Bronchiolitis
advertisement

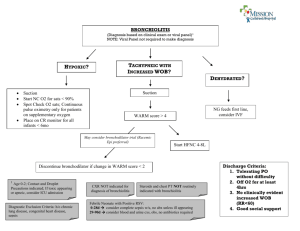
Bronchiolitis Abdullah M. Al-Olayan MBBS, SBP, ABP. Assistant Professor of Pediatrics. Pediatric Pulmonologist. Objectives ① Discuss the epidemiology, etiology and clinical manifestations of acute bronchiolitis. ② Discuss the differential diagnosis. ③ Discuss the diagnostic evaluation for recurrent wheezing. ④ Discuss the treatment of acute bronchiolitis. Etiology Bronchiolitis is a disease of small bronchioles with increased mucus production and occasional bronchospasm, sometimes leading to airway obstruction. Bronchiolitis is most commonly seen in infants and young children. Respiratory syncytial virus (RSV) is a primary cause of bronchiolitis. Etiology Other causative organisms : ① Human metapneumovirus. ② Parainfluenza viruses. ③ Pnfluenza viruses. ④ Adenoviruses. ⑤ Rhinoviruses. ⑥ Coronaviruses. ⑦ Mycoplasma pneumoniae. Etiology Viral bronchiolitis is extremely contagious and is spread by contact with infected respiratory secretions. Hand carriage of contaminated secretions is the most frequent mode of transmission. Epidemiology Bronchiolitis is a leading cause of hospitalization of infants. Bronchiolitis occurs almost exclusively during the first 2 years of life. Peak age at 2 to 6 months. In the US, annual peaks are usually in the late winter months from December through March. Clinical Manifestations Bronchiolitis caused by RSV has an incubation period of 4 to 6 days. its early phase started by cough and rhinorrhea. It progresses over 3 to 7 days to : ① Noisy, and rapid breathing. ② Audible wheezing. ③ Low-grade fever. ④ Irritability. ⑤ Decreased oral intake. Clinical Manifestations Young infants infected with RSV may have apnea as the first sign of infection. Physical signs include : ① Wheezing and crackles with Prolongation of the expiratory phase ② Nasal flaring. ③ Suprasternal and Intercostal retractions. ④ Air trapping with hyperexpansion of the lungs. ⑤ With more severe disease, grunting and cyanosis may be present. Laboratory and Imaging Routine laboratory tests are not required to confirm the diagnosis. ① Pulse oximetry is adequate for monitoring oxygen saturation. ② Frequent, regular assessments and cardiorespiratory monitoring of infants are necessary because respiratory failure may develop. ③ Antigen tests of nasopharyngeal secretions for RSV, parainfluenza viruses, influenza viruses, and adenoviruses are sensitive tests to confirm the infection. Laboratory and Imaging Chest radiographs frequently show signs of lung hyperinflation, including : ① Increased lung lucency. ② Flattened or depressed diaphragms. Areas of increased density may represent either viral pneumonia or localized atelectasis. Differential Diagnosis Asthma : ① Age of presentation. ② Presence of fever. ③ Absence of personal or family history of asthma. Differential Diagnosis Airway foreign body. Congenital airway obstructive lesion. Cystic fibrosis. Exacerbation of chronic lung disease. Viral or bacterial pneumonia. Cardiogenic asthma. GERD. Treatment Supportive therapy : ① Oxygen administration, if needed. ② Respiratory monitoring. ③ Control of fever. ④ Hydration. ⑤ Upper airway suctioning. ⑥ Bronchodilators and corticosteroids are seldom effective and are not generally recommended. Treatment Indications for hospitalization : ① Moderate to marked respiratory distress. ② Hypoxemia. ③ Apnea. ④ Inability to tolerate oral feeding. ⑤ Lack of appropriate care available at home. ⑥ High-risk children. Complications and Prognosis Most hospitalized children show marked improvement in 2 to 5 days. Tachypnea and hypoxia may progress to respiratory failure requiring assisted ventilation. Most cases of bronchiolitis resolve completely. Recurrence is common but tends to be mild and should be assessed and treated similarly to the first episode. Complications and Prognosis The incidence of asthma seems to be higher for children hospitalized for bronchiolitis as infants. There is a 1% to 2% mortality rate, highest among infants with preexisting cardiopulmonary or immunologic impairment. Prevention Monthly injections of palivizumab, an RSV specific monoclonal antibody. Initiated just before the onset of the RSV season. Indications : Infants under 2 years old with : ① chronic lung disease with prematurity. ② Very low birth weight. ③ Hemodynamically significant cyanotic and acyanotic congenital heart disease. Prevention Immunization with influenza vaccine is recommended for all children older than 6 months and may prevent influenzaassociated disease. Reference