Cochrane RS He et al 2016
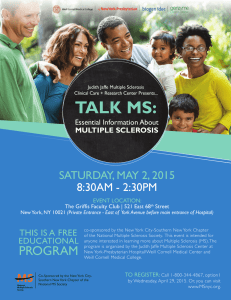
advertisement

Cochrane Database of Systematic Reviews
Teriflunomide for multiple sclerosis (Review)
He D, Zhang C, Zhao X, Zhang Y, Dai Q, Li Y, Chu L
He D, Zhang C, Zhao X, Zhang Y, Dai Q, Li Y, Chu L.
Teriflunomide for multiple sclerosis.
Cochrane Database of Systematic Reviews 2016, Issue 3. Art. No.: CD009882.
DOI: 10.1002/14651858.CD009882.pub3.
www.cochranelibrary.com
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
TABLE OF CONTENTS
HEADER . . . . . . . . . . . . . . . . . . . .
ABSTRACT . . . . . . . . . . . . . . . . . . .
PLAIN LANGUAGE SUMMARY . . . . . . . . . . .
SUMMARY OF FINDINGS FOR THE MAIN COMPARISON
BACKGROUND . . . . . . . . . . . . . . . . .
OBJECTIVES . . . . . . . . . . . . . . . . . .
METHODS . . . . . . . . . . . . . . . . . . .
RESULTS . . . . . . . . . . . . . . . . . . . .
Figure 1.
. . . . . . . . . . . . . . . . . .
Figure 2.
. . . . . . . . . . . . . . . . . .
Figure 3.
. . . . . . . . . . . . . . . . . .
DISCUSSION . . . . . . . . . . . . . . . . . .
AUTHORS’ CONCLUSIONS . . . . . . . . . . . .
ACKNOWLEDGEMENTS
. . . . . . . . . . . . .
REFERENCES . . . . . . . . . . . . . . . . . .
CHARACTERISTICS OF STUDIES . . . . . . . . . .
DATA AND ANALYSES . . . . . . . . . . . . . . .
APPENDICES . . . . . . . . . . . . . . . . . .
WHAT’S NEW . . . . . . . . . . . . . . . . . .
CONTRIBUTIONS OF AUTHORS . . . . . . . . . .
DECLARATIONS OF INTEREST . . . . . . . . . . .
SOURCES OF SUPPORT . . . . . . . . . . . . . .
DIFFERENCES BETWEEN PROTOCOL AND REVIEW . .
INDEX TERMS
. . . . . . . . . . . . . . . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1
1
2
4
11
11
12
15
16
18
19
24
26
26
26
30
47
47
47
47
47
48
48
48
i
[Intervention Review]
Teriflunomide for multiple sclerosis
Dian He1 , Chao Zhang2 , Xia Zhao3 , Yifan Zhang1 , Qingqing Dai1 , Yuan Li1 , Lan Chu1
1 Department
of Neurology, Affiliated Hospital of Guizhou Medical University, Guiyang, China. 2 Department of Internal Medicine,
Jinan No. 6 People’s Hospital, Jinan, China. 3 Department of Nursing, Jinan No. 6 People’s Hospital, Jinan, China
Contact address: Lan Chu, Department of Neurology, Affiliated Hospital of Guizhou Medical University, No. 28, Gui Yi Street,
Guiyang, Guizhou Province, 550004, China. chulan8999@yeah.net.
Editorial group: Cochrane Multiple Sclerosis and Rare Diseases of the CNS Group.
Publication status and date: New search for studies and content updated (conclusions changed), published in Issue 3, 2016.
Review content assessed as up-to-date: 7 November 2015.
Citation: He D, Zhang C, Zhao X, Zhang Y, Dai Q, Li Y, Chu L. Teriflunomide for multiple sclerosis. Cochrane Database of Systematic
Reviews 2016, Issue 3. Art. No.: CD009882. DOI: 10.1002/14651858.CD009882.pub3.
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
ABSTRACT
Background
This is an update of the Cochrane review “Teriflunomide for multiple sclerosis” (first published in The Cochrane Library 2012, Issue
12).
Multiple sclerosis (MS) is a chronic immune-mediated disease of the central nervous system. It is clinically characterized by recurrent
relapses or progression, or both, often leading to severe neurological disability and a serious decline in quality of life. Disease-modifying
therapies (DMTs) for MS aim to prevent occurrence of relapses and disability progression. Teriflunomide is a pyrimidine synthesis
inhibitor approved by both the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) as a DMT for
adults with relapsing-remitting MS (RRMS).
Objectives
To assess the absolute and comparative effectiveness and safety of teriflunomide as monotherapy or combination therapy versus placebo or
other disease-modifying drugs (DMDs) (interferon beta (IFNβ), glatiramer acetate, natalizumab, mitoxantrone, fingolimod, dimethyl
fumarate, alemtuzumab) for modifying the disease course in people with MS.
Search methods
We searched the Cochrane Multiple Sclerosis and Rare Diseases of the CNS Group Specialised Trials Register (30 September 2015). We
checked reference lists of published reviews and retrieved articles and searched reports (2004 to September 2015) from the MS societies
in Europe and America. We also communicated with investigators participating in trials of teriflunomide and the pharmaceutical
company, Sanofi-Aventis.
Selection criteria
We included randomized, controlled, parallel-group clinical trials with a length of follow-up of one year or greater evaluating teriflunomide, as monotherapy or combination therapy, versus placebo or other approved DMDs for people with MS without restrictions
regarding dose, administration frequency and duration of treatment.
Data collection and analysis
We used the standard methodological procedures of Cochrane. Two review authors independently assessed trial quality and extracted
data. Disagreements were discussed and resolved by consensus among the review authors. We contacted the principal investigators of
included studies for additional data or confirmation of data.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
1
Main results
Five studies involving 3231 people evaluated the efficacy and safety of teriflunomide 7 mg and 14 mg, alone or with add-on IFNβ,
versus placebo or IFNβ-1a for adults with relapsing forms of MS and an entry Expanded Disability Status Scale score of less than 5.5.
Overall, there were obvious clinical heterogeneities due to diversities in study designs or interventions and methodological heterogeneities
across studies. All studies had a high risk of detection bias for relapse assessment and a high risk of bias due to conflicts of interest.
Among them, three studies additionally had a high risk of attrition bias due to a high dropout rate and two studies had an unclear
risk of attrition bias. The studies of combination therapy with IFNβ (650 participants) and the study with IFNβ-1a as controls (324
participants) also had a high risk for performance bias and a lack of power due to the limited sample.
Two studies evaluated the benefit and the safety of teriflunomide as monotherapy versus placebo over a period of one year (1169
participants) or two years (1088 participants). A meta-analysis was not conducted. Compared to placebo, administration of teriflunomide
at a dose of 7 mg/day or 14 mg/day as monotherapy reduced the number of participants with at least one relapse over one year (risk
ratio (RR) 0.72, 95% confidence interval (CI) 0.59 to 0.87, P value = 0.001 with 7 mg/day and RR 0.60, 95% CI 0.48 to 0.75, P value
< 0.00001 with 14 mg/day) or two years (RR 0.85, 95% CI 0.74 to 0.98, P value = 0.03 with 7 mg/day and RR 0.80, 95% CI 0.69
to 0.93, P value = 0.004 with 14 days). Only teriflunomide at a dose of 14 mg/day reduced the number of participants with disability
progression over one year (RR 0.55, 95% CI 0.36 to 0.84, P value = 0.006) or two years (RR 0.74, 95% CI 0.56 to 0.96, P value =
0.02). When taking the effect of drop-outs into consideration, the likely-case scenario analyses still showed a benefit in reducing the
number of participants with at least one relapse, but not for the number of participants with disability progression. Both doses also
reduced the annualized relapse rate and the number of gadolinium-enhancing T1-weighted lesions over two years. Quality of evidence
for relapse outcomes at one year or at two years was low, while for disability progression at one year or at two years was very low.
When compared to IFNβ-1a, teriflunomide at a dose of 14 mg/day had a similar efficacy to IFNβ-1a in reducing the proportion
of participants with at least one relapse over one year, while teriflunomide at a dose of 7 mg/day was inferior to IFNβ-1a (RR 1.52,
95% CI 0.87 to 2.67, P value = 0.14; 215 participants with 14 mg/day and RR 2.74, 95% CI 1.66 to 4.53, P value < 0.0001; 213
participants with 7 mg/day). However, the quality of evidence was very low.
In terms of safety profile, the most common adverse events associated with teriflunomide were diarrhoea, nausea, hair thinning, elevated
alanine aminotransferase, neutropenia and lymphopenia. These adverse events had a dose-related effects and rarely led to treatment
discontinuation.
Authors’ conclusions
There was low-quality evidence to support that teriflunomide at a dose of 7 mg/day or 14 mg/day as monotherapy reduces both the
number of participants with at least one relapse and the annualized relapse rate over one year or two years of treatment in comparison
with placebo. Only teriflunomide at a dose of 14 mg/day reduced the number of participants with disability progression and delayed
the progression of disability over one year or two years, but the quality of the evidence was very low. The quality of available data was
too low to evaluate the benefit teriflunomide as monotherapy versus IFNβ-1a or as combination therapy with IFNβ. The common
adverse effects were diarrhoea, nausea, hair thinning, elevated alanine aminotransferase, neutropenia and lymphopenia. These adverse
effects were mostly mild-to-moderate in severity, but had a dose-related effect. New studies of high quality and longer follow-up are
needed to evaluate the comparative benefit of teriflunomide on these outcomes and the safety in comparison with other DMTs.
PLAIN LANGUAGE SUMMARY
Teriflunomide modifies the disease course in people with multiple sclerosis
Background
Teriflunomide was first used in rheumatoid arthritis, and is known to possess both anti-proliferative (inhibiting cell growth) and antiinflammatory (counteracting a local response to cellular injury) actions. In 2012, its use was approved for these characteristics by the US
Food and Drug Administration for people with relapsing (with recurrent exacerbations of neurological symptoms) forms of multiple
sclerosis (MS) and in 2013 also by the European Medicines Agency.
Objectives
To assess the effectiveness and safety of two different doses of teriflunomide, alone or in combination with other medicines, for modifying
the course of MS in people with the relapsing forms, with or without progression.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
2
Study characteristics
The review authors considered the effectiveness of teriflunomide mainly in terms of the number of participants with at least one relapse,
the number of people with disability progression, the annualized rate of relapse (number of relapses per participant-year) and the time
to disability progression. They evaluated safety as the number of participants with side effects, number of participants with serious
side effects, and number of participants who withdrew or dropped out from the study because of side effects at one year or two years.
Among the pertinent literature, five studies met the inclusion criteria. They involved 3231 participants and evaluated the effectiveness
and safety of teriflunomide alone or with another medicine called interferon-β (IFNβ), versus placebo (a pretend medicine) or IFNβ1a. The evidence is current to September 2015.
Key results
The authors found low-quality evidence that both doses of teriflunomide reduced the occurrence of relapses after one year or two years
of treatment, while there is very low-quality evidence showing that the medicine prevented disability progression at one year or two
years. High-dose rather than low-dose teriflunomide had a similar efficacy to IFNβ-1a in reducing relapse at one year, but the quality
of evidence was very low. As far as safety was concerned, the most commonly reported side effects were diarrhoea (frequent, loose
stools), nausea (feeling sick), hair thinning, neutropenia (low levels of white blood cells called neutrophils, which fight off infection)
and lymphopenia (low levels of white blood cells called lymphocytes, which fight off infection). In general, these side effects are mild
to moderate, and do not usually lead to treatment being stopped, but higher dose is more prone to cause these side effects.
Quality of evidence
The low/very low quality of the results is mainly due to the inadequate blinding of relapse assessment (assessors were aware of which
treatment the person had received), the high dropout rate (people left the trial), disability progression confirmed in less than six months,
the low number of participants, and the different length of treatments within the studies. The duration of the studies is a key point
for a lifetime disease with chances of chronic treatments as MS, also suggesting the need of studies with a longer period of monitoring
(follow-up). The five studies included in this review were sponsored by pharmaceutical companies, and this is known as a potential
source of conflict of interest and thus of bias.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
3
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
S U M M A R Y O F F I N D I N G S F O R T H E M A I N C O M P A R I S O N [Explanation]
Teriflunomide compared to placebo for multiple sclerosis
Patient or population: people with relapsing multiple sclerosis
Settings: US, Austria, France, Canada, Germany, UK, Sweden, Netherlands, Turkey, Poland, Chile, Ukraine, China, Italy, Australia, etc.
Intervention: teriflunomide at a dose of 14 mg orally once daily
Comparison: placebo
Outcomes
Illustrative comparative risks* (95% CI)
Assumed risk
Corresponding risk
Placebo
Teriflunomide
Proportion of partici- 394 per 1000
pants with at least 1 relapse at 1 year
Follow-up: 1 year
237 per 1000
(189 to 296)
Relative effect
(95% CI)
No of Participants
(studies)
Quality of the evidence
(GRADE)
Comments
RR 0.60
(0.48 to 0.75)
761
(1 study)
⊕⊕
lowa
This outcome was considered low, because we
considered there were
very serious limitation in
study design and execution. The bias that influenced the validity of the
results for this outcome
included: the high risks
of bias due to unblinded
assessments for relapse
and conflicts of interest
(sensitivity analysis according to a likely-case
scenario showed a robustness for the results
of this outcome, we considered that the high attrition bias did not influence
the robustness of the re-
4
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
sults on relapse). Therefore, we downgraded the
quality of evidence for this
outcome by 2 levels
The proportion of partic- 545 per 1000
ipants with at least 1 relapse at 2 years
Follow-up: 2 years
436 per 1000
(376 to 507)
RR 0.80
(0.69 to 0.93)
722
(1 study)
⊕⊕
lowb
This outcome was considered low, because we
considered there were
very serious limitation in
study design and execution. The bias that influenced the validity of the
results for this outcome
included: the high risks
of bias due to unblinded
assessments for relapse
and conflicts of interest.
(Sensitivity analysis according to a likely-case
scenario showed a robustness for the results of
this outcome, we considered that the unclear attrition bias did not influence
the robustness of the results on relapse.) Therefore, we downgraded the
quality of evidence for this
outcome by 2 levels
The proportion of partici- 142 per 1000
pants with disability progression at 1 year
Follow-up: 1 year
78 per 1000
(51 to 119)
RR 0.55
(0.36 to 0.84)
761
(1 study)
⊕
very lowc,e
This outcome was considered very low based on
the following reasons:
• we considered
there were very serious
limitation in study design
and execution. The bias
5
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
that influenced the
validity of the results for
this outcome included:
the high risks of bias due
to the high attrition bias
and conflicts of interest.
Sensitivity analysis
according to a likelycase scenario showed an
unsteadiness for the
results of this outcome,
we considered that the
high attrition bias
influenced the
robustness of the results
on progression disability.
Therefore, we
downgraded the quality
of evidence for this
outcome by 2 levels
• This outcome was
an indirect outcome
because disability
progression was
confirmed at 3 months of
follow-up. We had
serious doubts about
directness. Therefore, we
downgraded the quality
of evidence for this
outcome by 1 level
The proportion of partici- 273 per 1000
pants with disability progression at 2 years
Follow-up: 2 years
202 per 1000
(153 to 262)
RR 0.74
(0.56 to 0.96)
722
(1 study)
⊕
very lowd,e
This outcome was considered very low based on
the following reasons:
• We considered
there were very serious
6
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
limitation in study design
and execution. The bias
that influenced the
validity of the results for
this outcome included:
the high risks of bias due
to unclear attrition bias
and conflicts of interest.
Sensitivity analysis
according to a likelycase scenario showed an
unsteadiness for the
results of this outcome,
we considered that the
unclear attrition bias
influenced the
robustness of the results
on progression disability.
Therefore, we
downgraded the quality
of evidence for this
outcome by 2 levels
• This outcome was
an indirect outcome
because disability
progression was
confirmed at 3 months of
follow-up. We had
serious doubts about
directness. Therefore, we
downgraded the quality
of evidence for this
outcome by 1 level
7
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
The proportion of partic- 89 per 1000
ipants with diarrhoea at
2 years
Follow-up: 2 years
179 per 1000
(120 to 267)
RR 2.01
(1.35 to 3.00)
718
(1 study)
⊕⊕⊕
moderatef
The follow-up periods were diverse in
Confavreux 2014 and
O’Connor 2011 (at least
48 weeks (Confavreux
2014) and 108 weeks
(O’Connor 2011)). Treatment duration of participants in Confavreux 2014
was variable, ending 48
weeks after the last participant was included (a
maximum treatment duration of 173 weeks). Actually, the data on adverse
events in Confavreux
2014 were not at 2 years.
There was a heterogeneity in follow-up period between the studies. Therefore, we did not combine the data on adverse
events in Confavreux
2014 and O’Connor 2011
The proportion of partic- 33 per 1000
ipants with hair thinning
at 2 years
Follow-up: 2 years
131 per 1000
(71 to 243)
RR 3.94
(2.13 to 7.30)
718
(1 study)
⊕⊕⊕
moderatef
The follow-up periods were diverse in
Confavreux 2014 and
O’Connor 2011 (at least
48 weeks (Confavreux
2014) and 108 weeks
(O’Connor 2011)). Treatment duration of participants in Confavreux 2014
was variable, ending 48
weeks after the last par-
8
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
ticipant was included (a
maximum treatment duration of 173 weeks). Actually, the data on adverse
events in Confavreux
2014 were not at 2 years.
There was a heterogeneity in follow-up period between the studies. Therefore, we did not combine the data on adverse
events in Confavreux
2014 and O’Connor 2011
The proportion of partic- 67 per 1000
ipants with elevated ALT
levels at 2 years
Follow-up: 2 years
143 per 1000
(90 to 226)
RR 2.14
(1.35 to 3.39)
718
(1 study)
⊕⊕⊕
moderatef
The follow-up periods were diverse in
Confavreux 2014 and
O’Connor 2011 (at least
48 weeks (Confavreux
2014) and 108 weeks
(O’Connor 2011)). Treatment duration of participants in Confavreux 2014
was variable, ending 48
weeks after the last participant was included (a
maximum treatment duration of 173 weeks). Actually, the data on adverse
events in Confavreux
2014 were not at 2 years.
There was a heterogeneity in follow-up period between the studies. Therefore, we did not combine the data on adverse
events in Confavreux
2014 and O’Connor 2011
9
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
*The basis for assumed risk is the placebo group risk. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative
effect of the intervention (and its 95% CI).
ALT: alanine aminotransferase; CI: confidence interval; RR: risk ratio.
The assumed risk was defined as placebo group risk because only one study was evaluated
GRADE Working Group grades of evidence
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: We are very uncertain about the estimate.
a
High risks of bias existed in Confavreux 2014 due to unblinded assessments for relapse and conflicts of interest.
High risks of bias existed in O’Connor 2011 due to unblinded assessments for relapse and conflicts of interest.
c High risks of bias existed in Confavreux 2014 due to effects of the high attrition bias on progression disability and conflicts of interest.
d High risk of bias existed in O’Connor 2011 due to effects of the unclear attrition bias on progression disability and conflicts of interest.
e Serious indirectness existed in Confavreux 2014 or in O’Connor 2011 because disability progression was confirmed at 3 months of
follow-up.
f High risk of bias existed in O’Connor 2011 due to an unclear attrition bias and conflicts of interest.
b
10
BACKGROUND
Description of the condition
Multiple sclerosis (MS) is a chronic immune-mediated disease of
the central nervous system. It is pathologically characterized by
inflammation, demyelination, and axonal and neuronal loss. Clinically it is characterized by recurrent relapses or progression, or
both, typically striking adults during the primary productive time
of their lives and ultimately leading to severe neurological disability.
In 1996, the clinical course of MS was characterized as relapsingremitting, primary progressive, secondary progressive or progressive relapsing. Initially, more than 80% of individuals with MS
experience a relapsing-remitting disease course (RRMS) characterized by clinical exacerbations of neurological symptoms followed
by complete or incomplete remission (Lublin 1996). After 10 to
20 years, or median age of 39.1 years, about half of them gradually accumulate irreversible neurological deficits with or without
clinical relapses (Confavreux 2006), which is known as secondary
progressive MS (SPMS). Another 10% to 20% of individuals with
MS are diagnosed with primary progressive MS (PPMS), clinically
defined as a disease course without any clinical attacks or remission
from onset (Lublin 1996). A significantly rarer form is progressive
relapsing MS (PRMS), which initially presents as PPMS, however,
during the course of the disease, these individuals develop true
neurological exacerbations (Tullman 2004). In 2013, the clinical
course of MS was re-defined. In the new revisions, clinically isolated syndrome was added, and PRMS was eliminated, from the
clinical course descriptions. All forms of MS should be further
subcategorized as either active or non-active. Active MS is defined
as the occurrence of clinical relapse or the presence of new T2
or gadolinium-enhancing lesions over a specified period of time,
preferably at least one year. An additional subcategory for people with progressive MS differentiates between people who have
shown signs of disability progression over a given time period and
people who have remained stable (Lublin 2014a; Lublin 2014b).
MS causes a major socioeconomic burden, both for the individual and for society. Increased economic and quality of life
(QoL) burden is associated with disease progression and relapses
(Karampampa 2012; O’Connell 2014; Parisé 2013). From a person’s perspective, an MS relapse is associated with a significant increase in economic costs as well as a decline in health-related quality of life (HRQoL) and functional ability (Oleen-Burkey 2012).
Effective treatment that reduces relapse frequency and prevents
progression could have an impact both on costs and HRQoL, and
may help to reduce the social burden of MS (Karampampa 2012).
Description of the intervention
Teriflunomide, the active metabolite of leflunomide, is known
to possess both anti-proliferative and anti-inflammatory actions.
Data from human trials of leflunomide in rheumatoid arthritis
showed that teriflunomide demonstrated linear pharmacokinetics
over a dose range of 5 mg/day to 25 mg/day. The mean plasma
half-life is 15 days to 18 days and teriflunomide is extensively
(greater than 99%) protein bound and exhibits linear protein binding at therapeutic concentrations. Clearance is via biliary and renal routes so administration of cholestyramine can be used to facilitate rapid elimination of teriflunomide from the circulation
(Tallantyre 2008). Teriflunomide decreases disease severity and reduces inflammation, demyelination and axonal loss in a dose-dependent manner in the Dark Agouti rat model of experimental
autoimmune encephalomyelitis (EAE) (Merrill 2009). Teriflunomide (Aubagio®) was approved by the US Food and Drug Administration (FDA) in 2012 for people with relapsing forms of
MS (7 mg or 14 mg orally once daily). In 2013, it was approved
by the European Medicines Agency (EMA) for adults with RRMS
(the recommended dose: 14 mg once a day).
How the intervention might work
Teriflunomide has an ability to non-competitively and reversibly
inhibit the mitochondrial enzyme dihydro-orotate dehydrogenase
(DHODH), a key cellular enzyme involved in the de novo synthesis of pyrimidine (Bruneau 1998; Greene 1995). By inhibiting
DHODH and diminishing deoxyribonucleic acid (DNA) synthesis, teriflunomide has a cytostatic effect on proliferating B and
T lymphocytes (Cherwinski 1995). Teriflunomide also inhibits
protein tyrosinekinase activity (Xu 1996), resulting in the reduction of T-cell proliferation, T-cell production of interferon gamma
(IFN-γ ) and interleukin 2 (IL2), as well as B-cell immunoglobulin
(Ig)G1 production and inhibition of nuclear factor B (NF B)
(Manna 1999; Siemasko 1998; Xu 1995). In addition, teriflunomide diminishes the ability of antigen-presenting cells (APC) to
activate T cells and for stimulated T cells to activate monocytes
in vitro (Zeyda 2005), and inhibits interleukin 1 beta, matrix
metalloproteinases (Deage 1998), and cyclo-oxygenase-2 activity
(Hamilton 1999). In EAE, teriflunomide reduces activation of
myelin basic protein (MBP)-specific T cells then reduces the production of IFN-γ and chemotaxis (Korn 2004).
Why it is important to do this review
This is an update of the Cochrane review “Teriflunomide for multiple sclerosis” (first published in The Cochrane Library 2012 Issue
12).
OBJECTIVES
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
11
To assess the absolute and comparative effectiveness and safety
of teriflunomide as monotherapy or combination therapy versus placebo or other disease-modifying drugs (DMDs) (interferon
beta (IFNβ), glatiramer acetate, natalizumab, mitoxantrone, fingolimod, dimethyl fumarate, alemtuzumab) for modifying the disease course in people with MS.
METHODS
Criteria for considering studies for this review
Types of studies
All randomized, controlled, parallel-group clinical trials (RCTs)
evaluating teriflunomide, as monotherapy or combination therapy, versus placebo or any approved DMDs for people with MS.
We excluded trials with a length of follow-up shorter than one
year.
or improving symptoms and signs not associated with fever or
infection that occurred at least 30 days after the onset of a
preceding relapse and lasted more than 24 hours. The relapse
should be verified by the examining neurologist within seven
days after its occurrence and be accompanied by an increase of at
least half a point in the EDSS score or at least one point in two
functional systems (excluding change in sphincteric or cerebral
functions).
• The proportion of participants with disability progression
as assessed by the EDSS (Kurtzke 1983) at one year or two years.
Disability progression was defined as an increase in the EDSS
score of at least 1.0 point in participants with a baseline score of
1.0 or higher or an increase of at least 1.5 points in participants
with a baseline score of 0, with the increased score sustained for
six months. We used the data where disability progression was
confirmed in less than six months, however, we downgraded the
study for indirectness of evidence when we performed the
GRADE assessment.
Safety
Types of participants
We included participants aged 18 years or older with definite diagnoses of MS according to Poser’s (Poser 1983) or Mc Donald’s
(McDonald 2001; Polman 2005; Polman 2011) criteria, any clinical phenotypes categorized according to the classification of Lublin
and Reingold (Lublin 1996), and an Expanded Disability Status
Scale (EDSS) scores of 6.0 or lower.
Types of interventions
Experimental intervention
Treatment with teriflunomide orally, as monotherapy or combination therapy, without restrictions regarding dose, administration
frequency and duration of treatment.
Control intervention
• The number of participants with adverse events (AEs),
number of participants with serious adverse events (SAEs), and
number of participants who withdrew or dropped out from the
study because of AEs at one year or two years.
Secondary outcomes
• The annualized relapse rate at one year or two years, defined
as the mean number of confirmed relapses per participant
adjusting for the duration of follow-up to annualize it.
• The number of gadolinium-enhancing T1-weighted lesions
at one year or two years. Lesions that persisted for more than
four weeks were counted more than once.
• The time to disability progression at one year or two years.
• Changes in T1 hypointensity or magnetization transfer
ratio of lesion damage at one year or two years.
Placebo or an approved DMDs.
Types of outcome measures
Primary outcomes
• Mean change in HRQoL. The following scales were
accepted: 36-item Short Form (SF-36) scores (Ware 1992),
Multiple Sclerosis Quality of Life (MSQoL-54) questionnaire
scores (Vickrey 1995), Multiple Sclerosis Quality of Life
Inventory (MSQLI) (Fischer 1999), or Functional Assessment of
Multiple Sclerosis (FAMS) (Cella 1996) at one year or two years.
Efficacy
• The proportion of participants with at least one relapse at
one year or two years. Confirmed relapse was defined as the
occurrence of new symptoms or worsening of previously stable
Search methods for identification of studies
We applied no language restrictions to the search.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
12
Electronic searches
The Trials Search Co-ordinator searched the Cochrane Multiple
Sclerosis and Rare Diseases of the CNS Group Specialised Trials
Register (30 September 2015), which, among other sources, contains trials from:
• the Cochrane Central Register of Controlled Trials
(CENTRAL) (2015 Issue 9);
• MEDLINE (PubMed) (1966 to 30 September 2015);
• EMBASE (EMBASE.com) (1974 to 30 September 2015);
• Cumulative Index to Nursing and Allied Health Literature
(CINAHL) (EBSCOhost) (1981 to 30 September 2015);
• Latin American and Caribbean Health Science Information
Database (LILACS) (Bireme) (1982 to 30 September 2015);
• Clinical trial registries (clinicaltrials.gov);
• World Health Organization (WHO) International Clinical
Trials Registry Portal (apps.who.int/trialsearch/).
Information on the Trials Register and details of search strategies
used to identify trials is in the ’Specialised Register’ section within
the Cochrane Multiple Sclerosis and Rare Diseases of the CNS
Group’s module.
Appendix 1 shows the keywords used to search for trials for this
review.
Searching other resources
We checked the reference lists of published reviews and retrieved articles for additional trials. We searched reports (2004
to September 2015) from the MS Societies (National Multiple Sclerosis Society (United States, United Kingdom)) (
www.nationalmssociety.org) and the Congress of the European
Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS (www.ectrims.eu) and Americas Committee for
Treatment and Research in Multiple Sclerosis (ACTRIMS (
www.actrims.org)). We communicated with investigators participating in trials of teriflunomide. We also contacted the
Sanofi-Aventis company in an effort to identify further studies (
en.sanofi.com).
not meet the inclusion criteria in the Characteristics of excluded
studies table with the reasons for exclusion. We resolved any disagreement regarding inclusion by discussion or by referral to a
third review author (LC) if necessary.
Data extraction and management
Two review authors (DH and YZ) independently extracted information and data from the selected trials using standardized forms,
including information about eligibility criteria, methods
(study design, total study duration, sequence generation, allocation sequence concealment, blinding and other concerns about
bias), participants (total number, setting, diagnostic criteria, age,
sex and country), interventions (total number of intervention
groups and specific intervention) and outcomes (outcomes and
time points, outcome definition and unit of measurement), results
(number of participants allocated to each intervention group, sample size, missing participants and summary data for each intervention group) and funding source. Where the standard deviation was
not reported, we calculated it from the standard error, confidence
interval, t values or P values. We contacted the principal investigators of included studies to request additional data or confirmation
of methodological aspects of the study. We discussed and resolved
disagreements by consensus among the review authors.
Assessment of risk of bias in included studies
We assessed the risk of bias of the included studies using the
Cochrane Handbook for Systematic Reviews of Interventions (Higgins
2011). Two review authors (DH and YZ) independently evaluated each study using the ’Risk of bias’ tool under the domains of
sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete
outcome data, selective outcome and other biases. We judged a
study to have a high risk of attrition bias if it had a dropout rate
higher than 20%, or the reasons for drop-outs were not balanced
across intervention groups. We judged a study to be at high risk
of bias if at least one of the seven domains was rated at high risk
of bias. Conversely, we judged a study to be at low risk of bias if
all key domains were rated at low risk of bias, unless one or more
of the domains was reported at unclear risk of bias, in which case
we judged the study to be at unclear risk of bias.
Data collection and analysis
Measures of treatment effect
Selection of studies
Two review authors (DH and YZ) independently screened titles
and abstracts of the citations retrieved by the literature search for
inclusion or exclusion. We obtained the available full texts of potentially relevant studies for further assessment. We independently
evaluated the eligibility of these studies (on the basis of information available in the published data) and listed papers that did
We calculated the treatment effects of interventions based on the
available data in the original studies using the Review Manager
5 analysis software (RevMan 2015). For dichotomous outcomes,
such as the proportion of participants with at least one relapse,
disability worsening and at least one AE, we used the risk ratio
(RR) as the measure of treatment effect. We also calculated the
risk difference (RD) (also called the absolute risk reduction) and
the number needed to treat for an additional beneficial outcome
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
13
(NNTB) or the number needed to treat for an additional harmful
outcome (NNTH) (NNTB = 1/RD). We used the rate ratio as the
measure of treatment effect for count data, such as the numbers
of relapses and new gadolinium-enhancing T1-weighted lesions.
Changes in T1 hypointensity and magnetization transfer ratio of
lesion damage were continuous outcomes and we used the mean
difference (MD) as the measure of treatment effect. We treated the
data on QoL scales as continuous because they were longer ordinal rating scales and had a reasonably large number of categories.
Therefore, we used the MD for trials that used the same rating
scale. The time to disability progression was a time-to-event outcome, we summarized such data using methods of survival analysis and expressed the treatment effect as a hazard ratio (HR). We
calculated 95% CIs for each treatment effect.
order to identify heterogeneity across studies. An I2 value higher
than 30% may indicate moderate heterogeneity (Higgins 2011).
Assessment of reporting biases
The trials included in this review did not permit an assessment
of publication bias. If we include a sufficient number of RCTs in
meta-analysis (10 or more RCTs) in future updates, we will examine potential publication bias using a funnel plot. For continuous
outcomes, we will use the standard error as the vertical axis and
MDs as the horizontal axis in funnel plots. For dichotomous outcomes, we will plot RRs on a logarithmic scale as the horizontal
axis and use the standard error as the vertical axis.
Data synthesis
Unit of analysis issues
Most RCTs on teriflunomide for MS are multi-arm studies with
two experimental intervention groups (7 mg/day or 14 mg/day of
teriflunomide) and a common control group, and involving repeated observations on participants. In future updates, where data
are presented for each of the groups to which participants were
randomized, we will create two pair-wise comparisons of intervention groups to conduct independent meta-analyses (high-dose
dimethyl fumarate group versus placebo group; low-dose dimethyl
fumarate group versus placebo group). Where outcomes are measured at multiple time points, we will define time frames to reflect
short-term (one year) and long-term (two years) follow-up.
Dealing with missing data
We did not conduct meta-analyses because of the clinical and
methodological diversity across the included studies. We included
intention-to-treat data. We analysed the available data when the
missing data can be reasonably assumed to be missing at random,
but for data not missing at random, we performed sensitivity analyses according to a likely-case scenario analysis, in which we assumed that both participants who dropped out both in the experimental group and in the control group had poor outcomes. We
addressed the potential impact of missing data on the findings of
the review in the Discussion section.
Assessment of heterogeneity
We assessed clinical heterogeneity by examining the characteristics
of the studies and the similarity between the types of participants,
interventions and outcomes. We also evaluated the variability in
study design and risk of bias (methodological heterogeneity). We
found obvious clinical and methodological heterogeneity across
the included studies. If further data become available, we will evaluate statistical heterogeneity where clinical and methodological
heterogeneity are not obvious across the included studies. When
pooling trials in meta-analyses, we will calculate the I2 statistic in
We could not combine the outcome data because of the different
study designs and interventions across studies; instead, we gave a
descriptive summary of the results in the original studies. If we
consider studies to be sufficiently clinically and methodologically
similar in future updates, we will conduct formal meta-analysis
using Review Manager 5 software (RevMan 2015). We will conduct separate analyses in which higher-dose teriflunomide (14 mg
once daily) and lower-dose teriflunomide (7 mg once daily) are
compared to placebo. We will examine one-year and two-year outcomes separately. If we consider that all studies in a meta-analysis are likely to be estimating the same underlying treatment effect, then we will use a fixed-effect model, otherwise we will use
a random-effects model for meta-analysis. For dichotomous outcomes, we will use the Mantel-Haenszel method (Greenland 1985;
Mantel 1959). For continuous outcomes, we will use the inversevariance method (DerSimonian 1986).
Subgroup analysis and investigation of heterogeneity
We could not carry out subgroup analysis because of the lack of
data, but in future updates and if further data become available,
we intend to undertake subgroup analyses according to:
• different types of MS (e.g. people with RRMS or people
with progressive MS);
• baseline EDSS scores (e.g. 3.5 or lower, between 3.5 and 6);
• different duration of MS (e.g. five years, more than five
years);
• risk of bias in included studies.
Sensitivity analysis
We undertook sensitivity analyses to assess the robustness of our
review results. We conducted sensitivity analyses according to a
likely-case scenario in order to assess the effect of study withdrawal
on the primary outcomes. Based on the intention-to-treat principle, we included all randomly assigned participants (including
those who did not receive study treatment) into sensitivity analysis.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
14
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded
studies and Characteristics of ongoing studies.
Results of the search
In total, the search strategy retrieved 193 records after we removed
duplicates. After screening of titles and abstracts, we selected
seven studies reported in 42 articles provisionally and obtained
the full papers for further assessment for eligibility. We excluded
two studies (reported in 14 articles) due to a length of follow-up
shorter than one year or participants without a diagnosis of definite
MS (Miller 2014; O’Connor 2006). Five studies met the inclusion criteria (Confavreux 2014; Freedman 2012; NCT01252355;
O’Connor 2011; Vermersch 2014) (reported in 28 articles, the results of NCT01252355 were published on clinicaltrials.gov). We
included the trials that we classified in ongoing studies in previous versions of this review (NCT00751881 and NCT01252355)
in the current review (Confavreux 2014; NCT01252355). See
Figure 1.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
15
Figure 1. Study flow diagram.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
16
Included studies
The review included five studies involving 3231 people (
Confavreux 2014; Freedman 2012; NCT01252355; O’Connor
2011; Vermersch 2014). Among them, two studies evaluated the
efficacy and safety of teriflunomide 7 mg/day or 14 mg/day versus
placebo for 2257 adults with relapsing forms of MS (Confavreux
2014; O’Connor 2011). Two studies primarily evaluated the safety and tolerability of teriflunomide 7 mg/day or 14 mg/day with
add-on IFNβ versus placebo in 650 people with relapsing MS
(Freedman 2012; NCT01252355). One study evaluated the efficacy, safety and tolerability of teriflunomide 7 mg/day or 14 mg/
day in comparison to IFNβ-1a in 324 people with relapsing MS
(Vermersch 2014).
Characteristics of the interventions
Participants in Confavreux 2014 and O’Connor 2011 received
oral teriflunomide 7 mg once daily or oral teriflunomide 14 mg
once daily or a matching placebo for at least 48 weeks (core treatment period: 48 weeks to 152 weeks, a maximum of 173 weeks)
(Confavreux 2014) and 108 weeks (O’Connor 2011). Participants
in Freedman 2012 and NCT01252355 received oral administration of 7 mg/day of teriflunomide added to IFNβ, 14 mg/day of
teriflunomide added to IFNβ or matching placebo added to IFNβ
for 48 weeks (Freedman 2012) and at least 24 weeks (a maximum
of 108 weeks) (NCT01252355). Participants in Vermersch 2014
received oral teriflunomide 7 mg once daily or oral teriflunomide
14 mg once daily or IFNβ-1a 44 µg by subcutaneous injection
three times per week for at least 48 weeks (a maximum of 115
weeks).
Characteristics of the study design
Confavreux 2014 and O’Connor 2011 were randomized, double-blind, placebo-controlled, parallel-group studies over at least
48 weeks (a maximum of 173 weeks) (Confavreux 2014) and
108 weeks (O’Connor 2011). Freedman 2012 was a randomized,
placebo-controlled, 24-week double-blind study followed by a 24week blinded extension. Participants completing 24 weeks of treatment who continued to meet the eligibility criteria could select
to enter a 24-week blinded extension during which participants
continued to receive their originally assigned treatment regimen.
NCT01252355 was a randomized, double-blind, placebo-controlled, parallel-group study over 24 weeks (a maximum of 108
weeks). Vermersch 2014 was an approved DMD-controlled, parallel-group, rater-blinded study over at least 48 weeks (a maximum
of 115 weeks).
Characteristics of the participants
All participants had a diagnosis of definite MS according to McDonald’s diagnostic criteria (McDonald 2001; Polman 2005), an
age ranging from 18 to 55 years and a relapsing clinical course
with or without progression (RRMS, SPMS or PRMS). All participants had an entry score of 5.5 or lower on the EDSS and no
relapse for at least 30 days before randomization. The participants
in Confavreux 2014 and O’Connor 2011 had at least one relapse
in the previous year or at least two clinical relapses in the previous
two years. The participants in NCT01252355 had disease activity
in the one year prior to randomization and after first three months
of IFNβ treatment. Baseline demographic and disease characteristics were well balanced among the groups in most studies except
for Vermersch 2014, in which DMD use in the past two years
in the teriflunomide 14 mg/day group was lower than that in the
IFNβ-1a group.
Characteristics of the outcome measures
All studies reported the proportion of participants with at least
one relapse. Two studies reported sustained disability progression,
which was defined as an increase from baseline of at least 1.0 point
in the EDSS score (or at least 0.5 points for participants with a
baseline EDSS score greater than 5.5) that persisted for at least 12
weeks (Confavreux 2014; O’Connor 2011). All studies reported
the number of participants with AEs, number of participants with
SAEs and number of participants who withdrew or dropped out
from the study because of AEs.
All studies reported the annualized relapse rate. Three trials reported the number of gadolinium-enhancing T1-weighted lesions
(Freedman 2012; NCT01252355; O’Connor 2011). Three trials reported the time to disability progression (Confavreux 2014;
NCT01252355; O’Connor 2011). One trial reported changes
in T1 hypointensity of lesion damage (O’Connor 2011). Two
trials reported mean change in QoL measured by SF-36 scores
(Confavreux 2014; NCT01252355). None of the studies reported
magnetization transfer ratio of lesion damage. One trial did not
provide data at one year (O’Connor 2011).
Excluded studies
We excluded two studies (reported in 14 articles) from this review;
the reasons for their exclusion are listed in the Characteristics of
excluded studies table.
Risk of bias in included studies
Further details of this assessment are available in the Characteristics
of included studies table and are also presented in the ’Risk of bias’
graph (Figure 2) and ’Risk of bias’ summary (Figure 3).
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
17
Figure 2. Risk of bias graph: review authors’ judgements about each risk of bias item presented as
percentages across all included studies.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
18
Figure 3. Risk of bias summary: review authors’ judgements about each risk of bias item for each included
study.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
19
Allocation
In Confavreux 2014 and O’Connor 2011, sequence generation
and allocation concealment were adequate. Allocation sequence
was generated by randomization number list (Confavreux 2014)
or a permuted-block randomization schedule with stratification
(O’Connor 2011). Randomization was done centrally, via an interactive voice recognition system (IVRS) in both studies. In
NCT01252355, sequence generation was probably made by software. Assignment to groups was done centrally using an IVRS.
In Freedman 2012 and Vermersch 2014, sequence generation was
probably made by software, and central randomization was probably used.
Blinding
In Confavreux 2014 and O’Connor 2011, the treating neurologist who recorded adverse events was responsible for assessment
of relapses, blinding of relapse assessment was probably not adequate. The risk of detection bias was high. Participants included in
Freedman 2012 and NCT01252355 received diverse regimens of
IFNβ, they were not truly double-blind, double-dummy studies.
The control (IFNβ-1a) group was open-label in Vermersch 2014,
it was not a truly double-blind study. In addition, the treating neurologist who reported or managed adverse events was responsible
for assessment of relapses in Freedman 2012, NCT01252355, and
Vermersch 2014, blinding of relapse assessment was probably not
adequate. The risks of performance bias and detection bias were
high.
Incomplete outcome data
Three studies had a high risk of attrition bias due to a high dropout
rate of 29.8% (Confavreux 2014), 36.4% (Freedman 2012), and
100% (NCT01252355). There was an overall dropout rate of
20.1% in O’Connor 2011, but there was no sufficient information to understand the reasons for study discontinuation and their
balance among the groups. The risk of attrition bias was unclear.
One study did not report the number and reasons of drop-outs
and the incomplete outcome data were unclear (Vermersch 2014).
Selective reporting
All studies reported all listed outcomes adequately.
Other potential sources of bias
All studies were sponsored by Sanofi-Aventis. In Confavreux 2014
and O’Connor 2011, the sponsor analysed the data and some
co-authors were affiliated to Sanofi-Aventis. In Vermersch 2014,
Sanofi-Aventis funded editorial support. Conflicts of interest were
obvious, and there was a high risk of bias in all studies.
Effects of interventions
See: Summary of findings for the main comparison
Teriflunomide compared to placebo for multiple sclerosis
We did not conduct meta-analyses because of the high risk of
bias and clinical diversities of the included studies. The study
designs in Confavreux 2014 and O’Connor 2011 were similar,
however, the follow-up periods were diverse (at least 48 weeks
(Confavreux 2014) and 108 weeks (O’Connor 2011)). Treatment
duration in Confavreux 2014 was variable, ending 48 weeks after
the last participant was included (a maximum treatment duration
of 173 weeks). Furthermore, the data at one year in O’Connor
2011 were unavailable. The study designs in Freedman 2012
and NCT01252355 were also similar, but the follow-up periods
were diverse (48 weeks (Freedman 2012) and at least 24 weeks
(NCT01252355)). Treatment duration in NCT01252355 was
variable (24 weeks to 108 weeks). Consequently, we could only
calculate the treatment effects of interventions based on the available data in the original studies.
Primary outcomes
Efficacy: proportion of participants with at least one relapse
at one year or two years
All studies reported proportion of participants with at least one
relapse at one year or two years.
Confavreux 2014 reported the proportion of participants with at
least one relapse at one year of follow-up were 28.10% with lowdose teriflunomide, 23.70% with high-dose teriflunomide and
39.40% with placebo, and the RD was 11.30% with low-dose
teriflunomide and 15.70% with high-dose teriflunomide. Compared to placebo, the results showed low dose of teriflunomide
as monotherapy reduced the number of participants with at least
one relapse at one year of follow-up (RR 0.72, 95% CI 0.59 to
0.87, P value = 0.001; 797 participants) and the NNTB was 9,
which means that they needed to treat nine participants with lowdose teriflunomide to prevent one participant relapsing during the
one years of follow-up. Similarly, high dose of teriflunomide as
monotherapy also reduced the number of participants with at least
one relapse at one year of follow-up (RR 0.60, 95% CI 0.48 to
0.75, P value < 0.00001; 761 participants) and the NNTB was 6,
which means that they needed to treat six participants with highdose teriflunomide to prevent one participant relapsing during the
one year of follow-up. Assuming participants who withdrew from
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
20
study both in experimental groups and control group had a relapse, the likely-case scenario analyses showed both doses of teriflunomide reduced the number of participants with at least one
relapse at one year of follow-up (low dose: RR 0.83, 95% CI 0.75
to 0.93, P value = 0.0008, 797 participants; high dose: RR 0.79,
95% CI 0.70 to 0.88, P value < 0.0001, 761 participants).
Similarly, at two years of follow-up in O’Connor 2011, compared
to placebo, both doses of teriflunomide as monotherapy reduced
the number of participants with at least one relapse at two years
of follow-up (low dose: RR 0.85, 95% CI 0.74 to 0.98, P value =
0.03; 729 participants; high dose: RR 0.80, 95% CI 0.69 to 0.93,
P value = 0.004; 722 participants). The proportion of participants
with at least one relapse at two years of follow-up were 46.30%
with low-dose teriflunomide, 43.50% with high-dose teriflunomide and 54.40% with placebo, and the RD was 8.10% with lowdose teriflunomide and 10.90% with high-dose teriflunomide,
corresponding to an NNTB of 12 with low-dose teriflunomide and
9 with high-dose teriflunomide, which means that they needed to
treat 12 participants with low-dose teriflunomide, and nine participants with high-dose teriflunomide to prevent one participant
relapsing during the two years of follow-up. When taking the effect of drop-outs into consideration, the likely-case scenario analyses still showed a benefit in reducing the number of participants
with at least one relapse for both doses of teriflunomide (low dose:
RR 0.88, 95% CI 0.80 to 0.97, P value = 0.008; 729 participants;
high dose: RR 0.87, 95% CI 0.79 to 0.96, P value = 0.005; 722
participants).
Freedman 2012 showed neither doses of teriflunomide added to
IFNβ were superior to placebo added to IFNβ concerning the
proportion of participants with at least one relapse at one year
of follow-up (low dose: RR 1.08, 95% CI 0.45 to 2.59, P value
= 0.86; 79 participants; high dose: RR 0.79, 95% CI 0.30 to
2.07, P value = 0.63; 80 participants). However, NCT01252355
showed opposite results, both doses of teriflunomide added to
IFNβ were superior to placebo added to IFNβ concerning the
proportion of participants with at least one relapse at one year
of follow-up (low dose: RR 0.60, 95% CI 0.42 to 0.87, P value
= 0.007; 353 participants; high dose: RR 0.58, 95% CI 0.40 to
0.84, P value = 0.004; 354 participants). When administrated as
monotherapy for 48 weeks to 115 weeks in Vermersch 2014, low
dose of teriflunomide was inferior to IFNβ-1a on the proportion
of participants with at least one relapse (RR 2.74, 95% CI 1.66
to 4.53, P value < 0.0001; 213 participants), but there was no
difference in reducing the number of participants with at least one
relapse for high dose of teriflunomide (RR 1.52, 95% CI 0.87 to
2.67, P value = 0.14; 215 participants).
Efficacy: proportion of participants with disability
progression
Confavreux 2014 reported the proportions of participants with
progression of disability at one year of follow-up were 12.10%
with low-dose teriflunomide, 7.80% with high-dose teriflunomide
and 14.20% with placebo, and the RD was 2.10% with low-dose
teriflunomide and 6.40% with high-dose teriflunomide. Compared to placebo, the results showed high dose of teriflunomide as
monotherapy reduced the number of participants with disability
progression at one year of follow-up (RR 0.55, 95% CI 0.36 to
0.84, P value = 0.006; 761 participants), and the NNTB was 16,
which means that they needed to treat 16 participants with highdose teriflunomide to prevent one participant having disability
progression during the one year of follow-up. However, there was
no difference for low dose of teriflunomide in disability progression at one year of follow-up (RR 0.85, 95% CI 0.59 to 1.22, P
value = 0.37; 797 participants). When taking the effect of dropouts into consideration, the likely-case scenario analysis showed
neither dose of teriflunomide reduced the number of participants
with disability progression at one year of follow-up (low dose: RR
0.94, 95% CI 0.80 to 1.11, P value = 0.47; 797 participants; high
dose: RR 0.88, 95% CI 0.74 to 1.04, P value = 0.14; 761 participants).
O’Connor 2011 reported the risk of disability progression at two
years of follow-up was 21.70% with low-dose teriflunomide and
20.20% with high-dose teriflunomide lower than that in participants receiving placebo (27.3%). The RD was 5.60% with
low-dose teriflunomide and 7.10% with high-dose teriflunomide.
Compared to placebo, the results showed high dose of teriflunomide as monotherapy reduced the proportion of participants with
disability progression at two years of follow-up (RR 0.74, 95% CI
0.56 to 0.96, P value = 0.02; 722 participants), and the NNTB
was 14, which means that they needed to treat 14 participants
with high-dose teriflunomide to prevent one participant against
disability progression during the two years of follow-up. However,
there was no difference for low dose of teriflunomide (RR 0.79,
95% CI 0.61 to 1.02, P value = 0.08; 729 participants). However,
the likely-case scenario analysis showed neither dose of teriflunomide reduced the number of participants with disability progression at two years of follow-up (low dose: RR 0.89, 95% CI 0.75 to
1.06, P value = 0.20; 729 participants; high dose: RR 0.92, 95%
CI 0.77 to 1.09, P value = 0.32; 722 participants).
Safety
Confavreux 2014 reported the safety of teriflunomide as
monotherapy after the core treatment period of 48 weeks to 152
weeks. Compared to placebo, there was no difference for both
doses of teriflunomide in the incidence of AEs (low dose: RR 1.01,
95% CI 0.95 to 1.08, P value = 0.71; 794 participants; high dose:
RR 1.04, 95% CI 0.98 to 1.10, P value = 0.23; 756 participants)
or SAEs (low dose: RR 1.04, 95% CI 0.72 to 1.51, P value =
0.83; high dose: RR 0.97, 95% CI 0.66 to 1.43, P value = 0.88).
However, the incidence of AEs leading to discontinuation of the
study medication in both teriflunomide groups was higher than
that in the placebo group (low dose: RR 2.08, 95% CI 1.31 to
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
21
3.30, P value = 0.002; NNTH 15; high dose: RR 2.51, 95% CI
1.59 to 3.95, P value < 0.0001; NNTH 11). The most common
AEs with an increased incidence in both teriflunomide groups included hair thinning (low dose: RR 2.33, 95% CI 1.35 to 4.01,
P value = 0.002; NNTH 17; high dose: RR 3.05, 95% CI 1.79
to 5.19, P value < 0.0001; NNTH 11), neutropenia (low dose:
RR 2.48, 95% CI 1.26 to 4.90, P value = 0.009; NNTH 24; high
dose: RR 3.30, 95% CI 1.70 to 6.40, P value = 0.0004; NNTH
15), neutrophil counts less than 1.5 x 109 /L (low dose: RR 1.85,
95% CI 1.18 to 2.90, P value = 0.008; NNTH 18; high dose:
RR 2.47, 95% CI 1.60 to 3.82, P value < 0.001; NNTH 10),
lymphocyte counts less than 0.8 x 109 /L (low dose: RR 1.82, 95%
CI 1.18 to 2.80, P value = 0.007; NNTH 17; high dose: RR 1.78,
95% CI 1.14 to 2.77, P value = 0.01; NNTH 18), and elevated
alanine aminotransferase (ALT) levels greater than one time the
upper limit of the normal range (low dose: RR 1.30, 95% CI 1.11
to 1.53, P value = 0.001; NNTH 9; high dose: RR 1.44, 95% CI
1.23 to 1.68, P value < 0.00001; NNTH 6).
There was a similar incidence of elevated ALT levels three times or
greater the upper limit of the normal range and neutrophil counts
less than 0.5 x 109 /L between the placebo group and the teriflunomide groups. Elevated ALT and lymphocyte counts less than 0.5 x
109 /L occurred at higher frequency with high-dose teriflunomide
compared to placebo (elevated ALT: RR 1.69, 95% CI 1.11 to
2.56, P value = 0.01; NNTH 18; elevated lymphocyte count: RR
11.42, 95% CI 1.48 to 87.98, P value = 0.02; NNTH 59), but
there was no difference for low-dose teriflunomide. In addition,
diarrhoea was more common with low-dose teriflunomide rather
than high-dose teriflunomide (RR 1.65, 95% CI 1.06 to 2.57,
P value = 0.03). The proportion of other AEs most commonly
reported in teriflunomide groups, such as headache, fatigue, nausea, nasopharyngitis, upper respiratory tract infection, back pain
and urinary tract infection, were not higher than in the placebo
group. The AEs leading to treatment discontinuation mainly included elevated ALT levels (3% with low-dose teriflunomide and
2% with high-dose teriflunomide), neutropenia (1% with lowdose teriflunomide and 2% with high-dose teriflunomide), hair
thinning (2% with high-dose teriflunomide) and diarrhoea (1%
in both teriflunomide groups). There were 18 pregnancies in 14
female participants and four female partners of male participants.
Of the 14 female participants, 10 elected to have induced abortions and four pregnancies resulted in healthy babies (one in the
placebo group, two in the low-dose teriflunomide group and one
in the high-dose teriflunomide group). Of the four pregnancies
in partners of male participants, one woman elected to have an
induced abortion and three pregnancies resulted in healthy babies
(all in the low-dose teriflunomide group).
O’Connor 2011 reported the safety of teriflunomide as monotherapy at two years of follow-up. Compared to placebo, there was no
difference for both doses of teriflunomide in the incidence of AEs
(low dose: RR 1.02, 95% CI 0.97 to 1.07, P value = 0.49; 728
participants; high dose: RR 1.04, 95% CI 0.99 to 1.09, P value =
0.16; 718 participants), SAEs (low dose: RR 1.11, 95% CI 0.76
to 1.60, P value = 0.59; high dose: RR 1.25, 95% CI 0.87 to 1.79,
P value = 0.23) and AEs leading to discontinuation of the study
medication (low dose: RR 1.21, 95% CI 0.76 to 1.94, P value =
0.41; high dose: RR 1.35, 95% CI 0.86 to 2.14, P value = 0.20).
The most common adverse events with an increased incidence in
both teriflunomide groups included diarrhoea (low dose: RR 1.65,
95% CI 1.09 to 2.49, P value = 0.02; NNTH 17; high dose: RR
2.01, 95% CI 1.35 to 3.00, P value = 0.0006; NNTH 11), hair
thinning or decreased hair density (low dose: RR 3.10, 95% CI
1.65 to 5.83, P value = 0.0005; NNTH 14; high dose: RR 3.94,
95% CI 2.13 to 7.30, P value < 0.0001; NNTH 10), elevated
ALT levels (low dose: RR 1.79, 95% CI 1.11 to 2.89, P value =
0.02; NNTH 19; high dose: RR 2.14, 95% CI 1.35 to 3.39, P
value = 0.001; NNTH 13). The incidence of nausea in high-dose
teriflunomide group rather than in low-dose teriflunomide group
was higher than that in placebo group (low dose: RR 1.24, 95%
CI 0.76 to 2.03, P value = 0.39; high dose: RR 1.90, 95% CI 1.21
to 2.98, P value = 0.006; NNTH 15). The incidence of elevated
ALT levels one times or greater the upper limit of the normal range
in both doses was higher than that in placebo group (low dose:
RR 2.61, 95% CI 1.23 to 5.53, P value = 0.01; NNTH 6; high
dose: RR 3.24, 95% CI 1.56 to 6.75, P value = 0.002; NNTH
5), but there was no difference for both doses of teriflunomide
in the incidence of elevated ALT levels three times or greater the
upper limit of the normal range. These events rarely led to discontinuation of the study medication: diarrhoea (0.3% in both teriflunomide groups), nausea (0.3% with low-dose), hair thinning or
decreased hair density (0.5% with low-dose and 1.4% with highdose). The proportion of other AEs (10% or greater) most commonly reported in any teriflunomide group, such as nasopharyngitis, headache, fatigue, influenza, back pain and urinary tract infection, occurred with a similar frequency in the placebo group. Mean
reductions in neutrophil and lymphocyte counts from baseline
values were small in magnitude (1.0 x 109 /L or less for neutrophil
counts and 0.3 x 109 /L or less for lymphocyte counts) but were
slightly more marked with high-dose teriflunomide than with lowdose teriflunomide or placebo. Moderate neutropenia (defined as
a neutrophil count of less than 0.9 x 109 /L) developed in three
participants receiving teriflunomide. Eleven pregnancies occurred,
leading to four spontaneous abortions (one in the placebo group
and three in the high-dose teriflunomide group), six induced abortions (five in the low-dose teriflunomide group and one in the
high-dose teriflunomide group). One participant in the high-dose
teriflunomide group (treated for 31 days of the pregnancy) delivered a healthy baby with no reported health concerns after two
years.
Vermersch 2014 reported the safety of teriflunomide as monotherapy after the core treatment period of 48 weeks to 115 weeks.
Compared to IFNβ-1a, there was no difference for both doses of
teriflunomide in the incidence of AEs (low dose: RR 0.97, 95%
CI 0.92 to 1.04, P value = 0.43; 211 participants; high dose: RR
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
22
0.97, 95% CI 0.90 to 1.03, P value = 0.29; 211 participants) or
SAEs (low dose: RR 1.57, 95% CI 0.64 to 3.84, P value = 0.32;
high dose: RR 0.79, 95% CI 0.27 to 2.26, P value = 0.66). However, the incidence of AEs leading to discontinuation in the IFNβ
group was higher than those in the teriflunomide groups (low dose:
RR 0.38, 95% CI 0.18 to 0.78, P value = 0.008; high dose: RR
0.50, 95% CI 0.26 to 0.96, P value = 0.04). The most commonly
reported AEs (10% or greater) in either teriflunomide group were
nasopharyngitis, headache, paraesthesia, diarrhoea, hair thinning,
back pain and elevated ALT levels. Among these AEs, the incidence of diarrhoea in both teriflunomide groups was higher than
that in the IFNβ-1a group (low dose: RR 2.87, 95% CI 1.36 to
6.07, P value = 0.006; high dose: RR 2.64, 95% CI 1.24 to 5.63,
P value = 0.01). Compared to IFNβ-1a, hair thinning was more
common with high-dose teriflunomide rather than low-dose teriflunomide (RR 20.20, 95% CI 2.77 to 147.14, P value = 0.003).
However, elevated ALT levels occurred with a lower frequency in
the teriflunomide groups (low dose: RR 0.36, 95% CI 0.19 to
0.65, P value = 0.0009; high dose: RR 0.33, 95% CI 0.17 to 0.61,
P value = 0.0005). In addition, influenza-like illness was reported
more frequently with IFNβ-1a than with teriflunomide (low dose:
RR 0.07, 95% CI 0.03 to 0.18, P value < 0.00001; high dose:
RR 0.05, 95% CI 0.02 to 0.16, P value < 0.00001). There was a
similar incidence of other AEs between the IFNβ-1a group and
teriflunomide groups.
Freedman 2012 reported the safety of teriflunomide added to
IFNβ at one year of follow-up. Compared to placebo added to
IFNβ, there was no difference for either dose of teriflunomide in
the incidence of AEs (low dose: RR 1.11, 95% CI 0.96 to 1.29, P
value = 0.17; 78 participants; high dose: RR 1.02, 95% CI 0.85 to
1.21, P value = 0.85; 79 participants), SAEs (low dose: RR 2.22,
95% CI 0.43 to 11.40, P value = 0.34; high dose: RR 0.54, 95%
CI 0.05 to 5.71, P value = 0.61) and AEs leading to discontinuation (low dose: RR 1.66, 95% CI 0.29 to 9.40, P value = 0.57;
high dose: RR 1.62, 95% CI 0.29 to 9.16, P value = 0.59). The
most commonly reported AEs (10% or greater) in either teriflunomide group were elevated ALT levels, headache, decreased lymphocyte counts, nasopharyngitis, nausea, fatigue, decreased neutrophil counts, hypertension, back pain, vomiting, diarrhoea and
urinary tract infection. However, these AEs occurred with a similar frequency in the IFNβ group.
NCT01252355 reported the safety of teriflunomide added to
IFNβ after the treatment period of 28 weeks to 108 weeks. Compared to placebo added to IFNβ, the incidences of AEs in both
teriflunomide groups were higher than those in the placebo group
(low dose: RR 1.15, 95% CI 1.01 to 1.31, P value = 0.03; 354
participants; high dose: RR 1.16, 95% CI 1.02 to 1.31, P value =
0.02; 353 participants). However, there was no difference for either dose of teriflunomide in the incidence of SAEs (low dose: RR
1.59, 95% CI 0.68 to 3.74, P value = 0.29; high dose: RR 1.72,
95% CI 0.74 to 4.00, P value = 0.21). The incidence of AEs leading to discontinuation with high-dose teriflunomide rather than
with low-dose teriflunomide was higher than that in the placebo
group (low dose: RR 1.74, 95% CI 0.79 to 3.83, P value = 0.17;
high dose: RR 2.40, 95% CI 1.14 to 5.07, P value = 0.02). There
was no difference for either dose of teriflunomide in the incidence
of elevated ALT levels three times or greater the upper limit of the
normal range (low dose: RR 1.46, 95% CI 0.53 to 4.01, P value =
0.47; high dose: RR 1.47, 95% CI 0.53 to 4.03, P value = 0.46).
Secondary outcomes
Annualized relapse rate
All studies reported the annualized relapse rate. Confavreux 2014
reported annualized relapse rate after the core treatment period of
48 weeks to 152 weeks (low dose: annualized relapse rate 0.39,
95% CI 0.33 to 0.46; 407 participants; high dose: annualized relapse rate 0.32, 95% CI 0.27 to 0.38; 370 participants; placebo:
annualized relapse rate 0.50, 95% CI 0.43 to 0.58; 388 participants), but we could not calculate the total number of relapses and
standard errors due to the variable duration of follow-up, consequently we could not calculate the rate ratio. However, the authors
reported the RRs on annualized relapse rate, showing both doses
of teriflunomide as monotherapy reduced annualized relapse rate
during the follow-up period of 48 weeks to 132 weeks (low dose:
RR 0.78, 95% CI 0.63 to 0.96, P value = 0.0183; 797 participants;
high dose: RR 0.64, 95% CI 0.51 to 0.79, P value = 0.0001; 761
participants).
There were similar results at two years of follow-up in O’Connor
2011 (low dose: rate ratio 0.69, 95% CI 0.59 to 0.81, P value
< 0.00001; 729 participants; high dose: rate ratio 0.69, 95% CI
0.59 to 0.80, P value < 0.00001; 722 participants).
Freedman 2012 showed neither doses of teriflunomide added to
IFNβ were superior to placebo added to IFNβ concerning annualized relapse rate at one year of follow-up (low dose: rate ratio
0.42, 95% CI 0.15 to 1.16, P value = 0.10; 79 participants; high
dose: rate ratio 0.67, 95% CI 0.29 to 1.54, P value = 0.35; 80
participants).
NCT01252355 reported only the data of annualized relapse rate
after the treatment duration of 24 weeks to 108 weeks (low dose:
annualized relapse rate 0.242, 95% CI 0.152 to 0.386; 178 participants; high dose: annualized relapse rate 0.238, 95% CI 0.162
to 0.351; 179 participants; placebo: annualized relapse rate 0.298,
95% CI 0.206 to 0.432; 175 participants). Therefore, we could
not calculate the total number of relapses and the standard error
due to the variable duration of follow-up, consequently we could
not calculate the rate ratio.
Vermersch 2014 reported the data of annualized relapse rate after
the treatment period of 48 weeks to 115 weeks (low dose: annualized relapse rate 0.41, 95% CI 0.27 to 0.64; 109 participants;
high dose: annualized relapse rate 0.26, 95% CI 0.15 to 0.44; 111
participants; IFNβ-1a: annualized relapse rate 0.22, 95% CI 0.11
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
23
to 0.42; 104 participants). However, we could not calculate the
total number of relapses and the standard error due to the variable
duration of follow-up, consequently we could not calculate the
rate ratio. However, the authors reported the RR on annualized
relapse rate, showing that low-dose teriflunomide was inferior to
IFNβ-1a on annualized relapse rate (RR 1.90, 95% CI 1.05 to
3.43, P value = 0.03; 213 participants), but there was no difference
in reducing annualized relapse rate for high-dose teriflunomide
(RR 1.20, 95% CI 0.62 to 2.30, P value = 0.59; 215 participants).
Number of gadolinium-enhancing T1-weighted lesions
Three studies reported the number of gadolinium-enhancing T1weighted lesions (Freedman 2012; NCT01252355; O’Connor
2011).
Compared to placebo, the results of O’Connor 2011 showed both
doses of teriflunomide as monotherapy reduced the number of
gadolinium-enhancing T1-weighted lesions at two years of followup (low dose: rate ratio 0.43, 95% CI 0.37 to 0.51, P value <
0.00001; 729 participants; high dose: rate ratio 0.19, 95% CI 0.15
to 0.24, P value < 0.00001; 722 participants).
Freedman 2012 showed neither dose of teriflunomide added to
IF-β was superior to placebo added to IFNβ concerning the number of gadolinium-enhancing T1-weighted lesions at one year of
follow-up (low dose: rate ratio 0.67, 95% CI 0.29 to 1.55, P value
= 0.35; 79 participants; high dose: rate ratio 0.42, 95% CI 0.16
to 1.09, P value = 0.08; 80 participants).
NCT01252355 reported only the data of the number of gadolinium-enhancing T1-weighted lesions after the treatment period of
24 weeks to 108 weeks (low dose: 0.257, 95% CI 0.127 to 0.523;
142 participants; high dose: 0.158, 95% CI 0.070 to 0.360; 151
participants; placebo: 0.542, 95% CI 0.344 to 0.855; 151 participants). We could not calculate the annualized relapse rate due
to the variable duration of follow-up, consequently we could not
calculate the rate ratio.
Time to disability progression
Three studies reported the time to disability progression (
Confavreux 2014; NCT01252355; O’Connor 2011).
Compared to placebo, the results of Confavreux 2014 showed
high-dose teriflunomide as monotherapy delayed the progression
of disability after the core treatment period of 48 weeks to 152
weeks (HR 0.68, 95% CI 0.47 to 1.00, P value = 0.04; 758 participants), but there was no difference in delaying the progression
of disability for low-dose teriflunomide (HR 0.95, 95% CI 0.68
to 1.35, P value = 0.76; 795 participants).
The results of O’Connor 2011 showed high-dose teriflunomide
as monotherapy delayed the progression of disability at two years
of follow-up (HR 0.70, 95% CI 0.51 to 0.96, P value = 0.03; 721
participants), but there was no difference in delaying the progression of disability for low-dose teriflunomide (HR 0.76, 95% CI
0.56 to 1.05, P value = 0.08; 728 participants).
Data of the time to disability progression in NCT01252355 were
insufficient because of early study termination and were not reported in the original publication.
Changes in T1 hypointensity or magnetization transfer ratio
of lesion damage
One study reported changes in T1 hypointensity lesion damage
(O’Connor 2011). The results showed high-dose teriflunomide
as monotherapy, compared to placebo, reduced the volume of
hypointense lesions on T1-weighted images at two years (MD 0.20, 95% CI -0.35 to -0.05, P value = 0.009, 728 participants).
However, there was no difference for low-dose teriflunomide (MD
-0.03, 95% CI -0.19 to 0.13, P value = 0.71; 721 participants).
None of the studies reported magnetization transfer ratio of lesion
damage.
Change in health-related quality of life
Two studies reported change in QoL measured by SF-36 scores
(Confavreux 2014; NCT01252355).
Confavreux 2014 found that compared to placebo, there was no
difference for teriflunomide as monotherapy in change of SF-36
physical health summary score and in SF-36 mental health summary score at 48 weeks (low dose: physical health: MD 0.68, 95%
CI -0.44 to 1.80, P value = 0.24 and mental health: MD 0.88,
95% CI -0.72 to 2.48, P value = 0.28; 797 participants; high dose:
physical health: MD 0.97, 95% CI -0.18 to 2.12, P value = 0.10
and mental health: MD 1.48, 95% CI -0.18 to 3.14, P value =
0.08; 761 participants).
Data of change in QoL measured by SF-36 scores in
NCT01252355 were insufficient because of early study termination and were not reported in the original publication.
DISCUSSION
Summary of main results
This systematic review included five RCTs involving 3231 adults
with relapsing MS. All participants had a score of less than 5.5 on
the EDSS and a relapsing clinical course with or without progression (RRMS, SPMS or PRMS). Two studies were large-scale RCTs
in which participants had disease activity with at least one relapse
in the previous year or at least two clinical relapses in the previous
two years. These two studies primarily evaluated the benefit of
teriflunomide at a dose of 7 mg/day or 14 mg/day as monotherapy
versus placebo in respect of relapse, disability worsening and safety
over at least 48 weeks (a maximum of 173 weeks) (Confavreux
2014) or two years (O’Connor 2011). The other three studies
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
24
mainly evaluated the efficacy on relapse and the safety and tolerability of teriflunomide 7 mg/day or 14 mg/day with add-on IFNβ
versus placebo over 48 weeks (Freedman 2012) or at least 24 weeks
(a maximum of 108 weeks) (NCT01252355), or teriflunomide
7 mg/day or 14 mg/day alone versus IFNβ-1a (Vermersch 2014)
at least 48 weeks (a maximum of 115 weeks). The study design
and interventions of the five studies were diverse. There were obvious clinical heterogeneities due to the diversities in study designs
or interventions and methodological heterogeneities across studies. All studies had a high risk of detection bias for relapse assessment and a high risk of bias due to conflicts of interest. Among
them, Confavreux 2014, Freedman 2012, and NCT01252355
had a high risk of attrition bias due to a high dropout rate
(29.8% (Confavreux 2014), 36.4% (Freedman 2012) and 100%
(NCT01252355). O’Connor 2011 and Vermersch 2014 had an
unclear risk of attrition bias. Freedman 2012, NCT01252355,
and Vermersch 2014had a high risk for performance bias and a
lack of power due to the limited sample. The data at one year
in O’Connor 2011 were not available. As a result, we could not
conduct meta-analyses. We calculated the treatment effects of interventions based on the available data in the original studies.
Compared to placebo, administration of teriflunomide at a dose
of 7 mg/day or 14 mg/day as monotherapy reduced the number of
participants with relapse by one year or by two years, as well as the
annualized relapse rate by two years. Both doses of teriflunomide
as monotherapy reduced the number of gadolinium-enhancing
T1-weighted lesions by two years, However, only teriflunomide
at a dose of 14 mg/day as monotherapy significantly reduced the
number of participants with disability progression and delayed the
progression of disability by one year and two years. High dose
rather than low dose of teriflunomide as monotherapy reduced
the volume of hypointense lesions on T1-weighted images by two
years. Neither doses of teriflunomide improved QoL measured by
SF-36 scores by one year. When taking the effect of drop-outs
into consideration, the likely-case scenario analyses still showed a
benefit in reducing the number of participants with relapse, but
not for the number of participants with disability progression.
When administrated as combination therapy with IFNβ for one
year, neither doses of teriflunomide added to IFNβ were superior
to placebo added to IFNβ concerning annualized relapse rate and
the number of gadolinium-enhancing T1-weighted lesions. When
compared to IFNβ-1a, low-dose teriflunomide was inferior to
IFNβ-1a in respect of the annualized relapse rate and the number
of participants with relapse, but there was no difference for highdose teriflunomide.
Overall, the risks for AEs and SAEs in participants receiving teriflunomide were similar to those in participants receiving placebo
both at one year and two years of follow-up. However, the risks
for study drug discontinuation due to AEs were increased by both
doses of teriflunomide administration at one year of follow-up,
but not at two years of follow-up. The most common
AEs associated with teriflunomide included diarrhoea, nausea,
hair thinning, elevated ALT levels, neutropenia and lymphopenia.
These AEs rarely led to discontinuation of the study medication,
but did have a dose-related effect.
Overall completeness and applicability of
evidence
In this review, we excluded one RCT due to length of follow-up
shorter than one year. Generally, DMT for MS needs an adequate
administration duration and follow-up to determine the benefit
and safety outcomes accurately. A minimum duration of administration of one year, pre-defined in the criteria of types of interventions, was a reasonable treatment length that partly avoided the
inclusion of misleading evidence. We did not perform meta-analyses due to the diversities in the study design and interventions.
Two large-scale RCTs contributed to the main evidence for this
review. The evidence was only applicable to adults with relapsing
MS, who had a score of less than 5.5 on the EDSS and disease
activity with at least one relapse in the previous year or at least two
clinical relapses in the previous two years.
Quality of the evidence
We included five RCTs in this review, involving 3231 adults with
relapsing MS to evaluate mainly the benefit and safety of two
doses of teriflunomide (7 mg/day and 14 mg/day) as monotherapy or combination therapy with IFNβ by direct comparison with
placebo or IFNβ-1a. Overall, there were obvious clinical heterogeneities due to the diversities in study designs or interventions
and methodological heterogeneities across studies. All studies had
a high risk of detection bias for relapse assessment and a high risk
of bias due to conflicts of interest. Among them, three studies also
had a high risk of attrition bias due to a high dropout rate and
two studies had an unclear risk of attrition bias. Generally, the
higher the ratio of participants with missing data to participants
with events, the greater potential there is for bias, especially for the
high frequency of events. The potential impact of missing continuous outcomes increases with the proportion of participants with
missing data. In addition, the studies of combination therapy with
IFNβ and the study with IFNβ-1a as controls also had a high
risk of performance bias and a lack of power due to the limited
sample. The evidence in this review was mainly derived from the
two large-scale RCTs, in which the high risk of bias lead to lowquality evidence for the results of relapse. The results of disability
progression were also subjected to a serious indirectness of evidence because disability progression was confirmed in less than six
months in both studies. The evidence for disability progression
was very low.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
25
Potential biases in the review process
An extensive and comprehensive search was undertaken to limit
bias in the review process. The two review authors’ independent
assessments of the eligibility of studies for inclusion in this review
and extraction of data minimized the potential for additional bias
beyond that detailed in the ’Risk of bias’ tables. The review authors
had no conflicts of interest.
Agreements and disagreements with other
studies or reviews
There are three network meta-analyses that compared the benefit or acceptability of teriflunomide and other DMDs by mixed
treatment comparison (Hadjigeorgiou 2013; Tramacere 2015;
Zagmutt 2015). We have found no other systematic review on
teriflunomide for MS that used only direct head-to-head comparisons. In this systematic review, our extensive and comprehensive
search found only one RCT comparing teriflunomide to other
DMDs, and it was very low-quality. There was a lack of evidence
to show the comparative benefit and safety of teriflunomide in
comparison with other DMDs. As with the results of the network
meta-analyses, this systematic review also emphasized the need for
randomized trials of direct comparisons between teriflunomide
and other active agents.
and the number of participants with a relapse over one year and
two years of treatment. Only teriflunomide at a dose of 14 mg/day
as monotherapy reduced the number of participants with disability
progression and delayed the progression of disability over one year
or two years, but the quality of the evidence was very low. The
quality of available data was too low to evaluate the benefit of
teriflunomide as monotherapy versus interferon beta-1a (IFNβ1a) or as combination therapy with interferon beta (IFNβ). The
common adverse effects were diarrhoea, nausea, hair thinning,
elevated alanine aminotransferase, neutropenia and lymphopenia.
These adverse effects were mostly mild-to-moderate in severity,
but had a dose-related effect.
Implications for research
The ideal target of disease-modifying therapy for multiple sclerosis
(MS) is to prevent disability progression and improve quality of
life, which are two key aspects generally needed to be considered
when evaluating and deciding whether a disease-modifying drug
has superior benefit. MS is a chronic disease with a duration of
decades that requires long-term treatment. Therefore, new studies
of high quality and longer follow-up are needed to evaluate the
comparative benefit of teriflunomide on these outcomes and safety
in comparison with other disease-modifying drugs.
ACKNOWLEDGEMENTS
AUTHORS’ CONCLUSIONS
Implications for practice
There was low-quality evidence to support that teriflunomide at a
dose of 7 mg and 14 mg orally once daily as monotherapy by direct
comparison with placebo reduced both the annualized relapse rate
We thank Andrea Fittipaldo, Trials Search Co-ordinator, and Liliana Coco, Managing Editor of the Cochrane Multiple Sclerosis
and Rare Diseases of the CNS Group, for their help and support
in developing this review. We also thank Dr. Zhou Hongyu, Xu
Zhu, Dong Shuai, Zhang Hong, Wang Lu and Zhang Shihong
for their contributions to the first version of this review.
REFERENCES
References to studies included in this review
Confavreux 2014 {published data only}
Comi G, Freedman MS, Kappos L, Miller A, Olsson TP,
Wolinsky JS, et al. Effect of teriflunomide on lymphocyte
and neutrophil counts in patients with relapsing multiple
sclerosis: results from the TOWER study. Journal of the
Neurological Sciences 2013;333:e376.
∗
Confavreux C, O’Connor P, Comi G, Freedman MS,
Miller AE, Olsson TP, et al. Oral teriflunomide for patients
with relapsing multiple sclerosis (TOWER): a randomised,
double-blind, placebo-controlled, phase 3 trial. Lancet
Neurology 2014;13(3):247–56.
Kappos L, Comi G, Confavreux C, Freedman MS,
Miller AE, Olsson TP, et al. The efficacy and safety of
teriflunomide in patients with relapsing MS: results from
TOWER, a phase , placebo-controlled study. Multiple
Sclerosis 2012;18:50–1.
Miller A, Kappos L, Comi G, Confavreux C, Freedman
M, Olsson T, et al. Teriflunomide efficacy and safety in
patients with relapsing multiple sclerosis: results from
tower, a second, pivotal, phase 3 placebo-controlled study.
Neurology. 2013; Vol. 80.
Miller AE, Macdonell R, Comi G, Freedman MS, Kappos
L, Maurer M, et al. Teriflunomide reduces relapses with
sequelae and relapses leading to hospitalizations: results
from the TOWER study. Journal of Neurology 2014;261(9):
1781–8.
Moses H, Freedman M, Kappos L, Miller A, Olsson T,
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
26
Wolinsky J, et al. Pre-defined subgroups analyses of tower,
a placebo-controlled phase 3 trial of teriflunomide in
patients with relapsing multiple sclerosis. Proceedings of
the American Academy of Neurology’s 65th AAN Annual
Meeting; 2013 Mar 16-23; San Diego (CA).
O’Connor P, Lublin F, Wolinsky J, Comi G, Confavreux C,
Freedman M, et al. Teriflunomide reduces relapse-related
sequelae, hospitalizations and corticosteroid use: a postHOC analysis of the phase 3 TOWER study. Proceedings
of The American Academy of Neurology’s 65th AAN
Annual Meeting; 2013 Mar 16-23; San Diego (CA).
Freedman 2012 {published data only}
Freedman MS, Wolinsky JS, Wamil B, Confavreux C, Comi
G, Kappos L, et al. Teriflunomide added to interferon-β
in relapsing multiple sclerosis: a randomized phase
Neurology 2012;78(23):1877–85.
trial.
NCT01252355 {published data only}
NCT01252355. Efficacy and Safety of Teriflunomide in
Patients with Relapsing Multiple Sclerosis and Treated with
Interferon-beta (TERACLES). www.clinicaltrials.gov/ct2/
show/results/NCT01252355 (accessed 12 January 2016).
O’Connor 2011 {published data only}
Comi G, Benzerdjeb H, Wang L, Truffinet P, O’Connor P.
Effect of teriflunomide on lymphocyte and neutrophil levels
in patients with relapsing multiple sclerosis: results from the
TEMSO study. Journal of Neurological Science 2013;333
(Suppl 1):e376.
Comi G, O’Connor P, Wolinsky J, Confavreux C, Kappos
trial (TEMSO)
L, Olsson T, et al. Extension of a phase
of oral teriflunomide in multiple sclerosis with relapses:
safety outcomes with up to 4 years of follow-Up. Multiple
Sclerosis 2011;17:S182–3.
Freedman M, Wolinsky J, Comi G, Kappos L, Olsson
T, Miller A, et al. Long-term safety and efficacy of
teriflunomide in patients with relapsing forms of multiple
sclerosis in the TEMSO extension trial. Multiple Sclerosis
2013;19:225.
Freedman M, Wolinsky J, Comi G, Kappos L, Olsson T,
Miller A, et al. Safety and efficacy of teriflunomide for up
to 9 years in relapsing forms of multiple sclerosis: Update
of the TEMSO extension trial. Neurology 2014; Vol. 82,
issue Suppl 10:3–150.
Freedman MS, Delhay JL, Benamor M. Gastrointestinal
symptoms infrequently lead to discontinuation of
teriflunomide therapy. Multiple Sclerosis 2012;18:S13.
Miller A, Lublin F, O’Connor P, Taniou C, Dive-Pouletty C.
Impact of relapses with sequelae on disability, health-related
quality of life, and fatigue in a population with relapsing
forms of multiple sclerosis using data from TEMSO, a
pivotal phase
teriflunomide trial. Neurology 2012;78:
P07.082.
Miller A, Lublin F, O’Connor P, Wolinsky J, Comi G,
Kappos L, et al. Effect of teriflunomide on relapses
with sequelae and relapse leading to hospitalization in a
population with relapsing forms of multiple sclerosis: results
from the TEMSO study. Neurology 2012;78:S30.003.
Miller A, O’Connor P, Wolinsky J, Confavreux C, Comi G,
Kappos L, et al. Efficacy of oral teriflunomide in multiple
sclerosis with relapses: cognitive outcomes from a phase
trial (TEMSO). Multiple Sclerosis 2011;17:S182.
Miller AE, O’Connor P, Wolinsky JS, Confavreux C,
Kappos L, Olsson TP, et al. Pre-specified subgroup analyses
of a placebo-controlled phase
trial (TEMSO) of oral
teriflunomide in relapsing multiple sclerosis. Multiple
Sclerosis 2012;18(11):1625–32.
O’Connor P, Briggs A, Carita P, Bego-Le-Bagousse G.
Impact on health-related quality of life of teriflunomide
treatment by estimating utilities in patients with relapsing
multiple sclerosis: results from TEMSO post hoc analysis.
Journal of Neurology 2012;259:S107.
O’Connor P, Burrell A, Wang L, Wei L, Carita P, Zhang Q.
Effect of teriflunomide on longitudinal patterns of relapse
and relapse-related hospitalization in multiple sclerosis.
Multiple Sclerosis 2011;17:S414.
O’Connor P, Lublin F, Wolinsky J, Comi G, Kappos L,
Freedman M, et al. Effect of teriflunomide on relapses
leading to healthcare resource use: results from the TEMSO
study. Multiple Sclerosis 2011;17:S95–6.
O’Connor P, Wolinsky J, Confavreux C, Comi G, Kappos
trial (TEMSO)
L, Olsson T, et al. Extension of a phase
of oral teriflunomide in multiple sclerosis with relapses:
clinical and MRI data 5 years after initial randomization.
Multiple Sclerosis 2011;17:S414–5.
∗
O’Connor P, Wolinsky JS, Confavreux C, Comi G,
Kappos L, Olsson TP, et al. Randomized trial of oral
teriflunomide for relapsing multiple sclerosis. New England
Journal of Medicine 2011;365(14):1293–303.
O’Connor PW, Lublin FD, Wolinsky JS, Confavreux C,
Comi G, Freedman MS, et al. Teriflunomide reduces
relapse-related neurological sequelae, hospitalizations and
steroid use. Journal of Neurology 2013;260(10):2472–80.
Wolinksy JS, Wang L, Truffinet P, Narayana PA, Nelson F,
O’Connor P. Magnetic resonance imaging as a surrogate for
clinical endpoints in multiple sclerosis. Multiple Sclerosis
2012;18:470–1.
Wolinsky JS, Narayana PA, Nelson F, Datta S, O’Connor P,
Confavreux C, et al. Magnetic resonance imaging outcomes
trial of teriflunomide. Multiple Sclerosis
from a phase
2013;19(10):1310–9.
Vermersch 2014 {published data only}
Vermersch P, Czlonkowska A, Grimaldi LM, Confavreux
C, Comi G, Kappos L, et al. A multicenter, randomized,
parallel-group, rater-blinded study comparing the
effectiveness and safety of teriflunomide and subcutaneous
interferon beta-1a in patients with relapsing multiple
sclerosis. Multiple Sclerosis 2012;18:S9–10.
Vermersch P, Czlonkowska A, Grimaldi LM, Confavreux C,
Comi G, Kappos L, et al. Evaluation of patient satisfaction
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
27
from the TENERE study: a comparison of teriflunomide
and subcutaneous interferon beta-1a in patients with
relapsing multiple sclerosis. Journal of Neurology 2012;259:
S38.
∗
Vermersch P, Czlonkowska A, Grimaldi LM, Confavreux
C, Comi G, Kappos L, et al. Teriflunomide versus
subcutaneous interferon beta-1a in patients with relapsing
multiple sclerosis: a randomised, controlled phase 3 trial.
Multiple Sclerosis 2014;20(6):705–16.
References to studies excluded from this review
Miller 2014 {published data only}
Comi G, Miller AE, Wolinsky JS, Benamor M, Bauer D,
Truffinet P, et al. The effect of teriflunomide on lymphocyte
and neutrophil count in patients with a first clinical episode
consistent with multiple sclerosis: results from the TOPIC
study. European Journal of Neurology 2014;21:127–8.
Miller A, Wolinsky J, Kappos L, Comi G, Freedman M,
Olsson T, et al. TOPIC: efficacy and safety of once-daily
oral teriflunomide in patients with first clinical episode
consistent with multiple sclerosis. Neurology. 2014; Vol.
82.
Miller A, Wolinsky J, Kappos L, Comi G, Freedman MS,
Olsson T, et al. TOPIC main outcomes: efficacy and safety
of once-daily oral teriflunomide in patients with clinically
isolated syndrome. Multiple Sclerosis 2013;19:25–6.
∗
Miller AE, Wolinsky JS, Kappos L, Comi G, Freedman
MS, Olsson TP, et al. Oral teriflunomide for patients
with a first clinical episode suggestive of multiple sclerosis
(TOPIC): a randomised, double-blind, placebo-controlled,
phase 3 trial. Lancet Neurology 2014;13(10):977–86.
Turner B, Bauer D, Benamor M, Truffinet P, Miller A.
Teriflunomide in early stage MS: results from TOPIC.
Journal of Neurology, Neurosurgery and Psychiatry 2014;85:
A40.
Wolinsky JS, Comi G, Kappos L, Bauer D, Truffinet P,
Miller AE. Effect of teriflunomide on MRI activity in
patients with early MS: outcomes from the phase 3 TOPIC
study. European Journal of Neurology 2014;21:103.
Wolinsky JS, Truffinet P, Bauer D, Miller AE. Efficacy of
teriflunomide in patients with early stage MS: analysis of
the TOPIC study using 2010 McDonald diagnostic criteria.
Multiple Sclerosis 2014;20:109–10.
Wolinsky JS, Truffinet P, Bauer D, Miller AE. MRI
outcomes in patients with early multiple sclerosis treated
with teriflunomide: subgroup analyses from the TOPIC
phase 3 study. Multiple Sclerosis 2014;20:84.
O’Connor 2006 {published data only}
Confavreux C, Li DK, Freedman MS, Truffinet P,
Benzerdjeb H, Wang D, et al. Long-term follow-up of a
phase 2 study of oral teriflunomide in relapsing multiple
sclerosis: safety and efficacy results up to 8.5 years. Multiple
Sclerosis 2012;18(9):1278–89.
Confavreux C, O’Connor P, Freedman M, Benzerdjeb H,
Wang D, Bar-Or A. Long term safety and tolerability of
teriflunomide in multiple sclerosis: 9-year follow-up of a
study. Multiple Sclerosis 2011;17:S409–10.
phase
Jumah MA, Li DB, Yamout B, Truffinet P, Dukovic D,
O’Connor PW. Long-term clinical and magnetic resonance
imaging outcomes from patients treated with teriflunomide:
results from a phase 2 extension study. Multiple Sclerosis and
Related Disorders 2014;3:755–56.
Li D, O’Connor P, Confavreux C, Truffinet P, Wang D,
Traboulsee A. Efficacy of teriflunomide in relapsing multiple
extension study with 8-year follow-up.
sclerosis: phase
Multiple Sclerosis 2011;17:S183–4.
Li DBK, Traboulsee AL, Truffinet P, Dukovic D, O’Connor
PW. Long-term MRI outcomes from patients treated with
teriflunomide: results from a phase 2 extension study.
Multiple Sclerosis 2014;20:102–3.
∗
O’Connor PW, Li D, Freedman MS, Bar-Or A, Rice GP,
Confavreux C, et al. A Phase
study of the safety and
efficacy of teriflunomide in multiple sclerosis with relapses.
Neurology 2006;66(6):894–900.
Additional references
Bruneau 1998
Bruneau JM, Yea CM, Spinella-Jaegle S, Fudali C,
Woodward K, Robson PA, et al. Purification of human
dihydro-orotate dehydrogenase and its inhibition by A77
1726, the active metabolite of leflunomide. Biochemical
Journal 1998;336(Pt 2):299–303.
Cella 1996
Cella DF, Dineen K, Arnason B, Reder A, Webster KA,
Karabatsos G, et al. Validation of the functional assessment
of multiple sclerosis quality of life instrument. Neurology
1996;47(1):129–39.
Cherwinski 1995
Cherwinski HM, McCarley D, Schatzman R, Devens B,
Ransom JT. The immunosuppressant leflunomide inhibits
lymphocyte progression through cell cycle by a novel
mechanism. Journal of Pharmacology and Experimental
Therapeutics 1995;272(1):460–8.
Confavreux 2006
Confavreux C, Vukusic S. Natural history of multiple
sclerosis: a unifying concept. Brain 2006;129(Pt 3):
606–16.
Deage 1998
Deage V, Burger D, Dayer JM. Exposure of T lymphocytes
to leflunomide but not to dexamethasone favors the
production by monocytic cells of interleukin-1 receptor
antagonist and the tissue-inhibitor of metalloproteinases1 over that of interleukin-1beta and metalloproteinases.
European Cytokine Network 1998;9(4):663–8.
DerSimonian 1986
DerSimonian R, Laird N. Meta-analysis in clinical trials.
Controlled Clinical Trials 1986;7(3):177–88.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
28
Fischer 1999
Fischer JS, LaRocca NG, Miller DM, Ritvo PG, Andrews
H, Paty D. Recent developments in the assessment of
quality of life in multiple sclerosis (MS). Multiple Sclerosis
1999;5(4):251–9.
Lublin 2014a
Lublin FD, Reingold SC, Cohen JA, Cutter GR, Sørensen
PS, Thompson AJ. Defining the clinical course of multiple
sclerosis: the 2013 revisions. Neurology 2014;83(3):
278–86.
Greene 1995
Greene S, Watanabe K, Braatz-Trulson J, Lou L. Inhibition
of dihydroorotate dehydrogenase by the immunosuppressive
agent leflunomide. Biochemical Pharmacology 1995;50(6):
861–7.
Lublin 2014b
Lublin FD. New multiple sclerosis phenotypic classification.
European Neurology 2014;72 Suppl:1–5.
Greenland 1985
Greenland S, Robins JM. Estimation of a common effect
parameter from sparse follow-up data. Biometrics 1985;41
(1):55–68.
Hadjigeorgiou 2013
Hadjigeorgiou GM, Doxani C, Miligkos M, Ziakas P,
Bakalos G, Papadimitriou D, et al. A network metaanalysis of randomized controlled trials for comparing the
effectiveness and safety profile of treatments with marketing
authorization for relapsing multiple sclerosis. Journal of
Clinical Pharmacy and Therapeutics 2013;38(6):433–9.
Hamilton 1999
Hamilton LC, Vojnovic I, Warner TD. A771726, the active
metabolite of leflunomide, directly inhibits the activity
of cyclo-oxygenase-2 in vitro and in vivo in a substratesensitive manner. British Journal of Pharmacology 1999;127
(7):1589–96.
Higgins 2011
Higgins JPT, Green S (editors). Cochrane Handbook
for Systematic Reviews of Interventions Version 5.1.0
[updated March 2011]. The Cochrane Collaboration,
2011. Available from www.cochrane-handbook.org.
Karampampa 2012
Karampampa K, Gustavsson A, Miltenburger C, Kindundu
CM, Selchen DH. Treatment experience, burden, and
unmet needs (TRIBUNE) in multiple sclerosis: the costs
and utilities of MS patients in Canada. Journal of Population
Therapeutics and Clinical Pharmacology 2012;19(1):11–25.
Manna 1999
Manna SK, Aggarwal BB. Immunosuppressive leflunomide
metabolite (A77 1726) blocks TNF-dependent nuclear
factor-kappa B activation and gene expression. Journal of
Immunology 1999;162(4):2095–102.
Mantel 1959
Mantel N, Haenszel W. Statistical aspects of the analysis of
data from retrospective studies of disease. Journal of the
National Cancer Institute 1959;22(4):719–48.
McDonald 2001
McDonald WI, Compston A, Edan G, Goodkin D,
Hartung HP, Lublin FD, et al. Recommended diagnostic
criteria for multiple sclerosis: guidelines from the
International Panel on the diagnosis of multiple sclerosis.
Annals of Neurology 2001;50(1):121–7.
Merrill 2009
Merrill JE, Hanak S, Pu SF, Liang J, Dang C, IglesiasBregna D, et al. Teriflunomide reduces behavioral,
electrophysiological, and histopathological deficits in the
Dark Agouti rat model of experimental autoimmune
encephalomyelitis. Journal of Neurology 2009;256(1):
89–103.
O’Connell 2014
O’Connell K, Kelly SB, Fogarty E, Duggan M, Buckley L,
Hutchinson M, et al. Economic costs associated with an
MS relapse. Multiple Sclerosis and Related Disorders 2014;3
(6):678–83.
Oleen-Burkey 2012
Oleen-Burkey M, Castelli-Haley J, Lage MJ, Johnson
KP. Burden of a multiple sclerosis relapse: the patients
perspective. Patient 2012;5(1):57–69.
Korn 2004
Korn T, Magnus T, Toyka K, Jung S. Modulation of
effector cell functions in experimental autoimmune
encephalomyelitis by leflunomide - mechanisms
independent of pyrimidine depletion. Journal of Leukocyte
Biology 2004;76:950–60.
Parisé 2013
Parisé H, Laliberté F, Lefebvre P, Duh MS, Kim E,
Agashivala N, et al. Direct and indirect cost burden
associated with multiple sclerosis relapses: excess costs of
persons with MS and their spouse caregivers. Journal of the
Neurological Sciences 2013;330(1-2):71–7.
Kurtzke 1983
Kurtzke JF. Rating neurological impairment in multiple
sclerosis: an Expanded Disability Status Scale (EDSS).
Neurology 1983;33:1444–52.
Polman 2005
Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP,
Kappos L, et al. Diagnostic criteria for multiple sclerosis:
2005 revisions to the “McDonald Criteria”. Annals of
Neurology 2005;58(6):840–6.
Lublin 1996
Lublin FD, Reingold SC. Defining the clinical course
of multiple sclerosis: results of an international survey.
National Multiple Sclerosis Society (USA) Advisory
Committee on Clinical Trials of New Agents in Multiple
Sclerosis. Neurology 1996;46:907–11.
Polman 2011
Polman CH, Reingold SC, Banwell B, Clanet M, Cohen
JA, Filippi M, et al. Diagnostic criteria for multiple
sclerosis: 2010 revisions to the McDonald criteria. Annals
of Neurology 2011;69(2):292–302.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
29
Poser 1983
Poser CM, Paty DW, Scheinberg L, McDonald WI, Davis
FA, Ebers GC, et al. New diagnostic criteria for multiple
sclerosis: guidelines for research protocols. Annals of
Neurology 1983;13(3):227–31.
RevMan 2015 [Computer program]
The Nordic Cochrane Centre, The Cochrane Collaboration.
Review Manager (RevMan). Version 5.3. Copenhagen:
The Nordic Cochrane Centre, The Cochrane Collaboration,
2015.
Siemasko 1998
Siemasko K, Chong AS, Jäck HM, Gong H, Williams
JW, Finnegan A. Inhibition of JAK3 and STAT6
tyrosine phosphorylation by the immunosuppressive drug
leflunomide leads to a block in IgG1 production. Journal of
Immunology 1998;160(4):1581–8.
Tallantyre 2008
Tallantyre E, Evangelou N, Constantinescu CS. Spotlight
on teriflunomide. International MS Journal 2008;15(2):
62–8.
Tramacere 2015
Tramacere I, Del Giovane C, Salanti G, D’Amico R,
Filippini G. Immunomodulators and immunosuppressants
for relapsing-remitting multiple sclerosis: a network metaanalysis. Cochrane Database of Systematic Reviews 2015,
Issue 9. [DOI: 10.1002/14651858.CD011381]
Tullman 2004
Tullman MJ, Oshinsky RJ, Lublin FD, Cutter GR. Clinical
characteristics of progressive relapsing multiple sclerosis.
Multiple Sclerosis 2004;10(4):451–4.
Vickrey 1995
Vickrey BG, Hays RD, Harooni R, Myers LW, Ellison
GW. A health-related quality of life measure for multiple
sclerosis. Quality of Life Research 1995;4(3):187–206.
Ware 1992
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form
health survey (SF-36). I. Conceptual framework and item
selection. Medical Care 1992;30(6):473–83.
Xu 1995
Xu X, Williams JW, Bremer EG, Finnegan A, Chong AS.
Inhibition of protein tyrosine phosphorylation in T cells by
a novel immunosuppressive agent, leflunomide. Journal of
Biological Chemistry 1995;270(21):12398–403.
Xu 1996
Xu X, Williams JW, Gong H, Finnegan A, Chong AS.
Two activities of the immunosuppressive metabolite
of leflunomide, A77 1726. Inhibition of pyrimidine
nucleotide synthesis and protein tyrosine phosphorylation.
Biochemical Pharmacology 1996;52(4):527–34.
Zagmutt 2015
Zagmutt FJ, Carroll CA. Meta-analysis of adverse events
in recent randomized clinical trials for dimethyl fumarate,
glatiramer acetate and teriflunomide for the treatment of
relapsing forms of multiple sclerosis. International Journal
of Neuroscience 2015;125(11):798–807.
Zeyda 2005
Zeyda M, Poglitsch M, Geyeregger R, Smolen JS, Zlabinger
GJ, Hörl WH, et al. Disruption of the interaction of T
cells with antigen-presenting cells by the active leflunomide
metabolite teriflunomide: involvement of impaired integrin
activation and immunologic synapse formation. Arthritis
and Rheumatism 2005;52(9):2730–9.
References to other published versions of this review
He 2012
He D, Xu Z, Dong S, Zhang H, Zhou H, Wang L, Zhang
S. Teriflunomide for multiple sclerosis. Cochrane Database
of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/
14651858.CD009882.pub2]
∗
Indicates the major publication for the study
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
30
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
Confavreux 2014
Methods
Randomized, double-blind, placebo-controlled, phase 3 trial (TOWER study)
Population included in data analyses: all randomly assigned participants who received at
least 1 dose of study drug or placebo
Did not use the ITT analysis principle
Participants
Inclusion criteria: people aged 18-55 years; with relapsing MS meeting 2005 McDonald
criteria; with or without underlying progression; an EDSS score ≤ 5.5 points; at least 1
relapse in the previous year or at least 2 relapses in the previous 2 years, and no relapse
in the 30 days before randomization
Key exclusion criteria: people with other relevant diseases; pregnant, breastfeeding or
planning to conceive or father a child during the study; previously or concomitantly receiving cytokine therapy, IFNβ or glatiramer acetate within 3 months of randomization;
ever using natalizumab or other immunosuppressive agents
1169 participants were randomly assigned in a 1:1:1 ratio to receive 3 different interventions. 1 participant in placebo group, 1 participant in teriflunomide 7 mg/day group
and 2 participants in teriflunomide 14 mg/day group did not receive treatment
Baseline demographic and clinical characteristics were generally well balanced among
the study groups
Summary of participant characteristics at baseline (placebo: G1 (n = 389), teriflunomide
7 mg/day: G2 (n = 408), teriflunomide 14 mg/day: G3 (n = 372)
Age (mean ± SD): G1 = 38.1 ± 9.1 years, G2 = 37.4 ± 9.4 years, G3 = 38.2 ± 9.4 years
Women: G1 = 273 (70%), G2 = 300 (74%), G3 = 258 (69%)
Race: white G1 = 318 (82%), G2 = 329 (81%), G3 = 313 (84%); Asian G1 = 60 (15%)
, G2 = 60 (15%), G3 = 49 (13%); black G1 = 7 (2%), G2 = 8 (2%), G3 = 7 (2%); other
G1 = 4 (1%), G2 = 11 (3%), G3 = 3 (1%)
Region: Western Europe and Tunisia G1 = 121 (31%), G2 = 127 (31%), G3 = 120
(32%); Eastern Europe G1 = 117 (30%), G2 = 124 (30%), G3 = 116 (31%); America
G1 = 84 (22%), G2 = 92 (23%), G3 = 81 (22%); Asia and Australia G1 = 67 (17%),
G2 = 65 (16%), G3 = 55 (15%)
Time from first symptoms of MS (mean ± SD): G1 = 7.64 ± 6.70 years, G2 = 8.18 ± 6.
75 years, G3 = 8.18 ± 6.73 years
Time since most recent relapse onset (mean ± SD): G1 = 5.29 ± 3.41 months, G2 = 5.
18 ± 3.41 months, G3 = 5.33 ± 3.32 months
Relapses per participant: within previous year (mean ± SD): G1 = 1.4 ± 0.8, G2 = 1.4 ±
0.7, G3 = 1.4 ± 0.7; within previous 2 years: G1 = 2.1 ± 1.1, G2 = 2.1 ± 1.1, G3 = 2.1
± 1.2
MS subtype: relapsing-remitting G1 = 379 (97%), G2 = 393 (96%), G3 = 366 (99%)
; secondary progressive G1 = 4 (1%), G2 = 3 (1%), G3 = 2 (1%); progressive relapsing
G1 = 6 (2%), G2 = 12 (3%), G3 = 2 (1%)
Use of MS medication in the previous 2 years: G1 = 135 (35%), G2 = 123 (30%), G3
= 126 (34%); IFNβ-1a G1 = 59 (15%), G2 = 63 (15%), G3 = 64 (17%); glatiramer
acetate G1 = 52 (13%), G2 = 47 (12%), G3 = 37 (10%); IFNβ-1b G1 = 38 (10%), G2
= 27 (7%), G3 = 35 (9%)
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
31
Confavreux 2014
(Continued)
EDSS total score (mean ± SD): G1 = 2.69 ± 1.36, G2 = 2.71 ± 1.39, G3 = 2.71 ± 1.35
FIS score (mean ± SD): G1 = 54.67 ± 37.89, G2 = 56.16 ± 38.20, G3 = 55.25 ± 38.26
Interventions
Experimental group 1: oral teriflunomide 7 mg once daily (n = 408)
Experimental group 2: oral teriflunomide 14 mg once daily (n = 372)
Control group: matching oral placebo once daily (n = 389)
Core treatment period: 48-152 weeks (maximum treatment duration 173 weeks). Treatment duration was variable, ending 48 weeks after the last participant was included. The
median duration of study treatment was similar across all groups (581 days (IQR 392756) in the placebo group vs. 556 days (IQR 385-749) in the teriflunomide 7 mg group
vs. 588 days (IQR 351-765) in the teriflunomide 14 mg group)
Outcomes
Primary outcome:
• annualized relapse rate (number of relapses per participant-year)
Secondary outcomes:
• time to 12 week sustained accumulation of disability
• time to first relapse
• proportion of participants free from relapses
• proportion of participants free of accumulation of disability
• change from baseline in EDSS score at week 48
• change in FIS at week 48
• change in SF-36 scores at week 48
Relapse was defined as new or worsening clinical signs or symptoms lasting at least 24
hours without fever. Protocol-defined relapses constituted an increase of either 1 point
in at least 2 EDSS functional system scores, or 2 points in 1 EDSS functional system
score (excluding bowel and bladder function, and cerebral function), or 0.5 points in
total EDSS score from a previous clinically stable assessment
Sustained accumulation of disability was defined as an increase from baseline of at least 1
EDSS point (or ≥ 0.5 points when baseline EDSS score was > 5.5 points) that persisted
for at least 12 weeks
Notes
The investigators obtained the data and the sponsor (Genzyme, owned by Sanofi-Aventis)
analyzed the data. Both the sponsor and the authors interpreted the data
ClinicalTrials.gov number: NCT00751881
Risk of bias
Bias
Authors’ judgement
Random sequence generation (selection Low risk
bias)
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Support for judgement
Quote: “An interactive voice recognition
system generated an allocation sequence
using a permuted-block randomisation
schedule with stratification according to
study site and baseline EDSS score (≤3.5
or > 3.5)”
Comment: sequence generation was adequate
32
Confavreux 2014
(Continued)
Allocation concealment (selection bias)
Low risk
Quote: “Randomisation was done centrally, via an interactive voice recognition
system”
Comment: allocation concealment was adequate
Blinding of participants and personnel Low risk
(performance bias)
All outcomes
Quote: “Patients, individuals administering the interventions, and those assessing
the outcomes were masked to treatment assignment” “The experimental drugs were
identical in taste and appearance”
Comment: participants and personnel were
blinded to the allocated interventions
Blinding of outcome assessment (detection High risk
bias)
All outcomes
Quote: “Those assessing the outcomes were
masked to treatment assignment.” “A treating neurologist was responsible for assessment of patient eligibility, supervision of
administration of study drug or placebo,
recording of adverse events, and assessment of relapses.” “An examining neurologist, certified in the Neurostatus system for
consistent EDSS assessment, 12 assigned
EDSS scores at screening, randomisation,
and every 12 weeks until the last treatment
visit, and on any unscheduled visits for assessment of suspected relapse or disability
worsening”
Comment: treating neurologist who
recorded adverse events was responsible for
assessment of relapses, blinding of relapse
assessment was probably not adequate
Incomplete outcome data (attrition bias)
All outcomes
High risk
According to the Figure 1 (Trial profile),
overall, 348 (29.8%) participants withdrew
from study (115 (29.6%) participants in
placebo group, 119 (29.2%) participants
in teriflunomide 7 mg/day group and 114
(30.6%) participants in teriflunomide 14
mg/day group)
Comment: to a large degree, missing data
and reasons were not balanced between
groups. The high overall dropout rate of
29.8% over a period of 48 weeks had potential impacts on the results, a high risk of
attrition bias existed
Selective reporting (reporting bias)
Low risk
All listed outcomes were reported adequately. Risk of reporting bias was low
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
33
Confavreux 2014
Other bias
(Continued)
High risk
Quote: “The study was sponsored by Genzyme.” “Data were obtained by the investigators and analysed by the sponsor (Genzyme),” “Interpretation of the data was
done by the sponsor and the authors,” “4
co-authors (TB, J-LD, DD, and PT) of the
published paper are all employees of Genzyme”
Comment: conflicts of interest probably
existed. There was probably a high risk of
bias
Freedman 2012
Methods
Phase 2 multicentre, placebo-controlled, double-blind, randomized study
Follow-up period: 48 weeks
Population included in data analyses: all randomly assigned participants exposed to at
least 1 dose of any study medication
Did not use the ITT analysis principle
Participants
Inclusion criteria: people aged 18-55 years; with a diagnosis of MS as per the 2005
McDonald criteria; with a relapsing clinical course; with or without progression; having
a score of ≤ 5.5 on the EDSS; with no relapse for 8 weeks; having a clinically stable
condition for 4 weeks pre-study; receiving a stable dose of IFNβ for at least 26 weeks
before screening
Baseline demographic and disease characteristics were well balanced among the groups
Summary of baseline characteristics of participants in the initial 24-week study (placebo
+ IFNβ: G1 (n = 41), teriflunomide 7 mg + IFNβ: G2 (n = 37), teriflunomide 14 mg
+ INFβ: G3 (n = 38)
Age (mean ± SD): G1 = 39.2 ± 9.0 years, G2 = 41.4 ± 6.8 years, G3 = 39.6 ± 8.1 years
Women: G1 = 31 (75.6%), G2 = 25 (67.6%), G3 = 25 (65.8%)
White: G1 = 40 (97.6%), G2 = 34 (91.9%), G3 = 38 (100%)
MS subtype: relapsing-remitting: G1 = 38 (92.7%), G2 = 30 (81.1%), G3 = 34 (89.
5%); secondary progressive: G1 = 2 (4.9%), G2 = 2 (5.4%), G3 = 3 (7.9%); progressive
relapsing: G1 = 1 (2.4%), G2 = 5 (13.5%), G3 = 1 (2.6%)
Number of relapse within the past 12 months (mean ± SD): G1 = 0.9 ± 0.9, G2 = 0.6
± 0.8, G3 = 0.9 ± 0.8
Proportion of participants with ≥ 1 relapse in the past 12 months: G1 = 58.5%, G2 =
48.6%, G3 = 65.8%
EDSS score: mean ± SD G1 = 2.6 ± 1.3, G2 = 2.4 ± 1.4, G3 = 2.5 ± 1.6; median (range)
G1 = 2.5 (0-5.5), G2 = 2.0 (0-5.5), G3 = 2.5 (0-5.5)
Proportion with IFNβ neutralizing antibodies: < 20 titre G1 = 86.5%, G2 = 80.6%, G3
= 87.9%; 20-640 titre: G1 = 10.8%, G2 = 11.1%, G3 = 9.1%; > 640 titre: G1 = 2.7%,
G2 = 8.3%, G3 = 3.0%
The number of T1-Gd lesions: 0: G1 = 77.5%, G2 = 78.4%, G3 = 78.9%; ≥ 1: G1 =
22.5%, G2 = 21.6%, G3 = 21.1%
Baseline state of IFNβ: high dose: G1 = 68.3%, G2 = 67.6%, G3 = 63.2%; low dose:
G1 = 31.7%, G2 = 32.4%, G3 = 36.8%
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
34
Freedman 2012
(Continued)
Interventions
Experimental group 1: teriflunomide 7 mg/day orally added to IFNβ
Experimental group 2: teriflunomide 14 mg/day orally added to IFNβ
Control group: matching placebo orally added to IFNβ
The ongoing IFNβ regimens were IFN-1a (Avonex; Biogen Idec, Cambridge, MA), 30
g IM once a week (classified as low-dose), IFNβ-1a (Rebif; EMD Serono Inc., Rockland,
MA), 22 or 44 g SC 3 times per week (classified as low-dose and high-dose, respectively)
, and IFNβ-1b (Betaseron; Bayer HealthCare Pharmaceuticals Inc, Montville, NJ), 0.
25 mg SC every other day (classified as high-dose)
Outcomes
Primary outcome:
• safety and tolerability (treatment-emergent adverse events occurring with an
incidence > 10%)
Secondary outcomes:
• annualized relapse rates
• MRI activity: the total number of Gd-enhancing T1 lesions and the total Gdenhancing T1 lesion volume per MRI scan
• burden of disease: least squares mean change from baseline and least squares mean
difference from placebo
• mean number of unique active lesions per scan
• volume of post-Gd T1 hypointense lesions (black holes)
• T2 lesion component volume change from baseline
• atrophy change from baseline
• white matter change from baseline
• grey matter change from baseline
• Z4 composite score change from baseline (the Z4 composite score integrated
quantitative measures of volume of T1-Gd lesions, burden of disease, volume of T1hypointense lesions and the proportion of total intracranial contents segmented as
CSF. The Z4 score was defined as the sum of individual Z scores derived from each of
these 4 parameters)
A relapse was defined as the appearance of a new clinical sign or symptom or worsening
of a previous symptom that persisted for ≥ 24 hours in the absence of fever
Notes
NCT00489489 [24-week study] and NCT00811395 [24-week extension]. This study
was sponsored by Sanofi-Aventis
Risk of bias
Bias
Authors’ judgement
Support for judgement
Random sequence generation (selection Low risk
bias)
The authors reported that randomization
was stratified by country and IFN regimen (high-dose or low-dose). This was an
international multicentre clinical trial, the
random sequence generation was probably
made by software
Allocation concealment (selection bias)
The authors did not describe the method
of allocation concealment. This was an in-
Low risk
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
35
Freedman 2012
(Continued)
ternational multicentre clinical trial, central randomization was probably used
Blinding of participants and personnel High risk
(performance bias)
All outcomes
Quote: “A phase II
multicenter, placebo controlled, double-blind, randomised study comparing 2 doses of teriflunomide in patients with relapsing MS
receiving a stable dose of IFNβ was conducted”
Comment: IFNβ regimens were diverse.
It was not a truly double-blind, doubledummy study
Blinding of outcome assessment (detection High risk
bias)
All outcomes
Quote: “Each occurrence of relapse was
confirmed by the treating neurologist,
based on objective assessments by an independent evaluator who was blinded to
treatment allocation.” “Adverse events were
reported by the patient or the investigator”
Comment: relapse was confirmed by the
treating neurologist, who was also responsible for reporting. Blinding of outcome assessment was probably not adequate
Incomplete outcome data (attrition bias)
All outcomes
High risk
According to the study disposition, 118
participants were randomly assigned. 2 participants (1 in each teriflunomide group)
were excluded before treatment because of
protocol violations, leaving 116 exposed to
study medication for 24 weeks. 86 participants entered the 24-week extension phase.
75 participants completed 1 year. 43 (36.
4%) participants withdrew from study at
48 weeks
Comment: the authors did not report the
reasons why some participants were not
rolled over into extension. Most of reasons for drop-outs differed between groups.
Missing data and reasons were not carefully recorded and did not balance between
groups. The high overall rate of drop-outs
(36.4%) and the unbalanced reasons for
drop-outs contributed to a high risk of attrition bias
Selective reporting (reporting bias)
Low risk
All listed outcomes were reported adequately
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
36
Freedman 2012
Other bias
(Continued)
High risk
Quote: “The study funding was supported
by Sanofi-Aventis”
Comment: conflicts of interest probably
existed. There was probably a high risk of
bias
NCT01252355
Methods
Phase 3, multicentre, placebo-controlled, double-blind, randomized study (TERACLES
study)
Treatment duration: 24-108 weeks
ITT population: all randomized and treated participants. Participants were considered in
the treatment group to which they were randomized regardless of the drug they actually
received
Participants
Inclusion criteria: aged 18-55 years; diagnosis of MS by McDonald’s criteria; participant
with relapsing forms of MS treated with IFNβ; stable dose of IFNβ for at least 6 months
prior to randomization; disease activity in the 12 months prior to randomization and after
first 3 months of IFNβ treatment (at least 1 relapse supported by EDSS or equivalent
neurological examination, or, at least 1 brain or spinal cord MRI with at least 1 T1 Gdenhancing lesion)
Exclusion criteria: McDonald’s criteria for MS diagnosis not met at time of screening
visit; EDSS score > 5.5 at screening visit; not treated with a stable dose of IFNβ for
≥ 6 months prior to randomization or not tolerating IFNβ or not expected to remain
on IFNβ for the duration of the study; a relapse within 30 days prior randomization;
human immunodeficiency virus-positive; prior or concomitant use of cladribine, mitoxantrone or other immunosuppressant agents such as azathioprine, cyclophosphamide,
ciclosporin, methotrexate, mycophenolate or fingolimod in previous 6 months; prior use
in the 3 months preceding randomization of cytokine therapy (except baseline IFNβ),
glatiramer acetate or intravenous immunoglobulins, or concomitant use of these treatments; prior or concomitant use of natalizumab (Tysabri®) in previous 6 months; pregnant, breastfeeding or planning to become pregnant during the study
Baseline demographic and clinical characteristics were generally well balanced among
the study groups
Summary of baseline characteristics of participants (placebo + IFNβ: G1 (n = 177),
teriflunomide 7 mg + IFNβ: G2 (n = 178), teriflunomide 14 mg + INFβ: G3 (n = 179)
Age (mean ± SD): G1 = 38.3 ± 8.9 years, G2 = 38.7 ± 9.5 years, G3 = 37.7 ± 9.2 years
Women: G1 = 113 (63.8%), G2 = 125 (70.2%), G3 = 114 (63.7%)
Region of enrolment: America G1 = 33 (32.8%), G2 = 30 (16.9%), G3 = 37 (20.7%);
Western Europe G1 = 86 (48.6%), G2 = 86 (48.3%), G3 = 79 (44.1%); Eastern Europe
G1 = 51 (28.8%), G2 = 51 (28.7%), G3 = 56 (31.3%); Asia, Africa and Australia G1 =
7 (4.0%), G2 = 11 (6.2%), G3 = 7 (3.9%)
Time since first diagnosis of MS (mean ± SD): G1 = 7.0 ± 5.6 years, G2 = 6.6 ± 5.6
years, G3 = 6.8 ± 5.9 years
MS subtype: relapsing-remitting: G1 = 174 (98.3%), G2 = 173 (97.2%), G3 = 175 (97.
8%); secondary progressive: G1 = 2 (1.1%), G2 = 3 (1.7%), G3 = 4 (2.2%); progressive
relapsing: G1 = 1 (0.6%), G2 = 2 (1.1%), G3 = 0 (0%)
Number of relapse within the past 12 months (median (range)): G1 = 1 (0-4), G2 = 1
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
37
NCT01252355
(Continued)
(0-3), G3 = 1 (0-4)
Number of relapse within the past 2 years (median (range)): G1 = 2 (0-6), G2 = 2 (0-8)
, G3 = 2 (0-8)
Time since most recent MS relapse onset) (median (range)): G1 = 5.0 (1.0-75.0) months,
G2 = 5.0 (1.0-36.0) months, G3 = 4.0 (1.0-174.0) months
EDSS score (mean ± SD): G1 = 2.67 ± 1.25, G2 = 2.63 ± 1.37, G3 = 2.64 ± 1.18
Dose level of IFNβ based on IVRS: high dose: G1 = 120 (67.8%), G2 = 128 (71.9%),
G3 = 120 (67.0%); low dose: G1 = 57 (32.2%), G2 = 50 (28.1%), G3 = 59 (33.0%)
Interventions
Experimental group 1: teriflunomide 7 mg once daily + IFNβ (any of the IFNβ) (n =
178)
Experimental group 2: teriflunomide 14 mg once daily + IFNβ (any of the IFNβ) (n =
179)
Control group: matching placebo (for teriflunomide) once daily + IFNβ (any of the
IFNβ) (n = 177)
Outcomes
Primary outcome:
• annualized relapse rate = total number of confirmed relapses that occurred during
the treatment period divided by the total number of participant-years treated. Each
episode of relapse (appearance, or worsening of a clinical symptom that was stable for
at least 30 days, that persisted for a minimum of 24 hours in the absence of fever) was
confirmed by an increase in EDSS score or Functional System scores
Secondary outcomes:
• number of Gd-enhancing T1-lesions as measured by brain MRI
• time to 12-week sustained disability progression as assessed by EDSS
• volume of Gd-enhancing T1-lesions
• change from baseline in total lesion volume
• time to first confirmed relapse
• change from baseline in FIS total score
• change from baseline in Short Form Generic Health Survey-36 Items, version 2
Summary Score
• resource utilization when relapse
• overview of adverse events
• liver function
Notes
The recruitment initiated in January 2011 was discontinued in December 2012 following
the decision of the Sponsor (Sanofi-Aventis) to discontinue the study, the common
treatment end date was defined as 28 February 2013 (treatment duration 24-108 weeks)
846 participants were screened at 185 sites in 28 countries
ClinicalTrials.gov number: NCT01252355
Risk of bias
Bias
Authors’ judgement
Random sequence generation (selection Low risk
bias)
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Support for judgement
Quote: “Randomisation was stratified by
investigational site and Interferon-β dose
level (high/low)”
Comments: this was an international mul38
NCT01252355
(Continued)
ticentre clinical trial, the random sequence
generation was probably made by software
Allocation concealment (selection bias)
Low risk
Quote: “Assignment to groups was done
centrally using an IVRS in a 1:1:1 ratio after
confirmation of selection criteria”
Comments: allocation concealment was
adequate
Blinding of participants and personnel High risk
(performance bias)
All outcomes
Any of the IFNβ was used, as long as the
IFNβ was approved for marketed use in the
country where the participant was enrolled
Comments: IFNβ regimens were diverse.
It was not a truly double-blind, doubledummy study
Blinding of outcome assessment (detection High risk
bias)
All outcomes
Participant, investigator and outcomes assessor were blinded
Comments: unclear whether all outcome
assessors were independent of the treating
neurologist who recorded and managed adverse events
Incomplete outcome data (attrition bias)
All outcomes
High risk
Study was prematurely terminated by the
sponsor. All participants did not complete
the study
Comments: high risk of attrition bias existed
Selective reporting (reporting bias)
Low risk
All pre-set outcomes in the protocol were
described in the results
Comments: reporting bias was low
Other bias
High risk
Quote: “The study was sponsored by
Sanofi-Aventis”
Comment: conflicts of interest probably
existed. There was probably a high risk of
bias
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
39
O’Connor 2011
Methods
Phase 3, randomized, double-blind, placebo-controlled, parallel-group study (TEMSO
study)
Follow-up period: 108 weeks
Population included in data analyses: people who underwent randomization and were
exposed to study medication for at least 1 day
Did not use the ITT analysis principle
Participants
Inclusion criteria: people aged 18-55 years; meeting the 2001 McDonald criteria for a
diagnosis of MS; with a relapsing clinical course; with or without progression; having a
score of ≤ 5.5 on the EDSS; having at least 2 clinical relapses in the previous 2 years or
1 relapse during the preceding year, but no relapses in the 60 days before randomization
Exclusion criteria: people with other systemic diseases; pregnant; planning to conceive
during the trial period
All baseline characteristics were well matched among the groups
Summary of participant characteristics at baseline (placebo: G1 (n = 363), teriflunomide
7 mg: G2 (n = 366), teriflunomide 14 mg: G3 (n = 359)
Age (mean ± SD): G1 = 38.4 ± 9.0 years, G2 = 37.4 ± 9.0 years, G3 = 37.8 ± 8.2 years
Women: G1 = 275 (75.8%), G2 = 255 (69.7%), G3 = 225 (71.0%)
White: G1 = 356 (98.3%), G2 = 355 (97.3%), G3 = 347 (96.9%)
Region: Western Europe G1 = 167 (46.0%), G2 = 167 (45.6%), G3 = 170 (47.4%);
Eastern Europe G1 = 114 (31.4%), G2 = 116 (31.7%), G3 = 108 (30.1%); Americas
G1 = 82 (22.6%), G2 = 83 (22.7%), G3 = 81 (22.6%)
Time from first symptom of MS (mean ± SD): G1 = 8.6 ± 7.1 years, G2 = 8.8 ± 6.8
years, G3 = 8.7 ± 6.7 years
Relapse (mean ± SD): in previous year G1 = 1.4 ± 0.7, G2 = 1.4 ± 0.7, G3 = 1.3 ± 0.7;
in previous 2 years G1 = 2.2 ± 1.0, G2 = 2.3 ± 1.2, G3 = 2.2 ± 1.0
MS subtype: relapsing-remitting G1 = 329 (90.6%), G2 = 333 (91.0%), G3 = 333
(92.8%); secondary progressive G1 = 22 (6.1%), G2 = 17 (4.6%), G3 = 12 (3.3%);
progressive relapsing G1 = 12 (3.3%), G2 = 16 (4.4%), G3 = 14 (3.9%)
Use of DMT in previous 2 years: G1 = 90 (24.8%), G2 = 102 (27.9%), G3 = 102 (28.
4%); IFNβ-1a G1 = 58 (16.0%), G2 = 74 (20.2%), G3 = 62 (17.3%); IFNβ-1b G1 =
18 (5.0%), G2 = 22 (6.0%), G3 = 27 (7.5%); glatiramer acetate G1 = 36 (9.9%), G2 =
23 (6.3%), G3 = 43 (12.0%)
EDSS score (mean ± SD): G1 = 2.68 ± 1.34, G2 = 2.68 ± 1.34, G3 = 2.67 ± 1.24
FIS score (mean ± SD): G1 = 53.2 ± 37.9, G2 = 50.4 ± 35.6, G3 = 50.3 ± 35.9
Total lesion volume on MRI (mean ± SD): G1 = 19.34 ± 18.94 mL, G2 = 20.37 ± 20.
59 mL, G3 = 18.08 ± 17.49 mL
Number of participants with Gd-enhancing lesions: G1 = 137 (38.2%), G2 = 127 (35.
3%), G3 = 125 (35.2%)
Number of Gd-enhancing lesions on T1-weighted images (mean ± SD): G1 = 1.66 ± 3.
55, G2 = 1.50 ± 3.96, G3 = 1.81 ± 5.17
Volume of hypointense lesions on T1-weighted images (mean ± SD): G1 = 3.26 ± 3.64,
G2 = 3.35 ± 3.96, G3 = 2.91 ± 3.25
Brain parenchymal fraction (mean ± SD): G1 = 0.76 ± 0.02, G2 = 0.76 ± 0.02, G3 = 0.
76 ± 0.02
Interventions
Experimental group 1: oral teriflunomide 7 mg once daily (n = 366)
Experimental group 2: oral teriflunomide 14 mg once daily (n = 359)
Control group: matching oral placebo once daily (n = 363)
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
40
O’Connor 2011
(Continued)
Outcomes
Primary outcome:
• annualized relapse rate (defined as the number of confirmed relapses per
participant-year). A relapse was defined as the appearance of a new clinical sign or
symptom, or clinical worsening of a previous sign or symptom that had been stable for
at least 30 days and that persisted for a minimum of 24 hours in the absence of fever
Secondary outcomes:
• time to 12-week sustained disability progression. Sustained disability progression
was defined as an increase from baseline of at least 1.0 point in the EDSS score (or at
least 0.5 points for participants with a baseline EDSS score > 5.5) that persisted for at
least 12 weeks
• total lesion volume
• number of Gd-enhancing lesions on T1-weighted images
• volume of hypointense lesion components on T1-weighted images
• number of unique active lesions (defined as the number of Gd-enhancing lesions
on T1-weighted images or new or enlarged lesions on T2-weighted images, without
double counting)
• brain atrophy
• participant-reported fatigue, assessed using the FIS
A relapse was defined as the appearance of a new clinical sign or symptom, or clinical
worsening of a previous sign or symptom that had been stable for at least 30 days and
that persisted for a minimum of 24 hours in the absence of fever. Confirmed relapses
required an increase of 1 point in each of 2 EDSS functional-system scores or of 2 points
in 1 EDSS functional-system score (excluding bowel and bladder function and cerebral
function) or an increase of 0.5 points in the EDSS score from the previous clinically
stable assessment
Sustained disability progression was defined as an increase from baseline of at least 1.
0 point in the EDSS score (or at least 0.5 points for participants with a baseline EDSS
score > 5.5) that persisted for at least 12 weeks
Notes
This was the Teriflunomide Multiple Sclerosis Oral (TEMSO) trial, sponsored by SanofiAventis. The investigators collected the data and the sponsor analysed the data
ClinicalTrials.gov number: NCT00134563
Risk of bias
Bias
Authors’ judgement
Random sequence generation (selection Low risk
bias)
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Support for judgement
The authors reported that randomization
was stratified according to the baseline
EDSS score (≤ 3.5 or > 3.5) and according to trial site, with a block size of 6. We
wrote to the principal author for random
sequence generation, the principal author
described that the IVRS assigned the randomization number from a list that was
loaded in the database
Comment: sequence generation was adequate
41
O’Connor 2011
(Continued)
Allocation concealment (selection bias)
Low risk
The method of allocation concealment was
not reported. We wrote to the principal author, the principal author offered central
randomization via an IVRS
Comment: allocation concealment was adequate
Blinding of participants and personnel Low risk
(performance bias)
All outcomes
Quote: “Treating neurologist was unaware
of treatment assignments but was aware of
any side effects that could potentially be
related to active therapy”
The principal author described the study
medication teriflunomide (7 mg and 14
mg) and placebo were supplied as identical
tablets
Comment: participants and personnel were
blinded to the allocated interventions
Blinding of outcome assessment (detection High risk
bias)
All outcomes
Quote: “A treating neurologist at each site
was responsible for recording and managing adverse events, assessing relapses, and
monitoring safety assessments.” “An independent, specially trained and certified
examining neurologist determined all the
EDSS scores and performed all assessments
of functional systems.” “The examining
neurologists were unaware of treatment assignments, only the treating neurologist
was aware of any side effects that could potentially be related to active therapy”
Comment: treating neurologist who
recorded adverse events was responsible for
assessment of relapses, blinding of relapse
assessment was probably not adequate
Incomplete outcome data (attrition bias)
All outcomes
According to the Figure 1, 104 participants
in placebo group, 92 participants in teriflunomide 7 mg group and 96 participants
in teriflunomide 14 mg group discontinued study treatment
Quote: “Of the patients who discontinued
the study medication prematurely, 31, 22,
and 20 patients in the placebo, teriflunomide 7 mg group, and higher-dose teriflunomide groups, respectively, completed
the planned follow-up”
Comment: overall, 219 (20.1%) participants were lost-to follow-up (73 (20.1%)
Unclear risk
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
42
O’Connor 2011
(Continued)
participants in placebo group, 70 (19.1%)
participants in teriflunomide 7 mg group,
76 (21.2%) participants in teriflunomide
14 mg group). There was no sufficient information to understand the reasons for
study discontinuation and their balance
among the 3 groups
Selective reporting (reporting bias)
Low risk
All listed outcomes were reported adequately
Other bias
High risk
Quote: “The study was sponsored by
Sanofi-Aventis.” “Data were collected by
the investigators and analysed by the sponsor.” “3 co-authors (HB, PT and LW) of the
published paper were affiliated to SanofiAventis”
Comment: conflicts of interest probably
existed. There was probably a high risk of
bias
Vermersch 2014
Methods
Phase 3, multicentre, parallel-group, rater-blinded study (TENERE study)
Population included in data analyses: efficacy analyses were conducted on the ITT population, which included all randomized participants. The safety analysis included all
randomized participants exposed to study medication
Participants
Inclusion criteria: people aged≥ 18 years; meeting the 2005 McDonald criteria for a
diagnosis of MS; having a relapsing clinical course; with or without progression; with an
EDSS score ≤ 5.5 at screening; being relapse free for 30 days prior to randomization
Exclusion criteria: people with prior use of SC IFNβ-1a, teriflunomide or leflunomide;
prior or ongoing use of natalizumab, cladribine, mitoxantrone or other immunosuppressants; use of other interferons, glatiramer acetate, intravenous immunoglobulins or
cytokine therapy within 3 months; having other relevant systemic illnesses; being pregnant, breast-feeding, or both; planning to conceive
Baseline demographics and characteristics were balanced except for a lower DMT use in
the past 2 years in the teriflunomide 14 mg group compared with the IFNβ-1a group
Summary of participant characteristics at baseline (IFNβ-1a: G1 (n = 104), teriflunomide
7 mg: G2 (n = 109), teriflunomide 14 mg: G3 (n = 111)
Age (mean ± SD): G1 = 37.0 ± 10.6 years, G2 = 35.2 ± 9.2 years, G3 = 36.8 ± 10.3 years
Female: G1 = 71 (68.3%), G2 = 70 (64.2%), G3 = 78 (70.3%)
White: G1 = 104 (100%), G2 = 109 (100%), G3 = 111 (100%)
Region: Eastern Europe G1 = 35 (33.7%), G2 = 39 (35.8%), G3 = 41 (36.9%); Western
Europe and Africa G1 = 62 (59.6%), G2 = 62 (56.9%), G3 = 64 (57.7%); Americas G1
= 7 (6.7%), G2 = 8 (7.3%), G3 = 6 (5.4%)
Time since first symptom of MS (mean ± SD): G1 = 7.7 ± 7.6 years, G2 = 7.0 ± 6.9
years, G3 = 6.6 ± 7.6 years
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
43
Vermersch 2014
(Continued)
Relapse (mean ± SD): within previous year G1 = 1.2 ± 1.0, G2 = 1.3 ± 0.8, G3 = 1.4 ±
0.8; within previous 2 years G1 = 1.7 ± 1.1, G2 = 1.7 ± 0.9, G3 = 1.7 ± 0.9
MS subtype: relapsing-remitting G1 = 104 (100%), G2 = 109 (100%), G3 = 108 (97.
3%); secondary progressive G1 = 0, G2 = 0, G3 = 1 (0.9%); progressive relapsing G1 =
0, G2 = 0, G3 = 2 (1.8%)
Use of DMT in previous 2 years: G1 = 25 (24.0%), G2 = 23 (21.1%), G3 = 13 (11.7%)
; IFNβ-1a G1 = 6 (5.8%), G2 = 6 (5.5%), G3 = 3 (2.7%); IFNβ-1b G1 = 10 (9.6%),
G2 = 9 (8.3%), G3 = 5 (4.5%); glatiramer acetate G1 = 12 (11.5%), G2 = 10 (9.2%),
G3 = 7 (6.3%)
Baseline EDSS score (mean ± SD): G1 = 2.0 ± 1.2, G2 = 2.0 ± 1.2, G3 = 2.3 ± 1.4
Baseline FIS score (mean ± SD): G1 = 34.2 ± 32.7, G2 = 39.5 ± 34.8, G3 = 42.5 ± 37.8
Interventions
Experimental group 1: oral teriflunomide 7 mg once daily (n = 109)
Experimental group 2: oral teriflunomide 14 mg once daily (n = 111)
Control group: IFNβ-1a 44 µg, SC injection 3 times per week (n = 104)
Treatment duration: 48-115 weeks. The study was completed 48 weeks after the last participant was randomized, resulting in a variable duration of follow-up. Median duration
of exposure was 60.1 weeks in the IFNβ-1a group, 66.6 weeks in the teriflunomide 7 mg
group and 64.2 weeks in the teriflunomide 14 mg group. Median duration of exposure
for all treatment groups was 63.6 weeks; actual maximum exposure was 115 weeks in
any group
Outcomes
Primary outcome:
• time to failure, defined as first occurrence of confirmed relapse or permanent
treatment discontinuation for any cause
Secondary outcomes:
• annualized relapse rate (number of confirmed relapses during the treatment
period per participant-year)
• changes in participant-reported fatigue (using the FIS)
• treatment satisfaction (using the Treatment Satisfaction Questionnaire for
Medication (TSQM, version 1.4), with domains for effectiveness, adverse effects,
convenience and global satisfaction
• safety and tolerability
Relapse criteria required the appearance of a new clinical sign/symptom or clinical worsening of a previous sign/symptom (previously stable for at least 30 days) that persisted
for at least 24 hours without fever
Notes
Study funded by Genzyme, a Sanofi company. Editorial support was provided by Meg
Church, Fishawack Communications, Ltd, also funded by Genzyme
ClinicalTrials.gov number: NCT00883337
Risk of bias
Bias
Authors’ judgement
Random sequence generation (selection Low risk
bias)
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Support for judgement
Quote: “Patients were randomised 1:1:1
to teriflunomide 7 mg or 14 mg (doubleblind) or IFNβ-1a (open-label), and stratified by country (Americas, Eastern Europe,
44
Vermersch 2014
(Continued)
Western Europe and Africa) and baseline
EDSS score (≤3.5 or >3.5)”
Comment: this was an international multicentre clinical trial, the random sequence
generation was probably made by software
Allocation concealment (selection bias)
Low risk
Comment: this was an international multicentre clinical trial, central randomization
was probably used
Blinding of participants and personnel High risk
(performance bias)
All outcomes
Participants were randomized 1:1:1 to teriflunomide 7 mg or 14 mg (double-blind)
or IFNβ-1a (open-label)
Comment: control (IFNβ-1a) group was
open-label
Blinding of outcome assessment (detection High risk
bias)
All outcomes
Quote: “The treating neurologist was responsible for managing adverse events, and
relapse and safety assessments, while an examining neurologist scored the Functional
Systems and EDSS. The examining neurologist remained blinded to treatment and
associated adverse events”
Comment: treating neurologist who managed adverse events was responsible for assessment of relapses, blinding of relapse assessment was probably not adequate
Incomplete outcome data (attrition bias)
All outcomes
Unclear risk
The number and reasons of drop-outs from
the study were not reported in the published article
Comment: incomplete outcome data were
unclear, the risk of attrition bias was unclear
Selective reporting (reporting bias)
Low risk
All listed outcomes were reported adequately
Other bias
High risk
Quote: “This study was funded by Genzyme, a Sanofi company. Editorial support
was provided by Meg Church, Fishawack
Communications, Ltd, also funded by
Genzyme, a Sanofi company”
Comment: conflicts of interest probably
existed. There was probably a high risk of
bias
CSF: cerebrospinal fluid; DMT: disease-modifying therapy; EDSS: Expanded Disability Status Scale; FIS: Fatigue Impact Scale; Gd:
gadolinium; IFNβ: interferon beta; IM: intramuscular; ITT: intention-to-treat; IQR: interquartile range; IVRS: interactive voice
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
45
response system; MS: multiple sclerosis; MRI: magnetic resonance imaging; n: number of participants; SC: subcutaneous; SD:
standard deviation; SF-36: 36-item Short Form.
Characteristics of excluded studies [ordered by study ID]
Study
Reason for exclusion
Miller 2014
Participants were diagnosed with a first clinical episode suggestive of MS rather than definite diagnosis of MS
O’Connor 2006
An RCT with a length of follow-up shorter than 1 year
MS: multiple sclerosis; RCT: randomized controlled trial.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
46
DATA AND ANALYSES
This review has no analyses.
APPENDICES
Appendix 1. Keywords for searching the Cochrane MS Group Specialised Register
{HMR1726} OR {A77 1726} OR {Leflunomide} OR {Arava} OR {teriflunomide} OR {TFN} OR {teriflunomide-D4} OR
{A771726} OR {Dihydroorotate dehydrogenase(DHODH) inhibitors} OR {(Z)-2-Cyano-3-hydroxy-N-[4-(trifluoromethyl)phenyl]2-butenamide}
WHAT’S NEW
Last assessed as up-to-date: 7 November 2015.
Date
Event
Description
7 November 2015
New search has been performed
Search updated up to 30 Semptember 2015. The review
now includes five trials
7 November 2015
Amended
The review team has been amended.
7 November 2015
New citation required and conclusions have changed
Three studies have been added. Conclusion changed.
In this version of the review the quality of the evidence
from the included studies was assessed using GRADE
approach and a “Summary of Findings” table has been
added
CONTRIBUTIONS OF AUTHORS
All correspondence: Dian He and Lan Chu.
Drafting of review versions: Dian He.
Search for trials: Chao Zhang and Xia Zhao.
Obtaining copies of trial reports: Qingqing Dai and Yuan Li.
Selection of trials for inclusion/exclusion: Dian He and Yifan Zhang.
Extraction of data: Dian He and Yifan Zhang.
Entry of data: Dian He and Yifan Zhang.
Interpretation of data analyses: Dian He and Lan Chu.
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
47
DECLARATIONS OF INTEREST
DH - none.
CZ - none.
XZ - none.
YZ - none.
QD - none.
YL - none.
LC- none.
SOURCES OF SUPPORT
Internal sources
• The Affiliated Hospital of Guizhou Medical University, China.
External sources
• The Health and Family Planning Commission of Guizhou Province (No.gzwjkj2014-2-107), China.
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
In the current review, we added ’the proportion of participants with at least one relapse’ in the primary outcomes and moved ’the
annualized rate of relapse’ into the secondary outcomes, because the former has a greater significance. We replaced ’the proportion of
patients free of disability progression’ with ’the proportion of participants with disability progression’ in the primary outcomes. In this
review, we created the ’Summary of findings’ table. We removed the restriction of ’double-blind studies’ specified in the protocol. In
addition, we removed duration of follow-up and dose level, and added duration of multiple sclerosis and risk of bias in included studies
as co-variates for subgroup analysis in future updates.
INDEX TERMS
Medical Subject Headings (MeSH)
Crotonates [adverse effects; ∗ therapeutic use]; Immunologic Factors [adverse effects; therapeutic use]; Immunosuppressive Agents
[adverse effects; ∗ therapeutic use]; Multiple Sclerosis, Chronic Progressive [∗ drug therapy]; Multiple Sclerosis, Relapsing-Remitting
[∗ drug therapy]; Randomized Controlled Trials as Topic; Toluidines [adverse effects; ∗ therapeutic use]
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
48
MeSH check words
Adult; Humans; Middle Aged; Young Adult
Teriflunomide for multiple sclerosis (Review)
Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
49