texas children`s hospital - Dell Children`s Medical Center of Central
advertisement
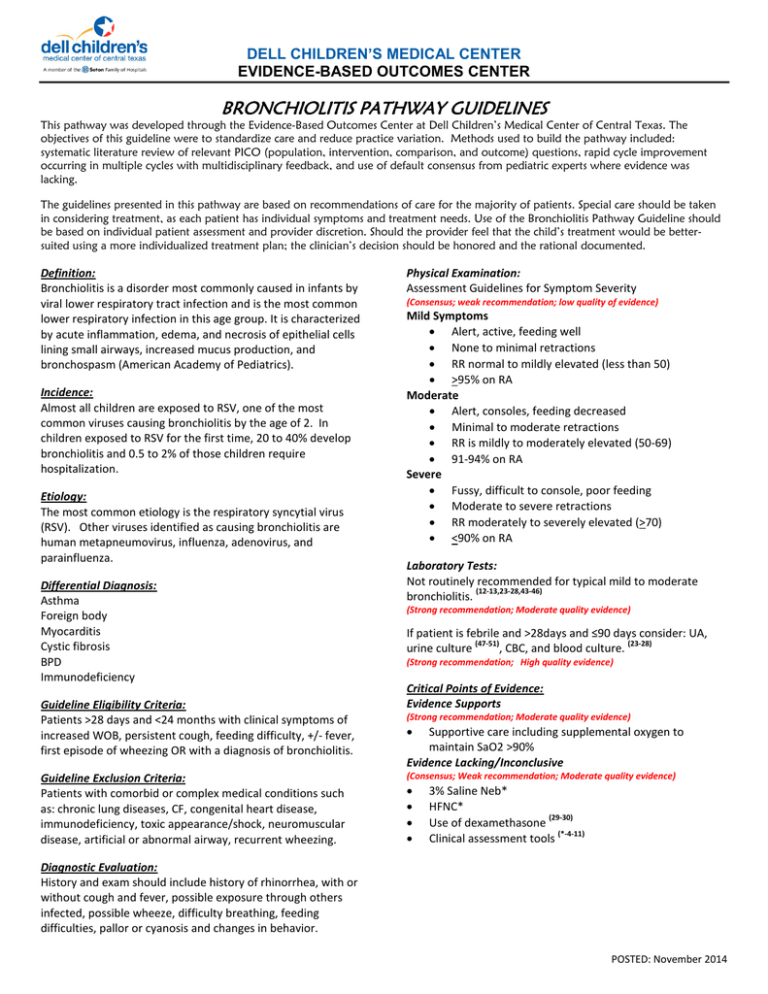
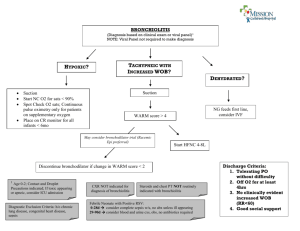
DELL CHILDREN’S MEDICAL CENTER EVIDENCE-BASED OUTCOMES CENTER BRONCHIOLITIS PATHWAY GUIDELINES This pathway was developed through the Evidence-Based Outcomes Center at Dell Children’s Medical Center of Central Texas. The objectives of this guideline were to standardize care and reduce practice variation. Methods used to build the pathway included: systematic literature review of relevant PICO (population, intervention, comparison, and outcome) questions, rapid cycle improvement occurring in multiple cycles with multidisciplinary feedback, and use of default consensus from pediatric experts where evidence was lacking. The guidelines presented in this pathway are based on recommendations of care for the majority of patients. Special care should be taken in considering treatment, as each patient has individual symptoms and treatment needs. Use of the Bronchiolitis Pathway Guideline should be based on individual patient assessment and provider discretion. Should the provider feel that the child’s treatment would be bettersuited using a more individualized treatment plan; the clinician’s decision should be honored and the rational documented. Definition: Bronchiolitis is a disorder most commonly caused in infants by viral lower respiratory tract infection and is the most common lower respiratory infection in this age group. It is characterized by acute inflammation, edema, and necrosis of epithelial cells lining small airways, increased mucus production, and bronchospasm (American Academy of Pediatrics). Incidence: Almost all children are exposed to RSV, one of the most common viruses causing bronchiolitis by the age of 2. In children exposed to RSV for the first time, 20 to 40% develop bronchiolitis and 0.5 to 2% of those children require hospitalization. Etiology: The most common etiology is the respiratory syncytial virus (RSV). Other viruses identified as causing bronchiolitis are human metapneumovirus, influenza, adenovirus, and parainfluenza. Differential Diagnosis: Asthma Foreign body Myocarditis Cystic fibrosis BPD Immunodeficiency Guideline Eligibility Criteria: Patients >28 days and <24 months with clinical symptoms of increased WOB, persistent cough, feeding difficulty, +/- fever, first episode of wheezing OR with a diagnosis of bronchiolitis. Guideline Exclusion Criteria: Patients with comorbid or complex medical conditions such as: chronic lung diseases, CF, congenital heart disease, immunodeficiency, toxic appearance/shock, neuromuscular disease, artificial or abnormal airway, recurrent wheezing. Physical Examination: Assessment Guidelines for Symptom Severity (Consensus; weak recommendation; low quality of evidence) Mild Symptoms • Alert, active, feeding well • None to minimal retractions • RR normal to mildly elevated (less than 50) • >95% on RA Moderate • Alert, consoles, feeding decreased • Minimal to moderate retractions • RR is mildly to moderately elevated (50-69) • 91-94% on RA Severe • Fussy, difficult to console, poor feeding • Moderate to severe retractions • RR moderately to severely elevated (>70) • <90% on RA Laboratory Tests: Not routinely recommended for typical mild to moderate (12-13,23-28,43-46) bronchiolitis. (Strong recommendation; Moderate quality evidence) If patient is febrile and >28days and ≤90 days consider: UA, (47-51) (23-28) , CBC, and blood culture. urine culture (Strong recommendation; High quality evidence) Critical Points of Evidence: Evidence Supports (Strong recommendation; Moderate quality evidence) • Supportive care including supplemental oxygen to maintain SaO2 >90% Evidence Lacking/Inconclusive (Consensus; Weak recommendation; Moderate quality evidence) • • • • 3% Saline Neb* HFNC* (29-30) Use of dexamethasone (*-4-11) Clinical assessment tools Diagnostic Evaluation: History and exam should include history of rhinorrhea, with or without cough and fever, possible exposure through others infected, possible wheeze, difficulty breathing, feeding difficulties, pallor or cyanosis and changes in behavior. POSTED: November 2014 DELL CHILDREN’S MEDICAL CENTER EVIDENCE-BASED OUTCOMES CENTER Critical Points of Evidence Contiued: Evidence Against (Strong recommendation; Moderate quality evidence) • • • • • • • • • (14-22) CXR (43-46) RSV testing Deep suctioning CPT* (23-28) CBC/blood culture (unless clinically indicated) Antibiotics (unless confirmed bacterial source present) Corticosteroids Epinephrine* Use of inhaled bronchodilators* Practice Recommendations and Principles of Clinical Management The bronchiolitis diagnosis should consist of supportive care treatments as the main foundation for care. Support of respiratory symptoms, clearance of airways and dietary support are essential in the care and treatment of a child with bronchiolitis. Treatment Recommendations (for full recommendations see attached pathway and addendums) Supportive Care: • Supplemental oxygen should be administered to maintain SaO2 >90% • Nasal suction using nasal aspirator to maintain and clear airway • Assess and treat hydration status o Give PO challenge o Administer fluids as needed o Administer tube feeds as required (see addendum 2) 3% Saline Neb: • Care Provider can order 4ml Q4 hrs for severe symptoms • Multiple doses may be required to assess for effectiveness • Patient should be re-evaluated Q24 hours and the treatment should be reordered if it is to be continued • Once initiated: If the patient moves to a moderate assessment, the treatment can be continued if it is found to be effective • If the treatment has been stopped, it can ONLY be reordered if the patient is experiencing severe symptoms (31-39) High Flow Nasal Cannula (Addendum 1) • Patient to be watched for at least 30 minutes after starting high Flow in the ER. If no worsening of symptoms, PCRS IMC resident notified. • Any flow rates above what is listed below require an Intensivist consult: • For further guidelines and recommendations for use please see addendum 1. Pediatric Bronchiolitis Severity Score (BSS)* The BSS serves as a method to document patient status and acuity over the course of care. It can also be used to assess response to interventions. The tool is based on five key assessment areas; respiratory rate, oxygen need, wheezing, work of breathing, and presence of retractions. The Bronchiolitis Severity Score (BSS) is an assessment tool and is not intended to determine admission and/or placement of the patient. Admission Criteria Floor: • Moderate WOB, tachypnea • O2 requirement • Requires frequent suctioning • Dehydrated or unable to maintain oral feedings • Parent unable to care for infant at home Pulmonary Unit- High Acuity (Floor criteria + any of the following): • Moderate to severe WOB • O2 requirement (< 50% FiO2) • HFNC (see Addendum 1) IMC (Floor, Pulmonary Unit criteria + any of the following): • HFNC (see Addendum 1) • Co-morbidities (CLD) • BP requires close monitoring PICU (Floor, Pulmonary Unit, IMC criteria + any of the following): • Positive pressure ventilation • Witnessed episode of apnea • Severe dehydration/shock • HFNC (see Addendum 1) or if not improving on HFNC after 30 minutes POSTED: November 2014 DELL CHILDREN’S MEDICAL CENTER EVIDENCE-BASED OUTCOMES CENTER Consults and Referrals Consults and referrals should be ordered on an individual basis based on patient requirements. Infection Control Bronchiolitis/ RSV require CONTACT isolation. Special Considerations: • Patients with additional symptoms of influenza should be placed into droplet isolation until the diagnosis of influenza is confirmed as negative. • Staff should wear additional personal protective equipment when suctioning or performing assessments or treatments bringing them into close contact with the patient. • Wash hands thoroughly after contact with the patient Caregiver Education • Hand washing after handling the patient or the patients belongings • Importance of not bringing other siblings to the hospital for visits • Understanding of signs/symptoms of increasing respiratory distress • Proper nasal suctioning (must demonstrate ability with bulb suction) • Risk of passive smoke exposure • Encourage Direct Breastfeeding whenever possible Discharge Criteria • SpO2 ≥ 90% on RA for ≥ 2 hours • Respirations less than 60 per minute and/or minimal to no evidence of increased work of breathing • Oral feedings tolerated at a level to maintain hydration • Parents comfortable with providing home care, and parent education complete, including understanding: o Signs/symptoms of increasing respiratory distress o Proper nasal suctioning (must demonstrate ability with o bulb suction) o Risk of passive smoke exposure o Need for PCP follow-up Follow-Up Care Ideally follow-up care should be planned for 2-3 days postdischarge with the patient’s primary care doctor Prevention Avoid contact with others who are ill Wash hands Outcome Measures Length of stay Cost (testing, antibiotics) Pathway compliance POSTED: November 2014 Exclusion Criteria: Children w/ Comorbid/ complex medical conditions such as: chronic lung diseases, CF, congenital heart disease, immunodeficiency, toxic appearance/shock, neuromuscular disease, artificial or abnormal airway, recurrent wheezing ED Bronchiolitis Pathway Bronchiolitis Severity Score (BSS) If respiratory arrest imminent- triage and initiate care in resuscitation room Inclusion criteria: >28 days and <24 months with clinical symptoms of ↑WOB, persistent cough, feeding difficulty, +/- fever, first episode of wheezing OR with a diagnosis of bronchiolitis NOT Recommended in ED - CPT - CXR - RSV testing - CBC/Blood culture for patients > 90 days (unless clinically indicated) - Antibiotics- unless confirmed bacterial source present - Hypertonic Saline - Corticosteroids - Inhaled bronchodilators - Epinephrine Supplemental oxygen should be administered to maintain SaO2>90% Nasal suction If febrile and >28days & ≤90 days consider: UA, urine culture, CBC, & blood culture As s es s ment 0 1 Respiratory < 40 per 40-50 per mi n. Rate mi n. O2- >90% SaO2 RA Wheezing none WOB none Retractions none NC < 2L 2 >50 per min. NC > 2L i ns pi ra toy expira tory & expira tory Grunti ng Na s a l Fla ri ng +/- Hea d Bobbing Supra s ubcos ta l +/Sterna l +/intercos ta l Cla vicula r The BSS is an assessment tool and is not intended to determine admission and/or placement of the patient. Assess Disease Severity * *Moderate Symptoms *Mild Symptoms - Nasal suction using nasal aspirator - Assess hydration status (PO ad lib OR NPO w/IVF or NG feeds) - Observe - Nasal suction using nasal aspirator - Assess hydration status - Give po challenge *Severe Symptoms - Notify Provider - Nasal suction using nasal aspirator - Assess hydration status (consider IVF, check glucose/electrolytes for significant dehydration) - Consider 3% Saline Neb- (4ml Q4hr) - Consider starting high flow nasal cannula**** Reassess Disease Severity * Meets Discharge Criteria** Meets Admission Criteria*** Admit to Inpatient Unit Based on Admit Criteria (not score) Discharge Home INTERVENTIONS: All interventions should have a pre and post score to evaluate for effectiveness. (including, but not limited to: suctioning, repositioning, switch to NPO, implementation or discontinuation of O2) *Assessment Guidelines Mild - Alert, active, feeding well - None to minimal retractions - RR normal to mildly elevated (less than 50) - >95% RA Moderate - Alert, consoles, feeding decreased - Minimal to moderate retractions - RR is mildly to moderately elevated (50-69) - 91-94% on RA Severe - Fussy, difficult to console, poor feeding - Moderate to severe retractions - RR moderately to severely elevated (>70) - <90% on RA **Discharge Criteria - SpO2 ≥ 90% RA - Respirations less than 60 per minute and/or minimal to no evidence of increased work of breathing - Oral feedings tolerated at a level to maintain hydration - Parents comfortable with providing home care, and parent education complete, including understanding: - signs/symptoms of increasing respiratory distress - proper nasal suctioning (must demonstrate ability with bulb suction) - risk of passive smoke exposure - Need for PCP follow-up - encourage continued DBF - prevention education - Need for PCP follow-up ***Admission (Unit) Criteria Floor: - Moderate WOB, tachypnea - O2 requirement - Requires frequent suctioning - Dehydrated or unable to maintain oral feedings - Parent unable to care for infant at home Pulmonary Unit- High Acuity (Floor criteria +): - Moderate to severe WOB - O2 requirement (< 50% FiO2) - HFNC (see right) IMC (Floor, Pulmonary Unit criteria +): - HFNC (see right) - Co-morbidities (CLD) - BP requires close monitoring PICU (Floor, Pulmonary Unit, IMC criteria +): - Positive pressure ventilation - Witnessed episode of apnea - Severe dehydration/shock - HFNC (see right) or if not improving on HFNC after 30 minutes High Flow Nasal Cannula Guidelines ****(see addendum 1) Patient to be watched for at least 30 minutes after starting High Flow in the ER. If no worsening of symptoms, PCRS IMC resident is notified Any flow rates above what is listed below require an Intensivist consult. Weight (kg) <7 7 –9 >9 Initial flow Max flow rate (lpm) rate (lpm) 4 6 6 8 6 10 PC 02-19-15 DELL CHILDREN’S MEDICAL CENTER EVIDENCE-BASED OUTCOMES CENTER Addendum 1 High Flow Nasal Cannula (HFNC) Recommended Guidelines for Use by PCRS Recommendations: 1. It is desirable that all PCRS faculty have the same general approach for this technology in the interest of safety, mutual understanding of what to expect when cross covering, and to be consistent in our education roles 2. This document is not a protocol but rather an internal document to guide us 3. Variation from this guideline is appropriate so long as documentation exists 4. Patient to be watched for at least 30 minutes after starting High Flow in the ER. If patient improves or there is no worsening of symptoms, PCRS IMC resident is notified. 5. Criteria for use on the Pulmonary Unit: • “Classic Bronchiolitis” w/o significant comorbidity (e.g. no chronic lung disease [abn compliance], no symptomatic congenital heart disease and without suggestion of impending respiratory failure) • Post-conceptual age > 44 wks but < 2 yrs • Moderate to severe disease (further definition of this pending) • FiO2 < 50% to maintain SaO2> 90% • Flow Rates are recommended within the following parameters: Weight (kg) Initial flow rate (lpm) Max flow rate (lpm) <7 4 6 7–9 6 8 >9 6 10 6. Use of HFNC in IMC: • Same age criteria as the floor • Comorbidities above may be managed in IMC • Patients with mild respiratory acidosis may be managed in IMC at provider’s discretion 7. Critical Care consultation suggested for: • Any patient worsening after 30 minutes on HFNC • Any patient in severe distress not improving after 30 minutes on HFNC • FiO2 >50% • Flow rates above the recommended parameters • Apnea 8. Feeding while on HFNC (see addendum 2): • No evidence exists regarding risks of feeding while on HFNC • Consider NPO initially with decision for NGT or PO trial made after some stability reached 9. Weaning: • O2 wean by RT based on SaO2 goals • Flow wean to start by a physician’s order but generally not until stabilized for 8 -12 hrs. • Decrease flow by 2 lpm every 4 hrs Change to NC when on 2 lpm for 4 hrs prepared by: Duc, Cossey, Iyer & Holt POSTED: November 2014 Inpatient Bronchiolitis Pathway Exclusion Criteria: Children with Comorbid or complex medical conditions such as: chronic lung diseases, CF, congenital heart disease, immunodeficiency, toxic appearance/shock, neuromuscular disease, artificial or abnormal airway, recurrent wheezing NOT RECOMMENDED on Inpatient Units Inclusion criteria: >28 days and <24 months with clinical symptoms of ↑WOB, persistent cough, feeding difficulty, +/- fever, first episode of wheezing OR with a diagnosis of bronchiolitis - CPT - CXR - RSV test - Blood tests (CBC/Blood culture): unless clinically indicated - Antibiotics unless confirmed bacterial source present - Corticosteroids - Use of inhaled bronchodilators Supplemental oxygen should be administered to maintain SaO2>90% If febrile and >28days & ≤90 days consider: UA, urine culture, CBC, and blood culture α Assess Disease Severity NO *Mild Symptoms YES Meets Discharge Criteria - Supportive Care - BSS Score Q4hrs and prn - PO ad lib - Strict I&O - Nasal suction using nasal aspirator *Assess Disease Severity STOP Notify Provider NOT Effective NO *Moderate Symptoms YES YES **Discharge Using Discharge Criteria - Supportive Care - BSS Score Q4hrs and prn - PO ad lib OR NPO w/ IVF or NG feeds - Strict I&O - Nasal suction using nasal aspirator NO *** Transfer to Pulmonary Unit, IMC OR Consult w/Intensivist for transfer to PICU *Severe Symptoms NO Improvement After Interventions, Initiation of HFNC, OR Minimal Improvement - Notify Provider - NPO w/ IVF - Interventions as ordered - Consider initiation of HFNC**** Treatment Option Treatment OPTION (Ordered by MD): 3% Saline Neb-Order 4ml Q4 hrs - Multiple doses are required to assess for effectiveness - Pt should be re-evaluated Q24 hrs and the treatment should be reordered if it is to be continued - Once initiated: If the pt moves to a moderate assessment, the treatment can be continued if it is found to be effective - If the treatment has been stopped, it can ONLY be reordered if the pt is experiencing severe symptoms Effective NO Improvements After Interventions YES α INTERVENTIONS: All interventions should have a pre and post score to evaluate for effectiveness. (including, but not limited to: suctioning, repositioning, switch to NPO, implementation or discontinuation of O2, nebs) Scoring- RN: Q4 hrs and pre/post intervention and RT: pre/post intervention *Assessment Guidelines Mild - Alert, active, feeding well - None to minimal retractions - RR normal to mildly elevated (less than 50) - >95% RA Moderate - Alert, consoles, feeding decreased - Minimal to moderate retractions - RR is mildly to moderately elevated (50-69) - 91-94% on RA Severe - Fussy, difficult to console, poor feeding - Moderate to severe retractions - RR moderately to severely elevated (>70) - <90% on RA **Discharge Criteria - SpO2 ≥ 90% RA for ≥ 2 hours - Respirations less than 60 per minute and/or minimal to no evidence of increased work of breathing - Oral feedings tolerated at a level to maintain hydration - Parents comfortable with providing home care, and parent education complete, including understanding: - signs/symptoms of increasing respiratory distress - proper nasal suctioning (must demonstrate ability with bulb suction) - risk of passive smoke exposure - encourage continued DBF - prevention education - Need for PCP follow-up ***Admission (Unit) Criteria Floor: - Moderate WOB, tachypnea - O2 requirement - Requires frequent suctioning - Dehydrated or unable to maintain oral feedings - Parent unable to care for infant at home Pulmonary Unit- High Acuity (Floor criteria +): - Moderate to severe WOB - O2 requirement (< 50% FiO2) - HFNC (see right) IMC (Floor, Pulmonary Unit criteria +): - HFNC (see right) - Co-morbidities (CLD) - BP requires close monitoring PICU (Floor, Pulmonary Unit, IMC criteria +): - Positive pressure ventilation - Witnessed episode of apnea - Severe dehydration/shock - HFNC (see right) or if not improving on HFNC after 30 minutes High Flow Nasal Cannula Guidelines HFNC**** (see addendum 1) Any flow rates above what is listed below require an Intensivist consult. (See addendum 2 for feeding guidelines) Weight (kg) <7 7 –9 >9 Initial flow Max flow rate (lpm) rate (lpm) 4 6 6 8 6 10 PC 02-19-15 DELL CHILDREN’S MEDICAL CENTER EVIDENCE-BASED OUTCOMES CENTER Addendum 2 Bronchiolitis and High Flow Nasal Cannula FEEDING Guidelines Recommended Guidelines for Use by PCRS Nutrition remains an important element to the treatment and healing of a child with bronchiolitis. There is little research that specifically addresses the safety of PO feeding a child with bronchiolitis AND has been started on high flow nasal cannula (HFNC). Below are guidelines based on literature review and the medical opinion of the DCMC Bronchiolitis workgroup. Upon initiation of HFNC, the child should remain NPO to assess clinical response for approximately 1 hour. At that time, a discussion amongst the medical team and led by the attending physician will determine the appropriate method of nutrition. • Should the child’s hydration status at the induction of HFNC be of concern, the medical team can choose from the following options: o Nasogastric tube (NGT)* o IVF o NGT + IVF o NJT ( Nasojejunal tube) If PO feeds have been started, it is strongly recommended to make the child NPO and consider the above options if: • Choking/gasping and/or an increase in work of breathing during or acutely after PO feeding • Respiratory rate consistently >60 bpm beyond 15 minutes • Child is titrated to the maximum flow rate of HFNC for weight At any time, the physician has the option to make the child NPO and hydrate the child by other means. *Recommend initial NGT trial of pedialyte before (EBM or formula) to assess the child’s tolerance gastric distention while experiencing respiratory distress. PCRS/ GMiner POSTED: November 2014 DELL CHILDREN’S MEDICAL CENTER EVIDENCE-BASED OUTCOMES CENTER References *American Academy of Pediatrics Recommendations Shawn L. Ralston, Allan S. Lieberthal, H. Cody Meissner, et. al., Clinical Practice Guideline: The Diagnosis, Management, and Prevention of Bronchiolitis. Pediatrics: The official journal of the Americal Academy of Pediatrics. 2014. E1474-e1503. Link: http://pediatrics.aappublications.org/content/early/2014/10/21/peds.2014-2742 Albuterol 1. Gadomski AM, Brower M. Bronchodilators for bronchiolitis. Cochrane Database of Systematic Reviews 2010, Issue 12. 2. Del Veccio MT, Doerr LE, Gaughan JP. The use of albuterol in young infants hospitalized with acute RSV bronchiolitis. Interdisciplinary Perspectives on Infectious Diseases 2012: Article ID 585901. 3. Dobson JV, Stephens-Groff SM, McMahon SR, Stemmler MM, Brallier SL, Bay C. The Use of epine in Hospitalized Infants With Bronchiolitis. Pediatrics 1998;101;361 Assessment Tools 4. Corneli HM, Zorc JJ, Mahajan P, Shaw KN, Holubkov R, Reeves SD, Ruddy RM, Malik B, Nelson KA, Bregstein JS, Brown KM, Denenberg MN, Lillis KA, Cimpello LB, Tsung JW, Borgialli DA, Baskin MN, Teshome G, Goldstein MA, Monroe D, Dean JM, Kuppermann N, Bronchiolitis Study Group of the Pediatric Emergency Care Applied Research Network (PECARN). A multicenter, randomized, controlled trial of dexamethasone for bronchiolitis. N Engl J Med. 2007 Jul 26; 357 (4) :331-9. PubMed PMID:17652648. 5. Lowell DI, Lister G, Von Koss H, McCarthy P. Wheezing in infants: the response to epinephrine. Pediatrics. 1987 Jun; 79 (6) :939-45. PubMed PMID:3295741. 6. Gorelick MH, Stevens MW, Schultz TR, Scribano PV. Performance of a novel clinical score, the Pediatric Asthma Severity Score (PASS), in the evaluation of acute asthma. Acad Emerg Med. 2004 Jan; 11 (1) :10-8. PubMed PMID:14709423. 7. Chalut DS, Ducharme FM, Davis GM. The Preschool Respiratory Assessment Measure (PRAM): a responsive index of acute asthma severity. J Pediatr. 2000 Dec;137(6):762-8. PubMed PMID: 11113831. 8. Birken CS, Parkin PC, Macarthur C. Asthma severity scores for preschoolers displayed weaknesses in reliability, validity, and responsiveness. J Clin Epidemiol. 2004 Nov; 57 (11) :1177-81. PubMed PMID:15567635. 9. Grewal S, Ali S, McConnell DW, Vandermeer B, Klassen TP. A randomized trial of nebulized 3% hypertonic saline with epinephrine in the treatment of acute bronchiolitis in the emergency department. Arch Pediatr Adolesc Med. 2009 Nov; 163 (11) :1007-12. PubMed PMID:19884591. 10. Westley CR, Cotton EK, Brooks JG. Nebulized racemic epinephrine by IPPB for the treatment of croup: a double-blind study. Am J Dis Child. 1978 May;132(5):484-7. PubMed PMID: 347921. 11. CMP Resource Center. (2010). Clinical practice guideline: Bronchiolitis/ respiratory syncytial virus (RSV). CMP Resource Center. Spring release 2010, 1-9. Basic Metabolic Panel Testing 12. Lieberthal, A. S., Bauchner, H., Hall, C. B., Johnson, D. W., Kotagal, U., Light, M. J., ... & Davidson, C. (2006). Diagnosis and management of bronchiolitis.Pediatrics, 118(4), 1774-1793. PubMed PMID: 17015575. 13. Papoff, P., Moretti, C., Cangiano, G., Bonci, E., Roggini, M., Pierangeli, A., ... & Midulla, F. (2011). Incidence and predisposing factors for severe disease in previously healthy term infants experiencing their first episode of bronchiolitis.Acta Paediatrica, 100(7), e17-e23. PubMed PMID: 21284715. Chest X-ray 14. Lieberthal, A. S., Bauchner, H., Hall, C. B., Johnson, D. W., Kotagal, U., Light, M. J., ... & Davidson, C. (2006). Diagnosis and management of bronchiolitis.Pediatrics, 118(4), 1774-1793. PubMed PMID: 17015575. 15. Schuh, S., Lalani, A., Allen, U., Manson, D., Babyn, P., Stephens, D., ... & Dick, P. (2007). Evaluation of the utility of radiography in acute bronchiolitis.The Journal of pediatrics, 150(4), 429-433. PubMed PMID: 17382126. 16. Yong, J. H. E., Schuh, S., Rashidi, R., Vanderby, S., Lau, R., Laporte, A., ... & Ungar, W. J. (2009). A cost effectiveness analysis of omitting radiography in diagnosis of acute bronchiolitis. Pediatric pulmonology, 44(2), 122-127. PubMed PMID: 19142890. 17. Mansbach, J. M., Clark, S., Barcega, B. R., Haddad, H., & Camargo Jr, C. A. (2009). Factors Associated With Longer Emergency Department Length of Stay for Children With Bronchiolitis: A Prospective Multicenter Study. Pediatric emergency care, 25(10), 636-641. PubMed PMID: 21465688. 18. Knapp, J. F., Hall, M., & Sharma, V. (2010). Benchmarks for the emergency department care of children with asthma, bronchiolitis, and croup. Pediatric emergency care, 26(5), 364-369. PubMed PMID: 20404778. 19. Papoff, P., Moretti, C., Cangiano, G., Bonci, E., Roggini, M., Pierangeli, A., ... & Midulla, F. (2011). Incidence and predisposing factors for severe disease in previously healthy term infants experiencing their first episode of bronchiolitis.Acta Paediatrica, 100(7), e17-e23. PubMed PMID: 21284715. 20. Ralston, S., Garber, M., Narang, S., Shen, M., Pate, B., Pope, J., ... & Ryan, M. (2013). Decreasing unnecessary utilization in acute bronchiolitis care: Results from the value in inpatient pediatrics network. Journal of Hospital Medicine, 8(1), 25-30. PubMed PMID: 23047831. 21. Johnson, L. W., Robles, J., Hudgins, A., Osburn, S., Martin, D., & Thompson, A. (2013). Management of Bronchiolitis in the Emergency Department: Impact of Evidence-Based Guidelines?. Pediatrics, 131(Supplement 1), S103-S109. PubMed PMID: 23457145. 22. Knapp, J. F., Simon, S. D., & Sharma, V. (2013). Variation and trends in ED use of radiographs for asthma, bronchiolitis, and croup in children. Pediatrics,132(2), 245-252. PubMed PMID: 23878045. Complete Blood Count and Blood Culture Testing 23. Christakis, D. A., Cowan, C. A., Garrison, M. M., Molteni, R., Marcuse, E., & Zerr, D. M. (2005). Variation in inpatient diagnostic testing and management of bronchiolitis. Pediatrics, 115(4), 878-884. PubMed PMID: 15805359. 24. Lieberthal, A. S., Bauchner, H., Hall, C. B., Johnson, D. W., Kotagal, U., Light, M. J., ... & Davidson, C. (2006). Diagnosis and management of bronchiolitis.Pediatrics, 118(4), 1774-1793. PubMed PMID: 17015575. 25. Purcell, K., & Fergie, J. (2007). Lack of usefulness of an abnormal white blood cell count for predicting a concurrent serious bacterial infection in infants and young children hospitalized with respiratory syncytial virus lower respiratory tract infection. The Pediatric infectious disease journal, 26(4), 311-315. PubMed PMID: 17414393. 26. Tarini, B. A., Garrison, M. M., & Christakis, D. A. (2007). Institutional variation in ordering complete blood counts for children hospitalized with bronchiolitis.Journal of Hospital Medicine, 2(2), 69-73. PubMed PMID: 17427246. POSTED: November 2014 DELL CHILDREN’S MEDICAL CENTER EVIDENCE-BASED OUTCOMES CENTER 27. Ralston, S., Hill, V., & Waters, A. (2011). Occult serious bacterial infection in infants younger than 60 to 90 days with bronchiolitis: a systematic review.Archives of pediatrics & adolescent medicine, 165(10), 951. PubMed PMID: 21969396. 28. Haidopoulou, K., Goutaki, M., Lemonaki, M., Kavga, M., & Papa, A. (2011). Reactive thrombocytosis in children with viral respiratory tract infections.Minerva pediatrica, 63(4), 257-262. PubMed PMID: 21909061. Epinephrine and Dexamethasone 29. Hartling L, Fernandes RM, Bialy L, Milne A, Johnson D, Plint A, Klassen TP. Steroids and bronchodilators for acute bronchiolitis in the first two years of life: systematic review and meta-analysis. BMJ 2011;342:d1714. 30. Plint AC, Johnson DW, Patel H, Wiebe N, Correll R, Brant R, Mitton N, Gouin S, Bhatt M, Joubert G, Black K, Turner T, Whitehouse S, Klassen TP. Epinephrine and dexamethasone in children with bronchiolitis. N Engl J Med 2009;360:2079-89. High Flow Nasal Cannula 31. Dysart K, Miller T, Wolfson M, Shaffer T. Research in high flow therapy. Respiratory Medicine 2009;103:1400-1405 32. Motoyama EK and Finder JD. 2011, Respiratory Physiology in Infants and Children. Motoyama & Davis: Smith's Anesthesia for Infants and Children, 8th ed. Mosby, 22-79 33. Holleman-Duray D, Kaupie D, and Weiss MG. Heated humidified high-flow nasal cannula: use and a neonatal early extubation protocol. Journal of Perinatology 2007;27:776–781 34. Milesi C, Baleine J, Matecki S, Durand S, Combes C, Novais A, Combonie G. Is treatment with high flow cannula effective in acute viral bronchiolitis? A physiologic study. Intensive Care Medicine 2013;39:1088-1094 35. Arora B, Mahajan P, Zidan M, Sethuraman U. Nasopharyngeal Airway Pressures in Bronchiolitis Patients Treated with High Flow Nasal Cannula Oxygen Therapy. Pediatric Emergency Care 2012;28:1179-1184 36. McKiernan C, Chua LC, Visintainer PF, Allen H. High Flow Nasal Cannulae Therapy in Infants with Bronchiolitis. The Journal of Pediatrics 2010;156:634-8 37. Abboud PA, Roth PJ, Skiles CL, Stolfi A, Rowin ME. Predictors of failure in infants with viral bronchiolitis treated with high-flow, high-humidity nasal cannula therapy. Pediatric Critical Care Medicine 2012;12(6):e343-349 38. Wing R, James C, Maranda LS, Armsby CC. Use of High-Flow Nasal Cannula Support in the Emergency Department Reduces the Need for Intubation in Pediatric Acute Respiratory Insufficiency. Pediatric Emergency Care 2012;28(11):1117-1123 39. Kelly GS, Simon HK, Sturm JJ. High-Flow Nasal Cannula Use in Children with Respiratory Distress in the Emergency Department: Predicting the Need for Subsequent Intubation. Pediatric Emergency Care 2013;29(8);888-892 Pulse Oximetry Monitoring 40. Fouzas, S., Priftis, K. and Anthracopoulos, M. (2011). Pulse oximetry in pediatric practice. Pediatrics, 128, 740-752. 41. Zorc, J. and Hall, C. (2010). Bronchiolitis: Recent evidence on diagnosis and management. Pediatrics, 125, 342-349. 42. Mallory, M., Shay, D., Garrett, J. and Bordley, W. (2003). Bronchiolitis management preferences and the influence of pulse oximetry and respiratory rate on decision to admit. Pediatrics, 111, e45-e51. Respiratory Synctial Virus Testing 43. Christakis, D. A., Cowan, C. A., Garrison, M. M., Molteni, R., Marcuse, E., & Zerr, D. M. (2005). Variation in inpatient diagnostic testing and management of bronchiolitis. Pediatrics, 115(4), 878-884. PubMed PMID: 15805359. 44. Lieberthal, A. S., Bauchner, H., Hall, C. B., Johnson, D. W., Kotagal, U., Light, M. J., ... & Davidson, C. (2006). Diagnosis and management of bronchiolitis.Pediatrics, 118(4), 1774-1793. PubMed PMID: 17015575. 45. Jafri, H. S., Ramilo, O., Makari, D., Charsha-May, D., & Romero, J. R. (2007). Diagnostic virology practices for respiratory syncytial virus and influenza virus among children in the hospital setting: a national survey. The Pediatric infectious disease journal, 26(10), 956-958. PubMed PMID: 17901805. 46. Flaherman, V., Li, S., Ragins, A., Masaquel, A., Kipnis, P., & Escobar, G. J. (2010). Respiratory syncytial virus testing during bronchiolitis episodes of care in an integrated health care delivery system: a retrospective cohort study.Clinical therapeutics, 32(13), 2220-2229. PubMed PMID: 21316538. Urinalysis and Urine Cultures 47. Levine, D. A., Platt, S. L., Dayan, P. S., Macias, C. G., Zorc, J. J., Krief, W., ... & Kuppermann, N. (2004). Risk of serious bacterial infection in young febrile infants with respiratory syncytial virus infections. Pediatrics, 113(6), 1728-1734. PubMed PMID: 15173498. 48. Christakis, D. A., Cowan, C. A., Garrison, M. M., Molteni, R., Marcuse, E., & Zerr, D. M. (2005). Variation in inpatient diagnostic testing and management of bronchiolitis. Pediatrics, 115(4), 878-884. PubMed PMID: 15805359. 49. Lieberthal, A. S., Bauchner, H., Hall, C. B., Johnson, D. W., Kotagal, U., Light, M. J., ... & Davidson, C. (2006). Diagnosis and management of bronchiolitis.Pediatrics, 118(4), 1774-1793. PubMed PMID: 17015575. 50. Ralston, S., Hill, V., & Waters, A. (2011). Occult serious bacterial infection in infants younger than 60 to 90 days with bronchiolitis: a systematic review.Archives of pediatrics & adolescent medicine, 165(10), 951. PubMed PMID: 21969396. 51. Yarden-Bilavsky, H., Ashkenazi-Hoffnung, L., Livni, G., Amir, J., & Bilavsky, E. (2011). Month-by-Month Age Analysis of the Risk for Serious Bacterial Infections in Febrile Infants With Bronchiolitis. Clinical Pediatrics, 50(11), 1052-1056. PubMed PMID: 21685212. POSTED: November 2014