- Wiley Online Library
advertisement

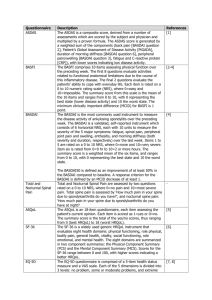
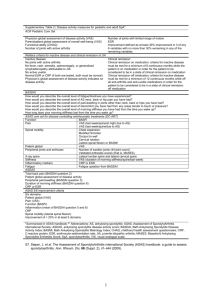
ARTHRITIS & RHEUMATISM Vol. 46, No. 3, March 2002, pp 766–773 DOI 10.1002/art.10139 © 2002, American College of Rheumatology A Six-Month Randomized, Controlled, Double-Blind, Dose-Response Comparison of Intravenous Pamidronate (60 mg Versus 10 mg) in the Treatment of Nonsteroidal Antiinflammatory Drug–Refractory Ankylosing Spondylitis Walter P. Maksymowych,1 Gian S. Jhangri,1 Avril A. Fitzgerald,1 Sharon LeClercq,1 Peter Chiu,2 Alex Yan,2 Kenneth J. Skeith,2 Stephen L. Aaron,1 Joanne Homik,1 Paul Davis,1 Dale Sholter,2 and Anthony S. Russell1 Objective. To determine the safety and efficacy of intravenous (IV) pamidronate treatment in ankylosing spondylitis (AS) patients who have had a suboptimal response to nonsteroidal antiinflammatory drugs (NSAIDs). Methods. Pamidronate at 60 mg was compared with pamidronate at 10 mg rather than placebo in view of the high incidence of transient arthralgias upon first IV exposure to the drug. The drug were given monthly for 6 months in a randomized, double-blind, controlled trial. The inclusion criterion was active disease (Bath AS Disease Activity Index [BASDAI] of >4 or morning stiffness of >45 minutes) despite stable NSAID therapy. The primary outcome measure was the BASDAI, and secondary outcomes included the Bath AS Functional Index (BASFI), Bath AS Global Index (BASGI), Bath AS Metrology Index (BASMI), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) level, and percentage of patients achieving a reduction of >25% in the BASDAI. Outcome assessments were done at ⴚ2, 0, 12, and 24 weeks, and analysis was by intent to treat. Results. Eighty-four AS patients (67 men and 17 women; mean age 39.6 years and mean disease duration 15.1 years) were enrolled. Dosage groups were well matched at baseline for demographics, disease activity, and functional indices. At 6 months, the mean BASDAI had decreased by 2.22 (34.5%) in the 60-mg group and by 0.93 (15%) in the 10-mg group (P ⴝ 0.002). Significantly greater reductions in the 60-mg group were also noted for the BASFI (P < 0.001), BASGI (P ⴝ 0.01), and BASMI (P ⴝ 0.03). Significantly more patients achieved a reduction of >25% in the BASDAI in the 60-mg group versus the 10-mg group (63.4% versus 30.2%; P ⴝ 0.004). Differences in ESR/CRP were not significant (NS). Withdrawals included 9 (20.9%) from the 10-mg group and 3 (7.3%) from the 60-mg group (P NS). Adverse events were confined to transient arthralgias/ myalgias after the first IV infusion, occurring in 68.3% and 46.5% of patients in the 60-mg and 10-mg groups, respectively (P NS). Conclusion. Pamidronate has dose-dependent therapeutic properties in AS. Supported by the Arthritis Society of Canada and the Canadian Institutes of Health (MCT-37411). Dr. Maksymowych is a Scholar of the Alberta Heritage Foundation for Medical Research. 1 Walter P. Maksymowych, FRCP, Gian S. Jhangri, MSc, Avril A. Fitzgerald, FRCP, Sharon LeClercq, FRCP, Stephen L. Aaron, FRCP, Joanne Homik, FRCP, Paul Davis, FRCP, Anthony S. Russell, FRCP: University of Alberta, Edmonton, Alberta, Canada; 2Peter Chiu, FRCP, Alex Yan, FRCP, Kenneth J. Skeith, FRCP, Dale Sholter, FRCP: Edmonton, Alberta, Canada. Address correspondence and reprint requests to Walter P. Maksymowych, FRCP, 562 Heritage Medical Research Building, University of Alberta, Edmonton, Alberta T6G 2S2, Canada. E-mail: walter.maksymowych@ualberta.ca. Submitted for publication July 27, 2001; accepted in revised form October 24, 2001. For the past several decades, nonsteroidal antiinflammatory drugs (NSAIDs) and physiotherapy have been the mainstay of management of ankylosing spondylitis (AS). Most NSAIDs, including the cyclooxygenase 2 selective inhibitors (1), are symptomatically beneficial, although there is no evidence that they modify disease, and they may be associated with significant gastrointestinal and renal toxicity (2). Sulfasalazine has been evaluated in several clinical trials of patients with spondylarthropathy (SpA). Results of 2 large multicenter trials indicated that there were no significant beneficial effects, with the exception of those patients 766 TRIAL OF PAMIDRONATE IN AS with concomitant peripheral joint disease (3,4). This therapy was also associated with a significant incidence of adverse events and a high rate of withdrawal from the study. Further progress in the development of new therapeutic strategies has, until recently, been hampered by the lack of understanding of immunopathologic processes associated with disease, particularly early in the disease course. The development of new magnetic resonance imaging (MRI) technologies has prompted the reappraisal of the pathogenesis of this disease. In particular, the ability to suppress the signal derived from marrow fat has revealed the presence of significant edema within the underlying subchondral bone marrow of both sacroiliac and peripheral joints in patients with SpA (5,6). The MRI findings have, in turn, prompted the reappraisal of the histopathology of SpA. Although enthesopathy has been traditionally considered to be the pathologic hallmark of this group of disorders, evaluation of sacroiliac and hip joints has primarily revealed the presence of significant subchondral marrow inflammation consistent with the view that enthesopathy alone does not account for the entire pathologic spectrum of disease (7–9). Bisphosphonates have become the mainstay of management of osteoporosis and other disorders of bone metabolism. They accumulate at sites of increased bone turnover, and recent work has shown that they specifically inhibit the enzyme farnesyl diphosphate synthase in the mevalonate pathway (10). This leads to impaired prenylation of a variety of proteins involved in diverse cellular processes, e.g., the GTP binding proteins Ras, Rho, and Rac, which ultimately leads to the induction of osteoclast apoptosis (11). However, there is also a considerable body of data that shows that they exert additional effects on other cells of the monocyte/ macrophage lineage (12,13). Alendronate has been shown to impair the antigen-presenting function of peripheral blood monocytes, which is restored by the addition of interleukin-1 (14). Bisphosphonates have also been shown to be effective in animal models of established arthritis, particularly adjuvant- and antigeninduced arthritis (15,16). In 2 previous open analyses, we have shown that intravenous (IV) administration of pamidronate appears to be beneficial in patients with NSAID-refractory AS (17,18). Nevertheless, previous studies have highlighted significant placebo responses (3,4). We have now examined this therapeutic strategy in a 6-month, randomized, double-blind, controlled trial. The IV administration of pamidronate is associated with a high incidence of transient postinfusion arthralgia and myalgia after the 767 initial dose (19) that significantly compromises effective patient blinding in the context of a placebo-controlled trial. The lowest dose of pamidronate shown to induce this initial infusion response has been reported to be 10 mg (20). Therefore, we designed this study as a doseresponse comparison rather than a placebo-controlled trial. PATIENTS AND METHODS Overall study design. This was a 6-month, randomized, double-blind, dose-response (60 mg versus 10 mg) study of pamidronate administered IV in patients with active AS. After a 2-week run-in period, patients were randomized in a 1:1 ratio to receive either 60 mg or 10 mg pamidronate IV for 6 months. In view of the absence of industrial support and limited formal grant support, the study was conducted in a single center, and a blinded interim analysis was performed midway through the study to allow for additional sample size calculations and to ensure appropriate recruitment. The study protocol was approved by the research ethics board of the University of Alberta. Patients. The patients enrolled in the trial were all older than 18 years. Patients met the modified New York diagnostic criteria for AS (21) and had symptoms of AS for 6 months or more. Active disease was defined by a Bath AS Disease Activity Index (BASDAI) (22) score of ⱖ4 or morning stiffness of ⱖ45 minutes despite maximum recommended or tolerated doses of NSAIDs. NSAID background therapy required a stable dosage for 1 month prior to study entry. Patients could receive second-line therapy (sulfasalazine, methotrexate) provided the dosage had been stable for 3 months prior to study entry. Dosages remained constant for the duration of the study. Exclusion criteria were end-stage ankylosis with diffuse involvement of the spine, intraarticular corticosteroid injections or IV infusion with methylprednisolone within the past 3 months prior to study entry, serum creatinine ⱖ30% above the upper limit of normal, major surgery within the previous 3 months or planned in the ensuing 6 months, severe infections/ comorbidities, or active peptic ulcer disease. Patients were recruited by rheumatologists in the Alberta Capital Health Region from both university and community-based outpatient clinics. Administration of pamidronate. Pamidronate was administered at a dosage of either 60 mg/ml or 10 mg/ml in 500 ml of 5% dextrose over 6 hours for the first dose, and over 4 hours for subsequent doses. The first infusion was given over a longer period in an attempt to decrease the likelihood of postinfusion arthralgia/myalgia. The study drug was administered monthly for 6 months in an outpatient facility at the University of Alberta Hospital that routinely administers IV therapy. Randomization. A randomization list was computer generated. The randomization code was concealed from study participants in a sealed envelope and kept in a locked office. The study drug was administered by a nurse clinician who was blinded to treatment allocation. 768 Efficacy assessment. The primary efficacy measure was the BASDAI (22). Secondary clinical efficacy measures examined included the following: the Bath AS Functional Index (BASFI) (23), the Bath AS Global Index (BASGI) (24), the Bath AS Metrology Index (BASMI) (25), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) level, and the percentage of patients achieving a ⱖ25% decrease in each of these parameters. Swollen joint counts were recorded; however, since peripheral synovitis occurs in ⬍20% of our AS population (data not shown), the study was not powered to detect significant treatment effects. Clinical assessments were done at screening (⫺2 weeks), baseline, 3 months, 2 weeks prior to the final assessment (6 months), and at 6 months. Assessments were also performed at any time a patient withdrew from the study. Mean values were obtained for the final 2 assessments and constituted the primary end point for assessment of treatment effect over the 6-month period. A 25% decrease in the BASDAI was chosen as an outcome criterion because previous work had demonstrated a 16.4% reduction in the mean BASDAI following an intensive 3-week inpatient physiotherapy program (22). Our previous open analysis of pamidronate had also shown that 5 of 7 patients who received 3 monthly infusions of pamidronate at 30 mg followed by 3 additional monthly infusions at 60 mg not only demonstrated reductions in the BASDAI of ⬎30% but were also able to substantially reduce their intake of analgesics, suggesting a clinically meaningful response (17). A nurse clinician, who was blinded to treatment allocation, provided the self-administered questionnaires and was also trained to assess the anthropometric measures of the BASMI. Withdrawal and monitoring for side effects. A patient was to be withdrawn from therapy if serious side effects occurred that were considered to be related to the study drug or in the event of an inadequate therapeutic effect requiring a change in concomitant antiinflammatory medication. Information regarding side effects was ascertained in a standard manner and potential cause or relationship to pamidronate therapy was assessed by the primary investigator (definitely, probably, uncertain, probably not, definitely not), who also assessed its severity (mild, moderate, severe). A severe adverse event was defined as a reaction that led to withdrawal of the patient from the study. A data safety and monitoring committee was formed to monitor for adverse events, to review the results of the interim analysis, and to provide recommendations about the conduct of the study and the merits of its continuation (Dr. John Hanly, Dalhousie University, Halifax, Nova Scotia; Dr. Liam Martin, University of Calgary, Calgary, Alberta; Dr. Paul Peloso, University of Iowa, Iowa City). Statistical analysis. Sample size calculations. Sample size calculations were based on the mean and SD. In our open study, BASDAI scores were observed at baseline (mean score 6.7) and at 6 months, which revealed a mean reduction of 38% (17). At the time of study initiation, placebo response rates for the BASDAI had not been documented in the literature in the context of a pharmacologic intervention because this instrument had only been validated during an 18-day inpatient physiotherapeutic intervention study (22). This revealed a 16.4% reduction in the mean BASDAI score. Consequently, the study was designed with a 2-tailed ␣ level set at 0.05, an SD of 2.1 for each group, and ⬎80% probability for detecting a MAKSYMOWYCH ET AL reduction of 15% in the mean BASDAI in the 10-mg group and 35% in the 60-mg group, assuming a 10% withdrawal rate (6.25% withdrawal was noted in our open study). This resulted in a target sample size of 84 patients. Efficacy analysis. Statistical analysis of the effects of 60 mg versus 10 mg of pamidronate was based on an intent-totreat strategy so that all patients entered into the study who received at least 1 dose of pamidronate were included in the analysis. In the event of withdrawal, the last documented outcome values were carried forward to the primary end point for inclusion in the analysis. A preliminary analysis was performed to compare the baseline characteristics of both treatment groups, using the t-test for 2 independent samples for continuous variables and the chi-square test for categorical variables. The primary outcome assessment compared the mean reduction in the BASDAI scores at 6 months versus baseline for the 2 treatment groups, using the t-test. The mean reduction in the BASFI, BASGI, and BASMI scores as well as the ESR and CRP measurements between baseline and 6 months was examined using the t-test, and percentage responders by Fisher’s exact test. RESULTS A total of 99 patients were screened for eligibility in the study from September 1997 to October 2000. Eighty-four were eventually enrolled and randomly assigned to treatment. Eight patients did not meet the eligibility criteria, 6 patients did not attend for treatment after initially agreeing to participate and completing the outcome assessments at ⫺2 weeks, and 1 patient withdrew after being provided with informed consent. Seventy-two patients completed the study, although all 84 patients were entered in the efficacy analysis. Fortyone patients were randomly assigned to the 60-mg dose and 43 to the 10-mg dose. The demographic characteristics of the 2 treatment groups at baseline were similar, revealing no statistically significant differences (Table 1). Most patients (73 of 84) were receiving NSAIDs at study entry, although 11 patients were intolerant of NSAID therapy. Two patients were receiving concomitant methotrexate therapy, 1 was receiving sulfasalazine, and 1 was receiving prednisone. Nine patients with a BASDAI of ⬍4 were admitted on the basis of morning stiffness ⱖ45 minutes. Sixteen had concomitant peripheral synovitis, 10 had inflammatory bowel disease, and 3 had psoriasis. Similar proportions in each group were HLA–B27 positive. A dose-dependent reduction in the mean BASDAI was observed over the 6 months of pamidronate administration (Figure 1). Differences between treatment arms were not significant at 3 months, but by 6 months significantly greater reductions in the mean BASDAI, BASFI, BASGI, and BASMI were noted in those pa- TRIAL OF PAMIDRONATE IN AS 769 Table 1. Demographic characteristics of the 2 pamidronate treatment groups at baseline* Mean (range) age, years No. of men/no. of women Mean (range) disease duration, years Treatment, no. NSAID Methotrexate Sulfasalazine Prednisone Peripheral synovitis, no. Inflammatory bowel disease, no. Psoriasis, no. % HLA–B27⫹ BASDAI, mean ⫾SD BASFI, mean ⫾SD BASGI, mean ⫾SD BASMI, mean ⫾SD ESR, mean ⫾ SD CRP, mean ⫾ SD 60 mg (n ⫽ 41) 10 mg (n ⫽ 43) 38.8 (24–65) 35/6 14.3 (2–33) 40.3 (25–65) 32/11 15.9 (1–44) 37 1 0 0 8 3 0 92.1 6.4 ⫾ 1.4 5.6 ⫾ 1.7 6.9 ⫾ 1.4 2.2 ⫾ 1.6 25.4 ⫾ 12.9 22.2 ⫾ 19.6 36 1 1 1 8 7 3 95.1 6.2 ⫾ 1.9 5.4 ⫾ 2.4 6.8 ⫾ 2.1 2.9 ⫾ 2.5 29.7 ⫾ 14.2 29.8 ⫾ 33.8 * NSAID ⫽ nonsteroidal antiinflammatory drug; BASDAI ⫽ Bath Ankylosing Spondylitis (AS) Disease Activity Index; BASFI ⫽ Bath AS Functional Index; BASGI ⫽ Bath AS Global Index; BASMI ⫽ Bath AS Metrology Index; ESR ⫽ erythrocyte sedimentation rate; CRP ⫽ C-reactive protein. tients who received the 60-mg dose (Figure 2). The mean BASDAI decreased by 2.22 (34.5%) in those patients who received 60 mg and by 0.93 (15%) in those who received 10 mg (P ⫽ 0.002). Significantly more patients who received the 60-mg dose (63.4%) also achieved a reduction of ⱖ25% in the BASDAI versus Figure 1. Reduction in Bath AS Disease Activity Index (BASDAI) over 6 months in patients who received either 60 mg or 10 mg pamidronate. Figure 2. Reduction in Bath AS Disease Activity Index (BASDAI), Bath AS Functional Index (BASFI), Bath AS Global Index (BASGI), and Bath AS Metrology Index (BASMI) at 6 months compared with baseline in patients who received either 60 mg or 10 mg pamidronate. those who received the 10-mg dose (30.2%) (P ⫽ 0.004) (Figure 3). Furthermore, reductions of ⱖ50% and ⱖ70% were noted in 39% and 17%, respectively, in the 60-mg group versus 16.3% (P ⫽ 0.027) and 4.7% (P ⫽ 0.08) in the 10-mg group. The mean score for axial pain (item 2 of the BASDAI) decreased by 2.58 in the 60-mg group versus 1.01 in the 10-mg group (P ⫽ 0.003). The mean score for morning stiffness (item 6 of the BASDAI) decreased by 3.01 in the 60-mg group versus 1.38 in the 10-mg group (P ⫽ 0.003). The mean score for peripheral pain (item 3 of the BASDAI) did not differ significantly between treatment groups (data not shown). The mean BASFI decreased by 1.69 (30.3%) in those patients who received the 60-mg dose versus 0.15 (2.8%) in those who received the 10-mg dose (P ⬍ 0.001). In the 60-mg group, 63.4% of patients reported a decrease of ⱖ25% in the BASFI compared with 20.9% of those in the 10-mg group (P ⬍ 0.001). Global improvement (BASGI) and spinal mobility score (BASMI) were also significantly greater in those who received 60 mg versus those who received 10 mg. For patients with peripheral synovitis, reduction in swollen joint count was not significant (data not shown), and a similar percentage of patients with peripheral synovitis achieved an improvement of 770 MAKSYMOWYCH ET AL Figure 3. Percentage of patients who had an improvement of ⱖ25% in the BASDAI, BASFI, BASGI, BASMI, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). See Figure 2 for other definitions. ⱖ25% in the BASDAI in the 2 dosage groups (data not shown). Reductions in ESR and CRP were not significant (NS). Treatment was generally well tolerated. Adverse events consisted primarily of transient arthralgia and myalgia after the first IV infusion. This was noted in 68.3% of patients who received the 60-mg dose and in 46.5% of those who received the 10-mg dose (P NS). A total of 3 patients withdrew from the 60-mg group. One patient experienced severe postinfusion arthralgia and myalgia, 1 patient did not attend for the sixth and final infusion and was lost to followup, and 1 patient withdrew at 4 months for lack of efficacy. Nine patients withdrew from the 10-mg group. Two withdrew for severe postinfusion arthralgia and myalgia, 1 patient did not attend for the sixth and final infusion and was lost to followup, 1 patient had major surgery at 5 months, 1 patient received an intramuscular injection of corticosteroid for the treatment of Crohn’s disease at 3 months, and 4 patients withdrew for lack of efficacy. Differences in withdrawal between treatment groups were not significant (P ⫽ 0.12). DISCUSSION This report describes the first controlled evaluation of pamidronate in patients with AS. Patients who received 60 mg of pamidronate IV on a monthly basis for 6 months had significantly better clinical outcomes than those who received pamidronate at a dose of 10 mg. Treatment was well tolerated, with adverse events primarily confined to the first IV infusion. No unexpected toxicities were observed and there were no significant differences between the 2 dose groups in frequency of adverse events. We therefore conclude that pamidronate appears to possess dose-dependent therapeutic properties in AS. The demographic characteristics, disease activity, and disease severity scores, as defined by the mean BASFI and BASMI, were similar at baseline to those reported in previous studies of patients with AS (3,4). The 2 groups were also reasonably well matched at baseline, attesting to the effectiveness of the randomization procedure. A high frequency of arthralgia and myalgia after the first IV infusion of pamidronate, even in those who received only 10 mg, highlights the potential difficulties in ensuring effective patient blinding during the conduct of a placebo-controlled trial with this agent. The observed frequency was higher than that reported in previous studies evaluating pamidronate in metabolic bone disease (26), and our results therefore could at least partly reflect some degree of expectation bias. On the other hand, the similar high frequency of adverse events in the 2 treatment arms does suggest that the strategy of using a 10-mg dose of pamidronate as the comparator arm as opposed to placebo was successful in ensuring effective patient blinding. Furthermore, it could be argued that the therapeutic effects of a 60-mg dose represent a conservative estimate. It remains possible that even 10 mg of pamidronate could have a significant therapeutic effect, which would minimize differences in outcomes between the 2 groups. In particular, pamidronate exerts significant antiresorptive effects, being at least 100-fold more potent than etidronate (27), and is concentrated at sites of active bone turnover such as subchondral bone in affected joints, so that even 10 mg could be efficacious. A recent placebo-controlled trial of NSAID (meloxicam or piroxicam) showed a reduction of 6.9% in the mean BASDAI in placebotreated patients (28) as compared with the 15% reduction noted in those patients treated with 10 mg pamidronate. Finally, patients were clearly aware that they were all receiving an active IV-based therapy, which could further minimize treatment group differences. The mean reductions in disease activity in patients receiving 60 mg pamidronate in this study were similar to those recorded in our previous open analysis using this same dose (17). This might be anticipated in TRIAL OF PAMIDRONATE IN AS circumstances where disease activity is measured solely by a self-administered, patient-based questionnaire (the BASDAI). Efficacy assessments were also performed in the patient’s home prior to therapy at baseline and at 6 months, to more reliably reflect the impact of disease on usual daily activities. As in the open analysis, treatment effects were delayed, implying that at least 6 months constitutes a reasonable trial of therapy. The minimal clinically detectable change in the BASDAI has yet to be determined. However, previous work has demonstrated a reduction of 29.5% in the mean BASDAI in AS patients who were treated with NSAIDs in the course of a 6-week, placebo-controlled, double-blind trial (28). This suggests that the therapeutic effects of pamidronate may be modest, although in contrast to this latter study we included NSAIDrefractory patients who may constitute a subgroup with more severe disease and an adverse prognosis (29). Nevertheless, almost 40% of patients appeared to have a substantial clinical response, as shown by a ⱖ50% reduction in the BASDAI. This will require further study in unselected patients with AS. Recent examination of the chimeric, neutralizing, monoclonal antibody to tumor necrosis factor ␣ (TNF␣) in patients with SpA demonstrated significant clinical responses commensurate with significant reductions in the acute-phase reactants ESR and CRP (30,31). This contrasts with the lack of significant reduction in the acute-phase reactants seen with pamidronate in this study. This could reflect the likelihood that pamidronate exerts its primary symptom-modifying effects at sites of high bone turnover in subchondral bone, where it accumulates at high concentrations (32) and may not ameliorate the adjacent synovitis with the regimen used in this study. This could also account for the limited efficacy demonstrable in clinical trials of IV pamidronate in patients with rheumatoid arthritis (RA) (33), a disease in which synovitis is generally more florid than in AS. A previous open analysis from our group has shown that pamidronate markedly reduces bone marrow edema in affected joints, as detected by fat-suppressed MRI (18). Furthermore, this more intensive regimen of pamidronate therapy, in which 5 60-mg infusions were given over a 2-month period, induced more impressive antiinflammatory effects within bone marrow rather than within the adjacent synovium, as demonstrated by dynamic MRI with gadolinium augmentation of affected joints, and was also accompanied by substantial reduction in ESR and CRP. Previous studies have also documented a poor correlation between clinical para- 771 meters of disease activity and levels of ESR and CRP in SpA (34). Our observations raise the possibility that orally bioavailable bisphosphonates may also be beneficial in patients with AS, particularly more potent antiresorptive agents such as alendronate and risedronate. However, the high serum levels obtained by IV administration may be relevant to the therapeutic effects observed with pamidronate. In particular, induction of apoptosis and suppression of proinflammatory cytokines appear to be dose-dependent properties of bisphosphonates (35– 37). These effects may not reflect the hierarchy of antiresorptive potency of different bisphosphonates (Maksymowych W: unpublished observations). In addition, IV administration of aminobisphosphonates, such as pamidronate and alendronate, is associated with the induction of short-lived lymphopenia over a period of 7–10 days (20,38), which could reflect systemic redistribution of lymphocyte subsets and some degree of apoptosis (39). Whether this could be associated with an antiinflammatory effect in AS is presently speculative, although it would be consistent with the more impressive antiinflammatory effects observed with a more intensive regimen of pamidronate administration. The potential dose-dependent antiinflammatory effects of bisphosphonates in chronic inflammatory arthritis are highlighted by a recent report describing beneficial clinical responses, suppression of acute-phase reactants, and decreased serum proinflammatory cytokines with high-dose alendronate therapy (40 mg/day for 90 days) in patients with RA (40). Furthermore, the association of bone marrow edema with symptomatic osteoarthritis (41) and an increased risk for developing erosions at the site of prior edema in patients with RA (42) indicates that this therapeutic approach may have more widespread implications. In conclusion, IV pamidronate therapy appears to represent a new direction in the management of AS. The rationale for this approach is further reinforced by the increased prevalence of osteoporosis together with increased markers of bone resorption, particularly in patients with early disease and elevated levels of acutephase reactants (43). A recent histopathologic and immunohistochemical examination of entheses obtained at arthroplasty revealed osteoclasts as well as CD8⫹ T cells in subchondral bone marrow from SpA patients but not RA patients or controls (44). The long-term efficacy and safety of pamidronate in AS remains to be established. Results of our previous work suggest, however, that pulse therapy incorporating more frequent infusions over a shorter period may be more effective and may 772 MAKSYMOWYCH ET AL induce more prolonged suppression of disease activity (18). This approach will need to be further evaluated in a controlled trial. From the perspective of safety, reassurance stems from the observation that 90 mg pamidronate IV every 3–4 weeks for 2 years was not associated with any significant toxicity in patients with breast malignancy (45). Although anti-TNF␣–directed therapies are efficacious in SpA, they are costly, require repeated administration, and long-term side effects remain to be determined. A trial of IV pamidronate therapy in patients with NSAID-refractory disease may therefore constitute a reasonable treatment alternative. REFERENCES 1. Dougados M, Behier JM, Jolchine I, Calin A, van der Heijde D, Olivieri I, et al. Efficacy of celecoxib, a cyclooxygenase 2–specific inhibitor, in the treatment of ankylosing spondylitis: a six-week controlled study with comparison against placebo and against a conventional nonsteroidal antiinflammatory drug. Arthritis Rheum 2001;44:180–5. 2. Bjarnason I, Hayllar J, MacPherson AJ, Russell AS. Side effects of nonsteroidal antiinflammatory drugs on the small and large intestine in humans. Gastroenterology 1993;104:1832–47. 3. Dougados M, van der Linden S, Leirisalo-Repo M, Huitfeldt B, Juhlin R, Veys E, et al. Sulfasalazine in the treatment of spondylarthropathy: a randomized, multicenter, double-blind, placebocontrolled study. Arthritis Rheum 1995;38:618–27. 4. Clegg DO, Reda DJ, Weisman MH, Blackburn WD, Cush JJ, Cannon GW, et al. Comparison of sulfasalazine and placebo in the treatment of ankylosing spondylitis. Arthritis Rheum 1996;39: 2004–12. 5. Ahlstrom H, Feltelius N, Nyman R, Hallgren R. Magnetic resonance imaging of sacroiliac joint inflammation. Arthritis Rheum 1990;33:1763–9. 6. McGonagle D, Gibbon W, O’Connor P, Green M, Pease C, Emery P. Characteristic magnetic resonance imaging entheseal changes of knee synovitis in spondylarthropathy. Arthritis Rheum 1998;41: 694–700. 7. Pasion EG, Goodfellow JW. Pre-ankylosing spondylitis: histopathological report. Ann Rheum Dis 1975;34:92–7. 8. Schichikawa K, Tsyimoto M, Nishioka J, Nishibayashi Y, Matsumoto K. Histopathology of early sacroiliitis and enthesitis in ankylosing spondylitis. In: Ziff M, Cohen SB, editors. Advances in inflammation research: the spondyloarthropathies. Vol. 9. New York: Raven Press; 1985. p. 15–24. 9. Francois RJ, Gardner DL, Degrave EJ, Bywaters EGL. Histopathologic evidence that sacroiliitis in ankylosing spondylitis is not merely enthesitis. Arthritis Rheum 2000;43:2011–24. 10. Van Beek E, Pieterman E, Cohen L, Lowik C, Papapoulos S. Farnesyl pyrophosphate synthase is the molecular target of nitrogen-containing bisphosphonates. Biochem Biophys Res Commun 1999;264:108–11. 11. Luckman SP, Hughes DE, Coxon FP, Russell G, Rogers MJ. Nitrogen-containing bisphosphonates inhibit the mevalonate pathway and prevent post-translational prenylation of GTP-binding proteins, including Ras. J Bone Miner Res 1998;13:581–9. 12. Cecchini MG, Fleisch H. Bisphosphonates in vitro specifically inhibit, among the hematopoietic series, the development of the mouse mononuclear phagocyte lineage. J Bone Miner Res 1990; 5:1019–27. 13. Stevenson PH, Stevenson JR. Cytotoxic and migration inhibitory 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. effects of bisphosphonates on macrophages. Calcif Tissue Int 1986;38:227–33. Sansoni P, Passeri G, Fagnoni F, Mohagheghpour N, Snelli G, Brianti V, et al. Inhibition of antigen-presenting cell function by alendronate in vitro. J Bone Miner Res 1995;10:1719–25. Francis MD, Hovancik K, Boyce RW. NE-58095: a diphosphonate which prevents bone erosion and preserves joint architecture in experimental arthritis. Int J Tissue React 1989;11:239–52. Barbier A, Breliere JC, Remandet B, Roncucci R. Studies on the chronic phase of adjuvant arthritis: effect of SR 41319, a new diphosphonate. Ann Rheum Dis 1986;45:67–74. Maksymowych WP, Jhangri GS, LeClercq S, Skeith K, Yan A, Russell AS. An open study of pamidronate in the treatment of refractory ankylosing spondylitis. J Rheumatol 1998;25:714–7. Maksymowych WP, Lambert R, Jhangri GS, LeClercq S, Chiu P, Wong B, et al. Clinical and radiological amelioration of refractory peripheral spondyloarthritis by pulse intravenous pamidronate therapy. J Rheumatol 2001;28:144–55. Schweitzer DH, Oostendorp-Van de Ruit M, Van der Pluijm G, Lowik CW, Papapoulos SE. Interleukin-6 and the acute phase response during treatment of patients with Paget’s disease with the nitrogen-containing bisphosphonate dimethylaminohydroxypropylidene bisphosphonate. J Bone Miner Res 1995;10:956–62. Adami S, Bhalla AK, Dorizzi R, Montesanti F, Rosini S, Salvagno G, et al. The acute-phase response after bisphosphonate administration. Calcif Tissue Int 1987;41:326–31. Van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthritis Rheum 1984;27:361–8. Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 1994;21:2286–91. Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P, et al. A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 1994;21:2281–5. Jones SD, Steiner A, Garrett SL, Calin A. The Bath Ankylosing Spondylitis Patient Global Score (BAS-G). Br J Rheumatol 1996; 35:66–71. Jenkinson TR, Mallorie PA, Whitelock HC, Kennedy LG, Garrett SL, Calin A. Defining spinal mobility in ankylosing spondylitis (AS): the Bath AS Metrology Index. J Rheumatol 1994;21:1694–8. Fenton AJ, Gutteridge DH, Kent GN, Price RI, Retallack RW, Bhagat CI, et al. Intravenous aminobisphosphonate in Paget’s disease: clinical, biochemical, histomorphometric and radiological responses. Clin Endocrinol (Oxford) 1991;34:197–204. Russell RG, Croucher PI, Rogers MJ. Bisphosphonates: pharmacology, mechanisms of action and clinical uses. Osteoporos Int 1999;9 Suppl 2:S66–80. Calin A, Nakache JP, Gueguen A, Zeidler H, Mielants H, Dougados M. Defining disease activity in ankylosing spondylitis: is a combination of variables (Bath Ankylosing Spondylitis Disease Activity Index) an appropriate instrument? Rheumatology (Oxford) 1999;38:878–82. Amor B, Dougados M, Khan MA. Management of refractory ankylosing spondylitis and related spondyloarthropathies. Rheum Dis Clin North Am 1995;21:117–28. Van den Bosch F, Kruithof E, Baeten D, De Keyser F, Mielants H, Veys EM. Effects of a loading dose regimen of three infusions of chimeric monoclonal antibody to tumour necrosis factor ␣ (infliximab) in spondyloarthropathy: an open pilot study. Ann Rheum Dis 2000;59:428–33. Brandt J, Haibel H, Cornely D, Golder W, Gonzalez J, Reddig J, et al. Successful treatment of active ankylosing spondylitis with the anti–tumor necrosis factor ␣ monoclonal antibody infliximab. Arthritis Rheum 2000;43:1346–52. TRIAL OF PAMIDRONATE IN AS 32. Sato M, Grasser W. Effects of bisphosphonates on isolated rat osteoclasts as examined by reflected light microscopy. J Bone Miner Res 1990;5:31–40. 33. Ralston SH, Hacking L, Willocks L, Bruce F, Pitkeathly DA. Clinical, biochemical, and radiographic effects of aminohydroxypropylidene bisphosphonate treatment in rheumatoid arthritis. Ann Rheum Dis 1989;48:396–9. 34. Ruof J, Stucki G. Validity aspects of erythrocyte sedimentation rate and C-reactive protein in ankylosing spondylitis: a literature review. J Rheumatol 1999;26:966–70. 35. Russell RG, Rogers MJ, Frith JC, Luckman SP, Coxon FP, Benford HL, et al. The pharmacology of bisphosphonates and new insights into their mechanisms of action. J Bone Miner Res 1999;14:53–65. 36. Van Offel JF, Schuerwegh AJ, Bridts CH, Bracke PG, Stevens WJ, De Clerck LS. Influence of cyclic intravenous pamidronate on proinflammatory monocytic cytokine profiles and bone density in rheumatoid arthritis treated with low dose prednisolone and methotrexate. Clin Exp Rheumatol 2001;19:13–20. 37. Pennanen N, Lapinjoki S, Urtti A, Monkkonen J. Effect of liposomal and free bisphosphonates on the IL-1, IL-6 and TNF␣ secretion from RAW 264 cells in vitro. Pharm Res 1995;12:916–22. 38. Vasikaran SD, Khan S, McCloskey EV, Kanis JA. Sustained response to intravenous alendronate in postmenopausal osteoporosis. Bone 1995;17:517–20. 39. Pietschmann P, Stohlawetz P, Brosch S, Steiner G, Smolen JS, 773 40. 41. 42. 43. 44. 45. Peterlik M. The effect of alendronate on cytokine production, adhesion molecule expression, and transendothelial migration of human peripheral blood mononuclear cells. Calcif Tissue Int 1998;63:325–30. Cantatore FP, Acquista CA, Pipitone V. Evaluation of bone turnover and osteoclastic cytokines in early rheumatoid arthritis treated with alendronate. J Rheumatol 1999;26:2318–23. Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, et al. The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med 2001;134:541–9. McQueen FM, Stewart N, Crabbe J, Robinson E, Yeoman S, Tan PL, et al. Magnetic resonance imaging of the wrist in early rheumatoid arthritis reveals progression of erosions despite clinical improvement. Ann Rheum Dis 1999;58:156–63. Toussirot E, Wendling D. Bone mass in ankylosing spondylitis. Clin Exp Rheumatol 2000;18 Suppl 21:S16–20. Laloux L, Voisin MC, Allain J, Martin N, Kerboull L, Chevalier X, et al. Immunohistological study of entheses in spondyloarthropathies: comparison in rheumatoid arthritis and osteoarthritis. Ann Rheum Dis 2001;60:316–21. Lipton A, Theriault RL, Hortobagyi GN, Simeone J, Knight RD, Mellars K, et al. Pamidronate prevents skeletal complications and is effective palliative treatment in women with breast carcinoma and osteolytic bone metastases: long term follow-up of two randomized, placebo-controlled trials. Cancer 2000;88:1082–90.