2. Composition, Formation & Function 3
advertisement

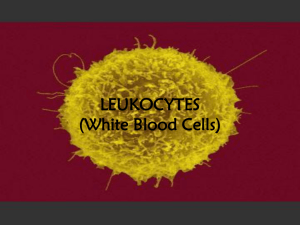
Production of Specific Cell lineages 2. Leucocyte Production (Leucopoiesis) Objectives After completion of lesson, you will be able to Describe the pathways and progenitor cells involved in the derivation of leucocytes from HSC to mature cells Name the five stages of maturation of granulocytes and describe their morphologies Discuss functions of granulocytes Describe morphology of monocytic and lymphocytic series and discuss the process of their production Leucopoiesis Leucopoiesis Leucopoiesis Granulopoiesis takes 10 to 13 days but mature neutrophil remain 1014hrs in circulation before entering to tissue, soon dies There are 3 pools of development of neutrophil: Stem cell, proliferation, maturation CMP: CFU-GEMMs; GMP: CFU-GMP and not distinguished from myeloblasts with light microscope Source: Rodak’s hematology; 5th edition page 151 Leucopoiesis • Myeloblast is the earliest recognizable precursor • Gives rise to promyelocyte, early myelocytes, late myelocytes, and then metamyelocytes • Promyelocyte contain • Abundant dark “azurophilic (primary) granules: overlie nucleus and cytoplasm Myeloblast Promyelocyte Myelocyte (B,N,E) Metamyelocyte (B,N,E) • Primary granules become progressively diluted by the secondary, less conspicuous “neutrophilic” granules that are characteristic of the mature cells. Band (B,N,E) Segmented (B,N,E) Myeloblast Size and shape • 14 – 20 m in diameter • Round or oval in shape Nucleus: Large, round or oval and eccentric • Abundant, unclumped, light purple reticulated chromatin • 2 – 5 light blue-gray nucleoli • Auer rods present Cytoplasm: Stains basophilic (bluish) • Shows a small indistinct, paranuclear, lighter staining halo (golgi apparatus) Type I: have no visible granules: high N:C: 8:1 to 4:1 Type II: contains up to 20 visible primary (azurophilic) granules Constitute ~1- 3% of the total nucleated BM cells Myeloblast… • Auer rods are clumps of azurophilic granular material that form elongated needles seen in the cytoplasm • Mostly seen in malignant cells of the neutrophil lineage Promyelocyte Size and Shape: relatively larger than myeloblast • 16- 25m in diameter and round or oval in shape. Nucleus: Similar to myeloblast nucleus • Round or oval eccentrically located , surrounded by a thin membrane • A Golgi zone may be visible as a paranuclear halo or hof or clearing. • The nuclear chromatin is finely dispersed, and nucleoli may be visible. • Nucleoli (1-3) begin to fade and Obscured by granules • Cytoplasm is more evident: basophilic (pale blue) • N:C ratio 4:1 or 5:1 • Contain abundant dark azurophilic (primary) granules that overlie both nucleus and cytoplasm • These non-specific granules contain peroxidase • Constitutes 1 - 2% BM cells. Myeloblast Vs Promyelocyte Myeloblast Promyelocyte Type I: Meyeloblast • Large number of azure granules and nucleoli Type II: Meyeloblast with few azure granules Neutrophil Myelocyte Last stage capable of cell division First stage to differentiate into eosinophil, basophil, or neutrophil 10-18m in diameter and round. Sometimes divide in to early and late myelocytes Nucleus: • Condensed, oval, slightly indented and eccentric • Chromatin is coarse • Nucleoli are absent Cytoplasm: Light pink • Primary granules production ceases • Secondary granules production begins • N:C ration is about 2:1 6% to 17% of marrow cells Myelocytes Two early myelocyte (similar to promyelocyte except several light areas in their cytoplasm where specific granules are beginning to appear Three late myelocyte (arrow) few primary granules and lavender secondary granules Neutrophil Metamyelocyte (Juvenile cell) Observed in bone marrow or peripheral blood in infections No longer capable of division 14-16m in diameter Nucleus: Major morphologic change • Eccentric, condensed and indented or kidney-bean shaped • Chromatin increasingly clumped • Stains darker • Nucleoli absent Cytoplasm: abundant and pale or pink • Secondary granules are more evident • Tertiary (gelatinase) granules synthesis begins • May contain few primary granules • N:C ratio: 1:1 Constitute 3 - 20% of marrow cells Myelocyte Vs Metamyelocyte Early neutrophil myelocytes Late myelocytes Metamyelocytes Neutrophil band (Stab cell) Youngest granulocyte normally found in peripheral blood and recommended by to be counted with Seg. Neutrophil by CLSI Nucleus is elongated, curved and very clumped • “U” or “C” or “S” shaped or twisted >5% in peripheral blood = abnormal (0-5%) • May be due to infection Cytoplasm is abundant with many fine granules • More secondary granules are evident • Tertiary granules continue to be formed • Secretory granules may begin to be forms • Is pink or colorless • N;C ratio: 1:2 9% to 32% of marrow cells Segmented granulocyte (Seg) Purpose is to engulf and destroy bacteria 50-70% circulate in peripheral blood 7% to 30% of nucleated cells in the bone marrow Capable of diapedesis and phagocytosis Seg to band ratio: 10:1 Nucleus is pinched into segments connected with a fine filament • Chromatin is coarse • 2-5 lobes are observed • Most recommend if a filament is not seen, call it band Abundant pink cytoplasm with secondary granules, do not overlay the nucleus …. Tertiary granules Secretory granules continue to be formed Hypersegmented N. Eosinophil development Eosinophils mature in the same manner as neutrophils. Arise from CMP through interactions of cytokines IL-3, Il-5, CSF-GM and three transcription factors (GATA-1, PU.1 and c/EBP). • IL-5 is critical for growth and survival E. promyelocytes can be identified with cytochemically due to presence of CharcotLeyden crystal protein in their primary granules • Granule are at first bluish and later mature into orange granules E. Myelocyte: identified with light microscope. • Large, pale, reddish-orange secondary granules 1-3% of marrow cells and peripheral blood. (up to 0.4 x 109/L) in peripheral blood Mature Eosinophil Size and shape: 10-16m in diameter, slightly larger than neutrophil Nucleus: Eccentric and usually bilobed Rarely single- or tri-lobed and contains dense chromatin masses. Eosinophils with more than two nuclear lobes are seen in • Vitamin B12 and folic acid deficiency • In allergic disorders Cytoplasm: • Densely filled with orange-pink specific granules. • The granules are • Uniform in size • Large and individualized, Do not cover the nucleus • Highly metabolic and contain histamine and other substances Basophilic Granulocyte and Precursors Early maturation of the basophilic is similar to that of the neutrophil Mature Basophil Size: Somewhat smaller than eosinophils • Measuring 10-14m in diameter Nucleus: Indented giving rise to an S pattern. • It is difficult to see the nucleus • It contains less chromatin and is • Masked by the cytoplasmic granules. Cytoplasm: Pale blue to pale pink • contains granules that often overlie the nucleus but do not fill the cytoplasm as completely as the eosinophils granules do • Basophil granules are water soluble, may be washed if BF washed too much • 0-2% in peripheral blood and <1% marrow cells Name the Granulocyte precursors Band Promyelocyte Myelocyte Development of Monocytes and Macrophages Cells of the macrophage system are formed from the progenitor cells in the bone marrow. These cells are derived from the CFU-GM, which can differentiate into either the CFU-M and develop into a monocyte or macrophage or CFU-G and develop into a segmented neutrophil. The chromatin is clumped, although the clumps are smaller and more elongated than in neutrophils. The shape of the nucleus of the monocyte may be round or oval, but it is frequently convoluted or twisted. Functionally, monocytes and macrophages have phagocytosis as their major role, although they also have regulatory and secretory functions. Monoblast Monoblast cannot be differentiated from the myeloblast on morphologic or histochemical criteria Size: 15-20m in diameter. Nucleus: Round or oval and at times notched and indented • The chromatin is delicate blue to purple stippling with small regular, pink, pale or blue parachromatin areas • Pale blue, large and round nucleoli (3-5 in #) Cytoplasm: Relatively large in amount • May contains a few azurophilic granules (rare) • Stains pale blue or gray • Auer bodies may be observed • The cytoplasm filling the nucleus indentation is lighter in color than the surrounding cytoplasm Promonocyte Is the earliest monocytic cell recognizable as belonging to the monocytic series is capable of mitotic division Its product, the mature monocyte, is only capable of maturation into a macrophage Size: 12-20m in diameter. Nucleus: Large, ovoid to round, convoluted, grooved, and indented • The chromatin forms a loose open network containing a few larger clumps • There may be two or more nucleoli. Cytoplasm: • sparse, gray-blue, contains fine azurophilic granules N:C ratio is about 3:1 Monocyte Size: 12-20m in diameter. Nucleus: Pale, Eccentric or central and has different shapes • Brainy convolutions to lobulated and S shaped (often lobulated), kidney shaped, twisted • The chromatin network consists of fine, pale, loose, linear threads producing small areas of thickening at their junctions • No nucleolus is seen Cytoplasm: • Abundant, opaque, gray-blue with moderate granules • unevenly stained and may be vacuolated • N:C ratio 1:1 Monoblast Monocyte maturation 1 Promonocyte Monocyte 2 Monocyte Tissue Monocyte/Macrophage 3 Formation of lymphocytes (Lymphopoiesis) Lymphopoiesis Lymphocytes are derived from committed stem cells that originate from pluripotent stem cell. Early lymphoid cells further differentiates into B. & T.lymphocytes. B LYMPHOCYTES Developed in bone marrow or fetal liver Maturation culminates in migration to other lymphoid organs and tissues (e.g. spleen, gut, liver , tonsils, lymph nodes) They proliferate and mature into antibody forming cells. T lymphocytes Differentiation and maturation take place in thymus, These thymocytes loose their antigenic surface molecules and finally mature into • Helper/ effector T lymphocytes and • Suppressor T lymphocytes Lymphocyte Maturation 1 Lymphoblast: • Round or oval nucleus with 1 or 2 nucleoli, 2 3 Prolymphocyte: Mature Lymph: • Oval or slightly • Round or oval nucleus, indented nucleus with 0may have an 1 nucleoli indentation (cleft). • Delicate chromatin pattern • cytoplasm is medium blue and may have a darkerblue border, • No granules are present. • Slightly condensed chromatin • Nucleoli are not visible. • Clumped chromatin, • Cytoplasm is medium blue with a thin, darker blue rim. • Cytoplasm is light sky blue and very scanty. Plasma Cells Plasma cells Little capacity to undergo mitosis. ultimate stage for synthesis and secretion of antibodies • Main purpose is to make antibodies • B cell becomes a plasma cell • Plasmablast->proplasmacell->plasmacyte • Mature plasma cell • Nucleus is round and eccentric with clumped chromatin • Cytoplasm is dark blue with pale perinuclear zone • Cornflower blue Production of Specific Cell lineages 3. Thrombocyte Production (Thrombopoiesis) Formation of platelets (Thrombopoiesis) Platelets are produced in the bone marrow by fragmentation of the cytoplasm of megakaryocytes Stimulated by Thrombopoietin The megakaryoblast produces megakaryocytes, distinctive large cell that are the source of circulating platelets. Megakaryocyte development takes place in a unique manner. • These cells undergo endomitosis, whereby the cell does not divide; instead, it becomes larger and the nucleus becomes polyploid, as much as 64 N. Thrombopoiesis Three stages of maturation of megakaryocytes 1. Basophilic stage, megakaryocyte is small, has diploid nucleus and abundant basophilic cytoplasm. 2. Granular stage, here the nucleus is more polyploid, cytoplasm is more eosinophilic and granular 3. Mature stage, megakaryocyte is very large, abundance of granular cytoplasm. It undergoes shedding to form platelets (thrombopoiesis) stages of megakaryocyte progenitors • Reaches its full ploidy level by the end of the MK-II stage. • At the MK-III stage, the megakaryocyte is easily recognized at 10× magnification Platelet maturation Bone Marrow Megakaryocytic Platelet Thrombocyte maturation Giant Platelet Any questions? Lymphopoiesis The precursor of the lymphocyte is believed to be the primitive mulipotential stem cell that also gives rise to the pluirpotenital myeloid stem cell for the granulocytic, erythyroid, and megakaryocytic cell lines Lymphoid precursor cells travel to specific sites There, they differentiate into cells capable of either expressing cell-mediated immune responses or secreting immunoglobulins The influence for the former type of differentiation in humans is the thymus gland; the resulting cells are defined as thymus-dependent lymphocytes, or T cells. Lymphopoiesis cont’d The site of the formation of lymphocytes with the potential to differentiate into antibody-producing cells has not been identified in humans, although it may be the tonsils or bone marrow In chickens it is the bursa of Fabricius, and for this reason these bursa-dependent lymphocytes are called B cells B cells ultimately differentiate into morphologically distinct, antibody-producing cells called plasma cells. Lymphocytes and Precursors Lymphoblast Size: 10-20m in diameter. Nucleus: Central, round or oval the chromatin has a stippled pattern The nuclear membrane is distinct and one or two pink nucleoli are present and are usually well outlined Cytoplasm: Non-granular and sky blue may have a deep blue border It forms a thin perinuclear ring. N:C ratio 4:1 Prolymphocyte Size: 9-18m in diameter. Nucleus: Oval but slightly indented may show a faint nucleolus The chromatin is slightly condensed into a mosaic pattern. Cytoplasm: Gray blue, mostly blue at the edges may show a few azurophilic granules and vacuoles Lymphocytes There are two varieties the morphologic difference lies mainly in the amount of cytoplasm Small Lymphocyte Size: 7-18m in diameter. Nucleus: round or oval to kidney shaped occupies nine tenths of the cell diameter The chromatin is dense and clumped A poorly defined nucleolus may be seen. Lymphocytes cont’d Cytoplasm: It is basophilic and forms a narrow rim around the nucleus or at times a thin blue line only with few azurophilic red granules N:C ratio is 4:1 Distinguishing characteristics of a small lymphocyte: clumping of chromatin around the nuclear membrane may help to distinguish this from a nucleated red cell Large Lymphocyte Size: 9-12m in diameter Nucleus: the dense, oval, or slightly indented nucleus is centrally or eccentricity located Its chromatin is dense and clumped. Cytoplasm: Abundant gray to pale blue, unevenly stained, and streaked at times A few azurophilic granules are contained in 30-60% of the cells. These are large granular lymphocytes (LGLs). Large Lymphocyte cont’d N:C ratio is 4:1 Distinguishing characteristics: Cytoplasm is mor abundant with tendency for azurophilic granules Formation of platelets (Thrombopoiesis) Platelets are produced in the bone marrow by fragmentation of the cytoplasm of megakaryocytes The precursor of the megakaryocyte-the megakaryoblast-arises by a process of differentiation for the hemopoietic stem cell The megakaryoblast produces megakaryocytes, distinctive large cell that are the source of circulating platelets. Megakaryocyte development takes place in a unique manner. The nuclear DNA of megakaryoblasts and early megakaryocytes reduplicates without cell division, a process known as endomitosis. Thrombopoiesis cont’d As a result, a mature megakaryocytes has a polyploidy nucleus, that is, multiple nuclei each containing a full complement of DNA and originating from the same locust within the cell. Mature megakaryocytes are 8 n to 36 n. The final stage of platelet production occurs when the mature megakaryocyte sends cytoplasmic projections into the marrow sinusoids and sheds platelets into the circulation. Thrombopoiesis cont’d It takes approximately 5 days from a megakaryoblast to become a mature megakaryocyte. Each megakaryocyte produces from 1000 to 8000 platelets. The platelet normally survives form 7 to 10 days in the peripheral blood. Morphology of the Platelets and their Precursors Megakaryoblast Size: ranges from 10-30m in diameter. The cell is smaller than its mature forms but larger than all other blast cells. Nucleus: the single, large, oval or indented nucleus has a loose chromatin structure and a delicate nuclear membrane Multi-lobulated nuclei also occur representing a polyploid stage. Several pale blue nucleoli are difficult to see The parachromatin is pink. Megakaryoblast cont’d Cytoplasm: the cytoplasm forms a scanty, bluish, patchy, irregular ring around the nucleus The periphery shows cytoplasmic projections and pseudopodia like structures. The immediate perinuclear zone is lighter than the periphery. Promegakaryocyte Size: ranges from 20-50m in diameter. It is larger than the megakaryoblast in the process of maturation it reaches the size of the stage III cell. Nucleus: large, indented and poly-lobulated. the chromatin appears to have coarse heavily stained strands and may show clumping The total number of nucleoli is decreased and they are more difficult to see than in the blast cell. The chromatin is thin and fine. Promegakaryocyte cont’d Cytoplasm: intensely basophilic filled with increasing numbers of azurophilic granules radiating from the golgi apparatus toward the periphery sparing a thin peripheral ring that remains blue in color. Granular Megakaryocyte The majority of the megakaryocytes of a bone marrow aspirate are in stage III which is characterized by progressive nuclear condensation and indentation and the beginning of platelet formation within the cytoplasm. Size: ranges from 30-100m in diameter is the largest cell found in the bone marrow. Cytoplasm: a large amount of polychromatic cytoplasm produces blunt, smooth, pseudopodia-like projections that contain aggregates of azurophilic granules surrounded by pale halos These structures give rise to platelets at the periphery of the megakaryocytes. Platelets Size: varies from 1-4m in diameter. Nucleus: no nucleus is present. In Wright - Giemsa stained films, platelets appear as small, bright azure, rounded or elongated bodies with a delicately granular structure. Review Questions/Summary 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. What is hemopoiesis and how is the process regulated? What are the hemopoietic tissues during fetal life, in infancy, in childhood and in adulthood? What are the effects of the hormone erythropoietin on red cell development and maturation. Describe the microenvironment briefly. Explain megaloblastic erythropoiesis. Describe general Characteristic feature of cells during maturation (nuclear , cytoplasmic, etc ) State the composition of blood. State the main functions of blood. List main characteristics of blood. What is extramedulary hemopoiesis and when does it occur? Summary