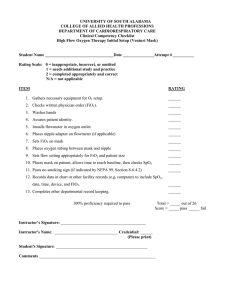
Oxygen Therapy Dr.Indubala Maurya MD,DNB,MNAMS Assistant Professor Dept of Aanesthesia & Critical Care,MGMCRI • Definition • Physiology – O2 content – Hypoxia • Orthobaric Oxygen Therapy – Indication – Device for oxygen therapy • Hyperbaric oxygen therapy • Side effects of Oxygen Therapy Why oxygen is required for survival? Aerobic metabolism oxidative phosphorylation Glucose → CO2 + H2O + 38 ATP Anaerobic metabolism Glucose → Lactic acid + 2 ATP ↓ H+ + lactate – c i s a B s Anoxia No oxygen availability in tissues Hypoxia Lack of oxygen availability in tissues Hypoxemia Lack of oxygen in the blood What is O2 Therapy ? Oxygen therapy is the administration of oxygen at concentrations greater than that in room air to treat or prevent hypoxia. Types of Oxygen Therapy • Giving Oxygen more than 21% at ambient atm pressure • Giving Oxygen more than 21% at high atm pressure ( >1 atm) Orthobaric Hyperbaric Three clinical goals of O2 therapy 1. Treat hypoxia 2. Decrease work of breathing 3. Decrease myocardial Work • FIO2 ( Fraction of O2 in inspired gas) – 0.21 (21%) • PaO2(Partial pressure of Oxygen in arterial blood – 98-100 mmHg ( 5 -6 times of FIO2) • SaO2(saturation of Hb in arterial Blood) – 100% • PvO2 (Partial pressure of Oxygen in Venous blood ) – 40 mmHg • SvO2 (saturation of Hb in Venous Blood) – 75% Oxygen Transport O2 Content in Blood Hemoglobin-Bound O2 • • Oxygen-binding capacity of hemoglobin : 1.34 mL O2 /gm of Hb) SO2 : O2 saturation of Hb Hb X 1.34 X SaO2 Dissolved O2 • • Solubility of oxygen in plasma – solubility coefficient 0.003 mL/100 mL/mm Hg Partial pressure of oxygen (PO2) in blood. 0.003 X PaO2 mmHg Arterial O2 Content (CaO2) Hb X 1.34 X SaO2 0.003 X PaO2 mmHg eg Normal person Hb: 14g SaO2: 98-100% PaO2: 100 mmHg Art. blood = 14g x 1.39 x 100% + 0.3 = 20 ml / 100ml of blood Venous O2 Content (CvO2) Hb X 1.34 X SvO2 0.003 X PvO2 mmHg Normal Person Hb: 14g SvO2: 75 % PvO2: 40 mmhg Ven. blood 14g x 1.39 x 75% + 0.1 = 15ml /100ml of blood Tissue extraction = 5ml/ 100 ml of blood Dissolved O2 in plasma 0.003ml / mm PO2 / 100ml of blood Breathing Air (PaO2 100mm Hg) 0.3ml / 100ml of blood O2 therapy Orthobaric Breathing 100% O2 (PaO2 600mm Hg) 1.8ml / 100ml of blood Hyperbaric Breathing 100% O2 at 3 Atm. Pressure What are the Types of Hypoxia? Types of hypoxia • Hypoxic hypoxia – PaO2↓ • Anaemic hypoxia – O2 content ↓, PaO2 normal • Stagnant hypoxia • Histotoxic hypoxia Hypoxic hypoxia • Causes – O2 poor air, hypoxic gas mixture – High altitude – Hypoventilation – Shunts – Septal defects – Diffusion defects - pneumonia, lobar collapse Anaemic hypoxia • Oxygen carrying capacity of blood is decreased. – Anemia :↓ haemoglobin – Altered haemoglobin • CO poisoning • meth / sulph-haemoglobin Normal Person (breathing 100% O2) (14gm x 1.34ml ) + 1.8ml = 20.5ml (1.8 is 9% 20.5) Anaemic patient (breathing 100% O2) (4gm x 1.34ml )+ 1.8ml = 7.2 ml (1.8 is 25% of 7.2) Stagnant hypoxia • Inadequate tissue perfusion • Generalized: - Hypovolemia - Mitral stenosis - Constrictive pericerditis - Myocardial ischaemia • Localized hypo perfusion: - Arterial obstruction, thrombus, oedema Histotoxic hypoxia • Cells can not utilize the oxygen . • Electron transfer system of cytochrome oxidase is paralysed. • e.g. – cyanide poisoning Benefit of O2 therapy in Hypoxia Hypoxic hypoxia Anaemic hypoxia Stagnant hypoxia Histotoxic hypoxia +++ + + - Clinical presentation of Hypoxia Effects of hypoxia • Acute hypoxia : - Restlessness - Disorientation, confusion - In-coordination, Impaired judgment - Hyperventilation air hunger -Circulatory changes (tachycardiabrady ) • Chronic hypoxia : - fatigue, drowsiness, ↓ work capacity - inattentiveness ,apathy, delayed reaction time Assessment of need • • Presence of clinical indicators Measurement of inadequate oxygen saturations – by invasive or noninvasive methods, • Arterial blood gas • Pulse oximetry Errors in pulse oximetry • • • • • • • • Artificial fingernails Dark pigmentation Electrical interference Intravenous dyes Movement Nail Polish Pulsatile venous system Radiated light How to assess oxygenation ? • • • • Arterial blood gases PaO2 = 100 mmhg Pulse oximetry SpO2=98-100% Oxygen therapy is must whenever PaO2 < 60 mmHg or SpO2 < 90 % FACTORS THAT DETERMINE WHICH SYSTEM TO USE 1. Patient comfort / acceptance 2. The level of FiO2 that is needed 3. The requirement that the FiO2 be controlled within a certain range 4. The level of humidification and /or nebulization 5. Minimal resistance to breathing 6. Efficient & economical use of oxygen Orthobaric Oxygen therapy Oxygen therapy devices Variable performance devices • No capacity – nasal catheters, cannulae • Small capacity – masks • Large capacity – mask with bag Fixed performance devices • HAFOE systems (High air flow oxygen enrichment device » Venti Mask • Anaesthesia circuits • Ventilators Variable performance device FiO2 depends on •O2 flow •Patient factors •Device factors e.g. • Nasal cannula • Simple face mask • Partial rebreathing mask • Non - rebreathing mask Nasal Catheter O2 Flowrate (L/min) Fi O2 1 2 3 4 5 6 0.24 0.28 0.32 0.36 0.40 0.44 Nasal Catheter Merits • • • • Easy to fix Keeps hands free Not much interference with further airway care Useful in both spont. breathing and apnoeic Demerits • • Mucosal irritation (uncomfortable) Gastric dilatation (especially with high flows) Nasal cannula • Simple plastic tubing + prongs Simple Face Mask – ? Simple face mask Simple Face Mask Simple face mask NO YES Simple face mask Placing of mask over the patient’s face increases .the size of the oxygen reservoir beyond the limits of the anatomic reservoir ;therefore a higher FiO2 can be delivered. Simple face mask O2 Flowrate (L/min) Fi O2 5-6 6-7 7-8 0.40 0.50 0.60 • Advantages: – Simple – lightweight, FiO2 upto 0.60 • Disadvantages: – need to remove when speak, eat, drink, vomiting, expectoration of secretions – drying / irritation of eyes – uncomfortable when facial burns / trauma – Application problem when RT in situ Partial Rebreathing mask (polymask) Partial Rebreathing mask (polymask) O2 Flowrate (L/min) Fi O2 6 7 8 0.60 0.70 0.80 Advantages: • FiO2 delivered >0.60 is delivered in mod. to severe hypoxia, • Exhaled oxygen from anatomic dead space is conserved. Disadvantages: • insufficient flow rate may lead to rebreathing of CO2, • Claustrophobia • drying and irritation of eyes Non Rebreathing mask 10 – 15 Ltr/min flow rate – 50-100 O2 conc. Merits • Higher Oxygen Conc. Demerits • Air dilution (if not fitting properly) • Rebreathing (if O2 flow is inadequate) • Interfere with further airway care • Uncomfortable (sweating, spitting) Fixed performance device: Ventimask Simple Face Mask Simple face mask NO YES VENTURI VALVE Venturi valve Color FiO2 O2 Flow Blue White 24% 28% 2 L/min 4 L/min Orange 31% 6 L/min Yellow 35% 8 L/min Red Green 40% 60% 10 L/min 15 L/min Venturi principle Hyperbaric Oxygen therapy Hyperbaric oxygen (HBO) exposure (breathing oxygen at increased ambient pressure, typically 23 atmospheres absolute [ATA]) causes an increase in PaO2. Indication For HBOT • Poisoning : • Carbon monoxide • Infections : – Clostridial myonecrosis • Acute ischemia – Crush injury • Chronic ischemia – Radiation necrosis • Ischemic ulcers – diabetic ulcers O2 Toxicity If conc. of O2 which a patient is getting is not known then the situation is similar to a drug being administered without knowing the dose which can do harm if given more or provide insufficient effect if given less Side Effects • Rentrolental fibroplasia in neonates • Resp system: – Loss of surfactant – Atelactasis – Hypoventilation in COPD pt • CNS: – Convulsion (HBOT) 100% - not more than 12hrs 80% - not more than 24hrs 60% - not more than 36hrs