-160
2. ECT (Electro – Convulsive Therapy)
Schizophrenia is not a primary indication for ECT. Indications for ECT in schizophrenia
include:
Catatonic stupor
Uncontrolled catatonic excitement
A cute exacerbation not controlled with drugs.
Severe side effect with drugs in presence of untreated schizophrenia
Usually 8-12 ECTs are needed (although up to 18 have been given in proper
responders), given three times a week.
II. PSYCHOLOGICAL TREATMENT
Hospitalization
Psychotherapy
Rehabilitation - social , vocational
Aftercare – day treatment, halfway homes
Education about illness for patients and families
III. NURSING MANAGEMENT OF SCHIZOPHRENIA
PRINCIPLES OF TREATMENT
The patient is initially admitted to a hospital or day hospital for assessment over a
period of time. Out-patient treatment is unsatisfactory, especially in more acute cases
because of the patient’s un-cooperativeness and unpredictability usually during his
medication.
First the nurse should understand the following general principles of management of
schizophrenic patients:
1. Schizophrenia is a chronic illness hence the maintenance of long term treatment
is essential. Total cure may not be possible in most of the cases.
2. What one should aim at is good improvement with regular appropriate treatment.
3. Furthermore in time stress the patient may get a relapse of symptoms inspite of
regular treatment.
4. A schizophrenic patient:
(a) Requires a substantial increase in his own self esteem.
(b) Needs to be live with the real world.
(c) Needs to live in a place where he gets a change to use his own initiative and
judgment.
(d) Needs to have human contacts.
(e) Needs to find a nurse who will be a stable and consistent model. He needs
assurance as to his own personal identity.
(f) Needs patience and fore-bearance.
5. Accept his as he is. That means the nurse should realize the limitations and
weaknesses of the patient.
6. The nurse can minimize her own frustrations by learning not to except the
impossible for him. The patient’s condition can be made to improve but slowly.
Hence it is the duty of the nurse to refrain from rejecting him and accepting him
whole heartedly as he is.
7. Assign small responsibilities to the patient.
8. Engage and support the patient.
9. Supervise him in all his needs.
10. Appreciate him even if he does a small task.
11. Do not – Ignore
- Criticize
- Exert social behavior
- Refrain from over involvement
Secondly a careful assessment should be made to provide diagnosis and to confirm or
to help to formulate a treatment plan.
The nursing management needs may vary from defining reality handling patient control
strengthening the patient’s self image and strengthening the interpersonal relationship.
By giving emotional support, the patient can incorporate positive feelings and feel good
about himself. Thus he will have a strong chance to be able to return to the community
to lead a normal life again.
The nurse should use the skills and techniques appropriate to the specific therapy
NURSING MANAGEMENT OF ACUTELY ILL SCHIZOPHRENICS
Schizophrenic patients may become acutely ill, mostly during the initial stage of
the illness or they may get acute exacerbations during their long term course of
illness.
An acute excitement is more common in catatonic and paranoid types. The main
nursing care is concerned in controlling his impulsive behavior when he hears
voices and responds to them.
He will be also verbally abusive to the staff. It may be difficult to communicate
with someone who is psychotic but it is important to obtain valuable data on how
severe the thought disorder is. These data can be obtained by the nurse who can
establish some degree of trust with the patient. During the acute phase the most
important thing is to meet the physical need of the patient.
Proper nutritional care is essential since the patient may refuse food because of
Suspicion
Indifference (negligence) or too busy or over active that he forgets to take food.
So, it is important to supervise the patient‘s nutrition and if necessary , IV
fluids are given to avoid dehydration.
In the acute phase, schizophrenic patients require drugs mainly by parenteral
form for eg.
o Inj Chlorpromazine 100 mg IM;
o Inj haloperidol 10 to 20 mg IM or IV.
These injections are to be continued periodically till the patient is able to take
oral drugs.
During acute state it is important to look for any injuries sustained during
excitement and injuries sustained during excitement and these should be
attended to. The acutely excited patients should always be approached with the
assistance of other nursing staff or attenders
NURSING CARE OF CHRONIC SCHIZOPHRENICS
Schizophrenia is a disease which is chronic in nature and the chronic patients are
usually withdrawn and have a lot of negative symptoms. So, very important in the
nursing care of chronic schizophrenia is to engage the patient in some useful
activity. To make him lead a beneficial life with the existing potential, he should be
encouraged to do some positive physical work. This is otherwise known as
rehabilitation. It is the role of the nurse to encourage and motivate the patient to
have some occupation or to work in some industrial therapeutic unit. The nurse
should also constantly supervise the patient’s appropriate time.
Following are physical, emotional and therapeutical needs of the chronic patients:
Physical needs
1. Appropriate nutrition-regular diet and supervision of his diet.
2. Taking care of personal hygiene-regular bath and cleanliness.
3. Elimination has to be carefully watched attend to care of the skin because
chronic schizophrenic living in a crowded, closed space are prone to develop
skin problems like scabies, eczema etc.
Emotional needs
1. The withdrawn patient’s main problem is lock of communication and poor
interpersonal relationship because of loss social contact. It is the responsibility of
the nurse to improve his communication and also his social contacts by
encouraging the relatives/friends to visit him often.
2. It is also responsibility of the nurse to give importance to the personal identity of
the patient.
Therapeutic needs
He should be accepted as a human being and should be given responsible work in the
ward set–up. Patiently and positively hear the suggestions from the patient himself in
implementing the routine ward-work. This type of therapeutic environment will minimize
the damage and will improve the quilt of the person. This will again prevent “institutional
neurosis” – a condition which may occur in a long – term mentally ill patient in a mental
hospital set-up.
In the chronic patient need stimulation, occupational and recreational therapies.
In the nursing care should be placed on the five “R”s.
o Reassurance
o Readjustment
o Re-education
o Rehabilitation
o Recreation
NURSING DIAGNOSIS
Disturbed thoughts related to disease process evidenced by suspiciousness.
Altered nutritional pattern related to disease process as evidenced by lack of
appetite.
Altered sleep pattern related to hospitalization as evidenced by restlessness.
Anxiety related to hospitalization.
Knowledge deficit related to disease and its management
GOALS
SHORT TERM GOALS
1) To help the patient to communicate his problem effectively.
2) To improve the sleep pattern.
3) To maintain optimum nutritional pattern.
4) To enhance self concept by being active.
5) To help the patient to accept reality.
6) To help the patient to concentrate on his task and care.
7) To decrease anxiety associated factors while interacting.
LONG TERM GOALS
1)
2)
3)
4)
5)
6)
7)
To reduce his fantasies that may be leading to loosing of thoughts and autism.
To make the patient independent.
To relieve anxiety.
To verbalize the feelings.
To enable the patient lead productive life.
To increase social interaction with others.
To encourage the patient for follow up after discharge