AANA Journal Course - American Association of Nurse Anesthetists
advertisement

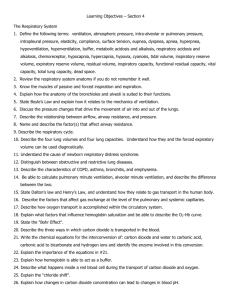
*6 CE credits AANA Journal Course 1 Respiratory System I Preoperative evaluation and physical assessment of the patient NANCY J. WITTSTOCK, CRNA, MS Detroit, Michigan Traditionally,the physical examination and assessment of the patient has been exclusively in the physician'sdomain. Recent expansion of the role of the nurse in critical care and the evolvement of the nurse practitionerhas necessitated the development of expertise in physical assessment. It is equally important that nurse anesthetists develop these skills in order to provide optimum anesthesia care in the pre-, intra-,and post-operative periods. While it is true that physical assessment is now included in the majority of nurse anesthesiacurriculums, this did not occur until approximately the mid-1970's or even later, depending on the area. The purpose of this article, the first in the "Preoperative PhysicalAssessment of the Patient"series, is to provide not only the "how to" of physical assessment, but also to discuss the implicationsof abnormalphysical findings and their impact on planning the anesthesia care plan. Objectives: 1. Describe the technique of inspection, palpation, percussion and auscultation of the lungs and thorax. 2. Discuss several significant findings in the preoperative evaluation of the respiratory system. 3. Discuss the key points in the intraoperative management of the patient with obstructive lung disease. A thorough history and physical are the foundation of the patient's preoperative evaluation. If pulmonary dysfunction is suspected a more complete evaluation is indicated including pulmonary function tests, chest x-ray, ECG and arterial blood gases. Three basic goals should be kept in mind when evaluating the patient: (1) determination of the severity of disease; (2) formation of a plan to optimally prepare the patient for surgery and (3) application of appropriate prophylactic measures in the preoperative period so as to minimize or eliminate postoperative complications. *As part of the AANA Continuing Education Program, this course has prior approval for continuing education credit. The course will consist of six successive articles, each with a self-test and sources for additional reading.At the conclusion of the six-part series, a final examination will be printed in the AANA Journal. Successful completion of the examination will yield the participant 6 CE Credits. April/1981 History In reviewing the pulmonary history, it is important to look for dyspnea, cough, sputum production, color of sputum, past history of pulmonary disease, occupational exposure to airborn irritants (coal dust, paint fumes, silicone dust, and the like) and the patient's smoking history. Cigarette smoking, if excessive, and sputum production greater than 2 ounces per day are associated with increased risk of postoperative complications. Physical assessment of the lungs and thorax The four basic methods of physical assessment are inspection, palpation, percussion and auscultation, commonly referred to as IPPA. The examination should proceed in an orderly fashion, working from the top of the chest toward the bottom. The patient should be seated comfortably and undressed to the waist for the first part of the examination. Proper lighting is important for visual inspection. Physiological variations are not only common from one patient to the next, but can be present on an individual basis as well. Thus, it is useful to compare one side to the other during the examination; in this way, the patient can serve as his or her own control. The posterior chest should be examined first while the patient is sitting. Then, he or she can lie down for examination of the anterior chest. Like any new skill, physical assessment examining techniques require knowledge and consider- able practice in order for the anesthetist to become adept at them. Until these skills are developed, it is important to have someone already experienced in physical examination check on your performance and the accuracy of your findings. Localization of findings is accomplished by using important landmarks such as the suprasternal notch or Angle of Louis. First, palpate the suprasternal notch at the top of the manubrium, then "walk" your fingers down a few centimeters until you feel a bony ridge which joins the manubrium to the body of the sternum (Figure 1). The second rib attaches to the sternum at the Angle of Louis and the second intercostal space lies directly below. As you proceed downward, the ribs and interspaces can be palpated down to the tenth rib. Anatomical lines are also useful for reference points and, when used in conjunction with a particular rib or interspace, can be used to localize abnormal findings. Inspection. During the physical examination, a general impression of the patient's respiratory status should be ascertained. The patient should be observed for the work of breathing, use of accessory muscles, posture, facial expression, nasal flaring, and respiratory rate and pattern. Extrathoracic signs indicative of chronic hypoxemia such as digital clubbing and cyanosis should also be noted. The thorax is visually observed both posteriorly and anteriorly for any number of ab- Journal of the American Asscauat on of Nurse Aneathetsuu chial structures transmit vibration. Decreased vocal fremitus may occur with bronchiole obstruction or if there is an abnormal accumulation of air or fluid in the pleural space. normalities that could be a sign of pulmonary distress (Table I). Palpation. The chest is manually palpated to identify areas of tenderness and to assess any abnormalities that were observed during the inspection stage. Palpation. further assesses respiratory excursion and elicits vocal or tactile fremitus. Vocalization causes a vibration of air in the tracheobronchial tree which can be felt by the anesthetist when palpating the chest wall. This vibration can be palpated and is called vocal fremitus. It can be elicited when the patient is instructed to say "ninety-nine" at each area of palpation. During this phase of the examination, the anesthetist should place the palmar bases of the fingers of one hand on the patient's chest, com- Percussion. Percussion of the chest produces motion in the chest wall and underlying lung which causes audible sounds and palpable vibrations. Different sounds are elicited depending on the density of the underlying tissue. Percussion helps the anesthetist to determine whether the underlying tissue is air filled (as in the normal lung), fluid filled or solid. Since percussion usually penetrates less than 7 cm, it is not useful in detecting dec, lesions. With practice, you should learn to distinguish five percussive notes, each differentiated by variances in intensity, pitch and duration (Table II). Start at the lung apex and percuss the entire lung field, working progressively from top to bottom. The technique of percussion involves pressing the distal phalanx of the middle finger on the paring each region that is palpated. For example, compare the left apex to the right, the left middle lung region to the right, and so forth. Vocal fremitus is normally increased in the parasternal area near the second right interspace where major bron__ Table I Visual observations of the thorax Examplee of abnormalktiea 1'. Thoracic deformities Kyphoscollosls, pectus carinatum (pigeon chest), pectus excavatum (funnel chest), barrel chest (Increase AP diameteremphysema) 2. Slope of the ribs More horizontal-emphysema 3. RetractIon or bulging of the interspaces Obstruction-asthma, COPD 4. Impaired respiratory movement Obesity, neuromuscular weakness, COPD 5. Rate and pattern of breathing Tachypnea, COPD, prolonged expiration, shortness of breath 6. Use of accessory muscles: Inspiration-neck muscles Expiration-abdominal muscles Asthma, emphysema, COPD Table II Slgnificance of percussive notes Intensity Pitch Duration Location Abnormality Flatness soft high short thigh fluid in pleural space Dullness medium medium medium liver atelectasis Resonance loud low long normal lung Hyperresonance very loud low longer emphysematous lung Tympany loud gastric air bubble I *pri/1981 pneumothorax , - - 199 chest. Avoid contact with any other part of the hand as this would damp the vibrations. With the middle finger of the other hand, strike a sharp blow on the distal phalanx making sure the wrist is relaxed (Figure 2). The action involves a rhythmic flexing of the wrist using short, staccato blows. Auscultation. The last part of the physical assessment examination is auscultation of the lung fields, usually done with the diaphragm of the stethoscope. Auscultation aids in both determining air flow through the tracheobronchial tree and lung parenchyma and the presence of secretions or obstruction resulting in abnormal or absent breath sounds. The patient should breath deeply through his mouth as each area is auscultated. Care should be taken in the pacing of the examination so that the patient does not become dizzy from hyperventilating. Listen for the quality and intensity of breath sounds and the presence of adventitious or abnormal sounds (Table III). Figure 2 Finger positioning for palpation 1 The lungs are also auscultated for voice sounds which are useful in detecting atelectasis, pleural effusion and consolidation. Surprisingly enough, in the presence of these abnormalities, voice sounds are actually transmitted more clearly. This phenomenon is called bronchophony. Whispered pectoriloquy is an exaggeration of bronchophony and indicates a very clear transmission of whispered words heard with the stethoscope. Egophony is present if the spoken "EE" sounds more like "AY". Additional considerations during the examination Adventitious sounds. There are a number of adventitious or abnormal sounds, important for the anesthetist to observe, which can be categorized into friction rubs, rhonchi and rales. A pleural friction rub, a coarse, grating sound, is generally heard in late inspiration and early expiration, and is associated with an inflamed pleura. Friction rubs often clear when fluid accumulates in the pleural space. Rhonchi are sounds produced in the airways from an accumulation of secretions. They produce a deep rumbling sound from turbulent air flow and will generally clear with coughing. A wheeze is a particular type of rhonchi that has a musical quality and is heard primarily during expiration when bronchoconstriction is present. Rales sound somewhat like the crinkling of cellophane and occur when there is an accumulation of fluid in the alveoli, as in pulmonary edema, congestive heart failure or pneumonia. In emphysema, a marked decrease in the intensity of breath sounds is the chief and single most reliable physical symptom. Other signs, in decreasing order of reliability are: prolonged exhalation, decreased lung expansion, use of accessory muscles, decreased diaphragmatic activity, pursed-lip breathing and barrel chest (increased A-P diameter). The patient with chronic bronchitis presents different physical findings although both emphysema and bronchitis are manifested in marked expiratory obstruction to airflow. The classic picture of chronic obstructive Table III Auscultation interpretations Normal breath Insp:Exp Expiratory Expiratory sounds duration pitch Intensity Location Vesicular Insp. > Exp. low soft majority of lungs Broncho-vesicular Insp. = Exp. medium medium near the main stem bronchi Bronchial Exp. > Insp. high usually loud over the trachea Journal of the American Association of Nurse Anesthetists pulmonary disease (COPD) generally involves a mixture of the symptoms of chronic bronchitis and emphysema. The bronchitic patient frequently has rhonchi and wheezing, and "noisy breathing" can often be heard without the aid of a stethoscope. A simple test for retained secretions common in chronic bronchitis is to ask the patient to take a deep breath and forcibly exhale a few times. This usually results in an attack of paroxysmal coughing and wheezing. Chest x-ray Examination of the chest is incomplete without a chest x-ray. Normal lung parenchyma appears black on film, whereas atelectasis or an accumulation of fluid in the alveoli appears as a whitish density. Acute changes noted on the chest film should be treated and surgery postponed until improvement is evident both clinically and on repeat film. A very important point to remember is that significant pulmonary dysfunction may be present even though the chest x-ray appears perfectly normal. ECG An electrocardiogram (ECG) is included in the evaluation procedure, with attention directed to right atrial hypertrophy or right ventricular strain pattern. Electrocardiographic changes are a late sign of pulmonary disease and usually do not develop until the patient has pulmonary hypertension (which may lead to right heart failure or cor pulmonale). Arterial blood gas measurements The ease with which arterial blood gases can be obtained and measured is one of the outstanding developments in respiratory care in the last decade. Many hospitals that have a large surgical schedule now have a blood gas machine in the recovery room where it is readily available for use in evaluating patients postoperatively. Even the smallest hospital should be equipped with at least one blood gas machine; the valuable information it gives far out-weighs the purchase price. The primary function of the lungs, exchange of oxygen and carbon dioxide, is easily assessed by measuring blood gases (Table IV). The PaO2 is often less than 80 torr with advancing age (patients older than 60 years), due to progressive ventilation perfusion inequality that is a normal part of the aging process. A PaOs less than 70 torr on room air should always be investigated. While blood gases are not routinely drawn preoperatively, they should be drawn and April/1981 evaluated if the patient has significant clinical symptoms of pulmonary dysfunction and/or grossly abnormal pulmonary function tests. Pulmonary function tests Pulmonary function tests are vital in documenting the existence of and assessing the degree of dysfunction. Frequently, physical examination and chest x-ray fail to reveal significant airway obstruction in patients with obstructive lung disease. The spirometer functions as an extension of the stethoscope and should be used routinely in patients with pulmonary disease, just as the ECG is used in patients with heart disease. Abnormal spirometric studies are generally categorized as restrictive or obstructive. A restrictive abnormality indicates inspiratory obstruction to airflow and is reflected in a decreased vital capacity in the presence of normal expiratory flow rates. An obstructive abnormality indicates expiratory obstruction to airflow and is reflected in a decreased forced expiratory volume in one second (FEV1), peak flow rate (PFR), mean forced expiratory flow (FEF 25-75%) and forced vital capacity (FVC). Currently utilized spirometry varies from simple bedside tests, such as the vital capacity and peak flow rate, to sophisticated computerized programs that provide complete spirometric evaluation. The volume of air exhaled during the first second of the FVC is the FEV1. It is a standard means of evaluating large airway (greater than 2 mm in diameter) obstruction. When expressed as a percent of FVC, less than 80% indicates obstructive disease and greater than 80% indicates restrictive disease. (Figure 3). FEF 25-75%. This test measures the maximum mid-expiratory flow rate during the middlehalf of the FVC. A decrease is indicative of early Table IV Arterial blood gas interpretations Arterial Normal blood gases rage ?MeaWsre PaCO 2 35-45 torr Adequacy of ventilation (respiratory parameter) PaO 2 80-100 torr Adequacy of oxygenation pH 7.35-7.45 HCO 3 22-25 meq/L Metabolic parameter Base excess +2 -2 Acid-base status Metabolic parameter small airway disease (less than 2 mm in diameter). This important prognostic test is indicated for asymptomatic smokers because it detects small airway disease, the earliest manifestation of chronic bronchitis. Closing volumes. The closing volume is a measurement of the lung volume at which airways begin to close in the dependent areas of the lung. This test is also a sensitive indicator of early small airway disease. When abnormal, this test provides a valuable prognostic sign of probable development of obstructive lung disease. Simple bedside screening tests. These tests encompass (1) tidal volume and minute volume, (2) forced vital capacity, (3) negative inspiratory force, and (4) peak flow rate. Simple spirometry-like tidal volume, minute volume and forced vital capacity can be directly measured at the bedside with a hand-held respirometer attached to an anesthesia face mask. The patient can hold the mask on his or her face and breathe through it one full minute while the respiratory rate is counted. At the end of the minute, the face mask is removed and the minute ventilation volume can be read directly off the face of the respirometer. The average tidal volume is calculated by dividing the minute ventilation in milliliters by the respiratory rate. Normal values for tidal volume are 6-7 ml/kg. For minute ventilation, the values are 58 liters. Forced vital capacity (FVC) is measured by instructing the patient to hold the mask onz his or her face, take a maximal inspiration, and then exhale as rapidly as possible through the mask. At this point, the mask is removed, and the FVC is read directly off the face of the respirometer. Patient cooperation is essential to correctly perform this maneuver; since errors are common, it is a good idea to repeat the maneuver three times, recording the best of three readings. The FVC is a rough measurement of the patient's ventilatory reserve. It has been deter- mined that a minimum of 15 mI/kg is essential in order to have sufficient mechanical ability to take a deep enough breath to generate an effective cough. For this reason, patients are generally not extubated until their FVC is at least 15 mI /kg. If less, the endotracheal tube is left in place and used as a route for tracheobronchial suctioning. The negative inspiratoryforce (NIF) is an alternate means of assessing ventilatory reserve and is especially useful in the uncooperative or obtunded patient who is unable to perform a forced vital capacity. A manometer that registers negative pressure is adapted to a face mask or artificial airway. The manometer is occluded for 15-20 seconds during which time the patient inspires against an occluded airway. This creates a negative pressure reading on the manometer. The normal NIF is as much as -80 cm H 2 0 pressure in a patient with normal ventilatory mechanics. It has been determined that a min- imum of - 20 cm H 2 0 pressure is necessary to have muscle power sufficient to generate an effec- tive cough. Therefore, patients should not be extubated unless this minimal value is attained. Peak flow rate (PFR). The PR is the fastest, easiest and most sensitive single breath pulmonary function test available. An example of the instru- Figur. 3 mentation available is the Wright's peak flowmeter. Such a flowmeter is inexpensive and port- Normal, obstructive, and restrictive patterns of a forced expiration. able so it may be used at the patient's bedside to Norm#al Obstructive Restrictive measure the expiratory flow rate. Since maximal flow rates occur at the beginning of expiration, a complete exhalation spirogram is not (which may FI £ FEV used -- :: FEV=4.Q FVC-5.O :Fvra: 1 FVC PVC FVC:~: .I FEV=1.3 FVC-3.1 %_O%42 (Adapted with permlslon franm W~rt.12 ) FEV: is not necessary. Because a used, initial breath holding be difficult for the dyspneic patient) is unnecessary. The patient is instructed to take a deep breath then exhale as rapidly as possible through the mouthpiece. The expiratory flow rate is read directly on the face of the peak flowmeter. used This is a valuable, pulmonary screening tool that can be used not only for preoperative evalua- FEV-2.8 FVC-3.1 tion, but also for postoperative follow up. Decreases in flow rate associated with obstructive lung %,mg0 disease can be demonstrated earlier in the peak flow rate than with any other single breath maneuver. Journal o/ sta Aeri*.n Ae.fsku ej o Nunt. An~ahkoide Preoperative management Since COPD is undoubtedly the most common type of pulmonary dysfunction the anesthetist faces in everyday practice, the remainder of this article will focus on pre-, intra- and post-operative management considerations in the patient with obstructive lung disease. The identification of risk factors associated with pulmonary complications is a key part of preoperative anesthetic management. Of all the risk factors, bronchospasm, retained secretions and infection are the most amenable to therapy. A thorough evaluation of the patient provides sufficient information to formulate an effective plan of therapy designed to optimize lung function before surgery. Numerous studies have indicated that appropriate therapy before surgery decreases morbidity and mortality. A statistically significant decrease in postoperative complications was reported by Gracey and colleagues, who recommend a systematic approach to preoperative preparation using a standard protocol that can be understood and followed by the nursing staff and other health care professionals. Preoperative mobilization of secretions from the airways may be the main beneficial result of such intensive preparations for surgery, thus preventing or minimizing retention and consequent infection and atelectasis. After identifying the patient's needs, various therapeutic modalities may be indicated. It is desirable for the patient to stop smoking three to four weeks prior to elective surgery. Unfortunately, this is not always a realistic goal; and it is difficult to improve bronchial hygiene if the patient continues to smoke. Bronchial hygiene therapy Systemic hydration. Adequate systemic hydration is the most important method of decreasing the vicosity of thick secretions to promote expectoratio. Patients should be encouraged to drink at least two quarts of water a day. Supplemental parenteral fluids may be indicated in the aged and debilitated. Some authorities feel that aerosol therapy is no more than an adjunct to good systemic hydration and can never be as effective alone. Aerosol Therapy. Bland mist aerosols such as saline, sodium bicarbonate, or propylene glycol solutions may be useful in hydrating the airway and liquefying secretions. Many fail to realize that 10.15 min aerosol treatments probably deposit very little moisture in the airways. The length of therapy depends on the patient's problem and may range from 30 min treatments four times a day to April/1981 virtually continuous inhalation to aid in evacuation of secretions. Mobilization of secretions. Once secretions are adequately hydrated, mobilization and expectoration should not present a problem if the patient has an adequate cough mechanism. Patients with significant decreases in expiratory flow rates may not be able to generate an effective cough and will have to be assisted with percussion, vibration, postural drainage, and tracheobronchial suctioning to clear the airways. Infection. Acute infection must be eliminated with the appropriate antibiotics, as determined by culture and sensitivity of the sputum. It is sometimes difficult to distinguish between acute and chronic infection. Purulent sputum usually indicates the need for antibiotics. Chest physiotherapy-postural drainage. The patient with limited ability to cough may require chest physiotherapy maneuvers such as percussion, vibration and clapping to aid in mucociliary clearance. Various positions are indicated to clear specific bronchopulmonary segments. Frequent turning from side to side is very important to prevent increasing ventilation-perfusion inequality in the immobilized patient. Bronchospasm. Various bronchodilators are available to alleviate bronchial spasm. Isoproterenol, at one time very popular when administered as an aerosol, has declined in clinical use in favor of beta, agonists such as terbutaline. Undesirable side effects of tachycardia and palpitations occur less often with these betas agonists. On occasion, the physician may have to try more than one bronchodilator to find one that is effective for a particular patient. Steroids may be useful if the patient does not respond or responds poorly to bronchodilators. Though prednisolone has been frequently used, beclomethasone, a new inhalant steroid, is becoming increasingly popular because it does not have the untoward side effects of systemic steroids such as sodium and water retention, hypokalemia, and psychological disturbances. It is important to appreciate that beclomethasone and another relatively new inhalant drug, cromolyn sodium, are only useful to prevent bronchospasm and are ineffective during an acute attack. In addition to routine laboratory tests, the patient should have electrolytes and baseline arterial blood gases to assess the adequacy of oxygenation, ventilation and acid base status. Ventilation-perfusion inequality due to shunting and increased physiologic dead space is the primary cause of hypoxemia in COPD. The degree of hypo- xemia can be accurately determined only by direct measurement of arterial blood gases. An abnormal chest x-ray can be a reliable predictor of the presence of moderate to severe emphysema. A normal film does not exclude the presence of emphysema and no single finding or combination of findings has been described which serves especially well to detect early asymptomatic disease. Typical findings in long-standing disease include: low, flat diaphragms; hyperinflation; increased anterior-posterior diameter and increased lung markings. Roentgenographic abnormalities, considered by some authorities to be due to bronchitis, include over-inflation, parallel lines, "tram tracks" which may represent thickened bronchial walls and an increase in lung markings. Electrocardiographic abnormalities commonly associated with COPD include tall, peaked P waves, right axis deviation and right ventricular hypertrophy. Generally, these abnormalities appear to be secondary to increased pulmonary vascular resistance and are seen only in relatively advanced disease. Atrial and ventricular arrhythmias attributable to hypoxemia are common and have been found to occur in a large number of patients on routine electrocardiograms. Monitoring for 72 hours demonstrates that arrhythmias occur in the majority of hospitalized patients with moderate to severe COPD. Prior to surgery, the patient should be counseled as to the importance of deep breathing and coughing after surgery. One of the most valuable respiratory maneuvers designed to prevent atelectasis and maintain optimal lung function is the sustained inspiratory maneuver or voluntary maximal inhalation. Deep-breathing exercises with emphasis on sustained inspiration to total lung capacity have been consistently effective in expanding alveoli and preventing pulmonary complications. A device called the incentive spirometer is becoming increasingly popular in helping the patient to perform sustained inspiratory maneuvers. Utilizing such devices, the patient is able to observe his or her own progress and is stimulated to improve. Incentive spirometry is goal oriented and often has a positive psychological effect because patients feel they are personally contributing to their recovery from surgery. Intraoperative management The COPD patient should arrive in the operating room only after receiving thorough preoperative preparation designed to optimize lung function. Preoperative medication should be sufficiently light to avoid respiratory depression. If the patient is not in pain, a mild tranquilizer such as hydroxyzine or oral diazepam is usually sufficient. A small dose (25 mg) of intravenous lidocaine will prevent the burning sensation that often occurs with the injection of diazepam into a superficial vein. Since it interferes least with ventilatory mechanics, regional anesthesia is desirable for surgery on the extremities. Spinal anesthesia may interfere with the patient's ability to contract abdominal musculature and should be used with caution in patients with advanced COPD who must use their abdominal muscles to effectively exhale. If general anesthesia is required, several factors must be kept in mind for safe, successful management. The induction of general anesthesia is associated with the development of a 10-15% increase in right to left intrapulmonary shunting which can be attributable to a variety of factors. Functional residual capacity (FRC) decreases between 15-30% whether ventilation is spontaneous or controlled. This appears to be a constant occurrence during anesthesia although the exact mechanism is unknown. As FRC falls below critical alveolar volume, airway closure occurs, particularly in dependent parts of the lungs. These factors lead to increasing ventilation perfusion inequality and impaired oxygen transport; therefore, it is advisable to administer at least 40% oxygen when anesthetizing patients with known pulmonary dysfunction. A patient with normal lung function can be denitrogenated by inhaling 100% oxygen within approximately five minutes. The COPD patient may require 15-30 minutes to denitrogenate because of an increase in physiologic dead space which is most common in emphysema. Physiologic dead space is defined as that portion of the total ventilation that does not exchange with pulmonary capillary blood and is thus "wasted ventilation." Preoxygenation should begin as soon as possible to attain an optimal PaO2 prior to induction of anesthesia. A patient with severe hypoxemia and hypercarbia, whose primary stimulus to breathe is through the "hypoxic drive," must be observed carefully during preoxygenation since respiratory depression may develop. The choice of halothane, enflurane or a bal. anced technique (nitrous oxide, narcotic, relaxant) is probably not as critical as the technique and skill with which the anesthesia is administered. The key points of management are: awareness of the underlying problems associated with the disease process and assuring adequacy of oxygenation, ven- Journal of the American Association of Nwrse Aaesthetist tilation and acid base balance. Halothane, a bronchodilator, is advantageous in the COPD patient who has bronchospasm. A recent study by Rodriquez and Gold suggests that enflurane is equally satisfactory for general anesthesia. In addition, an inhalation agent facilitates the use of high oxygen concentrations. While changes in PaCOa and PaO 2 are relatively predictable in patients with normal lung function, the COPD patient does not respond predictably to changes in ventilation and fractional inspired oxygen concentrations (F10O). Therefore, it is necessary to monitor arterial blood gases. If the patient had compensated respiratory acidosis preoperatively, as evidenced by an elevated PaCO2 and HCO3 and normal pH, excessive ventilation could result in a severe alkalosis. Various hazards have been attributed to alkalosis, including cardiac arrhythmias, hypokalemia, shift of the O,-Hb dissociation curve to the left resulting in both increased Hb-O affinity and decreased tissue oxygenation, and decreased cerebral blood flow. Whether ventilation is assisted or controlled, an appropriate I:E (inspiration to expiration) ratio is important to facilitate adequate distribution of ventilation and assure sufficient time for exhalation. A two second inspiration and four second exhalation is usually satisfactory, although some patients with marked obstruction may require longer to completely exhale. If air trapping is to be avoided, exhalation should be allowed to continue until no further breath sounds are audible via esophageal or precordial stethoscope. Many emphysematous patients have blebs or surface bullae which may rupture during positive pressure ventilation. All lung fields should be auscultated as frequently as possible. Peak inspiratory pressures should be monitored to help in the recognition of a tension pneumothorax, which, if present, requires immediate insertion of a thoran tpmy tube. Postoperative mana ament Several factors impact on the immediate postanesthetic care of the patient: type and duration of surgery, severity of pulmonary disease and condition of the patient at the time of surgery. A patient with a preoperative forced expiratory flow in one second (FEVi) of less than 2 L and a forced vital capacity (FVC)of less than 15 ml/kg is a high risk for development of postopetative respiratory falure and should receive elective mechanical ventilation. An intermittent mandatory ventilation (IMV) mode is advantageous because it allows s patient to maintain spontaneous ventilation during April/1981 which gas is primarily distributed to the dependent areas of the lung. IMV offers several advantages in that it: (1) minimizes respiratory muscle asynchrony, (2) minimizes deleterious hemodynamic effects, (3) minimizes sedation requirements, and (4) simplifies weaning. In contrast, controlled ventilation tends to deliver a larger portion of the tidal volume to nondependent areas of the lung where perfusion is less, thus causing an increase in the ratio of dead space to tidal volume (VD/VT). IMV maximizes any spontaneous ventilatory activity the patient may have. The decrease in intrapleural pressure that occurs with each spontaneous breath enhances venous return and aids in maintaining hemodynamic stability. The same sophisticated monitoring that was utilized intraoperatively should be continued in the immediate postoperative period until the patient is fully recovered from the effects of anesthesia. Meticulous clinical assessment of the patient's ability to maintain adequate spontaneous ventilation should be utilized prior to extubation, along with objective measurable criteria such as forced vital capacity (FVC) and negative inspiratory force. Should it be necessary for the patient to remain intubated for tracheobronchial toilet, a small amount of positive end expiratory pressure (PEEP) is currently recommended to prevent the fall in PaO that often occurs in intubated patients. The oxygen deficit is usually reversed when 3-5 cm HiO PEEP is applied. Extubation should occur as soon as feasible since the presence of an endotracheal tube prevents glottic closure and interferes with the ability to cough effectively. Controlled oxygen therapy which is sufficient to maintain a normal PaO2 should be monitored with serial arterial blood gases. Deep breathing exercises and sustained maximal inspirations (SMI) should be instituted as soon as possible to prevent atelectasis. Narcotics should be given judiciously to avoid respiratory depression yet control pain sufficiently to enable the patient to take deep breaths. Post-thoracotomy, intercostal nerve blocks will facilitate deep breathing and help prevent atelectasis. Conclulson This article has outlined the key points in evaluating and preparing the patient with pulmonary dysfunction for surgery. These points represent the ideals for which to strive. Unfortunately, conditions are not always optimum and occasionally, in an emergency situation, one is forced to anesthetize a patient with severe pulmonary dys- function who has not had the benefit of preoperative extensive evaluation and preparaion. In such caines, it is safest to anticipate pro emus gical procedure, because alarming degrees of hypounder 'anesthesia in the patient xemia may occur with undocumented pulmonary disease. Serious consideration should be given to postoperative mechanical ventilation until a more thorough evaluation of the patient's pulmonary status is I which is the tN~~, Wit; A4I L OWLWGEMENT Flue au~thor wishes to expresa her gratitude to Rosmary Iscretarl! of the ~Iey Ford Ho0ptal Universty of ur * ~ e Pro resui for her patdmuce anal aadt lie p r a ,o this areids. tgla Cum Laude t Nursin in Dervt WMin She "RNA, KS, ,la 4tast cool.-of Anaduesa, ))etroit. In r. Uatb*~s ad Master's degree. in ate Uniesty Colleg of Phuiquay hii pra tcedI clinical ass anmbser of years. In lW s nw the Waybw ate Utulverulty PI als held various academic ap-, fteCu~c %l ri ator at the iAe sd 44usty of Detroit, Mt'She & els br Re.rougot the a speer at uember of the -pat Sea r The Johns Hopkins University School of Medicine presents A LOOK AT ANESTHESIA TODAY MAY 9-10, 1981 NURSE ANESTHETIST CERTIFIED-REGISTERED Progressive extremely modern 470-bed university affiliated teaching hospital noted for high quality of patient care offers attractive positions involving a broad range of surgical procedures. Certification and registration required. The hospital is easily commutable from Manhattan, Brooklyn and northern N.J. For Further Information: Program Coordinator Turner Auditorium Building Room 22 720 Rutland Avenue Baltimore, Maryland 21205 (301) 955-5880 Call us about our NEW SALARY RATES and arrange an interview appointment at 390-9305. STATEN ISLAND HOSPITAL 475 Seaview Ave. Staten Island, N. Y. 10305 an equal opportunity employer m/f/h I CHARLES C THOMAS New! COMMUNICATION AND COMPLIANCE IN A HOSPITAL SETTING edited by David J. Withersty, West Virginia Univ. School of Medicine, Morgantown. (13 Contributors) Contributors from the disciplines of medicine, physical therapy, social work, and mental health define the problem of patient noncompliance, explore its probable causes, and offer solutions. A sampling of chapter topics includes noncompliance as a diagnostic issue, environmental influences upon compliance, practical aspects of communications research, and educating students and housestaff regarding compliance and other psychosocial issues. '80, 208 pp., 11 il., 4 tables, $18.50 SPUBLISHER New! DIMENSIONAL ANALYSIS IN THE BIOMEDICAL SCIENCES by Bernard Schepartz, Jefferson Medical College, Philadelphia.The author herein employs a pragmatic, instrumental approach to explain the application of dimensional analysis to the biomedical sciences. By operating largely on the level of algebra, he facilitates the nonmathematician's understanding of these processes. Beginning with an explication of the basic concepts of dimensional analysis, the author then shows how dimensional analysis can help to solve complex problems related to the biomechanics of solids and fluids; surface phenomena, diffusion, and membranes; energy and work; enzymes and metabolism; and allometry and scaling. '80, 184 pp., 9 il., $19.75 SYNOPSIS OF PATHOLOGY FOR THE ALLIED HEALTH PROFESSIONS by Alvin F. Gardner, Food and Drug Administration, Washington, D.C. This text explains the latest concepts in general pathology while providing the reader with a thorough understanding of the local and systemic basis of disease. Specific areas of pathology covered include, among others, congenital anomalies and hereditary diseases, repair and regeneration, heart and blood vessels, the respiratory system, blood and bone marrow, the skin, and the nervous system. Numerous appendices feature laboratory values, chemical compounds, and a wealth of other valuable data. '79, 480 pp., $34.50 A PICTORIAL HISTORY OF MEDICINE (5th Ptg.) by Otto L. Bettmann, Bettmann Archive, New York City. Foreword by Philip S. Hench. This profusely illustrated volume depicts the great physicians, the key inventions, and the crucial discoveries of medicine. Each medical landmark is presented in a compact pictorial unit that delineates the technical perspective and relates the healing arts to their concurrent cultural movements. A review in Surgery, Gynecology and Obstetrics stated, "Perhaps nowhere else can one obtain so clearly and quickly a broad grasp of medical history." '79, 336 pp. (8 1/2 x 11), 1000 il., $16.00, paper MONITORING SURGICAL PATIENTS IN THE OPERATING ROOM edited by J. S.sGravenstein, Case Western Reserve Univ., Cleveland, Ohio; Ronald S. Newbower, Harvard Univ., Cambridge, Massachusetts; Allen K. Ream, Stanford Univ., Stanford, California; and N. Ty Smith, Univ. of California, San Diego. (34 Contributors) Clinical aspects, developing trends, and new concepts are reviewed in this volume on cardiovascular, respiratory, and central nervous system monitoring. Specific topics include monitoring neuromuscular functions, systolic time intervals, ventilation, anesthesia management systems, and anesthesia keyboard systems. '79, 288 pp., 78 il., 19 tables, $25.75 REGIONAL BLOCKS FOR NURSE ANESTHETISTS: A Technical Manual by Phyllis Adams Roberts, Des Moines, Iowa. This text describes methods for administering spinal, axillary block, and intravenous regional anesthesia. The author discusses the most commonly used drugs, premedication drugs, and dosage calculation. The section on spinal anesthesia includes information on positions, methods of holding the needle, prevention of hypotension, and techniques for puncturing the subarachnoid space when difficulties arise. The patient's anesthetic record, the basic mid-line decubitis approach, a variation of that method using the lateral approach to the mid-line, and the Taylor approach are also detailed. '78, 128 pp., 26 il., 1 table, $11.75 A MANUAL OF THORACIC SURGERY by Arndt von Hippel, Private Practice, Anchorage, Alaska. Foreword by Alfred Tector. The author brings together useful old and new approaches and concepts for mediastinal and pericardial drainage; he expands upon simple and clinically proven practices; he clearly and definitively identifies and analyzes the hazards inherent in many currently marketed chest drainage devices. The approaches and techniques outlined in this carefully organized and eminently practical book will improve patient care and expedite recovery in any thoracic surgical service. '78, 264 pp., 9 il., cloth-$18.75, paper-$11.50 RESPIRATORY INTENSIVE CARE edited by Robert M. Rogers, Univ. of Oklahoma Health Sciences Center, Oklahoma City. (38 Contributors) Contributors provide selections on diagnosis and clinical presentation of respiratory failure, the logistics of establishing a respiratory intensive care unit or service, acid-base balance as it relates to respiratory failure, gas exchange in chronic obstructive lung diseases, oxygen transport, oxygen therapy and nonventilatory therapy of respiratory failure, and the principles of mechanical ventilation. '77, 448 pp., 138 il. (3 in color), 36 tables, $37.50 THE PHARMACOLOGY OF ANESTHETIC DRUGS: A Syllabus for Students and Clinicians (5th Ed., 3rd Ptg.) by John Adriani, Tulane Univ. School of Medicine, New Orleans, Louisiana. The format of this volume is one of succinct statements describing the effect of a particular anesthetic or combination of anesthetics on a specific organ system. Sections are included on uptake and distribution of anesthetics, which summarizes present day concepts; on the new inhalation anesthetics such as halothane, fluoroxene, and vinyl ethyl ether; on adjunctive drugs; and on premedication, hyperthermic and hypotensive anesthesia, and carbon dioxide absorption. '77, 320 pp. (9 x 12), 128 il., $30.00 PHYSICS FOR ANAESTHETISTS by James Duffin, Univ. of Toronto, Toronto, Ontario, Canada. Foreword by R. A. Gordon. Using the necessary basics - mathematics, mechanics, and units of measurement - this text examines the elementary behavior of atoms, heat, gases, vapors, and fluids. Essential aspects of fluid flow and electricity are given careful and thorough consideration. Overall concepts of patient monitoring and commonly used methods of gas analysis also are examined. An underlying philosophy of problem solving forms the basis for this introductory text. '76, 296 pp., 109 il., 19 tables, $22.25 Orders with remittance sent, on approval, postpaid * Catalog of 2924 titles sent on request 301-327 East Lawrence Avenue * Springfield * Illinois * 62717