P274 Diagnostic accuracy of fecal calprotectin and M2
advertisement

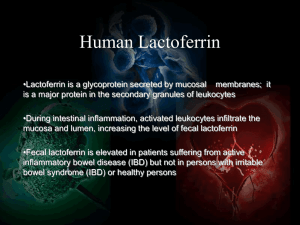
Abstracts of the 10th Congress of ECCO - European Crohn’s and Colitis Organisation P274 Diagnostic accuracy of fecal calprotectin and M2pyruvate kinase in the prediction of endoscopic activity Crohn's disease V.M. Juan María*, P.-M. Héctor, B.-R. Beatriz, O.-M. Rosario, C.-C. Manuel, R.-L. Manuel Hospital General Juan Ramón Jiménez, UGC Aparato Digestivo, Huelva, Spain Background: Fecal calprotectin and M2-pyruvate kinase (M2-PK) are useful biomarkers to diagnose inflammatory bowel disease. Several studies have shown a high correlation between intestinal injury and the levels of fecal biomarkers but no consensus on the optimal cutoff for establishing endoscopic activity. The aim this of study is to analyze the diagnostic accuracy of fecal calprotectin and M2-PK to predict endoscopic activity in Crohn´s disease (CD). Methods: An observational and prospective study was designed. 71 patients with CD underwent a colonoscopy calculated simple endoscopic score for Crohn´s disease (SES-CD) and Crohn disease activity index (CDAI). Fecal calprotectina, M2-PK, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were measured. Results: Forty-nine (69%) patients had endoscopic activity (SES-CD > 2). The fecal calprotectin concentration was higher among the patients with endoscopic activity than in remission: 375 µg/g (95% CI 303-448) versus 80 µg/g (95% CI 53-107); p<0.01. For the fecal M2-PK concentration also differences were observed: 17.4 U/l (95% CI 14-21) versus 4.7 U/l (95% CI 1.8-7.6); p<0.01. The SES-CD correlated closest with calprotectin (Spearman´s rank correlation coefficient r=0.739), followed by M2-PK (r=0.576), CRP (r=0.534) and ESR (r=0.516). The overall accuracy for the detection of endoscopically active disease was 92% for calprotectin (cutoff 120 µg/g), 85% for M2-PK (cutoff 4.5 U/l), 81% for CDAI, 74% for CRP and 72% for ESR. Conclusions: Fecal calprotectin was the biomarker to predict more accurately endoscopic activity, followed by M2-PK. Serological biomarkers and CDAI have less accuracy. Fecal biomarkers, especially calprotectina, are tools with high precision to predict endoscopic activity. P275 Relevance of ultrasonographic parameters in predicting inflammatory bowel disease in a pediatric population. A. Dell'Era*1, D. Dilillo2, E. Galli2, F. Meneghin3, F. Furfaro1, C. Bezzio1, F. Penagini2, C. Mantegazza2, F. Scrignoli2, G.V. Zuccotti2, G. Maconi1 1 Ospedale L. Sacco. Gastroenterology Unit, Università degli Studi di Milano, Department of Biomedical and Clinical Sciences, Milan, Italy, 2Ospedale dei Bambini V. Buzzi, Università degli Studi di Milano, Department of Paediatrics, Milan, Italy, 3Ospedale L. Sacco. Università degli Studi di Milano, Department of Paediatrics, Milan, Italy Background: Bowel ultrasound (B-US) has been widely recognized as a useful examination in patients with suspected IBD, particularly in children, owing to its lack of invasiveness. However, its accuracy relies essentially on one criteria: the detection of increased bowel wall thickening (BWT). The relevance of BWT and the additional value of other US parameters, such as lymph node enlargement and mesenteric hypertrophy (MH), in the diagnosis of IBD have not been investigated so far. This study aims at investigating the diagnostic accuracy of several US parameters in detecting IBDs in a pediatric population. Methods: All patients aged 2-18 years referred to the Pediatric Gastroenterology Clinic of our Hospital from 2007 to 2013 for initial assessment for recurrent abdominal pain and/or altered bowel habits were retrospectively considered.Patients presenting with known organic diseases or already investigated with digestive endoscopy were excluded. Patients were considered eligible if they had a complete B-US report including: altered US bowel pattern (US-BP), BWT, MH, pathologic lymph nodes, free abdominal fluid, presence of stenosis, abscesses or fistulae. Ileocolonoscopy, performed in patients with a high index of suspicion of IBD, on the Variables Se, % (95% CI) Sp, % (95% CI) PPV, % (95% CI) NPV, % (95% CI) Altered US-BP Mesenteric hypertrophy BWT > 3 mm BWT>3 mm + US-BP + MH BWT>3 mm or US-BP or MH 78.3 (69.3–85.2) 65.2 (55.6–73.8) 69.6 (60.1–77.7) 56.5 (46.9–65.7) 82.6 (74.1–88.9) 93.3 (86.6–96.9) 92.2 (85.2–96.2) 96.7 (90.9–99.0) 100 (95.9–100) 86.7 (78.7–92.1) 75.0 (65.8–82.5) 68.2 (58.7–76.4) 84.2 (75.9–90.1) 100 (95.9–100) 61.3 (51.6–70.2) 94.4 (87.9–97.6) 91.2 (84.0–95.5) 92.6 (85.6–96.4) 90.0 (82.6–94.6) 95.1 (88.9–98.1) Downloaded from http://ecco-jcc.oxfordjournals.org/ by guest on October 2, 2016 Methods: A multitude of leftover stool samples, kindly provided by a local routine clinical laboratory, were extracted with the CALEX® Valve device and by conventional laboratory Methods. The stool extracts were then either loaded onto immunochromatograhic test cassettes or analyzed with a commercial ELISA test. The test cassettes were read via the CalApp® installed on different iPhones and Android phones, whereas the ELISA was performed in a spectrophotometer. All common technical performance characteristics of the IBDoc® system were determined, and the quantitative IBDoc® Results were compared to the Results obtained by the laboratorybased ELISA method. Results: The IBDoc® test system produces a quantitative test result between 30 and 1000 µg of calprotectin/g of stool which covers the clinically relevant range of this biomarker. Smartphone model specific calibration parameters were established to correct the measured raw data for differences in camera optics and image processing resulting in correct and equal test Results among a broad range of smartphone models. Measuring the same test cassette 20-times resulted in CVs of 3-6%, while measuring the same stool extract on 20 different cassettes gave CVs of 10-20%. The total imprecision considering variations in stool extraction, test cassette runs and smartphone readouts is in the range of 25% CV. The IBDoc® home test correlates well with a state-of-the-art laboratory-based ELISA method showing a bias of < 20% and R2 of >0.85. Conclusions: IBDoc® is the first complete and validated test system which allows the IBD patient to monitor and follow his inflammatory status by measuring the IBD biomarker, fecal calprotectin, using his own smartphone. The performance of the IBDoc® home testing system is comparable to professional, laboratory-based Methods. S213