Cell-cell interactions in regulating lung function
advertisement

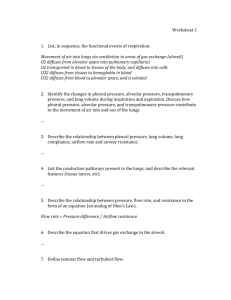
Am J Physiol Lung Cell Mol Physiol 287: L455–L459, 2004; 10.1152/ajplung.00172.2004. EB2004 FEATURED TOPIC REPORT Cell-cell interactions in regulating lung function Scott Boitano,1 Zeenat Safdar,2,3 Donald G. Welsh,4 Jahar Bhattacharya,2 and Michael Koval5 1 Department of Physiology, University of Arizona Health Sciences Center, Tucson, Arizona 85724; 2Lung Biology Laboratory and 3Division of Pulmonary-Critical Care Medicine, St. Luke’s-Roosevelt Hospital Center, College of Physicians and Surgeons, Columbia University, New York, New York 10019; 4Department of Physiology and Biophysics, University of Calgary, Calgary, Alberta, Canada T2N 4N1; and 5Department of Physiology and Institute for Environmental Medicine, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania 19104 tight junction; gap junction; claudin; connexin; cadherin; calcium TO FUNCTION AS A COHESIVE TISSUE, the activities of individual cells are coordinated at cell-cell contact sites. These sites are composed of transmembrane and peripheral protein components that provide a scaffold to interlink these elements with the cytoskeleton and serve to cluster cell adhesion molecules, ion channels, and junctional components into a functional complex (29, 48). Cell-cell contact sites provide important spatial cues to generate cell polarity and enable cells to sense and respond to adjacent cells (32). Junctional complexes at cell-cell contact sites are also control points for regulating solute flow across cell monolayers (through tight junctions) and from one cell to another (through gap junctions). Progress in understanding the regulation of pulmonary barrier function and roles for gap junctional communication by lung epithelium and endothelium was presented at the 2004 Experimental Biology Meeting held in Washington, DC. DIFFERENTIAL CLAUDIN LOCALIZATION BY ALVEOLAR EPITHELIUM Disruption of the paracellular alveolar permeability barrier is a significant pathological consequence of acute lung injury (8). Transmembrane proteins in the claudin family act in concert Address for reprint requests and other correspondence: M. Koval, Univ. of Pennsylvania School of Medicine, Dept. of Physiology, B-400 Richards Bldg./6085, 3700 Hamilton Walk, Philadelphia, PA 19104 (E-mail: mkoval@mail.med.upenn.edu). http://www.ajplung.org with other transmembrane and peripheral proteins to form the physical basis for tight junctions (41, 42). There are roughly two dozen different claudins. Epithelial cells simultaneously express up to six or more claudin isoforms. Cells expressing different claudins have different paracellular permeability characteristics (7, 43– 45). Whereas individual claudins have been shown to support the paracellular transport of ions, the mechanisms used by multiple claudins to form a tight junction barrier has not been well established. Because cells often express multiple claudins, this raises the possibility that two or more different claudins in adjacent cells might interact heterotypically, through head-to-head interactions. A study of transfected fibroblasts suggests that claudin head-to-head compatibility is limited to specific claudin combinations rather than being universal (14). Although claudin compatibility is an issue in a homogeneous epithelium, it is a more critical concern in the mature alveolus, where there are heterologous contact sites between type II cells and type I cells that express different claudins (45). In this case, exclusion of incompatible claudins from type II-type I cell interfaces could potentially help regulate tight junction composition and thus paracellular permeability. Whether this is the case remains to be determined. However, it seems likely that the paracellular permeability of heterologous type II-type I alveolar epithelial cell interfaces will differ from that of homologous type I-type I and type II-type II contact sites. This could have functional ramifications for maintaining fluid balance in the adult lung. In contrast to the mature alveolus, which is a heterogeneous epithelium, the developing air space consists of a more uniform monolayer of fetal type II cells. A tight seal is important for alveolar development, since accumulated fetal lung fluid induces mechanical distension and differentiation of fetal alveolar epithelial cells (11, 31). Given this, barrier function of isolated human fetal alveolar epithelial cells in culture was examined (16). Isolated fetal alveolar epithelial cells cultured in medium containing dexamethasone and cAMP plus IBMX (DCI) differentiate to a type II-like phenotype, whereas cells cultured in the absence of added hormones remain undifferentiated (16). DCI-treated fetal alveolar epithelial cells cultured on permeable supports formed high-resistance monolayers (⬎1,700 ⍀ 䡠cm2), consistent with the ability of fetal type II cells to form tight junctions. In contrast, undifferentiated fetal alveolar cells formed leaky monolayers (⬍300 ⍀䡠cm2). At the mRNA level, the major tight junction proteins upregulated by DCI treatment were claudin-5 and claudin-18. None of the other proteins examined showed more than a twofold change in mRNA expression, including other claudins, occludin, junction 1040-0605/04 $5.00 Copyright © 2004 the American Physiological Society L455 Downloaded from http://ajplung.physiology.org/ by 10.220.33.6 on October 2, 2016 Boitano, Scott, Zeenat Safdar, Donald G. Welsh, Jahar Bhattacharya, and Michael Koval. Cell-cell interactions in regulating lung function. Am J Physiol Lung Cell Mol Physiol 287: L455–L459, 2004; 10.1152/ajplung.00172.2004.—Tight junction barrier formation and gap junctional communication are two functions directly attributable to cell-cell contact sites. Epithelial and endothelial tight junctions are critical elements of the permeability barrier required to maintain discrete compartments in the lung. On the other hand, gap junctions enable a tissue to act as a cohesive unit by permitting metabolic coupling and enabling the direct transmission of small cytosolic signaling molecules from one cell to another. These components do not act in isolation since other junctional elements, such as adherens junctions, help regulate barrier function and gap junctional communication. Some fundamental elements related to regulation of pulmonary barrier function and gap junctional communication were presented in a Featured Topic session at the 2004 Experimental Biology Conference in Washington, DC, and are reviewed in this summary. L456 EB2004 FEATURED TOPIC REPORT Fig. 1. Differential claudin localization by fetal alveolar epithelial cells. Isolated human fetal alveolar epithelial cells were cultured for 4 days in Waymouth medium containing dexamethasone, cAMP, and IBMX to promote differentiation toward a type II cell phenotype (A) or under control conditions to remain undifferentiated (B). The cells were then fixed, permeabilized, and immunostained for claudin-7. Claudin-7 was preferentially localized to the plasma membrane by differentiated cells; however, undifferentiated cells had a significant intracellular claudin-7 pool (arrowheads). Other claudins expressed by these cells had a similar intracellular distribution (not shown). This difference in claudin localization correlated with increased barrier function of differentiated fetal alveolar epithelial cells. Bar, 10 m. AJP-Lung Cell Mol Physiol • VOL claudin incorporation into tight junctions as a posttranslational means to regulate barrier function. Although the mechanisms that fetal alveolar cells use to regulate claudin localization remain to be elucidated, these data suggest that coordinated increases in fetal type II cell differentiation and barrier function might provide a positive feedback loop with the potential to help drive fetal lung development (11, 31). INTERCELLULAR SIGNALING BETWEEN ALVEOLAR EPITHELIAL CELLS Physiological function of the alveolar epithelium requires intercellular signaling between type I alveolar epithelial cells and type II alveolar epithelial cells. The overall contribution of specific cell-cell interactions to lung function has been difficult to assess due to problems working with whole lung tissue and the lack of a culture model that contains both type I and type II cells. In an attempt to develop a heterocellular culture of type I and type II cells, type II cells were isolated and cultured on a rat tail collagen/fibronectin matrix supplemented with a limited amount of another extracellular matrix protein, laminin 5. After 7 days on this matrix, alveolar cell cultures contained a mixed monolayer of epithelial cells morphologically resembling either type I-like or type II-like cells, based on immunohistochemical staining of cell-specific markers, distribution of cell types, and cell morphology (24). These heterocellular cultures of type I-like and type II-like cells provide an accessible in vitro model system to study alveolar epithelial cell interactions between and among the two alveolar epithelial phenotypes. The cells of the alveolar epithelium are interconnected by gap junction channels that enable the flow of cytoplasmic metabolites, antioxidants, and signals from one cell to its nearest neighbor (26). There are at least six gap junction protein (connexin) isoforms expressed by alveolar epithelial cells. The connexins expressed by type I-like and type II-like cells in heterocellular cultures resembled those expressed by type I and type II cells in situ (25). This contrasts with the pattern of connexins expressed by alveolar epithelial cells grown in homogenous cultures and suggests that connexin expression by alveolar epithelial cells is influenced by neighboring cell phenotype and/or cell matrix interactions (1, 2, 4, 18, 21, 28). The expression of comparable connexins by heterocellular cultures and cells in situ suggested an improved model for studying alveolar epithelial cell-cell communication in vitro. Consistent with the presence of connexins in both alveolar epithelial cell types, cells in heteroculture were coupled through gap junctions, as measured by transfer of microinjected dyes between cells with similar and distinct phenotype (25). Connexin mimetic peptides inhibited dye transfer between cells in heteroculture, although dye transfer from type I-like cells to type II-like cells was less sensitive to peptide inhibition. The transmission of stretch-induced Ca2⫹ transients between alveolar epithelial cells suggests that changes in intracellular Ca2⫹ concentration ([Ca2⫹]i) can contribute to integrated signaling in lung epithelium. For instance, mechanical stimulation of type I cells in situ initiates a transient increase in [Ca2⫹]i that is transmitted to type II cells through gap junctions to stimulate surfactant secretion (3). Direct mechanical stimulation of type II cells can also stimulate changes in [Ca2⫹]i and surfactant 287 • SEPTEMBER 2004 • www.ajplung.org Downloaded from http://ajplung.physiology.org/ by 10.220.33.6 on October 2, 2016 adhesion molecule-1, and scaffold proteins. In addition, at the total protein level, differences between DCI-treated and untreated fetal alveolar cells were modest. The difference between DCI-treated and untreated cells was more dramatic when the cells were examined by immunofluorescence microscopy (Fig. 1). In DCI-treated differentiated cells, claudin-3, claudin-4, claudin-5, and claudin-7 were localized to the plasma membrane. In contrast, undifferentiated alveolar epithelial cells had a prominent intracellular claudin pool and showed discontinuous claudin labeling of the plasma membrane. The intracellular pool of claudins colocalized with early endosome antigen-1, suggesting that undifferentiated cells constitutively internalized claudins from the plasma membrane and that this process might compete for claudin incorporation into tight junction strands. This suggests that fetal type II cells either inhibit claudin endocytosis or stabilize EB2004 FEATURED TOPIC REPORT Fig. 2. Signaling pathways for Ca2⫹ communication between cultured alveolar epithelial cells. Cells were mechanically stimulated to initiate intercellular communication (A, arrowhead, gray). Increases in cytosolic calcium, [Ca2⫹]i, are transmitted through homogenous cultures of type I-like cells through gap junctions. B: homogenous cultures of type II cells use nucleotide trisphosphate (NTP) release and paracrine stimulation to transmit increases in [Ca2⫹]i. C: in heterocellular cultures, increases in [Ca2⫹]i generated by stimulation of type I-like cells are transmitted to both type I-like and type II-like cells through gap junctions. D: in contrast, type II-like cells stimulated in heterocellular cultures transmitted increases in [Ca2⫹]i to type I-like cells through NTP release, or to type II-like cells through both NTP release and gap junctions. AJP-Lung Cell Mol Physiol • VOL fibronectin matrix provides a new model for the study of coordinated cellular physiology of the alveolar epithelium. Initial studies with this model show distinct connexin profiles and unique functional coupling pathways between the two cell phenotypes that may provide insight on interactions used by type I and type II cells to regulate alveolar epithelial function in vivo. Further study on cell communication and physiological outcome will help to elucidate roles for different connexin isoforms and changes in mechanisms of Ca2⫹ communication in the alveolar epithelium. ENDOTHELIAL CA2ⴙ REGULATION BY CONNEXIN 43 IN ALVEOLAR CAPILLARIES OF RAT LUNG In lung microvessels, endothelial cells serve a variety of functions, such as maintenance of the vascular permeability barrier, establishment of a nonthrombogenic luminal surface, and secretion of vasodilatory factors such as nitric oxide. Many microvascular endothelial functions are [Ca2⫹]i dependent, and their signaling mechanisms involve critical increases in [Ca2⫹]i. Previous studies using the fura 2 ratio imaging method to measure [Ca2⫹]i in intact lung microvessels of the subpleural capillary bed demonstrated the transmission of [Ca2⫹]i along the capillary wall through gap junctions (49). Stimuli such as increased pressure or histamine increase the amplitude of [Ca2⫹]i (27, 49). However, the frequency of lung capillary Ca2⫹ oscillations appears to be controlled by a subset of endothelial cells, called pacemaker cells, that actively generate [Ca2⫹]i transients even under resting conditions (49). Analysis of 20- to 25-m-diameter lung venular capillaries facilitates measurements in a vascular wall consisting purely of endothelial cells, since lung vessels of ⬍30-m diameter lack smooth muscle, especially in the venous system. Also, the endothelial phenotype of cells in these vessels was confirmed by DiI-AcLDL labeling and the lack of smooth muscle actin expression (49). This helps simplify the analysis of endothelial cell-cell [Ca2⫹]i transmission, since these vessels lack myoendothelial junctions that can confound analysis of intercellular communication in the vasculature (5, 38, 46, 47). Connexin 37 and connexin 40 tend to be uniformly expressed by vascular endothelial cells in situ (39). In general, large vessel endothelial cells show more connexin 43 expression than microvascular cells, which correlates with the extent of gap junctional coupling (35). Here, connexin 43 expression by lung capillaries was confirmed by immunohistochemistry, consistent with other studies demonstrating connexin 43 expression by microvascular endothelial cells (19, 20). Note that connexin 43 expression tends to be upregulated in areas with turbulent flow, such as vessel branch points, although connexin 37 and connexin 40 expression in situ are much less sensitive to flow (9, 15). Interestingly, endothelial pacemaker cells also tend to be localized to microvessel branch points (49), raising the possibility that they might express more connexin 43 than other capillary endothelial cells. Transmission of [Ca2⫹]i transients through gap junctions can occur either through the direct flow of Ca2⫹ or through the flow of second messengers, such as inositol trisphosphate (13, 33, 34). To examine the transmission of Ca2⫹ through gap junctions, lung capillary endothelial cells in situ were loaded with a “caged” Ca2⫹ compound and a Ca2⫹-sensitive dye, fluo 4. UV-induced photolysis increased endothelial Ca2⫹ both at the 287 • SEPTEMBER 2004 • www.ajplung.org Downloaded from http://ajplung.physiology.org/ by 10.220.33.6 on October 2, 2016 secretion (12). However, alveolar epithelial cells have the capacity to transmit changes in [Ca2⫹]i both directly (through gap junctions) and indirectly (through nucleotide secretion and paracrine stimulation of purinergic receptors). These differences have been observed in alveolar epithelial monocultures, where mechanical stimulation of type I-like cells induces gap junction-mediated transmission of changes in [Ca2⫹]i (21), whereas mechanical stimulation of type II-like cells induces paracrine signaling (23) (Fig. 2). To determine the pathway for intercellular Ca2⫹ waves between phenotypically distinct alveolar cell types in heteroculture, we mechanically stimulated cells to initiate Ca2⫹ waves and applied inhibitors of either gap junctional communication or purinergic receptor stimulation. Initiation of Ca2⫹ waves from type I-like cells communicated increases in [Ca2⫹]i to neighboring type I-like or type II-like cells via a gap junctional pathway (Fig. 2). In contrast, communication of Ca2⫹ waves from type II-like cells in heterocellular culture was more complex. Stimulated type II-like cells communicated increases in [Ca2⫹]i to neighboring type I-like and type II-like cells via extracellular nucleotide release; however, communication to neighboring type II-like cells also occurred via gap junctions. Similar to the dye-coupling experiments, these Ca2⫹ communication data are suggestive of selective molecular transfer between and among type I and type II cells (25). In summary, the heterocellular culture model of type I-like and type II-like cells grown for 7 days on a laminin 5/collagen/ L457 L458 EB2004 FEATURED TOPIC REPORT 3. 4. 5. 6. 7. E-CADHERIN EXPRESSION IN LUNG VENULAR CAPILLARIES The lung capillary barrier critically regulates fluid flux into lung tissue (10, 40). Microvascular endothelial cells in culture have a biphasic response to treatment with hyperosmolar sucrose solution (36). With short-term (1 min) exposure, the cells shrink and their barrier function decreases. However, with longer-term exposure (15 min), the microvascular cells recover and have increased barrier function. In part, this is due to stimulation of focal adhesion kinase activity which, in turn, promotes remodeling of the actin cytoskeleton (30, 36). Ecadherin expression is also increased, which further promotes cell adhesion and provides a cytoskeletal anchor point for actin at cell-cell contact sites (17). As opposed to the significant increase in E-cadherin expression, microvascular cells in culture expressed only low levels of vascular endothelial (VE)cadherin, in contrast to previous reports that VE-cadherin is expressed by endothelial cells of the lung (6). The cadherin isoforms expressed by lung capillaries in situ have not been characterized. To examine this, capillaries of the isolated, blood-perfused lung were immunostained using instilled anti-cadherin antibodies and then viewed by confocal microscopy (37). E-cadherin was evident in both alveolar septal and venular capillaries. Costaining for actin with rhodamine phalloidin revealed occasional colocalization of E-cadherin and actin in resting capillaries. However, VE-cadherin expression was not detected. Consistent with studies on cultured microvascular cells, hyperosmolar infusion for 15 min increased capillary barrier function immunofluorescence (37). This increase in barrier function was accompanied by an increase in detection of E-cadherin at the endothelial cell surface as measured by in situ immunofluorescence (37). The level of filamentous actin also increased in response to hyperosmolar infusion, as did the extent of overlap between Ecadherin and actin in the pulmonary capillaries. Significant levels of VE-cadherin were not detected in hyperosmolar infused lung capillaries. Together, these data suggest that E-cadherin is the dominant cadherin expressed by endothelial cells of lung capillaries. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 23. REFERENCES 1. Abraham V, Chou ML, DeBolt KM, and Koval M. Phenotypic control of gap junctional communication by cultured alveolar epithelial cells. Am J Physiol Lung Cell Mol Physiol 276: L825–L834, 1999. 2. Abraham V, Chou ML, George P, Pooler P, Zaman A, Savani RC, and Koval M. Heterocellular gap junctional communication between alveolar AJP-Lung Cell Mol Physiol • VOL 24. epithelial cells. Am J Physiol Lung Cell Mol Physiol 280: L1085–L1093, 2001. Ashino Y, Ying X, Dobbs LG, and Bhattacharya J. [Ca2⫹]i oscillations regulate type II cell exocytosis in the pulmonary alveolus. Am J Physiol Lung Cell Mol Physiol 279: L5–L13, 2000. Carson JL, Reed W, Moats-Staats BM, Brighton LE, Gambling TM, Hu SC, and Collier AM. Connexin 26 expression in human and ferret airways and lung during development. Am J Respir Cell Mol Biol 18: 111–119, 1998. Christ GJ, Spray DC, el-Sabban M, Moore LK, and Brink PR. Gap junctions in vascular tissues. Evaluating the role of intercellular communication in the modulation of vasomotor tone. Circ Res 79: 631– 646, 1996. Corada M, Zanetta L, Orsenigo F, Breviario F, Lampugnani MG, Bernasconi S, Liao F, Hicklin DJ, Bohlen P, and Dejana E. A monoclonal antibody to vascular endothelial-cadherin inhibits tumor angiogenesis without side effects on endothelial permeability. Blood 100: 905–911, 2002. Coyne CB, Gambling TM, Boucher RC, Carson JL, and Johnson LG. Role of claudin interactions in airway tight junctional permeability. Am J Physiol Lung Cell Mol Physiol 285: L1166 –L1178, 2003. Crandall ED and Matthay MA. Alveolar epithelial transport. Basic science to clinical medicine. Am J Respir Crit Care Med 163: 1021–1029, 2001. DePaola N, Davies PF, Pritchard WF Jr, Florez L, Harbeck N, and Polacek DC. Spatial and temporal regulation of gap junction connexin43 in vascular endothelial cells exposed to controlled disturbed flows in vitro. Proc Natl Acad Sci USA 96: 3154 –3159, 1999. Dudek SM and Garcia JG. Cytoskeletal regulation of pulmonary vascular permeability. J Appl Physiol 91: 1487–1500, 2001. Flecknoe S, Harding R, Maritz G, and Hooper SB. Increased lung expansion alters the proportions of type I and type II alveolar epithelial cells in fetal sheep. Am J Physiol Lung Cell Mol Physiol 278: L1180 – L1185, 2000. Frick M, Bertocchi C, Jennings P, Haller T, Mair N, Singer W, Pfaller W, Ritsch-Marte M, and Dietl P. Ca2⫹ entry is essential for cell strain-induced lamellar body fusion in isolated rat type II pneumocytes. Am J Physiol Lung Cell Mol Physiol 286: L210 –L220, 2004. Fry T, Evans JH, and Sanderson MJ. Propagation of intercellular calcium waves in C6 glioma cells transfected with connexins 43 or 32. Microsc Res Tech 52: 289 –300, 2001. Furuse M, Sasaki H, and Tsukita S. Manner of interaction of heterogeneous claudin species within and between tight junction strands. J Cell Biol 147: 891–903, 1999. Gabriels JE and Paul DL. Connexin43 is highly localized to sites of disturbed flow in rat aortic endothelium but connexin37 and connexin40 are more uniformly distributed. Circ Res 83: 636 – 643, 1998. Gonzales LW, Guttentag SH, Wade KC, Postle AD, and Ballard PL. Differentiation of human pulmonary type II cells in vitro by glucocorticoid plus cAMP. Am J Physiol Lung Cell Mol Physiol 283: L940 –L951, 2002. Gumbiner BM. Regulation of cadherin adhesive activity. J Cell Biol 148: 399 – 404, 2000. Guo Y, Martinez-Williams C, Yellowley CE, Donahue HJ, and Rannels DE. Connexin expression by alveolar epithelial cells is regulated by extracellular matrix. Am J Physiol Lung Cell Mol Physiol 280: L191– L202, 2001. Gustafsson F, Mikkelsen HB, Arensbak B, Thuneberg L, Neve S, Jensen LJ, and Holstein-Rathlou NH. Expression of connexin 37, 40 and 43 in rat mesenteric arterioles and resistance arteries. Histochem Cell Biol 119: 139 –148, 2003. Haas TL and Duling BR. Morphology favors an endothelial cell pathway for longitudinal conduction within arterioles. Microvasc Res 53: 113–120, 1997. Isakson BE, Evans WH, and Boitano S. Intercellular Ca2⫹ signaling in alveolar epithelial cells through gap junctions and by extracellular ATP. Am J Physiol Lung Cell Mol Physiol 280: L221–L228, 2001. Isakson BE, Lubman RL, Seedorf GJ, and Boitano S. Modulation of pulmonary alveolar type II cell phenotype and communication by extracellular matrix and KGF. Am J Physiol Cell Physiol 281: C1291–C1299, 2001. Isakson BE, Seedorf GJ, Lubman RL, and Boitano S. Heterocellular cultures of pulmonary alveolar epithelial cells grown on laminin-5 supplemented matrix. In Vitro Cell Dev Biol Anim 38: 443– 449, 2002. 287 • SEPTEMBER 2004 • www.ajplung.org Downloaded from http://ajplung.physiology.org/ by 10.220.33.6 on October 2, 2016 uncaging site as well as at a distant location lying outside the uncaging area, indicating that the increase of Ca2⫹ at the uncaging site was communicated to the distant site. Infusion of peptides that block intercellular communication through connexin 43-containing gap junctions completely blocked the photolysis-induced Ca2⫹ increase at the distant capillary site but not at the photo-targeted site. A major conclusion of this study was that Ca2⫹ increases in endothelial cells of lung capillaries are rapidly conducted to adjoining endothelial cells of the capillary. This has the potential to act as a signaling pathway and also provides a mechanism for decreasing localized increases in [Ca2⫹]i by transmitting Ca2⫹ throughout the interconnected endothelium. Diffusion of Ca2⫹ through connexin 43-containing gap junctions appears to be the major mechanism for this protective response. EB2004 FEATURED TOPIC REPORT AJP-Lung Cell Mol Physiol • VOL 37. Safdar Z, Wang P, Ichimura H, Issekutz AC, Quadri S, and Bhattacharya J. Hyperosmolarity enhances the lung capillary barrier. J Clin Invest 112: 1541–1549, 2003. 38. Sandow SL and Hill CE. Incidence of myoendothelial gap junctions in the proximal and distal mesenteric arteries of the rat is suggestive of a role in endothelium-derived hyperpolarizing factor-mediated responses. Circ Res 86: 341–346, 2000. 39. Severs NJ, Rothery S, Dupont E, Coppen SR, Yeh HI, Ko YS, Matsushita T, Kaba R, and Halliday D. Immunocytochemical analysis of connexin expression in the healthy and diseased cardiovascular system. Microsc Res Tech 52: 301–322, 2001. 40. Stevens T, Garcia JG, Shasby DM, Bhattacharya J, and Malik AB. Mechanisms regulating endothelial cell barrier function. Am J Physiol Lung Cell Mol Physiol 279: L419 –L422, 2000. 41. Tsukita S, Furuse M, and Itoh M. Multifunctional strands in tight junctions. Nat Rev Mol Cell Biol 2: 285–293, 2001. 42. Van Itallie C and Anderson JM. The role of claudins in determining paracellular charge selectivity. Proc Am Thorac Soc 1: 38 – 41, 2004. 43. Van Itallie C, Rahner C, and Anderson JM. Regulated expression of claudin-4 decreases paracellular conductance through a selective decrease in sodium permeability. J Clin Invest 107: 1319 –1327, 2001. 44. Van Itallie CM, Fanning AS, and Anderson JM. Reversal of charge selectivity in cation or anion-selective epithelial lines by expression of different claudins. Am J Physiol Renal Physiol 285: F1078 –F1084, 2003. 45. Wang F, Daugherty B, Keise LL, Wei Z, Foley JP, Savani RC, and Koval M. Heterogeneity of claudin expression by alveolar epithelial cells. Am J Respir Cell Mol Biol 29: 62–70, 2003. 46. Welsh DG and Nelson MT. A case for myoendothelial gap junctions. Circ Res 87: 427– 428, 2000. 47. Yashiro Y and Duling BR. Integrated Ca2⫹ signaling between smooth muscle and endothelium of resistance vessels. Circ Res 87: 1048 –1054, 2000. 48. Yeaman C, Grindstaff KK, Hansen MD, and Nelson WJ. Cell polarity: versatile scaffolds keep things in place. Curr Biol 9: R515–R517, 1999. 49. Ying X, Minamiya Y, Fu C, and Bhattacharya J. Ca2⫹ waves in lung capillary endothelium. Circ Res 79: 898 –908, 1996. 287 • SEPTEMBER 2004 • www.ajplung.org Downloaded from http://ajplung.physiology.org/ by 10.220.33.6 on October 2, 2016 25. Isakson BE, Seedorf GJ, Lubman RL, Evans WH, and Boitano S. Cell-cell communication in heterocellular cultures of alveolar epithelial cells. Am J Respir Cell Mol Biol 29: 552–561, 2003. 26. Koval M. Sharing signals: connecting lung epithelial cells with gap junction channels. Am J Physiol Lung Cell Mol Physiol 283: L875–L893, 2002. 27. Kuebler WM, Ying X, and Bhattacharya J. Pressure-induced endothelial Ca2⫹ oscillations in lung capillaries. Am J Physiol Lung Cell Mol Physiol 282: L917–L923, 2002. 28. Lee YC, Yellowley CE, Li Z, Donahue HJ, and Rannels DE. Expression of functional gap junctions in cultured pulmonary alveolar epithelial cells. Am J Physiol Lung Cell Mol Physiol 272: L1105–L1114, 1997. 29. Matter K and Balda MS. Signalling to and from tight junctions. Nat Rev Mol Cell Biol 4: 225–236, 2003. 30. Mehta D, Tiruppathi C, Sandoval R, Minshall RD, Holinstat M, and Malik AB. Modulatory role of focal adhesion kinase in regulating human pulmonary arterial endothelial barrier function. J Physiol 539: 779 –789, 2002. 31. Moessinger AC, Harding R, Adamson TM, Singh M, and Kiu GT. Role of lung fluid volume in growth and maturation of the fetal sheep lung. J Clin Invest 86: 1270 –1277, 1990. 32. Nelson WJ. Adaptation of core mechanisms to generate cell polarity. Nature 422: 766 –774, 2003. 33. Niessen H, Harz H, Bedner P, Kramer K, and Willecke K. Selective permeability of different connexin channels to the second messenger inositol 1,4,5-trisphosphate. J Cell Sci 113: 1365–1372, 2000. 34. Paemeleire K, Martin PE, Coleman SL, Fogarty KE, Carrington WA, Leybaert L, Tuft RA, Evans WH, and Sanderson MJ. Intercellular calcium waves in HeLa cells expressing GFP-labeled connexin 43, 32, or 26. Mol Biol Cell 11: 1815–1827, 2000. 35. Pepper MS, Montesano R, el Aoumari A, Gros D, Orci L, and Meda P. Coupling and connexin 43 expression in microvascular and large vessel endothelial cells. Am J Physiol Cell Physiol 262: C1246 –C1257, 1992. 36. Quadri SK, Bhattacharjee M, Parthasarathi K, Tanita T, and Bhattacharya J. Endothelial barrier strengthening by activation of focal adhesion kinase. J Biol Chem 278: 13342–13349, 2003. L459