CE ONLINE
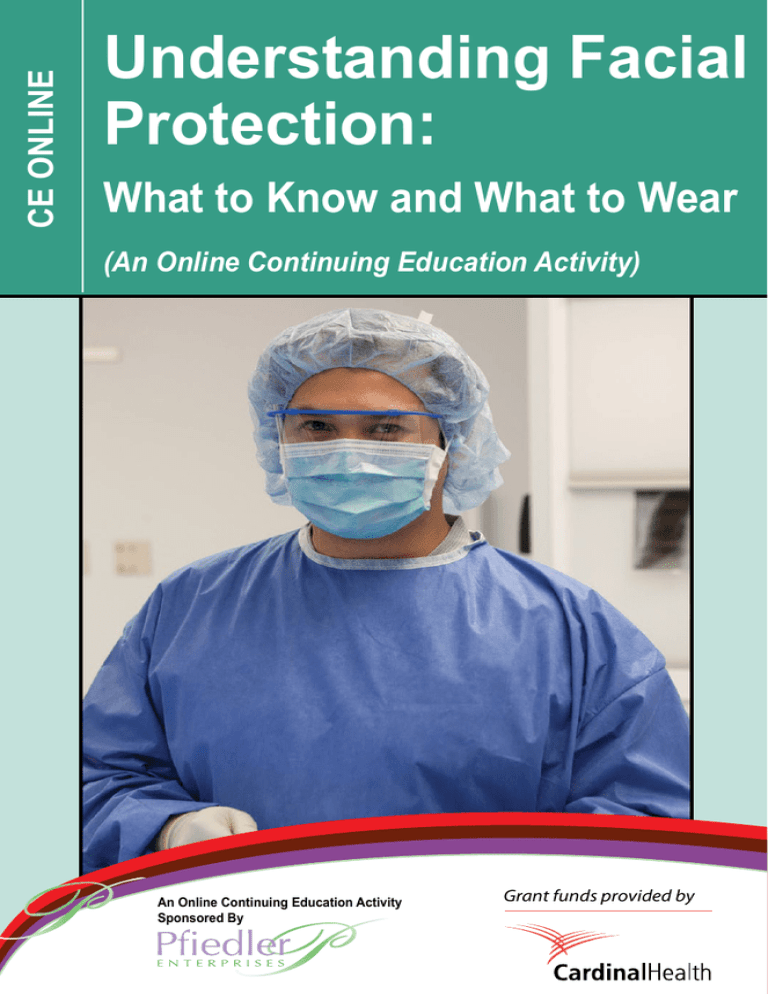
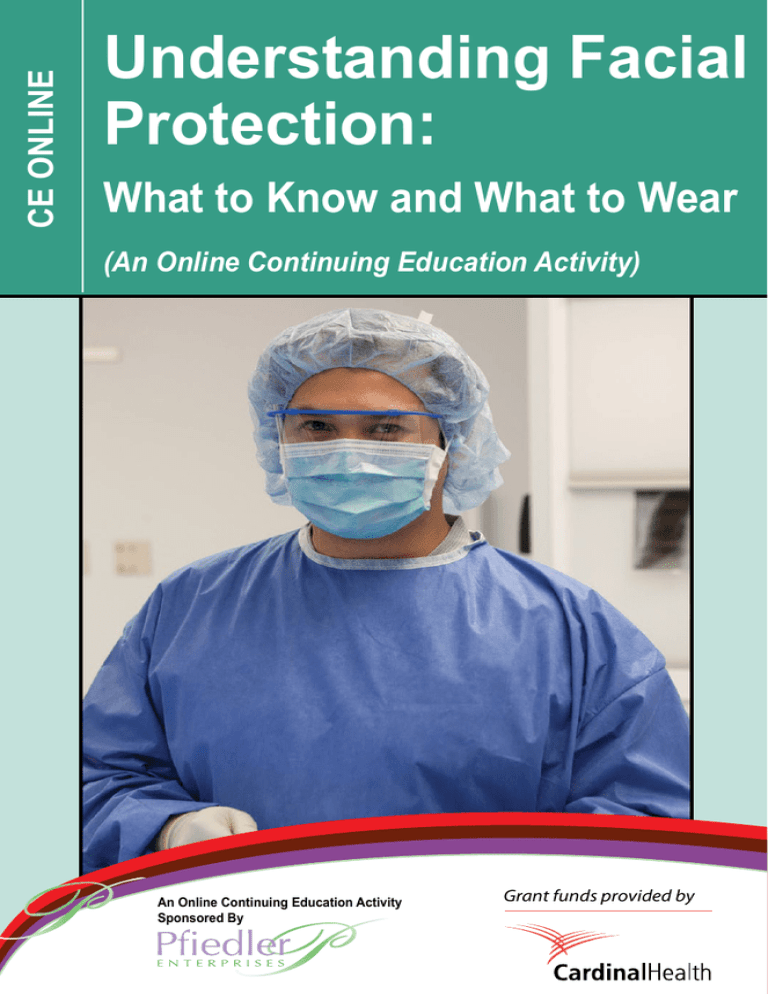
Understanding Facial
Protection:
What to Know and What to Wear
(An Online Continuing Education Activity)
An Online Continuing Education Activity
Sponsored By
Grant funds provided by
Welcome to
Understanding Facial
Protection:
What to Know and What to Wear
(An Online Continuing Education Activity)
CONTINUING EDUCATION INSTRUCTIONS
This educational activity is being offered online and may be completed at any time.
Steps for Successful Course Completion
To earn continuing education credit, the participant must complete the following steps:
1. Read the overview and objectives to ensure consistency with your own learning needs and objectives. At the end of the activity, you will be assessed on the
attainment of each objective.
2. Review the content of the activity, paying particular attention to those areas that reflect the objectives.
3. Complete the Test Questions. Missed questions will offer the opportunity to re-read
the question and answer choices. You may also revisit relevant content.
4. For additional information on an issue or topic, consult the references.
5. To receive credit for this activity complete the evaluation and registration form.
6. A certificate of completion will be available for you to print at the conclusion.
Pfiedler Enterprises will maintain a record of your continuing education credits
and provide verification, if necessary, for 7 years. Requests for certificates must
be submitted in writing by the learner.
If you have any questions, please call: 720-748-6144.
CONTACT INFORMATION:
© 2014
All rights reserved
Pfiedler Enterprises, 2101 S. Blackhawk Street, Suite 220, Aurora, Colorado 80014
www.pfiedlerenterprises.com Phone: 720-748-6144 Fax: 720-748-6196
Overview
Originally, face masks were designed to minimize the risk of wound infection for surgical
patients by preventing the spread of microorganisms expelled from the nose and mouth
of operating room (OR) personnel. Today, confronted with the challenges of new
and drug-resistant pathogens, facial protection devices are used in the perioperative
practice setting to protect health care workers from a variety of potential bloodborne
and inhalation hazards. Furthermore, the proper use of facial protection devices is a key
component in the implementation of Standard Precautions in the OR. The purpose of this
continuing nursing education activity is to provide a review of the clinical considerations
regarding the appropriate selection and use of facial protection devices in various
surgical practice settings. It will provide an overview of the health hazards inherent to the
perioperative environment. The various types of facial protection devices available today
will be reviewed, followed by a discussion of the relevant regulations and professional
recommendations for both the manufacture and use of facial protection devices. Finally,
criteria for appropriate selection and use of facial protections devices will be outlined.
Learner Objectives
Upon completion of this continuing education activity, the participant should be able to:
1. Identify the various occupational health hazards inherent to the surgical practice
setting.
2. Describe the types of facial protection devices available today and their
components.
3. List the regulations governing the manufacture and performance standards of facial
protection devices.
4. Discuss pertinent regulations and professional recommendations regarding the use
of facial protection in the OR.
5. Identify key criteria in the selection and use of facial protection devices for specific
clinical applications.
Intended Audience
This independent learning activity is intended for use by perioperative nurses, certified
surgical technologists, and other healthcare professionals who are interested learning more
about the importance of selecting and using facial protection devices appropriately in the
OR.
3
Credit/Credit Information
State Board Approval for Nurses
Pfiedler Enterprises is a provider approved by the California Board of Registered Nursing,
Provider Number CEP14944, for 2.0 contact hours.
Obtaining full credit for this offering depends upon attendance, regardless of circumstances,
from beginning to end. Licensees must provide their license numbers for record keeping
purposes.
The certificate of course completion issued at the conclusion of this course must be retained
in the participant’s records for at least four (4) years as proof of attendance.
AST Credit
This continuing education activity is approved for 4.5 CE credits by the Association of
Surgical Technologists, Inc., for continuing education for the Certified Surgical Technologists
and Certified Surgical First Assistant. This recognition does not imply that AST approves or
endorses any product or products that are discussed or mentioned in enduring material.
IACET
Pfiedler Enterprises has been accredited as an Authorized Provider by the International
Association for Continuing Education and Training (IACET).
CEU Statements
• As an IACET Authorized Provider, Pfiedler Enterprises offers CEUs for its programs
that qualify under the ANSI/IACET Standard.
• Pfiedler Enterprises is authorized by IACET to offer 0.2 CEUs for this program.
RELEASE AND EXPIRATION DATE
This continuing education activity was planned and provided in accordance with accreditation
criteria. This material was originally produced in June 2014 and can no longer be used after
June 2016 without being updated; therefore, this continuing education activity expires in June
2016.
DISCLAIMER
Accredited status as a provider refers only to continuing nursing education activities and does
not imply endorsement of any products.
SUPPORT
Grant funds for the development of this activity were provided by Cardinal Health.
4
Author/Planning Committee/Reviewer
Rose Moss, RN, MN, CNOR
Nurse Consultant/Author
Moss Enterprises
Elizabeth, CO
Judith Pfister, RN, BSN, MBA
Program Manager/Planning Committee
Pfiedler Enterprises
Aurora, CO
Penny Austin, CSTAurora, CO
Surgical Technologist/Planning Committee/Reviewer
Medical Center of Aurora
Julia A. Kneedler, RN, MS, EdD
Program Manager/Reviewer
Pfiedler Enterprises
Aurora, CO
DISCLOSURE OF RELATIONSHIPS WITH COMMERCIAL ENTITIES FOR
THOSE IN A POSITION TO CONTROL CONTENT FOR THIS ACTIVITY
Pfiedler Enterprises has a policy in place for identifying and resolving conflicts of interest for
individuals who control content for an educational activity. Information below is provided to
the learner, so that a determination can be made if identified external interests or influences
pose potential bias in content, recommendations or conclusions. The intent is full disclosure
of those in a position to control content, with a goal of objectivity, balance and scientific rigor
in the activity. For additional information regarding Pfiedler Enterprises’ disclosure process,
visit our website at: http://www. pfiedlerenterprises.com/disclosure
Disclosure includes relevant financial relationships with commercial interests related to the
subject matter that may be presented in this continuing education activity. “Relevant financial
relationships” are those in any amount, occurring within the past 12 months that create a
conflict of interest. A commercial interest is any entity producing, marketing, reselling, or
distributing health care goods or services consumed by, or used on, patients.
Author/ Planning Committee/Reviewer
Julia A Kneedler, RN, MS, EdD
Co-owner of company that receives grant funds from commercial entities
Judith Pfister, RN, BSN
Co-owner of company that receives grant funds from commercial entities
Rose Moss, RN, MN, CNOR
No conflicts of interest
Penny Austin, CST
No conflicts of interest
5
Privacy and Confidentiality Policy
Pfiedler Enterprises is committed to protecting your privacy and following industry best
practices and regulations regarding continuing education. The information we collect
is never shared with other organizations for commercial purposes. Our privacy and
confidentiality policy covers the site www.pfiedlerenterprises.com and is effective on
March 27, 2008.
To directly access more information on our Privacy and Confidentiality Policy, type
the following URL address into your browser: http://www.pfiedlerenterprises.com/
Privacypolicy.pdf or View the Privacy and Confidentiality Policy using the following link:
http://www.pfiedlerenterprises.com/online_courses.htm
In addition to this privacy statement, this Website is compliant with the guidelines for
internet-based continuing education programs.
The privacy policy of this Website is strictly enforced.
CONTACT INFORMATION
If site users have any questions or suggestions regarding our privacy policy, please
contact us at:
Phone: 720-748-6144
Email:
registrar@pfiedlerenterprises.com
Postal Address: 2101 S. Blackhawk Street, Suite 220
Aurora, Colorado 80014
Website URL:
http://www.pfiedlerenterprises.com
6
Introduction1,2,3
Perioperative personnel are well aware of the value of wearing masks and other types
of facial protection devices during operative procedures. Originally, surgical face masks
were developed to contain and filter droplets of microorganisms expelled from the mouth
and nasopharynx during talking, sneezing, and coughing. This practice promotes a high
level of cleanliness and hygiene within the operating room (OR), thereby protecting the
patient by providing the best possible environment for surgical intervention. In recent
decades, with the increasing awareness and prevalence of epidemiologically significant
diseases, such as hepatitis B, acquired immunodeficiency syndrome (AIDS), a variety of
types of influenza A viruses (e.g., A [H1N1], A [H3N2]), one or two influenza B viruses,
and the recognition of the hazards of surgical smoke, face masks and other respiratory
protection devices are now being worn to protect the health care worker as well as the
patient. Ultimately, when the appropriate products are combined with education and
the implementation of effective workplace strategies, facial protection devices serve to
protect perioperative personnel in all surgical practice settings.
Hazards in the OR: The Danger is Real
Before reviewing the various types of facial protection devices available today, it is first
helpful to examine the dangers present in the perioperative practice setting, which,
by its nature, places staff members at higher risk for exposure to potentially harmful
and infectious substances. Some of the hazards unique to the OR environment which
increase the risk for exposure incidents include:
• Airborne particles (generated by the use of powered surgical equipment such as
saws and/or drills);
• Gases and vapors (e.g., waste anesthetic gases, use of certain materials such as
bone cement); • Smoke/plume (generated during the use of electrosurgery, lasers, and ultrasonic
devices); and
• Large particle droplets from infected patients or health care workers during:
Coughing.
Sneezing.
Talking.
Therapeutic manipulations.
Potential Hazards Transmitted via Blood and Respiratory Routes 4,5,6,7
In the perioperative practice setting, employees are exposed to potentially hazardous
substances on a daily basis. During the 1980s, health care workers became concerned
about the risk of occupational exposure to the human immunodeficiency virus (HIV)
after its transmission was first reported in the literature. Other pathogens which were
identified as significant included hepatitis B (HBV) and hepatitis C (HCV). In 1991, the
Occupational Safety and Health Administration (OSHA) issued its Bloodborne Pathogens
7
Standard, with the intent to help protect workers from occupation exposure to blood and
other potentially infectious material (OPIM). In 2003, the transmission of severe acute
respiratory syndrome-associated Coronavirus (SARS-CoV), a variant of the Coronavirus,
in emergency departments by patients and family members during the SARS outbreaks,
highlighted the need for vigilance, as well as new strategies, to contain respiratory
diseases. Other organisms of interest today include:
• Multidrug resistant organisms (MDROs):
o Bacteria with extended-spectrum betalactamase resistance.
oMethicillin-resistant Staphylococcus aureus (MRSA).
oVancomycin-resistant enterococci (VRE).
oVancomycin-intermediate Staphylococcus aureus.
oVancomycin-resistant Staphylococcus aureus.
• Clostridium difficile (C.diff).
• Crutzfeldt-Jakob disease (CJD).
• Avian flu.
• Norovirus.
Most recently, the Middle East Respiratory Syndrome (MERS) has been identified as an
emerging threat in the U.S. This viral respiratory illness, which was first reported in 2012
in Saudi Arabia, is caused by the coronavirus MERS-CoV. The majority of people with
confirmed MERS-CoV infection have developed severe, acute respiratory illness with a
cough, fever, and shortness of breath. Moreover, approximately 30% of those confirmed
to have MERS-CoV infection have died. In the U.S., two cases were identified in early
May 2014; both cases involved travelers who came from Saudi Arabia, but are not linked.
On May 16, 2014, an Illinois resident who had contact with the first case of MERS in the
U.S. tested positive for MERS-CoV. Standard Precautions, previously known as Universal Precautions, have become the
primary tool for reducing disease transmission from patients to health care workers. Standard Precautions are based on the principle that all blood, body fluids, secretions,
and excretions may contain transmissible infectious agents. These precautions apply in
any health care practice setting and to all patients, regardless of suspected or confirmed
infection status. More recently, the strategy to contain respiratory diseases has been
termed “Respiratory Etiquette” and should be incorporated into infection control practices
a new component of Standard Precautions. One key element of Standard Precautions
is the use of appropriate personal protective equipment, which includes the use of facial
protection devices, and will be explored throughout this study guide.
Surgical Smoke 8,9
In addition to the potential health risks posed by blood, other body fluids, and respiratory
diseases, the dangers of surgical smoke have also become a recognized health hazard
8
for perioperative personnel. Surgical smoke, which is both seen and smelled, results
from the interaction of tissue and mechanical tools or heat-producing equipment that are
used for hemostasis and/or tissue dissection, such as electrosurgery, lasers, ultrasonic
devices, and powered surgical instruments. Smoke is also generated by mixing
chemicals in the OR, such as methyl methacrylate bone cement.
Surgical smoke is composed of 95% water or steam and 5% cellular debris in the form
of particulate matter. This particulate matter contains chemicals, blood and tissue
particles, viruses, and bacteria. The smoke and aerosol are potential vehicles for the
transmissions of infectious agents. Since the mid-1970s, there is a growing body of
evidence documenting the hazardous components of surgical smoke. The gaseous
component of smoke generated by electrosurgery units (ESU) produces the noxious
odor. This smoke also can contain chemical by-products similar to other smoke plumes
(e.g., cigarette smoke), including benzene, carbon monoxide, formaldehyde, hydrogen
cyanide, methane, phenol, styrene, and toluene (see Table 1 for a listing of the chemical
contents of surgical smoke). These by-products also are known to have mutagenic
potential and to be carcinogenic. Surgical smoke has been found to contain toxic gases
and vapors, as well as bioaerosols and viruses; in high concentrations, it can cause
adverse health conditions (see Table 2).
Particle size and the number of particles are also important factors in surgical smoke.
The mass median aerodynamic diameter of the particles contained in surgical smoke
and aerosol is 0.31 microns (µm), with a range of 0.10 to 0.80µm. This is also the most
dangerous particle size, because it is the optimal size to be deposited in the lower
respiratory tract. The sizes of some of the most significant human pathogens are as
follows:
• Hepatitis B virus: 0.042 µm
• Human Immunodeficiency Virus: 0.180 µm
• Human Papilloma Virus: 0.045 µm
• Mycobacterium Tuberculosis: 0.500 µm
• Fungal Spores: 2 - 5 µm
• Viruses: .02 - .30 µm
The actual numbers of particles present in surgical smoke and aerosol can vary
depending on the type of surgery and its duration, but generally range from 1,000,000 to
1,000,000,000 particles.
The distribution of airborne particles associated with surgical smoke is an important
consideration in respiratory protection from surgical smoke. Due to the required air
exchanges in the OR, smoke is evenly distributed throughout the room; smoke particles
travel at about 40 mph. Further, with electrosurgery use, the concentration rises from
60,000 particles per cubic feet to over 1 million within five minutes of ESU activation; it
takes 20 minutes after electrosurgery is used to return to normal.
9
Table 1 - Chemical Contents of Surgical Smoke*
Acetonitrile
Acetylene
Acroloin
Acrylonitrile
Alkyl benzene
Benzaldehyde
Benzene
Benzonitrile
Butadiene
Butene
3-Butenenitrile
Carbon dioxide
Creosol
1-Decene
2,3-Dihydro indene
Ethane
Ethyl benzene
Ethylene
Formaldehyde
Furfural
Hexadecanoic acid
Hydrogen cyanide
Indole
Methane
2-Methyl butenal
6-Methyl indole
4-Methly phenol
2-Methyl propanol
Methyl pyrazine
Phenol
Propene
2-Propylene nitrile
Pyridine
Pyrrole
Styrene
Toluene
1-Undecene
Xylene
* Barrett, W.L. & Garber, S.M. Surgical smoke – a review of the literature. Business Briefing:
Global Surgery. 2004: 1-7.
Table 2 - Risks of Surgical Smoke*
Acute and chronic inflammatory respiratory changes (i.e., asthma, chronic bronchitis, emphysema)
Anemia
Anxiety
Carcinoma
Cardiovascular dysfunction
Colic
Dermatitis
Eye irritation
Headache
Hepatitis
HIV
Hypoxia or dizziness
Lacrimation
Leukemia
Lightheadedness
Nasopharyngeal lesions
Nausea or vomiting
Sneezing
Throat irritation
Weakness
* Alp, E., Bijl, D., Bleichrodt, R.P., Hansson, A., Voss, A. Surgical smoke and infection control. J
Hosp Infect. 2006;62(1): 1-5.
10
Types and Components of Facial Protection Devices10,11,12
Overview
In order to understand how facial protection devices protect healthcare workers in the OR
from blood, body fluids, and aerosols released into the atmosphere, it is first helpful to
review the various types of devices available today. As noted, facial protection is intended
to protect both the patient (from the sneeze or cough respiratory droplets of health
care workers – see Figure 1) and the health care worker from exposure to blood, other
potentially infectious material, and airborne contaminants (by removing them from the air
before they are inhaled).
Figure 1 – Respiratory Droplets
Types of Facial Protection Devices
A facial protection device is a loose-fitting, disposable device that creates a physical
barrier between the mouth and nose of the wearer and potential infectious contaminants
in the immediate environment. These devices are constructed in various thicknesses
and with different abilities to protect the wearer from contact with liquids and in some
cases, airborne particulates. These properties may also affect how easily the wearer can
breathe through the face mask and also how well the face mask protects the wearer. The design and construction of facial protection devices will be reviewed later in this
study guide.
Today, because facial protection devices are used in a wide range of hospital and health
care settings and are intended for various applications and levels of protection, there
are a number of options available. In general, there are three basic categories of facial
protection devices, based upon their intended use and their donning mechanism: flat
masks, specialty masks, and N95 respirators. These devices are described below and
summarized in Table 3.
• Flat masks are defined as either procedure or surgical masks (see Figure 2).
oThese masks are frequently made with three layers of material.
oProcedure masks are used when non-invasive procedures are performed on
11
patient floors. It is held in place by earloops rather than surgical ties, which
means it can be donned quickly. However, some find that this mask to be
uncomfortable (too tight) or find it difficult to obtain a tight seal on the sides
of the face.
o Surgical masks are worn in the OR and in other clinical areas where
invasive procedures are performed. These masks have ties instead of
earloops, which provide a better fit and level of protection through face seal. Figure 2 – Flat Masks
Ear loops Ties
• Specialty masks are high-filtration masks designed for specific surgical
procedures, such as procedures involving the use of lasers and electrosurgical
devices (during which smoke plume is generated) and other procedures using
powered equipment that generate airborne particulates (see Figure 3). These
masks are constructed with an advanced filter that blocks plume particles as
small as 0.1 micron. Surgical masks may not filter chemical contaminants,
therefore OR personnel should consult the facility’s policy to ensure they are
using the correct mask for the procedure. Fluid resistant masks can also be
categorized as specialty masks. Another type of specialty mask is the cone mask
(see Figure 4). This type of mask is often selected, as it is economical, fluid
resistant, easy to don (with an elastic, adjustable head strap and nosepiece) and
is often perceived to be more comfortable than a typical flat mask. Figure 3 – High Filtration Mask
12
Figure 4 – Cone Mask
• An N95 respirator is a respiratory protective device designed to achieve a
very close facial fit that forms a seal that provides a physical barrier to block
splashes, sprays, and large droplets. Additionally, an N95 respirator is designed
to prevent the wearer from breathing in very small airborne particles (0.3 microns
or larger in diameter) that cause infectious diseases (e.g., microorganisms that
cause tuberculosis [TB], SARS, and avian flu). The ‘N95’ designation means
that the respirator blocks at least 95% of these small particles. In order to work
properly, an N95 respirator requires a proper fit. To determine the proper fit, the
wearer should don the respirator and adjust the strap(s) so that it fits tightly, but
comfortably to the face (see Figure 5). If properly fitted, the filtration capabilities
of N95 respirators exceed those of face masks. However, even a properly
fitted N95 respirator does not completely eliminate the risk of illness or death.
OSHA requires that all N95 respirators are certified by the National Institute for
Occupational Safety and Health (NIOSH). Figure 5 – N95 Respirators
One-strap Two-strap
13
Table 3 – Categories/Applications of Facial Protection Devices
Categories / Type(s) of Facial
Protection Device
Flat Masks
► Procedure Masks
►
Surgical Masks
Specialty Masks
► High-filtration Flat
Masks
► Cone Masks
N95 Respirators
Donning Mechanism
►
Earloops
►
Ties (vertical or
horizontal)
►
Applications
►
Noninvasive procedures in
any general clinical setting
► Surgical procedures in the
OR; invasive procedures
in other areas
Ties (vertical or
horizontal)
► Elastic head
strap
►
►
► Procedures
Straps (single
or double)
Components of Facial Protection Devices
Procedures using laser,
electrosurgery, and/
or powered surgical
equipment where
protection against airborne
particulates is needed
during which
very small airborne
particles (0.3 microns or
larger) are generated in
patients known to have
an infectious airbornetransmitted disease
Facial protection devices are constructed of various materials (see Table 4) in four
multiple layers: inner; middle (filtering – which is designed to trap particulate matter
away from the wearer’s face - and non-filtering); and outer. The types of fabrics used in
facial protection devices typically include polypropylene, either spunbonded, meltblown,
or wetlaid; and other materials such as metals, for example, used in nose features;
colorants; elastic materials, e.g., used in devices with ear loops; foam and other anti-fog
materials; and face shield materials. While two surgical masks may be generally similar
in their construction, for example, each consisting of four layers of material, the same
type of donning mechanism, and a nose wire, they may be distinctly different in their
feel and performance. Facial protection devices are generally composed of nonwoven
fabrics, which are engineered materials that are bonded together by mechanical, thermal,
or chemical means. Nonwoven fabrics are made directly from natural or plastic fibers
or plastic film. Nonwoven fabrics have both single use and multiple use applications, all
face masks, with the exception of N95 respirators, are intended for single use only.
14
Table 4 – Materials Used in the Manufacture of Facial Protection Devices
Inner Layer
►Cellulose
►Spunbond
polypropylene
►Tissue
►Carded polyester
Middle Layer
(Filtering)
Middle Layer
(Non-Filtering)
►Meltblown
►Film
►SMS
(polypropylene)
►Other non-woven
(polypropylene)
►Other non-woven
►Cellulose
►SMS
polypropylene
Outer Layer
(polypropylene)
►Spunbound
polypropylene
►Tissue
Regulation and Testing of Facial Protection Devices13,14
The U.S. Food and Drug Administration (FDA)15,16
The FDA is the U.S. government agency that oversees most medical
products; within FDA, the Center for Devices and Radiological Health
(CDRH) oversees the safety and effectiveness of medical devices.
Personal protective equipment (PPE) that is intended for use in
preventing or treating disease (including surgical masks and N95
respirators) is subject to regulation under the device provisions of the
Federal Food, Drug, and Cosmetic Act. Surgical face masks and N95
NIOSH certified respirators are considered a Class II Medical Devices.
Before these devices can be sold in the U.S., the FDA evaluates the
manufacturer’s new product applications (i.e., premarket notifications
or 510[k]s) to ensure that the new devices are similar to (substantially
equivalent to) existing products already on the market. The FDA refers
to this as clearing the products for market. Once the FDA has cleared
the products, it:
• Maintains databases of those products and their manufacturers;
• Ensures that manufacturers use reliable methods for manufacturing and
packaging the products (e.g., Good Manufacturing Practices); and
• Reviews and analyzes reports concerning problems with medical devices.
If the FDA finds ongoing problems with a medical product, it may oversee a
manufacturer›s recall, recommend changes to the labeling or instructions, or
propose corrective actions.
The FDA recommends that manufacturers demonstrate surgical mask performance in
four areas: fluid resistance, filtration efficiency, differential pressure, and flammability. These will be discussed in greater detail later in this study guide. The FDA requires no
minimum level of filter performance.
Occupational Safety and Health Administration (OSHA)17,18
The U.S. Department of Labor’s Occupational Safety and Health Administration’s
Bloodborne Pathogens Standard requires employers to provide appropriate PPE for
workers who could be exposed to blood or other infectious materials (i.e., bloodborne
15
pathogens). OSHA may also require employers to provide PPE to protect against other
hazards at work. Although OSHA requires the use of specific equipment, it does not
regulate the marketing of these devices, nor does it grant claims of disease prevention.
In its Respiratory Protection Standard, OSHA regulates the selection and use of
respirators in a workplace. Facilities are required to have a respirator program that
includes individual medical evaluation, training, and fit testing. OSHA has designated
assigned protection factors that indicate to employers how well respirators in a particular
class will reduce exposure to airborne contaminants. A fit test is then used to evaluate
the fit of a respirator on an individual. The OSHA standards will be discussed in greater
detail later in this study guide.
The National Institute for Occupational Safety and Health (NIOSH)19
The National Institute for Occupational Safety and Health (NIOSH) is a federal agency
and branch of the Department of Health and Human Services (DHHS) whose function is
to identify substances that pose potential health problems and recommends exposure
limits to OSHA. NIOSH conducts in-depth research on safety and health issues, provides
technical assistance, and recommends standards for adoption by OSHA. NIOSH
also performs testing and certification of respiratory protection equipment through its
established certification requirements for various types of respiratory PPE. The NIOSH
tests filters for the effects of loading (particle burden), temperature, and relative humidity
and requires a minimum filtration efficiency of 95%, 99%, or 99.97%. Certification tests
also evaluate effects of oil aerosols for filter designations of N (not resistant to oil), R
(somewhat resistant to oil), and P (strongly resistant - oil proof). NIOSH also evaluates
the fit performance of some respiratory protective devices using human panels with
specified facial dimensions. Certification of filtering face-piece respirators, however, does
not currently include an assessment of fit performance. NIOSH issues a certification for
products that comply with these regulations. However, NIOSH certification evaluates
the performance of respiratory protection equipment in functional terms and not in terms
of claims for use in preventing disease. While NIOSH certification is not required for
a non-medical respirator to be sold, employers subject to OSHA regulation may be
required to provide NIOSH-certified respiratory protection equipment to satisfy the OSHA
requirements. N95 respirators cleared by FDA for use in the healthcare setting are called
surgical N95 respirators. These devices meet some of the same performance standards
as surgical face masks and are also NIOSH certified to meet the N95 respirator
performance requirements.
The shared regulatory approach of NIOSH and OSHA to respiratory protection
recognizes the two most important aspects of respiratory protection: providing known
filtration efficiency while also ensuring the proper use and selection of devices, which
includes initial and ongoing individual fit.
16
Performance Characteristics of Facial Protection
Devices20
As noted, the FDA recommends that manufacturers demonstrate the performance of
surgical masks in four areas: fluid resistance, filtration efficiency, differential pressure,
and flammability. These parameters and the corresponding tests are described below.
Fluid Resistance
Fluid or splash resistance is the ability of the mask’s material to resist the penetration of
blood and body fluids; it tests the mask’s material construction for the ability to minimize
fluids from traveling through the material and potentially coming into contact with the
wearer. The recognized test for fluid resistance is ASTM F1862 Standard Test Method
for Resistance of Medical Face Masks to Penetration by Synthetic Blood.21 This test
method is used to evaluate the resistance of face masks to penetration by a fixed volume
of blood at high velocity over a relatively short period of time (0 to 2.5 seconds). The
test results are intended to enable end-users to objectively compare the performance
of different masks. According to ASTM F 1862, surgical masks are tested on a pass/fail
basis at three velocities corresponding to the range of human blood pressure (i.e., 80,
120, 160 mm Hg). Fluid resistance may be claimed if the device passes ASTM F1862
at any of the three pressures. Any visual evidence of synthetic blood penetration to
the inside of the face mask constitutes failure. At least 29 of 32 samples must pass the
test for the mask to pass at the given blood pressure. Surgical masks that demonstrate
passing results at higher velocities are more fluid resistant, however, labeling is not
required to specify the pressure at which it passed, meaning there is no way for the HCW
to know the specific level of fluid resistance unless the information is requested. It is important to note that all face masks which are labeled as fluid-resistant do not
provide the same level of protection. Additionally, one manufacturer may label a
mask that passed ASTM F1862 at 80mm Hg as “highly fluid resistant,” while another
manufacturer may label a mask that passed at 160mm Hg as “fluid resistant.” In this
scenario, the user would naturally believe that the mask labeled “highly fluid resistant”
provides more protection than the one labeled only “fluid resistant,” when in fact, the
opposite is true.
Filtration Efficiency
For surgical masks that are not NIOSH certified N95 Respirators, the FDA recommends
evaluation of bacterial filtration efficiency through the use of the following test:
• Particulate Filtration Efficiency (PFE): This method tests the ability of face
masks to filter sub-micron particles, generally 0.1µm (0.1 micron) in size. The
ASTM F1215 Standard Test Method for Determining the Initial Efficiency of
Flatsheet Filter Medium in an Airflow Using Spheres uses an unneutralized
aerosol of 0.1-micrometer latex spheres at a challenge velocity between 0.5 cm/
second and 25 cm/second (i.e., approximately 8 L/min to 380 L/min for a 9-cm
mask).22 A PFE test result of 99%, means that the mask has successfully filtered
99% of all particles of 0.1µm size or greater.
17
• Bacterial Filtration Efficiency (BFE): This is a measure of the ability of the
mask’s material to prevent the passage of aerosolized bacteria. BFE is expressed
in the percentage of a known quantity that does not pass through the mask
material at a given aerosol flow rate. The ASTM F2101-07 Standard Test Method
for Evaluating the Bacterial Filtration Efficiency (BFE) of surgical masks using a
Biological Aerosol of Staphylococcus aureus is often used.23 This test uses an
unneutralized 3± 0.3-micrometer Staphylococcus aureus aerosol at a flow rate of
28.3 L/minute.
Breathability
For surgical masks that are not NIOSH certified N95 Respirators, the FDA recommends
evaluation of differential pressure. Differential Pressure (Delta-P) is the measured
pressure drop (measured in mm H20/cm²) across a surgical face mask material, which
determines the resistance of the surgical face mask to air flowing through the mask.24
The pressure drop relates to the breathability and comfort of the surgical mask. Test
results are reported on a scale of 1 to 5; in general, a lower Delta-P translates to
increased breathability (see Table 5). ASTM requires that general use masks have Delta
P value of less than 4.0; fluid resistant masks must have Delta P values of less than 5.0.
Table 5 - Comfort Scale Used in Delta-P Testing
Score
Wearer’s Perception
Above 5.0
Hot
4.0 to 5.0
Very warm
3.0 to 4.0
Warm
2.0 to 3.0
Cool
1.0 to 2.0
Very cool
Flammability
Flammability is defined as the relative ease with which a material can ignite and sustain
combustion; it is determined by igniting the material and testing the time of flame spread.
The FDA recommends one of the three standards below to determine flammability by
class:
• CPSC CS-191-53 Flammability Test Method (16 CFR 1610) Standard for
Flammability of Clothing Textiles.25 The standard provides a test to determine
whether such clothing and fabrics exhibit ‘‘rapid and intense burning,’’ and are
therefore highly flammable. To determine the appropriate classification, the
Standard prescribes the method of testing. The classifications are defined as
follows:
oClass 1 – Normal Flammability. Class I textiles exhibit normal flammability;
the burn time is 3.5 seconds or more).
oClass 2 – Intermediate Flammability. Class 2 fabrics have a burn time from 4
through 7 seconds.
18
oClass 3 – Rapid and Intense Burning. . Class 3 textiles exhibit rapid and
intense burning (burn time is less than 3.5 seconds) are dangerously
flammable.
• National Fire Protection Association NFPA Standard 702-1980: Standard for
Classification of Flammability of Wearing Apparel.26 In 1987, the NFPA removed
this from their list of current standards, but it is still used as a reference by
manufacturers and the FDA as one of the standards to be used for evaluating the
safety and performance characteristics of facial protection devices.
• Underwriters Laboratories (UL) 2154 Standard for Fire Tests of Surgical Fabrics.27
This is a test that measures the level of atmospheric oxygen required to
propagate flame when ignition is caused by an electrosurgery unit or laser. Higher
levels of oxygen required for flame propagation indicate materials which are more
flame resistant for electrosurgery or laser procedures.
The ASTM requires all face masks to meet or exceed Class 1 flammability. The FDA
recommends that only Class 1 and Class 2 flammability materials be used in surgical
masks intended for use in the operating room. Class 3 surgical masks should have a
flammability warning on their label.
Material Performance
The ASTM F2100-11 Standard Specification for Performance of Materials used in Medical
Face Masks28 covers testing and requirements for materials used in the construction of
medical face masks. Medical face mask material performance is based on the testing
described above, i.e., resistance to penetration by synthetic blood, particulate filtration
efficiency, bacterial filtration efficiency, differential pressure, and flammability. With the
recent revisions to this standard, the following barrier levels can now be applied to face
masks to indicate protection levels based on the barrier performance properties of the
materials used (see Table 6):
oLevel 1 Barrier face mask materials are evaluated for their ability to capture
sub-micron particles, their resistance to synthetic blood penetration at
the minimum velocity (as specified in ASTM F1862), bacterial filtration
efficiency, and differential pressure.
oLevel 2 Barrier face mask materials are tested for their ability to capture
sub-micron particles and are also evaluated for resistance to synthetic blood
penetration at the middle velocity (as specified in ASTM F1862), bacterial
filtration efficiency, and differential pressure.
oLevel 3 Barrier face mask materials are tested for their resistance to
synthetic blood penetration at the maximum velocity (as specified in ASTM
F1862), sub-micron particulate filtration, bacterial filtration efficiency, and
differential pressure.
This revised ASTM standard also states that the primary packaging containing the face
masks must include a graphic representation that prominently and clearly indicates the
19
performance level met (ie, Level 1, 2, or 3, as outlined in Table 6). This new labeling
not only simplifies the mask selection process, but also helps to ensure that health care
workers select the appropriate mask for the task.29
Other elements of performance related to facial protection device design and materials
are outlined in Table 7.
Table 6 – Medical Face Mask Material Requirements by Performance Class
Characteristic
Level 1 Barrier
Level 2 Barrier
Level 3 Barrier
Resistance to Penetration by
Synthetic Blood
(minimum pressure in mmHg for
passing result)
80
120
160
≥ 95 %
≥ 98 %
≥ 98 %
≥ 95 %
≥ 98 %
≥ 98 %
< 4.0
< 5.0
< 5.0
Class 1
Class 1
Class 1
Sub-micron Particulate
Filtration Efficiency at 0.1
micron (%)
Bacterial Filtration Efficiency
(%)
Differential Pressure
(mm H2O/cm²)
Flame Spread
Table 7 – Facial Protection Devices: Elements of Performance
Feature
Filtration
Fit
Speech
Purpose
Function of
Allow permeation of air
during inhaling/exhaling.
Prevent respiratory
distress i.e. Low work of
breathing.
Prevent penetration of
particles, bio-aerosols,
smoke, plume.
Stay sealed during usual
physical maneuvers of
head and neck.
Allow coherent
communication.
20
Mask material
Priority
High
High
High
Mask design
High
Mask design and
material
Low
Clinical Considerations: Regulations and
Recommendations Regarding Appropriate Selection and
Use of Facial Protection Devices
In addition to the regulations outlined for the design and manufacture of facial protection
devices, various regulatory agencies and professional associations have outlined
standards, guidelines, and recommended practices for their effective and appropriate
use, as outlined below.
OSHA
Bloodborne Pathogens Standard30
As noted, the OSHA Bloodborne Pathogens Standard outlines the required use of
facial protection when there is a reasonable likelihood of occupational exposure to
blood or body fluids. In these situations, the employer shall provide, at no cost to the
employee, appropriate personal protective equipment such as, but not limited to, gloves,
gowns, laboratory coats, face shields or masks and eye protection, and mouthpieces,
resuscitation bags, pocket masks, or other ventilation devices. Personal protective
equipment will be considered “appropriate” only if it does not permit blood or other
potentially infectious materials to pass through to or reach the employee’s work clothes,
street clothes, undergarments, skin, eyes, mouth, or other mucous membranes under
normal conditions of use and for the duration of time which the protective equipment will
be used. Masks, in combination with eye protection devices, such as goggles or glasses
with solid side shields, or chin-length face shields, shall be worn whenever splashes,
spray, spatter, or droplets of blood or other potentially infectious materials may be
generated and eye, nose, or mouth contamination can be reasonably anticipated.
Respiratory Protection Standard31
Surgical masks are not a substitute for respirators because they are not designed
to prevent inhalation of airborne contaminants. However, bacteria and viruses are
particles that can be filtered by particulate respirators such as N95 respirators. OSHA’s
Respiratory Protection Standard requires the use of a NIOSH certified respirator, as well
as the implementation of a comprehensive respiratory protection program. This standard
also outlines three measures that must be taken before a health care worker uses a
respirator:
• Employees must be medically evaluated and approved to wear a respirator. Medical evaluations can be performed by using a medical questionnaire or by
performing an initial medical evaluation that obtains the same information as
the medical questionnaire. This evaluation must be conducted during normal
working hours or at a time that is convenient to the employee and employers are
responsible for paying for the service.
• The employee must be fit tested to ensure that the respirator is working
effectively. OSHA requires that N95 respirators be fit-tested either quantitatively
or qualitatively to ensure that every worker is provided with the correct size and
type of respirator.
21
o Quantitative fit testing – this test involves two measurements:
▪▪ Aerosolized particles inside the respirator (using a sampling probe);
and
▪▪ Air leakage into the respirator.
These two measurements are taken while the individual is wearing the respirator, and
is performing various test exercises, e.g., normal breathing, deep breathing, turning
the head, moving the head up and down. The result of this testing is a numerical “fit
factor, “which is based on the ratio of the concentration of the aerosolized particles in
the ambient air to the concentration of the aerosolized particles inside the respirator
while it is being worn. Regardless of the numerical result of the testing, the wearer is still
questioned about the comfort of the respirator. If the individual considers the respirator
unacceptable, the testing must be repeated using another type of N95 respirator.
oQualitative fit testing – this is a pass/fail test in which, first the worker
subjectively assesses the comfort of the respirator using the following
criteria:
▪▪
▪▪
▪▪
▪▪
▪▪
▪▪
▪▪
▪▪
Position of the mask on the nose.
Room for eye protection.
Room to talk.
Position of the mask on the face and cheeks.
Proper placement of the chin.
Adequate strap tension, but not overly tight.
Fit across the bridge of the nose.
Respirator of proper size to span the distance from the nose to the
chin.
▪▪ Tendency of the respirator to slip.
▪▪ Self-observation in a mirror to evaluate fit and respirator protection.
The individual, while wearing the mask and a hood, is then asked to detect odors and
tastes associated with selected aerosolized test solutions. If the worker is able to smell
or taste the test aerosols while wearing the respirator, of if he/she finds the fit of the
respirator unacceptable, then the fit testing must be repeated with a different respirator.
This test is referred to as an individual’s fit factor, which must be equal to or greater than
the assigned protection factor multiplied by a safety factor. In the case of a filtering face
piece respirator, an individual’s fit factor must be greater than 100 (assigned protection
factor = 10; safety factor = 10).
• The employee must be trained to use the respirator.
22
Pandemic Influenza Preparedness and Response
Guidance for Healthcare Workers and Healthcare
Employers32
In 2009, OSHA published its Pandemic Influenza Preparedness and Response Guidance
for Healthcare Workers and Healthcare Employers, recognizing that seasonal, avian,
and pandemic influenza can occur in humans; therefore, it is important to have a basic
understanding of these terms as well as the appropriate prevention strategies. The
General Duty Clause requires employers to provide their employees with a workplace
free from recognized hazards that are likely to cause death or serious physical harm. A successful infection control program for pandemic influenza is comprised of the same
strategies that are implemented for any infectious agent; these include engineering (ie,
facility and environmental) controls; administrative controls (e.g., standard operating
procedures; personal protective clothing and equipment; and safe work practices. These
strategies form the basis of standard precautions and transmission-based precautions.
Because the exact transmission pattern or patterns are not known until after a pandemic
influenza virus emerges, transmission-based infection control strategies may have to be
modified to include additional engineering controls, administrative controls, PPE, and/or
safe work practices. Special Considerations for Pandemic Preparedness
Respiratory protection against pandemic influenza will be more effective when employers
are prepared appropriately. The establishment of a comprehensive respiratory protection
program with all of the elements specified in OSHA’s Respiratory Protection standard
is necessary to achieve the highest levels of protection. Acquiring an adequate supply
of the appropriate respirators, ensuring that they properly fit key personnel, conducting
appropriate training, and performing other aspects of respiratory protection can all
be accomplished before an outbreak of pandemic influenza. These measures should
be repeated annually, before a pandemic is declared, in order to assure ongoing
preparedness.
Centers for Disease Control and Prevention (CDC)
The CDC also outlines recommendations for protecting health care workers from
infection, including the use of a surgical mask in health care settings.
Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in
Healthcare Settings, 2007 33
The CDC’s Guideline for Isolation Precaution in Hospitals, originally issued in 1995,
provides recommendations related to mask and respirator use by providing two tiers
of precautions (i.e., standard and transmission-based precautions) to help prevent
transmissions of infections from both recognized and unrecognized sources in hospitals. The three categories of transmission-based precautions are:
• Contact precautions should be used when providing care for patients who are
known or suspected to be infected or colonized with microorganisms that are
23
transmitted by direct or indirect contact with patients or items and surfaces in
patients’ environments (e.g., herpes simplex, impetigo, infectious diarrhea,
smallpox, MRSA, and VRE). Contact precautions include wearing a mask when it
is anticipated that aerosolized exposure to infectious microorganisms is possible. • Droplet precautions should be used when caring for patients who are known
or suspected to be infected with microorganisms that can be transmitted by
infectious large particle droplets (i.e., those larger than 5 microns in size) and
generally travel short distances of three fee or less (e.g., diphtheria, pertussis,
influenza, mumps, pneumonic plague). Droplet precautions include wearing a
mask when within three feet of infectious patients.
• Airborne precautions should be used when caring for patients who are known
or suspected to be infected with microorganisms that can be transmitted by
the airborne route (e.g., rubeola, varicella, tuberculosis [TB], and smallpox). Microorganisms carried by airborne transmission (e.g., droplet nuclei or dust
particles) can be widely dispersed by air currents, remain suspended in the air for
extended periods, and may become inhaled by a susceptible host within the same
room or over a longer distance from the source patient. Airborne precautions
should include NIOSH-approved N95 respirators worn by health care personnel.
This guideline was updated and expanded in 2007, based on the following
developments:
• The transition of healthcare delivery from primarily acute care hospitals to other
healthcare settings (e.g., home care, ambulatory care, free-standing specialty
care sites, long-term care) created a need for recommendations that can be
applied in all healthcare settings using common principles of infection control
practice, yet can be modified to reflect setting-specific needs. Accordingly,
the revised guideline addresses the spectrum of healthcare delivery settings.
Furthermore, the term “nosocomial” infections was replaced by the term
“healthcare-associated” infections (HAIs) to reflect the changing patterns in
healthcare delivery as well as the difficulty in determining the geographic site of
exposure to an infectious agent and/or acquisition of infection.
• The emergence of new pathogens (e.g., SARS-CoV associated with the
severe acute respiratory syndrome [SARS], avian influenza in humans),
renewed concern for evolving known pathogens (e.g., C. diff, noroviruses,
community-associated MRSA [CA-MRSA]), development of new therapies (e.g.,
gene therapy), and increasing concern for the threat of bioweapons attacks,
established a need to address a broader scope of issues than in previous
isolation guidelines.
• The successful experience with Standard Precautions, first recommended in
the 1996 guideline, has led to a reaffirmation of this approach as the foundation
for preventing transmission of infectious agents in all healthcare settings. New
additions to the recommendations for Standard Precautions were the Respiratory
Hygiene/Cough Etiquette and safe injection practices, including the use of a
24
mask when performing certain high-risk, prolonged procedures involving spinal
canal punctures (e.g., myelography, epidural anesthesia). As noted, the need
for a recommendation for Respiratory Hygiene/Cough Etiquette grew out of
observations during the SARS outbreaks where failure to implement simple
source control measures with patients, visitors, and health care workers with
respiratory symptoms may have contributed to SARS-CoV transmission. The
recommended practices have a strong evidence base. The continued occurrence
of outbreaks of hepatitis B and hepatitis C viruses in ambulatory settings indicated
a need to re-iterate safe injection practice recommendations as part of Standard
Precautions. The addition of a mask for certain spinal injections grew from recent
evidence of an associated risk for developing meningitis caused by respiratory
flora.
• Evidence that organizational characteristics (e.g., nurse staffing levels and
composition, establishment of a safety culture) influence healthcare personnel
adherence to recommended infection control practices, and therefore are
important factors in preventing transmission of infectious agents, led to a
new emphasis and recommendations for administrative involvement in the
development and support of infection control programs.
• Continued increase in the incidence of HAIs caused by MDROs in all healthcare
settings and the expanded body of knowledge concerning prevention of
transmission of MDROs created a need for more specific recommendations for
surveillance and control of these pathogens that would be practical and effective
in various types of healthcare settings.
Guidelines for Preventing the Transmission of Mycobacterium tuberculosis
in Health-Care Settings, 2005 34
In 1994, the CDC first published its Guidelines for Preventing the Transmission of
Mycobacterium tuberculosis in Health Care Facilities. These guidelines were issued
in response to a resurgence of TB disease that occurred in the United States in the
mid-1980s and early 1990s, including the documentation of multiple high-profile healthcare--associated (previously called nosocomial) outbreaks related to an increase in
the prevalence of TB disease and HIV coinfection; lapses in infection control practices;
delays in the diagnosis and treatment of persons with infectious TB disease; and the
appearance and transmission of multidrug-resistant TB strains. The guidelines presented
recommendations for TB infection control based on a risk assessment process. In this
process, health-care facilities were classified according to categories of TB risk, with a
corresponding series of environmental and respiratory protection control measures.
In 2005, these guidelines were updated to reflect the evidence-based science that was
used to support its recommendations for the health care environment today. All health
care settings need a TB infection control program designed to ensure prompt detection,
airborne precautions, and treatment of persons who have suspected or confirmed TB
disease (or prompt referral of persons who have suspected TB disease for settings in
which persons with TB disease are not expected to be encountered). Such a program is
based on a three-level hierarchy of controls, described below:
25
• Administrative Controls. The first and most important level of TB controls is the
use of administrative measures to reduce the risk for exposure to persons who
might have TB disease. Administrative controls consist of, but are not limited to,
the following activities:
o Assigning responsibility for TB infection control in the setting;
o Conducting a TB risk assessment of the setting;
o Developing and instituting a written TB infection control plan;
o Ensuring the timely availability of recommended laboratory processing,
testing, and reporting of results to the ordering physician and infection
control team;
oImplementing effective work practices for the management of patients with
suspected or confirmed TB disease; and
oEnsuring proper cleaning and sterilization or disinfection of potentially
contaminated equipment.
• Environmental Controls. The second level of the hierarchy is the use of
environmental controls to prevent the spread and reduce the concentration of
infectious droplet nuclei in ambient air. Primary environmental controls consist of
controlling the source of infection by using local exhaust ventilation (e.g., hoods,
tents, or booths) and diluting and removing contaminated air by using general
ventilation. Secondary environmental controls consist of controlling the airflow to
prevent contamination of air in areas adjacent to the source and cleaning the air
by using high efficiency particulate air (HEPA) filtration.
• Respiratory Protection Controls. The first two control levels minimize the number
of areas in which exposure to M. tuberculosis might occur and, therefore, aim
to minimize the number of persons exposed. These control levels also reduce,
but do not eliminate, the risk for exposure in the limited areas in which exposure
can still occur. Because persons entering these areas might be exposed to M.
tuberculosis, the third level of the hierarchy is the use of respiratory protective
equipment in situations that pose a high risk for exposure. Use of respiratory
protection can further reduce risk for exposure of health care workers to infectious
droplet nuclei that have been expelled into the air from a patient with infectious
TB disease. The following measures can be taken to reduce the risk for exposure:
o Implementing a respiratory protection program;
o Training health care workers on respiratory protection; and
o Training patients on respiratory hygiene and cough etiquette procedures.
Recommendations for Facemask and Respirator Use to Reduce Seasonal
Influenza 35
The CDC recently published Prevention Strategies for Seasonal Influenza in Healthcare
Settings, which supersedes the previous 2009 guidance for both seasonal influenza and
the H1N1 influenza in health care settings since a safe an effective vaccine for the 2009
26
H1N1 virus became available and the overall risk of hospitalization and death among
those infected with this strain is now known to be considerably lower than pre-pandemic
assumptions. Also, recently presented or published information indicates that the use
of a face mask and hand hygiene decrease the risk of influenza infection in health
care, as well as household, settings; therefore, an update of the recommendations was
warranted. In regards to facial protection, the recommendations include:
• For patients or persons with symptoms of any respiratory infection, before and
upon arrival to a health care setting, appropriate prevention actions (eg, wear
a facemask upon entry; adhere to respiratory hygiene, cough etiquette, hand
hygiene; and follow triage procedures) should be taken throughout the duration of
the visit. The patient should wear a facemask, if possible, and follow respiratory
hygiene and cough etiquette and hand hygiene, if he/she must be transported
from his/her room
• Health care workers should adhere to Standard Precautions and Droplet
Precautions. They should don a facemask when entering the room of a patient
with either suspected or confirmed influenza, remove it when leaving the patient’s
room, dispose of it in an appropriate waste container, and then perform hand
hygiene. If a facility chooses to provide its employees with alternative PPE,
this equipment should offer the same nose and mouth protection from splashes
and sprays as that provided by facemasks (eg, face shields, N95 respirators,
or powered air purifying respirators). Health care workers should also wear
respiratory protection that is equivalent to a fitted N95 filtering facepiece respirator
or equivalent N95 respirator (eg, powered air purifying respirator, elastomeric)
when participating in aerosol-generating procedures. When respiratory protection
is needed in a workplace setting, respirators must be used in the context of a
comprehensive respiratory protection program that includes training and fittesting, as mandated in OSHA’s Respiratory Protection standard.
Recommendations for Facemask and Respirator Use to Reduce MERS36
As noted above, the first cases of MERS have been identified in the U.S. Standard,
contact, and airborne precautions are recommended for management of hospitalized
patients with known or suspected MERS-CoV infection, based on CDC’s case definition
for a patient under investigation (PUI). Additional infection prevention precautions may
be needed if a MERS-CoV patient has other conditions or illnesses that require specific
measures (e.g., TB, Clostridium difficile, or multi-drug resistant organisms).
Recommendations for health care workers in regards to facial protection include the
use of respiratory protection that is at least as protective as a fit-tested NIOSH-certified
disposable N95 filtering facepiece respirator. A facemask should be worn in situations
where a respirator is not available; however, respirators should be made available as
quickly as possible. The recommended PPE should be worn by health care workers
upon entry into patient rooms or care areas for any reason (eg, clinical care, specimen,
environmental cleaning, etc.). When leaving the room or care area, PPE should be
removed and either discarded or cleaned and disinfected according to the manufacturer’s
instructions (for reusable PPE); hand hygiene should be performed after PPE is
removed.
27
Patients should be placed in an airborne infection isolation room (AIIR); while pending
placement in the AIIR, the patient should wear a face mask and be placed in a singlepatient room with the door closed. Once the patient is in the AIIR, his/her face mask can
be removed; however, when outside of the AIIR, the patient should wear a face mask to
contain secretions.
The Association of periOperative Registered Nurses (AORN)
AORN addresses facial protection devices in three of its recommended practices, as
outlined below.
• Recommended Practices for Surgical Attire37
o Recommendation VI states that “all individuals entering restricted areas
should were a surgical mask when open sterile supplies and equipment
are present.” The recommendation goes on to say that a single surgical
mask should be worn to protect the health care worker from contact with
infectious materials from the patient and also protect the patient and sterile
field from transmission of respiratory microorganisms expelled by the health
care worker during talking, sneezing and coughing. A mask should fully
cover both the nose and mouth and be secured in a manner that prevents
venting. The practice of using a double mask does not increase filtration;
furthermore, because it creates an impediment to breathing, this practice
is not recommended. Other recommendations include that a fresh, clean
mask should be used for every procedure; masks should not be worn
handing down from the neck; and masks should be removed by the ties and
discarded after each procedure, followed by hand hygiene.
• Recommended Practices for Laser Safety in Perioperative Practice Settings38
o Recommendation V states that “potential hazards associated with surgical
smoke generated in the laser practice setting should be identified and
safe practices established.” Surgical smoke should be removed with
a smoke evacuation system during both open and minimally invasive
procedures; local exhaust ventilation (LEV) is the primary measure to
protect perioperative personnel from exposure to laser-generated airborne
contaminants. In regards to facial protection, the recommendations go on
to state that perioperative personnel should wear respiratory protection
(eg, a fit-tested surgical N95 filtering respirator or high-filtration surgical
masks) in procedures where surgical smoke is generated as secondary
protection against residual smoke that is not captured by LEV. While these
masks are specifically designed to filter particulate matter 0.1 micron or
larger in size, they should not be used as the first line of protection against
inhalation of surgical smoke or as protection from the chemical or particulate
contaminants in surgical smoke. Because both surgical and high-filtration
masks do not seal the face, they may permit dangerous contaminants to
enter the wearer’s breathing zone.
28
• Recommended Practices for Prevention of Transmissible Infections in the
Perioperative Practice Setting39
o Recommendation III states that “droplet precautions should be used
throughout the perioperative environment (ie, preoperative, intraoperative,
postoperative) when providing care to patients who are known or suspected
to be infected with microorganisms that can be transmitted by large
droplets. In addition to Standard Precautions, droplet precautions are used
to reduce the risks associated with pathogens that are spread through close
respiratory or mucous membrane contact. Personal protective equipment
should be worn as a component of droplet precautions; in regards to facial
protection, perioperative personnel should wear a surgical mask when in
close contact with a patient requiring droplet precautions. The patient who
requires droplet precautions should wear a mask when being transported.
• Recommendation IV states that “airborne precautions should be used when
providing care to patients who are known or suspected to be infected with
microorganisms that can be transmitted by the airborne route.” Personal
protective equipment should be worn as a component of airborne precautions;
perioperative personnel should wear a surgical mask or N95 or higher level
respirator, based on disease-specific recommendations, prior to entering the room
of a patient requiring airborne precautions. The respiratory protective devices
used during care of a patient with TB should be NIOSH-certified as a nonpowered
particulate filtering respirator (N-, R-, or P-95, 99, or 100), including a disposable
respirator or powered air-purifying respirator with a high efficiency filter. These
devices should be available in various models and sizes to accommodate the
facial characteristics and sizes of perioperative staff members. During transport, a
patient requiring airborne precautions should wear a mask if clinically appropriate.
The Association for Professionals in Infection Control and Epidemiology (APIC)
APIC outlines recommendations for the use of facial protection devices as follows:40
• Procedure masks should be readily available throughout a health care facility for
use by both health care workers and patients.
• A face mask with a fluid resistance of 160 mm/Hg should be worn for any
procedure during which there is any risk of exposure to body fluids.
• A properly fitted N-95 respirator should be worn when there is a risk of exposure
to tuberculosis. In addition, N-95 respirators should be worn by non-immune
health care workers who will have contact with patients who have rubeola or
varicella; health care personnel who are not immune to these diseases should
also wear N-95 respirators in the vicinity of patients who are known or suspected
to have these infections.
29
Infection Control Today
In 2009 there was a debate within the medical community due to conflicting research
and guidelines between government agencies regarding the transmission of H1N1.
Initially, the Association for Professionals in Infection Control and Epidemiology (APIC)
and the Society for Healthcare Epidemiology of America (SHEA) supported the CDC
recommendations of N95’s; however, due to recent research SHEA supported Standard
surgical masks for routine care of patients with H1N1. In November, 2009, APIC and
SHEA issued a letter to President Obama expressing concern over the current federal
guidance surrounding the use of personal protective equipment (PPE) by healthcare
workers in treating suspected or confirmed cases of 2009 H1N1 influenza. The letter
was precipitated by a re-evaluation of a study in which no significant differences were
observed among healthcare workers wearing surgical masks or N95 respirators. Of
note, this study was initially reported to show a significant benefit associated with the
use of N95 respirators; in addition, this preliminary report was cited in the Institute of
Medicine’s Sept. 3, 2009 Letter Report, which recommended the routine use of N95
respirators. APIC reported that in its letter, it urged the Obama administration to modify
the guidance to reflect the position best supported by the available science – which is
first-line use of surgical masks for routine H1N1 patient care. The letter also requested an
immediate moratorium on OSHA’s requirement for healthcare facilities related to the use
of N95 respirators in relation to H1N1 influenza. It was pointed out that permitting OSHA
to continue to enforce a policy not grounded in science will force healthcare facilities to
waste time and resources while working to comply with this requirement, rather than to
enact measures that will significantly benefit patient care and healthcare worker safety
during this national emergency. Additionally, the letter expressed concern over the
existing shortage of respirators, potentially precluding their use in situations where they
are most needed. The letter detailed the advantages of surgical masks by providing
appropriate protection for all routine patient encounters.41
Facial Protection Devices: Selection and Use Criteria
As discussed throughout this study guide, facial protection devices are worn by health
care personnel to provide protection against the spread of infections by reducing the
passage of bacterial particles from the wearer into the environment. They also protect
the wearer from blood and body fluid splash or spatter and inhaling airborne infectious
agents originating from the patients’ or staffs’ respiratory tract during talking, coughing,
or sneezing. Facial protection devices, which are available in a variety of shapes with
different features, are selected based on the wearer’s protection needs, as well as
personal preference of style and fit. Other selection criteria are described below.
Protection
The level of protection needed should be a primary consideration in the selection and
use of facial protection devices; the appropriate level of protection will vary based on
the clinical application. In some clinical situations, high filtration efficiency might be
important; in other uses, high fluid resistance might be needed. The discussion of the
various types of mask demonstrate how different levels of protection are appropriate
30
for different clinical applications. There are basically three types of procedure masks
– tissue-tissue, polypropylene-polypropylene, and fluid resistant. Tissue-tissue masks
provide minimal protection to the clinician and the patient. It is most often preferred
because it is very lightweight and comfortable. It is appropriate for use when there is NO
risk of splash or other exposure to blood or body fluids; therefore, it is not recommended
for respiratory etiquette protocols. Polypropylene-polypropylene masks are the most
commonly used and offer more protection than tissue-tissue, as some may pass at the
lowest level of fluid resistance; therefore this mask is often preferred for use in respiratory
etiquette protocols. Fluid resistant procedure masks should be worn if there is the risk
of fluid exposure. In clinical situations that require health care workers to be in contact
with patients who are known or suspected to be infected with microorganisms that are
transmitted via the airborne route (most commonly TB), wearing a NIOSH approved, N95
particulate respirator is indicated.
Features
Because the selection of facial protection devices is a highly personal decision, certain
device features may influence an individual’s decision. Specific features are built into
some masks for special applications; these include fog-free foams, adhesive tapes or
films, eye shields (also mandated by the OSHA Bloodborne Pathogens Standard), and
materials designed to avoid skin sensitivity (see Table 8). The design and means of
attachment of eye shields vary. For example, an eye shield may be glued to the mask
or sonically welded to it. A disadvantage of glued-on eye shields is that the glue may
degrade over time, causing a noxious odor or skin irritation. With the increased use of
eye protection, the importance of devices with features to reduce or eliminate fog, due
to moisture from the wearer’s breath, has also increased. The three most common of
these features are foam, film, and tape; of these, the most commonly used is foam, for
example, a foam strip with a moisture trap or flap may be preferable. Alternatively, some
masks use a vapor film to trap moisture and prevent fogging. Tape may also be used,
although the tape often used to prevent fogging can cause dermal irritation.
Table 8 – Features of Facial Protection Devices
Feature
Fog-Free
Nose Wire
Donning Mechanism
Tie Attachment
Eye Shield
Options
• Foam
• Film
• Tape
• Aluminum
• Coated
Steel
• Earloops
• Ties – vertical and
horizontal
• Strap –single or
double
• Inside
• Outside
• Sewn, stapled,
glued
• Sonically welded
• Polyester
Film
• Anti-glare
Film
Fit
Facial protection devices are effective only if worn properly. The fit should assure that the
nose and mouth are covered completely and that there is no tenting at the sides of the
mouth that would allow dispersion or entry of microbes. To ensure a secure fit, the mask
should fit underneath the mouth; conform to the shape of the cheekbones; and cover the
nose (the nose wire, i.e., the small pliable strip at the nose area, should promote a close
31
fit. For surgical masks, the top ties are tied at the crown of the head, and the bottom
ties are tied at the base of the neck. For procedure masks, the earloops are placed over
each ear. The wearer should not have to readjust the mask after it is initially donned.
Comfort
Facial protection devices must be effective for their intended use; it is equally important
that they are comfortable for the wearer, in order to encourage proper and consistent
use. One important element of comfort is breathability. The wearer should not feel that
the face mask is inhibiting his or her ability to breathe; in addition, the mask should not
get “hot” over long periods of use. Comfort is affected by several factors, including the
softness of the inner facing material; the feel of the earloops or ties (i.e., soft and stretchy
versus scratchy and non-stretchy); whether the ties are on the outside or inside of the
mask; and if the nose wire is malleable and/or possesses memory.
Wearer Acceptance
The effectiveness of any mask can also be assessed by evaluating the level of
acceptance by the wearer. Two primary considerations in acceptance are the wearer’s
ability to communicate and the provision of a clear, unobstructed field of vision. Perioperative personnel will also notice the level of distraction, which is influenced by
factors such as odor and texture, interference with job performance, ease of donning and
removal, and the tendency to cause fogging. Dermal sensitivity to masks is another issue
affecting wearer acceptance. Lastly, the wearer also must have confidence in the mask’s
effectiveness.
Summary
Health care facilities, especially the surgical practice environment, are inherently
dangerous for their employees. The protection of the health care worker, as well as the
patient, has become an issue of greater awareness in surgical suites today; furthermore,
it is becoming more complex. As all members of the perioperative team know, wearing
appropriate facial protection devices is a key component in minimizing the spread of
potentially infectious diseases, especially in the face of today’s drug resistant organisms,
new pathogens, and the recognition of the hazards associated with exposure to surgical
smoke. Regardless of the surgical practice setting, it is clear that better facial protection
for all personnel is an appropriate objective in the current health care environment.
Today, facial protection devices are available with a wide range of features, fit,
efficiency, and elements of performance to meet the challenges faced by the changing
demands. Better protection, through the use of improved facial protection devices, an
understanding of the applicable regulations and guidelines; and the implementation of
effective policies and procedures, is essential to reduce the risk of occupational exposure
and infectious disease transmission for all perioperative personnel.
32
GLOSSARY
Airborne Precautions Precautions that decrease the risk of an
airborne transmission of infectious airborne
droplet nuclei, i.e., small particle residue 5
microns or smaller, that can remain suspended
in the air for extended periods of time or
infectious dust particles that can be circulated
by air currents.
Bacterial Filtration Efficiency (BFE)
The measure of the percent efficiency at which
a face mask filters bacteria passing through the
mask.
Bloodborne Pathogens Pathogenic microorganisms that are present
in human blood and can cause disease in
humans. These pathogens include, but are not
limited to, hepatitis B virus (HBV) and human
immunodeficiency virus (HIV).
Contact Precautions Precautions designed to decrease the risk of
transmission of epidemiologically significant
microorganism by direct or indirect contact.
Droplet Precautions
Precautions that decrease the risk of large
particle droplet (i.e., 5 microns or larger)
transmission of infectious agents.
Delta P
The measure of a face mask’s breathability;
Delta P is the pressure drop across a facemask,
expressed in mm H20/cm²; the higher the Delta
P, the more difficult the mask is to breathe
through.
Employee Exposure Exposure via specific eye, mouth, or other
mucous membranes; nonintact skin; or
parenteral contact with blood or other
potentially infectious materials that results
from the performance of an employee’s duties;
exposure to a concentration of an airborne
contaminant that would occur if the employee
were not using respiratory protection.
Fit Test
The use of a protocol to qualitatively or
quantitatively evaluate the fit of a respirator on
an individual. (See also Qualitative Fit Test and
Quantitative Fit Test below.)
33
Flammability
The relative ease with which a material can
ignite and sustain combustion.
Fluid Resistance
The ability of a face mask’s material
construction to minimize fluids from traveling
through the material and potentially coming
into contact with the wearer, Fluid resistance
helps to reduce potential exposure to blood
and body fluids caused from splashes, spray
or spatter.
High Filtration Mask
Masks having a filtering capacity of particulate
matter at 0.3 microns to 0.1 microns in size.
Particulate
A very small solid which is suspended in the
air or in a liquid.
Particulate Filtration Efficiency (PFE)
The measure of the percent efficiency at
which a face mask filters particulate matter
passing through the mask.
Personal Protective Equipment (PPE) Protective equipment (e.g., masks, gloves,
goggles, face shields, and gowns) for eyes,
face, head, and extremities; protective
clothing; respiratory devices; and protective
shields and barriers designed to protect the
wearer from injury.
Potentially Infectious Material
Blood; all body fluids, secretions, and
excretions (except sweat), regardless
of whether they contain visible blood;
nonintact skin; mucous membranes; and
airborne, droplet, and contact-transmitted
epidemiologically important pathogens.
Qualitative Fit Test
A pass/fail test to assess the adequacy
of N95 respirator fit, as determined by
an individual’s response to the certain
aerosolized test solutions.
Quantitative Fit Test
A test assessing the adequacy of N95
respirator fit by numerically measuring the
amount of leakage into the respirator.
34
Standard Precautions
The primary strategy for successful infection
control and reduction of worker exposure.
Standard precautions are used when caring
for all patients, regardless of their diagnosis
or presumed infectious status.
Surgical Smoke
Smoke that is generated when tissue is
heated and cellular fluid is vaporized by the
thermal action of an energy source.
35
REFERENCES / SUGGESTED READINGS
1. AORN. Recommended practices for surgical attire. In: Perioperative Standards and
Recommended Practices. Denver, CO: AORN, Inc; 2014; 49-60.
2. Lipp A, Edwards P. Disposable surgical face masks for preventing surgical wound
infection in clean surgery. Cochrane Database Syst Rev. 2014;(2):CD002929.
3. CDC. Seasonal influenza. http://www.cdc.gov/flu/about/disease/index.htm. Accessed
May 27, 2014.
4. AORN. Recommended practices for prevention of transmissible infections in the
perioperative practice setting. In: Perioperative Standards and Recommended
Practices. Denver, CO: AORN, Inc; 2014; 385-417.
5. Cuming RG, Rocco TS, McEachern AG. Improving compliance with Occupational
Safety and Health Administration Standards. AORN J. 2008; 87(2): 347-356.
6. Tarrac SE. Application of the updated CDC isolation guidelines for health care
facilities. AORN J. 2008; 87(3): 534-542.
7. CDC. Middle East Respiratory Syndrome (MERS). http://www.cdc.gov/
CORONAVIRUS/MERS/INDEX.HTML. Accessed May 28, 2014.
8. Ulmer BC. The hazards of surgical smoke. AORN J. 2008; 87(4): 721-734.
9. AORN. Management of surgical smoke in the perioperative setting. In: Management
of Surgical Smoke Tool Kit. http://www.aorn.org/Clinical_Practice/ToolKits/Surgical_
Smoke_Evacuation_ToolKit/Management_of_Surgical_Smoke_Tool_Kit.aspx.
Accessed May 27, 2014.
10.Oberg T, Brosseau LM. Surgical mask filter and fit performance. Am J Infect Control.
2008; 36(4): 276-282.
11.US FDA. Guidance for industry and FDA staff: surgical masks—premarket
notification [510(k)] submissions; guidance for industry and FDA. http://www.fda.gov/
MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm072549.
htm. Accessed May 27, 2014
12.US FDA. Medical Devices: Masks and N95 respirators. http://www.fda.gov/
medicaldevices/productsandmedicalprocedures/generalhospitaldevicesandsupplies/
personalprotectiveequipment/ucm055977.htm. Accessed May 27, 2014.
13.Oberg T, Brosseau LM. Surgical mask filter and fit performance. Am J Infect Control.
2008; 36(4): 276-282.
14.Belkin NL. The surgical mask: are new tests relevant for OR practice? AORN J.
2009;89(5): 883-891.
15.US FDA. Medical devices. FDA’s role in regulating PPE. http://www.fda.gov/
medicaldevices/productsandmedicalprocedures/generalhospitaldevicesandsupplies/
personalprotectiveequipment/ucm056084.htm. Accessed May 27, 2014.
36
16.US FDA. Guidance for industry and FDA staff: surgical masks—premarket notification
[510(k)] submissions; guidance for industry and FDA. http://www.fda.gov/MedicalDevices/
DeviceRegulationandGuidance/GuidanceDocuments/ucm072549.htm. Accessed May 27,
2014
17. US Department of Labor. OSHA. Regulations (Standards - 29 CFR) Bloodborne
pathogens - 1910.1030. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_
table=STANDARDS&p_id=10051. Accessed May 27, 2014.
18. US Department of Labor. OSHA. Regulations (Standards - 29 CFR) Respiratory
Protection - 1910.134. http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_
id=12716&p_table=standards. Accessed May 27, 2014.
19. CDC NIOSH. 42 CFR Part 84: Respiratory protective devices. http://www.cdc.gov/niosh/
npptl/topics/respirators/pt84abs2.html. Accessed May 27, 2014.
20. US FDA. Guidance for industry and FDA staff: surgical masks - premarket
notification [510(k)] submissions; guidance for industry and FDA. http://www.fda.gov/
MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm072549.htm.
Accessed May 27, 2014.
21. ASTM. ASTM Standard F1862/F1862M-13. Standard Test Method for Resistance of
Medical Face Masks to Penetration by Synthetic Blood (Horizontal Projection of Fixed
Volume at a Known Velocity). West Conshohocken, PA: ASTM International; 2013.
22. ASTM. ASTM Standard F1215-89. Test Method For Determining the Initial Efficiency of
a Flatsheet Filter Medium in an Air-Flow Using Latex Spheres [withdrawn 1998]. West
Conshohocken, PAA; ASTM International; 1989. 23. ASTM. ASTM Standard F2101 – 07. Standard Test Method for Evaluating the Bacterial
Filtration Efficiency (BFE) of Medical Face Mask Materials, Using a Biological Aerosol of
Staphylococcus aureus. West Conshohocken, PAA; ASTM International; 2007. 24. Department of Defense. MIL-M-36945C 4.4.1.1.1 Method 1 Military specifications:
Surgical mask, disposable. Washington, DC; Department of Defense; June 12, 1975.
25. Code of Federal Regulations. Part 1610 - Standard for the flammability of clothing
textiles. http://www.gpo.gov/fdsys/pkg/CFR-2011-title16-vol2/xml/CFR-2011-title16-vol2part1610.xml. Accessed May 27, 2014.
26. NFPA. NFPA 702: Standard for Classification of the Flammability of Wearing Apparel.
Quincy, MA; NFPA; 1980.
27. UL. Fire Tests of Surgical Fabric, 2nd ed. Camas, WA: Underwriters Laboratories; 2000.
28. ASTM. ASTM Standard F2100-11. Standard Specification for Performance of Materials
Used in Medical Face Masks. West Conshohocken, PA; ASTM International; 2011.
29. Akridge J. Personal protective equipment aids patients, clinicians and bottom line. http://
www.hpnonline.com/inside/2012-07/1207-ip-ppe.html. Accessed May 27, 2014.
37
30. US Department of Labor. OSHA. Regulations (Standards - 29 CFR) Bloodborne
pathogens - 1910.1030. https://www.osha.gov/pls/oshaweb/owadisp.show_
document?p_table=STANDARDS&p_id=10051. Accessed May 27, 2014.
31. US Department of Labor. OSHA. Regulations (Standards - 29 CFR) Respiratory
Protection - 1910.134. http://www.osha.gov/pls/oshaweb/owadisp.show_
document?p_id=12716&p_table=standards. Accessed May 27, 2014.
32. OSHA. Pandemic influenza preparedness and response guidance for healthcare
workers and healthcare employers. https://www.osha.gov/Publications/OSHA_
pandemic_health.pdf. Accessed May 28, 2014.
33. CDC. 2007 guideline for isolation precautions: preventing transmission of infectious
agents in healthcare settings. http://www.cdc.gov/hicpac/pdf/isolation/Isolation2007.
pdf. Accessed May 28, 2014.
34. CDC. Guidelines for preventing the transmission of Mycobacterium tuberculosis in
health-care settings, 2005. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5417a1.
htm?s_cid=rr5417a1_e. Accessed May 28, 2014.
35. CDC. Prevention strategies for seasonal influenza in healthcare settings. http://www.
cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm. Accessed May 28,
2014.
36. CDC. Interim infection prevention and control recommendations for hospitalized
patients with Middle East Respiratory Syndrome Coronavirus (MERS-CoV).
http://www.cdc.gov/coronavirus/mers/downloads/MERS-Infection-ControlGuidance-051414.pdf. Accessed May 28, 2014
37. AORN. Recommended practices for surgical attire. In: Perioperative Standards and
Recommended Practices. Denver, CO: AORN, Inc; 2014; 49-60.
38. AORN. Recommended practices for laser safety in perioperative practice settings.
In: Perioperative Standards and Recommended Practices. Denver, CO: AORN, Inc;
2014: 141-154.
39. AORN. Recommended practices for prevention of transmissible infections in the
perioperative practice setting. In: Perioperative Standards and Recommended
Practices. Denver, CO: AORN, Inc; 2014; 385-417.
40. APIC Personal protective equipment (PPE) education. Washington, DC: APIC; 2005.
41.Infection Control Today. Groups ask Obama to rethink N95 issue. http://www.
infectioncontroltoday.com/news/2009/11/groups-ask-obama-to-rethink-n95-issue.
aspx. Accessed May 28, 2014.
38
Please click here for the
Post-Test and Evaluation
39