THE ANATOMY OF THE VENOUS
advertisement

THE ANATOMY OF THE VENOUS SYSTEM OF THE LIMBS
Arterial blood flows through the main axial arteries of the upper and lower limbs before returning via
the deep and superficial veins. All of the veins of the upper and lower limbs contain valves, which
ensure that blood flows towards the heart.
The superficial venous trunks in the leg are the greater (long) Although the long saphenous vein is
classically
said to join the femoral vein at the saphenofemoral junction, a fixed point in the groin 2.5 cm below and lateral
to the pubic tubercle, it is usually encountered somewhat higher.
lesser (short or small) saphenous veins which lie above the muscle fascia of the limb. saphenous vein
joins the popliteal vein at the saphenopopliteal junction at a variable site in the popliteal fossa but
generally proximally to the knee joint crease.
Blood passing up the superficial veins enters the deep veins at the saphenopopliteal and
saphenofemoral junctions.
In the calf and thigh there are a number of valved perforating (communicating) veins that join the
superficial to the deep
veins at inconstant sites and which allow blood to flow from the superficial to the deep venous system. The
most important of these are the direct perforating veins of the medial and lateral calf and the communicating
veins around the knee and in the mid-thigh.
The deep veins of the lower limb include three pairs of venae commitantes, which accompany the
three crural arteries (anterior and posterior tibial and peroneal arteries). These six veins
intercommunicate and join in the popliteal fossa to form the popliteal vein, which also receives the
soleal and gastrocnemius veins.
The popliteal vein passes up through the adductor hiatus to enter the subsartorial canal as the
superficial femoral vein, which receives the deep (profunda) femoral vein (or veins) in the femoral
triangle to become the common femoral vein, which then changes its name to the external iliac vein as
it passes behind the inguinal ligament.
The internal iliac vein joins with the external iliac vein in the pelvis to form the common iliac vein. The
left common iliac vein passes behind the right common iliac artery to join the right common iliac vein
on the right side of the abdominal aorta to form the inferior vena cava.
The cephalic and basilic veins are the superficial venous trunks of the arm
VENOUS PATHOPHYSIOLOGY
Blood enters the lower limb through the femoral arteries before passing through arterioles into the
capillaries, which have a pressure of about 32 mmHg at their arterial ends. This pressure is reduced
along the course of the capillaries and is approximately 12 mmHg at the venular end of the capillary.
The pressure continues to fall in the main veins and is as low as −5 mmHg at the upper end of the
vena cava where it enters the right atrium.
The venous pressure in a foot vein on standing is equivalent to the height of a column of blood
extending from the heart to the foot, e.g. approximately 100 mmHg To enable blood to be returned
against gravity in the standing position, an auxiliary pump is required in the lower limb. This is the calf
muscle pump, which is augmented to a lesser extent by the thigh and foot pumps. The deep veins of
the calf are capacious and are joined by blind-ending sacks called the soleal sinusoids, which force
blood into the popliteal and crural veins during calf muscle
pump contraction, e.g. walking.
The foot pump also ejects blood from the plantar veins during walking. As the calf muscles contract,
the veins are compressed and the valves only allow blood to pass in the direction of the heart. The
pressure within the calf compartment rises to 200–300 mmHg during muscle contraction. During
muscle relaxation the pressure falls and blood from the superficial veins enters the deep veins through
the saphenous junctions and the perforating veins. Each time this occurs the pressure falls in the
superficial venous compartment until a threshold is reached, when the venous inflow keeps pace with
ejection from the deep veins. This is normally around 30 mmHg, a fall of approximately two-thirds of
the resting venous pressure.
The net reduction in the pressure of the superficial system is dependent on the* presence of patent
deep veins, *perforating veins and superficial veins, which must contain competent valves.
Ambulatory venous hypertension is a consequence of valve failure (refl ux) or obstruction in the
venous system and may eventually lead to lipodermatosclerosis and ulceration.
.
B&L 26th
‘Micky Mouse’ transverse B mode image of right common femoral vein (R CFV) and right common femoral artery (R CFA) and
greater saphenous vein (GSV) at the saphenofemoral junction (SFJ).
Saphenous eye’ transverse B mode view of long saphenous vein in fascial compartments of the thigh.
patient position for venous duplex examination of the long saphenous system.
Foam sclerotherapy; cannulation of varicosities for ultrasound- guided foam sclerotherapy.
Foam sclerotherapy; Tessari method of foam sclerosant preparation.
Endovenous laser ablation fibre introduced through catheter
Radiofrequency ablation – introducing catheter through sheath.
Low, medium and high-risk patient groups for DVT and pulmonary embolism.
Risk groups
Low
Minor surgery <30 minutes. Any age. No risk factors
Major surgery >30 minutes. Age <40. No other risk factors
Minor trauma or medical illness, any age. No risk factors.
Moderate Major surgery. Age 40+ or other risk factors
High
Major medical illness: heart/lung disease, cancer,
inflammatory bowel disease
Major trauma/burns
Minor surgery, trauma, medical illness in patient with
previous DVT, PE or thrombophilia
Major orthopaedic surgery or fracture pelvis, hip, lower limb
Major abdominal/pelvic surgery for cancer
Major surgery, trauma, medical illness in patient with
DVT, PE or thrombophilia
Lower limb paralysis (e.g. stroke, paraplegia)
Major lower limb amputation.
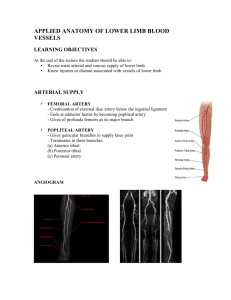
ANATOMY OF VEINS OF LOWER LIMB
Deep Veins
1. Tibial, popliteal, femoral veins are called as “veins of conduits” which drain blood into iliac veins and
then to IVC.
2. Pumping veins: They are venous sinuses existing in the calf muscles which pump blood towards major
veins. They are better termed as musculovenous pumps. They are also called as the peripheral heart.
Superficial Veins
• Long saphenous vein: It is a subcutaneous vein over the inner aspect of the leg and thigh, joins into
femoral vein at fossa ovalis. Tributaries of long saphenous vein are posterior arch vein, anterior vein of
leg, anterolateral vein, posteromedial vein and sometimes accessory saphenous vein.
• Short saphenous vein: It is over the lateral and posterior aspect of the leg enters the deep fascia in the
upper calf region and later joins popliteal vein at variable distance.
• Posterior arch vein of ‘Leonardo’ (from medial ankle to the long sephanous vien below the knee).
• Anterior arch vein to peroneal veins. Superficial veins have got multiple valves which facilitates blood
flow towards heart. Superficial veins usually drain about 10% of lower limb blood i.e. from skin and
subcutaneous tissues.
Perforator Veins
They are the veins which connect superficial to deep veins at various levels. They travel from superficial
fascia through an opening in the deep fascia before entering the deep veins. The direction of blood flow
here is from superficial to deep veins. These perforators are also guarded by valves so that the blood flow
is unidirectional, i.e. towards deep veins. Reversal of flow occurs due to incompetence of perforators
which will lead to varicose veins.
Types
• Ankle perforators (May or Kuster)
• Lower leg perforators: I, II, III (of Cockett)
• Gastrocnemius perforators (of Boyd)
• Mid thigh perforators (Dodd)
• Hunter’s perforator in the thigh
PHYSIOLOGY OF VENOUS BLOOD FLOW IN LOWER LIMB
Veins are thin-walled vessels with collapsible walls, that assume an elliptical configuration in collapsed
state and circular configuration in the filled state.
Venous valves are abundant in the distal lower extremity and the number of valves decreases proximally,
with no valves in superior and inferior vena cava.
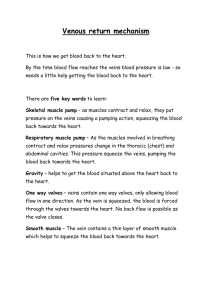
Venous Return
1. Arterial pressure across the capillary increases the pumping action of vein.
2. Calf musculovenous pump: During contraction phase of walking, pressure in the calf muscles
increases to
200-300 mmHg. This pumps the blood towards the heart. During relaxation phase of walking, pressure in
the calf falls and so it allows blood to flow from superficial to deep veins through perforators. Normally
while walking, pressure in the superficial system at the level of ankle is 20 mmHg.
3. During walking, foot pump mechanism propels blood from plantar veins into the leg.
4. Gravity.
Note: Pressure in arteriolar end of the capillary is 32 mmHg; venular end of capillary is 12 mm Hg.
Factors responsible for venous return
1. Negative pressure in thorax
2. Peripheral pump—calf muscles
3. Vis-a-tergo of adjoining muscles
4. Nonrefluxing valves in course of veins
Prevention of DVT
• Categorise the patient as low/moderate and high risk
• Mechanical methods – elastic compression bandage; elevation; external pneumatic bandage
• Pharmacological – low molecular weight heparin – once a day.
Effects and sequelae of DVT
1. Pulmonary embolism
2. Infection
3. Venous gangrene
4. Partial recanalisation, chronic venous hypertension around the ankle region causing venous ulcers
5. Recurrent DVT
6. Propagation of thrombus proximally—20-30%.
Classification of lower-extremity venous diseases
(CEAP classification)
C — Clinical signs (grade 0-6); -(A) for asymptomatic or (S) for symptomatic presentation.
E — Etiologic classification- (congenital, primary, secondary).
A — Anatomic distribution- (superficial, deep or perforator).
P — Pathophysiologic dysfunction- (reflux or obstruction).
Causes of pain / cramps in varicose veins / venous diseases
• Increased venous wall tension – chronic venous hypertension
• Hypoxia of tunica media of the venous wall due to altered function of vasa vasorum
• Increased capillary pressure
• Hyperviscosity of red cells – haemorrheological disorders
• Platelet hyperaggregation
• Reduction in capillary permeability causing capillary functional disorder
• Altered cutaneous microcirculation due to leukocyte adhesion and accumulation into the venous wall;
release of free radicals cause microvascular lesional disease
Oedema in venous diseases
• Can be localised or generalised
• Localised oedema is due to ankle flare or dilatation of medial marginal vein
• Cellulitis and lymphangitis association causes oedema
• Scarring and thickening of dermal and subdermal tissues – lipodermatosclerosis (brawny induration)
• Ankle becomes narrower due to contraction of skin and subcutaneous tissues but calf remains
prominent – champagne bottle appearance
• Pale atrophic skin with white patches surrounded by dilated capillaries and pigmentation – atrophic
Blanche
Three tourniquet test: To find out the site of incompetent perforator,
three tourniquets are tied after emptying the vein.
1. at sapheno-femoral junction
2. above knee level
3. another below knee level.
Patient is asked to stand and looked for filling of veins and site of filling. Then tourniquets are released
from below upwards, again to see for incompetent perforators.
Treatment of VV
1. Conservative treatment:
• Elastic crepe bandage application from below upwards or use of pressure stockings to the limb—
pressure gradiant of 30-40 mmHg is provided.
• Diosmin therapy which increases the venous tone.
• Elevation of the limb—relieves oedema.
• Unna boots—provide nonelastic compression therapy. It comprises a gauze compression dressings that
contain zinc oxide, calamine, and glycerine that helps to prevent further skin break down. It is changed
once a week.
• Pneumatic compression method—provide dynamic sequential compression.
2. Drugs used for varicose veins: Benefits of all these drugs are doubtful.
• Calcium dobesilate—500 mg BD. Calcium dobesilate improves lymph flow; improves macrophage
mediated proteolysis; and reduces oedema.
• Diosmin—450 mg BD
• Diosmin 450 mg + Hesperidin 50 mg (DAFLON 500 mg). Mainly used in relieving night cramps but not
to improve healing of ulcers.
• Toxerutin 500 mg BD, TID. Anti erythrocyte aggregation agent which improves capillary dynamics.
3. Injection—sclerotherapy: (Fegan’s technique). By injecting sclerosants into the vein, complete
sclerosis
of the venous walls can be achieved.
Indications
• Uncomplicated perforator incompetence.
• In the management of smaller varices—reticular
veins, thread veins (telangiectasis).
• Recurrent varices.
• Isolated varicosities.
• Aged/unfit patients.
Sclerosants used are—
• Sodium tetradecyl sulphate 3% (STDS)–commonly used
• Sodium morrhuate
• Ethanolamine oleate
• Polidocanol
Mechanisms of action of scerisent agent:
• Causes aseptic inflammation
• Causes perivenous fibrosis leading to block
• Causes approximation of intima leading to obliteration by endothelial damage
• Alters intravascular pH/osmolality
• Changes surface tension of plasma membrane
A 23 gauge needle is inserted into the vein (3-8 mm sized) and vein is emptied. 0.5-1 ml of sclerosant is
injected into the vein and immediately compression is applied on the vein (prevent the entry of blood
which may cause thrombosis, which later gets recanalised, further worsening the condition) so as to allow
the development of sclerosis and to have proper endothelial apposition.Usually injection is started at the
ankle region and then proceeded upwards along the length of the veins at different points. Later pressure
bandage is applied for six weeks.
Often injections may have to be repeated at 2-4 weeks intervals for 2-4 sessions.
Technique is called as macrosclerotherapy.
Remember about sclerotherapy
• Current place of sclerotherapy is mainly for recurrent varicosities and thread/telangiectatic veins
• Sodium tetradecyl sulphate (STDS) is most commonly used sclerosant
• Hyperpigmentation is common after STDS
• Anaphylaxis is common after sodium morrhuate
• Anaphylaxis is least with polidocanol
• Extravasation (presence of pain/irritation/burning) should be avoided as it will cause skin necrosis
• Post sclerotherapy walking immediately after injection for 30 minutes with elastic bandage in
place prevents/minimises the chances of DVT
• Compression bandage should be worn for minimum period of 6 weeks
• Sclerotherapy can be –1 macrosclerotherapy;2 microsclerotherapy; 3echo (ultrasound guided)
sclerotherapy;4 foam sclerotherapy; 5transilluminated sclerotherapy
Rx of venous/gravitational ulcer
Bisgaard method of treating venous ulcer:
• Measures to reduce oedema, increase venous drainage, so as to promote ulcer healing.
• Elevation.
• Massage of the indurated area and whole calf.
• Passive and active exercise.
Pressure bandage (crepe bandage).
• Care of ulcer by regular cleaning with povidone iodine, H2O2.
• Dressing with EUSOL.{ EUSOL is Edinburgh University solution of lime containing boric acid, sodium
hypochlorite, calcium hydroxide.)
• Four layer bandage (45 mm Hg pressure) technique to achieve high compression pressure. It is
changed
once a week.
• Antibiotics depending on culture and sensitivity of the discharge.
Once ulcer bed granulates well, split skin graft (SSG) is placed (Thiersch Graft).
COMPRESSION THERAPY FOR VARICOSE VEINS
Intro: Compression improves ulcer healing rate , Multi-layered bandage system is most effective.
Pathology:
Mechanism of action:
• Compression reduces the venous wall tension; prevents reflux; controls the venous over-distension
• Compression diverts the blood towards deep veins through perforating veins; prevents the outward flow
of blood in perforator incompetence; improves the efficacy of calf muscle pump. Compression reduces.
the oedema and improves the venous and lymphatic drainage; improves venous elasticity;
improves the microcirculation and more important is it prevents further damage of the venous wall
Types:
Compression may be
1.elastic
2.inelastic
3.combination of elastic and inelastic (Unna boot)- Unna boot is three-layered paste gauze
compression dressing containing calamine, zinc oxide, glycerin, sorbitol, gelatin and aluminium silicate
which has mainly inelastic inner component with partly elastic outer layer wrap
1.multilayered (four layered) compression system which can provide sustained high compression for
several days – usually up to a week
2.intermittent pneumatic compression.
.
Compression garments standard
British standard
• Class I: 14-17 mm Hg
• Class II: 17-24 mm Hg
• Class III: 24-35 mm Hg
International (European) standard
• Class I: 20-30 mm Hg
• Class II: 30-40 mm Hg
• Class III: 40-50 mm Hg
• Class IV: 50-60 mm Hg
Recommended pressure,
1. mild varicose veins e.g.pregnancy and postoperative period is 20 mmHg.
2. symptomatic varicose veins and after sclerotherapy is 30 mm Hg;
3. venous ulcer and post phlebitic leg is 40-45 mm Hg;
4. phlebolymphoedema (venous oedema with lymphatic oedema which is more
dangerous) it is more than 45 mm Hg.
Complications:
1.
2.
3.
4.
Skin maceration,
Skin excoriation,
Skin dryness,
infection,
5. ulceration and failure.
Contraindication: ABPI <0.9
Neuropathy- diabetic & others type of neuropathy
Co-exsisting arterial disease
ANTICOAGULANTS
These are the agents used to prevent and treat thrombosis and thromboembolic events.
HEPARIN
• It is a natural anticoagulant, a mucopolysaccharide.
• It prevents clotting of blood both in vivo and in vitro by acting on all three stages of coagulation. It
prolongs clotting time and activated thromboplastin time in specific (by 1.5-2.0 times the control).
• Heparin also causes hyperkalaemia, thrombocytopenia.
• Commercial heparin is derived from lung and intestinal mucosa of pigs and cattle.
• The onset of action is immediate after administration, lasting for 4 hours.
• It is metabolised in the liver by heparinase.
• It does not cross placental barrier and is not secreted in breast milk.
Indications
• As prophylaxis in major surgeries, postoperative period, puerperium.
• As therapy in DVT.
Dose
• For prophylaxis: 5,000 units/subcutaneously 8th hourly.
• For therapy: 10,000 units/IV 6th or 8th hourly. Later changed to subcutaneous dose.
• In severe cases, 5,000 units to 20,000 units is given daily through IV infusion at a rate of 1,000 units per
hour. Daily dose should not exceed 25,000 units.
Heparin should not be given intramuscularly and should not be combined with streptokinase or urokinase.
Heparin is not given orally.
Heparin administration should always be monitored with APTT.
Complications
Allergy, bleeding, thrombocytopenia.
Danaparoid is an antifactor Xa, heparinoid, is an anticoagulant used in patients where heparin is
contraindicated.
LOW MOLECULAR WEIGHT HEPARIN (LMWH)
It is a commercially prepared heparin with a molecular weight of 4,000 to 6,500.
• Enoxaparin.
• Dalteparin.
• Parnaparin.
• Reviparin.
• Fraxiparin
Advantages
• Have a longer duration of action - once a day
• Have a better anticoagulant effect
• Less interaction with platelets
• Less antigenic
• Usage is easier and more acceptable
• Monitoring is not necessary
Disadvantages
They are expensive.
Presently LMWH are becoming very popular.
Heparin antagonist: 50 mg of 1% protamine sulphate solution is given slow intravenous. 1 gm reverses
100 units of heparin. It is given only after doing activated thromboplatin time. Overdosing or infusion
without indication may itself precipitate bleeding.
ORAL ANTICOAGULANTS
They are given orally and are slow acting.
Types
1. Coumarin derivatives: Bishydroxycoumarin (Dicoumarol): First coumarin drug derived from sweet
clover. Warfarin sodium: Commonest oral anticoagulant used.
2. Indandione derivative: Phenindione, anisindione.
Mode of Action of Oral Anticoagulant Therapy
• By suppressing synthesis of prothrombin, factors VII, IX and X.
• By inhibiting Vit K mediated carboxylation of glutamic acid.
• Oral anticoagulant does not have in vitro action.
• They are slow acting, and long acting.
• Control of oral anticoagulant therapy is by monitoring prothrombin time.
• PT comes to normal only 7 days after cessation of the drug.
• They cross placental barrier and are known to cause teratogenicity when given in 1st trimester.
• They are secreted in breast milk.
Indications
1. In DVT after cessation of heparin for maintenance therapy.
2. After valve replacement surgery. To achieve adequate anticoagulant effect and to prevent
thromboembolic episodes the INR has to be maintained within 2-3.
Side Effects
1. Bleeding—It may require blood transfusion or vitamin K injection intramuscular or oral to control.
2. Cutaneous gangrene.
3. Fetal haemorrhage and teratogenicity.
4. Alopecia, urticaria, dermatitis.
5. Drug interactions: with NSAIDS, cimetidine, omeprazole, metronidazole, cotrimoxazole, erythromycins,
barbiturates, rifampicin, griseofulvin.
1. WARFARIN (Wiskonian Alumini Research Foundation + coumARIN derivative) SODIUM is the
commonest drug used.
2. It has got lesser side effects.
3. It has got cumulative action and so given in tapering dose.
4. Dose is 5 mg, once a day.
5. It should be discontinued 7 days before any surgery like tooth extraction and prothrombin time
should return to normal level.
6. During surgery, if excess bleeding occurs, fresh frozen plasma may be given.
7. The effects of warfarin sodium is reversed by inj. Vit K; the dose depends on INR and emergency
of reversal (takes 24 times to reverse).
8. IN VITRO ANTICOAGULANTS: Oxalates, citrates, EDTA (Ethylene diamine tetra-acetic acid).
Thrombolytic agents
•
•
•
•
Streptokinase
Urokinase
Anistreplase
Alteplase
Differences between oral anticoagulants and heparin
Oral anticoagulant
Slow acting Long acting Only in vivo
Monitored by: Prothrombin time
Crosses placental barrier
Heparin
Immediate Short acting Both in vitro and in vivo
Partial thromboplastin time
Does not cross placenta
Secreted in milk
Administration: Orally
Not secreted in milk
Intravenously
Contraindications for anticoagulant therapy:
1. Ongoing bleeding
2. Recent surgery/invasive procedure
3. Severe trauma
4. Bleeding tendency (clotting factor deficiency)
5. Intracranial haemorrhage
6. Pericarditis/pericardial effusion
7. Patient prone to fall.
DIRECT THROMBIN INHIBITORS
A. Recombinant hirudin and hirudin analogues— derived from leeches, are direct inhibitors of thrombin.
B. Argatroban—synthetic direct thrombin inhibitor.
ANTIPLATELET DRUGS
1. Small dose aspirin—inhibits platelet synthesis of thrombaxane A2
2. Ticlopidine (125 mg BD)—alters platelet membrane, thereby platelet aggregation
3. Clopidogrel—action similar to ticlopidine
4. Dextran—decreases platelet aggregation
5. Abciximab—glycoprotein IIb/IIIa inhibitors, block platelet aggregation, and platelet adhesion to
fibrin.
6. Dipyridamole—xanthine oxidase inhibitor.