Hemostasis, Coagulation & Blood Transfusion Presentation
advertisement

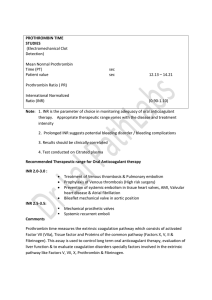
DR. spiro A. Tawil Consultant Surgeon F.R.C.S.I. What is haemostasis? Platelet Normal blood flow Vasoconstriction 1. Vasoconstriction Primary haemostasis Loose platelet plug Collagen 1. Vasoconstriction 2. Primary haemostasis Primary haemostasis – adhesion of platelets 1. Adhesion The role of platelets Primary haemostasis – activation of platelets Activated Platelet Secondary haemostasis – coagulation and formation of fibrin Coagulation system Coagulation factors Factor I (Fibrinogen) Factor II (Prothrombin) Factor III (Tissue Factor) Factor IV (Ca++) Some new factors involved in coagulatio Factor V Protein C Factor VII Protein S Factor VIII Thrombomodulin Factor IX Antithrombin Factor X Tissue Factor Pathway Inhibitor Factor XI Carboxypeptidase U Factor XII Thrombin Activatable Fibrinolysis Inhibitor Factor XIII Prothrombin time (PT) 1.Add tissue factor 2.Add Ca++ Initiation and start the clock Amplification Tissue factor Factor XIa Factor VIIa / Tissue factor Factor IXa Factor X Factor Xa Prothrombin Fibrinogen Factor Xa Thrombin Fibrin Thrombus formation Normal range: 12 to 20 s Activated partial thromboplastin time (aPTT) Initiation Amplification Tissue factor Factor XIa 1. Contact activation Factor VIIa / Tissue factor Factor X Prothrombin Fibrinogen Factor Xa Factor IXa 2. Add Ca++ and start the clock Factor Xa Thrombin Fibrin Thrombus formation Normal range: 30 to 40 s Thrombin time (TT) Initiation Amplification Tissue factor Factor XIa Factor VIIa / Tissue factor Factor IXa Factor X Factor Xa Prothrombin Fibrinogen Factor Xa Thrombin Fibrin 1. Add a known amount of thrombin Thrombus formation Normal range: 15 to 25 s NovoSev en Human/porci ne factor VIII FEIBA Initiation phase of coagulation Tissue factor FVIIa FX Prothrombin FXa TFPI/FXa Tissue factor pathway inhibitor (TFPI) Fibrinogen Thrombin Fibrin Primary platelet plug Fibrin bound thrombin Amplification phase of coagulation Tenase complex FIXa FVIIIa FIXa FVIIIa Platelet membrane FX FV and FVIII FXa Activation of more platelets Generation of more fibrin Prothrombinase complex Clot stabilisation FXa FVa FXIIIa Prothrombin Antithrombin Thrombin FXIII The protein C system and termination of coagulation Tenase complex FIXa FVIIIa FX FVIIIa FXa inactive APC Prothrombinase complex FVa inactive FXa FVa Protein C Thrombin Thrombomodulin Prothrombin Thrombi n Thrombin Fibrinogen Fibrin Fibrinolysis Thrombin has a central role in blood coagulation The coagulation system is a complex interaction of several enzymes, cofactors and inhibitors in which thrombin is the “conductor of the orchestra” as it is involved in coagulation, anticoagulation and fibrinolysis Thrombin Cleaves fibrinogen to fibrin Induces platelet aggregation Stimulates its own generation Downregulates its own formation Fibrinogen binding to thrombin Fibrinogen binding site D E Active site D Fibrinogen Fibrinopeptides Laboratory tests of haemostasis Test Purpose Normal range Platelet count No of platelets in the blood 150-300 x 109/l blood Bleeding time Functional platelet aggregation <12 min Activated partial thromboplastin time (aPTT) Activity of all coagulation factors in the amplification loop 35-45 s* Prothrombin time (PT) Activity of vitamin K-dependent10-20 s* coagulation factors International normalised Calculated from PT as the ratio 1.0 ratio (INR) between PT in patient plasma and reference sample Thrombin time (TT) Activity of thrombin 10-30 s* Ecarin clotting time (ECT) Effect of direct thrombin inhibitors 20-40 s** Fibrin degradation products (FDPs) Fibrinolytic system <10 mg/l plasma D-dimers Fibrinolytic system <0.5 mg/l plasma*** * Depends on the amount of thrombin added to the sample **Depends on the amount of ecarin added to the sample *** May also be expressed as fibrinogen equivalent units (FEU) FRESH BLOOD COMPONENTS WHOLE BLOOD RED BLOOD CELL IN ADDITIVE SOLUTION PLATELETS FRESH FROZEN PLASMA (FFP) CRYOPRECIPITATE PLASMA FRACTION HUMAN ALBUMIN PROTHROMBIN COMPLEX CONCENTRATES IMMUNOGLOBULIN PREPARATION (90% Ig G) RED CELL SEROLOGY ABO ANTIGENS RHESUS ANTIGENS (Rh) OTHER RED CELL ANTIGENS Kell antigens Duffy antigens Kidd antigens PRETRANFUSION TESTING TYPE AND SCREEN CROSS- MATCHING EMERGENCY REQUIREMENTS FOR BLOOD ORDERING BLOOD IN AN EMERGENCY Immediately take samples for cross-matching Inform the blood bank of the emergency,the volume of blood required,and where blood is to be delivered One individual should take responsibility for all communications with the blood bank, and should ensure that it is clear who will be responsible for the blood delivery In cases of exsanguinations use emergency group O Rh(D)-negetive blood. Do not ask for cross-matched blood in an emergency BLOOD ADMINISTRATION Before administrating blood 2 staff members (one of whom must be a doctor or trained staff nurse) must check the patient’s full identity the blood pack,compatability label and report form the blood pack for signs of haemolysis or leakage from the pack. Any discrepancies means that the blood must not be transfused and that the laboratory must be informed TRANSFUSION ERRORS Almost all deaths from transfusion reaction are due to ABO incompatility Errors in patient identification at the time of blood sampling or administration are the major cause When taking the initial blood sample check the patient’s identity verbally and on the wrist identification band label the sample fully before leaving the bedside make sure that the blood request form is clearly and accurately completed. ADVERSE EFFECTS OF TRANSFUSION HYPOCALACAEMIA HYPERKALEMIA & HYPOKALAMIA HYPOTHERMIA ADULT RESPIARATORY DISTRESS SYNDROME (ARDS) AUTOLOGOUS TRANSFUSION PREOPERATIVE DONATION ISOVOLAEMIC HAEMODILUTION CELL SALVAGE TRANSFUSION REQUIREMENTS IN SPECIAL SURGICAL SETTINGS MASSIVE TRANSFUSION THROMBOCYTOPENIA COAGULATION FACTOR DEFICIENCY MASSIVE BLOOD TRANSFUSION This is defined as the transfusion of the equivalent of the the circulating blood volume within a 24hour period (in practice 10-20 units in an adult) Common identifications for massive blood transfusion are major trauma, gastrointestinal bleeding and obstetrics complications. Major problems associated with massive blood transfusion include underlying coagulopathy thrombocytopenia lack of coagulation factor 5 & 8 hyperkalaemia hypothermia METHODS TO REDUCE THE NEED FOR BLOOD TRANSFUSION ACUTE VOLUME REPLACEMENT HYDROXYETHYL STARCH (HES) DEXRAN 70 DEXTRAN40 UREA-BRIDGED GELATIN (HAEMACCEL MECHANISM FOR REDUCED BLOOD USE IN SURGERY PREOPERATIVE * Surgery elective – Correct the Haemoglobin level. Stop drugs that interfere Haemostasis INTRAOPERATIVE Posture Use of Vasoconstrictors Use of tourniquets Use of anti-fibrinolytic drugs eg Aprotinin Using Fibrin Sealant POST OPERATIVELY Blood can be salvaged from drains into collection devices that permit reinfusion Decision to transfuse post operatively should depend * Age of the patient * Ability to tolerate lower levels of anaemia * Rate & amount of continuing blood loss Clinical Scenarios A 65 year old man has undergone a left nephrectomy 3 days ago. He required 3 units of packed cells intra-operatively. He looks pale and is dyspnoeic but his vital signs and urinary output are satisfactory. You check his FBP. Hb is 7 PCV 0.28. What would you do? A 34 year old man presents in the resuscitation room of the A/E department. He is anxious, short of breath, sweating and his BP is 80 systolic, Pulse 120. There is a stab wound on the right side of the chest. A chest drain was inserted by the SHO and 1000mls of blood drained immediately. What would you do with respect to his fluid A 57 year old man needs a left hemicolectomy for carcinoma. He declares himself to be a Jehovah’s witness and refuses a blood transfusion under any circumstances. What will you do? Case 1 It is Friday at 4:40pm Lab calls You are patient is being preped for urgent surgery. INR 6.5 What to do ? Vitamin K Warfarin affects factors II,VII,IX and X These are the vitamin K dependent factors Can reverse warfarin effect Takes time Available forms ? Reversing INR wityh vitamin K Depends on clinical scenario Complete reversal Partial reversal (too high INR) IV or oral forms prefered For complete reversal 5-10 mg IV q12h for 2 doses will reverse completely in 36-48 hours. 1-2 mg will decrease INR to therapeutic Level within 12-24 hrs Case 2 You are on call for ENT and are asked to see an 18 year old girl with refractory nosebleed. The nose is packed and bleeding does not stop. You notice a few bruises Blood sent off to lab. The lab calls at 6:00 Pm with a “critical” platelet count of 10 What is likely diagnosis What to do ? ITP Immune thromboctopenic purpura What is needed for diagnosis Bone marrow examination Anti platelet antibodies When isolated and very low ITP is most likely diagnosis Could be a part of another disease but not likely (SLE , inf mono) Does it require hospitalization ? ITP continued If mucosal bleeding platelets are less than 6 Needs action Steroids IVIG Anti D What about splenectomy New treatments Rituximab TPO agonists Case3 A 48 year old woman appears in emerg with jaundice of 3 weeks duration Exam – jaundice - some RUQ pain an palpation Blood tests CBC Hgb 125, WBC 7.6 Plat 345 INR 2.6 ptt 42 What is likely diagnosis What to Do ? Vitamin K deficiency Obstructive jaundice Malabsorption of Vit K dependent factors Older people at risk Post surgery at risk Treatment Oral or IV Vitamin K Case 4 A 54 year old male comes to office feeling unwell. Exam Mild jaundice, some telangectasis on skin Mod ascites. CBC - Hgb 110 WBC 2.5 plat 68 INR 1.6 Ptt 41 TT 25 What is likely diagnosis ? Hepatic dysfunction - Cirrhosis Liver makes and degrades Coagulation is affected by decreased production and impaired degradation of activated factors Chronic DIC Splenomegaly Trearment only if bleeding Liver transplant Case 5 18 year old male scheduled for tonsillectomy History of easy bleeding Exam normal no bruises CBC normal INR 1.1 PTT 45 What is likely diagnosis ? How to diagnose ? Hemophilia X linked bleeding disorders characterized by spontaneous development of large hematomes in deep tissues. May lead to joint bleeding, or into other closed structures Joint cavity bleeding leads to deformed joints bleeding may be spontaneous or asssociated with mild or moderate injury Hemophilia types Hemophilia A absent or decreased factor VIII Hemophilia B lack of factor IX similar in symptoms to Hemophilia A Hemophilia A is 10 times more common than hemophilia B Case 6 17 year old girl with mennorhagia History of easy bruising Possible history of easy bruising CBC normal INR 1.1 PTT 32 (2 sec prolonged) What is diagnosis How to diagnose ? Treatment ? Von Willebrand’s Disease Most frequent inherited bleeding disorder 1% - 1/100 of western population less severe than hemophilia Disease results from a decrease or absence of Von Willebrand factor for platelet adhesion Affects primary hemostasis Von Willebrand’s Disease and Factor VIII VW factor produced in megakaryocytes and endothelial cells Coded on chromosome 12 Autosomal dominant inheritance Large molecule, and multimeric Monomers undergoglycolisation and multimerization before secretion Different multimer size = disease