British Journal of Ophthalmelogy
British Journal of Ophthalmclogy
July 2005
(Volume 89, Number 7).
Special Data Supplement for this Issue
BJO at a glance
BJO at a glance
Creig Hoyt
Br J Ophthalmol 2005; 89: 789.
Editorials
The order is rapidly fadin’
J D Chidambaram and T M Lietman
Br J Ophthalmol 2005; 89: 789-790.
Let green lead not astray
J Sebag
Br J Ophthalmol 2005; 89: 790-792.
Vision restoration therapy: confounded by eye movements
J C Horton
Br J Ophthalmol 2005; 89: 792-794.
World view
Onchocerciasis: a potential risk factor for glaucoma
P R Egbert, D W Jacobson, S Fiadoyor, P Dadzie, and K D Ellingson
Br J Ophthalmol 2005; 89: 796-798.
Cover
Can you keep a secret?
I R Schwab
Br J Ophthalmol 2005; 89: 795.
Clinical science - Scientific reports
Visual loss following removal of intraocular silicone oil
S Cazabon, C Groenewald, I A Pearce, and D Wong
Br J Ophthalmol 2005; 89: 799-802.
Decreased tear lipocalin concentration in patients with meibomian gland dysfunction
M Yamada, H Mochizuki, M Kawai, K Tsubota, and T J Bryce
Br J Ophthalmol 2005; 89: 803-805.
The use of low dose methotrexate in children with chronic anterior and intermediate uveitis
A R Malik and C Pavesio
Br J Ophthalmol 2005; 89: 806-808.
Intraocular pressure changes in the contralateral eye after trabeculectomy with mitomycin C
I Vysniauskiene, T Shaarawy, J Flammer, and I O Haefliger
Br J Ophthalmol 2005; 89: 809-811.
The visual field in toxoplasmic retinochoroiditis
M R Stanford, E A Tomlin, O Comyn, K Holland, and C Pavesio
Br J Ophthalmol 2005; 89: 812-814.
The angiopoietin/Tie-2 system in proliferative sickle retinopathy: relation to vascular endothelial growth factor, its soluble receptor Flt-1 and von Willebrand factor, and to the effects of laser treatment
J S Mohan, P L Lip, A D Blann, D Bareford, and G Y H Lip
Br J Ophthalmol 2005; 89: 815-819.
Abnormal crossing of the optic fibres shown by evoked magnetic fields in patients with ocular albinism with a novel mutation in the OA1 gene
L Lauronen, R Jalkanen, J Huttunen, E Carlsson, S Tuupanen, S Lindh, H Forsius, E-M
Sankila, and T Alitalo
Br J Ophthalmol 2005; 89: 820-824.
Human extraocular muscles in mitochondrial diseases: comparing chronic progressive external ophthalmoplegia with Leber’s hereditary optic neuropathy
A Carta, V Carelli, T D’Adda, F N Ross-Cisneros, and A A Sadun
Br J Ophthalmol 2005; 89: 825-827.
The effect of digital image resolution and compression on anterior eye imaging
R C Peterson and J S Wolffsohn
Br J Ophthalmol 2005; 89: 828-830.
The telomere of human chromosome 1p contains at least two independent autosomal dominant congenital cataract genes
J D McKay, B Patterson, J E Craig, I M Russell-Eggitt, M G Wirth, K P Burdon, A W
Hewitt, A C Cohn, Y Kerdraon, and D A Mackey
Br J Ophthalmol 2005; 89: 831-834.
Clinical science - Extended reports
Knowledge and beliefs on corneal donation in Singapore adults
Y-W Yew, S-M Saw, J C-H Pan, H-M Shen, M Lwin, M-S Yew, and W-J Heng
Br J Ophthalmol 2005; 89: 835-840.
Histopathological and immunohistochemical studies of lenticules after epikeratoplasty for keratoconus
H Nakamura, F Riley, H Sakai, W Rademaker, B Y J T Yue, and D P Edward
Br J Ophthalmol 2005; 89: 841-846.
A comparison of four methods of tonometry: method agreement and interobserver variability
P-A Tonnu, T Ho, K Sharma, E White, C Bunce, and D Garway-Heath
Br J Ophthalmol 2005; 89: 847-850.
The influence of central corneal thickness and age on intraocular pressure measured by pneumotonometry, non-contact tonometry, the Tono-Pen XL, and
Goldmann applanation tonometry
P-A Tonnu, T Ho, T Newson, A El Sheikh, K Sharma, E White, C Bunce, and D
Garway-Heath
Br J Ophthalmol 2005; 89: 851-854.
Ahmed valve drainage implant surgery in the management of paediatric aphakic glaucoma
C Kirwan, M O’Keefe, B Lanigan, and U Mahmood
Br J Ophthalmol 2005; 89: 855-858.
Outcomes in persistent hyperplastic primary vitreous
A Hunt, N Rowe, A Lam, and F Martin
Br J Ophthalmol 2005; 89: 859-863.
"Light" versus "classic" laser treatment for clinically significant diabetic macular oedema
F Bandello, A Polito, M Del Borrello, N Zemella, and M Isola
Br J Ophthalmol 2005; 89: 864-870.
Serum prorenin levels and diabetic retinopathy in type 2 diabetes: new method to measure serum level of prorenin using antibody activating direct kinetic assay
H Yokota, F Mori, K Kai, T Nagaoka, N Izumi, A Takahashi, T Hikichi, A Yoshida, F
Suzuki, and Y Ishida
Br J Ophthalmol 2005; 89: 871-873.
Classification of abnormal fundus autofluorescence patterns in the junctional zone of geographic atrophy in patients with age related macular degeneration
A Bindewald, S Schmitz-Valckenberg, J J Jorzik, J Dolar-Szczasny, H Sieber, C
Keilhauer, A W A Weinberger, S Dithmar, D Pauleikhoff, U Mansmann, S Wolf, F G
Holz for the FAM Study Group
Br J Ophthalmol 2005; 89: 874-878.
Digital imaging of the optic nerve head: monoscopic and stereoscopic analysis
J E Morgan, N J L Sheen, R V North, Y Choong, and E Ansari
Br J Ophthalmol 2005; 89: 879-884.
Expression of growth differentiation factor-5 and bone morphogenic protein-7 in intraocular osseous metaplasia
S Toyran, A Y Lin, and D P Edward
Br J Ophthalmol 2005; 89: 885-890.
The impact of the Health Technology Board for Scotland’s grading model on referrals to ophthalmology services
S Philip, L M Cowie, and J A Olson
Br J Ophthalmol 2005; 89: 891-896.
Laboratory science - Scientific reports
The effects of indocyanine green and endoillumination on rabbit retina: an electroretinographic and histological study
A K H Kwok, T Y Y Lai, C-K Yeung, Y-S Yeung, W W Y Li, and S W Chiang
Br J Ophthalmol 2005; 89: 897-900.
Microglial stability and repopulation in the retina
T A Albini, R C Wang, B Reiser, E Zamir, G S Wu, and N A Rao
Br J Ophthalmol 2005; 89: 901-903.
Laboratory science - Extended reports
TLRs and NODs mRNA expression pattern in healthy mouse eye
S Rodríguez-Martínez, M E Cancino-Díaz, L Jiménez-Zamudio, E García-Latorre, and J
C Cancino-Díaz
Br J Ophthalmol 2005; 89: 904-910.
Generation of transgenic mice with mild and severe retinal neovascularisation
C-M Lai, S A Dunlop, L A May, M Gorbatov, M Brankov, W-Y Shen, N Binz, Y KY
Lai, C E Graham, C J Barry, I J Constable, L D Beazley, and E P Rakoczy
Br J Ophthalmol 2005; 89: 911-916.
Letters
Subconjunctival corticosteroid injection for the treatment of non-necrotising anterior scleritis
H N Sen, R Ursea, R B Nussenblatt, and R R Buggage
Br J Ophthalmol 2005; 89: 917-918.
Visual field defect in association with chiasmal migration of intraocular silicone oil
D Eckle, A Kampik, C Hintschich, C Haritoglou, J-C Tonn, E Uhl, and A Lienemann
Br J Ophthalmol 2005; 89: 918-920.
Congenital hypertrophy of retinal pigment epithelium: a clinico-pathological case report
M A Parsons, I G Rennie, P A Rundle, S Dhingra, H Mudhar, and A D Singh
Br J Ophthalmol 2005; 89: 920-921.
Finding malignant change in a necrotic choroidal melanocytoma: a clinical challenge
M Kurli, P T Finger, T Manor, S A McCormick, and H E Grossniklaus
Br J Ophthalmol 2005; 89: 921-922.
Improvement after transvitreal limited arteriovenous crossing manipulation without vitrectomy for complicated branch retinal vein occlusion using 25 gauge instrumentation
R R Lakhanpal, M Javaheri, R A Equi, and M S Humayun
Br J Ophthalmol 2005; 89: 922-923.
"Ecstasy" induced immunosuppression and herpes zoster ophthalmicus
O M Zwick, D H Fischer, and J C Flanagan
Br J Ophthalmol 2005; 89: 923-924.
Reversible posterior leucoencephalopathy syndrome: a cause of temporary cortical blindness
N Niyadurupola, C A M Burnett, and L E Allen
Br J Ophthalmol 2005; 89: 924-925.
Morquio syndrome: electron microscopic findings
T Leslie, M A R Siddiqui, D A Aitken, C M Kirkness, W R Lee, and A I Fern
Br J Ophthalmol 2005; 89: 925-926.
Importance of early morning intraocular pressure recording for measurement of diurnal variation of intraocular pressure
P P Syam, I Mavrikakis, and C Liu
Br J Ophthalmol 2005; 89: 926-927.
Autoimmune retinopathy associated with intravesical BCG therapy
S Sharan, C E Thirkill, and J R Grigg
Br J Ophthalmol 2005; 89: 927-928.
Mailbox
Preoperative videotape sessions and patient satisfaction with cataract surgery
K S C Yuen, A C K Cheng, and W-M Chan
Br J Ophthalmol 2005; 89: 928.
Optical coherence tomography in photodynamic therapy
S Mennel, F Liu, and C H Meyer
Br J Ophthalmol 2005; 89: 928-929.
Optical coherence tomography of the vitreomacular interface in photodynamic therapy
A J Witkin, J S Duker, J Sahni, and S Harding
Br J Ophthalmol 2005; 89: 929.
From the library
From the Library
Br J Ophthalmol 2005; 89: 930.
Miscellanea
RP1 mutations cause autosomal recessive retinitis pigmentosa
Br J Ophthalmol 2005; 89: 824
789
EDITORIAL
Onchocerciasis
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
The order is rapidly fadin’
J D Chidambaram, T M Lietman
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Onchocerciasis and trachoma may become historical diseases within our lifetime
I n this issue of the BJO (p 796), Egbert et al utilise a case-control design to demonstrate that onchocerciasis and glaucoma are associated in an area of
Ghana. Perhaps this is not surprising, as onchocerciasis is known to cause anterior segment inflammation and peripheral anterior synechiae, which can in turn lead to increased intraocular pressure.
However, this association had never really been proved in the past, in part because reliable glaucoma data in the developing world have been difficult to come by. Interestingly, as glaucoma has become more recognised, onchocerciasis has become less so—glaucoma has moved up to number two in the WHO’s latest rankings, while onchocerciasis may have made the list for the last time at number 8 (table 1).
1 This may be the ideal time to make such an association between these two diseases when awareness of both diseases is relatively high—it would have been difficult in the past or the future.
Many factors go into the disease rankings. To some extent, they reflect the efficacy of treatment. Programmes have had remarkable success with those diseases amenable to mass drug distributions (neonatal ophthalmia, xerophthalmia, onchocerciasis, and trachoma).
In fact, onchocerciasis and trachoma may become historical diseases within our lifetime. As developing countries become wealthier with improved diet and longer life expectancies, we expect worldwide rankings to reflect diseases now found often in the developed countries.
Worldwide, diabetes is increasing at an alarming rate, and diabetic retinopathy is now fifth on the list. Older populations are more susceptible to age related macular degeneration (AMD), now third.
1 Both diabetic retinopathy and
AMD had not even appeared on previous rankings.
2 This echoes what has been previously been noted with mortality statistics, where projected worldwide rankings are similar to current rankings in developed countries.
3 Difficulties in the diagnosis of disease also come into play.
Some diseases are easily found on the external examination (trachoma), or at least with an undilated examination
(mature cataract). Others, such as glaucoma, require equipment and dilated examination—the harder people look, the more glaucoma they find. Glaucoma moved up to third in the 1990s 2 and to second in the most recent survey, 1 in part the result of better diagnosis. There are also fluctuations in the awareness and politics of disease. More than one country has been reluctant to attribute blindness to trachoma, since it had been declared eliminated in the past. To some extent, the changes in rankings reflect secular, socioeconomic trends. Trachoma is disappearing in much of the world, even in the absence of programmes specifically targeting the disease. This may be the
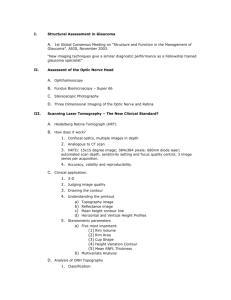
Table 1 Global blindness rankings for 1994 and 2002
Cause
6
7
4
5
2
3
1994 ranking *
1
6
7
4
5
8
2
3
2002 ranking *
1
Cataract
Trachoma
Glaucoma
Vitamin A deficiency
Trauma
Onchocerciasis
Leprosy
Cataract
Glaucoma
Age related macular degeneration
Corneal opacities
Diabetic retinopathy
Childhood blindness
Trachoma
Onchocerciasis
* Adapted from references 1 and 2.
%
47.8
12.3
8.7
5.1
4.8
3.9
3.6
0.8
41.8
15.5
13.5
1.3
1.3
0.9
0.7
result of better hygiene, fewer flies, and perhaps even widespread use of antibiotics for other purposes that incidentally cover chlamydia.
4 The rankings also reflect the vagaries of estimation. In the past decade trachoma has gone from second to seventh in the rankings, in part because of mass treatment programmes, the presence of a secular trend, and the realisation that previous estimates of the burden of trachomatous blindness were just too high.
Associations between diseases and rankings of their importance worldwide are not just curiosities. They can be of great practical importance. Programmes targeting onchocerciasis, trachoma, lymphatic filariasis, and schistosomiasis all distribute antimicrobials to large segments of the population. Groups are beginning to study how the geographical distributions of these infections overlap.
Immunisation campaigns have already demonstrated that mass administrations can be used for the delivery of other preventive health services such as vitamin A distribution. Synergy in surgical programmes may exist as well; for example, trachoma programmes often pick up more mature cataracts than trichiasis. As programmes expand, it will be important to integrate, so as not to overburden public health programmes with limited resources. Just as important is not to overburden rural, subsistence farmers with requests to attend separate onchocerciasis days, trachoma days, polio days, etc. The rankings of the major causes of blindness not only appeal to our love of lists, but also help to set priorities and demonstrate our long term successes and failures. The recent rankings may serve to alert the international community that not enough is being done for management of some diseases.
Diabetes and AMD researchers can be forgiven if they tout the newly recognised importance of their diseases in papers and grant applications. Likewise onchocerciasis and trachoma programmes can be forgiven if they take some of the credit for the decline of their diseases, and now brag that they are number 8.
Br J Ophthalmol 2005; 89 :789–790.
doi: 10.1136/bjo.2005.065847
. . . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
J D Chidambaram, T M Lietman, FI Proctor
Foundation, University of California, San
Francisco, CA, USA
T M Lietman, Institute for Global Health, and
Department of Ophthalmology, University of
California, San Francisco, CA, USA
Correspondence to: Dr Thomas M Lietman, FI
Proctor Foundation, Room 307, 95 Kirkham
Street, University of California San Francisco,
San Francisco, CA 94143-0944, USA; tml@ itsa.ucsf.edu
www.bjophthalmol.com
790
REFERENCES
1 Resnikoff S , Pascolini D, Etya’ale D, et al.
Global data on visual impairment in the year
2002.
Bull World Health Organ
2004; 82 :844–51.
EDITORIAL
2 Thylefors B , Ne´grel AD, Pararajasegaram R, et al.
Global data on blindness.
Bull World Health
Organ 1995; 73 :115–21.
3 Murray CJL , Lopez AD, eds.
The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020 .
Boston: Harvard University Press, 1996.
4 Chidambaram JD , Bird M, Schiedler V, et al.
Trachoma decline and widespread use of antimicrobial drugs.
Emerg Infect Dis
2004; 10 :1895–9.
Indocyanine green
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Let green lead not astray
J Sebag
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Trepidations of ICG use in macular hole surgery
A t the close of the 20th century the medical world was witness to a most remarkable advance when therapy was developed for a previously incurable disease. Macular hole surgery is one of the great success stories in ophthalmology, if not modern medicine.
Predicated upon an increased awareness of the role of vitreous in the pathogenesis of retinal disorders, this achievement results from the work of pioneering surgeons who had the ingenuity and courage to devise and attempt a new surgical approach that now restores vision to many grateful patients. However, recent modifications of the surgical technique may jeopardise visual outcomes and ‘‘lead us astray’’ from early successes.
Vitreous is an extended extracellular matrix, whose molecular composition and supramolecular organisation result in a clear gel that firmly adheres to the retina in youth.
1–3 Ageing induces liquefaction and vitreoretinal dehiscence, which occur concurrently in the overwhelming majority of individuals, resulting in innocuous posterior vitreous detachment (PVD).
4 Anomalous PVD results from vitreous liquefaction with-
5 out sufficient vitreoretinal dehiscence.
This may preclude the posterior vitreous cortex from separating cleanly from the internal limiting lamina (ILL) of the retina. The untoward consequences of anomalous PVD vary depending upon where in the vitreous body the gel is most liquefied and where on the retina there is greatest vitreous adherence.
5
Anomalous PVD in the periphery, for example, results in retinal tears. Along blood vessels, liquefaction without vitreoretinal dehiscence induces vitreous haemorrhage. Another important effect of anomalous PVD is vitreoschisis, a split in the posterior vitreous cortex that has been identified with biomicroscopy, 6 especially myofibroblasts, 14 resulting in a dehiscence of the central macula.
5 The importance of the posterior aspect of the posterior vitreous cortex in the pathogenesis of macular holes is underscored by the salubrious outcome when this tissue is successfully removed in its entirety.
ultrasonography, 7 tomography.
8 and optical coherence
Vitreoschisis has been confirmed by histopathological studies 9 and has also been documented during surgery by intravitreal triamcinolone injection.
10
Anomalous PVD is hypothesised to have a role in the pathogenesis of macular holes via vitreoschisis.
5 11 12
Studies have identified premacular membranes by histopathology in 73% of cases (n = 22) 13 and by stereoscopic fundus photography in 65% of eyes
(n = 224).
14 The origin of this membrane is postulated to be the outer wall of a vitreoschisis cavity in the posterior vitreous cortex, since this tissue has been identified as prefoveal vitreous by histopathology.
15 In a recent clinical study 16 of 69 cases of macular hole, optical coherence tomography detected a prefoveal membrane that could be an advanced form of the outer wall of a posterior vitreoschisis cavity. Migration of cells from the retina, such as fibrous astrocytes and Mueller cells, and recruitment of cells from the circulatory system by hyalocytes result in some degree of cellularity. New collagen (type
I) synthesis further alters the appearance of this tissue that, when it began as the outer wall of a vitreoschisis cavity, was thin, composed primarily of type II collagen, and only contained hyalocytes.
Centrifugal (outward from the fovea) traction forces are induced by the detached vitreous body, which is still attached to the peripheral circumference of the vitreoschisis cavity, where the inner and outer walls fuse into an intact posterior vitreous cortex. The extent of this anomalous PVD from the fovea has been shown to correlate with the stage of macular hole—that is, stage 2 holes have a less extensive PVD than stage 4 holes.
17 Traction by this tissue is augmented by various contractile cells,
And missing thee, I walk unseen
On the dry smooth-shaven green…
Like one that had been led astray
Through the heav’n’s wide pathless way…
John Milton, Il Penseroso [1631]
Although previously praised in print, 18 the seminal contributions of Kelly and
Wendell 19 to the treatment of macular holes cannot be overemphasised, as their pioneering work paved the way for the relatively high success rate experienced by many patients. The outer wall of the vitreoschisis cavity is usually
‘‘unseen’’ in their procedure until it is elevated off the retinal surface. While vitreous invisibility 3 is critical to its physiological function, 1–3 this poses challenges for clinical imaging.
20
Echography and optical coherence tomography often fail to identify the outer layer of a vitreoschisis cavity because it is usually thinner than the level of resolution of these techniques.
In an attempt to assure that the
‘‘unseen’’ pathogenic tissues are removed and thereby increase the rate of hole closure, surgeons began to dissect farther posteriorly and tried to remove what was thought to represent the ILL. The results from one large retrospective study, 21 comparing no ILL peel in 417 cases with ILL peeling in 175 cases found that ILL peeling increased the initial closure rate from 81% to 92% and decreased the reopening rate from
7% to 0.6%. However, there did not appear to be any difference in visual outcomes when the hole was closed by either technique. Complete ILL removal would damage Mueller cells and negatively impact upon retinal neurophysiology and vision. Thus, it is highly unlikely that the entire ILL is removed in patients who experience improved vision. Rather, the deeper dissection undertaken during attempted ILL removal most probably creates a surgical plane between the three laminae of the www.bjophthalmol.com
EDITORIAL
791
ILL, 22 leaving the innermost layer, the lamina rara externa, intact and the underlying neural retina undamaged.
In surgery, however, it is often difficult to accurately assess whether the ILL is being removed in part, in total, or at all.
Intraoperative efforts to enhance the visualisation of pathogenic tissues in macular holes led to the use of indocyanine green (ICG) dye to stain the tissue. Unfortunately, this was undertaken without any preclinical studies to determine safety and efficacy. Thus, while this ‘‘smooth-shaven green’’ approach did increase the rate of hole closure, it was associated with untoward effects on postoperative visual acuity.
23–25
That ICG was the cause of poor visual acuity in spite of hole closure was, to a degree, substantiated in a subsequent study where one of these same surgeons found that a short exposure to a lower dose of ICG was associated with improved visual acuity.
26 Why ICG was not found to be associated with poor postoperative visual acuity in other series 27 may relate to differences in surgical technique that probably employed a more shallow plane of dissection.
However, a true understanding of these discrepant findings requires a better understanding of the mechanism of
ICG toxicity.
ICG may have untoward effects via several mechanisms that are not mutually exclusive. As alluded to above, the use of ICG could result in a deeper surgical plane of dissection with damage to neural retinal elements.
Histopathological analysis of tissues removed at surgery support this postulate.
28
There may a direct toxic effect upon retinal neurons by a chemical interaction. In postmortem human eyes, ICG alone was associated with rupture of
Mueller cells and detachment of the
ILL.
29 Apoptosis was induced in human
RPE cells in culture with ICG.
30 Since
ICG is a photosensitiser, there is potential for light toxicity via a photodynamic effect. Studies 31 have shown that in the presence of ICG, light from a standard endoilluminator has a dose dependent toxicity on retinal ganglion cells in vitro.
Experiments in postmortem human eyes identified wavelengths longer than
620 nm as phototoxic, determined by light and electron microscopy.
29 However, other postmortem studies 32 in pig eyes found no such effects. The results of postmortem studies are often difficult to interpret, however, as they sometimes lead ‘‘through the heav’n’s wide pathless way,’’ and thus in vivo experimentation is needed to properly address this issue.
In this issue of the BJO (p 897) Kwok and associates in Hong Kong report the results of in vivo studies on the effects of
ICG plus endoillumination in rabbits, assessed by electroretinography (preoperatively and postoperatively) and histopathological analyses. At 1 week after surgery, there was significant reduction in the light-adapted a-wave amplitude and significant delays in the light and dark adapted b-wave latencies.
Histopathological findings included focal loss of photoreceptor outer segments, some foci of photoreceptor absence, focal oedema of the inner and outer nuclear layers, and localised areas of RPE irregularities. In the absence of a retinal break, it is surprising to find RPE and outer retinal abnormalities. Since these findings were focal in distribution, the abnormalities may have resulted from mechanical trauma (retinal elevation off the RPE) during the experimental surgery. It is well known that the rabbit vitreous is very firmly adherent to the retina. Subsequent studies must rule out any mechanical effects that might have been induced during dissection of the posterior vitreous cortex off this very adherent interface.
One possible solution would be to undertake pharmacological vitreolysis 33 34 with agents intended to lyse the vitreoretinal interface, making dissection of the posterior vitreous cortex easier with less traction upon the retina.
However, as these enzymes might introduce other effects, perhaps even artefacts, it would be simpler to employ a species with less adhesion at the vitreoretinal interface, such as the mini-pig, whose vitreoretinal interface more closely resembles that of humans.
The authors are to be thanked for contributing to our understanding of the effects of ICG upon retinal physiology and structure. As their studies were conducted in the absence of a retinal hole, the findings may also help interpret the observations of ICG toxicity in surgery for macular pucker 35 and diabetic macular oedema.
36
Br J Ophthalmol 2005; 89 :790–792.
doi: 10.1136/bjo.2005.065821
Correspondence to: J Sebag, MD, FACS,
FRCOphth, Doheny Eye Institute, University of
Southern California, and VMR Institute, 7677
Center Avenue, suite 400, Huntington Beach,
CA 92647, USA; jsebag@VMRinstitute.com
REFERENCES
1 Sebag J .
The vitreous—structure, function, and pathobiology . New York: Springer-Verlag, 1989.
2 Sebag J . The vitreous. In: Hart WM Jr, ed. In:
Adler’s physiology of the eye , ed. St Louis:
Mosby, 1992:268–347.
3 Sebag J . Vitreous–from biochemistry to clinical relevance. In: Tasman W, Jaeger EA, eds. In:
Duane’s foundations of clinical ophthalmology .
Philadelphia: Lippincott Williams & Wilkins,
2005, Vol 1, Ch 16.
4 Sebag J . Classifying posterior vitreous detachment—a new way to look at the invisible.
Br J Ophthalmol 1997; 81 :521–2.
5 Sebag J . Anomalous PVD—a unifying concept in vitreo-retinal diseases.
Graefes Arch Clin Exp
Ophthalmol 2004; 242 :690–8.
6 Kakehashi A , Schepens CL, de Sousa-Neto A, et al.
Biomicroscopic findings of posterior vitreoschisis.
Ophthalmic Surg 1993; 24 :846–50.
7 Chu TG , Lopez P, Cano MR, et al.
Posterior vitreoschisis. An echographic finding in proliferative diabetic retinopathy.
Ophthalmology
1996; 103 :315–22.
8 Carpineto P , Ciancaglini M, Aharrh-Gnama A, et al.
Optical coherence tomography imaging of surgical resolution of bilateral vitreomacular traction syndrome related to incomplete posterior vitreoschisis.
Eur J Ophthalmol 2004; 14 :438–41.
9 Schwartz SD , Alexander R, Hiscott P, et al.
Recognition of vitreoschisis in proliferative diabetic retinopathy. A useful landmark in vitrectomy for diabetic traction retinal detachment.
Ophthalmology 1996; 103 :323–8.
10 Sonoda KH , Sakamoto T, Enaida H, et al.
Residual vitreous cortex after surgical posterior vitreous separation visualized by intravitreous triamcinolone acetonide.
Ophthalmology
2004; 111 :226–30.
11 Sebag J . Vitreous anatomy and vitreo-macular interface. In: Madreperla S, McCuen B, eds. In:
Macular hole—pathogenesis, diagnosis, and treatment . Woburn, MA: Butterworth-
Heinemann, 1999:1–24.
12 Green WR , Sebag J. Vitreous and the vitreoretinal interface. In: Ryan SJ, ed. In: Retina . St
Louis: Mosby, 2001;Vol, III :1882–960.
13 Guyer DR , Green WR, de Bustros S, et al.
Histopathologic features of idiopathic macular holes and cysts.
Ophthalmology
1990; 97 :1045–51.
14 Cheng L , Freeman WR, Ozerdem U, et al.
Prevalence, correlates, and natural history of epiretinal membranes surrounding idiopathic macular holes.
Ophthalmology
2000; 107 :853–9.
15 Yooh HS , Brooks HL Jr, Capone A Jr, et al.
ltrastructural features of tissue removed during idiopathic macular hole surgery.
Am J Ophthalmol
1996; 122 :67–75.
16 Mizushima T , Uemura A, Sakamoto T.
Prefoveolar membrane in macular hole opercula formation.
Jpn J Ophthalmol 2004; 48 :478–85.
17 Ito Y , Terasaki H, Suzuki T, et al.
Mapping posterior vitreous detachment by optical coherence tomography in eyes with idiopathic macular hole.
Am J Ophthalmol 2003; 13 :351–5.
18 Sebag J . ICG-assisted macular hole surgery—too pioneering ?
(Guest editorial) Am J Ophthalmol
2004; 137 :744–6.
19 Kelly N , Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study.
Arch Ophthalmol 1991; 109 :654–9.
20 Sebag J . Seeing the invisible: the challenge of imaging vitreous.
J Biomed Opt 2004; 9 :38–46.
21 Kumagai K , Furukawa M, Ogino N, et al.
Vitreous surgery with and without internal limiting membrane peeling for macular hole repair.
Retina 2004; 24 :721–7.
22 Sebag J . Hageman GS. Interfaces.
Eur J Ophthalmol 2000; 10 :1–3.
23 Haritoglou C , Gandorfer A, Gass CA, et al.
Indocyanine green-assisted peeling of the internal limiting membrane in macular hole surgery affects visual outcome: a clinicopathologic correlation.
Am J Ophthalmol 2002; 134 :836–41.
24 Gass CA , Haritoglou C, Schaumberger M, et al.
Functional outcome of macular hole surgery with and without indocyanine green-assisted peeling of the internal limiting membrane.
Graefes Arch
Clin Exp Ophthalmol 2003; 241 :716–20.
25 Ando F , Sasano K, Ohba N, et al.
Anatomic and visual outcomes after indocyanine green-assisted peeling of the retinal internal limiting membrane in idiopathic macular hole surgery.
Am J Ophthalmol 2004; 137 :609–14.
26 Ando F , Sasano K, Suzuki F, et al.
Indocyanine green-assisted ILM peeling in macular hole surgery revisited.
Am J Ophthalmol
2004; 138 :886–7.
27 Da Mata AP , Burk SE, Foster RE, et al.
Long-term follow-up of indocyanine green-assisted peeling of the retinal internal limiting membrane during vitrectomy surgery for idiopathic macular hole repair.
Ophthalmology 2004; 111 :2246–53.
www.bjophthalmol.com
792
EDITORIAL
28 Gandorfer A , Haritoglou C, Gass CA, et al.
Indocyanine green-assisted peeling of the internal limiting membrane may cause retinal damage.
Am J Ophthalmol
2001; 132 :431–3.
29 Gandorfer A , Haritoglou C, Gandorfer A, et al.
Retinal damage from indocyanine green in experimental macular surgery.
Invest Ophthalmol
Vis Sci 2003; 44 :316–23.
30 Rezai KA , Farrokh-Siar L, Ernest JT, et al.
Indocyanine green induces apoptosis in human retinal pigment epithelial cells.
Am J Ophthalmol
2004; 137 :931–3.
31 Iriyama A , Uchida S, Yanagi Y, et al.
Effects of indocyanine green on retinal ganglion cells.
Invest
Ophthalmol Vis Sci 2004; 45 :282–6.
32 Grisanti S , Szurman P, Gelisken F, et al.
Histological findings in experimental macular surgery with indocyanine green.
Invest
Ophthalmol Vis Sci 2004; 45 :282–6.
33 Sebag J . Pharmacologic vitreolysis. (Guest editorial) Retina 1998; 18 :1–3.
34 Sebag J . Is Pharmacologic vitreolysis brewing ?
(Guest editorial) Retina , 2002; 22 :1–3.
35 Haritoglou C , Gandorfer A, Gass CA, et al.
The effect of indocyanine-green on functional outcome of macular pucker surgery.
Am J Ophthalmol 2003; 135 :328–37.
36 Ando F , Yasui O, Hirose H, et al.
Optic nerve atrophy after vitrectomy with indocyanine greenassisted internal limiting membrane peel in diffuse macular edema.
Graefes Arch Clin Exp
Ophthalmol 2004; 242 :995–9.
Vision restoration therapy
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Vision restoration therapy: confounded by eye movements
J C Horton
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Treatment claims not supported by data
not improve after vision restoration therapy when testing is done with
¨bingen automated perimetry.
3 Once again, Sabel has placed himself in the position of refuting his own work. High resolution perimety refers to the technique used by Sabel to measure the visual fields before and after vision restoration therapy.
3 Its drawback, as mentioned earlier, is poor control over eye movements. This deficiency was the reason for turning to the scanning laser ophthalmoscope in the first place.
R ecently Sabel, Kenkel, and Kasten co-authored a report showing that vision restoration therapy does not improve field defects in patients with cortical lesions.
1 This finding was a disappointment because it dashed hopes that vision restoration therapy might benefit patients who suffer visual field loss from stroke, tumour, or trauma involving the occipital lobe. In a new twist, Sabel and colleagues have now written an editorial stating that ‘‘we have no objections to the data as presented’’ (an unusual remark from the co-authors of a study), followed in the next breath by a long argument repudiating the main thrust of their report.
2 If readers are confused, they are not to blame.
Vision restoration therapy was described previously in a series of papers by
Sabel and colleagues.
3–8 In brief, it attempts to restore visual field defects by having patients practise perimetry every day at home using a software package loaded onto their personal computers. The idea is that repeated visual stimulation, especially just inside a scotoma boundary, can salvage neurons in damaged cortex at the fringe of a lesion. Sabel’s previous studies suffered from a major flaw: eye movements were not recorded or controlled. Patients with homonymous field loss often compensate by making surveillance saccades into their blind hemifield. Although
Sabel and colleagues used the blind spot position to monitor fixation, they never reported fixation losses, false positives, or false negatives in their papers. Moreover, the blind spot position is an imperfect method for detecting small saccades, and useless for fixation assessment in an eye with a temporal hemianopia.
For these reasons, most neuro-ophthalmologists were sceptical of Sabel’s claims for vision restoration therapy.
To his credit, Sabel responded by undertaking a collaborative study with scientists employing the scanning laser ophthalmoscope.
1 This instrument allows one to present stimuli while monitoring fixation with great precision. Trials in which the patient sneaks a saccade can be discarded, solving the problem of fixation instability. Under these testing conditions, Sabel and coworkers found no improvement in the visual fields after vision restoration therapy.
Sabel had hoped that proper monitoring of fixation with the scanning laser ophthalmoscope would vindicate vision restoration therapy. Instead, he saw its apparent therapeutic benefit evaporate once the artefact of eye movements was eliminated. Rather than accept this negative outcome, he has written a commentary defending vision restoration therapy and criticising the methods used in his own paper.
2 This is worthy of further comment, if only to highlight the inconsistencies behind this about face.
Sabel’s rebuttal relies on a paper in press elsewhere, showing that the same patients who failed to show improvement with the scanning laser ophthalmoscope did improve when tested with
Tu automated perimetry and high resolution perimetry.
9 It is difficult to comment on a paper that is still unpublished, but it should be recalled that Sabel has reported previously that patients with homonymous field loss do
Sabel’s data will remain uninterpretable until he adopts a technique that eliminates the artefact created by small saccades
In his editorial, Sabel reproduces a figure from his upcoming paper, comparing the fields before and after vision restoration therapy in a patient with a hemianopia.
2 Before treatment, the scanning laser ophthalmoscope shows a field cut that deviates only about half a degree from the vertical meridian. This reflects the excellent control of eye movements afforded by that technique.
mated perimetry and high resolution perimetry deviate by 1 ˚ –8 ˚ from the vertical meridian, yet they are measuring the same field defect defined by scanning laser ophthalmoscope, the gold standard. Immediately, this discrepancy should raise a warning flag. How can one define an improvement equal to only 2.5
˚ –3.5
˚ degrees azimuth, when one’s baseline measurement of the field defect is inaccurate by this amount?
Sabel’s data will remain uninterpretable until he adopts a technique that eliminates the artefact created by small saccades. Parenthetically, it should be pointed out that the figure shows an unexplained discrepancy between
Tu automated perimetry and high resolution perimetry in the elevation of the field defect before treatment.
After vision restoration therapy, Sabel shows a thin sliver of residual field loss that hugs the horizontal meridian, extending no further from the vertical meridian than it did before treatment.
He asserts that such a change following treatment could not be produced by www.bjophthalmol.com
EDITORIAL
793 undetected horizontal saccades. In this single anecdotal case he is correct, but why rely on such an indirect, inferential approach to deal with the problem of fixation control? And in this particular case, why did the field cut improve dramatically in elevation but not azimuth? Anyone familiar with the visual field map in striate cortex will be puzzled by the pattern of field improvement attributed to vision restoration therapy in this case.
Sabel asserts that field testing using the scanning laser ophthalmoscope was difficult for patients, preventing vision restoration therapy from showing any benefit. It is true that patients had to report verbally their perception of three vertically aligned targets, rather than simply push a buzzer.
1 However, there is no evidence that this requirement made their task more difficult or that it led to selective inaccuracy in the post-treatment assessment of their visual fields. It is also true that the scanning laser ophthalmoscope targets were dark against a bright background, to avoid light scatter. Sabel states that ‘‘Simultaneous stimulus discrimination and detection of negative stimuli on a bright background are probably tasks beyond the abilities of a damaged visual system.’’ In fact, cells in the visual cortex respond overall equally well to stimuli that are dark, rather than light, compared to background. The retina contains approximately equal numbers of on-centre and off-centre cells, and it is no harder for a subject to detect a dark spot than a light spot, provided the contrast is high.
The stimuli used with the scanning laser ophthalmoscope were large (0.33
˚ ) and high contrast, chosen deliberately to detect absolute scotomas (much like the
V4e stimulus of the Goldmann perimeter). Sabel states that ‘‘The SLO method appears to be insensitive to relative defects describing areas with residual function as being absolutely blind.’’ 2 In fact, the opposite is true. A technique that measures only absolute defects will characterise relative defects as normal. Sabel argues that the scanning laser ophthalmoscope missed regions of relative field depression that might have improved from vision restoration therapy. He forgets that with a cortical lesion, the first indication of recovery is provided by shrinkage of the absolute portion of the scotoma, even while the relative portion persists. To draw again an analogy with Goldmann perimetry, the V4e isoptre will sometimes expand in a recovering field defect, whereas the I2e isoptre will continue to show a defect. Thus, a technique that defines the patient’s absolute scotoma is the most sensitive to any potential improvement.
Sabel et al write that ‘‘Horton is concerned that vision restoration therapy improvements may simply be a result of placebo effect.’’ 2 That is not quite an accurate paraphrase of my position. In my editorial, I noted that patients had the subjective impression that they had benefited from visual restoration therapy, despite lack of improvement in their fields.
10 I attributed this discrepancy between negative field results and positive patient perception to a placebo effect. I expressed concern about using patient satisfaction as an outcome criterion, because patients will clamour for a treatment they believe works, even if it’s humbug.
Although neuroplasticity is active in many regions of the brain, this fact does not mean that vision restoration therapy can promote visual field recovery following lesions of the striate cortex.
Sabel notes that ‘‘normal adult subjects are capable of perceptual learning, and there is an entire body of evidence on activity dependent use and neuroplasticity, such as studies on adult receptive field expansions following retinal or brain lesions.’’ 2 These statements are true, yet when examined closely they are irrelevant to Sabel’s position.
Perceptual learning refers to the improvement in psychophysical performance that comes with practice. For example, anyone who takes a computerised visual field test a few times will show a slight improvement in retinal sensitivity. This phenomenon is well known, and must be taken into account when assessing the response to any proposed therapy, such as pressure lowering medications in glaucoma.
11 For vision restoration therapy, perceptual learning is a confounding factor that must be controlled for by incorporating a placebo arm into studies. All subjects show a slight degree of improvement with practice, whether they have had vision restoration therapy or not.
Several investigators have reported that after retinal lesions (Sabel mistakenly refers to retinal or brain lesions), cells in the visual cortex become responsive to stimulation just outside the zone of retinal damage.
12 13
The visual field does not improve, nor does the brain suffer a direct lesion.
Individual cortical cells undergo expansion of their receptive fields, without any special therapy, simply because they have lost their normal input. Sabel advocates vision restoration therapy for an utterly different scenario: the restoration of lost visual field after a lesion that has injured the brain.
Sabel reminds us that the visual system is not purely sensory, because
‘‘it utilises many cognitive mechanisms as seen, for example, in the phenomenon of physiological blindspot ‘‘filling in.’’ 2 It is unclear how the ability of the visual system to fill in blind areas is relevant here. Such areas remain blind, and subjects cannot detect visual stimulation. The fill-in phenomenon has nothing to do with the concept behind vision restoration therapy, and makes it no more plausible.
Sabel states that ‘‘the Food and Drug
Administration has cleared vision restoration therapy to be offered in the
United States and has done so in recognition of the results from the
¨bingen-Magdeburg trial.’’ 2 It is true that the FDA granted a 510 (k) clearance to NovaVision’s vision restoration therapy on 22 April 2003, in response to an application filed on 25 October 2002.
A 510 (k) clearance is required before marketing certain types of new medical devices in the United States. The applicant must demonstrate that the device is
‘‘substantially equivalent’’ to a legally marketed device introduced previously.
In this case, the predicate device was
DynaVision 2000, a similar program for treating amblyopia. A 510 (k) clearance is not based on recognition of the results of a clinical trial, and Sabel’s application to the FDA did not rely on the
Tu trial.
(Readers can judge the veracity of Sabel’s statement by inspecting his application at www.fda.gov/cdrh/pdf2/k023623.pdf)
Sabel asserts that ‘‘several clinical centres throughout the United States are now beginning to observe similar improvements with their first patients.’’ 2 The
NovaVision website features anecdotal case vignettes of patients who experienced huge recovery from scotomas, hardly representative of the mean
2.5
˚ –4.9
˚ improvement reported by Sabel in his studies.
3 9 The website also announces that NovaVision has raised
$20 million in venture capital funds to finance its expansion into the US marketplace. Sabel’s financial stake is undisclosed in all his publications.
The saga of Sabel’s visual restoration therapy provides a cautionary tale. An investigator proposes a new therapy for a condition that has no treatment. He adduces supporting evidence by carrying out a number of trials, but fails to control properly for a source of artefact. Meanwhile, he launches a commercial venture, based on his own research, and becomes financially involved. When his data are challenged, he agrees to an independent test of his therapy in collaboration with a third party. When the results prove him wrong, he rejects them. Meanwhile, trusting patients continue to sign up for the treatment programme, motivated by hope and the knowledge that nothing else is available.
www.bjophthalmol.com
Br J Ophthalmol 2005; 89 :792–794.
doi: 10.1136/bjo.2005.072967
Correspondence to: J C Horton, UCSF, San
Francisco, CA 94143, USA; hortonj@vision.ucsf.edu
REFERENCES
1 Reinhard J , Schreiber A, Schiefer U, et al.
Does visual restitution training change absolute homonymous visual field defects ?
A fundus controlled study.
Br J Ophthalmol 2005; 89 :30–5.
2 Sabel BA , Kenkel S, Kasten E. Vision restoration therapy.
Br J Ophthalmol 2005; 89 :521–4.
3 Kasten E , Wust S, Behrens-Baumann W, et al.
Computer-based training for the treatment of partial blindness.
Nat Med 1998; 4 :1083–7.
4 Kasten E , Wuest S, Sabel BA. Residual vision in transition zones in patients with cerebral blindness.
J Clin Exp Neuropsychol
1998; 20 :581–98.
5 Kasten E , Poggel DA, Muller-Oehring E, et al.
Restoration of vision II: Residual functions and training-induced visual field enlargement in braindamaged patients.
Restor Neurol Neurosci
1999; 15 :273–87.
6 Sabel BA , Kasten E. Restoration of vision by training of residual functions.
Curr Opin
Ophthalmol 2000; 11 :430–6.
7 Kasten E , Muller-Oehring E, Sabel BA. Stability of visual field enlargements following computerbased restitution training—results of a follow-up.
J Clin Exp Neuropsychol 2001; 23 :297–305.
8 Mueller I , Poggel DA, Kenkel S, et al.
Vision restoration therapy after brain damage:
Subjective improvements of activities of daily life and their relationship to visual field enlargements.
Visual Impairment Research 2003; 5 :157–78.
9 Sabel BA , Kenkel S, Kasten E. Vision restoration therapy (VRT) efficacy as assessed by comparitive perimetric analysis and subjective questionnaires.
Restor Neurol Neurosci 2005;(in press).
10 Horton JC . Disappointing results from
NovaVision’s visual restoration therapy.
Br J Ophthalmol 2005; 89 :1–2.
11 Heijl A , Bengtsson B. The effect of perimetric experience in patients with glaucoma.
Arch
Ophthalmol 1996; 114 :19–22.
12 Gilbert CD , Wiesel TN. Receptive field dynamics in adult primary visual cortex.
Nature
1992; 356 :150–2.
13 Kaas JH , Krubitzer LA, Chino YM, et al.
Reorganization of retinotopic cortical maps in adult mammals after lesions of the retina.
Science
1990; 248 :229–31.
www.bjophthalmol.com
Br J Ophthalmol 2005; 89 :795
Cover illustration
..............................................................................
Can you keep a secret
?
795
W orms seem taciturn and pedestrian, and yet these creatures may hold the secrets to the differences between the eyes of vertebrates and invertebrates. At least one rather well studied polychaete (many bristles or legs) annelid may provide the background to understanding the origins for the profound differences in ocular morphology found between chordates and non-chordates and can shed light on the question of the monophyletic versus polyphyletic appearance of eyes.
Platynereis dumerilii (closely related to our cover species— Platynereis bicaniculata ) spends its adult life in a self spun silky tube in the sublittoral zone, between the seashore and the edge of the continental shelf, and represents a frequent tasty morsel for many of the wading birds. The immature Platynereis , called atokes, are free swimming and must attach to the bottom as an adult, or epitoke, to spin a tube. The animal has lifelong development of segments and may have up to 75 segments through a process known as homonymous segmentation, each segment having a pair of appendages called parapodia.
The head, or prostomia, has peristomal cirri (specialised appendages seen on the cover image), two pairs of sensory appendages, and two pairs of eyes
These are old organisms—very old!
These animals have probably changed little since the Cambrian explosion ( BJO ,
February 2004), and may well have existed in a similar form since well before that, in the Precambrian fauna as represented in Ediacaran fossils.
Ediacaran fossils are Precambrian and are from the late Proterozoic (perhaps
600 million years ago to 543 million years ago when the Cambrian began).
The animals represented by these fossils were soft bodied and little remains of them except traces or imprints. Many of the individual traces found in the
Ediacaran fossils probably represent worms, which were early bilateralians.
Most of the other fossils of this era represent animals based on radial symmetry, such as starfish.
Bilateral symmetry is not an evolutionary ‘‘given’’ and understanding the first bilateralian will help in understanding the development of two symmetrical eyes among other features.
Molecular clock data are controversial, but hint that the first bilateralian diverged between 1.6 billion to 650 million years ago, and that represents quite a range. But, the last common ancestor of invertebrates and vertebrates (already a bilateralian) probably lived between 600–540 million years ago in the Ediacaran Precambrian.
So,
Platynereis is probably a direct descendent of the animal that immediately predated the split into vertebrates and invertebrates, and consequently, can teach us much about visual development.
The eyes of Platynereis are not complicated and are best described as pigment cups, although there is a very simple lens in front of the cups. This lens is little more than a condensation of tissue. In life, these pigmented depressions are burgundy or maroon in colour, principally because of orange visual pigment overlying more proximal black pigment in the supporting cells lining the cup. Although the eyes are interesting since they represent an early evolutionary step from eyespots to eyecups and exhibit the beginnings of a lens, the rather profound secrets of these eyes are found with the visual pigments of the prostomia, or head.
Metazoans possess basically two different types of photoreceptor cells which are divided along the lines of vertebrates and invertebrates, in general. Although both groups have transmembrane opsins permitting photoreception, invertebrates have rhabdomeric photoreceptors and vertebrates have ciliary photoreceptors. The rhabdomeric cells are microvillous cells and the visual pigment lines the numerous microvilli of the cell. In the ciliary cells, the single cilium of each cell is modified with many folds creating a stacked appearance with the photoreceptive transmembrane protein lining the infoldings of the modified cilium. The difference extends beyond the cell type and distribution of visual pigment, however, since the rhabdomeric opsin is different from the ciliary opsin.
Since Platynereis is an annelid, it is an invertebrate, and has the traditional rhabdomeric photoreceptors in all four of its eyes. Surprisingly, however, recent work shows that the ciliary cells and ciliary opsins exist within the brain somewhat more rostral and medial from the two pair of eyes (Arendt D, et al ,
Science 2004; 306 :869–71) It is doubtful whether these ciliary cells and their complement of photoreceptive pigment have any true visual function, but probably relate to setting the circadian rhythm. So, this worm has both the ciliary and rhabdomeric forms of visual pigment. But, it goes beyond this.
Vertebrates may not be so far away from these annelids after all. These same investigators suggest that the invertebrate visual pigment, opsin, is present in vertebrate eyes, albeit in the ganglion cells of the retina. That is, the rhabdomeric photoreceptive cells have been retained in the vertebrate eye in the form of retinal ganglion cells! A remnant of photoreception is present in these ganglion cells in the form of melanopsin. This ganglion cell visual pigment probably does not have a visible light function that we recognise, but may contribute to circadian rhythm control. It is also found in the pineal body and pineal eye in animals that have a pineal eye (reviewed in BJO ,
March 2005).
Interestingly, the vertebrates keep both forms of visual pigments (invertebrate and vertebrate) and have evolved an eye that unites these two different opsins from two different anatomical sources.
So, to see some of the wormy secrets of our beginnings we have only to look to our inner retina.
I R Schwab
University of California, Davis, Sacramento,
CA, USA; irschwab@ucdavis.edu
Thanks to the California Academy of Sciences for the specimen of Platynereis bicaniculata .
www.bjophthalmol.com
796
WORLD VIEW
Onchocerciasis: a potential risk factor for glaucoma
P R Egbert, D W Jacobson, S Fiadoyor, P Dadzie, K D Ellingson
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :796–798. doi: 10.1136/bjo.2004.061895
Series editors: W V Good and S Ruit
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Peter Egbert, MD,
Department of
Ophthalmology, Stanford
University School of
Medicine, Stanford Eye
Center, 900 Blake Wilbur
Drive, RoomW3002,
Stanford, CA 94305, USA; egbert@stanford.edu
Accepted for publication
1 January 2005
. . . . . . . . . . . . . . . . . . . . . . .
Background: Onchocerciasis is a microfilarial disease that causes ocular disease and blindness. Previous evidence of an association between onchocerciasis and glaucoma has been mixed. This study aims to further investigate the association between onchocerciasis and glaucoma.
Methods: All subjects were patients at the Bishop John Ackon Christian Eye Centre in Ghana, west Africa, undergoing either trabeculectomy for advanced glaucoma or extracapsular extraction for cataracts, who also had a skin snip biopsy for onchocerciasis. A cross sectional case-control study was performed to assess the difference in onchocerciasis prevalence between the two study groups.
Results: The prevalence of onchocerciasis was 10.6% in those with glaucoma compared with 2.6% in those with cataracts (OR, 4.45 (95% CI 1.48 to 13.43)). The mean age in the glaucoma group was significantly younger than in the cataract group (59 and 65, respectively). The groups were not significantly different with respect to sex or region of residence. In models adjusted for age, region, and sex, subjects with glaucoma had over three times the odds of testing positive for onchocerciasis (OR, 3.50 (95% CI 1.10 to
11.18)).
Conclusions: This study has shown a positive association between subclinical onchocerciasis and glaucoma. This finding emphasises the importance of eradication of onchocerciasis from west Africa.
A n estimated 18 million people worldwide are currently infected with onchocerciasis. Onchocerciasis is found in tropical regions, with over 99% of symptomatic cases occurring in sub-Saharan Africa, and causes blindness and visual impairment in one million to two million individuals.
1
Onchocerciasis is caused by the filarial nematode Onchocerca volvulus , which is transmitted by blackflies in the Simulium damnosum species complex. Infected people may be asymptomatic or have a pruritic skin rash, subcutaneous nodules, lymphadenopathy, or eye disease. However, little is known about the role of onchocerciasis infection in chronic progressive diseases of the eye such as glaucoma.
Ocular onchocerciasis results from an inflammatory reaction around the microfilariae. This initial punctate keratitis is reversible with treatment. Long term infection results in sclerosing keratitis and inflammation in the anterior chamber and retinal epithelium. Posterior involvement may follow, including chorioretinitis, optic neuritis, and optic atrophy.
2
Following years of exposure to the microfilariae, blindness may result.
3
In west Africa, current efforts to control onchocerciasis include the African Programme for Onchocerciasis Control, using a combined strategy of vector control and chemotherapy with ivermectin. Ivermectin has been shown to reduce or eliminate microfilariae from the eye without significant adverse reaction.
4 5 In spite of recent advances in prevention and treatment of onchocerciasis this disease continues as a significant health problem in many areas of west Africa. Until onchocerciasis is eradicated worldwide, a greater understanding of this disease and its manifestations is essential.
Clinically, onchocerciasis produces a low grade inflammation of the eye with formation of peripheral anterior synechiae.
6 7 Intraocular pressure can remain normal or even decrease in ocular onchocerciasis.
8 Pathology in infected eyes shows that although the trabecular system appears unchanged by onchocerciasis when viewed by light microscopy, the post-trabecular outflow system is affected in subjects with both glaucoma and onchocerciasis infection.
There is infiltration of inflammatory cells around Schlemm’s canal, the efferent veins, the episclera, and the vessels in
Tenon’s capsule. This inflammation could possibly raise resistance to outflow of aqueous humour. The presence of microfilariae in Tenon’s capsule serves as compelling evidence for onchocerciasis as the cause for the posttrabecular infiltrate. Furthermore, microfilariae have been found in the optic nerve sheath.
9–11 An older study found an
‘‘unexpectedly high prevalence of glaucoma’’ among patients with onchocerciasis, but the study did not contain control subjects and, therefore, could not calculate an odds ratio or control for other demographic factors to isolate the association. Additionally, the same study found that younger people with glaucoma were more likely to be infected with onchocerciasis.
12 Other studies also implicate onchocerciasis as a risk factor for optic nerve disease.
13 14 There is more glaucoma in advanced onchocerciasis where eyes tend to have uveitis, peripheral anterior synechiae, and angle closure, but not in those with mild onchocerciasis.
8 Despite a certain amount of anecdotal, epidemiological, clinical, and pathologic data, there exists only a loose association between onchocerciasis and glaucoma.
Our goal is to contribute to the existing evidence of an association between onchocerciasis and glaucoma in a cross section of patients. In this cross sectional case-control study, we therefore investigated the prevalence of onchocerciasis in patients with glaucoma compared to a control group.
METHODS
Subjects were patients of the Bishop John Ackon Christian
Eye Centre in Cape Coast, Ghana, who had advanced glaucoma and underwent a trabeculectomy or had cataracts and underwent an extracapsular cataract extraction. The cataract patients serve as controls. This study was approved by the investigational review board of the Bishop John Ackon
Christian Eye Centre in Cape Coast, Ghana. Records of consecutive patients who underwent either of the above procedures and who also had a skin snip biopsy evaluation for onchocerciasis were evaluated. The skin snip biopsy is standard protocol in the preoperative evaluation for all patients undergoing surgery at this clinic. The laboratory that performed the interpretation was unaware of the www.bjophthalmol.com
Onchocerciasis 797
Table 1 Demographic characteristics of the study population
Characteristic
Mean age
Sex
Males
Females
Ocular diagnosis
Glaucoma
Cataract
Onchocerciasis
Positive
Negative
Region
Central
Other
Western
Accra
Eastern
Northern
Brong Ahafo
Unspecified
No (%)
63.2 (SD 13.6)
138 (48.3)
148 (51.7)
94 (67.1)
192 (32.9)
15 (5.2)
271 (94.8)
136 (48.6)
106 (37.9)
17 (6.1)
10 (3.6)
10 (3.6)
1 (0.2)
6 subjects’ ocular diagnosis. Patients under the age of 20 were excluded from the study. Our final sample comprised 286 patients; Table 1 shows their demographic characteristics.
Each patient had a detailed eye examination by an ophthalmologist including visual acuity, slit lamp examination, intraocular pressure, and funduscopic examination.
Glaucoma was diagnosed by glaucomatous optic nerve cupping and intraocular pressure greater than 25 mm Hg.
Most patients had very advanced glaucoma with loss of central vision.
We used bivariate analysis to compare the prevalence of onchocerciasis in glaucoma subjects to that of cataract subjects. Further bivariate analyses investigated differences in cataract and glaucoma groups according to age, sex, and region of residence.
x
2
Analyses were used for categorical variables and t tests were used for continuous variables. Odds ratios and 95% confidence intervals were calculated. For the purposes of statistical analysis, region of residence was recoded as a dichotomous variable denoting whether a subject was from the Central Region or from any other region. Finally, to assess the validity of the relation between onchocerciasis and glaucoma we performed multivariate analysis with logistic regression to control for potential confounders. All analyses were conducted in SAS version 8.0
(SAS Institute Inc, Cary, NC, USA).
RESULTS
The prevalence of onchocerciasis was 10.6% in those with glaucoma compared with 2.6% in those with cataracts
(table 2). In bivariate analysis, those people with glaucoma had significantly higher odds of onchocerciasis than people with cataracts (OR 4.45; 95% CI 1.48 to 13.43).
Further bivariate analyses revealed that there were more women in the cataract group than in the glaucoma group, but the difference was not statistically significant. There was no difference in ethnicity between the two groups; all subjects were black Africans. A t test comparing the average age of the two groups resulted in a significant difference. The glaucoma group was younger (mean age 59 years, SD 15) than the cataract controls (mean age 65 years, SD 13) with a mean difference of 6 years (p value = 0.0003).
After adjusting for potential confounders, (age, sex, region of residence) in a multivariate logistic model, people with glaucoma remained more than three times more likely to test positive for onchocerciasis than people with cataracts
(adjusted OR 3.50; 95% CI 1.10 to 11.18). Age remained significant in the model, but sex and region of residence remained statistically insignificant in the adjusted model
(table 3).
DISCUSSION
In this study, we have found a highly significant association between onchocerciasis and glaucoma. Glaucoma and onchocerciasis are both very important health issues in sub-
Saharan Africa. Glaucoma is the second leading cause of blindness, after cataracts, and is a very difficult disease to treat.
15 Many ophthalmologists in Ghana believe that onchocerciasis is seen relatively frequently in patients with glaucoma, but the evidence for a link between the two diseases has been mixed. To our knowledge, this is the first study to show that onchocerciasis infection, even in the absence of ocular onchocerciasis, is a potential risk factor for the development of glaucoma. This is supported by previous epidemiological, clinical, and pathological data. Particularly, patients with onchocerciasis have more peripheral anterior synechiae and inflammation in the outflow system than control eyes that could cause increased resistance to aqueous humour outflow.
6 7 Furthermore, patients with advanced ocular changes from onchocerciasis have an increased prevalence of glaucoma.
8 Microfilariae have been found in the optic nerve sheath and could conceivably interfere with optic nerve blood profusion, thereby increasing the susceptibility to glaucoma.
10
The subjects in our study do not have advanced onchocerciasis eye findings; most of the subjects do not have any visible finding of eye infection on detailed ophthalmological examination. The study provides strong evidence that onchocerciasis, even in the visible absence of ocular damage, is associated with glaucoma.
A limitation of our study is that we cannot say definitively that onchocerciasis is a risk factor for glaucoma because the exposure and outcome data were collected simultaneously. A proved temporal relation of infection with onchocerciasis and
Table 2 Comparison of glaucoma and cataract groups
Variable
Mean age (SD)
Sex
Males
Females
Onchocerciasis
Positive
Negative
Region
Central
Other
Glaucoma
(n = 94)
59 (15)
53 (56.4%)
41 (43.6%)
10 (10.6%)
84 (89.4%)
50 (56.2%)
39 (43.8%)
Cataract
(n = 192)
65 (13)
85 (44.3%)
107 (55.7%)
5 (2.6%)
187 (97.4)
86 (45.0%)
105 (55.0%)
Test statistic
3.63
3.708
8.196
3.0235
p Value
0.0003
0.054
0.0042
0.0821
Odds ratio
(95 % CI)
0.61
(0.37 to 1.01)
4.45
(1.48 to 13.43)
1.57
(0.94 to 2.60) www.bjophthalmol.com
798 Egbert, Jacobson, Fiadoyor, et al
Table 3 Results of logistic regression
Variable
Onchocerciasis
Age
Region of residence
Sex
Beta (standard error)
1.25 (0.59)
2 0.04 (0.01)
2 0.65 (0.28)
2 0.61 (0.27)
Odds ratio (95% CI)
3.50 (1.10 to 11.18)
0.96 (0.94 to 0.98)
1.92 (1.11 to 3.33)
0.54 (0.32 to 0.93) development of glaucoma would give stronger evidence of causality. A frequent problem with case-control studies is that the groups compared are often not identical. This difference between groups may lead to results biased by confounding factors. We controlled for differences in common demographic factors through multivariate analysis. In our study, the cataract control group was older than the glaucoma group. However, because the likelihood of onchocerciasis infection increases with age, the older control group is likely to bias the results towards the null—that is, a better age matched control group may strengthen the association we found. Another limitation of our study is that the results may not apply exactly to other geographical areas. The severity of onchocerciasis eye disease varies from area to area. In Africa, for example, blindness is more common in the savannah and woodland areas than in forest areas. This is probably a consequence of different strains of Onchocerca volvulus .
16
Knowing that onchocerciasis is associated with glaucoma in this population strengthens the argument to eradicate onchocerciasis from the area by continuation of vector control programmes and drug treatment with ivermectin.
This is especially important in light of decreased support for onchocerciasis eradication programmes.
17 The results of this study suggest that the elimination of onchocerciasis might also reduce the incidence of glaucoma in Ghana.
ACKNOWLEDGEMENTS
We gratefully acknowledge the help of the staff of the Bishop John
Ackon Christian Eye Centre. We thank Lydia Hannah Gould for her entomological expertise.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
P R Egbert, Stanford University School of Medicine, Department of
Ophthalmology, Palo Alto, CA, USA
D W Jacobson, K D Ellingson, Yale University School of Medicine, New
Haven, CT, USA
S Fiadoyor, P Dadzie, Bishop John Ackon Christian Eye Centre, Cape
Coast, Ghana
Sponsor: This study was supported in part by the Elizabeth Butterway
Fund for ophthalmic research. None of the authors has any competing interests.
REFERENCES
1 World Health Organization .
Onchocerciasis and its control , Report of a
WHO Expert Committee on Onchocerciasis Control, 1995:1–104.
2 Newland HS , White AT, Greene BM, et al.
Ocular manifestations of onchocerciasis in a rain forest area of west Africa.
Br J Ophthalmol
1991; 75 :163–9.
3 Burnham G . Onchocerciasis.
Lancet 1998; 351 :1341–6.
4 Dadzie KY , Awadzi K, Bird AC, et al.
Ophthalmological results from a placebo controlled comparative 3-dose ivermectin study in the treatment of onchocerciasis.
Trop Med Parasitol 1989; 40 :355–60.
5 Dadzie KY , Remme J, De Sole G. Changes in ocular onchocerciasis after two rounds of community-based ivermectin treatment in a holo-endemic onchocerciasis focus.
Trans R Soc Trop Med Hyg
1991; 85 :267–71.
6 Yang YF , Cousens S, Murdoch IE, et al.
Intraocular pressure and gonioscopic findings in rural communities mesoendemic and nonendemic for onchoceriasis, Kaduna State, Nigeria.
Eye 2001; 15 :756–9.
7 Wormald R , Foster A. Clinical and pathological features of chronic glaucoma in north-east Ghana.
Eye 1990; 4 :107–14.
8 Thylefors B , Duppenthaler JL. Epidemiological aspects of intraocular pressure in an onchocerciasis endemic area.
Bull World Health Organ
1979; 57 :963–9.
9 Rodger F . The pathogenesis and pathology of ocular onchocerciasis.
Am J Ophthalmol 1960; 49 :560–594.
10 Paul EV , Zimmerman LE. Some observations on the ocular pathology of onchocerciasis.
Hum Pathol 1970; 1 :581–94.
11 Stilma JS . Onchocerciasis and glaucoma: ophthalmo-pathological aspects of the limbus and Tenon’s capsule in 25 surgical patients from Ghana.
Doc
Ophthalmol 1981; 50 :327–35.
12 Berghout E . Onchocerciasis and glaucoma in the forest area of Ghana.
Trop
Geogr Med 1973; 25 :233–7.
13 Abiose A , Murdoch I, Babalola O, et al.
Distribution and aetiology of blindness and visual impairment in mesoendemic onchocercal communities,
Kaduna State, Nigeria. Kaduna Collaboration for Research on
Onchocerciasis.
Br J Ophthalmol 1994; 78 :8–13.
14 Cousens SN , Yahaya H, Murdoch I, et al.
Risk factors for optic nerve disease in communities mesoendemic for savannah onchocerciasis, Kaduna State,
Nigeria.
Trop Med Int Health 1997; 2 :89–98.
15 Egbert PR . Glaucoma in west Africa: a neglected problem.
Br J Ophthalmol
2002; 86 :131–2.
16 Anderson J , Fuglsang H. Ocular onchocerciasis.
Trop Dis Bull
1977; 74 :257–72.
17 Stevenson P . Vision is failing for river-blindness control in Ghana.
Lancet
1999; 354 :2143.
www.bjophthalmol.com
799
SCIENTIFIC REPORT
Visual loss following removal of intraocular silicone oil
S Cazabon, C Groenewald, I A Pearce, D Wong
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :799–802. doi: 10.1136/bjo.2004.053561
Aim: To investigate the cause of visual loss following removal of intraocular silicone oil in patients who underwent vitrectomies for retinal detachment or giant retinal tear.
Methods: The clinical records of three cases with visual loss following removal of silicone oil were reviewed. Investigations carried out included fundus fluorescein angiogram, optical coherence tomography, and electrophysiological studies.
Results: Visual acuities dropped from 6/9 to 6/36 in two cases and 6/24 to 3/24 in the third. None of the three cases had macula detachment at any stage. Fundus fluorescein angiogram and optical coherence tomography were normal in all cases. Pattern electroretinogram showed reduced amplitudes of the P50 and N95 components. Multifocal electroretinogram indicated a selective damage to the central part of the macula.
Conclusions: The results suggest that the abnormality arises predominantly in the central part of the macula, especially the outer and middle layers. However, the exact mechanism still remains obscure.
S ilicone oil has a well established role in vitreoretinal surgery. With the improvement of microsurgical techniques, silicone oil has been successfully used in the management of complicated retinal detachments associated with proliferative vitreoretinopathy, giant retinal tears, proliferative diabetic retinopathy, severe trauma, and cytomegalovirus related retinal detachments.
1–5 It provides prolonged intraocular tamponade and because of its optical clarity, it allows for adequate postoperative assessment.
‘‘Unexplained’’ visual loss is a rare complication following oil removal. It has hitherto not been reported in the literature to the best of our knowledge, although oral case presentations have been made at successive meetings of the British and Eire Association of Vitreoretinal Surgeons (BEAVRS). We recently encountered three cases and decided to carry out special investigations to elucidate the nature and cause of the visual loss.
MATERIALS AND METHODS
We reviewed the clinical records of three cases with visual loss following removal of intraocular silicone oil 5700 centistokes (Oxane 5700, Bauch & Lomb). All three patients underwent uncomplicated pars plana vitrectomy and silicone oil injection for retinal detachments or giant retinal tear.
Hartman’s solution was used in exchange at the time of oil removal in each case. All three patients had optical coherence tomography (OCT) measurements of the central macula postoperatively. The OCT 3000 (Zeiss-Humphrey, USA) was used for the topographic mapping.
Horizontal line scans through the fovea of default length
5 mm at 0 ˚ and a fast macula thickness map consisting of six
6 mm radial line scans centred on fixation were obtained.
Full field electroretinograms (ERGs) were obtained following the International Society of Clinical Electrophysiology of
Vision (ISCEV) standards. Multifocal electroretinogram
(mfERG) recorded binocularly with a stimulus size of 61 hexagons using the RETI scan system (Roland Consult,
Wiesbaden, Germany) was used to assess macula function.
Pupils were dilated and refractive errors were corrected in each case. The stimulus was at a distance of 380 mm from the patient’s eye so that a field of 20 degree radius in 61 segments was stimulated. The patient fixated on the centre of a large diagonal cross, centred at the central hexagon. Each recording session consisted of eight trials over approximately
15 minutes. All three patients are still attending our clinic.
Patients 1 and 2 have been attending for at least 2 years and patient 3 for 1 year.
CASE 1
A 45 year old myopic male patient presented with a 1 week history of floaters in his right eye. He was otherwise fit and healthy. On examination, his corrected visual acuity was right eye 6/5, left eye 6/5. The anterior segment was normal in both eyes. Funduscopy of his right eye showed a giant retinal tear in the nasal aspect involving about 5 clock hours. The disc was normal and the macula was attached.
He underwent an uncomplicated three port pars plana vitrectomy and silicone oil injection under local anaesthetic the following morning. One week later his visual acuity was 6/9
+ 3 in the right eye and the IOP was 23 mm Hg. At the 3 month postoperative visit, the visual acuity dropped to
6/12 but he was noted to have a posterior subcapsular cataract.
One month later the silicone oil was removed, combined with phacoemulsification and intraocular lens (IOL) implantation under local anaesthetic. The surgery was uneventful, but a few days afterwards he complained of seeing a black shadow in the central aspect of his right eye. The unaided visual acuity was 1/60 improving to 6/36 on refraction. The anterior segment was normal and the IOP was 18 mm Hg in his right eye. Funduscopy revealed a healthy disc and normal looking macula with a flat retina.
Fundus fluorescein angiogram (FFA) and OCT did not reveal any abnormalities.
Pattern electroretinogram (PERG) was normal in both eyes but the right eye had smaller responses than the left eye.
Both the P50 and N95 amplitudes were reduced in the right eye (see table 1). Standard flash ERG in light background revealed delayed latency in the right eye compared to the left.
The oscillatory potential also showed reduced amplitude in the right eye compared to the left eye. MfERG indicated a well define hill of vision in the left eye but a more plateau effect in the right eye (see figs 1 and 2). The flash visual
Abbreviations: FFA, fundus fluorescein angiogram; IOL, intraocular lens; mfERG, multifocal electroretinogram; OCT, optical coherence tomography; PERG, pattern electroretinogram; VEP, visual evoked potential www.bjophthalmol.com
800 Cazabon, Groenewald, Pearce, et al
Figure 1 Multifocal ERG responses comparing affected right eye with unaffected left eye: case 1.
evoked potential (VEP) showed normal responses in both eyes.
CASE 2
A 55 year old myopic male presented with a 2 day history of reduced vision and floaters in his right eye. His visual acuity was 6/60 in the right eye and 6/5 in the left eye. The anterior segment was normal but he had a moderately dense vitreous haemorrhage in his right eye. Funduscopy revealed a superior bullous macula on retinal detachment and lattice degeneration with three tears superiorly and two inferiorly. He underwent a three port pars plana vitrectomy and silicone oil injection under local anaesthetic on the same day. The following day his visual acuity improved to 6/9
+ 3 in the right eye. The IOP was 20 mm Hg and funduscopy showed a flat retina. About 5 months later, the silicone oil was removed, combined with phacoemulsification and IOL implantation under local anaesthetic because of the formation of a cataract.
One week after surgery he complained of blurred vision in his right eye. The IOP was normal and funduscopy showed a flat retina with a normal looking disc and macula. His best corrected visual acuity was 6/36 in the right eye. OCT of his right eye was normal.
The amplitudes of the P50 and N95 waves were small in both eyes, but even smaller in the affected eye compared to the unaffected eye (see table 1). ERG tests including standard and dim flash in the dark and white flash in light background produced smaller amplitudes and delayed responses in the right eye compared to the left eye. Multifocal ERG again indicated reduced central macula function in the right eye.
The flash VEP was obtained and the responses were normal in both eyes.
CASE 3
A 42 year old myopic male complained of flashing lights and seeing a shadow in the lateral aspect of his left eye for 2 days.
His left eye was known to be amblyopic. On examination his corrected visual acuity was 6/9 in the right eye and 6/18 in the left. Funduscopy of his left eye showed a bulbous detachment involving the nasal half of the retina with two large breaks.
The macula was not involved. The next day he underwent an uncomplicated three port pars plana vitrectomy, cryotherapy to the breaks, and silicone oil injection under general anaesthesia. His visual acuity with the silicone oil in the left eye was 6/24 at 1 week postoperatively. The silicone oil was removed under a local anaesthetic 3 months after the vitrectomy.
One week later his visual acuity was reduced to 1/60 in the left eye. Clinical examination did not reveal any abnormal findings to account for his reduced vision. The retina was flat and the optic disc and macula appeared normal. His best corrected visual acuity was 3/24 in the left eye. OCT of his left eye did not reveal any abnormalities.
Pattern ERG showed markedly reduced amplitudes of the
P50 and N95 as well as increase latencies in the left eye (see table 1). Responses in the right eye were normal. Photopic
ERG revealed smaller amplitudes and delayed latency from the left eye to both standard flash and 30 Hz flicker stimulation. Multifocal ERG showed substantially reduced central macula function in the left eye compared to the right eye (see fig 3). The flash VEP revealed good amplitudes in both eyes.
DISCUSSION
Complications associated with the removal of silicone oil are well documented and include re-detachment, hypotony, expulsive haemorrhage, and vitreous haemorrhage.
6 We investigated three patients with ‘‘unexplained’’ visual loss following silicone oil removal.
Electrodiagnostic studies offer an objective method of assessing the visual pathway from the retina to the visual cortex. The results could be used to determine the location and possible nature of various dysfunctions along the pathway. It also provides information about the involvement of particular retinal cell types.
The PERG provides useful information in the distinction between optic nerve disease and macula disease in patients with poor central visual acuity. The N95 component reflects ganglion cell function where as the P50 component arises predominantly from the macula photoreceptors, horizontal, bipolar, and amacrine cells.
7
In all three cases (especially cases 1 and 3) the PERG revealed increased latency and reduced amplitude of the P50 component with concomitant decreased amplitude of the
N95 component in the affected eye. This is in keeping with abnormalities of the macula photoreceptors and middle layer function. In case 2, the PERG was reduced in both eyes which is presumably related to myopic degeneration. The mfERG showed a well defined hill of vision in the unaffected eye and a plateau effect in the affected eye indicating impaired
Table 1 Comparison of the electrophysiological responses between the normal and affected eye in all three cases
ERG test
30 Hz flicker amplitude ( m V)
30 Hz flicker latency (ms)
P50 ( m V)
N95 ( m V)
Case 1
Affected eye
85.0
29.0
2.92
5.27
Normal eye
106.0
26.0
4.00
7.91
Case 2
Affected eye
65.0
30.0
1.16
2.44
Normal eye
90.0
29.0
1.46
2.53
Case 3
Affected eye
50.0
34.0
0.94
1.04
Normal eye
80.0
30.0
2.91
3.97
ERG, electroretinogram.
www.bjophthalmol.com
Visual loss following removal of intraocular silicone oil 801
Figure 2 Multifocal ERG responses comparing affected right eye with unaffected fellow eye: case 1.
Figure 3 Multifocal responses comparing unaffected right eye with affected left eye: case 3.
macula function in that eye (especially in cases 1 and 3).
Additionally, it is the central ring that is affected more so than the outer ring, indicating a selective and severe damage to the fovea above and beyond what might be attributable to the original retinal damage (all three patients did not have any macula detachment at any stage and had good visual acuities following vitrectomies). The amplitudes of the four
ERG flash tests were reduced in the affected eye compared to the unaffected. The flash VEPs were normal in all cases indicating that the visual pathways from the optic nerve onward remained intact.
Our results did not show any anatomical pathology to explain the drop in visual acuities. OCT was normal in each case. PERG, and particularly mfERG, does suggest that the dysfunction arises predominantly in the central part of the macula, involving mainly the outer and middle layers of the retina. The close temporal relation between oil removal and sudden visual loss suggests an event occurring during or soon after surgical intervention. The exact nature of the pathology remains obscure but is most likely related to physiochemical changes surrounding the event.
buffer the extracellular potassium ion concentration by siphoning excess K
+ ions into the vitreous.
8–10 In normal eyes
K
+ buffering is dependent on the vitreal sink and also retinal capillaries.
8
When vitreous is replaced by silicone oil efficient buffering of intraretinal increases of K
+ ions is achieved by the aqueous fluid between the oil and the retina. We can speculate that www.bjophthalmol.com
802 Cazabon, Groenewald, Pearce, et al when the oil is removed there is a sudden dramatic physiochemical alteration in the aqueous milieu (potassium, glucose, depolarising transmitter molecules, and pH) resulting in impaired buffering of K
+ ions. Such increases of K
+ ions in the retina in turn, induce excitotoxicity and eventual neuronal cell damage, an effect similar to that described by
Winter et al .
11 It is also possible that an alteration in blood perfusion to the retina at the time of silicone oil removal may be a contributing factor. Another possible cause for visual loss could be the harmful effects of soluble growth factors and free radicals. Removing the oil, which acts as a physical barrier to these substances, allows more widespread dispersal and possibly damage to the macula as a result of accumulation at this site.
While retinal tamponade with intravitreal silicone oil is an effective method of treatment for complicated retinal detachments, its removal may be associated with the potential for retinal damage, from an as yet unidentified mechanism.
ACKNOWLEDGEMENT
We thank Richard Hagan of the Department of Clinical Engineering at the Royal Liverpool University Hospital, who carried out and provided the interpretation of the electrophysiological studies.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
S Cazabon, C Groenewald, I A Pearce, D Wong, St Paul’s Eye Unit,
Royal Liverpool University Hospital, Liverpool, UK
Correspondence to: Sunildath Cazabon, St Paul’s Eye Unit, Royal
Liverpool University Hospital, Prescott Street, Liverpool, L7 8XP, UK; jcazabon@hotmail.com
Accepted for publication 11 November 2004
REFERENCES
1 Azen SP , Scott IU, Flynn HW, et al.
Silicone oil in the repair of complex retinal detachments. A prospective observational multicentre study.
Ophthalmology
1998; 105 :1587–97.
2 Camacho H , Bajaire B, Mejia LF. Silicone oil in the management of giant retinal tears.
Ann Ophthalmol 1992; 24 :45–9.
3 Alexandridis E . Silicone oil tamponade in the management of severe haemorrhagic detachment of the choroids and ciliary body after surgical trauma.
Ophthalmologica 1990; 200 :189–93.
4 Federman JL , Schubert HD. Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery.
Ophthalmology
1988; 95 :870–5.
5 Lim JI , Enger C, Haller JA, et al.
Improved visual results after surgical repair of cytomegalovirus-related retinal detachments.
Ophthalmology
1994; 101 :264–9.
6 Casswell AG , Gregor ZT. Silicone oil removal. II. Operative and postoperative complications.
Br J Ophthalmol 1987; 71 :898–902.
7 Holder GE . Significance of abnormal pattern electroretinography in anterior visual pathway dysfunction.
Br J Ophthalmol 1987; 71 :166–71.
8 Newman EA . Distribution of potassium conductance in mammalian Mu¨ller
(glial) cells: a comparative study.
J Neurosci 1987; 7 :2423–32.
9 Newman EA , Frambach DA, Odette LL. Control of extracellular potassium levels by retinal glial cell K + siphoning.
Science 1984; 225 :1174–5.
10 Oakley B , Katz BJ, Xu Z, et al.
Spatial buffering of extracellular potassium by
Mu¨ller (glial) cells in the toad retina.
Exp Eye Res 1992; 55 :539–50.
11 Winter M , Eberhardt W, Scholz C, et al.
Failure of potassium siphoning by
Mu¨ller cells. A new hypothesis of perfluorocarbon liquid-induced retinopathy.
Invest Ophthalmol Vis Sci 2000; 41 :256–61.
bmjupdates
+ bmjupdates + is a unique and free alerting service, designed to keep you up to date with the medical literature that is truly important to your practice.
bmjupdates + will alert you to important new research and will provide you with the best new evidence concerning important advances in health care, tailored to your medical interests and time demands.
Where does the information come from ?
bmjupdates + applies an expert critical appraisal filter to over 100 top medical journals
A panel of over 2000 physicians find the few ’must read’ studies for each area of clinical interest
Sign up to receive your tailored email alerts, searching access and more… www.bmjupdates.com
www.bjophthalmol.com
803
SCIENTIFIC REPORT
Decreased tear lipocalin concentration in patients with meibomian gland dysfunction
M Yamada, H Mochizuki, M Kawai, K Tsubota, T J Bryce
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :803–805. doi: 10.1136/bjo.2004.055822
Background/aim: Recent studies have demonstrated that tear lipocalin (TL) and phospholipids have a crucial role in maintaining tear film stability. The level of TL in patients with meibomian gland dysfunction (MGD) was examined and these data were correlated with the severity of their clinical disorder.
Methods: 12 patients with obstructive MGD, 12 patients with seborrhoeic MGD, and 12 age matched normal control subjects participated in this study. 3 m l of unstimulated tears were collected with a micropipette from the inferior tear meniscus in the right eye of all subjects. Tear samples were fractionated by high performance liquid chromatography, and TL concentrations were assayed with a bicinchoninic acid technique.
Results: The mean concentration of TL in patients with obstructive and seborrhoeic MGD was significantly lower than in normal controls. TL concentration correlated positively with tear film break up time and negatively with fluorescein staining scores.
Conclusion: These results suggest that TL deficiency may be a predisposing factor for the manifestation of symptoms in
MGD.
T ear lipocalin (TL), formerly called tear specific prealbumin, comprises 15–33% of the mass of protein in tears.
1
TL is a member of the lipocalin superfamily that is produced in the lacrimal gland as well as in von Ebner’s gland.
2–4 A number of lipophilic substances of different chemical classes, including fatty acids, fatty alcohols, phospholipids, glycolipids and cholesterol, are endogenous ligands of this protein.
5 6 Although the physiological roles of
TL are not fully understood, recent studies have demonstrated that the low surface tension of tears is the result of a complex of TL with tear lipids.
7 8 Glasgow et al have stated that TL may be a key factor in maintaining tear film stability by acting as a lipid scavenger.
7 This protective function of TL may be compromised in dry eye syndrome.
9
Meibomian gland dysfunction (MGD), a common, chronic condition of the posterior eyelids, comprises a significant part of dry eye syndrome.
10–12 The lipid layer, the outermost layer of the tear film produced by the meibomian glands, stabilises tear films by retarding evaporation and lowering surface tension. The compositional changes in lipids of meibum (that is, an increase in polar lipids) in MGD compromise tear film stability, which is clinically manifest as a shortened tear film break up time.
12
The symptoms of MGD are non-specific and often similar to those of aqueous deficiency dry eye.
11 12 An important clinical feature of MGD is that findings on examination of the lid margin often do not correlate well with the severity of symptoms.
12 MGD is frequently associated with lacrimal insufficiency, and patients with both conditions are likely to be particularly symptomatic. These observations may suggest the presence of pathogenic factor(s) other than changes in the meibomian glands. In this study, we examined TL concentration in patients with MGD and correlated these results with the severity of their clinical disorder.
SUBJECTS AND METHODS
Twenty four patients with symptomatic MGD participated in this study. Diagnoses included obstructive MGD in 12 subjects (six female and six male, average age 67.8 (SD
11.5) years, and seborrhoeic MGD in 12 subjects (seven female and five male, age 62.4 (11.3) years). The diagnosis of obstructive MGD was made based on the presence of plugging of the meibomian gland orifices associated with thickened, erythematous eyelid margins. For the assessment of the meibomian gland orifices, digital pressure was applied on the upper tarsus. When cloudy meibum was expressed with more than moderate pressure, or when meibum could not be expressed even with the hard pressure, the diagnosis of obstructive MGD was confirmed. Seborrhoeic MGD was diagnosed based on the excessive expression of meibum, sometime associated with foam along the lateral lower eyelid margin. Twelve age matched normal subjects (six female and six male, age 61.0 (8.9) years) were used as normal controls.
Most patients had been treated with preservative free artificial tears and/or hyaluronic acid eye drops. Patients using antibiotic eye drops or steroidal eye drops at the time of study, or who had a history of ocular surgery, were excluded.
The principles of the World Medical Association Declaration of Helsinki were followed. Each subject received a full explanation of the study, all procedures involved in the study, and provided written informed consent before enrolment. Approval for this investigation was granted by the committee for the protection of human subjects at the Keio
University School of Medicine.
Non-masked observers performed a routine ocular examination on all subjects, followed by an examination of the ocular surface, including Schirmer testing, a cotton thread test, vital staining, and measurement of tear film break up time (BUT). For vital staining, 2 m l of a saline solution containing 1% fluorescein and 1% rose bengal was used.
13
Results were assessed semiquantitatively using a 0–9 grading scale for fluorescein staining in the cornea and for rose bengal staining in both the cornea and conjunctiva.
13 14 Tear film BUT was measured three times, and the measurements were averaged. Only the right eye of all subjects was used for analysis.
A volume of 3 m l of unstimulated tears were collected with a micropipette from the inferior tear meniscus in the right eye of all subjects on a separate day. Samples were stored at
2 80 ˚ C until assay. A volume of 1 m l of each tear sample was
Abbreviations: BCA, bicinchoninic acid; BUT, break up time; MGD, meibomian gland dysfunction; TL, tear lipocalin www.bjophthalmol.com
804 Yamada, Mochizuki, Kawai, et al
0
1
2
3
10 20
Elution time (min)
30
Figure 1 High performance liquid chromatography of tear proteins. The retention times of lactoferrin (1), tear lipocalin (2), and lysozyme (3) were
6.4 minutes, 10.8 minutes, and
14.1 minutes, respectively.
fractionated by high performance liquid chromatography
(HPLC).
15 The determination of peaks in HPLC was carried out by using standards of lactoferrin, albumin, and lysozyme
(Sigma, St Louis, MO, USA) based on the report of Baier et al .
15 The elution was performed using a TSK 3000SWxl column (Tosoh Inc, Tokyo, Japan) with a mobile phase of
0.5 M sodium chloride and 0.1 M sodium phosphate, pH 5.0.
The flow rate was 0.7 ml/min and detection was performed using a ultraviolet detector set at 230 nm. The fractions containing TL were collected, and then concentrated by evaporation under nitrogen gas. The amount of TL was determined by a bicinchoninic acid (BCA) method. Total protein concentration was also determined by a BCA method using a 1 m l tear sample. The final results are expressed as mg/ml.
RESULTS
The chromatograms demonstrated excellent separation of TL from other proteins, and were free from interference by endogenous compounds. A typical chromatogram is shown in figure 1. The retention time of TL was 10.8 minutes.
TL concentration, total protein concentration, and the results of ocular surface examination are shown in table 1.
The mean concentration (SD) of TL in patients with obstructive MGD and seborrhoeic MGD was 0.89 (0.19) mg/ ml, and 1.05 (0.22) mg/ml, respectively. In both groups, mean
TL concentration was significantly lower than that of normal controls (p = 0.00021 and p = 0.00042, respectively, Mann-
Whitney U test). There were no significant differences in total protein concentration among the three groups.
TL concentrations were not significantly correlated with the results of the Schirmer or cotton thread tests, or with the
6
4
2
0
0
14
12
10
8
0.5
1 1.5
Tear lipocalin concentration (mg/ml)
2
Figure 2 Tear lipocalin concentration was significantly correlated with tear film break up (BUT) time ( r = 0.67, p = 7.8
6 10 2 6 ).
rose bengal staining score, but did correlate positively with tear film BUT ( r = 0.67, p = 7.8
6 10
2 6 staining scores ( r = 2 0.74, p = 1.8
6 10
; fig 2) and fluorescein
2 7
; fig 3).
DISCUSSION
In this study, we have shown that mean TL concentrations in patients with MGD were significantly lower than concentrations in normal controls. This is not likely to be due to decreased tear secretion, because the same volume of tears was collected from all subjects, and the total tear protein concentration did not differ among patients with MGD and normal controls. Regression analyses revealed that TL concentrations were positively correlated with tear film BUT and negatively correlated with fluorescein staining scores.
These results suggest that decreased TL concentration is associated with tear film instability and a more severe clinical manifestation of MGD.
3
2
5
4
1
7
6
9
8
0
0 0.5
1 1.5
Tear lipocalin concentration (mg/ml)
2
Figure 3 Tear lipocalin concentration was significantly negatively correlated with fluorescence score ( r = 2 0.74, p = 1.8
6 10 2 7 ).
Table 1 Tear lipocalin concentration, total protein concentration, and results of ocular surface examination (SD)
Schirmer test (mm)
Cotton thread test (mm)
Tear film BUT (s)
Fluorescein score
Rose bengal score
Tear lipocalin (mg/ml)
Total protein (mg/ml)
Obstructive MGD
5.4 (2.1)
10.4 (4.3)
4.4 (1.7)
1.7 (1.5)
0.5 (0.7)
0.89 (0.19) *
8.66 (1.50)
Seborrhoeic MGD
6.4 (2.3)
12.7 (4.9)
4.9 (2.1)
0.9 (1.1)
0.5 (0.6)
1.05 (0.22) **
9.16 (1.76)
Normal controls
8.5 (3.2)
13.7 (3.1)
7.9 (1.9)
0
0.1 (0.3)
1.54 (0.23)
9.48 (1.72)
MCD, meibomian gland dysfunction.
The concentration of lipocalin in patients with obstructive MGD and seborrhoeic MGD was significantly lower than that of normal controls ( * p = 0.00021 and ** p = 0.00042, respectively).
www.bjophthalmol.com
Tear lipocalin and meibomian gland dysfunction
Recent studies have demonstrated that TL contributes to the high, non-Newtonian viscosity of tear film and its low surface tension.
7 8 These actions are thought to be exerted by the lipid binding properties of TL. In the lipocalin family, TL is unique because it binds most strongly the least soluble lipids.
5 6 In seborrhoeic MGD, excessive expression of meibum results in excessive concentrations of lipids in tear film. TL may contribute to tear film stability by acting as a lipid scavenger.
7 In obstructive MGD, low levels of two phospholipids, phosphatidylethanolamine, and sphingomyelin are associated with ocular surface abnormalities.
16 TL may adjust the lipid composition of tears by binding lipids from the tear fluid and/or releasing lipids into tear fluid. Intensive analysis of lipids compositions of tears and meibum from patients with MGD appears to be essential to test the hypothesis.
Lechner et al have recently reported that the expression of
TL in tetracarcinoma derived NT2 precursor cells is enhanced by oxidative stress and that TL binds to several lipid peroxidation products.
17 These observations suggest that TL acts as a physiological epithelial protective factor by scavenging potentially harmful lipid peroxidation products. TL also has anti-inflammatory and antimicrobial activity.
18 19 It may exert a regulatory, dampening influence on the inflammatory cascade, thereby protecting against tissue damage from excessive inflammation. The negative correlation between
TL concentration and fluorescein staining scores in the present study may be explained by the protective role of TL.
As mentioned in the introduction, findings on examination of the lid margin often do not correlate well with the severity of symptoms in patients with MGD.
12 MGD is frequently associated with lacrimal insufficiency, and patients with both conditions are likely to be particularly symptomatic. Our results suggest that decreased TL concentration in tears is one of the pathogenic factors other than changes in the meibomian glands for the development of clinical symptoms in MGD. Further investigations are required to determine the mechanism by which TL exerts protective effects on the ocular surface (that is, stabilising tear film by modulation of tear lipids, scavenging lipid peroxidation products, or regulating excessive inflammation).
To date, however, only a few investigators have reported pathophysiological changes in TL concentrations. The level of
TL remains constant in non-stimulated and stimulated tears of normal subjects.
20 In soft contact lens wearers, the level of lipocalin in tears was significantly higher than that of normal controls.
21 Intolerant contact lens wearers had significantly higher amounts of lipocalin in their tears than tolerant contact lens wearers.
22 These observations appear to conflict with the proposed protective role of TL in maintaining tear film stability and epithelial integrity. However, Glasson et al have speculated that the greater concentration of TL observed in tears from intolerant contact lens wearers may be a response to increased lipid peroxidation products.
22 Further studies should be done to clarify this issue.
In summary, mean TL concentration was significantly lower in patients with MGD than in normal control subjects.
TL concentrations correlated positively with tear film BUT and negatively with fluorescein staining scores. Our results suggest that a deficiency of TL may be a predisposing factor for the development of clinical symptoms in MGD.
805
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
M Yamada, H Mochizuki, M Kawai, K Tsubota, Department of
Ophthalmology, Keio University School of Medicine, Tokyo, Japan
M Yamada, H Mochizuki, Division for Vision Research, National
Institute of Sensory Organs, National Tokyo Medical Center, Tokyo,
Japan
T J Bryce, Department of Health Sociology, Tokyo University Graduate
School of Medicine, Tokyo, Japan
The authors have no proprietary interest in any materials in this manuscript.
Correspondence to: Masakazu Yamada, MD, Division for Vision
Research, National Institute of Sensory Organs, National Tokyo Medical
Center, 2-5-1 Higashigaoka, Meguro, Tokyo 152-8902, Japan; yamadamasakazu@kankakuki.go.jp
Accepted for publication 6 October 2004
REFERENCES
1 Fullard RJ , Kissner DM. Purification of the isoforms of tear specific prealbumin.
Curr Eye Res 1991; 10 :613–28.
2 Inada K . Studies of human tear proteins. 3. Distribution of specific tear prealbumin in lacrimal glands and other adnexa.
Jpn J Ophthalmol
1984; 28 :315–30.
3 Bla¨ker M , Kock C, Ahlers C, et al.
Molecular cloning of human von Ebner’s gland protein: a member of the lipocalin superfamily highly expressed in lingual salivary gland.
Biochim Biophys Acta 1993; 1172 :131–7.
4 Redl B , Holzfeind P, Lottspeich F. cDNA cloning and sequencing reveals tear lipocalin to be a member of the lipophilic-ligand carrier protein superfamily.
J Biol Chem 1992; 267 :20282–7.
5 Glasgow BJ , Abduragimov AR, Farahbakhsh ZT, et al.
Tear lipocalins bind a broad array of lipid ligands.
Curr Eye Res 1995; 14 :363–72.
6 Gasymov OK , Abduragimov AR, Yusifov TN, et al.
Binding studies of tear lipocalin: the role of the conserved tryptophan in maintaining structure, stability and ligand affinity.
Biochim Biophys Acta 1999; 1433 :307–20.
7 Glasgow BJ , Marshall G, Gasymov OK, et al.
Tear lipocalins: potential lipid scavengers for the corneal surface.
Invest Ophthalmol Vis Sci
1999; 40 :3100–7.
8 Nagyova´ B , Tiffany JM. Components responsible for the surface tension of human tears.
Curr Eye Res 1999; 19 :4–11.
9 Schoenwald RD , Vidvauns S, Wurster DE, et al.
Tear film stability of protein extracts from dry eye patients administrated a sigma agonist.
J Ocul
Pharmacol Ther 1997; 13 :151–61.
10 Bron AJ , Tiffany JM, Gouveia SM, et al.
Functional aspects of the tear film lipid layer.
Exp Eye Res 2004; 78 :347–60.
11 Bron AJ , Tiffany JM. The contribution of meibomian disease to dry eye.
Ocular
Surface 2004; 3 :149–64.
12 Driver P , Lemp MA. Seborrhea and meibomian gland dysfunction. In:
Krachmer JH, Mannis MJ, Holland EJ, eds.
Cornea: cornea and external disease: clinical diagnosis and management . St Louis: Mosby-Year Book, Inc,
1997:625–32.
13 Shimazaki J , Goto E, Ono M, et al.
Meibomian gland dysfunction in patients with Sjo¨gren syndrome.
Ophthalmology 1998; 105 :1485–8.
14 Van Bijsterveld OP . Diagnostic tests in the sicca syndrome.
Arch Ophthalmol
1969; 82 :10–4.
15 Baier G , Wollensak G, Mur E, et al.
Analysis of human tear proteins by differential high-performance liquid chromatographic techniques.
J Chromatogr 1990; 525 :319–28.
16 Shine WE , McCulley JP. Keratoconjunctivitis sicca associated with meibomian secretion polar lipid abnormality.
Arch Ophthalmol 1998; 116 :849–52.
17 Lechner M , Wojnar P, Redl B. Human tear lipocalin acts as an oxidativestress-induced scavenger of potentially harmful lipid peroxidation products in a cell culture system.
Biochem J 2001; 356 :129–35.
18 Gachon A-M F , Lacazette E. Tear lipocalin and the eye’s front line of defence.
Br J Ophthalmol 1998; 82 :453–5.
19 Lo¨gdberg L , Wester L. Immunocalins: a lipocalin subfamily that modulates immune and inflammatory responses.
Biochim Biophys Acta
2000; 1482 :284–97.
20 Fullard RJ , Snyder C. Protein levels in nonstimulated and stimulated tears of normal human subjects.
Invest Ophthalmol Vis Sci 1990; 31 :1119–26.
21 Grus FH , Sabuncuo P, Augustin AJ. Quantitative analyse der tro¨nenproteinmuster bei weichen kontaktlinsen—klinische studie.
Klin
Monatsbl Augenheilkd 2001; 218 :239–42.
22 Glasson MJ , Stapleton F, Wilcox MDP. Lipid, lipase and lipocalin differences between tolerant and intolerant contact lens wearers.
Curr Eye Res
2002; 25 :227–35.
www.bjophthalmol.com
806
SCIENTIFIC REPORT
The use of low dose methotrexate in children with chronic anterior and intermediate uveitis
A R Malik, C Pavesio
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :806–808. doi: 10.1136/bjo.2004.054239
Aim: To assess the efficacy of low dose methotrexate (MTX) therapy for children with chronic anterior and intermediate uveitis.
Methods: A retrospective case review of 10 children who received MTX for chronic uveitis at a tertiary referral centre was performed. The following data were recorded for each patient: age, sex, race, duration of uveitis, primary diagnosis, anatomical localisation of uveitis, corticosteroid therapy, dose range of MTX, duration of MTX therapy, and side effects of MTX therapy. Several clinical parameters were evaluated to study the effect of MTX. These included visual acuity, anterior chamber inflammation, and topical and oral corticosteroid requirement.
Results: After MTX VA of 6/6 or better was present in 100% right eyes and 80% left eyes (p = 0.055 and p = 0.016, respectively). Anterior chamber inflammation decreased in
60% of children after MTX (p = 0.0168). The requirement of topical steroid decreased from a mean of 5.6 times a day before MTX to 1.5 times a day after MTX (p = 0.005). The dose of oral steroid decreased from a mean of 18 mg per day to 2.85 mg per day (p = 0.012). The most common adverse effect was nausea (20%). No patient required discontinuation of MTX because of side effects.
Conclusion: MTX is effective and safe for chronic anterior and intermediate uveitis in children. An increase awareness of its efficacy is required among paediatricians and ophthalmologists to prevent sight threatening complication of chronic uveitis and its treatment with long term use of steroids.
A lthough uveitis is relatively uncommon in children it is a serious, potentially blinding disease with large potential social and economic consequences.
1 Juvenile idiopathic arthritis (JIA) is the most common cause followed by idiopathic uveitis and pars planitis.
1 2 Corticosteroids are the mainstay of treatment but long term treatment in all routes of administration is associated with adverse effects with ocular and systemic manifestations.
3–5
Because of the adverse effects associated with persistent uveitis or chronic use of corticosteroids it is recommended, for those in need of long term anti-inflammatory medication, to start corticosteroids in the acute stage of the disease and taper off subsequently with combined use of a steroid sparing medication.
6 7 MTX is a folate analogue that inhibits dihydrofolate reductase, inhibiting the production of tetrahydrofolate, which is necessary for DNA synthesis. The immunosuppressive effects of low dose MTX are primarily through its antiproliferative effect on rapidly dividing immune cells. The secondary effects of MTX include cytopenia, hepatotoxicity, and interstitial pneumonitis.
A few well documented reports exist in the paediatric literature on the use of MTX in JIA associated uveitis.
8 9
In this retrospective case series we present our experience with the use of low dose MTX in 10 children with chronic low grade anterior and intermediate uveitis, including cases secondary to sarcoidosis, and idiopathic type.
METHODS
The clinical records of all children with uveitis, seen at a uveitis service at Moorfields Eye Hospital between 1999 and
2003 and who were treated with MTX, were reviewed. Initial examination of each patient included a complete medical and ophthalmic history and an eye examination. The number of cells in the anterior chamber was quantified by a standard grading scale (0, occasional, 1 + to 4 + ) modified from Hogan et al .
10 Before initiation of MTX a complete blood count, liver function, and renal function tests were performed. These were monitored periodically for drug toxicity every 4 weeks.
The follow up of these patients before and during treatment was in close liaison with a paediatrician, who also carried out investigations for the diagnosis of any systemic associated disease.
The following data were recorded for each patient: age, sex, race, duration of uveitis, primary diagnosis, anatomical localisation of uveitis, corticosteroid therapy, dose range of
MTX, duration of MTX therapy, and side effects of MTX therapy.
Several clinical parameters were evaluated to study the effect of MTX. These included visual acuity, anterior chamber inflammation, and topical and oral corticosteroid requirement.
Statistical analysis
Data from the last clinic visit before initiating MTX were compared with those from the last available visit while on
MTX by using the Wilcoxon signed rank test. The p values of
0.05 or less were considered statistically significant.
RESULTS
Ten children (all had age of onset of uveitis at less than
16 years of age) who had treatment with MTX were identified and the data were analysed. Table 1 lists the patients, sex, dose and duration of MTX, initial and final topical and oral steroid doses, and initial and final visual acuities. There were eight girls and two boys. The mean age was 11.9 years (range 7–16 years). Three patients were white, three were Asian Indians, two were Afghani, one was Chinese, and one was African. The paediatrician in charge of the case was responsible for all investigations to exclude an underlying disease, including serology, ANA,
SACE, lysozyme, imaging, or any tests considered necessary.
The diagnosis of uveitis was idiopathic in seven cases and in three cases the diagnosis of presumed sarcoidosis was
Abbreviations: JIA, juvenile idiopathic arthritis; MTX, methotrexate www.bjophthalmol.com
Methotrexate in children with uveitis 807 established on clinical grounds by the paediatrician. The location of uveitis was anterior in six and intermediate in four cases. The uveitis was bilateral in all the children.
The mean duration of uveitis before commencement of
MTX was 24 months (range 6–36 months).
The indication for initiating MTX in all these children was either poor control of inflammation or development of side effects from conventional therapy with corticosteroids.
Patients 3 and 4 (table 1) had also received ciclosporin before introduction of MTX, and patient 4 continued with a combination of both drugs. Introduction of MTX was only considered after previous therapy was thought to be a failure, following a period of 2 months of use. All children were treated with oral MTX except one (table 1, child no 9) who was unable to tolerate oral MTX because of severe nausea and remained on subcutaneous MTX (sc) throughout the study.
All children were treated with low dose once weekly oral or sc
MTX for a mean of 22.5 months (range 4–40 months) at the time of analysis. All children received folic acid 2.5–5 mg/day from the start of MTX therapy.
Nausea was the only common complication associated with MTX use. One child receiving combination therapy
(MTX and ciclosporin), reported abdominal pain, but no change in therapy was necessary. Only one patient (case 9) had a small rise of ALT of 47 (0–40). No other patient had abnormality of liver function tests. No abnormalities in blood count or renal function were detected in any of the children.
Ocular complications associated with steroid use were ocular hypertension in two patients, which resolved following better control of inflammatory activity with MTX and reduction of topical steroid therapy, and cataract in two patients. One patient developed cystoid macular oedema during activity of the disease, which resolved following MTX therapy (right eye of patient 9).
Snellen visual acuity of 6/6 or better was present in eight
(80%) right eyes and six (60%) left eyes before MTX. After
MTX therapy VA was 6/6 or better in 10 (100%) right eyes
(p = 0.055) and in eight (80%) left eyes (p = 0.016) (table 1).
After MTX anterior chamber inflammation decreased in
60% (six children). In four children there was no change in inflammation. The decrease in inflammation after MTX was statistically significant (p = 0.0168) (table 1).
The topical corticosteroid frequency was six times per day in 70% of the children before MTX. After MTX, at the final visit, only one child was using topical steroid four times per day. The difference between pre-MTX and post-MTX topical steroid frequency was statistically significant (p = 0.005)
(table 1).
Seven children were using oral steroids before MTX. The dose of oral prednisolone was decreased in all children after
MTX. The mean initial dose was 18 mg (range 10–40 mg) and the mean final dose was 2.85 mg (range 5–7.5 mg). This difference between pre-MTX and post-MTX oral steroid use was statistically significant (p = 0.012).
The most common adverse effect was nausea (patients 9 and 10); however, this was mild in intensity and well tolerated. No patient required discontinuation of MTX as a result of adverse effects.
DISCUSSION
Uveitis in children is a serious disease which may go unrecognised because it may be asymptomatic or because of its insidious nature. The child may already have serious complications of chronic uveitis at the time of presentation to the ophthalmologist. The ophthalmologist is therefore posed with the challenge of prompt control of inflammation and preventing further development of ocular and systemic complications. The current therapy of choice is corticosteroids, topical initially for the anterior forms and subsequently www.bjophthalmol.com
808 Malik, Pavesio oral, when that fails, or in the presence of posterior disease
(intermediate uveitis type). Long term systemic corticosteroids have an adverse effect on the developing skeletal and immune system.
Low dose, once a week MTX has become the therapeutic agent of choice for children with JIA who fail to respond adequately to the non-steroidal anti-inflammatory drugs. In these selected patients with chronic active uveitis low dose
MTX was effective and well tolerated. At the time MTX was started all children had active uveitis despite frequent instillation of topical steroids and previous administration of oral steroids. After treatment with MTX there was significant reduction in the severity of uveitis.
Several authors have reported a favourable response of JIA associated uveitis to treatment with low dose MTX. In low doses MTX is less toxic than most immunosuppressants including corticosteroids.
Weiss et al describe the use of low dose subcutaneous MTX in seven children with JIA associated uveitis. All patients had chronic active uveitis for at least 1 year (range 1–17 years) inadequately suppressed with corticosteroids and had progressive steroid related cataract and glaucoma.
9 The use of
MTX decreased the severity of uveitis in six of seven patients and allowed for the discontinuation or reduction of corticosteroid. In another case series low dose oral MTX therapy was found to be effective in the treatment of four children with severe iritis secondary to JIA and sarcoidosis.
11
The use of systemic therapy in these patients differs from conventional indication for introduction of such agents. Most of the time, they are introduced in vision threatening uveitis when visual acuity falls below 6/12. In our patients the decision to introduce systemic therapy was based on the presence of severe anterior segment inflammation, in spite of frequent topical therapy. None of our patients had significant change in visual acuity as the justification for therapy.
Overall, MTX is well tolerated and despite its side effect profile, it continues to have a role as a corticosteroid sparing agent in the management of patients with ocular inflammatory disease.
12 Informed opinion would indicate that it should be used early in disease to prevent permanent damage to intraocular structure.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
A R Malik, East Surrey Hospital, Redhill, Surrey, UK
C Pavesio, Moorfields Eye Hospital, London EC1V 2PD, UK
Correspondence to: C Pavesio, MD, FRCOphth, Moorfields Eye
Hospital, London EC1V 2PD, UK; carlos.pavesio@moorfields.nhs.uk
Accepted for publication 12 November 2004
REFERENCES
1 Tugal-Tutkin I , Havrlikova K, Power WJ, et al.
Changing patterns in uveitis in childhood.
Ophthalmology 1996; 103 :375–83.
2 Kanski JJ , Shun-Shin A. Systemic uveitis syndromes in childhood. An analysis of 340 cases.
Ophthalmology 1984:91247–51.
3 Solomon SD , Cunningham Jr ET. Use of corticosteroids and non-corticosteroid immunosuppressive agents in patients with uveitis.
Comprehensive
Ophthalmology Update 2001; 1 :273–86.
4 Nussenblatt RB , Whitcup SM, Palestine AG.
Uveitis, fundamentals and clinical practice . 2nd ed. St Louis: Mosby, 1996:97–129.
5 Jabs DA , Rosenbaum JT, Foster CS, et al.
Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel.
Am J Ophthalmol 2000; 130 :492–513.
6 Rothova A . Corticosteroids in uveitis.
Ophthalmol Clin N Am 2002:389–94.
7 Tamesis RR , Rodriguez A, Christen GW, et al.
Systemic drug toxicity trends in immunosuppressive therapy of Immune and Inflammatory ocular disease.
Ophthalmology 1996; 103 :768–75.
8 Hemady R , Baer J, Foster C, et al.
Immunosuppressive drugs in the management of progressive corticosteroid-resistant uveitis with juvenile rheumatoid arthritis.
Int Ophthalmol Clin 1992; 32 :241–52.
9 Weiss HA , Wallace AC, Sherry DD. Methotrexate for resistant chronic uveitis in children with juvenile rheumatoid arthritis.
J Pediatr 1998; 133 :266–8.
10 Hogan MJ , KimuraSJ, Thygeson P. signs and symptoms of uveitis. 1. Anterior uveitis.
Am J Ophthalmol 1959; 47 :155–170.
11 Shetty KA , Zganjar EB, Ellis SG, et al.
Low-dose methotrexate in the treatment of severe juvenile rheumatoid arthritis and sarcoid iritis.
J Pediatr Ophthalmol
Strabismus 1999; 36 :125–8.
12 Djalilian AR , Nussenblatt RB. Immunosuppression in uveitis.
Ophthalmol
Clin N Am 2002; 15 :395–404.
Call for papers
11th European Forum on Quality Improvement in Health Care
26–28 April 2006, Prague, Czech Republic
Deadline 30 September 2005.
For further information and to submit online go to: www.quality.bmjpg.com
www.bjophthalmol.com
809
SCIENTIFIC REPORT
Intraocular pressure changes in the contralateral eye after trabeculectomy with mitomycin C
I Vysniauskiene, T Shaarawy, J Flammer, I O Haefliger
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :809–811. doi: 10.1136/bjo.2004.050294
Aim: To assess intraocular pressure (IOP) changes of the contralateral eyes of eyes undergoing trabeculectomy with mitomycin C (MMC).
Methods: Non-comparative retrospective study of 24 consecutive patients who underwent trabeculectomy with MMC that led to more than 45% reduction in IOP. In the contralateral eyes, IOP before surgery was compared with
IOP 1 day and 1 month after surgery. 11 fellow eyes were under topical hypotensive therapy while 13 contralateral eyes were not (12 contralateral eyes had previous filtering surgery and one had normal tension glaucoma). No patients had systemic ocular hypotensive therapy.
Results: Mean IOP in all contralateral eyes decreased from
15.5 (SD 5.5) mm Hg to 12.5 (3.8) mm Hg (p , 0.01), and
13.0 (4.7) mm Hg (p , 0.001) 1 day and 1 month after surgery, respectively. In the 11 fellow eyes under topical ocular hypotensive therapy mean IOP was reduced from
19.5 (4.0) mm Hg to 13.5 (2.2) mm Hg (p , 0.01), and 16.5
(2.8) mm Hg (p , 0.05) 1 day and 1 month after surgery, respectively. In the 13 fellow eyes not under topical ocular hypotensive therapy mean IOP was reduced from 12.1 (4.2) mm Hg to 11.6 (4.7) mm Hg (p not significant) and 9.8 (3.8) mm Hg (p0.01) 1 day and 1 month after surgery, respectively.
Conclusions: In the present population, a month after trabeculectomy, mean IOP in the contralateral eyes decreased independently of whether these contralateral eyes were undergoing topical ocular hypotensive therapy or not.
n 1924 Weekers, 1 I to describe changes of intraocular pressure (IOP) in contralateral eyes, coined the term
‘‘ophthalmotonic consensual reaction.’’ Since then many studies have reported how an fall in IOP in one eye occurs in the other eye too; such an effect seems to occur after ocular compression, tonography, trauma, cauterisation of the sclera, paracentesis, laser trabeculoplasty as well as fistulising surgery.
2–6
In contrast with many previously published reports, has recently been reported 7
2–6 it that after trabeculectomy, the IOP or the aqueous humour inflow was increased in the contralateral eyes. The purpose of this study was to assess
IOP changes in the contralateral eyes, 1 day and 1 month after trabeculectomy.
PATIENTS AND METHODS
The medical charts of 24 consecutive patients who underwent trabeculectomy with mitomycin C (MMC) performed by the same surgeon (IOH) between 1995 and 2000 at the University
Eye Clinic, Basel, were retrospectively reviewed. Inclusion criteria for this study were IOP reduction in the operated eye of more than 45%. No patients were undergoing systemic
Table 1 Demographic data of 24 patients
Characteristics
Eyes
Patients
Sex
Female
Male
Race
White
Age
Average (SD)
Eye
Right
Left
No
24
24
11 (46%)
13 (54%)
24 (100%)
72.0 (11.8) (43–90)
9 (38%)
15 (52%) hypotensive therapy. In these patients the contralateral eyes were divided into two groups, a first group of 11 fellow eyes that were undergoing topical ocular hypotensive therapy and a second group of 13 fellow eyes that were not. Among these
13 fellow eyes that had no topical ocular hypotensive therapy,
12 had previously had a trabeculectomy with MMC and one had normal tension glaucoma that did not need ocular hypotensive treatment.
The IOP in each fellow eye was recorded 1 day before surgery, as well as 1 day and 1 month after surgery. Data are presented as a means (SD). Statistical analysis of the data was performed using paired Student’s t test with a p value lower or equal to 0.05 considered to be statistically significant.
RESULTS
Demographic details of the present population and the type of glaucoma affecting each eye are shown in the tables 1 and
2, respectively. The treatment of fellow eye before and during this study is presented in table 3.
Mean IOP in the 24 fellow eyes was decreased after surgery from 15.5 (5.5) mm Hg to 12.5 (3.8) mm Hg (p , 0.01) and
13.0 (4.7) mm Hg (p , 0.001) 1 day, and 1 month after surgery, respectively (fig 1).
In the 11 fellow eyes under topical ocular hypotensive therapy, after surgery mean IOP was reduced from 19.5 (4.0) mm Hg to 13.5 (2.2) mm Hg (p , 0.01) and 16.5 (2.8) mm Hg
(p , 0.05) 1 day and 1 month after surgery, respectively
(fig 2). In the 13 fellow eyes not under topical ocular hypotensive therapy, after surgery, mean IOP was reduced from 12.1 (4.2) mm Hg to 11.6 (4.7) mm Hg (p not significant) and 9.8 (3.8) mm Hg (p , 0.01) 1 day and
1 month after surgery, respectively (fig 3).
Abbreviations: IOP, intraocular pressure; MMC, mitomycin C www.bjophthalmol.com
810 Vysniauskiene, Shaarawy, Flammer, et al
Table 2 Type of glaucoma affecting each eye
Type of glaucoma
Primary open angle
Pseudoexfoliation
Normal tension
Total
No (%) eyes
18 (75)
5 (21)
1 (4)
24 eyes
25
20
15
Table 3 Treatment of contralateral eyes
Treatment
No of eyes
(%)
Local hypotensive drops b blockers
Dorzolamide
Latanoprost
11 (45.8)
2 (8.3)
1 (4.2)
2 (8.3) b blockers + pilocarpine b blockers + dorzolamide
1 (4.2)
2 (8.3) b blockers + pilocarpine + dorzolamide 1 (4.2) b blockers + pilocarpine + latanoprost 1 (4.2) b blockers + pilocarpine + dorzolamide + latanoprost 1 (4.2)
No local hypotensive drops
Without glaucoma surgery
Glaucoma surgery
13 (54.2)
1 (4.2)
12 (50.0)
Average of time after surgery 13.1 (24.4) months.
DISCUSSION
This study indicates that 1 month after trabeculectomy with
MMC the mean IOP significantly decreased in the contralateral eyes independently of whether they were undergoing topical hypotensive treatment or not. These findings seem to indicate that this is probably not because of improved compliance after surgery.
The IOP changes in contralateral eyes have been described by many investigators after ocular compression, tonography, trauma, cauterisation of the sclera, and paracentesis.
3–5
Topical ocular hypotensive medications have been shown to cause a fall in IOP after unilateral application in the fellow, untreated eye. This has been described as an ophthalmotonic consensual reaction (OCR) 1 and the potential sympathetic influences have been studied.
8 9 However, this reduction had also been attributed to an effect caused by systemic absorption of the drug via the nasolacrimal pathways.
10 It was observed that in eyes of patients with Horner’s syndrome
10
5 n = 11
1 Day before surgery
1 Day after surgery
1 Month after surgery
Figure 2 In the 11 fellow eyes under topical ocular hypotensive therapy, IOP reduction was 4 mm Hg after 1 day (p , 0.01) and
3 mm Hg after 1 month (p , 0.05) after surgery.
OCR was less pronounced than in normal eyes.
workers 12
11 Cox and codescribed an ablation of experimental animal eyes in which there was a rise in IOP in response to water drinking after unilateral optic nerve sections. They concluded that their results support the hypothesis of a supraoptic nuclear control mechanism of IOP.
Wilmer 6 noted in experimental animals a fall in IOP in one eye after a fistulisation operation on the other eye. Also for short period of time the decrease in IOP after trabeculectomy was observed in human fellow eyes.
Diestelhorst and Krieglstein 10 studied the effect of trabeculectomy on the aqueous humour flow of the unoperated fellow eye, using computerised anterior chamber fluorophotometry. Aqueous humour flow was measured in these eyes before surgery and on the fifth day after trabeculectomy.
The average postoperative flow in the fellow eye increased from 2.56
m l/min to 2.9
m l/min (p , 0.05%). They concluded that filtration surgery in one eye triggers a CNS mediated, reflective increase in aqueous flow to maintain physiological stability in the anterior chamber of the surgically
25
25
20
20
15
15
10
5
0 n = 24
1 Day before surgery
1 Day after surgery
Figure 1 Mean IOP in the 24 fellow eyes.
1 Month after surgery
10
5 n = 13
1 Day before surgery
1 Day after surgery
1 Month after surgery
Figure 3 In the 13 fellow eyes not under topical ocular hypotensive therapy, IOP reduction was 0.5 mm Hg after 1 day (p, not significant) and 2.3 mm Hg after 1 month (p , 0.01) after surgery.
www.bjophthalmol.com
IOP decrease in the contralateral eye after trabeculectomy 811 treated eye. They argued that their results prove the existence of an ocular CNS reflex responsible for the regulation of IOP homeostasis, and that since this CNS reflex on aqueous humour dynamics affects both eyes, this would explain their clinical observation of IOP dysregulation in the unoperated fellow eye following unilateral trabeculectomy.
Regarding IOP in the unoperated fellow eyes, they reported no statistically significant change from the preoperative level.
Statistical analysis did not show a significant correlation between IOP changes and the increase in aqueous humour flow observed in the unoperated fellow eyes. This seems to imply that the facility of outflow was sufficient to compensate for the increase in aqueous humour flow.
In contrast, a recent publication 7 reported that the mean
IOP significantly increased after trabeculectomy in the unoperated fellow eyes. The same study reported a preoperative IOP in the operated eye of 37.0 (SD 10.0) mm Hg.
The authors report that they have not used any preoperative systemic ocular hypotensive therapy, and unfortunately they do not comment on how they were managing patients with such a high mean IOP preoperatively. As mentioned before, this report contrasts with previous literature reporting, for decades, on the tendency for a decrease in IOP in the contralateral eye.
A decrease of IOP in fellow eye after argon laser trabeculoplasty was also reported.
2 Such reduction of IOP in fellow eye was theoretically explained by a better compliance of patients after intervention, when the patient becomes more conscientious about taking his medications. In this study such an explanation could probably be excluded because a significant IOP decrease 1 month after surgery was also observed in the eyes without any local hypotensive treatment. In other words, our study not only confirms previously published literature on the significant decrease in
IOP in the contralateral eye but shows that there is a significant reduction irrespective of whether the patient was on topical ocular hypotensive medications or not. Our study results might lend more evidence to the theory of the existence of an ophthalmotonic consensual reaction. Further studies are needed to prove or disprove this mechanism, and to find ways to manipulate this reaction to the benefit of our patients.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
I Vysniauskiene, T Shaarawy, J Flammer, I O Haefliger, University Eye
Clinic Basel, Switzerland
Correspondence to: Tarek Shaarawy, MD, University Eye Clinic Basel,
Mittlere Strasse 91, 4012 Basel, Switzerland; tarek.shaarawy@hcuge.ch
Accepted for publication 12 September 2004
REFERENCES
1 Weekers L . Modification expe´rimentales de l’ophtalmotonous. Reaction ophtalmotonique consenuelle.
Arch Opthalmol (Paris) 1924; 41 :641–58.
2 Brooks AMV , West RH, Gillies. Argon laser trabeculoplasty five years on.
Aust N Z J Ophthalmol 1988; 16 :343–51.
3 Nagata N , Kurimoto S, Matsuka M. A study of consensual ophthalmotonic reaction.
Acta Soc Ophthalmol Japan 1954; 58 :38–46.
4 Prijot EL , Stone HH. A study of consensual ophthalmotonic reaction.
Am J Ophthalmol 1956; 42 :50–8.
5 Stocker FW . On changes in intraocular pressure after application of the tonometer.
Am J Ophthalmol 1958; 45 :192–6.
6 Wilmer WE . Discussion on the results of operative treatment of glaucoma.
Trans Ophthalmol Soc UK 1927; 47 :230–3.
7 Yarangu¨meli A , Ko¨zo¨zlem, KuralGu¨lcan. The effect of trabeculectomy on the intraocular pressure of the unoperated fellow eye.
J Glaucoma
2003; 12 :108–13.
8 Langham ME , Diggs EM.
b -Adrenergic responses in the eyes of rabbites, primates and man.
Exp Eye Res 1974; 19 :281–7.
9 Radius RL , Diamond GR, Pollack IP, et al.
A new drug for management of chronic simple glaucoma.
Arch Ophthalmol 1978; 96 :1003–7.
10 Diestelhorst M , Krieglstein G. The effect of trabeculkectomy on the aqueous humor flow of the unoperated fellow eye.
Graefes Arch Clin Exp Ophthalmol
1991; 229 :274–6.
11 Ten Tusscher MP , Beckers HJ, Vrensen GF, et al.
Peripheral neural circuits regulating IOP ?
A review of its anatomical backbone.
Doc Ophthalmol
1994; 87 :291–313.
12 Cox CE , Fitzgerald CR, King RL. A preliminary report on the supraoptic nucleus and control of intraocular pressure.
Invest Ophthalmol 1975; 14 :26–8.
www.bjophthalmol.com
812
SCIENTIFIC REPORT
The visual field in toxoplasmic retinochoroiditis
M R Stanford, E A Tomlin, O Comyn, K Holland, C Pavesio
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :812–814. doi: 10.1136/bjo.2004.055756
Aims: To document loss of central field in patients with scars from toxoplasmic retinochoroiditis close to the disc after resolution of disease.
Methods: Patients with a clinical diagnosis of toxoplasmic retinochoroiditis were enrolled from four centres. Automated central visual field testing was performed when their disease had settled and retinal photographs of the lesions were taken. The type of central field defect (whether absolute or relative) and whether it broke out to the periphery were correlated with the size of the retinochoroidal scar and its proximity to the optic nerve head.
Results: 69 eyes were enrolled; 16 (26%) were discarded because of poor field performance. Of the 53 remaining eyes, 31 showed absolute defects and 20 relative defects.
Scars within one disc diameter of the disc were more likely to be associated with absolute defects breaking out to the periphery.
Conclusion: The scarring induced by toxoplasmic retinochoroiditis is associated with considerable field loss when it occurs close to the optic nerve head. Current treatment is unlikely to ameliorate this situation. The degree of visual field loss should be an outcome measure for future trials of the efficacy of treatment trials for the disease.
T oxoplasmic retinochoroiditis classically presents as a focus of new retinitis adjacent to an old chorioretinal scar. After about 6 weeks, the focus of active retinitis slowly fades leaving a further, larger scar in its place, with resolution of other intraocular inflammatory signs.
1 Whether this process of healing can be accelerated by the use of antibiotics and/or corticosteroids has not been established through formal clinical trials.
2 Despite this, the main indications for treatment are the presence of fresh retinitis within the macular arcade or an active lesion lying within one disc diameter of the optic nerve head.
3–5 In this latter situation, it has been hypothesised that the necrotising retinitis leads to full thickness damage, with involvement of both photoreceptors and second order neurons as well as the nerve fibre layer itself. If this were the case then the resulting scotoma would not only be absolute in the area of photoreceptor destruction, but would also break out to the periphery because of interruption of distal signalling.
Similarly, the closer the damage is to the disc, the greater might be the resultant scotoma because of greater involvement of the nerve fibre layer.
Evidence supporting this hypothesis is sparse. Several textbooks on visual fields describe a typical scotoma with breakout to the periphery and this undoubtedly occurs in some cases.
6 However, since there has been no systematic examination of the visual fields after attacks of disease have settled, we undertook a prospective study of patients presenting with new toxoplasmic retinochoroiditis and measured their fields by automated perimetry when their disease was clinically quiet.
METHODS
Study design
A prospective, cross sectional, observational study of consecutive patients presenting to uveitis clinics with a diagnosis of toxoplasmic retinochoroiditis. Patients were derived from clinics in the United Kingdom (St Thomas’s Hospital and
Moorfields, London), Brazil (Federal University of Minas
Gerais, Belo Horizonte), and Mauritius (Subramania Bharati
Eye Hospital, Moka). The study received ethical permission from the local ethics committee of Moorfields Eye Hospital.
Inclusion criteria
An active or inactive retinochoroidal scar consistent with toxoplasmic retinochoroiditis was present in any position in the fundus. Wherever possible, anti-toxoplasma antibodies were detected by serological testing. Where active disease was present, this was managed appropriately and visual field testing was not undertaken until the lesion was considered resolved and the ocular media had cleared (less than 1 + vitreous cells or BINO score less than 1 + 7 ). Historical patients were recalled for this study.
Exclusion criteria
Patients who were unwilling or unable to perform visual field testing (see below) were excluded, as well as any patient with known ocular/neurological pathology giving rise to visual field loss.
Visual field testing
Visual field testing was undertaken in a number of ways depending on the clinic attended. In the United Kingdom, the central visual field was recorded using the Humphrey 24/2
FastPac strategy or if unavailable a 24/2 SITA fast or SITA standard strategy. The right eye was tested first and then the left eye. Wherever possible the test was repeated at least
4 weeks apart at a second visit to allow for the learning curve.
In Brazil, the central field was recorded using the Octopus
1-2-3, CT1 dynamic standard and in Mauritius, the Kowa AP
3000 automated perimeter, precision strategy was used.
Specifically excluded were patients who had more than
33% fixation losses, more than 20% false positive, or more than 20% false negative responses. Details of full ophthalmological investigation were prospectively recorded and dilated fundus photographs included for subsequent analysis.
Analysis of data
Field loss was assessed independently and scotomata were coded as absolute or relative; whether these broke out to the periphery was also determined. The mean defect was recorded where possible. Further analysis involved stratification of field loss and comparison with (a) the size of the scar, and (b) the position of the scar in relation to the optic disc derived from retinal photographs and drawings.
www.bjophthalmol.com
The visual field in toxoplasma retinochoroiditis 813
Figure 1 A FASTPAC Humphrey 24/2 visual field of the right eye.
RESULTS
Fields were recorded and photographs taken in 69 eyes. Of these, 16 (23.2%) were excluded because of low quality of field. This subgroup was analysed to see if there were any differences between those excluded and those included. The excluded eyes did not differ significantly in terms of age, sex, race, visual acuity, type of field defect, size of lesion, or distance of lesion from the disc. The remaining cohort of 53 eyes (29 R, 24 L) comprised 26 male, 22 female, mean age
30.7 years (range 12–69). These were divided among four main ethnic groups—Afro-Caribbean 14 (26.4%), white 13
(24.5%), Asian Indian (Mauritian) 12 (22.6%), and Latin
American 14 (26.4%).
Of the 53 eyes in the study, 39 (73.6%) had a Snellen acuity of better than 6/12; 11 (20.8%) fell between 6/12 and 6/60, and three (5.7%) had an acuity of worse than 6/60; 51 eyes had a demonstrable central field defect. Absolute defects were seen in 31 eyes (60.8%), of which 18 (58.1%) showed breakout to the periphery (figs 1 and 2), the remaining 13
(41.9%) remaining confined to the lesion. Relative field defects were detected in 20 (39.2%) eyes. Neither the size of the scar nor its distance from the disc correlated with the type of field defect present.
The characteristics of the field defect in relation to size of lesion are shown in table 1. It may be seen that there is no difference in whether the defect was relative or absolute in relation to the size of the lesion. For all patients where the mean defect was recorded (40), 22 had an absolute scotoma and 18 a relative one. For absolute scotomata, the average mean defect was 2 8.08 dB ( 2 1.80 to 2 18.61, SD 4.26). For relative scotomata the average mean defect was 2 3.96 dB
( 2 1.10 to 2 9.20, SD 2.22) (p = 0.0007).
An analysis of field defects by position of lesion in relation to the optic disc is shown in table 2. Lesions within one disc diameter of the optic disc were far more likely to be associated with an absolute defect with breakout to the periphery than lesions further away.
Figure 2 Colour fundus photograph of the right eye showing the area of retina with old toxoplasma scars. In this case there was an absolute defect with breakout to the periphery.
For lesions within one disc diameter of the disc, the average mean defect, where recorded was 2 8.44 dB ( 2 4.36
to 2 18.61, SD 4.26). For lesions outside one disc diameter from the disc, the mean defect, where recorded was 2 5.39 dB
( 2 1.10 to 2 13.42, SD 3.67: p = 0.03).
DISCUSSION
Visual field loss arising as a result of toxoplasma retinochoroiditis, particularly when the focus of inflammation is within one disc diameter of the optic disc is poorly documented in the literature. Despite this, lesions occurring in this position are an indication for systemic treatment, 4 5 although the benefit of this treatment has never been formally evaluated in terms of subsequent loss of field. Anecdotal evidence suggests that where such field loss occurs, it is likely to be absolute since all layers of the retina are involved in the inflammation induced by toxoplasmic retinochoroiditis.
In this study we have shown that absolute field defects were seen in 31 eyes. In approximately half of these there was breakout to the periphery, but in the other half the field defect remained localised to correspond to the area of the scar. There was no difference in the size of the scar with respect to whether defects were absolute or relative; however, absolute defects occurred when the scar was close to the optic nerve head. As might be expected the average mean defect was more for absolute compared to relative defects. Almost all (9/10) scars within one disc diameter of the optic nerve head gave rise to absolute defects with breakout.
Formal testing of the visual fields following attacks of toxoplasma retinochoroiditis has rarely been reported before.
In a retrospective consecutive case series, Schlaegel reported the Goldmann field findings in 60 eyes 8 ; 35% showed a field defect within 5 ˚ of fixation, with 27% being paracentral (from
6 ˚ to 13 ˚ ), and 38% being peripheral. Analysis of whether the field defect was absolute or relative or whether it broke out to the periphery was not reported, and many of the eyes had active uveitis at the time of inclusion.
The present study may include biases because of patient selection. For instance, not every patient had two field tests because of the constraints of time/location. This may have contributed to the large number (25%) of fields that had to be
Table 1 Characteristics of field defect by size of lesion
Size type of defect
Absolute
Relative
Nil
2 DD and below
21
12
1
.
2 DD
10
8
1
DD, disc diameter.
www.bjophthalmol.com
814 Stanford, Tomlin, Comyn, et al
Table 2 Analysis of field defects by position of lesion in relation to the optic disc
Within 1 DD
Outside 1 DD
Absolute
With breakout
9 (75.0%)
9 (22.0%)
No breakout
1 (8.3%)
12 (29.3%)
Relative
2 (16.7%)
18 (43.9%)
Nil
0 (0%)
2 (4.9%)
DD, disc diameter.
rejected, although analysis of the rejected patients showed no difference in the location of scars or their size compared to the included fields. Secondly, there may have been selection bias since patients with more visually disabling disease tend to remain in clinics. Finally, there may also have been recall bias in the patients selected. Despite the prospective nature of this study, patients could be included from historical data sets, and patients with less disabling disease may have been lost to follow up.
The results of this study suggest that toxoplasmic retinochoroidal scars close to the optic nerve head are associated with absolute field defects with breakout to the periphery. For lesions further away from the disc, the prevalence of absolute defects with breakout reduced and lesions were more likely to produce relative defects. This may imply less destructive disease in this location (that is, the disease process may have only affected the outer retinal layers), but it is more likely that this is because of the larger receptor field for distal ganglion cells.
In summary, our study has confirmed that retinochoroidal scars lying within one disc diameter of the optic nerve head are likely to cause absolute defects with breakout to the periphery and should still be considered an absolute indication for treatment. Furthermore, visual field testing should form a routine part of the clinical assessment of patients when disease has settled and should certainly be included as a tool for the measurement of treatment efficacy in future placebo controlled studies, particularly where such loss may have functional consequences for the patient.
ACKNOWLEDGEMENTS
Supported in part by the Iris Fund for the Prevention of
Blindness. The authors would like to thank Professor F Orefice
(Brazil) and Dr I Gaya (Mauritius) for allowing us to study their patients.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
M R Stanford, E A Tomlin, O Comyn, K Holland, Department of
Ophthalmology, St Thomas’s Hospital, Lambeth Palace Road, London
SE1 7EH, UK
C Pavesio, Uveitis Service, Moorfields Eye Hospital, London, UK
Competing interests: none declared
Correspondence to: Mr M R Stanford, MD, FRCOphth, Medical Eye
Unit, St Thomas’s Hospital, Lambeth Palace Road, London SE1 7EH, UK; miles.stanford@kcl.ac.uk
Accepted for publication 12 November 2004
REFERENCES
1 Rothova A . Ocular manifestations of toxoplasmosis.
Curr Opin Ophthalmol
2003; 14 :384–8.
2 Stanford MR , See SE, Jones LV, Gilbert RE. Antibiotics for toxoplasmic retinochoroiditis. An evidence-based systematic review.
Ophthalmology
2003; 110 :926–32.
3 Holland GN , O’Connor GR, Belfort R, et al.
Toxoplasmosis. In: Pepose JS,
Holland GN, Wilhelmus KR, eds.
Ocular infection and immunity . St Louis:
Mosby Year Book, 1996:1210.
4 Engstrom R , Holland GN, Nussenblatt RB, et al.
Current practices in the management of ocular toxoplasmosis.
Am J Ophthalmol 1991; 111 :601–10.
5 Holland GN , Kewis KG. An update on current practices in the management of ocular toxoplasmosis.
Am J Ophthalmol 2002; 134 :102–14.
6 Lachenmayr BJ , Vivell PMO, eds.
Perimetry and its clinical correlates .
Stuttgart: Georg Thienne Verlag, 1993:113–15.
7 Nussenblatt RB , Palestine A, Chan CC, et al.
Standardization of vitreal inflammatory activity in intermediate and posterior uveitis.
Ophthalmology
1985; 92 :467–71.
8 Schlaegel TF , Weber JC. The macula in ocular toxoplasmosis.
Arch
Ophthalmol 1984; 102 :697–8.
www.bjophthalmol.com
815
SCIENTIFIC REPORT
The angiopoietin/Tie-2 system in proliferative sickle retinopathy: relation to vascular endothelial growth factor, its soluble receptor Flt-1 and von Willebrand factor, and to the effects of laser treatment
J S Mohan, P L Lip, A D Blann, D Bareford, G Y H Lip
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :815–819. doi: 10.1136/bjo.2004.058164
Aim: To determine plasma levels of angiopoietin-1 and angiopoietin-2 (Ang-1, Ang-2), their soluble receptor Tie-2, vascular endothelial growth factor (VEGF), its soluble receptor Flt-1 (as indices of angiogenesis), and von
Willebrand factor (vWf, marking endothelial damage/ dysfunction) in sickle cell disease (SCD) patients with proliferative sickle retinopathy (PSR), with non-proliferative retinopathy (NPR), or no retinopathy (NR) and in control subjects with normal haemoglobin (AA subjects). In addition, to determine changes with panretinal laser photocoagulation
(PRP) therapy.
Methods: Research indices were measured (ELISA) in 24
SCD patients who had PSR, 16 with NPR, 16 with NR, and from 23 AA subjects. Eight patients received PRP therapy and plasma was obtained before laser treatment and at 6 months after the last PRP session.
Results: Ang-1, Ang-2, VEGF, and vWf (but not Tie-2 or sFlt-1) were raised in SCD patients compared to AA subjects
(p
,
0.01) but there were no differences among the three
SCD subgroups. Significant correlations were between
Ang-1 and VEGF, Ang-1 and Tie-2, and VEGF and sFlt-1 in patients with SCD ( r = 0.67–0.88). Plasma Ang-2, VEGF, sFlt-1, and vWf levels did not change, but Ang-1 fell and Tie-2 rose significantly following PRP therapy.
Conclusions: SCD patients have raised plasma angiopoietins
(Ang-1, Ang-2), VEGF, and vWf compared to AA subjects.
These indices did not differ according to severity of retinopathy and only limited changes occurred following
PRP. The elevated growth factor levels in SCD may have obscured any association with retinopathy.
I n sickle cell disease (SCD), a group of inherited disorders of haemoglobin where pathology is caused by sickle (HbS) haemoglobin, the major pathophysiological basis of the morbidity and mortality is microvascular vaso-occlusion.
Vaso-occlusion in the microcirculation of the peripheral retina in SCD results in ischaemia, a response to which is a sequence of pathological vascular events leading to proliferative sickle retinopathy (PSR), eventually causing visual loss in 10–12% of eyes.
1 2 However, the determinants of PSR progression or autoinfarction are unknown.
3
Vascular endothelial growth factor (VEGF), a potent, secreted growth factor that promotes angiogenesis, is a possible stimulus for retinal proliferation, as its expression is upregulated by hypoxia.
4 High intraocular VEGF is found in patients with active intraocular neovascularisation, 5 6 supporting the view of a role in vasoproliferation/neovascularisation.
Changes in both plasma and intraocular VEGF levels have been related to laser treatment.
5 7 VEGF interacts with endothelial cells via membrane spanning receptors Flt-1 and KDR and the role of Flt-1 in embryonic vasculogenesis and adult angiogenesis and its association with several diseases has been clearly established.
8
Angiopoietin-1 and angiopoietin-2 (Ang-1, Ang-2), members of another family of vascular growth factors, interact with the endothelial cell specific tyrosine kinase receptor
Tie-2.
9 Ang-1 acts via the Tie-2 receptor to remodel primitive vessels and help maintain and stabilise the mature vessels by promoting interaction between endothelial cells and surrounding support cells.
10 11 Ang-2, conversely, leads to destabilisation of vessels and dissociation of pericytes, and is upregulated by hypoxia and angiogenic cytokines, including VEGF 12 13 with tumours and in pathological angiogenesis associated
10 11 and choroidal neovasculariation associated with age related macular degeneration.
14 Thus, the precise balance of VEGF and the angiopoetin/Tie-2 system is essential for modulating growing vessels and maintaining the integrity of existing vessels, thereby determining whether vessels proliferate and become leaky.
Abnormally raised levels of VEGF have been reported in
SCD 15 but any role in associated eye disease is unclear. We therefore hypothesised abnormal Ang-1, Ang-2, sFlt-1, and sTie-2 in SCD, measuring VEGF as an effective positive control and vWf as an index of endothelial damage/ dysfunction. We further hypothesised a graded increase in these markers in SCD patients with no retinopathy (NR), others with non-proliferative retinopathy (NPR), and others with proliferative sickle retinopathy (PSR). To test these hypotheses, we undertook a cross sectional study. Finally, we hypothesised that these indices fall after treatment with panretinal laser photocoagulation (PRP), and conducted a longitudinal study, measuring our research indices before and 6 months after laser treatment.
PATIENTS AND METHODS
Patients with SCD who attended the Sickle Cell and
Thalassemia (SCAT) Centre were recruited.
Diagnosis
(HbSS or HbSC) was proved using routine high performance liquid chromatography (HPLC). Patients were excluded if they had previously received laser treatment for proliferative retinopathy or had eye surgery, were receiving regular red cell exchange tranfusion, had blood tranfusion within the
Abbreviations: Ang, angiopoietin; HbS, sickle haemoglobin; HPLC, high performance liquid chromatography; NPR, non-proliferative retinopathy; NR, no retinopathy; PRP, panretinal laser photocoagulation;
PSR, proliferative sickle retinopathy; SCD, sickle cell disease; VEGF, vascular endothelial growth factor; vWf, von Willebrand factor www.bjophthalmol.com
816 Mohan, Lip, Blann, et al
Table 1 Plasma levels of angiopoietin-1 (Ang-1) angiopoietin-2 (Ang-2), the soluble angiopoietin receptor Tie-2 (Tie-2), vascular endothelial growth factor (VEGF), its soluble receptor Flt-1, and von Willebrand factor (vWf) in patients with sickle cell disease (SCD) and subjects with normal haemoglobin (AA)
AA subjects
(n = 23) (IQR)
SCD patients
(n = 56) (IQR) p Value
Raw data
Ang-1 (ng/ml)
Ang-2 (ng/ml)
Tie-2 (ng/ml)
VEGF (pg/ml) sFlt-1 (ng/ml) vWf (IU/dl)
Ratios
Ang-2/VEGF
Ang-2/Ang-1
Ang 1/VEGF
(Ang-2/Ang-1) 6 100/VEGF
0.5 (0.5
2 2.5)
1.3 (1.0
2 2.0)
10.8 (10.0
2 12.0)
11 (10 2 110)
14.0 (4 2 140)
89 (80 2 98)
100.0 (28.0
2 136.0)
2.2 (0.6
2 2.8)
50.0 (10 2 80)
12.0 (1.7
2 26.0)
2.2 (1.0
2 11.4)
5.1 (2.3
2 7.7)
7.7 (5.5
2 28.3)
120 (72 2 780)
21.5 (2.5
2 420)
143 (117.3
2 161)
23.5 (9.2
2 56.2)
1.4 (0.7
2 3.1)
16.5 (4.6
2 29.9)
1.4 (0.07
2 4.6)
0.0004
, 0.001
0.105
, 0.001
0.419
, 0.001
0.009
0.825
0.0058
0.0002
The study cohort of 56 SCD (26 men, mean (SD) age 33.5 (10) years) patients comprised 36 with HbSC disease and 20 with HbSS disease. Data in the SCD patients were compared with 24 healthy age, sex, and race matched controls (11 men, mean age 34.4 (SD 10) years).
In HbSC and HbSS disease, respective plasma levels of Ang-1 (median 1.7 (IQR 1–11.3) v 3.1 (2.0–11.4) ng/ml, p = 0.0571), Tie-2 (7.0 (5.3–28.3) v 8.5 (5.7–26.3) ng/ml, p = 0.436), VEGF (115(60–413) v 122(103–6625) pg/ml, p = 0.411), or sFlt-1 (13.8 (1.3–295) v 48 (11.3–490) ng/ml), p = 0.289), and vWf 133.5 (113.5–155) v
151.5 (133.3–168) IU/dl; p = 0.094) did not differ between the groups, although Ang-2 was higher in the SS patients (5.9 (4.4–10) v 3.2 (2.0–7.2) ng/ml) p = 0.025).
previous 3 months, had any malignancy, connective tissue disease or vascular disease, diabetes, hypertension, were pregnant, or were on long term medication (such as hydroxyurea). None of the patients had a painful crisis within 2 weeks of the time of ocular examinations and blood sampling. The healthy control group of subjects with normal haemoglobin genotype (AA subjects) were matched for age, sex, and ethnic origin with the PSR patients.
The diagnoses of PSR, NPR, or no retinopathy (NR) were made using slit lamp biomicroscopy and fluorescein angiography.
5 The characteristic confirming feature of the diagnosis of peripheral retinal neovascularisation was intense hyperfluorescence caused by leakage of dye from new blood vessels. Patients with PSR who showed evidence of leakage on fluorescein angiogram (‘‘leaky PSR’’) were offered laser treatment with sectoral panretinal photocoagulation (PRP).
A volume of 10 ml of citrated venous blood was obtained for measurement of plasma Ang-1, Ang-2, Tie-2, VEGF, sFlt-1, and vWf. For patients with NR or with NPR, this was the only occasion on which a blood sample was taken. In patients with ‘‘leaky PSR’’ a blood sample was repeated at 5–7 (median
6) months after their last laser treatment. Blood samples were taken from the antecubital vein with minimal stasis into
Vacuette tubes containing 3.2% sodium citrate and centrifuged at 3000 rpm at 4 ˚ C for 20 minutes. The platelet free plasma was immediately separated and frozen at 2 70 ˚ C. Research indices were measured by ELISA using commercially available reagents and recombinant standards (R & D Systems,
Abingdon, UK).
Data are presented as mean (SD) or median (interquartile range (IQR)) and compared by the unpaired t test and by the Mann-Whitney U test, or the one way ANOVA and
Table 2 Plasma levels of angiopoietin-1 (Ang-1) angiopoietin-2 (Ang-2), the soluble angiopoietin receptor Tie-2 (Tie-2), vascular endothelial growth factor (VEGF), its soluble receptor Flt-1, and von Willebrand factor (vWf) in patients with different manifestations of sickle eye disease
NR * NPR PSR ` p Value
Raw data
Ang-1 (ng/ml)
Ang-2 (ng/ml)
Tie-2 (ng/ml
VEGF (pg/ml) sFlt-1(ng/ml) vWf (IU/dl)
Ratios
Ang-2/VEGF
Ang-2/Ang-1
Ang-1/VEGF
(Ang-2/Ang-1) 6 100 /VEGF
2.2 (0.6–10.4)
6.0 (4.1–9.3)
6.3 (5.0–36.0)
108 (61–728)
35.0 (3–421)
133 (108–164)
43.3 (15.5–60.5)
2.4 (0.8–4.3)
14.9 (3.8–27.1)
2.8 (0.2–5.7)
3.1 (1.2–13.8)
3.8 (2.0–10.0)
9.0 (6.1–31.5)
116 (72–2650)
16.5 (0.3–500)
147 (113–166)
20.5 (2.2–41.5)
1.1 (0.6–2.3)
13.6 (4.1–29.3)
0.8 (0.02–3.5)
2.0 (1.0–11.3)
4.7 (2.1–7.4)
7.4 (5.8–22.0)
137 (104–378)
18.8 (6.1–278)
143 (122–161)
18.2 (11.3–59.1)
1.6 (0.7–3.1)
17.2 (4.8–40.6)
1.1 (0.15–4.4)
0.682
0.395
0.714
0.748
0.941
0.690
0.290
0.260
0.856
0.013
The PSR group comprised 22 with HbSC and two with Hb SS (11 men, mean age 35 (SD 11)), NPR comprised nine with HbSC disease and seven with HbSS (seven men aged 34 (10) years), while the NR group was five with HbSC and 11 with Hb SS (eight men, aged 32 (10) years). There were more patients with HbSC in the PSR group
(p = 0.008) but the differences in sex and age were not significant (p = 0.936, p = 0.585 respectively).
NR, no retinopathy; NPR, non-proliferative retinopathy; PSR, proliferative retinopathy.
* No retinopathy bilaterally; no retinopathy unilaterally or NPR unilaterally or NPR bilaterally; ` unilateral or bilateral PSR. Values are median
(IQR) except for age, which is expressed as mean (SD). All p values by Mann-Whitney U test except for age which is by the Student’s unpaired t test.
www.bjophthalmol.com
Angiopoietin/Tie-2 in proliferative sickle retinopathy
Table 3 Correlations among plasma angiogenic growth factors, their receptors, and von Willebrand factor in 23 AA subjects and 56 SCD patients
VEGF sFlt-1 Ang-1 Ang-2 Tie-2 vWf
23 AA subjects
VEGF sFlt-1
Ang-1
2 0.026, 0.908
0.099, 0.624
0.269, 0.215
Ang-2
Tie-2
0.209, 0.338
2 0.074, 0.739
56 SCD patients
VEGF 0.120, 0.380
sFlt-1
Ang-1
Ang-2
Tie-2
0.114, 0.401
0.279, 0.037
0.165, 0.225
0.317, 0.017
*
–
0.627, 0.001
*
0.505, 0.014
*
0.369, 0.083
0.546, 0.007
*
–
0.882, , 0.001
*
0.677, , 0.001
*
0.645, , 0.001
*
0.743, , 0.001
*
–
–
0.483, 0.020
*
0.244, 0.263
0.526, 0.010
*
–
–
0.610, , 0.001
*
0.699, , 0.001
*
0.766, , 0.001
*
–
–
–
0.245, 0.260
0.501, 0.015
*
–
–
–
0.591, , 0.001
*
0.743, , 0.001
*
–
–
–
–
–
–
–
–
–
0.516, , 0.001
*
–
–
–
–
–
–
–
–
–
–
Data presented as Spearman correlation coefficient ( r ) followed by p values.
* p Values , 0.05.
Ang-1: angiopoietin-1, Ang-2: angiopoietin-2, Tie-2: the angiopoietin receptor Tie-2, VEGF, vascular endothelial growth factor, sFlt-1, the VEGF receptor Flt-1; vWf, von Willebrand factor.
817
Kruskall-Wallis test as appropriate. Correlations were performed using Spearman’s rank correlation test. Paired comparisons were tested using the paired Wilcoxon test.
RESULTS
Plasma levels of Ang-1, Tie-2, VEGF, sFlt-1, and vWf did not differ between the groups, although Ang-2 was higher in the
SS patients (p = 0.025); therefore, data were pooled for further analysis. Plasma levels of Ang-1 and Ang-2 (but not
Tie-2 or sFlt-1) were significantly raised in the SCD patients compared to levels in the AA subjects (table 1). As expected, 15 16 VEGF and vWf were higher in SCD. The ratios of Ang-2 to VEGF, Ang-1 to VEGF, and between all three growth factors (that is [Ang-1/Ang-2 6 100]/VEGF) were lower in the SCD patients than in the controls but there was no statistical difference in the Ang-2/Ang-1 ratio. There were no differences in Ang-1, Ang-2, Tie-2, VEGF, sFlt-1, and vWf levels among the patients (table 2). The ratio [(Ang-1/
Ang-2) 6 100]/VEGF was higher in NR than in the two other groups.
In the AA subjects, the most significant correlations were between Ang-1 and VEGF, Ang-1 and Tie-2, and VEGF and sFlt-1 (table 3). Stronger positive correlations were also apparent between the same molecules in the patients with
SCD (table 3). Furthermore, in SCD, Ang-2 was highly correlated with Ang-1, Tie-2 with VEGF, and Ang-1 weakly with vWf. Within each of the SCD subgroups, Ang-1 was significantly correlated with Ang-2, with VEGF and with
Tie-2; similarly, Ang-2 was significantly correlated with
VEGF and Tie-2, (except in the NPR patients) and VEGF with sFlt-1 (table 4).
Plasma Ang-2 fell but Tie-2 rose significantly in eight patients (one male, mean age 34 (SD 9)) following PRP therapy (table 5), but Ang-1, VEGF, sFlt-1, and vWf levels did not change. Ocular examination showed only partial or incomplete resolution of neovascularisation at the time of the follow up blood sample in all the patients.
DISCUSSION
The current novel findings of elevated plasma Ang-2 in SCD, alongside raised VEGF, are consistent with the concept of increased angiogenic activity in SCD generally. The observations of elevated plasma VEGF 15 (up to , 10-fold) and vWf 16 confirm previous reports. The precise cause for the increased angiogenesis is unclear, but increased systemic tissue hypoxia consequent to generalised subclinical vaso-occlusion may contribute to the elevated plasma Ang-2 and VEGF levels.
Marked endothelial damage/dysfunction is associated with
SCD 16 and endothelial proliferation as a means of effecting endothelial repair may be a mechanism for attempting to
Table 4 Correlations among angiogenic growth factors sFlt-1 vWf VEGF
16 SCD patients with no retinopathy
VEGF sFlt-1
Ang-1
Ang-2
Tie-2
2
2
2
0.331, 0.210
0.015, 0.956
0.044, 0.872
0.156, 0.565
0.156, 0.564
–
0.743, 0.001
*
0.689, 0.003
*
0.745, 0.001
0.459, 0.074
16 SCD patients with non-proliferative retinopathy
*
VEGF sFlt-1
0.094, 0.730
0.076, 0.779
–
0.881, , 0.001
*
Ang-1
Ang-2
0.320, 0.228
0.037, 0.891
0.756, , 0.001
*
0.869, , 0.001
*
Tie-2 0.413, 0.112
0.701, 0.003
*
24 SCD patients with proliferative retinopathy
VEGF sFlt-1
Ang-1
Ang-2
0.290, 0.169
0.215, 0.313
0.477, 0.018
*
0.247, 0.245
–
0.935, , 0.001
*
0.611, 0.002
*
0.549, 0.005
*
Tie-2 0.295, 0.162
0.871, 0.000
*
–
–
0.492, 0.053
0.881, , 0.001
*
0.742, 0.001
*
–
–
0.773, , 0.001
*
0.761, , 0.001
*
0.688, 0.003
*
–
–
0.470, 0.020
*
0.514, 0.010
*
0.831, , 0.001
*
Ang-1
–
–
–
0.615, 0.011
*
0.656, 0.006
*
–
–
–
0.681, 0.004
*
0.822, , 0.001
*
–
–
–
0.589, 0.002
*
0.642, 0.001
*
Ang-2
–
–
–
–
0.712, 0.002
*
–
–
–
–
0.475, 0.063
–
–
–
–
0.477, 0.019
*
Tie-2
–
–
–
–
–
–
–
–
–
–
–
–
–
–
–
Data presented as Spearman correlation coefficient ( r ) followed by p values.
* p Values , 0.05.
Ang-1: angiopoietin-1, Ang-2: angiopoietin-2, Tie-2: the angiopoietin receptor Tie-2, VEGF: vascular endothelial growth factor, sFlt-1: the VEGF receptor Flt-1 and vWf: von Willebrand factor.
www.bjophthalmol.com
818 Mohan, Lip, Blann, et al
Table 5 The effect of laser treatment (PRP) on plasma levels of angiopoietin-1 (Ang-1) angiopoietin-2 (Ang-2), the soluble angiopoietin receptor Tie-2, VEGF, sFlt-1 and vWf in eight patients with sickle haemoglobin C disease with ‘‘leaky PSR’’
HbSC patients with ‘‘leaky PSR’’
Baseline
(pre-laser)
6 months post-laser p Value
Raw data
Ang-1 (ng/ml)
Ang-2 (ng/ml)
Tie-2 (ng/ml
VEGF (pg/ml) sFlt-1(ng/ml) vWf (IU/dl)
Ratios
Ang-2/VEGF
Ang-2/Ang-1
Ang-1/VEGF
(Ang-2/Ang-1 6 100)/VEGF
1.2 (0.6–9.5)
3.6 (1.5–7.2)
6.0 (5.5–7.8)
120 (72–138)
15 (5–138)
133 (113–152)
16.1 (12.2–101.1)
3.1 (1.0–4.3)
16 (4.8–28.2)
2.6 (0.5–8.0)
0.5 (0.5–1.5)
1.1 (1.1–2.0)
10.0 (7.6–10.6)
115 (50–155)
0.1 (0.01–3.6)
144 (138–148)
20.0 (9.3–23.5)
2.3 (0.77–2.7)
10 (8.8–13.2)
1.7 (0.6–4.6)
0.106
0.022
0.022
0.834
0.402
0.673
0.076
0.035
0.151
0.554
Values are median (IQR) except for age, which is expressed as mean (SD).
All p values by Wilcoxon’s paired test.
preserve endothelial homeostasis. As Ang-1 has been shown to have anti-apoptotic effects on endothelial cells, 17 18 we speculate that because of the endothelial damage in SCD,
Ang-1 levels are raised in order to provide this support. Our observation of a significant correlation between Ang-1 and vWf in SCD, but not in controls, lends support to this hypothesis.
Destabilisation of growing blood vessels by Ang-2, in the absence of VEGF, leads to vessel regression, whereas such destabilisation in the presence of high VEGF levels facilitates the angiogenic response.
9–11 Thus, the precise balance of
VEGF and the angiopoetin/Tie-2 system is important in determining whether or not vessels auto-infarct and regress/ atrophy or proliferate and become leaky. We would therefore expect that in PSR patients, retinal vaso-occlusion leads to retinal ischaemia and hypoxia, which induces high levels of
VEGF and Ang-2. Conversely, in patients without retinopathy, there might be relatively greater retinal vaso-occlusion possibly also accompanied by greater levels of auto-infarction—leading to less retinal ischaemia and less hypoxia than in PSR patients, and lower levels of VEGF and Ang-2 than in
PSR patients. It follows that Ang-2, in the presence of very low levels of VEGF, might induce neovascular regression.
An ‘‘angiogenic index,’’ reflecting the ratio of Ang-2 to
VEGF and/or the combined angiopoietins to VEGF might be indicators of the presence or development of PSR, with a low index (high Ang-2/high VEGF) indicating the tendency to new vessel proliferation and leakiness, and a high index
(mid-high Ang2/low VEGF) indicating tendency to neovascular regression and atrophy. Our observations of lower ratios of the angiopoietins (individually or combined) in SCD compared to AA subjects as well as the trend of lower Ang-2/
VEGF from ‘‘no retinopathy’’ to PSR is consistent with this.
In SCD, the strong intercorrelations among the growth factors, suggest a high degree of coordinated and complementary angiogenic activity and perhaps a role for these factors in abnormal angiogenesis in SCD; however, no clear patterns emerged according to severity of retinopathy.
The role of the angiopoietins and their interaction with
VEGF (if any) in retinal neovascularisation is not fully understood. In human retinal tissue, Ang-2 and Tie-2 expression appears to be associated with ischaemic retinal disorders in SCD.
20
19 and VEGF expression with abnormal proliferation
However, the idea that angiogenic activity is further heightened in SCD patients with PSR was not supported by the present findings. The observed lack of difference in any molecule among the SCD patients may be attributable to their existing elevated levels that may obscure any further increase in their levels in different eye conditions.
ACKNOWLEDGEMENTS
We thank the staff of the Sickle Cell and Thalassemia Centre, City
Hospital, for their support of this research. We gratefully acknowledge the funding of the Sandwell and West Birmingham Hospitals
NHS Trust Research and Development programme for the
Haemostasis Thrombosis and Vascular Biology Unit.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
J S Mohan, A D Blann, G Y H Lip, Haemostasis, Thrombosis and
Vascular Biology Unit, University Department of Medicine, The
Birmingham and Midland Eye Centre, City Hospital, Birmingham B18
7QH, UK
J S Mohan, D Bareford, Department of Haematology, The Birmingham and Midland Eye Centre, City Hospital, Birmingham B18 7QH, UK
P L Lip, Department of Ophthalmology, The Birmingham and Midland
Eye Centre, City Hospital, Birmingham B18 7QH, UK
Correspondence to: Professor G Y H Lip, University Department of
Medicine, City Hospital, Birmingham B18 7QH, UK; g.y.h.lip@bham.
ac.uk
Accepted 12 November 2004
REFERENCES
1 Moriarty BJ , Acheson RW, Condon PI, et al.
Patterns of visual loss in untreated sickle cell retinopathy.
Eye 1988; 2 :330–5.
2 Goldberg MF . Natural history of untreated proliferative sickle retinopathy.
Arch Ophthalmol 1971; 85 :428–37.
3 Fox PD , Rupert Vessey SJ, Forshaw ML, et al.
Influence of genotype on the natural history of untreated proliferative sickle retinopathy—an angioraphic study.
Br J Ophthalmol 1991; 75 :229–31.
4 Shima DT , Deutsch U, D’Amore PA. Hypoxic induction of vascular endothelial growth factor (VEGF) in human epithelial cells is mediated by increases in mRNA stability.
FEBS Lett 1995; 370 :203–8.
5 Aiello LP , Avery RL, Arrigg PG, et al.
Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders.
N Engl J Med 1994; 331 :1480–7.
6 Aiello LP , Northrup JM, Keyt BA, et al.
Hypoxic regulation of vascular endothelial growth factor in retinal cells.
Arch Ophthalmol
1995; 113 :1538–44.
7 Lip PL , Belgore F, Blann AD, et al.
Plasma VEGF and soluble VEGF receptor
Flt-1 in proliferative retinopathy; relationship to endothelial dysfunction and laser treatment.
Invest Ophthalmol Vis Sci 2000; 41 :2115–19.
8 Barleon B , Hauser S, Schollmann C, et al.
Differential expression of the two
VEGF receptors flt and KDR in placenta and vascular endothelial cells.
J Cell
Biochem 1994; 54 :56–66.
9 Maisonpierre PC , Suri C, Jones PF, et al.
Angiopoietin-2, a natural antagonist for Tie-2 that disrupts in vivo angiogenesis.
Science 1997; 277 :55–60.
10 Holash J , Maisonpierre PC, Compton D, et al.
Vessel cooption, regression, and growth in tumors mediated by angiopoietins and VEGF.
Science
1999; 284 :1994–8.
www.bjophthalmol.com
Angiopoietin/Tie-2 in proliferative sickle retinopathy 819
11 Holash J , Wiegand SJ, Yancopoulos GD. New model of tumor angiogenesis: dynamic balance between vessel regression and growth mediated by angiopoietins and VEGF.
Oncogene 1999; 18 :5356–62.
12 Mandriota SJ , Pepper MS. Regulation of angiopoietin-2 mRNA levels in bovine microvascular endothelial cells by cytokines and hypoxia.
Circ Res
1998; 83 :852–9.
13 Oh H , Takagi H, Suzuma K, et al.
Hypoxia and vascular endothelial growth factor selectively up-regulateangiopoietin-2 in bovine microvascular endothelial cells.
J Biol Chem 1999; 274 :15732–9.
14 Otani A , Takagi H, Oh H, et al.
Expressions of angiopoietins and Tie-2 in human choroidal neovascular membranes.
Invest Ophthalmol Vis Sci 1999; 40 :1912–20.
15 Solovey A , Gui L, Ramakrishnan S, et al.
Sickle cell anemia as a possible state of enhanced anti-apoptotic tone: survival effect of vascular endothelial growth factor on circulating and unanchored endothelial cells.
Blood 1999; 93 :3824–30.
16 Blann AD , Marwah S, Serjeant G, et al.
Platelet activation and endothelial cell dysfunction in sickle cell disease is unrelated to reduced antioxidant capacity.
Blood Coag Fibrinolys 2003; 14 :255–9.
17 Kim I , Kim HG, So JN, et al.
Angiopoietin-1 regulates endothelial cell survival through the phosphatidylinositol 3’-Kinase/Akt signal transduction pathway.
Circ Res 2000; 86 :24–9.
18 Harfouche R , Hassessian HM, Guo Y, et al.
Mechanisms which mediate the antiapoptotic effects of angiopoietin-1 on endothelial cells.
Microvasc Res
2002; 64 :135–47.
19 Takagi H , Koyama S, Seike H, et al.
Potential role of the angiopoietin/Tie-2 system in ischemia-induced retinal neovascularization.
Invest Ophthalmol Vis
Sci 2003; 44 :393–402.
20 Cao J , Mathews MK, McLeod DS, et al.
Angiogenic factors in human proliferative sickle cell retinopathy.
Br J Ophthalmol 1999; 83 :838–46.
Clinical Evidence—Call for contributors
Clinical Evidence is a regularly updated evidence-based journal available worldwide both as a paper version and on the internet.
Clinical Evidence needs to recruit a number of new contributors. Contributors are healthcare professionals or epidemiologists with experience in evidence-based medicine and the ability to write in a concise and structured way.
Areas for which we are currently seeking authors:
N
Child health: nocturnal enuresis
N
Eye disorders: bacterial conjunctivitis
N
Male health: prostate cancer (metastatic)
N
Women’s health: pre-menstrual syndrome; pyelonephritis in non-pregnant women
However, we are always looking for others, so do not let this list discourage you.
Being a contributor involves:
N
Selecting from a validated, screened search (performed by in-house Information
Specialists) epidemiologically sound studies for inclusion.
N
Documenting your decisions about which studies to include on an inclusion and exclusion form, which we keep on file.
N
Writing the text to a highly structured template (about 1500–3000 words), using evidence from the final studies chosen, within 8–10 weeks of receiving the literature search.
N
Working with Clinical Evidence editors to ensure that the final text meets epidemiological and style standards.
N
Updating the text every six months using any new, sound evidence that becomes available.
The Clinical Evidence in-house team will conduct the searches for contributors; your task is simply to filter out high quality studies and incorporate them in the existing text.
N
To expand the topic to include a new question about once every 12–18 months.
If you would like to become a contributor for Clinical Evidence or require more information about what this involves please send your contact details and a copy of your CV, clearly stating the clinical area you are interested in, to Klara Brunnhuber (kbrunnhuber@ bmjgroup.com).
Call for peer reviewers
Clinical Evidence also needs to recruit a number of new peer reviewers specifically with an interest in the clinical areas stated above, and also others related to general practice. Peer reviewers are healthcare professionals or epidemiologists with experience in evidence-based medicine. As a peer reviewer you would be asked for your views on the clinical relevance, validity, and accessibility of specific topics within the journal, and their usefulness to the intended audience (international generalists and healthcare professionals, possibly with limited statistical knowledge). Topics are usually 1500–3000 words in length and we would ask you to review between 2–5 topics per year. The peer review process takes place throughout the year, and our turnaround time for each review is ideally 10–14 days.
If you are interested in becoming a peer reviewer for Clinical Evidence , please complete the peer review questionnaire at www.clinicalevidence.com or contact Klara
Brunnhuber (kbrunnhuber@bmjgroup.com).
www.bjophthalmol.com
820
SCIENTIFIC REPORT
Abnormal crossing of the optic fibres shown by evoked magnetic fields in patients with ocular albinism with a novel mutation in the
OA1
gene
L Lauronen, R Jalkanen, J Huttunen, E Carlsson, S Tuupanen, S Lindh, H Forsius, E-M Sankila,
T Alitalo
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :820–824. doi: 10.1136/bjo.2004.060582
Aim: To perform genealogical and clinical studies in Finnish families with X linked ocular albinism (OA1), including characterisation of the potential misrouting of optic fibres by evaluating visual evoked magnetic fields (VEFs), and to determine the mutation behind the disease.
Methods: Three families with OA1 were clinically examined.
VEFs were measured in two affected males and in one female carrier to characterise the cortical activation pattern after monocular visual stimulation. The neuronal sources of the
VEFs were modelled with equivalent current dipoles (ECDs) in a spherical head model. All coding exons of the OA1 gene were screened for mutations by single strand conformation analysis and direct polymerase chain reaction sequencing.
Results: Genealogical studies revealed that the three families were all related. The affected males had foveal hypoplasia with reduced visual acuity varying from 20/200 to 20/50, variable nystagmus, iris transillumination, and hypopigmentation of the retinal pigment epithelium. The ECD locations corresponding to the VEFs revealed abnormal crossing of the optic fibres in both affected males, but not in the carrier female. A novel point mutation, leading to a STOP codon, was identified in the fifth exon of the OA1 gene.
Conclusions: The data indicate that the novel mutation
640C .
T in the OA1 gene is the primary cause of the eye disease in the family studied. VEFs with ECD analysis was successfully used to demonstrate abnormal crossing of the optic fibres.
T births.
1 he X chromosomal Nettleship-Falls type ocular albinism
(OA1; OMIM 300500) is the most common form of ocular albinism with a prevalence of 1 in 60 000 live
Affected males have reduced visual acuity, nystagmus, iris translucency, fundus hypopigmentation, foveal hypoplasia, and loss of stereoscopic vision.
2–5 Skin colour of the patients appears to be normal.
4 6 The disease results from abnormal distribution of melanin. Microscopic examination of histological samples typically reveals macromelanosomes in pigment cells of skin and eye.
7 8 Carrier females are usually asymptomatic, but because of random X inactivation, 9 the majority of them show some signs of carriership including pigment changes in the fundus, iris translucency, and macromelanosomes in skin biopsy.
10–12
The disease phenotype results from mutations in the OA1 gene (albinism database: albinismdb.med.umn.edu/). The gene has been localised to Xp22.32, 13–16 and it consists of nine exons, encoding a protein of 404 amino acids.
17 18 The OA1 gene product is an intracellular G protein coupled receptor that localises to melanosomes, and is shown to be involved in melanosome biogenesis and maturation.
19–21
A typical feature of ocular albinism is abnormal crossing of the visual pathways at the chiasma: the majority of the fibres from each eye cross to the contralateral hemisphere, while in healthy subjects, only fibres from the nasal half of the retina cross. Accordingly, abnormal lateralisation of visual evoked potentials (VEPs) to monocular stimulation has been reported in ocular albinism, 22–25 although in some studies no abnormal lateralisation has been found.
26 A potential difficulty in evaluating VEP studies is that these have usually been recorded from a limited number of channels, which precludes accurate estimation of the underlying neuronal generators. In magnetoencephalography (MEG), the active brain areas are detected by recording the weak magnetic fields caused by activation of neuronal populations at the cortex.
27 In contrast with electric potentials, the magnetic fields are not altered by the different conductivities of the intervening tissues. Therefore, with multichannel MEG devices, the accurate location and strength of the neuronal generators of evoked responses can frequently be determined.
Thus, it is possible—for example, by recording visual evoked magnetic fields (VEFs), to determine whether a half field visual stimulus activates the visual cortex ipsilaterally or contralaterally to the stimulated eye. We have previously reported preliminary results to half field checkerboard stimulation in patients with ocular albinism.
28 Recently,
Ohde et al 29 used VEFs to show misrouting of the optic fibres in one patient with ocular albinism and two patients with oculocutaneous albinism. However, they used stroboscopic light with monocular or binocular stimulation instead of half field stimulation.
This study was conducted to evaluate clinical findings, including characterisation of the misrouting of the optic fibres with VEFs, in patients with X chromosomal ocular albinism. Molecular genetic analysis of the OA1 gene was performed to determine the mutation behind the disease.
MATERIALS AND METHODS
Clinical studies
Subjects and ophthalmic examination
Patients and carriers belonging to the three families
(descendants of VII-2, VII-5, and VII-10, fig 1) were clinically studied. Ocular examinations were performed using a Haag-
Streit slit lamp microscope and a 90 D or a three mirror lens.
Since the patients of the three families appeared to have both
Abbreviations: ECD, equivalent current dipole; MEG, magnetoencephalography; OA, ocular albinism; PCR, polymerase chain reaction; RPE, retinal pigment epithelium; SSCA, single strand conformation analysis; VEF, visual evoked magnetic field; VEP, visual evoked potential www.bjophthalmol.com
Novel mutation in the OA1 gene 821
1 2 3
I
1 2 3 4 5
II
1 2 3 4 5 6 7
III
IV
1 2 3 4 5 6 7 8
V
1
6
8 9 10
2 3
VI
VII
1 2 3 4 5 6 7 8 9 10 11
VIII
IX
1
1
2
2
1 2 3 4 5
3
3
4 5
4
6
5
7
6
8
6
7 8
M
9 10
7
9 10
M
8
11
9
11
M
12 13 14 15 16
12 13 14 15 16 17 18 19 20
17 18
10 11 12
X
1 2
XI
1
11
4
12
5
?
6 7
Figure 1 Pedigree of the Finnish OA1 family. Members of the I–VII generation are all dead, generations VIII–XI as shown.
* Indicates individuals who took part in molecular studies. M, patients examined by magnetoencephalography. Black squares, affected males; shaded squares, males having poor eyesight according to church registers; open circles with a black dot, carrier females; and open symbols, unaffected individuals. Question mark indicates that the phenotype is unknown.
a similar phenotype and ancestors from the island of Seiskari, we initiated genealogical studies using church registers to find out whether the families are related.
Magnetoencephalography
Two brothers (IX-8 and IX-10) with OA1, one carrier female
(VIII-11), and five healthy control subjects (age range 23–
51 years) underwent VEF studies. The two patients and all controls were measured with a 122 channel gradiometer
(Neuromag Ltd, Helsinki, Finland) and the carrier with a 306 channel system (Elekta Neuromag, Oy, Helsinki, Finland), located inside a magnetically shielded room. The subject sat with his/her head positioned inside the helmet-shaped sensor array, and watched a fixation point in the middle of the stimulus screen placed 1.5 metres in front of him/her. The nasal and temporal visual half fields of the left and right eye were stimulated separately with a black and white checkerboard pattern reversing at 1 Hz. The check size was approximately 3 ˚ . Two sets of 200 responses were averaged for both half fields of both eyes. The signals were band pass filtered between 0.1 Hz and 200 Hz and sampled at 616 Hz.
Epochs containing amplitudes exceeding 3000 fT/cm in the
MEG channels or 150 m V in the electro-oculogram were automatically discarded. An epoch lasted 600 ms, including a
100 ms prestimulus baseline. The evoked local cortical activity was modelled with equivalent current dipoles
(ECDs), representing the location, orientation, and strength of localised cortical activation.
27 The ECD locations were given in a cartesian head coordinate system, were the x axis passes through the preauricular points from left to right, the positive y axis passes through nasion, and the z axis points upwards.
The ECDs at the time of the most prominent activity (at about
100 ms after stimulus) were used in the analyses.
Molecular studies
DNA was extracted from blood samples using standard methods. All nine coding exons of OA1 were polymerase chain reaction (PCR) amplified from genomic DNA. Mutation analysis was carried out using single strand conformation analysis (SSCA), 30 31 and direct PCR sequencing (ABI310,
Applied Biosystems, Foster City, CA, USA).
RESULTS
Genealogical studies and clinical data
The three families were traced back to the 18th century using church registers. A common forefather, born on the island of
Seiskari in 1700, was identified (fig 1). Of the eight males studied, seven had foveal hypoplasia and hypopigmented fundi with visible choroidal vessels (table 1). Male IX-11 had foveal hypoplasia but normally pigmented fundi. Optic discs were slightly or markedly pale in four males. Male XI-2 had congenital nystagmus and strabismus and was first examined as a baby. His VEP recordings suggested misrouting of the optic fibres. All the six clinically studied carriers showed some carrier manifestations (table 2).
Table 1 Clinical findings of eight affected males
Pedigree code
VIII-9
IX-8
IX-10
IX-11
X-2
X-3
X-5
XI-2
Age
(years)
50
51
54
5
74
44
49
50
Nystagmus
+
+
+
+
+
+
( + ) *
( + ) *
Iris translucency
+
+
+
+
+
+
2
+
* Low frequency nystagmus at lateral gaze.
Refraction after cataract surgery.
VA, visual acuity; R/L, right and left eye; D, dioptre.
VA R//L
20/125//20/125
20/60//20/50
20/100//20/100
20/100//20/100
20/60//20/60
20/200//20/200
20/100//20/100
20/160//20/100
Refractive error (D) R/L
+ 2 0 2 2.5
6 50 / + 1.5
2 1.0
6 105
2 2.5
2 4.0
6 5/ 2 1.0
2 2.0
6 180
+ 2.25
2 6.0
6 160/ + 2.25
2 4.5
6 30
+ 2 0 2 3.5
6 15/ + 1.5
2 3.0
6 160
+ 3.25
2 2.25
6 25/ + 3.25
2 2.0
6 170
+ 5.0
2 1.0
6 170/ + 4.5
2 1.0
6 30
2 2.75
2 2.0
6 20/ 2 3.0
2 2.25
6 170
+ 6.5
2 1.0
6 170/ + 6.25
2 1.0
6 0 www.bjophthalmol.com
822
Table 2 Clinical findings in six female carriers
Pedigree code
VIII-8
VIII-11
IX-2
X-7
X-8
X-9
Age
(years)
70
72
71
23
15
12
Iris translucency
+
+
+
+
2
2
Fundus appearance
Patchy peripheral RPE
Patchy RPE
Patchy RPE
Normal
Patchy RPE
Patchy RPE
* Macular pucker.
Anisometropic amblyopia.
VA, visual acuity; R/L, right and left eye; D, dioptre; RPE, retinal pigment epithelium.
VA R//L
20/60 * //20/20
20/20//20/20
20/25//20/20
20/20//20/20
20/20//20/20
20/20//20/30
Lauronen, Jalkanen, Huttunen, et al
Refractive error (D) R/L
+ 2.25
2 1.5
6 100/ + 3.0
2 1.75
6 75
+ 1.75
2 0.5
6 130/ + 1.5
2 0.5
6 90
2 9.0
2 0.5
6 180/ 2 9.0
+ 2 0/ + 2 0
+ 2 0/ + 2 0
2 9.5/ 2 5.75
Magnetoencephalography
The monocular half field checkerboard stimulation resulted in responses over the occipital area in both controls and patients (fig 2). For stimulation of either eye, in all controls and in the carrier female, the maximum activation was over the left hemisphere for the right half field stimulation, and over the right hemisphere for the left half field stimulation.
In the patients, both left and right half field stimulation resulted in activation over the contralateral hemisphere. The most prominent deflection peaked at about 100 ms (table 3) and was designated as P100m, in analogy to the P100 VEP component. The topographic P100m magnetic field distributions showed dipolar patterns (fig 3), indicating that the
P100m was generated by localised cortical activity amenable to modelling with an ECD. In the patients, the P100m ECD to both left and right half field stimulation of the left eye was in the right visual cortex ( x .
0, table 3). The ECD source locations after stimulation of both half fields were close to each other in the patients, while a clear difference in the lateral direction (on the average 42 mm, table 3) was found in the controls. In the patients, the ECD strength was similar
Figure 3 Isofield contour maps showing the topographic magnetic field distribution at the peak of the P100m VEF deflection. The blue lines indicate magnetic flux entering the head and red lines magnetic flux exiting the head. Data from a control subject are shown at the top and from the two patients in the middle and at the bottom after stimulation of the left eye. In the control, the response to nasal half field stimulation was located ipsilaterally in the left hemisphere, whereas the temporal half field stimulation resulted in activation over the contralateral right hemisphere. In both patients, both the nasal and temporal half field stimulation caused activation over the contralateral right hemisphere.
The arrows denote the corresponding ECDs, size of the arrow being proportional to the ECD strength. The contour step is 20 fT/cm.
Figure 2 Visual evoked magnetic fields (VEFs) to stimulation of the left eye in a control (top) and in patient IX-8 (bottom). In the control, the nasal half field stimulation (blue line) resulted in maximum activation over the ipsilateral occipital area (blue box) and temporal half field stimulation (black line) over the contralateral occipital areas (black box).
In the patient, the maximum responses to stimulation of both half fields were over the contralateral visual cortex; in fact, the responses to both half field stimulations were almost identical. The schematic illustration on the left depicts the corresponding organisation of the optic pathways from the two halves of the retinal to the visual cortex.
to that in the controls for the temporal half field with normally crossing fibres, but clearly weaker for the nasal half field, which showed abnormal crossing (table 3, fig 3).
Mutation analysis
Sequence analysis revealed a novel base substitution,
640C .
T, in the fifth exon of the OA1 gene. This substitution changes the glutamine at position 214 to a stop codon. The mutation co-segregated with the disease phenotype in the
Finnish family and was not found in 140 normal male control samples.
www.bjophthalmol.com
Novel mutation in the OA1 gene 823
Table 3 The mean latencies, locations, and strengths of P100m ECDs for stimulation of the left eye in patients and controls. The standard deviations are in parentheses
Subjects
Patients
(n = 2)
Controls
(n = 5)
Stimulus
Left HF
Right HF
Left HF
Right HF
Latency
(ms)
99 (1)
100 (3)
103 (9)
106 (11)
Coordinates x (mm) y (mm)
20 (3)
26 (1)
34 (5)
2 8 (5)
2 54 (2)
2 59 (1)
2 57 (18)
2 57 (14) z (mm)
42 (2)
50 (1)
57 (7)
56 (11)
Strength
(nAm)
23 (5)
9 (4)
19 (17)
16 (12) g
%
92 (5)
88 (8)
88 (2)
92 (4) g = goodness of fit (indicates how much of the variance in the recorded signal set is explained by the ECD model), HF = half field, ECD = equivalent current dipole. A positive value of the x coordinate indicates right hemisphere, while negative x falls in the left hemisphere.
DISCUSSION
In this study of a large Finnish family, we identified a novel
OA1 mutation, 640C .
T, which leads to a truncated protein product. The predicted mutant protein lacks the putative transmembrane regions VI and VII, part of the transmembrane region V, and also the third sytosolic loop, which may be crucial for downstream signalling of the protein.
32 The mutation resulted in reduced visual acuity in all affected males studied, although iris translucency was absent in one patient, and hypopigmentation of the retina in another.
Preising et al 33 have hypothesised that in OA1, pigmentation of the iridal and the retinal pigment epithelium may increase postnatally because of constant melanin production of melanocytes, while the neuroretinal phenotype resulting in reduced visual acuity is permanent as a result of irreversible damage during embryogenesis. All the female carriers of the
640C .
T mutation studied here had at least some clinical carrier manifestations, but normal visual acuity and normal
VEF responses indicating that the routing of optic pathways was not altered
The optic fibre misrouting in OA1 patients was demonstrated by using VEFs with ECD analysis. The patients’ main
VEF response to stimulation of the nasal half fields was clearly abnormally lateralised to the contralateral hemisphere. Recently, Ohde et al 29 found a predominantly contralateral VEF activation pattern in the occipital cortex of three patients with albinims after full field stroboscopic stimulation. This was in contrast with healthy controls in whom full field stimulation led to more ambiguous activation pattern indicating activation of the visual cortex bilaterally.
Hence, the authors could infer an abnormal crossing of the optic fibres in the patients. In the present study, we have shown perhaps more directly with checkerboard half field stimulation that both hemifields indeed projected to the contralateral visual cortex.
Our results suggest that VEFs to half field stimulation could be used as a diagnostic tool to reveal abnormal crossing of optic fibres in patients suspected of having ocular albinism.
ACKNOWLEDGEMENTS
The authors thank the families with members affected by ocular albinism for participation and Dr Ilkka Kaitila for the help in collecting samples.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
L Lauronen * , J Huttunen, BioMag Laboratory, Helsinki University
Central Hospital, Helsinki, Finland
L Lauronen, Helsinki Brain Research Centre, Helsinki, Finland
L Lauronen, J Huttunen, Department of Clinical Neurophysiology,
Helsinki University Central Hospital, Helsinki, Finland
R Jalkanen * , E Carlsson, S Tuupanen, T Alitalo, Department of
Obstetrics and Gynecology, Helsinki University Central Hospital,
Helsinki, Finland
S Lindh, H Forsius, E-M Sankila, The Folkha¨lsan Institute of Genetics,
Department of Molecular Genetics, Helsinki, Finland
E-M Sankila, Department of Ophthalmology, Helsinki University Central
Hospital, Helsinki, Finland
* These authors contributed equally to this work.
Funding: This study was supported by the Helsinki University Hospital
Grant, TYH1338 (TA), and the Finnish Eye Foundation (E-MS).
Competing interests: No commercial relationships for any authors.
Ethical approval: The study conformed to the tenets of the Declaration of
Helsinki. Informed consent was obtained from all participants in accordance with the requirements of the Helsinki University Central
Hospital, Department of Ophthalmology Ethics Committee.
Correspondence to: Tiina Alitalo, Helsinki University Central Hospital,
Department of OB/GYN, Genetics, Haartmaninkatu 2, PO Box 140,
Helsinki, 00029 HUS, Finland; tiina.alitalo@hus.fi
Accepted for publication 9 November 2004
REFERENCES
1 Rosenberg T , Schwartz M. X-linked ocular albinism: prevalence and mutations—a national study.
Eur J Hum Genet 1998; 6 :570–7.
2 Charles SJ , Green JS, Grant JW, et al.
Clinical features of affected males with
X linked ocular albinism.
Br J Ophthalmol 1993; 77 :222–7.
3 Creel DJ , Summers CG, King RA. Visual anomalies associated with albinism.
Ophthalmic Paediatr Genet 1990; 11 :193–200.
4 Kriss A , Russell-Eggitt I, Harris CM, et al.
Aspects of albinism.
Ophthalmic
Paediatr Genet 1992; 13 :89–100.
5 King RA , Hearing VJ, Creel DJ, et al.
Albinism. In: Scriver CR, Beaudet AL,
Sly WS, et al , eds.
The metabolic and molecular bases of inherited disease .
New York: McGraw-Hill, 2001:5587–627.
6 Creel D , O’Donnell FE Jr, Witkop CJ Jr. isual system anomalies in human ocular albinos.
Science 1978; 201 :931–3.
7 O’Donnell FE Jr , Hambrick GW Jr, Green WR, et al.
X-linked ocular albinism.
An oculocutaneous macromelanosomal disorder.
Arch Ophthalmol
1976; 94 :1883–92.
8 Garner A , Jay BS. Macromelanosomes in X-linked ocular albinism.
Histopathology 1980; 4 :243–54.
9 Lyon MF . Sex chromatin and gene action in the mammalian X-chromosome.
Am J Hum Genet 1962; 14 :135–48.
10 Charles SJ , Moore AT, Grant JW, et al.
Genetic counselling in X-linked ocular albinism: clinical features of the carrier state.
Eye 1992; 6 :75–9.
11 Cortin P , Tremblay M, Lemagne JM. X-linked ocular albinism: relative value of skin biopsy, iris transillumination and funduscopy in identifying affected males and carriers.
Can J Ophthalmol 1981; 16 :121–3.
12 Lang GE , Rott HD, Pfeiffer RA. X-linked ocular albinism. Characteristic pattern of affection in female carriers.
Ophthalmic Paediatr Genet
1990; 11 :265–71.
13 Bergen AA , Zijp P, Schuurman EJ, et al.
Refinement of the localization of the
X-linked ocular albinism gene.
Genomics 1993; 16 :272–3.
14 Fialkow PJ , Giblett ER, Motulsky AG. Measurable linkage between ocular albinism and Xg.
Am J Hum Genet 1967; 19 :63–9.
15 Pearce WG , Sanger R, Race RR. Ocular albinism and Xg.
Lancet
1968; 1 :1282–3.
16 Schnur RE , Nussbaum RL, Anson-Cartwright L, et al.
Linkage analysis in Xlinked ocular albinism.
Genomics 1991; 9 :605–13.
17 Schiaffino MV , Bassi MT, Galli L, et al.
Analysis of the OA1 gene reveals mutations in only one-third of patients with X-linked ocular albinism.
Hum Mol
Genet 1995; 4 :2319–25.
18 Bassi MT , Schiaffino MV, Renieri A, et al.
Cloning of the gene for ocular albinism type 1 from the distal short arm of the X chromosome.
Nat Genet
1995; 10 :13–19.
19 Schiaffino MV , Baschirotto C, Pellegrini G, et al.
The ocular albinism type 1 gene product is a membrane glycoprotein localized to melanosomes.
Proc
Natl Acad Sci USA 1996; 93 :9055–60.
20 Shen B , Rosenberg B, Orlow SJ. Intracellular distribution and late endosomal effects of the ocular albinism type 1 gene product: consequences of www.bjophthalmol.com
824 Lauronen, Jalkanen, Huttunen, et al disease-causing mutations and implications for melanosome biogenesis.
Traffic 2001; 2 :202–11.
21 Schiaffino MV , d’Addio M, Alloni A, et al.
Ocular albinism: evidence for a defect in an intracellular signal transduction system.
Nat Genet
1999; 23 :108–12.
22 Creel D , Witkop CJ Jr, King RA. Asymmetric visually evoked potentials in human albinos: evidence for visual system anomalies.
Invest Ophthalmol
1974; 13 :430–40.
23 Apkarian P , Reits D, Spekreijse H, et al.
A decisive electrophysiological test for human albinism.
Electroencephalogr Clin Neurophysiol 1983; 55 :513–31.
24 Dorey SE , Neveu MM, Burton LC, et al.
The clinical features of albinism and their correlation with visual evoked potentials.
Br J Ophthalmol
2003; 87 :767–72.
25 Pott JW , Jansonius NM, Kooijman AC. Chiasmal coefficient of flash and pattern visual evoked potentials for detection of chiasmal misrouting in albinism.
Doc Ophthalmol 2003; 106 :137–43.
26 Bouzas EA , Caruso RC, Drews-Bankiewicz MA, et al.
Evoked potential analysis of visual pathways in human albinism.
Ophthalmology
1994; 101 :309–14.
27 Ha¨ma¨la¨inen M , Hari R, Ilmoniemi RJ, et al.
Magnetoencephalography— theory, instrumentation and applications to noninvasive studies of the working human brain.
Rev Mod Phys 1993; 65 :414–97.
28 Lauronen L , Sankila E-M, Salmi T, et al.
Visual evoked magnetic fields in the detection of optic pathway misrouting in ocular albinism [abstract]. In:
BioMag2002 . Jena, Germany, 2002.
29 Ohde H , Shinoda K, Nishiyama T, et al.
New method for detecting misrouted retinofugal fibers in humans with albinism by magnetoencephalography.
Vis
Res 2004; 44 :1033–8.
30 Orita M , Iwahana H, Kanazawa H, et al.
Detection of polymorphisms of human DNA by gel electrophoresis as single-strand conformation polymorphisms.
Proc Natl Acad Sci USA 1989; 86 :2766–70.
31 Bassam BJ , Caetano-Anolles G, Gresshoff PM. Fast and sensitive silver staining of DNA in polyacrylamide gels.
Anal Biochem 1991; 196 :80–3.
32 d’Addio M , Pizzigoni A, Bassi MT, et al.
Defective intracellular transport and processing of OA1 is a major cause of ocular albinism type 1.
Hum Mol Genet
2000; 9 :3011–8.
33 Preising M , Op de Laak JP, Lorenz B. Deletion in the OA1 gene in a family with congenital X linked nystagmus.
Br J Ophthalmol 2001; 85 :1098–103.
ECHO
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
RP1 mutations cause autosomal recessive retinitis pigmentosa
Please visit the
British Journal of
Ophthalmology website [www.
bjophthalmol.
com] for a link to the full text of this article.
R P1 gene mutations have been discovered for the first time in autosomal recessive retinitis pigmentosa (RP), according to a study of consanguineous Pakistani families with the condition. They are not a major cause of the disorder in Pakistanis, say the researchers.
All affected members of two families were homozygous at the RP1 locus, whereas their parents and unaffected siblings were heterozygous. A homozygous C R T missense mutation at nucleotide 1118 (thre R isoleu at codon 373) segregated with affected family members.
Unaffected members were all heterozygous for the mutation, and 100 ethnically matched, unrelated, healthy controls showed no homozygous mutation. A third family had a homozygous four base pair insertion at 1461–65 TGAA, producing a stop codon and a drastically shortened protein product. Again, the mutation segregated with affected family members; it was present in some other members and parents of affected members as a heterozygous mutation but not in the controls. Affected members of all three families had severe RP and were completely blind by age 18 years. Finally, a new heterozygous G R A missense mutation at nucleotide 2005 (ala R thre at codon 669) was found in one patient in a random panel of 150 patients with RP screened for RP1 mutations, but not in the controls.
All patients, their parents, and some of their unaffected siblings were thoroughly investigated and had electroretinographic examinations. Mutational analysis comprised amplification of DNA from blood samples, heteroduplex analysis, and direct DNA sequencing.
All previously known mutations in the RP1 gene cause autosomal dominant RP.
m
Khaliq S, et al .
Journal of Medical Genetics 2005; 42 :436–438.
www.bjophthalmol.com
825
SCIENTIFIC REPORT
Human extraocular muscles in mitochondrial diseases: comparing chronic progressive external ophthalmoplegia with Leber’s hereditary optic neuropathy
A Carta, V Carelli, T D’Adda, F N Ross-Cisneros, A A Sadun
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :825–827. doi: 10.1136/bjo.2004.060590
Aims: To compare the ultrastructural aspects of human extraocular muscles in two types of mitochondrial disease: chronic progressive external ophthalmoplegia (CPEO) and
Leber’s hereditary optic neuropathy (LHON).
Methods: Muscle samples of the medial rectus obtained from surgery in a sporadic case of CPEO associated with deleted mitochondrial DNA, and post mortem in a case of 3460/
ND1 LHON were processed for electron microscopy (EM).
The medial rectus from an autoptic time to fixation matched control was used to exclude postmortem artefacts.
Results: The CPEO specimen revealed focal areas of disruption and abnormalities of mitochondria in some muscle fibres, creating a ‘‘mosaic-like’’ pattern. In the LHON specimen a diffuse increase in both number and size of mitochondria (mean diameter 0.85
m m v 0.65
m m of control, p , 0.0001) with swollen appearance and disorganised cristae filled all spaces of sarcoplasmic reticulum. In some areas the excessive number of mitochondria slightly distorted myofibrils.
Conclusion: EM investigation of extraocular muscles in CPEO and LHON reveals marked differences. A ‘‘mosaic-like’’ pattern caused by a selective damage of muscle fibres was evident in CPEO, whereas a diffuse increase in mitochondria with preservation of myofibrils characterised the LHON case.
These ultrastructural changes may relate to the different expression of the two diseases, resulting in ophthalmoplegia in CPEO and normal eye movements in LHON.
T he extraocular muscles (EOMs) are among the fastest and yet most fatigue resistant skeletal muscles in the body. The complexity of actions performed by the EOMs is reflected in their cytoarchitecture and fibre type composition, which differ from ordinary skeletal muscles in many respects, including motor unit properties.
1 Their activity (of both saccades and pursuit movements) is continuous and highly energy dependent. Fatigue resistance may be the result of their use of glycolytic or oxidative enzymes, their mitochondrial content, and the extensive capillary network associated with individual myofibres. However, these biochemical characteristics and the elevated energy requirements expose EOMs to be targeted by mitochondrial dysfunction.
Both chronic progressive external ophthalmoplegia (CPEO) and Leber’s hereditary optic neuropathy (LHON) are the result of mitochondrial DNA (mtDNA) mutations that lead to mitochondrial dysfunction. CPEO is characterised by progressive loss of muscles activity and near complete ophthalmoplegia at the late stages.
2 On the other hand, LHON leads to optic neuropathy but is not associated with EOM dysfunction.
3 However, ultrastructural alterations in EOMs have been reported in a single case described at necropsy of
LHON carrying the 11778/ND4 mtDNA mutation.
4 In a previous report we studied the medial rectus muscle in a case of sporadic CPEO carrying a heteroplasmic mtDNA macrodeletion.
5
Here we report the ultrastructural features in the medial rectus (MR) of a further LHON case carrying the 3460/ND1 mutation in comparison with the previously reported CPEO case and with an age matched control. The quantitative and qualitative differences in myofibrillary damage, in relation to the different pathophysiology of these mtDNA defects, may explain the phenotypical expression in LHON and CPEO.
MATERIALS AND METHODS
The medial recti (MR) from three patients were obtained at surgery or necroscopy and prepared for ultrastructural analysis. Muscle was obtained from a 48 year old white male, affected since his 20s by a sporadic form of CPEO and carrying the heteroplasmic mtDNA ‘‘common deletion,’’ who underwent strabismus surgery because of a high degree of exotropia, as already detailed.
5 The second case was obtained at necropsy from a previously reported 75 year old white female with LHON carrying the mtDNA mutation at position
3460/ND1 in homoplasmic form.
6 The third muscle (normal control) was obtained from a 72 year old white female cornea donor after her death, which had been secondary to a cardiac infarction. The postmortem times to fixation for the normal and LHON cases were 20 hours and 24 hours, respectively.
All muscle specimens were immediately fixed in Karnovsky solution for 3 hours at room temperature, postfixed in
1% osmium tetroxide, dehydrated in graded acetone, and embedded in Araldite (Fluka Chemie, AG, Buchs,
Switzerland). Ultrathin (80 nm thick) sections were stained with uranyl acetate-lead citrate, and examined with a Philips
EM 208S electron microscope (Fei Electron Optics BV,
Eindhoven, Netherlands). In LHON and in the normal control case the diameter of a randomly chosen sample of mitochondria was calculated using the software analySIS
(Soft Imaging System GmbH, Munster, Germany).
Differences in the median diameter values between the two groups have been evaluated with the non-parametric Mann-
Whitney test for independent samples. Two sided p values less than 0.05 have been considered statistically significant.
RESULTS
Low magnification electron microscopy (EM) of the CPEO specimen showed normal myofibrils adjacent to abnormal myofibrils that had diffuse sarcomeric ultrastructural
Abbreviations: CPEO, chronic progressive external ophthalmoplegia;
EM, electron microscopy; EOMs, extraocular muscles; LHON, Leber hereditary optic neuropathy; MR, medial recti www.bjophthalmol.com
826 Carta, Carelli, D’Adda, et al
Figure 1 CPEO case. (A) Electron micrograph showing a normal fibre
(left side) in close proximity to an altered, swollen one. This pattern of distribution is observed within all the muscle examined, creating a
‘‘mosaic-like profile’’ (original magnification 6 24 000). (B) High magnification electron micrograph shows an altered muscle fibre. Many mitochondria have lost their inner cristae, thus creating a ‘‘ghost profile,’’ with a swollen appearance producing muscle displacement
(original magnification 6 40 000).
Figure 2 LHON case. All sarcoplasmic spaces are filled by mitochondria which occupy up to two thirds of the total muscle cells cytoplasm. The accumulation of mitochondria creates a ‘‘mitochondrial stream’’ (see between arrows) with distortion of myofibrils in some areas. Within many mitochondria can be seen elaboration and stacking of cristae (original magnification 6 8900).
paracrystalline structure in either disease after computer retrival of all images was performed.
These ultrastructural aspects were not likely related to postmortem artefacts, as suggested by the comparison with the postmortem time to fixation matched control.
DISCUSSION
The results of the present study point to the differences in the underlying pathophysiology between CPEO and LHON. The mtDNA ‘‘common deletion’’ in CPEO has the potential to produce much more severe disruption of mitochondrial oxidative phosphorylation (OXPHOS) than the point mutations in LHON.
2 In fact, this mutation is lethal in homoplasmic form and is always found heteroplasmic—that is, a mixture of wild type and mutant mtDNA genomes which may distribute with different loads in mitochondria within cells and tissues.
In contradistinction, the present case of LHON was homoplasmic mutant in relation to the milder OXPHOS impairment in LHON.
3 Morever, not only homoplasmic mutant mtDNA is compatible with life, but in most cases does not even induce the optic nerve pathology for which the co-occurrence of a further nuclear genetic modifying factor or of environmental exposure to trigger factors is currently alterations which resulted in a ‘‘mosaic-like’’ pattern (fig 1A).
Areas of mitochondrial swelling were often close to the normal mitochondria in an adjacent myofibril. At high magnification EM, abnormal fibres showed sarcomeric swelling and the presence of ‘‘ghost’’ mitochondrial profiles with partial to complete matrix emptying, whereas the external membrane was generally preserved (fig 1B). In other instances a profound rearrangement of the cristae with an ‘‘onion ring-like’’ appearance was also observed. The damage within muscle fibres appeared selectively distributed.
The number of mitochondria appeared not be increased without any evidence of inflammation or fibrosis.
In the LHON specimen there were an increased number of mitochondria which took up to two thirds of the sarcomeric space producing in some areas local distortion of myofibril organisation (fig 2). Otherwise the architecture of the muscle fibres was normal with a regular alternation of actin and myosin filaments and empty mitochondria forming dense clusters organised in columns in the sarcoplasmic reticulum
(fig 3). Frequent abnormal disruption and re-arrangement of the cristae characterised the LHON mitochondria, without any evidence of inflammation or fibrosis. The abnormalities of mitochondrial populations in LHON were seen homogeneously distributed throughout the specimen. Many mitochondria were characterised by homogeneous electron dense inclusions and flocculent material (fig 4). Moreover, most mitochondria had an increased size and a ‘‘swollen appearance’’ with a median diameter of 0.85
m m. This increase was very significant if compared to the normal autoptic control (p , 0.0001). We were unable to identify any
Figure 3 LHON case. The regular cytoarchitecture of the muscle fibre is appreciable. The anomalous ultrastructural features are the presence of swollen mitochondria which have increased their size two to three times
(average median diameter is 0.85
m m as measured on random sample).
They are organised in columns between myofilaments forming dense clusters in the sarcoplasmic reticulum (original magnification 6 11 000).
www.bjophthalmol.com
Ultastructural features of extraocular muscle in mitochondrial diseases 827
Figure 4 LHON case. Electron microscopic appearance of woolly bodies (arrowheads) and electron dense inclusion (arrows) of uncertain interpretation, probably related to mitochondrial matrix degeneration
(original magnification 6 41 000).
postulated.
7 Thus, each cell in the LHON case carries all mtDNA molecules harbouring the 3460/ND1 mutation.
The hallmark of the CPEO case was the ‘‘selective damage’’ of specific myofibrils: while some of the fibres were clearly abnormal, others showed a regular sarcoplasmic architecture without any evidence of damage. This selectivity is best explained by mosaic heteroplasmy with clonally expanded high mutant load and under-threshold low mutant load in different myofibrils. The same ‘‘mosaic-like’’ pattern is usually found in skeletal muscles biopsies of CPEO patients, which reveal the presence of classic ‘‘ragged red fibres’’ with cytochrome c oxidase negative histoenzymatic staining intercalated with normal fibres.
2
However, in CPEO there may be a complete loss of function in EOMs (strabismus fixus is a clinical landmark for CPEO) yet most other skeletal muscle is clinically not affected. Thus, heteroplasmy can only partially explain the prevalent involvement of EOMs. A possible explanation may be that
80% of EOMs fibres are type IIA singly innervated or global red singly innervated (myosin isoform expression and high mitochondrial content). These muscle fibres are strictly aerobic and may be more vulnerable in CPEO.
The ‘‘mosaic-like profile’’ observed may also reflect the sparing of the fibre types with anaerobic metabolic capacity and fast type ATPase profile (myosin heavy chain profile type
IIB and IIC of skeletal muscle fibres).
In contradistinction, our study of the 3460/ND1 LHON muscle demonstrated a different hallmark feature represented by the increased number of mitochondria filling up to two thirds of myofibrils sarcoplasm. Many of these mitochondria showed a swollen appearance with elongated and stretched inner cristae, similar to a previously described
LHON case carrying the 11778/ND4 mutation.
4 In the currently studied 3460/ND1 LHON case the cytoarchitecture of the muscle was essentially preserved without evidence of disorganised or impoverished myofibrils, nor inflammation or fibrosis. These ultrastructural findings in LHON support the general notion that an increase in mitochondria is, in muscles, a compensatory response to a decreased OXPHOS efficiency, particularly in EOMs.
2 8
The ultrastructural features we have described in this study may be related to the phenotypic differences in these two mitochondrial disorders. In CPEO the mitochondrial changes in EOMs seem more severe and lead to ophthalmoplegia, whereas in LHON the mitochondria are mostly increased in number and clinically the EOMs are never affected. Thus, it is plausible to hypothesise that in LHON the increase in mitochondrial number is a successful compensatory strategy for EOMs and skeletal muscle, despite evidence of subclinical impairment.
3 8 However, in LHON this compensatory strategy does not seem to work in the small calibre axons composing the papillomacular bundle of the optic nerve. In the latter physical constrains may limit the size and transport of mitochondria eventually leading to energy depletion and retinal ganglion cells degeneration.
3 9 10 At the present time, there is no proved form of therapy for LHON, CPEO, or any other genetic mitochondrial disease. Further studies should dissect in deep the intracellular events induced by mitochondrial impairment and the strategies operated by different tissues leading to presence or absence of clinical symptoms as an essential step towards devising a strategy for treatment.
ACKNOWLEDGEMENTS
The authors thank Ms Antonella Piazza from the University of Parma for technical assistance in reviewing the English version of this paper.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
A Carta, Institute of Ophthalmology, University of Parma, Parma, Italy
T D’Adda, Institute of Anatomic Pathology, University of Parma, and the
Department of Neurological Sciences, Italy
V Carelli, University of Bologna, Italy
F N Ross-Cisneros, A A Sadun, V Carelli, Department of
Ophthalmology, Doheny Eye Institute, Keck/USC School of Medicine,
Los Angeles, CA, USA
Correspondence to: Arturo Carta, MD, Neuro-Ophthalmology Service,
Head and Neck Department, University of Parma, Via Gramsci 14,
43100 Parma, Italy; acarta@unipr.it
Accepted for publication 1 December 2004
REFERENCES
1 Porter JD , Baker RS, Ragusa RJ, et al.
Extraocular muscles: basic and clinical aspects of structure and function.
Surv Ophthalmol 1995; 39 :451–84.
2 Smeitink J , van den Heuvel L, DiMauro S. The genetics and pathology of oxidative phosphorylation.
Nat Rev Genet 2001; 2 :342–52.
3 Carelli V , Ross-Cisneros FN, Sadun AA. Mitochondrial dysfunction as a cause of optic neuropathies.
Prog Retin Eye Res 2004; 23 :53–89.
4 Sadun AA , Kashima Y, Wurdeman AE, et al.
Morphological findings in the visual system in a case of Leber’s hereditary optic neuropathy.
Clin Neurosci
1994; 2 :165–72.
5 Carta A , D’Adda T, Carrara F, et al.
Ultrastructural analysis of extraocular muscle in chronic progressive external ophthalmoplegia.
Arch Ophthalmol
2000; 118 :1441–5.
6 Sadun AA , Win PH, Ross-Cisneros FN, et al.
Leber’s hereditary optic neuropathy differentially affects smaller axons in the optic nerve.
Trans Am
Ophthalmol Soc 2000; 98 :223–35.
7 Carelli V , Giordano C, d’Amati G. Pathogenic expression of homoplasmic mtDNA mutations needs a complex nuclear-mitochondrial interaction.
Trends
Genet 2003; 19 :257–62.
8 Wredenberg A , Wibom R, Wilhelmsson H, et al.
Increased mitochondrial mass in mitochondrial myopathy mice.
Proc Natl Acad Sci USA
2002; 99 :15066–71.
9 Sadun AA . Mitochondrial optic neuropathies.
J Neurol Neurosurg Psychiatry
2002; 72 :423–5.
10 Sadun AA . Acquired mitochondrial impairment as a cause of optic nerve disease.
Trans Am Ophthalmol Soc 1998:881–923.
www.bjophthalmol.com
828
SCIENTIFIC REPORT
The effect of digital image resolution and compression on anterior eye imaging
R C Peterson, J S Wolffsohn
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :828–830. doi: 10.1136/bjo.2004.062240
Aim: To determine the theoretical and clinical minimum image pixel resolution and maximum compression appropriate for anterior eye image storage.
Methods: Clinical images of the bulbar conjunctiva, palpebral conjunctiva, and corneal staining were taken at the maximum resolution of Nikon:CoolPix990 (2048 6 1360 pixels), DVC:1312C (1280 6 811), and JAI:CV-S3200
(767 6 569) single chip cameras and the JVC:KYF58
(767 6 569) three chip camera. The images were stored in
TIFF format and further copies created with reduced resolution or compressed. The images were then ranked for clarity on a 15 inch monitor (resolution 1280 6 1024) by 20 optometrists and analysed by objective image analysis grading. Theoretical calculation of the resolution necessary to detect the smallest objects of clinical interest was also conducted.
Results: Theoretical calculation suggested that the minimum resolution should be > 579 horizontal pixels at 25 6 magnification. Image quality was perceived subjectively as being reduced when the pixel resolution was lower than
767 6 569 (p , 0.005) or the image was compressed as a
BMP or , 50% quality JPEG (p , 0.005). Objective image analysis techniques were less susceptible to changes in image quality, particularly when using colour extraction techniques.
Conclusion: It is appropriate to store anterior eye images at between 1280 6 811 and 767 6 569 pixel resolution and at up to 1:70 JPEG compression.
T wo of the major considerations with digital imaging are the resolution needed to image the object of interest and the compression that can be utilised to minimise the space needed to store the image.
1 If photographs are to be used to detect pathology, monitor progression, and protect against litigation it is essential that the resolution is sufficient to allow all clinical features of interest to be detected and that this is not compromised by the image storage. Improvements in digital technology have resulted in a sensitivity and specificity to detect retinal pathology comparable with analogue images and direct observation of patients by ophthalmologists, 2–5 although this has not been assessed for anterior eye images.
Resolution is the ability to distinguish between two adjacent points. In digital imagery, this depends on the number of pixels that comprise the image.
6 The Diabetic
Retinopathy Screening Committee concluded that fundus photography with 1000 6 1000 pixels is adequate to match the resolving power of the human eye, but adjusted the requirement to 1365 6 1000 pixels to allow for the rectangular shape of digital camera image sensors.
7
Image compression is a technique to reduce file size by removing redundant information. In some compression methods the full information can be retrieved (termed
‘‘lossless’’ formats such as TIFF (tagged image file format)), but in others the information is permanently deleted (‘‘lossy’’ formats such as JPEG (Joint Photographic Experts Group)).
8
If all images are taken at maximum quality, storage and archiving can become an issue. Handling large file sizes slows a storage database owing to the amount of processing needed, thereby reducing the advantage of the speed of digital technology. Basu and colleagues 9 suggested that up to a JPEG compression ratio of 1:20 (between 100–75% JPEG) was appropriate, based on objective analysis with lesion counts. Others have identified 75% JPEG as an appropriate limit from subjective analysis of digital images.
10 11
Subjective grading, even with the use of grading scales, has been found to have significant levels of interobserver variability.
12 Various image analysis methods have been demonstrated to make grading objective, improving repeatability. Edge detection (in which relative changes between neighbouring pixels are compared) and colour extraction (in which the object of interest colour is compared to the overall colour intensity) techniques have been shown to be more discriminatory between scale grades, repeatable, and robust to changes in image luminance.
13
Therefore, this study aimed to determine the most appropriate resolution and compression for anterior eye imaging, by evaluating calculated, subjective, and objective results of image compression and reductions in resolution.
METHODS
Four cameras were utilised: Nikon-CoolPix990 (2048 6 1360;
Tokyo, Japan), DVC-1312C model (1280 6 811; Austin, TX,
USA), and JAI-CV-S3200 (767 6 569; Copenhagen, Denmark) single square chip cameras covered the range of maximum pixel resolutions (noted in parentheses) available at the time of the study. The JVC-KYF58 (767 6 569; Yokohama, Japan) camera had the same resolution as the JAI-CV:S3200, but consists of three chips of this resolution, with light split by prisms to each of the red, green, and blue filtered chips. The cameras were attached to the same Takagi slit lamp (Nagano-
Ken, Japan) in turn for images of the anterior eye to be captured.
Images of the bulbar conjunctiva, palpebral conjunctiva, and central corneal staining were taken with each camera and stored as TIFF files (non-compressed format). Copies of the images in TIFF format with reduced resolutions (by bicubic resampling) and compression were created using
Adobe Photoshop v5.0 (San Jose, CA, USA).
Twenty optometrists reordered the randomised images in order of quality compared to the original maximum resolution TIFF image. The images were displayed on a 15 inch
(LGV-77T5) cathode ray tube monitor with a resolution of
Abbreviations: BMP, bit mapped graphics format; JPEG, Joint
Photographic Experts Group; SVGA, super video graphics array; TIFF, tagged image file format www.bjophthalmol.com
Anterior eye imaging 829
Rated worse
100
90
80
70
Nikon
DVC
JAI
JVC
60
50
40
30
20
Rated better
10
0
1600 ×
1063
1280 ×
811
1024 ×
680
767 ×
569
640 ×
425
Resolution (pixels)
320 ×
213
160 ×
107
Figure 1 Mean subjective ranking for each camera model’s resolution range. Error bars = 1 SD (n = 20).
1280 6 1024 pixels. The images were also objectively analysed by purpose designed edge detection and colour extraction computer software.
13
RESULTS
Theoretical calculation
Microcysts are about the smallest objects of clinical relevance on the anterior eye, being 15–50 m m.
14–16 As the light from an object could fall across the diameter of two pixels, a pixel size equivalent to 15 m m is necessary for reliable image capture of objects > 30 m m. The magnification (and hence the field of view) of a slit lamp can be varied. The typical slit lamp imaging system requires 597 horizontal pixels at 25 6 magnification or 2367 pixels at 6.3
6 magnification.
Clinical subjective ranking
There was no significant difference in resolution ranking between each camera model (Friedman non-parametric test, p .
0.05). The ranked order of resolution images was random and the mean ranks did not differ from each other until the number of pixels had dropped to ( 640 6 425 for each camera
(Wilcoxon signed rank comparison test, p , 0.005; fig 1).
Interestingly, the relative rank of the highest resolution image, 1600 6 1063 pixels from the Coolpix990 camera, was ranked as significantly worse than the 1280 6 1024 image
(p , 0.001).
There was no significant difference in compression ranking between each camera model (p .
0.05). The ranked order of compression images was random and the mean ranks did not differ from each other until the compression was ( 25%
JPEG compression (compression ratio 1:109; p , 0.005; fig 2).
The BMP (bit mapped graphics) format is generally considered to be a comparatively lossless method of compression, yet BMP images were consistently (p , 0.005) ranked as a lower quality image, comparable to , 25% (1:109 ratio) JPEG compression.
Clinical objective grading
As objective grading results in a continuous scale the results were analysed by analysis of variance.
17 Changes in resolution showed a statistically significant difference with edge detection (F = 2.77, p , 0.05) when reduced to ( 320 6 213 pixels, but not with colour extraction (F = 0.01, p = 1.00; fig 3). Compression of images did not significantly affect edge detection (F = 0.26, p = 0.93) or colour extraction (F = 0.50, p = 0.99) image analysis. However, figure 4 indicates that the colour extraction technique to be relatively more affected by changes in compression then resolution.
The camera type significantly affected the image analysis results. Edge detection showed a significant difference between images taken with the Nikon-Coolpix and the other three cameras for both resolution (F = 8.14, p , 0.001) and compression (F = 11.06, p , 0.001). Colour extraction showed a difference between images taken with the Nikon-Coolpix and DVC-1312C for both resolution (F = 4.01, p , 0.01) and compression (F = 5.10, p , 0.01). In comparison with the commonly used Efron pictorial grading scale, the difference between camera types was 0.2 (SD 0.4) units for edge detection and 0.1 (SD 0.4) Efron scale units for edge detection 17 .
DISCUSSION
The theoretical resolution required to observe the smallest anterior eye pathological features varies with the magnification level of the slit lamp observation system. At a typical medium level of magnification (25 6 ), 567 pixels across the horizontal field of view is required to detect an object 30 m m in diameter. Subjective grading identified that an image could be reduced to 767 6 569 pixel resolution (an 88% reduction in file size compared to a 2048 6 1360 pixel image) with no perceivable loss in image quality and this was independent of the camera used to take the images. The necessary integration of pixels to display images of higher resolution than the 1280 6 1024 pixel monitor led to a perceived reduction in image quality. Objective grading was less susceptible to resolution degradation, such that images
Rated worse
100
90
80
70
60
50
40
30
20
Rated better
10
0
JPG
100%
Nikon
DVC
JAI
JVC
JPG
75%
JPG
50%
JPG
25%
JPG
0%
Compression (format)
Figure 2 Mean subjective ranking for each camera model’s compression range. Error bars = 1 SD (n = 20).
BMP
15
10
5
0
Nikon
DVC
JAI
JVC
0.01
0.00
–0.01
–0.02
1600 ×
1063
1280 ×
811
1024 ×
680
767 ×
569
640 ×
425
Resolution (pixels)
320 ×
213
160 ×
107
Figure 3 Mean objective edge detection and colouration grading for each camera model’s resolution range. Error bars = 1 SD.
www.bjophthalmol.com
830 Peterson, Wolffsohn
0.01
0.00
–0.01
–0.02
15
10
5
0
JPEG
100%
Nikon
DVC
JAI
JVC
JPEG
75%
JPEG
50%
JPEG
25%
JPEG
0%
Compression (format)
BMP
Figure 4 Mean objective edge detection and colouration grading for each camera model’s compression range. Error bars = 1 SD.
could be reduced up to 640 6 425 pixel resolution with no significant change in edge detection grading and even a reduction to 160 6 107 pixels had no effect on colour extraction. The lowest appropriate level of resolution identified theoretically, by subjective ranking and objective image analysis grading, was lower than the level recommended for digital retinal imaging.
7 The recommended government resolution is greater than SVGA (super video graphics array ) resolution monitor resolution and therefore if viewed on a standard monitor, the images will potentially be reduced in image quality compared to an image captured at a lower resolution.
Up to a 1:70 (50%) JPEG compression could be applied to an image (regardless of the camera with which the image was taken on or its pixel resolution) without any apparent loss in subjective image quality. JPEG compression is designed to remove spatial frequencies not utilised by the human eye (by using discrete cosine transforms) and therefore the ability to compress an image by 98.6%
(compared to a 2048 6 1360 TIFF) without a loss in subjective image quality confirms this strategy is successful. The compression is slightly greater than that suggested as appropriate for retinal images.
10 11 BMP compression is essentially lossless so it is not clear why BMP compressed images were subjectively rated as of lower image quality than the same resolution TIFF. Objective grading of photographs with image analysis (both edge detection and colour extraction) was unaffected even by 0% JPEG compression.
It would therefore appear that the frequencies removed by compression do not affect the image parameters examined.
Once an image was captured, there was no difference in degradation caused by resolution or compression between resolution matched (767 6 569 pixels) three chip and one chip cameras. However, there were differences between cameras, with the highest resolution camera examined affected by resolution and compression less when analysed by edge detection and more when analysed by colouration compared to the other cameras.
In conclusion, image sizes as small as 767 6 569 pixels together with 1:70 JPEG compression appear to result in no loss in subjective or objective image quality. A higher pixel resolution image results in a larger file size and potential loss of image quality if viewed on a standard monitor. Use of compression has a greater effect on decreasing image size than reducing resolution before subjective or objective loss of image quality occurs.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
R C Peterson, J S Wolffsohn, School of Life and Health Sciences, Aston
University, Aston Triangle, Birmingham B4 7ET, UK
Correspondence to: James S Wolffsohn, School of Life and Health
Sciences, Aston University, Aston Triangle, Birmingham B4 7ET, UK; j.s.w.wolffsohn@aston.ac.uk
Accepted for publication 3 December 2004
REFERENCES
1 Charman WN . Imaging in the 21st century.
Ophthal Physiol Opt
1998; 18 :210–23.
2 George LD , Leverton C, Young S, et al.
Can digitised colour 35 mm transparencies be used to diagnose diabetic retinopathy ?
Diabet Med
1997; 14 :970–3.
3 Lim JI , Labree L, Nichols T, et al.
Comparison of nonmydriatic digitized video fundus images with standard 35-mm slides to screen for and identify specific lesions of age-related macular degeneration.
Retina 2002; 22 :59–64.
4 Prasad S , Bannon P, Clearkin LG, et al.
Digital fundus imaging: a quality and cost comparison with 35-mm film.
Acta Ophthalmol Scand 1999; 77 :79–82.
5 Olson JA , Strachan FM, Hipwell JH, et al.
A comparative evaluation of digital imaging, retinal photography and optometrist examination in screening for diabetic retinopathy.
Diabet Med 2003; 20 :528–34.
6 Jensen P , Scherfig E. Resolution of retinal digital colour images.
Acta
Ophthalmol Scand 1999; 5 :526–9.
7 British Diabetic Association .
Guidelines on screening for diabetic retinopathy .
London: BDA, 1999.
8 Garcia JA , Fdez-Valdivia J, Fdez-Vidal XR, et al.
On the concept of best achievable compression ratio for lossy image coding.
Pattern Recognition
2003; 36 :2377–94.
9 Basu A , Kamal AD, Illahi W, et al.
Is digital image compression acceptable within diabetic retinopathy screening ?
Diabet Med 2003; 20 :766–71.
10 Newsom RS , Clover A, Costen MT, et al.
Effect of digital image compression on screening for diabetic retinopathy.
Br J Ophthalmol 2001; 85 :799–802.
11 Kocsis O , Costaridou L, Mandellos G, et al.
Compression assessment based on medical image quality concepts using computer-generated test images.
Comput Methods Programs Biomed 2003; 71 :105–15.
12 Fieguth P , Simpson T. Automated measurement of bulbar redness.
Invest
Ophthalmol Vis Sci 2002; 43 :340–7.
13 Wolffsohn JS , Purslow C. Clinical monitoring of ocular physiology using digital image analysis.
Contact Lens Ant Eye 2003; 26 :27–35.
14 Zantos SG . Cystic formations in the corneal epithelium during extended wear of contact lenses.
Int Contact Lens Clin 1983; 10 :128–68.
15 Keay L , Jalbert I, Sweeney DF, et al.
Microcysts: clinical significance and differential diagnosis.
Optometry 2001; 72 :452–60.
16 Tabery HM . Corneal surface changes in keratoconjunctivitis sicca. Part I: The surface proper. A non-contact photomicrographic in vivo study in the human cornea.
Eye 2003; 17 :482–7.
17 Wolffsohn JS . Incremental nature of anterior eye grading scales determined by objective image analysis.
Br J Ophthalmol 2004; 88 :1434–8.
www.bjophthalmol.com
831
SCIENTIFIC REPORT
The telomere of human chromosome 1p contains at least two independent autosomal dominant congenital cataract genes
J D McKay, B Patterson, J E Craig, I M Russell-Eggitt, M G Wirth, K P Burdon, A W Hewitt,
A C Cohn, Y Kerdraon, D A Mackey
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :831–834. doi: 10.1136/bjo.2004.058495
Aims: Multiple genetic causes of congenital cataract have been identified, both as a component of syndromes and in families that present with isolated congenital cataract.
Linkage analysis was used to map the genetic locus in a six generation Australian family presenting with total congenital cataract.
Methods: Microsatellite markers located across all known autosomal dominant congenital cataract loci were genotyped in all recruited family members of the Tasmanian family. Both two point and multipoint linkage analysis were used to assess each locus under an autosomal dominant model.
Results: Significant linkage was detected at the telomere of the p arm of chromosome 1, with a maximum two point LOD of 4.21 at marker D1S507, a maximum multipoint exact LOD of 5.44, and an estimated location score of 5.61 at marker
D1S507. Haplotype analysis places the gene inside a critical region between D1S228 and D1S199, a distance of approximately 6 megabases. The candidate gene PAX7 residing within the critical interval was excluded by direct sequencing in affected individuals.
Conclusion: This is the third report of congenital cataract linkage to 1ptel. The critical region as defined by the shared haplotype in this family is clearly centromeric from the
Volkmann cataract locus identified through study of a Danish family, indicating that two genes causing autosomal dominant congenital cataract map to the telomeric region of chromosome 1p.
A utosomal dominant congenital cataract (ADCC) is one of the most common causes of childhood blindness.
The disorder is clinically heterogeneous, with the presentation of cataract varying considerably between families and even between individuals carrying identical mutations.
1 Genetically, ADCC is also highly heterogeneous, but within a given family congenital cataract tends to be monogenic with high penetrance. Autosomal dominant inheritance is the most common form, although recessive forms have been described.
2 Mutations causing cataracts have been identified in genes from diverse classes including membrane proteins, cytoskeletal proteins, and transcription factors.
3–6 Causative genes remain to be identified at further mapped loci indicating that further genetic heterogeneity exists.
7–12
Here, we use linkage analysis to map the ADCC gene segregating in a large family from the Australian island state of Tasmania. Using linkage and haplotype based approaches we have shown that this locus is independent of the described Volkmann-type congenital cataract locus previously mapped to this region.
METHODS
We identified a six generation family originating from the
Australian island state of Tasmania with ADCC.
13 This is one of several families previously screened for mutations in crystallin genes.
14 Family members were recruited with written informed consent obtained from all participating individuals or their guardians. DNA was available from 16 members of the four most recent generations and was extracted from whole blood or buccal mucosal swabs using the PureGene DNA Isolation Kit (Gentra Systems). Ethics approval for this study was obtained from the human research ethics committees of the Royal Children’s Hospital,
Melbourne, the Royal Victorian Eye and Ear Hospital,
Melbourne, and the University of Tasmania, Hobart, and we adhered to the tenets of the Declaration of Helsinki.
Genotyping
Forward primers for each marker were labelled with fluorescent dyes to allow detection of polymerase chain reaction (PCR) fragments on an ABI PRISM 310 genetic analyser (Applied Biosystems). Primer sequences and PCR conditions are available from the Genome Database
(www.gdb.org). Microsatellites were genotyped by the
Australian Genome Research facility in or near all known
ADCC loci, including: D1S468-D1S2660 (1ptel) and D1S252-
D1S498 (1q21), D2S2358-D2S325 ( CRYG ), D3S1569-
D3S1593 ( BFSP2 ), D10S192-D10S597 ( PITX3 ), D11S898-
D11S4090 ( CRYAB ), D12S83-D12S313 ( MIP ), D13S1236-
D13S175 ( Cx46 ), D15S117-D15S1033 (15q21-q22),
D16S3066-D16S515 ( HSF4 ), D17S1857-D17S1824 ( CRYBA1 ),
D17S1847-D17S836 (17q24), D17S849-D17S831 (17p13),
D20S115-D20S871 (20p12-q12), D21S1255-D21S266
( CRYAA ), D22S315-D22S1154 ( CRYB ). Additional microsatellites located on the 1p telomere were genotyped: D1S214,
D1S450, D1S244, D1S2667, D1S489, D1S228, D1S507,
D1S2728, D1S436, D1S2644, D1S199.
Linkage analysis
The analysis model assumed a high genetic risk, autosomal dominant model. The disease gene frequency was assumed to be rare at 0.001 and genotype penetrances of aa 0.001 Aa 0.95
AA 0.95. Two point LOD scores were calculated using MLINK.
Multipoint LOD scores were calculated using approximate location scores using the SimWalk2 program 15 and exact LOD scores using the Vitesse program.
16 Analysis using Vitesse was limited to three markers (D1S507-D1S2728-D1S2644)
Abbreviations: ADCC, autosomal dominant congenital cataract; PCR, polymerase chain reaction; SNP, single nucleotide polymorphism www.bjophthalmol.com
832 McKay, Patterson, Craig, et al
Figure 1 Haplotype of the congenital cataract family from the Australian island state of Tasmania. Recombinants
16.10 and 16.14 define a critical region centromeric from D1S199 and telomeric from D1S228.
16-07
2
1
3
1
1
4
1
1
1
1
1
3
3
5
5
7
3
4
4
4
16-01
1
2
1
1
3
1
4
1
1
1
2
6
1
3
1
1
2
3
6
2
16-02
1
2
1
1
3
1
4
1
1
1
2
6
1
3
1
1
2
3
6
2
16-12
1
2
1
3
1
4
1
1
1
1
16-10
1
1
1
2
1
5
1
3
1
4
1
1
1
8
4
6
2
3
1
1
16-11
1
1
1
2
1
5
1
3
1
4
1
1
1
8
4
6
2
3
1
1
16-13
3
2
4
6
4
1
4
1
1
5
1
2
2
1
4
2
5
1
2
4
4
6
4
1
1
5
4
1
3
2
16-04
4
9
6
2
1
2
4
1
2
4
3
3
7
1
3
2
2
4
1
2
16-03
1
2
2
1
1
1
1
1
1
1
2
1
6
1
1
3
7
3
2
1
16-05
1
1
1
2
1
1
2
1
1
1
1
2
3
3
2
4
7
1
3
2
16-06
1
2
2
1
1
1
-
1
1
1
2
1
6
1
1
3
3
-
2
1
16-15
1
2
1
3
1
4
1
1
1
1
1
6
3
3
3
2
8
7
2
1
16-17
4
5
3
1
3
5
4
1
4
2
6
4
2
1
4
5
5
3
1
2
Order
D1S450
D1S244
D1S2667
D1S489
D1S228
D1S507
D1S2728
D1S436
D1S2644
D1S199
Physical position at 1 p (Mb)
9.4
10.2
11.2
11.7
13.3
14.3
14.5
15.2
18.4
19.4
16-16
1
1
1
2
1
1
1
3
1
4
1
2
6
4
5
3
2
1
4
5
16-08
1
2
1
1
3
1
4
1
1
1
2
7
1
8
1
2
5
1
1
6
Affected
Mildly affected
16-14
5
2
1
2
-
1
4
-
2
4
2
1
1
6
-
4
2
-
1
1 because of the size of the kindred. The genetic positions of the markers were taken from the Decode 17 and Marshfield 18 genetic maps and the marker order confirmed using their physical position in the human genome (genome.ucsc.edu/ cgi-bin/hgGateway). Allele frequencies were taken from the genome database. Individuals 16.10 and 16.11 are monozygotic twins and hence only patient 16.10 was included in the linkage analysis.
Re-sequencing of PAX7 in affected patients
The coding region of the candidate gene PAX7 was resequenced in two affected patients as well as one unaffected individual. Primers were designed to amplify each of the eight identified exons (primers available on request) from genomic DNA. Amplified products were purified using spin columns (MoBio) and sequencing was performed on an
ABI PRISM 310 genetic analyser (Applied Biosystems).
RESULTS
Clinical notes from two patients in the Tasmanian pedigree describe the phenotype as a complete cataract (16.05 and
16.14) although most affected members are elderly and aphakic, with no preoperative clinical notes available. The median age of diagnosis was less than 1 year (range birth to
9 years), however most were diagnosed shortly after birth and the mean age of cataract surgery was 3 years 4 months
(range 0–9 years). Twelve of the 13 patients had bilateral cataract surgery and were aphakic (eight had acuities , 6/60 and four had acuities 6/19–6/60), corrected with spectacles.
There is one affected member (16.16, fig 1) who is an obligate carrier but has a relatively mild phenotype, phakic with good vision (6/6–1 6/7.5
+ 2) but not available for slit lamp examination. Eleven of 12 of the aphakic individuals had nystagmus. Two individuals had exotropia (16.02, 16.08) and four esotropia (16.03, 16.06, 16.07, 16.11). Four individuals had bilateral aphakic glaucoma (16.03, 16.05,
16.08, 16.15). No other ocular or systemic abnormalities were noted.
Linkage analysis using the microsatellite markers genotyped across the known cataract loci detected significant linkage at the telomere of chromosome 1p. Two point LOD scores of greater than three were achieved at markers D1S507 and D1S2644, with LODs of 4.21 and 3.23 ( h = 0) respectively
(table 1). Multipoint analysis achieved maximum location scores 15 and LOD scores 16 of 5.61 and 5.44 respectively
(table 1). Combined, these results indicate significant linkage to this region making it highly probable that the gene segregating in this family maps to this locus. All other regions tested failed to reach significance or were inconsistent with linkage (data not shown).
www.bjophthalmol.com
Autosomal dominant congenital cataract genes
Table 1 Summary of linkage analysis results across 1p36
MLINK
0
LOD score
0.1
0.2
0.3
0.4
h value
D1S2660
D1S214
D1S450
D1S244
D1S2667
D1S489
D1S228
D1S507
D1S2728
D1S436
D1S2644
D1S199
2 0.19
2 4.68
1.09
2 0.11
2 2.23
2 3.67
2 0.54
4.21
1.47
1.15
3.24
2 0.17
1.14
2 1.64
0.86
1.11
1
2 0.48
0.78
3.34
1.06
0.79
2.51
1.15
0.85
2 0.78
0.59
0.82
0.91
2 0.22
0.52
2.43
0.69
0.48
1.77
0.86
0.5
2 0.36
0.34
0.47
0.61
2 0.13
0.24
1.51
0.39
0.25
1.07
0.52
0.2
2 0.13
0.15
0.19
0.29
2 0.07
0.06
0.68
0.16
0.09
0.47
0.22
SimWalk
Location score
0.021
2 2.84
2 2.02
2 2
2 1.79
2 1.69
2.58
5.62
5.62
5.55
5.32
2.63
Vitesse
LOD score
5.44
5.44
5.27
833
The inferred haplotypes across 1pter are displayed in figure 1. Two informative recombinants, 16.10 and 16.14, define a critical region between centromeric marker D1S199 and telomeric marker D1S228. The physical location of these markers indicated that the region containing the gene spans a physical distance of approximately 6 megabases (Mb).
Eiberg et al 7 studied a large Danish pedigree affected with
Volkmann-type congenital cataract to map the gene for this disorder to the interval between the 1p telomere and D1S214.
In the Tasmanian family the recombinants 16.14 and descendants of 16.20 all indicate that the gene segregating in this family is located at a position 6 Mb telomeric to
D1S214 (fig 2). As there is 6 Mb between the two critical regions defined by these studies, it is likely that the genes in the Tasmanian and Danish pedigrees are not allelic and provides strong evidence that there are at least two genes predisposing to ADCC on the telomeric region of chromosome
1p.
The PAX transcription factors have been implicated in ocular development and congenital cataract.
19 The presence of
D1S243 (2)
D1S214 (3.4)
Danish
Volkmann
Eiberg et al
Bristish posterior
7 polar
Ionides et al
8
This study
GLC3B congenital glaucoma
Akarsu et al
20
D1S2667 (11.2)
D1S228 (13.0)
D1S1176 (14.5)
D1S199 (19.0)
Figure 2 Physical position in megabases (Mb) of the genetic markers across 1ptel. Shaded boxes represent the critical regions from each congenital eye disease study.
the PAX7 gene inside the critical region defined by our study made it an excellent candidate gene. However, re-sequencing of the coding region of this gene in two of the affected patients from the Tasmanian family did not identify any mutations, apart from a common synonymous single nucleotide polymorphism (SNP) that has already been identified as a part of the human genome project
(rs2743201) and therefore was very unlikely to have any influence on disease. While we cannot exclude that a mutation in a regulatory region of this gene may have a role, the absence of a coding region mutation suggests that the disease allele may lie in another gene within the critical region.
DISCUSSION
The linkage analysis results from the Tasmanian family clearly indicate the existence of a susceptibility gene at 1p36.
This is the third report of significant linkage in congenital cataract to the telomere of 1p. Eiberg et al 7 studied a large
Danish pedigree affected with Volkmann-type cataract and mapped the predisposition gene for this disorder to the interval between the 1p telomere and D1S214. This region is
6 Mb telomeric to the region defined by the recombinant individuals in the Tasmanian family. Both the Danish and our own results have reached highly significant linkage
(Danish pedigree LOD = 14.04 Tasmanian pedigree LOD =
5.44) and with the physical positions better determined via the human genome project, we can determine that there is no ambiguity in the marker’s position used by either study.
The lack of overlap between the segregating haplotypes from the two studies makes it likely that the genes in the
Tasmanian and Danish pedigrees are not allelic and there are two genes predisposing to congenital cataract on the telomere of 1p.
The second report of linkage to this region was in a British family presenting with ADCC.
8 Based on the haplotype in this
British family, and particularly a homozygous stretch in a critical recombinant, the authors suggest that the gene segregating in this family might be allelic to the Danish
Volkmann cataract pedigree. However, in reviewing the haplotype segregating in the British family in light of the region outlined here, we believe it also possible, if not more likely, that the gene in the British family could be allelic to the Tasmanian pedigree.
Interestingly, the critical region defined by the Tasmanian family also overlaps with that of the recessive primary congenital glaucoma locus, GLC3B .
20 Four of 13 patients from the Tasmanian family had aphakic glaucoma. This is relatively high for congenital cataracts, suggesting possible involvement of the same gene with both congenital glaucoma www.bjophthalmol.com
834 McKay, Patterson, Craig, et al and cataract. However, the phenotypic differences between congenital cataract and congenital glaucoma, and genetic differences (a dominant versus recessive inheritance), make it equally likely that these disorders are not caused by the same gene. The mapping of the congenital cataract, congenital glaucoma and Volkmann-type cataract loci in this region indicates that the telomeric region of the p arm of chromosome 1 contains a number of genes that are relevant to both eye development as well as congenital eye disorders.
The physical distance defined as the critical region in the
Tasmanian family is about 6 Mb. Inside this interval are 30 named genes, of which 18 are clearly noted to be expressed in the eye (www.ncbi.nlm.nih.gov/unigene). Also in this region are many more undescribed mRNAs and algorithm predicted genes. This makes the positional cloning of the causative gene a formidable task at this point. The identification of additional families linked to this region and containing informative recombinants may further restrict this region so that a positional cloning attempt is realistic. Identification of this gene and others that cause congenital cataract increases our understanding of the molecular events that lead to the development of cataract as well as the development of the eye.
ACKNOWLEDGEMENTS
This project would not have been possible without the financial support provided by the Ophthalmic Research Institute of Australia, the Jack Brockhoff Foundation, and the Royal Hobart Hospital
Research Foundation and the National Health and Medical Research
Council.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
J D McKay, B Patterson, J E Craig, K P Burdon, A W Hewitt,
D A Mackey, Menzies Centre for Population Health Research, University of Tasmania, Hobart, Australia
J D McKay, Genome analysis team, International Agency for Research on Cancer, Lyons, France
J E Craig, A C Cohn, Y Kerdraon, D A Mackey, Centre for Eye Research
Australia, University of Melbourne, Royal Victorian Eye and Ear
Hospital, Melbourne, Australia
J E Craig, Department of Ophthalmology, Flinders University, Flinders
Drive, Bedford Park, South Australia
I M Russell-Eggitt, Great Ormond St Hospital for Children, London, UK
M G Wirth, Department of Ophthalmology, Royal Children’s Hospital,
Melbourne, Australia
K P Burdon, Department of Biochemistry, Wake Forest University School of Medicine, Winston-Salem, NC, USA
Competing interests: none declared
Correspondence to: Associate Professor David Mackey, The Royal
Victorian Eye and Ear Hospital, 32 Gisborne Street, East Melbourne, VIC
3002, Australia; d.mackey@utas.edu.au
REFERENCES
1 Litt M , Carrero-Valenzuela R, LaMorticella DM, et al . Autosomal dominant cerulean cataract is associated with a chain termination mutation in the human beta-crystallin gene CRYBB2.
Hum Mol Genet 1997; 6 :665–8.
2 Pras E , Levy-Nissenbaum E, Bakhan T, et al . A missense mutation in the LIM2 gene is associated with autosomal recessive presenile cataract in an inbred
Iraqi Jewish family.
Am J Hum Genet 2002; 70 :1363–7.
3 Berry V , Francis P, Kaushal S, et al . Missense mutations in MIP underlie autosomal dominant ‘polymorphic’ and lamellar cataracts linked to 12q.
Nat
Genet 2000; 25 :15–7.
4 Conley YP , Erturk D, Keverline A, et al . A juvenile-onset, progressive cataract locus on chromosome 3q21-q22 is associated with a missense mutation in the beaded filament structural protein-2.
Am J Hum Genet 2000; 66 :1426–31.
5 Semina EV , Ferrell RE, Mintz-Hittner HA, et al . A novel homeobox gene PITX3 is mutated in families with autosomal-dominant cataracts and ASMD.
Nat
Genet 1998; 19 :167–70.
6 Bu L , Jin Y, Shi Y, et al.
Mutant DNA-binding domain of HSF4 is associated with autosomal dominant lamellar and Marner cataract.
Nat Genet
2002; 31 :276–8.
7 Eiberg H , Lund AM, Warburg M, et al.
Assignment of congenital cataract
Volkmann type (CCV) to chromosome 1p36.
Hum Genet 1995; 96 :33–8.
8 Ionides AC , Berry V, Mackay DS, et al.
A locus for autosomal dominant posterior polar cataract on chromosome 1p.
Hum Mol Genet 1997; 6 :47–51.
9 Vanita , Singh JR, Sarhadi VK, et al.
A novel form of ‘‘central pouchlike’’ cataract, with sutural opacities, maps to chromosome 15q21-22.
Am J Hum
Genet 2001; 68 :509–14.
10 Berry V , Ionides AC, Moore AT, et al.
A locus for autosomal dominant anterior polar cataract on chromosome 17p.
Hum Mol Genet
1996; 5 :415–19.
11 Armitage MM , Kivlin JD, Ferrell RE. A progressive early onset cataract gene maps to human chromosome 17q24.
Nat Genet 1995; 9 :37–40.
12 Yamada K , Tomita H, Yoshiura K, et al.
An autosomal dominant posterior polar cataract locus maps to human chromosome 20p12–q12.
Eur J Hum
Genet 2000; 8 :535–9.
13 Wirth MG , Russell-Eggitt IM, Craig JE, et al.
Aetiology of congenital and paediatric cataract in an Australian population.
Br J Ophthalmol
2002; 86 :782–6.
14 Burdon KP , Wirth MG, Mackey DA, et al.
Investigation of crystallin genes in familial cataract, and report of two disease associated mutations.
Br J Ophthalmol 2004; 88 :79–83.
15 Sobel E , Lange K. Descent graphs in pedigree analysis: applications to haplotyping, location scores, and marker-sharing statistics.
Am J Hum Genet
1996; 58 :1323–37.
16 O’Connell JR , Weeks DE. The VITESSE algorithm for rapid exact multilocus linkage analysis via genotype set-recoding and fuzzy inheritance.
Nat Genet
1995; 11 :402–8.
17 Kong A , Gudbjartsson DF, Sainz J, et al.
A high-resolution recombination map of the human genome.
Nat Genet 2002; 31 :241–7.
18 Broman KW , Murray JC, Sheffield VC, et al.
Comprehensive human genetic maps: individual and sex-specific variation in recombination.
Am J Hum
Genet 1998; 63 :861–9.
19 Wolf MT , Lorenz B, Winterpacht A, et al.
Ten novel mutations found in aniridia.
Hum Mutat 1998; 12 :304–13.
20 Akarsu AN , Turacli ME, Aktan SG, et al.
A second locus (GLC3B) for primary congenital glaucoma (buphthalmos) maps to the 1p36 region.
Hum Mol
Genet 1996; 5 :1199–203.
www.bjophthalmol.com
835
EXTENDED REPORT
Knowledge and beliefs on corneal donation in Singapore adults
Y-W Yew, S-M Saw, J C-H Pan, H-M Shen, M Lwin, M-S Yew, W-J Heng
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :835–840. doi: 10.1136/bjo.2004.057372
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Seang-Mei Saw, MBBS,
MPH, PhD, Department of
Community, Occupational and Family Medicine,
National University of
Singapore, 16 Medical
Drive, Singapore 117597; cofsawsm@nus.edu.sg
Accepted for publication
29 November 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aim: To assess the knowledge and willingness of Singapore adults towards corneal donation.
Methods: The study population consists of a cluster random sample of the population living in Bedok North
(an area in the eastern part of Singapore). The study population comprised residents aged 21–65 years living in 675 randomly sampled housing units. The participation rate was 65.9% (544/825). All participants were interviewed face to face with a questionnaire formulated according to the modified
Horton and Horton model. Knowledge, values, attitudes, and spiritual beliefs of participants were assessed to evaluate their willingness to donate their corneas.
Results: 67.0% of participants were willing to donate their corneas. Ethnicity (Chinese) and religion
(Christians, Hindus, or those with no religion) were associated with increased willingness to donate corneas. Greater knowledge and increased altruistic values were also associated with increased willingness to donate corneas.
Conclusion: A proportion of participants were willing to donate their corneas. Awareness of corneal donation is high but specific knowledge should be further increased among adults.
C orneal transplant is a sight saving procedure and is the most common type of human transplant surgery.
Indications for cornea transplant include bullous keratopathy, regrafts, corneal dystrophies, and keratoconus.
Relatively few studies have described the characteristics and motivation of potential donors of corneas.
Two studies done in north western India
India, 2
1 and Hyderabad, specifically examine the attitudes towards corneal donation and awareness of corneal donation, respectively.
Both the north western India (n = 2000) and the Hyderabad
(n = 2954) study included individuals from a wide age range
( .
15 and 18–99 years) and all participants were Hindus,
Sikhs, or Muslims. Another study done in Toronto, Canada, 3 examined the public attitudes towards donation of body parts with particular emphasis on the eye. This Toronto (n = 595) study includes individuals who are above 16 years but it only examines the level of willingness towards donation of body parts and not just corneal donation. Therefore, there was a need to address the knowledge, attitudes, and beliefs regarding corneal donation in a multiracial Asian society like
Singapore. In this paper, we aimed to assess the willingness of Singapore adults to donate their corneas as well as to determine the factors influencing their willingness. We hoped to identify the demographics of Singapore adults who may be less inclined to donate their corneas.
MATERIALS AND METHODS
A community based cross sectional study was conducted in the eastern part of Singapore in Bedok North Estate. This study was part of a third year National University of
Singapore third year medical student research posting.
Study population
We included all residents who are Singapore citizens and permanent residents aged between 21–65 years old living in the sampled housing units at the time of our study. We excluded residents with physical or mental illnesses, which may impair their ability to communicate or respond logically.
Written informed consent was obtained after the nature of the study was explained to the participants. The study was approved by the Department of Community, Occupational and Family Medicine, Student Project Committee.
The sampling frame consists of a total of 8314 household units. One stage random cluster sampling was done, and 675 housing units were sampled. Non-participating household units and individuals consisted of those who refused to participate in the study or who were non-contactable. Failure to contact the household or individual after at least three revisits (at three different times of the day) will deem the household or individual as non-contactable. The household participation rate was (369/551 = 67.0%) and the individual participation rate was 65.9% (544/825).
Questionnaire based data
The questionnaire was developed with the aid of focus group discussions consisting of six participants aged 20–57 years old, encompassing all four races as well as the main religions in Singapore. Open ended questions were asked to generate ideas on possible views and opinions towards cornea donation and ideas gathered were used to develop the questionnaire. A pilot study in 67 adults was then conducted in order to assess the clarity and ease of comprehension of the questionnaire. Interviewer training was also conducted before the survey proper commenced.
We adapted Horton and Horton’s 4 basic model of people’s willingness to become potential donors in the development of our questionnaire. As proposed in the modified Horton and
Horton’s model, 5 knowledge, values and spiritual beliefs influence a person’s attitude towards cornea donation, and are mediating factors that lead to a person’s willingness to donate. Other questions asked about corneal donation include whether participants have heard about corneal donation and whether approval of close relatives and friends is important in one’s decision to donate corneas.
Other information in the questionnaire included demographic data (name, identification card number, age, sex, race, religion, marital status, educational status, housing type, monthly household income, and occupation).
Eligible individuals in the chosen housing units were interviewed face to face via a questionnaire. The average www.bjophthalmol.com
836 Yew, Saw, Pan, et al length of the interview was about 20 minutes. The questionnaire was translated into Chinese and Malay. A glossary was included and each interviewer was equipped with
Chinese and Malay translations of the questionnaire.
Data analysis
Data analysis was conducted using Statistical Package for
Social Sciences (SPSS) Version 12.0. Descriptive, univariate, and multivariate analyses were then performed.
The characteristics of those who were willing to donate corneas were compared to those who were not willing.
Proportions were compared using the x
2 test and means using the t test or medians using the Wilcoxon rank sum test, if parametric assumptions were not met. Statistical significance was determined at the 0.05 level.
RESULTS
Demographic profile of respondents
The age distribution of the participants was as follows: 201
(35.6%) were 21–35 years old, 221 (39.2%) were 36–50 years old, and 143 (25.2%) aged 51–65 years. There were 288
(51.1%) males and 278 (48.9%) females. There were 371
(65.8%) married, 164 (29.1%) single, 20 (3.5%) divorced or separated, and nine (1.6%) widowed participants. The ethnicity distribution of participants was as follows: 390
Chinese (69.1%), 143 Malays (25.4%), 25 Indians (4.4%), and six from other races (1.1%). The completed education level of the participants was as follows: 13.0% had no formal education, 21.1% primary school education (ages 6–
12 years), 41.5% secondary school education (ages 13–
16 years), and 34.3% had completed pre-university or tertiary education (ages 17 years and above).
Willingness to donate
In all, 364 (67%) out of a total of 544 indicated that they were willing to donate their corneas. A similar proportion of participants (68%) were willing to donate other organs.
Table 1 reflects the demographics of respondents who were willing to donate their corneas, according to age, sex, race, religion, and education level. Willingness to donate was not associated with age (p = 0.12) or sex (p = 0.81). Chinese people were the most willing to donate, with 75.3% of the
Chinese interviewed willing to donate. Malays were the least willing, with only 44.4% of Malay respondents willing to donate (p , 0.001). Atheists (84.4%, p , 0.001) were the most willing to donate their corneas; 75.6% of those who completed tertiary education were willing to donate compared to only 52.9% of those who have no formal education
(p = 0.012). In the final multiple logistic regression model
(table 2), race remained significantly associated with willingness to donate corneas after controlling for age, sex, and educational level. Similarly, religion remained significantly associated with willingness to donate corneas, after adjusting for age, sex, and educational level.
Educational level was no longer significantly associated with willingness to donate corneas, after controlling for age, sex, and religion.
Reasons for willingness to donate corneas
Among those who were willing to donate their corneas,
92.9% did so because they thought that donating a part of themselves after death made them feel they were doing good
(table 3). Other reasons cited for their willingness to donate included hearing good results from cornea transplants
(47.8%) or having read an article or heard a speaker talk about the topic (47.0%).
The most common reason cited by those who were unwilling to donate their corneas was that they preferred that their bodies remained intact after death (73.2%). Other reasons cited included that their families may be upset
(49.2%) or the fear that their bodies would not be treated with respect (49.2%) (table 4).
Knowledge
Awareness of corneal donation
in all, 80.7% of all respondents had heard of corneal donation. Chinese people (86.6%) were more aware of corneal donation than Malays (71.1%) and other races
(51.6%) (p , 0.001). Christians (88.7%) were the most aware
Table 1 Characteristics of adults willing to donate their corneas
Demographics
Total
Age (years)
21–30
31–40
41–50
51–60
.
60
Sex
Male
Female
Race
Chinese
Malay
Others
Religion
Buddhism/Taoism
Islam
Christianity
No religion
Hindus/others
Completed educational level
No formal education
Primary
Secondary
Pre-university, diploma, or tertiary
Willing to donate
No (%)
364 (67.0)
101 (71.1)
91 (70.0)
79 (59.8)
73 (68.9)
20 (58.8)
188 (67.4)
176 (66.4)
286 (75.3)
60 (44.4)
18 (62.1)
172 (70.5)
63 (42.6)
44 (83.0)
65 (84.4)
20 (90.9)
9 (52.9)
65 (55.1)
155 (69.5)
135 (72.6)
Unwilling to donate
No (%)
180 (33.0)
41 (28.9)
39 (30.0)
53 (40.2)
33 (31.1)
14 (41.2)
91 (32.6)
89 (33.6)
94 (24.7)
75 (55.6)
11 (37.9)
72 (29.5)
85 (57.4)
9 (17.0)
12 (15.6)
2 (9.1)
8 (47.1)
53 (44.9)
68 (30.5)
51 (27.4) p Value
0.21
0.81
, 0.001
, 0.001
0.006
www.bjophthalmol.com
Corneal donation in Singapore 837
Table 2 Characteristics of adults willing to donate their corneas
Multivariate adjusted odds ratio * 95% CI Demographics
Age (years)
21–30
31–40
41–50
51–60
.
60
Sex
Male
Female
Religion
Buddhism/Taoism
Islam
Christianity
No religion
Hindus/others
Completed educational level
No formal education
Primary
Secondary
Pre-university, diploma, or tertiary
1.00
0.69
0.45
0.84
0.52
1.00
0.90
1.00
0.26
2.00
2.24
3.88
1.00
1.00
2.02
1.41
(0.39 to 1.25)
(0.25 to 0.82)
(0.43 to 1.62)
(0.21 to 1.26)
(0.60 to 1.33)
(0.17 to 0.41)
(0.90 to 4.47)
(1.12 to 4.50)
(0.87 to 17.30)
(0.33 to 3.02)
(0.68 to 6.03)
(0.45 to 4.49)
* Adjusted for all other factors in the table.
p Value
0.22
0.009
0.60
0.15
0.59
, 0.001
0.090
0.023
0.076
1.00
0.21
0.56
of corneal donation, followed by the Buddhists or Taoists
(87.2%), those with no religion (84.6%), Muslims (67.9%), and Hindus/others (65.2%) (p , 0.001).
Responses to specific knowledge questions
There were a larger proportion of people who were willing to donate their corneas among those who answered the questions correctly. This was statistically significant for four out of the five knowledge questions. People who answered the questions correctly were more likely to donate their corneas than those who answered incorrectly (table 5)
Attitudes
A total of 96.6% of all participants thought that corneal donation could help someone to see again. Only 50.8% would be more willing to donate their corneas if their family members were to receive benefits. Our data show that a more positive attitude towards corneal donation led to increased willingness to donate.
Values
The relations between instrumental or terminal values and willingness to donate are described in tables 6 and 7.
Participants who were ‘‘broadminded’’ were more likely to donate corneas (70.5%) than participants who were not broadminded (52.6%) (p = 0.001). Other instrumental values that were statistically significant included ‘‘forgiving’’
(p = 0.022), ‘‘helpful’’ (p = 0.013), and ‘‘loving’’ (p = 0.022).
The terminal values ‘‘a world of peace’’ (p = 0.015), ‘‘family security’’ (p = 0.001), ‘‘happiness’’ (p = 0.020), ‘‘inner harmony’’ (p = 0.003), and ‘‘true friendship’’ (p = 0.001) were also associated with willingness to donate corneas. A person who thought that world peace was important would be more likely to donate corneas (68.1%) than someone who did not think that world peace was important (46.7%). Therefore, the more altruistic a person was, the greater his willingness to donate his corneas.
Religious and spiritual beliefs
A total of 54% of participants thought it was important to be a religious person. Chinese people were less likely to feel that it was important to be a religious person (59.4%) than the other ethnic groups (12.6% for the Malays, and 22.6% for
Indians and other races). People who did not think it was important to be a religious person were more likely to donate their corneas. Forty one per cent of participants believed that luck affects their everyday life. When asked if it was possible to communicate with the dead, only 15% agreed with the statement (table 8).
DISCUSSION
In all, 67.0% of participants were willing to donate their corneas. Willingness to donate was found to be associated with the following characteristics: Chinese, atheist, Hindus/ others, and Christians. The most common reason for donating corneas was willingness to do good. The modified
Horton and Horton model 5 is applicable to corneal donation in Singapore. Increased knowledge (awareness and specific
Table 3 Reasons affecting one’s willingness to donate corneas
Reason for willingness to donate corneas
Transplanting a part of you after death will make you feel that you are doing good
Heard good results from cornea transplant operations
Read an article or heard a speaker talk about cornea donations
Friend or relative benefited from a cornea transplant
Friend or relative donated cornea
Number who answered this question
364
Number who cited this reason
338
Proportion who cited this reason (%) Rank
92.9
1
364
364
363
362
174
171
67
39
47.8
47.0
18.5
10.8
2
3
4
5 www.bjophthalmol.com
838
Table 4 Reasons affecting one’s unwillingness to donate corneas
Reason for unwillingness to donate corneas
Think it is important that body remains intact after death
Family would be upset
Body would not be treated with proper respect
Not sure how cornea would be used
Do not like to think about death
Doctors would be anxious to declare patient dead before he/she actually is
Can still experience pain after death
Might not be able to have a funeral
Heard of poor results from cornea transplant operations
179
179
177
179
180
Number who answered this question
179
Number who cited this reason
Proportion who cited this reason (%) Rank
131 73.2
1
179
180
178
88
88
85
68
64
52
40
38
49.2
49.2
48.0
38.0
35.6
29.1
22.2
21.9
7
8
9
4
5
2
2
6
Yew, Saw, Pan, et al knowledge statements), increased altruism (instrumental and terminal values), and a positive attitude towards cornea donation led to an increased willingness to donate.
In our population, it was found that 67% of the residents were willing to donate their corneas compared with 52% in adults aged 18–99 in north western India (n = 2000) 1 and
44.9% in adults aged above 15 in Hyderabad, India
(n = 2954).
2 Therefore, the level of willingness towards corneal donation was found to be higher in Singapore than
India.
1 2 This may be due to greater awareness of corneal donation in Singapore (80.7%) compared with India (70.5%, 1
70.1% 2 ). Higher educational level and greater socioeconomic status in Singapore may also a possible factor. However, the studies may not be directly comparable. The age, ethnicity, and religion distributions of the individuals in the three studies are very different. The two studies in India included
Table 5 Relation between knowledge and attitudes regarding cornea donation and willingness to donate corneas
No
1
2
3
4
5
6
7
Knowledge statements
After a patient has been certified brain dead, there is still a possibility that he can recover and return back to normal daily functions
The donor’s family does not have to pay for the hospital and surgery costs for removing, preserving, and transporting the donor’s corneas
Organ donation generally does not result in any significant delay in normal funeral arrangements
A donor’s family can request compensation to offset the cost of the donor’s burial or cremation
Corneal donation after death leaves the body mutilated and disfigured
Cornea donation can help someone see again
More willing to donate corneas if family members were to receive benefits after that
Correct answer
False
True
True
False
False
–
–
Respondent answer
Correct
Incorrect
Correct
Incorrect
Correct
Incorrect
Correct
Incorrect
Correct
Incorrect
Agree
Disagree
Agree
Disagree
Willing to donate
No (%)
245 (67.7)
109 (67.8)
278 (71.8)
72 (56.7)
250 (73.1)
103 (58.5)
253 (71.9)
96 (60.4)
289 (75.1)
66 (46.8)
359 (69.2)
1 (5.6)
202 (74.0)
160 (60.6)
Unwilling to donate
No (%)
117 (32.3)
52 (32.3)
109 (28.2)
55 (43.3)
92 (26.9)
73 (41.5)
99 (28.1)
63 (39.6)
96 (24.9)
75 (53.2)
160 (30.8)
17 (94.4)
71 (26.0)
104 (39.4) p Value
0.10
0.001
0.001
0.010
, 0.001
, 0.001
0.001
The missing values for questions 1, 2, 3, 4, 6, and 7 are 2, 14, 10, 18, 7, and 7 respectively.
Table 6 Relation between instrumental values and willingness to donate corneas
Number
1
2
3
4
5
6
7
Instrumental values *
Broadminded
Cheerful
Courageous
Forgiving
Helpful
Honest
Loving
Importance
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
Willing to donate
No (%)
51 (52.6)
313 (70.5)
23 (56.1)
341 (67.8)
61 (60.4)
303 (68.6)
25 (52.1)
339 (68.3)
22 (50.0)
342 (68.4)
18 (52.9)
346 (67.8)
19 (50.0)
344 (68.1)
Unwilling to donate
No (%)
46 (47.4)
131 (29.5)
18 (43.9)
162 (32.2)
40 (39.6)
139 (31.4)
23 (47.9)
157 (31.7)
22 (50.0)
158 (31.6)
16 (47.1)
164 (32.2)
19 (50.0)
161 (31.9)
The missing values for questions 1, 3, and 7 are 3, 1, and 1 respectively.
* Instrumental values refer to the means of achieving the desired end states of existence.
7 p Value
0.001
0.13
0.12
0.22
0.013
0.074
0.022
www.bjophthalmol.com
Corneal donation in Singapore 839
Table 7 Relation between terminal values and willingness to donate corneas
Number
1
2
3
4
5
6
7
8
9
Terminal values
A world of peace
Equality
Family security
Freedom
Happiness
Inner harmony
Self respect
True friendship
Wisdom
Importance
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
Willing to donate
No (%)
14 (46.7)
350 (68.1)
28 (60.9)
335 (67.4)
4 (26.7)
360 (68.1)
26 (55.3)
338 (68.1)
7 (41.2)
357 (68.0)
16 (44.4)
346 (68.4)
23 (59.0)
341 (67.8)
19 (44.2)
344 (68.8)
34 (57.6)
330 (68.0)
The missing values for questions 2, 4, 5, 6, 7, and 8 are 1, 1, 2, 2, 2, and 1 respectively.
* Terminal values refer to the desired end states of existence that are worth attaining.
7
Unwilling to donate
No (%)
16 (53.3)
164 (31.9)
18 (39.1)
162 (32.6)
11 (73.3)
169 (31.9)
21 (44.7)
158 (31.9)
10 (58.8)
168 (32.0)
20 (55.6)
160 (31.6)
16 (41.0)
162 (32.2)
24 (55.8)
156 (31.2)
25 (42.4)
155 (32.0) p Value
0.015
0.37
0.001
0.074
0.020
0.003
0.26
0.001
0.11
individuals from a wider age range and the majority of their participants were Hindus. In contrast, majority of the participants in our study were Buddhists or Taoist (44.9%) and only 3.0% are Hindus. The study populations from the two countries are different in both their cultural and socioeconomical background.
In all, 92.9% of participants who were willing to donate cited doing good as the reason. This was in contrast with the study done in Toronto 3 where the main reasons were personal experiences with cornea donation and transplants, and good results from corneal transplant operations. This could be due to the effective use of a well established eye bank in Toronto.
More corneal transplant operations were carried out annually in Toronto than Singapore (1200 transplants are done in
Toronto annually compared to 994 done so far in Singapore from 1996 to 2001). In north western India, 1 the main reason for willingness to donate was the possibility of living on after death if they donated their corneas. This may reflect their belief of life after death.
On the other hand, the main reason for unwillingness to donate in our study was the belief that it was important to have an intact body after passing away.
8 9 This could be for religious or cultural reasons. The main reason for unwillingness in Toronto 3 and Hyderabad north western India 1
2 was religion, while that in was the concern with hurting their family members. In our study, it was found that one’s parents and spouse have a strong influence on one’s decision in becoming a potential corneal donor. This may be reflective of the prevalent societal family values in Singapore.
The modified Horton and Horton model 5 was found to be applicable to corneal donation in Singapore. It postulates that increased knowledge, increased altruism, weaker spiritual beliefs, and a positive attitude towards corneal donation are positive predictors for willingness to donate. We found that an increase in knowledge leads to a greater willingness to donate. Knowledge consists of awareness and factual knowledge; 80.7% of our participants had heard of cornea donation, compared with 98% in Toronto
Rico 6 and India.
1 2
3 and 61.0% to 70.5% in Puerto
The difference could be due to the higher literacy rate and better health promotion programmes in
Toronto and insufficient resources for health promotion in
India and Puerto Rico.
In Singapore, the lack of available corneas precludes availability of corneas for emergency corneal transplants.
Bullous keratopathy is one of the most common indications for cornea transplant in Singapore. Statistics show that in the year 2003, about 60 transplanted corneas were acquired from local donors but the bulk of the transplanted corneas (108) were foreign, coming mainly from the United States and Sri
Lanka. These figures reflect Singapore’s lack of self sufficiency in the provision of transplantable corneas for patients.
This study is a population based study in a multiracial
Asian society. Face to face interviews were conducted with the questionnaire formulated based on the modified Horton and Horton model, 5 a focus group discussion, and a pilot study. However, there are limitations to this study that need to be considered when interpreting the results. Our study population may not be entirely representative of the entire
Singapore population. Age and sex distributions are fairly similar to the Singapore population (Singapore Census,
2000). However, there were larger proportions of Malays and Muslims in our study. Our participants were also better
Table 8 Relation between religious beliefs and willingness to donate corneas
Belief
It is important to be a religious person
You have religious beliefs that provide meaning and purpose to life
Disagree
Neutral
Agree
Disagree
Neutral
Agree
Willing to donate cornea
No (%)
81 (82.7)
108 (72.0)
174 (59.0)
62 (75.6)
81 (65.9)
220 (65.3)
Unwilling to donate cornea
No (%)
17 (17.3)
42 (28.0)
121 (41.0)
20 (24.4)
42 (34.1)
117 (34.7) p Value
, 0.001
0.20
www.bjophthalmol.com
840 Yew, Saw, Pan, et al educated. Hence, our prevalence rate may be different from the true prevalence rate of Singapore. Results may also be skewed because of non-participation bias. Those who participated in our study may have a higher level of awareness about corneal donation or greater altruistic values.
However, our participation rate is 65.9%, which is fairly high.
Characteristics such as age and sex are also very similar among the participants and non-participants. Non-participation is also minimised with measures such as distributing cover letters and re-visiting households at least three other times on different days.
Public education programmes via primary care physician, mass media, health campaigns in community and schools, and religious talks may be implemented to increase awareness and knowledge of corneal donation. Misconceptions about corneal donation issues such as brain death and organ use may also be clarified.
CONCLUSION
Our study showed that 67.0% were willing to donate their corneas. Respondents who are the least willing to donate their corneas are the Malays and Muslims. The main reason for unwillingness to donate corneas is the importance that the body remains intact after death (73.2%). Our study also showed that Singapore adults’ awareness of corneal donation was high; 80.5% of participants had heard of cornea donation.
ACKNOWLEDGEMENTS
We wish to acknowledge the National University of Singapore
Community Health Project Group 4 2004 third year medical students who conducted this survey: Alagappan U, Ang KX, Ang Y, Chan KW,
Chan LH, Cheok LZ, Chuah SY, Chutatape A, Kee SC, Koh XL, Lim
SL, Lim YJ, Lim ZL, Lin HA, Liu SL, Loh KY, Mathews I, Ng LC, Ng
KP, Ong AH, Ong KL, Ong YM, Pang SY, Parekh PV, Phua BK, Phua
M, Sahaya N, Tan HT, Tee HW, Wang TJ, Wong HK, Wong ST, Wong
ZW, Xu HY, Yang LQ, Yang PL, Yeo YW.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
Y-W Yew, S-M Saw, H-M Shen, M-S Yew, Department of Community,
Occupational and Family Medicine, National University of Singapore,
16 Medical Drive, Singapore 117597
J C-H Pan, W-J Heng, Department of Ophthalmology, Tan Tock Seng
Hospital, 11 Jalan Tan Tock Seng, Singapore 308433
M Lwin, NUS Business School, Department of Marketing, 1 Business
Link, Singapore 117592
REFERENCES
1 Duggal M , Brar GS, Prasad VS, et al.
Public attitude toward eye donation in
NW India.
Transplant Proc 2003; 35 :19–20.
2 Dandona R , Dandona L, Naduvilath TJ, et al.
Awareness of eye donation in an urban population in India.
Aust N Z J Ophthalmol 1999; 27 :166–9.
3 Basu PK , Hazariwala KM, Chipman ML. Public attitudes towards donation of body parts, particularly the eye.
Canadian Ophthalmol 1989; 24 :216–20.
4 Horton RL , Horton PJ. A model of willingness to become a potential organ donor.
Soc Sci Med 1991; 33 :1037–51.
5 Lwin MO , Williams JD, Lan LL. Social marketing initiatives: National Kidney
Foundation’s organ donation programs in Singapore.
J Public Policy
Marketing 2002; 21 :66–77.
6 Dominguez JM , Gonzalez ZA, Morales Otero LA, et al.
Knowledge and attitude about organ donation in a Hispanic population . Transplant Proc
1991; 23 :1804–6.
7 Bilgel H , Bilgel N, Okan N, et al.
Public attitudes toward organ donation.
Transplant Int 1991; 4 :243–5.
8 Rasheed HZ . Organ donation and transplantation—a Muslim viewpoint.
Transplant Proc 1992; 24 :2116–17.
9 Lam WA , McCullough LB. Influence of religious and spiritual values on the willingness of Chinese-Americans to donate organs for transplantation.
Clin
Transplant 2000; 14 :449–56.
www.bjophthalmol.com
841
EXTENDED REPORT
Histopathological and immunohistochemical studies of lenticules after epikeratoplasty for keratoconus
H Nakamura, F Riley, H Sakai, W Rademaker, B Y J T Yue, D P Edward
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :841–846. doi: 10.1136/bjo.2004.054684
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Deepak P Edward,
University of Illinois at
Chicago, Department of
Ophthalmology and Visual
Sciences, 1855 W Taylor
Street, Chicago, IL 60612,
USA; deepedwa@uic.edu
Accepted for publication
1 December 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aims: To examine histopathological and immunohistochemical changes in lenticules and host of corneal buttons from patients who previously underwent epikeratoplasty for keratoconus.
Methods: 12 penetrating keratoplasty specimens from patients with keratoconus who had previously undergone epikeratoplasty, eight keratoconus, and seven normal corneas were examined.
Immunostaining for Sp1, a 1-proteinase inhibitor ( a 1-PI), and a 2-macroglobulin ( a 2M) were performed.
Results: In nine of the 12 lenticules, the keratoconus-like disruptions were found in Bowman’s layer.
Peripheral and posterior keratocyte repopulation of the lenticules was observed in all cases. Keratocyte repopulation in the anterior and mid-stromal regions of the lenticules appeared related to the time since epikeratoplasty. Sp1 nuclear staining of the basal and wing epithelial cells was more intense in lenticules and keratoconus corneas than in normal corneas. Lenticular, host, and keratoconus keratocytes showed positive Sp1 staining, whereas staining was absent in normal corneas. Compared to normal corneas, a 1-
PI and a 2M immunostaining was lower in the lenticules, host, and keratoconus specimens.
Conclusions: The epithelial cells and keratocytes repopulated in the lenticules retain keratoconus-like biochemical abnormalities such as upregulation of Sp1 and downregulation of a 1-PI and a 2M. The authors speculate that both keratocytes and the corneal epithelium may participate in the development of keratoconus.
E pikeratoplasty is a form of lamellar refractive corneal surgery introduced in 1980.
1 The surgical procedure was first used to correct aphakia (epikeratophakia), 1–3 was then adapted for the treatment of myopia.
4 and
In this procedure, the recipient cornea is denuded of epithelium, and the edges of a preshaped donor lenticule are sutured to an annular keratectomy in the peripheral host cornea.
5
Epikeratoplasty has also been a surgical option for treatment of keratoconus 6 7 —for instance, for patients who engaged in strenuous physical activity 8 or in regions, such as Saudi
Arabia, where patients do not have easy access to tertiary care facilities.
9
Keratoconus, a non-inflammatory disease, is characterised by disruption of Bowman’s layer, 10–12 thinning and scarring of the stroma, and the eventual protrusion of the central cornea.
13 Immunohistochemical and biochemical studies have shown that the defect of keratoconus may involve an abnormality in degradation processes.
14 15 Enzymes, such as cathepsin B, are elevated, and protease inhibitors such as a 1proteinase inhibitor ( a 1-PI) and a 2-macroglobulin ( a 2M) are downregulated in keratoconus corneas.
16–18 Furthermore, our laboratory has reported that Sp1, a ubiquitous transcription factor, is upregulated in the corneas of keratoconus patients.
19 In cultured human corneal fibroblasts and epithelial cells overexpression of Sp1 has been shown to reppress the promoter activity of the a 1-PI gene.
20 21 This suggests that the Sp1-mediated downregulation of the a 1-PI gene may be a key event leading to the increased degradation and pathology in keratoconus corneas.
Histopathological analyses of failed epikeratoplasty lenticules for keratoconus and other corneal disease have been previously described.
22–30 In those reports, Bowman’s layer abnormalities in lenticules, including bends, 23 24 27 breaks, 24 and absences, 24 25 28 were identified, and the keratocyte repopulation into lenticules was noted to be more frequent in the anterior than the posterior region of central lenticules.
22 23 29 However, the reported abnormalities were unlike those observed in keratoconus corneas. These included large defects of Bowman’s layer that were believed to result from long term epithelial defects. These breaks were dissimilar to the focal ‘‘z’’-shaped disruptions in Bowman’s layer or absence of small segments of Bowman’s layer more typically seen in keratoconus corneas.
10 31 Such keratoconus-like fractures in Bowman’s layer were noted in the recipient grafts of recurrent keratoconus after penetrating keratoplasty.
32–36 Recurrent cases of keratoconus are rare and immunohistochemical and/or biochemical investigation of the grafts were not reported.
In this study we evaluated the histopathological and immunohistochemical changes in 12 lenticules from patients who previously underwent epikeratoplasty for keratoconus.
We investigated the integrity of Bowman’s layer of the lenticules, keratocyte repopulation in lenticules, and biochemical changes in the epithelium and stroma of both lenticules and host corneas. We found that the grafted lenticules displayed abnormalities similar to those found in keratoconus corneas.
MATERIALS AND METHODS
Twelve corneal buttons were obtained from patients who had previously received epikeratoplasty for management of keratoconus at the time of penetrating keratoplasty from the King Khaled Eye Specialist Hospital, Riyadh. The grafts were done because of varying degrees of uncorrected refractive problems following the epikeratoplasty. Seven normal human eyes from donors (ages 22–83 years old) were obtained from the Illinois Eye Bank, Chicago, or from the National Disease Research Interchange, Philadelphia, PA, within 24 hours of death. None of the donors had any known ocular diseases, and their corneas were clear and unremarkable. As another set of controls, eight corneal buttons from
Abbreviations: a 1-PI, a 1-proteinase inhibitor; a 2M, a 2-macroglobulin;
ECM, extracellular matrix www.bjophthalmol.com
842 Nakamura, Riley, Sakai, et al
Table 1 Patient data
Case
1
8
9
6
7
4
5
2
3
10
11
12
Sex
F
M
M
M
M
F
F
F
M
M
M
F
Age at PKP
33
23
32
16
24
28
21
22
46
20
23
23
PKP, penetrating keratoplasty; epiK, epikeratoplasty.
Period after epiK (year)
2.6
4.3
2.5
4.4
5.7
2.6
2.2
2.9
1.3
2.0
8.2
9.3
Lenticule cryofrozen cryofrozen cryofrozen cryofrozen and lyophilised cryofrozen cryofrozen cryofrozen cryofrozen cryofrozen cryofrozen cryofrozen cryofrozen and lyophilised patients (ages 22–70 years) with typical clinical features of keratoconus but without undergoing epikeratoplasty surgery previously were obtained following transplantation from the
Cornea Service at the University of Illinois at Chicago.
Corneas excised from normal human eyes and keratoconus buttons were fixed in 10% buffered formalin, processed, and embedded in paraffin. Immunohistochemistry was performed on deparaffinised 5 m m sections using the indirect immunoperoxidase technique. The primary antibodies used in the study included (a) a polyclonal rabbit anti-Sp1 antibody (PEP 2, diluted 1:100, Santa Cruz Biotechnology,
Santa Cruz, CA, USA), (b) polyclonal goat antibodies specific for a 1-PI (1:100, ICN Biomedicals, Irvine, CA, USA), and (c) a 2M (1:100, ICN Biomedicals). The chromogen used for the anti-Sp1 was fast red TR/naphthol AS-MX phosphate (Sigma,
St Louis, MO, USA). For a 1-PI and a 2M, 3,3-diaminobenzidine tetrahydrochloride (Sigma) was used as the chromogen.
The staining intensity in each experiment was scored by three masked observers on a scale of 0 to 4, with 0 indicating no staining and 4 the most intense staining. Experiments were repeated three times.
Histopathological changes in the epikeratoplasty specimens were evaluated on haematoxylin and eosin stained slides. Alterations in Bowman’s layer of the lenticules were evaluated only in the central regions of the specimens to exclude breaks seen along suture tracks in the peripheral regions of the specimens.
To confirm the labelling intensity evaluated by the masked observers we performed image analysis on the selected images presented in the paper demonstrating imunostaining with the three antibodies (see figs 3, 5, and 6). The image file was converted from RGB to grey scale image using Adobe
Photoshop 7.01. Imaging Processing Tool kit 3.0 (Reindeer
Games, Inc), incorporated in the Adobe Photoshop 7.01, was used to measure the intensity of staining. The intensity, judged as 256 shades of grey with 0 representing black and
256 representing white, was measured in at least six basal epithelial cells, wing cells, keratocytes, and/or six areas
(25 m m diameter circle) in the stromal matrix. Background intensity was also taken in the empty space. The staining intensity of each cell type or the stromal matrix tissue was obtained by subtracting the background from the measured intensity values. Statistical analysis was performed using two tailed unpaired Student’s t test to compare the staining intensity of KC or EpiK cornea with normal control. Values of p , 0.05 was considered to be significant.
RESULTS
The salient clinical features of the 12 patients who had previously received epikeratoplasty as a treatment for keratoconus are summarised in table 1.
By histopathology, the keratoconus-like breaks in
Bowman’s layer were found in nine of the 12 failed lenticules
(table 2, fig 1).
The presence or the number of the breaks was not correlated with either the sex or the length of period since epikeratoplasty.
Keratocyte repopulation was observed in all lenticules at all levels of the peripheral stroma (table 2). Keratocytes were identified morphologically by the spindle-shaped nature of their nuclei, which are quite distinct from other cells such as leucocytes that might be resident in the corneal stroma. The
Table 2 Histopathology results
Case
7
8
5
6
9
3
4
1
2
10
11
12
+
+
+
+
+
+
+
+
+
Bowman’s layer disruption
+
+
+
+
Keratocyte repopulation
Centre
A
+
M
+
+
+
+
+
P
+
+
+
+
+
+
+
+
+
+
+
+
A, anterior; M, middle; P, posterior.
Periphery
A
+
+
++
+
++
++
+
+
+
++
++
+
M
+
+
+
+
++
+
+
+
+
+
+
+
P
+
+
+
+
+
+
+
+
+
+
+
+ www.bjophthalmol.com
Histopathological and immunohistochemical studies of lenticules 843
Figure 1 Lenticules from patients who underwent epikeratoplasty for keratoconus (cases 5, 10, and 11). Arrow indicates the focal disruption in Bowman’s layer. The disruption or break resembles that described in keratoconus corneas (bar indicates magnification).
cells with spindle-shaped nuclei accounted for most of the cells within the lenticules. Rare cells consistent with leucocytes in the stroma were also noted. In the central region, repopulation was also observed in all lenticules in the posterior portion. Keratocytes that repopulated the posterior portion of the lenticules were mainly seen adjacent to
Bowman’s layer of the host corneas. In some areas, keratocytes appeared to migrate through the Bowman’s break of the host tissues (fig 2). However, repopulation in the anterior and mid-stromal region of the central lenticule was noted in only five lenticules. In these cases, the patients had a significantly longer history of epikeraptolasty than the others (5.8 (SD 2.8) v 2.7 (1.4) years; p , 0.05, Mann-Whitney
U test, tables 1 and 2).
Figure 2 The central portion of the lenticules and host corneas from cases 3 and 6. Arrow indicates Bowman’s layer of the host cornea.
Arrowheads indicate keratocytes repopulated in the lenticules. Asterisk denotes a break observed in Bowman’s layer of host. The symbol
^ indicates disruption of Bowman’s layer in the lenticule. In case 3, a spindle cell appeared to extend through the break in Bowman’s layer from the host stroma to the lenticule. The repopulated keratocytes were situated adjacent and right above the host Bowman’s layer. In case 6, keratocyte repopulation was observed throughout the anterior and posterior regions of the lenticules (bar indicates magnification).
Immunohistochemical experiments showed positive Sp1 staining in the nuclei of basal corneal epithelial cells and wing cells in the lenticules, as well as keratocytes in both the lenticules and host stromas. The staining intensity in the epithelial cells of lenticules and that in the stromal cells in the lenticules and host corneas were statistically higher than that in normal human corneas (p , 0.05, figs 3 and 4).
Keratoconus corneas, used as positive controls, also showed strong nuclear staining of comparable intensity for Sp1 in both corneal epithelial cells and keratocytes.
Compared to that in normal human corneas, immunostaining for both a 1-PI and a 2M was considerably weaker in epithelial cells of the lenticules, and keratocytes in the lenticules and host stromas (figs 5 and 6). Each of these differences was statistically significant (p , 0.05, figs 7 and 8).
A similar reduction in staining intensity was likewise observed in keratoconus corneas. Staining intensity in the stromal lamellae for a 1-PI in the lenticules and host corneas was also statistically lower than that in normal corneas
(p , 0.05, figs 6 and 7). The staining for a 2M was also reduced but the difference was not statistically significant from the normal controls (figs 6 and 8). In the epikeratoplasty specimens the immunoreactivity with three antibodies in
Figure 3 Immunostaining for Sp1 in corneas from a 61 year old normal individual and a 22 year old keratoconus patient, as well as a lenticule of a patient after epikeratoplasty for keratoconus (case 12). In both the lenticule and keratoconus corneas (positive controls), the nuclear immunolabelling was stronger in basal corneal epithelial cells, wing cells, and keratocytes than cells in the normal cornea (chromagen fast red TR/naphthol AS-MX phosphate). Image analysis confirmed significant differences in labelling intensity between normal control (epithelium: basal: 35.8 (SD 4); wing: 32 (4); stromal cell: 9 (3)) and epikeratoplasty (epithelium, basal: 64 (7) (p = 0.000008); wing: 59 (8) (p = 0.001); stromal cell: 82 (4) (p = 0.00001)), and keratoconus (epithelium: basal: 55 (4) (p = 0/001); wing: 55 (3) (p , 0.00001); stromal cell: 81 (2) (p = , 0.00001)).
www.bjophthalmol.com
844 Nakamura, Riley, Sakai, et al
2.0
1.0
Normal
Keratoconus
Lenticule
Host cornea
† † † †
0
Basal Wing
Epithelial cell
Superficial
Keratocyte
Figure 4 Staining intensity for Sp1 in the corneal epithelial cells and keratocytes in the lenticules (n = 12), host stromas (n = 12), and normal human (n = 4) and keratoconus (n = 3) corneas as scored by three masked observers. The scores were analysed by Mann-Whitney U tests.
* p , 0.01 compared with normal human specimens; p , 0.05.
the lenticular stroma and the host was comparable (figs 6, 7, and 8). As expected, the staining intensity was comparable in the keratoconus and epikeratoplasty specimens.
Image analysis confirmed the staining differences that were observed on semiquantitative assessment of labelling intensity (see fig 3, 5, and 6)
DISCUSSION
To the best of our knowledge, this is the first demonstration of keratoconus-like breaks in Bowman’s layer in lenticules from eyes that previously underwent epikeratoplasty as a treatment for keratoconus. The breaks observed in our study occurred with or without keratocyte repopulation and closely resembled those described previously in keratoconus. Both the presence of Bowman’s breaks and absence of Bowman’s layer have been reported previously in lenticules after epikeratoplasty for myopia, 24 25 28 nus.
28 aphakia, 24 28 and keratoco-
However, those large breaks, at times with almost total loss of Bowman’s layer, differed from the focal breaks or fragmentation observed in our cases in the failed lenticules and in typical keratoconus corneas.
10–12 Absence of large fragments of Bowman’s layer is unusual in typical keratoconus and if seen may be associated with hydrops or associated contact lens related complications.
The incidence of
Bowman’s layer disruption was also much higher in our cases (nine of 12 cases) than that in previous reports (eight of a total of 21 cases in the literature).
22–28
This is also the first demonstration of remarkable keratocyte repopulation of the posterior stroma in the central lenticule. Keratocyte repopulation in lenticule had been reported to be slow process from peripheral region, and to take 48 months to complete.
30 In our cases, the central posterior repopulation was noted in all 12 cases examined including seven lenticules which were examined at the time of less than 4 years after epikeratoplasty (fig 2 and table 2).
Since all of the lenticules in this series were cryofrozen before the epikeratoplasty, the donor keratocytes would not be expected to survive through the cryofreezing process.
37 38
Therefore, we suggest that the cells present in the lenticules were host keratocytes, and that the keratocytes in the posterior region of the lenticule migrated from underlying host tissue through breaks in the host Bowman’s layer.
As previously reported in eyes with and without keratoconus, 22 23 29 30 we noted that keratocytes repopulated the lenticules in the periphery, and that keratocyte repopulation was not predominant in the superficial and central region of the lenticules (table 2). In five lenticules, repopulation in the anterior or mid-stromal portions of central region was observed and the extent of keratocyte repopulation in these regions, interestingly, seemed to correlate with the length of time since epikeratoplasty. The time dependence supports a previous conclusion 30 that the anterior and middle lenticular keratocyte repopulation perhaps takes place gradually from the periphery, along stromal lamella.
Immunohistochemical experiments demonstrated that in the epithelium overlying the lenticules, Sp1 staining was increased and staining for inhibitors a 1-PI and a 2M was decreased. These have been shown to be changes that are specific to keratoconus corneas.
16–19 The epithelium of the lenticules thus displayed a keratoconus-like phenotype, which is not surprising as the epithelium was derived from
Figure 5 Immunostaining for a 1-proteinase inhibitor in corneas from 83 year old (top) and 78 year old (bottom) normal individuals, and a 70 year old keratoconus patient, as well as lenticules of patients after epikeratoplasty for keratoconus (cases 3 and 12). Arrow indicates Bowman’s layer of the host cornea. Arrowheads indicate keratocytes. Note that the intensity of the brown positive staining is lower in the epithelium, keratocytes, and stromal lamellae in the lenticules and host corneas than that in normal corneas. Staining is also weaker in keratoconus corneas compared to normal controls
(chromagen 3-3’ diaminobenzidine). Image analysis confirmed significant differences in labelling intensity between normal control (epithelium: basal:
153.5 (3); wing: 141 (3); stromal cell: 179 (3); stromal extracellular matrix (ECM) 72 (5)) and epikeratoplasty case 3 (epithelium: basal: 63 (8)
(p , 0.0000001); wing: 53 (4) (p , 0.000001); stromal cell in lenticule: 31 (6) (p = 0.000001), stromal ECM in lenticule: 14 (2) (p , 0.000001); stromal cell in host: 19 (2) (p , 0.00001), stromal ECM in host: 12 (1) (p , 00001)) and keratoconus (epithelium: basal: 43 (4) (p , 0.0000001); wing: 49.3 (10)
(p , 0.00000001); stromal cell: 37 (8) (p , 0.000001); stromal ECM 12.5 (3) (p , 0.00001)). Image analysis for case 12 also showed highly significant differences from control.
www.bjophthalmol.com
Histopathological and immunohistochemical studies of lenticules 845
Figure 6 Immunostaining for a 2-macroglobulin in corneas from 83 year old (top) and 22 year old (bottom) normal individuals (NH), lenticules of patients after epikeratoplasty for keratoconus (cases 5 and 6), and a cornea from a 70 year old keratoconus patient (KC). Arrow indicates Bowman’s layer of the host cornea. Arrowheads indicate keratocytes. The symbol
^ indicates disruption of Bowman’s layer in the lenticule. Note that the intensity of the brown positive staining is decreased in the epithelium, keratocytes, and stromal lamellae in the lenticules, host corneas, and keratoconus specimens when compared to the normal corneas (chromogen 3-3’ diaminobenzidine). Image analysis confirmed significant differences in labelling intensity between normal control (epithelium: basal: 91 (2); wing: 98 (6); stroma cell: 51 (7); stromal ECM: 12 (1)); epikeratoplasty (case 5) (epithelium: basal: 29 (9) (p , 0.00009); wing: 27 (4) (p = 0.00003); stromal cell in lenticule: 11 (13) (p = 0.0001); stromal ECM in lenticule: 5 (1) (p , 0.0001); stromal cell in host: 15 (18) (p = 0.001); stromal ECM in host: 1.8 (2) (p , 0.00004)) and keratoconus (epithelium: basal: 52 (5) (p , 0.0000003); wing:
55 (5) (p , 0.00000004); stromal cell:52 (14) p = 0.90; stromal ECM: 10 (1) (p = 0.03)).
the host. The role of the corneal epithelium in development of keratoconus was proposed in the 1960s 10 11 39 based on electron microscopic studies. Further evidence was provided when biochemical abnormalities including upregulation of degradative enzymes and downregulation of inhibitors were prominently observed in the keratoconus epithelium.
16–18 A study by three dimensional scanning electron microscopy 12 further indicated that the changes in the Bowman’s layer precede those in the corneal stroma and that the corneal epithelium may be an important factor at the early stage of keratoconus development. The current finding of alterations in the epithelium overlying the lenticules is consistent with this theory. It is possible that the corneal epithelium overlying the lenticules, with imbalanced enzyme and inhibitor levels, may cause disruption in Bowman’s layer typically seen in keratoconus specimens.
In the lenticular stroma, upregulation of Sp1 was demonstrated in the repopulated keratocytes. Downregulation of
PI and a a 1-
2M was also observed. These results indicate that the repopulated keratocytes retained the biochemical abnormalities ascribed to keratoconus. The rarity of recurrent cases of keratoconus after penetrating keratoplasty seems to argue against the corneal epithelial theory. Indeed, if the epithelial cells were the sole causative factor, 10 11 39 frequent recurrence of keratoconus would occur as the epithelial cells are expected around 5 days to migrate from the recipient into the donor cornea.
7 It is possible that the corneal epithelial involvement is necessary but not sufficient. We speculate that perhaps both the disruption of the Bowman’s layer 10 11 12 39 and a predisposed defect in keratocytes are required for the disease development. The current study, showing defects in
Bowman’s layer, delayed keratocyte repopulation, and biochemical abnormalities ascribed to keratoconus in the repopulated keratocytes in failed lenticules 15 months to
9 years after epikeratoplasty, supports this possibility.
3.0
Normal
Keratoconus
Lenticule
Host cornea
† † † † †
3.0
† † †
Normal
Keratoconus
Lenticule
Host cornea
2.0
2.0
1.0
1.0
0
Epithelium Keratocyte Stromal ECM
Figure 7 Staining intensity for a 1-proteinase inhibitor in corneal epithelial cells, keratocytes, and stromal extracellular matrix (ECM) in the lenticules, host stromas, and normal human and keratoconus corneas as scored by three masked observers. The scores were analysed by Mann-
Whitney U tests.
* p , 0.01 compared with normal human specimens; p , 0.05.
0
Epithelium Keratocyte Stromal ECM
Figure 8 Staining intensity for a 2-macroglobulin in corneal epithelial cells, keratocytes, and stromal extracellular matrix (ECM) in the lenticules, host stromas, and normal human and keratoconus corneas as scored by three masked observers. The scores were analysed by Mann-
Whitney U tests.
* p , 0.01 compared with normal human specimens; p , 0.05.
www.bjophthalmol.com
846 Nakamura, Riley, Sakai, et al
In summary, we demonstrated keratoconus-like disruptions in Bowman’s layer in nine of the 12 lenticules. The keratocytes appeared to repopulate the lenticules from the peripheral and underlying host tissues. By immunohistochemistry, Sp1 nuclear staining in both epithelium and stroma was increased in the lenticules and keratoconus than that in normal corneas. In contrast, immunostaining for a 1-
PI and a 2M in epithelial cells, keratocytes, and stromal lamellae was less intense in the lenticule, host corneas, and keratoconus specimens than in normal cornea. These findings suggested that the epithelial cells and keratocytes that repopulated the lenticules retained keratoconus-like biochemical abnormalities resulting in some of the changes noted in the lenticules.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
H Nakamura, H Sakai, B Y J T Yue, D P Edward, Department of
Ophthalmology and Visual Sciences, University of Illinois at Chicago
College of Medicine, Chicago, IL, USA
F Riley, W Rademaker, D P Edward, King Khaled Eye Specialist
Hospital, Riyadh, Saudi Arabia
Grant supports: William Pendill Research Fund; EY 03890 (BYJTY), EY
05628 (BYJTY) and EY01792 (core) from the National Eye Institute.
Competing interests: none declared
REFERENCES
1 Kaufman HE . The correction of aphakia. XXXVI Edward Jackson Memorial
Lecture.
Am J Ophthalmol 1980; 89 :1–10.
2 Werblin TP , Kaufman HE, Friedlander MH, et al.
Epikeratophakia: the surgical correction of aphakia. III. Preliminary results of a prospective clinical trial.
Arch Ophthalmol 1981; 99 :1957–60.
3 McDonald MB , Kaufman HE, Aquavella JV, et al.
The nationwide study of epikeratophakia for aphakia in adults.
Am J Ophthalmol 1987; 103 :358–65.
4 McDonald MB , Kaufman HE, Aquavella JV, et al.
The nationwide study of epikeratophakia for myopia.
Am J Ophthalmol 1987; 103 :375–83.
5 Waring GO 3rd . aking sense of ‘keratospeak’. A classification of refractive corneal surgery.
Arch Ophthalmol 1985; 103 :1472–7.
6 Kaufman HE , Werblin TP. Epikeratophakia for the treatment of keratoconus.
Am J Ophthalmol 1982; 93 :342–7.
7 McDonald MB , Kaufman HE, Durrie DS, et al.
Epikeratophakia for keratoconus. The nationwide study.
Arch Ophthalmol 1986; 104 :1294–300.
8 Goosey JD , Prager TC, Goosey CB, et al.
A comparison of penetrating keratoplasty to epikeratoplasty in the surgical management of keratoconus.
Am J Ophthalmol 1991; 112 :103–5.
9 Wagoner MD , Smith SD, Rademaker WJ, et al.
Penetrating keratoplasty vs epikeratoplasty for the surgical treatment of keratoconus.
J Refract Surg
2001; 17 :138–46.
10 Chi H , Katzin H, Teng C. Histopathology of keratoconus.
Am J Ophthalmol
1956; 42 :847–60.
11 Teng CC . Electron microscopic study of pathology of keratoconus.
Am J Ophthalmol 1963; 55 :18–47.
12 Sawaguchi S , Fukuchi T, Abe H, et al.
Three-dimensional scanning electron microscopic study of keratoconus corneas.
Arch Ophthalmol 1998; 116 :62–8.
13 Rabinowitz YS . Keratoconus.
Surv Ophthalmol 1998; 42 :297–319.
14 Yue BYJT , Sugar J, Benveniste K. Heterogeneity in keratoconus: possible biochemical basis.
Proc Soc Exp Biol Med 1984; 175 :336–41.
15 Yue BYJT , Sugar J, Benveniste K. RNA metabolism in cultures of corneal stromal cells from patients with keratoconus.
Proc Soc Exp Biol Med
1985; 178 :126–32.
16 Sawaguchi S , Twining SS, Yue BY, et al.
Alpha-1 proteinase inhibitor levels in keratoconus.
Exp Eye Res 1990; 50 :549–54.
17 Whitelock RB , Fukuchi T, Zhou L, et al.
Cathepsin G, acid phosphatase, and alpha 1-proteinase inhibitor messenger RNA levels in keratoconus corneas.
Invest Ophthalmol Vis Sci 1997; 38 :529–34.
18 Sawaguchi S , Twining SS, Yue BY, et al.
Alpha 2-macroglobulin levels in normal human and keratoconus corneas.
Invest Ophthalmol Vis Sci
1994; 35 :4008–14.
19 Whitelock RB , Li Y, Zhou L, et al.
Expression of transcription factors in keratoconus, a cornea-thinning disease.
Biochem Biophys Res Commun
1997; 235 :253–8.
20 Li Y , Zhou L, Twining SS, et al.
Involvement of Sp1 elements in the promoter activity of the a 1-proteinase inhibitor gene.
J Biol Chem 1998; 273 :9959–65.
21 Maruyama Y , Wang X, Li Y, et al.
Involvement of Sp1 elements in the promoter activity of genes affected in keratoconus.
Invest Ophthalmol Vis Sci
2001; 42 :1980–5.
22 Baumgartner SD , Binder PS. Refractive keratoplasty. Histopathology of clinical specimens.
Ophthalmology 1985; 92 :1606–15.
23 Binder PS , Baumgartner SD, Fogle JA. Histopathology of a case of epikeratophakia (aphakic epikeratoplasty).
Arch Ophthalmol
1985; 103 :1357–63.
24 Binder PS , Zavala EY. Why do some epikeratoplasties fail ?
Arch Ophthalmol
1987; 105 :63–9.
25 Bechara SJ , Grossniklaus HE, Waring GO 3rd. ubepithelial fibrosis after myopic epikeratoplasty. Report of a case.
Arch Ophthalmol
1992; 110 :228–32.
26 Morgan KS , Beuerman RW. Interface opacities in epikeratophakia.
Arch
Ophthalmol 1986; 104 :1505–8.
27 Tamaki K , Yamaguchi T, McDonald MB, et al.
Histological study of epikeratophakia tissue lenses for myopia removed from two patients.
Ophthalmology 1986; 93 :1502–8.
28 Frangieh GT , Kenyon KR, Wagoner MD, et al.
Epithelial abnormalities and sterile ulceration of epikeratoplasty grafts.
Ophthalmology 1988; 95 :213–27.
29 Grossniklaus HE , Lass JH, Jacobs G, et al.
Light microscopic and ultrastructural findings in failed epikeratoplasty.
Refract Corneal Surg
1989; 5 :296–301.
30 Yoon YD , Waring GO 3rd, Stulting RD, et al.
eratocyte repopulation in epikeratoplasty specimens.
Cornea 1998; 17 :180–4.
31 Feder RS . Noninflammatory ectatic disorders. In: Krachmer JH, Mannis MJ,
Holland EJ, eds.
Cornea . St Louis, Missouri: Mosby, 1997:1091–106.
32 Abelson MB , Collin HB, Gillette TE, et al.
Recurrent keratoconus after keratoplasty.
Am J Ophthalmol 1980; 90 :672–6.
33 Nirankari VS , Karesh J, Bastion F, et al.
Recurrence of keratoconus in donor cornea 22 years after successful keratoplasty.
Br J Ophthalmol
1983; 67 :23–8.
34 Bechrakis N , Blom ML, Stark WJ, et al.
Recurrent keratoconus.
Cornea
1994; 13 :73–7.
35 Kremer I , Eagle RC, Rapuano CJ, et al.
Histologic evidence of recurrent keratoconus seven years after keratoplasty.
Am J Ophthalmol
1995; 119 :511–12.
36 Bourges JL , Savoldelli M, Dighiero P, et al.
Recurrence of keratoconus characteristics: a clinical and histologic follow-up analysis of donor grafts.
Ophthalmology 2003; 110 :1920–5.
37 Rich LF , Friedlander MH, Kaufman HE, et al.
Keratocyte survival in keratophakia lenticules.
Arch Ophthalmol 1981; 99 :677–80.
38 Zavala EY , Binder PS, Deg JK, et al.
Refractive keratoplasty: lathing and cryopreservation.
CLAO J 1985; 11 :155–62.
39 Iwamoto T , Devoe AG. Particulate structures in keratoconus.
Arch Ophthalmol
Rev Gen Ophtalmol 1975; 35 :65–76.
www.bjophthalmol.com
847
EXTENDED REPORT
A comparison of four methods of tonometry: method agreement and interobserver variability
P-A Tonnu, T Ho, K Sharma, E White, C Bunce, D Garway-Heath
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :847–850. doi: 10.1136/bjo.2004.056614
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
D F Garway-Heath, MD,
FRCOphth, Glaucoma
Research Unit, Moorfields
Eye Hospital, London
EC1V 2PD, UK; david.garway-heath@ moorfields.nhs.uk
Accepted for publication
12 November 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aim: To compare the inter-method agreement in intraocular pressure (IOP) measurements made with four different tonometric methods.
Methods: IOP was measured with the Goldmann applanation tonometer (GAT), Tono-Pen XL, ocular blood flow tonograph (OBF), and Canon TX-10 non-contact tonometer (NCT) in a randomised order in one eye of each of 105 patients with ocular hypertension or glaucoma. Three measurements were made with each method, and by each of two independent GAT observers. GAT interobserver and tonometer inter-method agreement was assessed by the Bland-Altman method. The outcome measures were 95% limits of agreement for IOP measurements between GAT observers and between tonometric methods, and 95% confidence intervals for intra-session repeated measurements.
Results: The mean differences (bias) in IOP measurements were 0.4 mm Hg between GAT observers, and
0.6 mm Hg, 0.1 mm Hg, and 0.7 mm Hg between GAT and Tono-Pen, OBF, and NCT, respectively. The
95% limits of agreement were smallest (bias ¡ 2.6 mm Hg) between GAT observers, and larger for agreement between the GAT and the Tono-Pen, OBF, and NCT (bias ¡ 6.7, ¡ 5.5, and ¡ 4.8 mm Hg, respectively). The OBF and NCT significantly underestimated GAT measurements at lower IOP and overestimated these at higher IOP. The repeatability coefficients for intra-session repeated measurement for each method were ¡ 2.2 mm Hg and ¡ 2.5 mm Hg for the GAT, ¡ 4.3 mm Hg for the Tono-Pen,
¡ 3.7 mm Hg for the OBF, and ¡ 3.2 mm Hg for the NCT.
Conclusions: There was good interobserver agreement with the GAT and moderate agreement between the NCT and GAT. The differences between the GAT and OBF and between the GAT and Tono-Pen probably preclude the OBF and Tono-Pen from routine clinical use as objective methods to measure IOP in normal adult eyes.
I ntraocular pressure (IOP) measurement has an important role in case detection and management of primary open angle glaucoma. Ocular hypertension (OHT) is associated with an increased risk of developing glaucoma, 1 and reducing
IOP has been shown to lessen progressive loss of the visual field.
2 Accurate and precise measurement of IOP is, therefore, fundamental to management of glaucoma.
Applanation tonometry is the method of measuring IOP with instruments that indent or flatten the corneal apex. The
Goldmann applanation tonometer (GAT) is regarded as the
’’gold standard.’’ However, there are other objective instruments such as the Tono-Pen, ocular blood flow tonograph
(OBF), and the non-contact tonometers (NCTs). The NCT has the potential advantage that it uses an air puff to indent the cornea, reducing the possible risk of cross infection with agents such as adenovirus and variant Creutzfeld-Jakob disease.
3 4 In the United Kingdom, most referrals for suspect glaucoma from the primary care setting (optometry practices) are on the basis of NCT measurements. It is therefore important to determine whether the NCT is sufficiently accurate and precise.
Various studies have compared one or two of these instruments with the GAT, 5–12 and most studies have not compared inter-tonometer agreement with GAT interobserver agreement (variation in measured IOP arise from both intertonometer and interobserver differences). To our knowledge, a broad comparison of all instruments in the same group of patients has not been published.
This study was designed to assess the relative agreement of four methods of tonometry (GAT, Tono-Pen, OBF, and NCT), and to compare inter-instrument agreement with interobserver agreement of GAT IOP measurements.
MATERIALS AND METHODS
The study was conducted in the glaucoma research unit at
Moorfields Eye Hospital (London, UK). One hundred and five untreated patients attending the ocular hypertension, normal tension glaucoma, or glaucoma primary care clinics participated in the study. The study was approved by the Moorfields
Eye Hospital institutional review board.
Examination was conducted on either eye (chosen randomly) of each patient. Eyes were anaesthetised with
Benoxinate and fluorescein drops (Moorfields Eye Hospital
Pharmacy, London, UK). Measurements (GAT, Tono-Pen,
OBF, and NCT) were performed in a randomised order, with a recovery of about 2 minutes between methods.
13 Three readings were taken with each instrument, and with the GAT three readings were recorded by each of two observers. The mean of the three readings was used for comparison between tonometers. All tonometers were calibrated at the start of the study and all IOP measurements (except for the GAT) were made and recorded by a single observer (P-AT).
CCT was measured with the Altair ultrasonic pachymeter
(Optikron 2000, Rome, Italy) after tonometric measurements had been performed.
Goldmann applanation tonometry
IOP was measured with the Goldmann Applanation
Tonometer (Haag-Streit, Bern, Switzerland) by two observers. Observer 1 was a medical student (P-AT) and observer 2 was any one of seven medical staff (four ophthalmologists
Abbreviations: CCT, central corneal thickness; GAT, Goldmann applanation tonometer; IOP, intraocular pressure; NCT, non-contact tonometer; OBF, ocular blood flow; OHT, ocular hypertension www.bjophthalmol.com
848 Tonnu, Ho, Sharma, et al
Table 1 Patient data
Age (years)
Sex (% male)
Eye side (% right)
CCT ( m m)
GAT observer 1 IOP (mm Hg)
GAT observer 2 IOP (mm Hg)
Tono-Pen IOP (mm Hg)
OBF IOP (mm Hg)
NCT IOP (mm Hg)
Mean
64.6
50
52
546.5
17.2
17.6
16.6
17.1
16.4
SD
13.2
39.8
4.3
4.9
4.4
5.9
5.0
Range
23–87
436–664
09–32
09–35
07–29
08–34
07–29
CCT, central corneal thickness; GAT, Goldmann applanation tonometer;
OBF, ocular blood flow; NCT, non-contact tonometer.
and three ophthalmic technicians). For the majority of measurements, observer 2 was an ophthalmologist (KS).
All observers were trained and validated in tonometry.
Measurements were made in a masked fashion: one observer set the dial to a ’’random 0’’ (between 5 mm Hg and
10 mm Hg); the other observer applanated, turned the dial to obtain the end point without looking at the dial, and the first observer recorded the pressure. The procedure was repeated with the two observers changing roles.
Tono-Pen tonometry
The Tono-Pen XL (Mentor, Santa Barbara, CA, USA) was calibrated daily. The operator touched the cornea with the pen tip several times until a reading was displayed. Only measurements with a standard error smaller than 5% were accepted. If successive measurements differed by more than
5 mm Hg, the procedure was repeated.
Ocular blood flow tonometry
Measurements with the ocular blood flow tonograph (OBF
Labs Ltd, Malmesbury, Wiltshire, UK) were made with the slit lamp mounted probe. A new disposable and calibrated
OBF tip was used for each subject. The subject’s cornea was applanated for 5–10 seconds while approximately 200 IOP measurements were taken and averaged to give the final digital readout.
Non-contact tonometry
The Canon TX-10 non-contact tonometer (Canon USA Inc,
One Canon Plaza, Lake Success, NY, USA) automatically recorded three IOP readings. Anaesthetic drops were administered to subjects randomised to have NCT first, so that examination conditions were equivalent to those who had other tonometric measurements beforehand.
Statistical analyses
Analyses were performed in Microsoft Excel 97 SR-2
(Microsoft Corp, Seattle, WA, USA), MedCalc version 7.2.10
15
10
5
0
–5
–10
–15
GAT
GAT
GAT
NCT
GAT
OBF
GAT
Tonopen
Inter-method comparisons
Figure 1 Box plot of inter-method differences. The box represents the interquartile range which contains the 50% of values. The line across the box indicates the median. The whiskers are lines that extend from the box to the highest and lowest values, excluding outliers. Circles indicate outliers.
(Mariakerke, Belgium), and SPSS for Windows version 10.0.0
(SPSS Inc, Chicago, IL, USA).
For randomisation, each method was assigned a number and a table of random permutations indicated the order of the instruments to be used for subject.
The effect of repeated testing on IOP was assessed for each technique as the difference between the first and third measurements.
Bland-Altman plots were constructed for comparisons between methods and between GAT observers. The systematic difference between methods was termed the ‘‘bias’’ and random differences were quantified by the ‘‘limits of agreement.’’ Where there was no relation between intermethod or interobserver differences and IOP magnitude, bias was calculated as the mean difference, and 95% limits of agreement computed (provided that the differences followed a normal distribution). Where there was a trend of increasing
(or decreasing) inter-method/interobserver difference across the range of IOP, regression was conducted and regression based limits of agreement calculated.
Repeatability coefficients were computed as 2.77 times the within subject standard deviation (wsSD) for repeated measurements by the same tonometric method:
RESULTS
Table 1 lists summary data.
Figure 1 is a summary plot of the median and range of IOP measurement differences between GAT observers and between GAT observer 1 and other tonometers. The median
Table 2 Agreement between tonometry methods: bias and 95% limits of agreement (or regression based equivalents) * either side of bias
Tonometry method
Tono-Pen (mm Hg)
Goldmann observer 2 (mm Hg)
OBF (mm Hg)
NCT (mm Hg)
Estimated bias
0.6
1.7–(0.12
6 mean)
6.0–(0.35
6 mean)
3.6–(0.17
6 mean)
95% limits of agreement
Bias
¡
6.5
Bias
¡
2.6
Bias
¡
5.4
Bias
¡
4.8
OBF, ocular blood flow; NCT, non-contact tonometer.
* GAT observer 1 was the reference for comparison.
Difference between methods related to mean of methods. Bias and 95% limits of agreement calculated from linear regression of method differences against method mean.
www.bjophthalmol.com
Comparison of tonometry methods
Table 3 Estimates (95% limits of agreement) for differences between GAT observer 1 and
GAT observer 2, and between GAT observer 1 and other tonometric methods, at various
IOP levels
Goldmann observer 2
OBF
NCT
Tono-Pen
IOP (mm Hg)
10
0.5 ( 2 2.1, 3.1)
2.6 ( 2 2.9, 8.0)
1.9 ( 2 2.9, 6.7)
0.6 ( 2 5.9, 7.1)
15
2 0.1 ( 2 2.7, 2.5)
0.8 ( 2 4.6, 6.3)
1 ( 2 3.7, 5.8)
0.6 ( 2 5.9, 7.1)
20
2 0.7 ( 2 3.3, 1.9)
2 0.9 ( 2 6.3, 4.6)
0.2 ( 2 4.6, 5.0)
0.6 ( 2 5.9, 7.1)
25
2 1.3 ( 2 3.9, 1.3)
2 2.6 ( 2 8.1, 2.8)
2 0.6 ( 2 5.4, 4.2)
0.6 ( 2 5.9, 7.1)
849 difference between GAT observers, and between GAT observer 1 and other tonometers was small.
Table 2 lists the bias and 95% limits of agreement for comparisons between GAT observer 1 and GAT observer 2 and other tonometers. The interobserver differences for the
GAT were small in comparison with inter-instrument differences (fig 1 and table 2). The 95% limits of agreement between other pairs of instrument were all wider than the comparisons with GAT (data not shown).
Observer 2, OBF, and NCT had a slight tendency to overestimate IOP measurements made by observer 1 at high pressures. Table 3 sets out the mean difference and 95% limits of agreement between instruments at four IOP levels.
The repeatability coefficient of the GAT observers
(2.2 mm Hg and 2.5 mm Hg) was lower than that of the other tonometers (3.2 mm Hg, 3.7 mm Hg, and 4.3 mm Hg for the NCT, OBF, and Tono-Pen, respectively). Two readings by the same observer will be within the repeatability coefficient for 95% of the subjects.
There was no significance difference between the first and third IOP measurements for GAT observer 1, Tono-Pen, or
NCT. For GAT observer 2 and the OBF, the first measurement was larger than the third (difference 0.2 mm Hg, p = 0.06 and
0.6 mm Hg, p = 0.02, respectively).
DISCUSSION
In this study, one GAT observer was constant and the other was any one of a number of trained staff (ophthalmologist or ophthalmic technician). This methodology reflects the clinical setting where patients have IOP measured by different personnel at each visit. There was good agreement between the observers (tables 1, 2), with 95% limits of agreement consistent with previous studies ( ¡ 2.2 to
¡ 3.1 mm Hg, table 4).
11 14 Agreement was better between the two GAT observers than between the GAT and other tonometers (table 2).
GAT/Tono-Pen comparisons
The 95% limits of agreement between the GAT observer 1 and
Tono-Pen XL (table 2) were consistent with previous reports
(table 4).
The average measurement difference (0.6–
1.0 mm Hg, table 1) was small, and there was no tendency for the difference to vary with the level of the IOP (table 2).
This is consistent with data reported by Bafa et al and
Bandyopadhyay et al (table 4).
9 15 In contrast, a tendency for the Tono-Pen to underestimate IOP at high IOP levels has been reported in studies comparing manometric and Tono-
Pen IOP measurements, 16 with the Tono-Pen 17 18 and in those comparing the GAT or Tono-Pen XL.
10
Table 4 Mean difference and 95% limits of agreement between GAT and other tonometric instruments—summary of findings from this and previous studies. Values (mm Hg) are given as means (95% CI); a positive mean difference indicates that
Goldmann values are higher
Study
This study
Thorburn, 1978 14
Bandyopadhyay et al , 2002 15
Iester et al , 2001 10
Bafa et al , 2001 9
Midelfart and Wigers, 1994 26
Geyer et al , 1992 5
Frenkel et al , 1988 18
Minckler et al , 1987 27
Kao et al , 1987 17
Gunvant et al , 2004 20
Yang et al , 2000 8
Bhan et al , 2003 19
Jorge et al , 2003 21
Jorge et al , 2002 12
Popovich and Shields, 1997 7
Hansen, 1995 6
Kretz and Demailly, 1992 23
Hollo et al , 1992 28
Myers et al , 1990 29
Parker et al , 2001 11
Mackie et al , 1996 22
GAT interobserver differences
2 0.4 (2.6) `
2 0.7 (3.1)
2 0.1 (2.2)
Tono-Pen
+ 0.6 (6.5) **
2 1.0 (4.5) **
+ 0.2 (6.3) **
2 0.6 (8.3) **
+ 2.4 (4.6) ***
+ 3.9 (6.5) *
+ 0.8 (6.1) *
+ 1.7 (6.1) *
2 0.5 (7.4) *
OBF
+ 0.1 (5.4) `
2 0.7 (7.7)
2 0.5 (6.3) `
+ 0.26 (4.6)
2 2.7 (6.6) `
NCT
+ 0.7 (4.8) `
2 0.1 (3.3)
2 0.1 (2.2)
+ 0.9 (2.5)
+ 0.6 (4.5)
+ 0.9 (4.9)
+ 0.1 (2.9)
2 3.9 (5.7)
2 0.7 (5.3)
2 0.5 (2.2)
2 1.0 (7.1)
NCT type
Canon TX-10
Reichert AT550
Reichert AT550
Reichert XpertP
Reichert XPERT
Reichert XPERT
Reichert XPERT
Reichert XPERT
Reichert XPERT
Keeler Pulsair 3000
Keeler Pulsair 2000
OBF, ocular blood flow; NCT, non-contact tonometer.
* Oculab Tono-Pen; ** Mentor Tono-Pen XL; *** Bio-Rad Tono-Pen XL; OBF tonograph (OBF Labs).
Overall value: tonometer overestimates GAT at low IOPs and underestimates at high IOPs.
` Overall value: tonometer underestimates GAT at low IOPs and overestimates at high IOPs.
www.bjophthalmol.com
850 Tonnu, Ho, Sharma, et al
GAT/OBF comparisons
On average, the OBF slightly underestimated IOP measurements by the GAT (table 1), in agreement with Yang et al .
8 In contrast, an overestimation by the OBF was reported by Bafa et al 9 and Bhan et al.
19 The 95% limits of agreement were similar to previous findings (table 4).
The OBF underestimated GAT IOP by 2.6 mm Hg at
15 mm Hg and overestimated GAT IOP by 2.6 mm Hg at
25 mm Hg (table 3). This finding is in agreement with those of Bhan et al 19 and Gunvant et al , 20 but contrary to those of
Yang et al .
8
GAT/NCT comparisons
There are no reports on the relative performance of Canon
TX-10. However, other NCT instruments have been evaluated
(table 4).
The 95% limits of agreement between the GAT and Canon
TX-10 correspond well with previous reports for the XPERT
NCT, but are not as good as those reported for the Keeler
Pulsair 3000, 11 and the Reichert AT550 in normal 12 and glaucomatous 21 eyes (table 4).
The NCT had a tendency to overestimate the GAT at high
IOP, and underestimate the GAT at low IOP (table 2).
Although this effect is not seen in most reports for GAT/NCT comparisons, 6 11 12 21 22 Kretz and Demailly 23 reported a marginal effect in the same direction. Factors such as CCT
(evaluated in the companion paper) may contribute to relative IOP overestimation at higher measured IOP levels.
The repeatability coefficient, for two readings by the same observer, was better for the GAT than the other tonometers, with values comparable to those reported by Pandav et al
(2.6 mm Hg).
24 The value for the NCT is comparable to
Vernon’s figure for the Keeler Pulsair 2000 (4.2 mm Hg and
3.6 mm Hg for right and left eyes, respectively).
25
The results indicate that repeated readings with the GAT, both within and between observers, are much more reproducible than any of the more automated forms of tonometry. There is moderate inter-instrument agreement between the NCT and GAT and poor agreement between the
Tono-Pen and OBF with GAT.
ACKNOWLEDGEMENTS
The authors thank Haag Streit UK for providing the Canon TX-10 non-contact tonometer.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
P-A Tonnu, T Ho, K Sharma, E White, D Garway-Heath, Glaucoma
Research Unit, Moorfields Eye Hospital, London EC1V 2PD, UK
C Bunce, Department of Research and Development, Moorfields Eye
Hospital, London EC1V 2PD, UK
REFERENCES
1 Gordon MO , Beiser JA, Brandt JD, et al.
The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma.
Arch Ophthalmol 2002; 120 :714–20.
2 Heijl A , Leske MC, Bengtsson B, et al.
Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial.
Arch
Ophthalmol 2002; 120 :1268–79.
3 Walia JS , Chronister CL. Possible iatrogenic transmission of Creutzfeldt-Jakob disease via tonometer tips: a review of the literature.
Optometry
2001; 72 :649–52.
4 Desai SP , Sivakumar S, Fryers PT. Evaluation of a disposable prism for applanation tonometry.
Eye 2001; 15 :279–82.
5 Geyer O , Mayron Y, Loewenstein A, et al.
Tono-Pen tonometry in normal and in post-keratoplasty eyes.
Br J Ophthalmol 1992; 76 :538–40.
6 Hansen MK . Clinical comparison of the XPERT non-contact tonometer and the conventional Goldmann applanation tonometer.
Acta Ophthalmol Scand
1995; 73 :176–80.
7 Popovich KS , Shields MB. A comparison of intraocular pressure measurements with the XPERT noncontact tonometer and Goldmann applanation tonometry.
J Glaucoma 1997; 6 :44–6.
8 Yang YC , Illango B, Cook A, et al.
Intraocular pressure and pulse rate measurements by the OBF tonograph—comparison to reference instruments.
Ophthal Physiol Opt 2000; 20 :401–407.
9 Bafa M , Lambrinakis I, Dayan M, et al.
Clinical comparison of the measurement of the IOP with the ocular blood flow tonometer, the Tonopen XL and the Goldmann applanation tonometer.
Acta Ophthalmol Scand
2001; 79 :15–18.
10 Iester M , Mermoud A, Achache F, et al.
New Tonopen XL: comparison with the Goldmann tonometer.
Eye 2001; 15 :52–8.
11 Parker VA , Herrtage J, Sarkies NJ. Clinical comparison of the Keeler Pulsair
3000 with Goldmann applanation tonometry.
Br J Ophthalmol
2001; 85 :1303–4.
12 Jorge J , Diaz-Rey JA, Gonzalez-Meijome JM, et al.
Clinical performance of the Reichert AT550: a new non-contact tonometer.
Ophthalmic Physiol Opt
2002; 22 :560–4.
13 Recep OF , Hasiripi H, Vayisoglu E, et al.
Accurate time interval in repeated tonometry.
Acta Ophthalmol Scand 1998; 76 :603–5.
14 Thorburn W . The accuracy of clinical applanation tonometry.
Acta
Ophthalmol (Copenh) 1978; 56 :1–5.
15 Bandyopadhyay M , Raychaudhuri A, Lahiri SK, et al.
Comparison of
Goldmann applanation tonometry with the Tonopen for measuring intraocular pressure in a population-based glaucoma survey in rural West Bengal.
Ophthalmic Epidemiol 2002; 9 :215–24.
16 Foster PJ , Wong JS, Wong E, et al.
Accuracy of clinical estimates of intraocular pressure in Chinese eyes.
Ophthalmology
2000; 107 :1816–21.
17 Kao SF , Lichter PR, Bergstrom TJ, et al.
Clinical comparison of the Oculab
Tono-Pen to the Goldmann applanation tonometer.
Ophthalmology
1987; 94 :1541–4.
18 Frenkel RE , Hong YJ, Shin DH. Comparison of the Tono-Pen to the Goldmann applanation tonometer.
Arch Ophthalmol 1988; 106 :750–3.
19 Bhan A , Bhargava J, Vernon SA, et al.
Repeatability of ocular blood flow pneumotonometry.
Ophthalmology 2003; 110 :1551–4.
20 Gunvant P , Baskaran M, Vijaya L, et al.
Effect of corneal parameters on measurements using the pulsatile ocular blood flow tonograph and Goldmann applanation tonometer.
Br J Ophthalmol 2004; 88 :518–22.
21 Jorge J , Gonzalez-Meijome JM, Diaz-Rey JA, et al.
Clinical performance of non-contact tonometry by Reichert AT550 in glaucomatous patients.
Ophthalmic Physiol Opt 2003; 23 :503–6.
22 Mackie SW , Jay JL, Ackerley R, et al.
Clinical comparison of the Keeler Pulsair
2000, American Optical MkII and Goldmann applanation tonometers.
Ophthalmic Physiol Opt 1996; 16 :171–7.
23 Kretz G , Demailly P. X-PERT NCT advanced logic tonometer valuation.
Int
Ophthalmol 1992; 16 :287–90.
24 Pandav SS , Sharma A, Gupta A, et al.
Reliability of proton and goldmann applanation tonometers in normal and postkeratoplasty eyes.
Ophthalmology
2002; 109 :979–84.
25 Vernon SA . Reproducibility with the Keeler Pulsair 2000 non-contact tonometer.
Br J Ophthalmol 1995; 79 :554–7.
26 Midelfart A , Wigers A. Clinical comparison of the ProTon and Tono-Pen tonometers with the Goldmann applanation tonometer.
Br J Ophthalmol
1994; 78 :895–8.
27 Minckler DS , Baerveldt G, Heuer DK, et al.
Clinical evaluation of the Oculab
Tono-Pen.
Am J Ophthalmol 1987; 104 :168–73.
28 Hollo G , Follmann P, Pap G. A clinical evaluation of XPERT NCT
(Reichert) for glaucoma screening by optometrists.
Int Ophthalmol
1992; 16 :291–3.
29 Myers KJ , Lalle P, Litwak A, et al.
XPERT NCT—a clinical evaluation.
J Am
Optom Assoc 1990; 61 :863–9.
www.bjophthalmol.com
851
EXTENDED REPORT
The influence of central corneal thickness and age on intraocular pressure measured by pneumotonometry, noncontact tonometry, the Tono-Pen XL, and Goldmann applanation tonometry
P-A Tonnu, T Ho, T Newson, A El Sheikh, K Sharma, E White, C Bunce, D Garway-Heath
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :851–854. doi: 10.1136/bjo.2004.056622
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
D F Garway-Heath, MD,
FRCOphth, Glaucoma
Research Unit, Moorfields
Eye Hospital, London
EC1V 2PD, UK; david.garway-heath@ moorfields.nhs.uk
Accepted for publication
12 November 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aims: To evaluate the influence of central corneal thickness (CCT) on intraocular pressure (IOP) measurements made with the Goldmann applanation tonometer (GAT), Tono-Pen XL, ocular blood flow tonograph (OBF), and Canon TX-10 non-contact tonometer (NCT).
Methods: CCT was recorded for either eye (randomly selected) of each of 105 untreated patients with ocular hypertension and glaucoma attending the glaucoma research unit at Moorfields Eye Hospital. For each of the selected eyes, IOP was measured with the GAT (two observers), Tono-Pen, OBF, and NCT in a randomised order. The relation of measured IOP and of inter-tonometer differences with CCT and subject age was explored by linear regression analysis.
Results: A significant association between measured IOP and CCT was found with each instrument. The change in measured IOP for a 10 m m increase in CCT was 0.28, 0.31, 0.38, and 0.46 for the GAT, Tono-
Pen, OBF, and NCT, respectively (all p ( 0.05). There was a significant association between the NCT/GAT differences and CCT, with a tendency of NCT to overestimate GAT in eyes with thicker corneas. There was a significant association between GAT/Tono-Pen and OBF/Tono-Pen differences and age, with a tendency of GAT and OBF to overestimate the Tono-Pen in eyes of older subjects.
Conclusion: IOP measurement by all four methods is affected by CCT. The NCT is affected by CCT significantly more than the GAT. Subject age has a differential effect on the IOP measurements made by the GAT and OBF compared to the Tono-Pen.
C entral corneal thickness (CCT) is known to affect the accuracy of intraocular pressure (IOP) measurements by applanation tonometry.
1 2 A thicker cornea requires greater force to applanate and, conversely, a thinner cornea is more easily flattened. A thin cornea is a significant risk factor for the development of glaucoma 3 and it has yet to be determined whether this is an independent effect or a result of the influence of CCT on IOP measurements.
Most published studies concerning the effect of CCT on measured IOP relate to the Goldmann applanation tonometer
(GAT). However, there is increasing evidence that other tonometers share this problem.
4–6 The GAT, Tono-Pen, ocular blood flow tonograph (OBF), and non-contact tonometer
(NCT) all use an applanation principle. Thin shell theory was used by Orssengo and Pye to demonstrate that corneal radius, thickness and material stiffness affect the applanation pressure for a given IOP. Reducing the applanation area reduces the difference between the applanation pressure and
IOP, because of the reduced resistance offered by the cornea for a smaller contact area.
7 There may also be some reduced effects from surface tension.
The GAT is based on the Imbert-Fick law, 1 8 which assumes that the cornea has a dry surface, is infinitely thin, and behaves as a ‘‘membrane’’ where the applanating pressure will equal the IOP. In practice, a resistance force, because of the thickness of the cornea, and a surface tension force, the result of the tear film, act upon the applanator causing this membrane assumption to be incorrect. These forces balance each other for the GAT (applanation diameter of 3.06 mm) when the CCT is 520 m m, providing a ‘‘reference’’ value where the applanating pressure does equal the IOP.
1
The NCT uses a puff of air directed at the cornea with an applanation area, for the Canon TX-10, similar to that of the
GAT. The force produced by the air puff is linearly increased over 8 ms and progressively flattens the cornea. When flat, the cornea acts as a mirror reflecting a light beam onto a sensor that triggers a reading. The Tono-Pen works on a principle similar to the MacKay-Marg tonometer 9 applanation area smaller (2.36 mm
2 and has an
) than that of the GAT
(7.35 mm 2 ).
10 The OBF, or pneumatonometer, measures the pressure in a flowing column of gas (tonometer chamber) directed towards a thin membrane (diameter about 2.5 mm) in contact with the surface of the cornea. The probe tip has an outer diameter of about 5 mm. A portion of the gas flow pushes the outer part of the tonometer tip against the cornea, depressing its surface, and a portion maintains the pressure required to balance the pressure on the other side of the tip membrane (that is, the IOP) in the central part of the probe tip.
11 12 The probe tip applanates the cornea for about 5–
10 seconds while a continuous IOP trace is recorded.
In the companion paper, we reported the level of agreement between IOP measurements made with the GAT,
Tono-Pen XL, OBF, and Canon TX-10 NCT. The effect of CCT and subject age on tonometric measurements made with these four techniques is described in this paper. The study reported in this paper is the first to compare all four tonometric methods in the same eyes.
Abbreviations: CCT, central corneal thickness; DCT, dynamic contour tonometer; GAT, Goldmann applanation tonometer; IOP, intraocular pressure; NCT, non-contact tonometer; OBF, ocular blood flow; ORA, ocular response analyser www.bjophthalmol.com
852
Table 1 Association between measured intraocular pressure and central corneal thickness for each method, as determined by linear regression analysis
GAT 1
GAT 2
Tono-Pen
OBF
NCT
Slope
0.028
0.026
0.031
0.038
0.046
95% CI for slope
0.006 to 0.049
0.0002 to 0.051
0.010 to 0.053
0.009 to 0.068
0.022 to 0.070
Adjusted R 2
0.05
0.04
0.07
0.05
0.12
p Value
0.011
0.033
0.004
0.012
0.000
Tonnu, Ho, Newson, et al
MATERIALS AND METHODS
Details of the study design, and materials and methods have been given in the companion paper. Table 1 of the companion paper lists patient data, CCT values and range of IOP measurements made with the four tonometers.
Statistical analyses
Linear regression analysis was used to explore the relations between measured IOP and CCT and subject age and between tonometry inter-method differences and CCT and age. With
105 subjects, the study had a power of 80% at p = 0.05 to detect a correlation of 0.245 ( ; r
2
0.06) between measured
IOP and CCT (one sided test). Estimation of the effect of age was a post hoc analysis justified by suggestions in the literature that the cornea stiffens with age.
13–15
The relation between tonometry inter-method differences and CCT and inter-method mean IOP was sought by stepwise multiple linear regression (CCT and IOP as the independent variables; probability of F to enter = 0.05 and to remove = 0.10).
RESULTS
The association of measured IOP and CCT with each tonometer is summarised in table 1. The effect of CCT was least for the GAT and greatest for NCT, although the 95% confidence limits for the slopes overlapped for all four methods.
The GAT/NCT differences were significantly related to CCT for both GAT observers (see fig 1 for GAT observer 1); the equations were:
Observer 1: GAT/NCT difference = ( 2 0.187
6 CCT) + 10.9
(adjusted R
2
= 0.07; p = 0.003)
Observer 2: GAT/NCT difference = ( 2 0.199
6 CCT) + 12.0
(adjusted R
2
= 0.08; p = 0.002)
GAT/NCT differences were significantly related both to method mean IOP and to CCT for GAT observer 1 only; the equations were:
GAT/NCT difference = ( 2 0.129
6 IOP) + ( 2 0.014
6 CCT) +
10.5 (adjusted R 2 = 0.11; p = 0.02 for the IOP coefficient and p = 0.03 for the CCT coefficient). Thus, the difference between GAT observer 1 and NCT increased both with the level of IOP and CCT.
4
2
8
6
0
–2
–4
–6
–8
450 500 550 600 650
Central corneal thickness ( µ m)
700
Figure 1 Differences between intraocular pressure measurements made with the Goldmann applanation tonometer by observer 1 and those made with the Canon TX-10 non-contact tonometer plotted against central corneal thickness.
OBF/NCT differences were also significantly related to IOP and CCT; the equation was:
OBF/NCT difference = ( 2 0.218
6 IOP) + ( 2 0.018
6 CCT) +
6.7 (adjusted R
2
= 0.12; p = 0.0003 for the IOP coefficient and p = 0.03 for the CCT coefficient)
GAT/tonometer differences for other pairs of instruments were not related to CCT.
CCT and IOP measured by each tonometer were unrelated to subject age. However, GAT/Tono-Pen (fig 2) and OBF/
Tono-Pen differences were significantly related to subject age; the equations were:
R
2
GAT/Tono-Pen difference = (0.05
6 age) 2 2.70 (adjusted
= 0.04; p = 0.035)
R
2
OBF/Tono-Pen difference = (0.06
6 age) 2 3.51 (adjusted
= 0.04; p = 0.045)
DISCUSSION
Several studies have examined the relation between IOP measured by various tonometers and CCT (table 2). The findings from an early study, in which eyes were cannulated and true IOP was measured with a manometer, showed an average tonometric (Perkins or Draeger) error of
¡ 0.7 mm Hg per 10 m m deviation of CCT from the normal thickness of 520 m m.
1 A lower average correction of 0.18–
0.23 mm Hg per 10 m m was observed by Whitacre et al in a similar in vivo study in 15 eyes with normal corneas.
2 This latter finding is close to that found in the present study.
However, an association between applanation tonometry error (the difference between Tono-Pen or Perkins tonometer and manometric IOP) and CCT was not found by Feltgen et al 16 or Foster et al .
17
In general, there is good agreement between clinic based and population based studies of an increase in GAT measured
IOP as CCT increases (table 2). The slope estimates in clinic based studies are slightly steeper than those in population based studies. This may result from a bias introduced by referral patterns, where tonometry is almost universally performed for glaucoma case finding.
NCT was significantly more susceptible to the effects of
CCT than GAT, in accordance with previous findings.
18–20 The slope of the relation GAT/NCT difference versus CCT was
10
5
0
–5
–10
–15
20 30 40 50 60
Age (years)
70 80 90
Figure 2 Differences between intraocular pressure measurements made with the Goldmann applanation tonometer by observer 1 and those made with the Tono-Pen plotted against subject age.
www.bjophthalmol.com
Central corneal thickness, age, and IOP 853
Table 2 Increase in IOP (mm Hg) for every 10 m m increase in CCT. Summary of previous findings regarding effect of CCT on
IOP measurements
Author
This study
Ko et al , 2004 6
Siganos et al , 2004 36
Bhan et al , 2002 5
Gunvant et al , 2004 21
Morgan et al , 2003 12
Shimmyo et al , 2003 22
Eysteinsson et al , 2002 23
Dohadwala et al , 1998 4
Foster et al , 2003 24
Study type
Clinic based
Clinic based
Clinic based
Clinic based
Clinic based
Clinic based
Clinic based
Population based
Population based
Population based
Country
United Kingdom
Taiwan
Greece
United Kingdom
United Kingdom
United Kingdom
United States
Iceland
Indian subcontinent
Singapore
GAT
0.28
0.37
0.26
0.23
0.27
0.16
Tono-Pen
0.31
0.10
0.29 (M)
0.12 (F)
OBF
0.38
0.47
0.28
0.48
0.30
NCT
0.46
0.63
0.39
0.22 (M)
0.28 (F)
Foster et al , 1998 25
Wolfs et al , 1997 38
Nemesure et al , 2003 39
Feltgen et al , 2001 16
Foster et al , 2000 17
Ehlers, 1975 1
Population based
Population based
Population based
Manometry
Manometry
Manometry
Mongolia
Netherlands
Barbados
Germany
Singapore
Denmark
0.15 (R)
0.18 (L)
0.18 (R)
0.24 (L)
0.19
none none none
0.71
M, male; R, right eye; F, female; L, left eye.
about 2 0.2 mm Hg per 10 m m, compared to 2 0.37 mm Hg per 10 m m reported by Graf.
18 In clinic and population studies, CCT explains between 1% and 6% of the variance in GAT measured IOP and 7% to 12% of the variance in NCT measured IOP.
21–25 A possible explanation of the greater effect of CCT on NCT measured IOP lies in the viscoelastic property of the cornea, 26 in which stiffness is related to the rate of application of strain. The cornea is deformed over about
8 ms, resulting in relatively greater stiffness than under the conditions of GAT, where IOP measurement is effectively static. Other possible explanations include the relative effects of ocular expansion in the rapid and slow applanation conditions and the effect of pressure waves reflected back and forth through the eye with rapid applanation. A new
NCT, the ocular response analyser (ORA; Reichert Inc,
Depew, NY, USA), exploits the viscoelastic properties of the cornea. The ORA measures two applanation events, one as the pressure in the air jet rises and one as it falls. There is a difference in pressure for the inward and outward applanation events—a property called hysteresis. Preliminary data suggest that the hysteresis value correlates well with CCT.
27
We observed an overestimation of IOP by NCT relative to
GAT and OBF at higher IOP levels. Possible explanations include a non-linear increase in corneal stiffness as IOP rises and corneal viscoelastic properties that are not accounted for by CCT. A small tonographic effect was seen with one of the
GAT observers and with the OBF, so there may be a contribution from the effect of reduced aqueous outflow facility on measured IOP differences, the effect being greater on tonometry with very rapid flattening of the cornea.
The finding in this study of an increase in IOP measured by the Tono-Pen of 0.31 mm Hg per 10 m m increase in CCT is greater than previously reported figures of 0.19 mm Hg/
10 m m 4 and 0.10 mm Hg/10 m m 5 (table 2), although the confidence intervals for the estimate are wide (table 1). It is thought that the Tono-Pen may be less affected by CCT than the GAT because it applanates a smaller area of the cornea.
7 10
Walker and Litovitz 28 proposed that IOP measurements by pneumotonometry would be little affected by CCT as flexural rigidity could be ignored, because the outer edges of the probe flatten the cornea and the tension forces, by which IOP is measured, occur under the central portion of the probe.
However, this and other studies have reported a dependence of OBF measured IOP on CCT.
5 12 21 29 An explanation is provided by Morgan et al.
12 A portion of the air flow of the pneumotonometer holds the probe against the cornea to provide the initial corneal flattening and is susceptible to the effects of the CCT.
The results of a re-analysis of published data demonstrated that a 10% difference in CCT results in a difference of 1.1 (SD
0.6) mm Hg in IOP measurements, 30 equivalent to a change of
0.20 mm Hg for every 10 m m change in CCT. This result is supported by more recent findings (table 2). The validity of this relation is based on the assumption of a linear dependence of measured IOP on CCT, and on the absence of a relation between true IOP and CCT. Ehlers et al found a significant (p , 0.001) correlation between the error of GAT
IOP readings and CCT. However, the relation was non-linear, and IOP measurements required correction for CCT in relation to true IOP.
1 The latter findings were confirmed by
Orssengo and Pye, who demonstrated that the modulus of elasticity of the cornea was related to true IOP.
7
Opinion is divided about the clinical significance of the effect of CCT on IOP measurements. Singh et al suggested that the effect was small and probably not relevant for most patients.
29 Conversely, a recent report suggested that a correction for corneal effects might be needed for some groups of patients.
5 In a literature review, Doughty and
Zaman reported a mean CCT of 544 (SD 34) m m for measurements made by ultrasound pachymetry.
30 From this,
95% of corneas should have a CCT in the range 477–611 m m.
If a value of 0.20 mm Hg IOP increase per 10 m m increase in
CCT is assumed, 30 then the CCT could account for a difference in measured IOP of 2.7 mm Hg between the thickest and the thinnest corneas. One in 20 eyes will fall outside these extremes. Although this difference may be quite small in relation to the GAT measurement error, the distribution of
CCT values in clinic populations is unlikely to reflect that of the general population. Falsely high IOP readings made
(especially by NCT) in the community will lead to a concentration of thicker corneas in clinic populations. Thus,
CCT measurement is useful to identify normal eyes falsely classified as ocular hypertensive. Similarly, the classification of eyes on the basis of IOP as normal or high tension glaucoma inevitably leads to a relatively greater proportion of eyes with thin corneas in the normal tension group.
The cornea is thought to stiffen with age 13 as a result of ultrastructural changes in the collagen fibrils of the corneal stroma.
14 15 The finding of a significant relation between GAT/ www.bjophthalmol.com
854 Tonnu, Ho, Newson, et al
Tono-Pen (fig 2) and OBF/Tonopen differences and subject age, with GAT and OBF overestimating IOP relative to the
Tono-Pen in older subjects, may be explained by a stiffer cornea in older subjects, if Tono-Pen IOP measurements are less dependent on the biomechanical properties of the cornea.
An effect of a reduced tear film may contribute. Eisenberg et al 31 measured IOP by manometry, Perkins tonometry, pneumotonometry, and the Tono-Pen in nine subjects aged from 0.1 to 85 years. There was a significant effect of subject age on Perkins IOP measurement error, but not on the measurement error of the Tono-Pen and pneumotonometry.
The Perkins overestimated the Tono-Pen at older ages. The magnitude of the effect in present study was a relative increase in measured IOP (by GAT or OBF over the Tono-Pen) of about 0.5 mm Hg per decade, or 3.2 mm Hg across the age range of subjects in the study.
The effect of corneal biomechanics on IOP measurement is a research area that is gaining importance, given the increasing prevalence of individuals having undergone corneal refractive surgery. Stromal thinning following refractive procedures has been demonstrated to result in changes in IOP measured by the
GAT, NCT, and Tono-Pen.
32–34 A new method of tonometry, the
Pascal dynamic contour tonometer (DCT; Ziemer Ophthalmic
Systems AG, Port Switzerland), is said not to be affected by corneal biomechanical properties. The applanation tip has a concave surface (radius of curvature 10.5 mm) with an embedded pressure sensor and, when contour matching between the tonometer tip and the cornea is achieved, the mechanical properties of the cornea do not contribute to the
IOP measurement. Two studies have reported that DCT measured IOP is independent of CCT 35 36 and studies on patients undergoing laser corneal refractive surgery have demonstrated that, unlike GAT IOP measurements, Pascal
IOP measurements are unaltered by the laser surgery.
36 37
In conclusion, the findings of the present study demonstrate that IOP measurements by the GAT, Tono-Pen, OBF, and NCT are all significantly influenced by CCT, and that the effect of CCT on NCT is significantly greater than on the GAT.
ACKNOWLEDGEMENTS
The authors thank Haag-Streit UK for providing the Canon TX-10 non-contact tonometer and the reviewer, Dr Gunvant, for the suggestion to explore tonometer measurement differences with respect to subject age.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
P-A Tonnu, T Ho, K Sharma, E White, D Garway-Heath, Glaucoma
Research Unit, Moorfields Eye Hospital, London EC1V 2PD, UK
T Newson, A E Sheikh, Division of Civil Engineering, Faculty of
Engineering, University of Dundee, Dundee DD1 4HN, UK
C Bunce, Department of Research and Development, Moorfields Eye
Hospital, London EC1V 2PD, UK
REFERENCES
1 Ehlers N , Bramsen T, Sperling S. Applanation tonometry and central corneal thickness.
Acta Ophthalmol 1975; 53 :34.
2 Whitacre MM , Stein RA, Hassanein K. The effect of corneal thickness on applanation tonometry.
Am J Ophthalmol 1993; 115 :592–6.
3 Gordon MO , Beiser JA, Brandt JD, et al.
The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma.
Arch Ophthalmol 2002; 120 :714–20.
4 Dohadwala AA , Munger R, Damji KF. Positive correlation between Tono-Pen intraocular pressure and central corneal thickness.
Ophthalmology
1998; 105 :1849–54.
5 Bhan A , Browning AC, Shah S, et al.
Effect of corneal thickness on intraocular pressure measurements with the pneumotonometer, Goldmann applanation tonometer, and Tono-Pen.
Invest Ophthalmol Vis Sci
2002; 43 :1389–92.
6 Ko YC , Liu CL, Hsu WM. Varying Effects of corneal thickness on intraocular pressure measurements with different tonometers.
Eye 2004; 16 :16.
7 Orssengo GJ , Pye DC. Determination of the true intraocular pressure and modulus of elasticity of the human cornea in vivo . Bull Math Biol
1999; 61 :551–72.
8 Gloster J , Perkins ES. The validity of the Imbert-Flick law as applied to applanation tonometry.
Exp Eye Res 1963; 44 :274–83.
9 Mackay RS , Marg E, Oechsli R. Automatic tonometer with exact theory: various biological applications.
Science 1960; 131 :1668–9.
10 Mok KH , Wong CS, Lee VW. Tono-Pen tonometer and corneal thickness.
Eye
1999; 13 :35–7.
11 Silver DM , Farrell RA. Validity of pulsatile ocular blood flow measurements.
Surv Ophthalmol 1994; 38 :S72–80.
12 Morgan AJ , Harper J, Hosking SL, et al.
The effect of corneal thickness and corneal curvature on pneumatonometer measurements.
Curr Eye Res
2002; 25 :107–12.
13 Friedenwald JS . Contribution to the theory and practice of tonometry.
Am J Ophthalmol 1937; 20 :985.
14 Malik NS , Moss SJ, Ahmed N, et al.
Ageing of the human corneal stroma: structural and biochemical changes.
Biochim Biophys Acta 1992; 1138 :222–8.
15 Daxer A , Misof K, Grabner B, et al.
Collagen fibrils in the human corneal stroma: structure and aging.
Invest Ophthalmol Vis Sci 1998; 39 :644–8.
16 Feltgen N , Leifert D, Funk J. Correlation between central corneal thickness, applanation tonometry, and direct intracameral IOP readings.
Br J Ophthalmol
2001; 85 :85–7.
17 Foster PJ , Wong JS, Wong E, et al.
Accuracy of clinical estimates of intraocular pressure in Chinese eyes.
Ophthalmology 2000; 107 :1816–21.
18 Graf M . [Significance of the corneal thickness in non-contact tonometry].
Klin
Monatsbl Augenheilkd 1991; 199 :183–6.
19 Matsumoto T , Makino H, Uozato H, et al.
The influence of corneal thickness and curvature on the difference between intraocular pressure measurements obtained with a non-contact tonometer and those with a Goldmann applanation tonometer.
Jpn J Ophthalmol 2000; 44 :691.
20 Recep OF , Hasiripi H, Cagil N, et al.
Relation between corneal thickness and intraocular pressure measurement by noncontact and applanation tonometry.
J Cataract Refract Surg 2001; 27 :1787–91.
21 Gunvant P , Baskaran M, Vijaya L, et al.
Effect of corneal parameters on measurements using the pulsatile ocular blood flow tonograph and Goldmann applanation tonometer.
Br J Ophthalmol 2004; 88 :518–22.
22 Shimmyo M , Ross AJ, Moy A, et al.
Intraocular pressure, Goldmann applanation tension, corneal thickness, and corneal curvature in Caucasians, Asians,
Hispanics, and African Americans.
Am J Ophthalmol 2003; 136 :603–13.
23 Eysteinsson T , Jonasson F, Sasaki H, et al.
Central corneal thickness, radius of the corneal curvature and intraocular pressure in normal subjects using noncontact techniques: Reykjavik Eye Study.
Acta Ophthalmol Scand
2002; 80 :11–5.
24 Foster PJ , Machin D, Wong TY, et al.
Determinants of intraocular pressure and its association with glaucomatous optic neuropathy in Chinese Singaporeans: the Tanjong Pagar Study.
Invest Ophthalmol Vis Sci 2003; 44 :3885–91.
25 Foster PJ , Baasanhu J, Alsbirk PH, et al.
Central corneal thickness and intraocular pressure in a Mongolian population.
Ophthalmology 1998; 105 :969–73.
26 Hjortdal JO , Jensen PK. In vitro measurement of corneal strain, thickness, and curvature using digital image processing.
Acta Ophthalmol Scand
1995; 73 :5–11.
27 Kotecha A , Shewry JM, Garway-Heath DF. Corneal thickness independent
IOP measurements [abstract].
Invest Ophthalmol Vis Sci 2004; 45 : ARVO
Abstract 956.
28 Walker RE , Litovitz TL. An experimental and theoretical study of the pneumatic tonometer.
Exp Eye Res 1972; 13 :14–23.
29 Singh RP , Goldberg I, Graham SL, et al.
Central corneal thickness, tonometry, and ocular dimensions in glaucoma and ocular hypertension.
J Glaucoma
2001; 10 :206–10.
30 Doughty MJ , Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach.
Surv
Ophthalmol 2000; 44 :367–408.
31 Eisenberg DL , Sherman BG, McKeown CA, et al.
Tonometry in adults and children. A manometric evaluation of pneumatonometry, applanation, and
TonoPen in vitro and in vivo.
Ophthalmology 1998; 105 :1173–81.
32 Mardelli PG , Piebenga LW, Whitacre MM, et al.
The effect of excimer laser photorefractive keratectomy on intraocular pressure measurements using the
Goldmann applanation tonometer.
Ophthalmology 1997; 104 :945–8; discussion 949.
33 Chatterjee A , Shah S, Bessant DA, et al.
Reduction in intraocular pressure after excimer laser photorefractive keratectomy. Correlation with pretreatment myopia.
Ophthalmology 1997; 104 :355–9.
34 Garzozi HJ , Chung HS, Lang Y, et al.
Intraocular pressure and photorefractive keratectomy: a comparison of three different tonometers.
Cornea 2001; 20 :33–6.
35 Kaufmann C , Bachmann LM, Thiel MA. Comparison of dynamic contour tonometry with goldmann applanation tonometry.
Invest Ophthalmol Vis Sci
2004; 45 :3118–21.
36 Siganos DS , Papastergiou GI, Moedas C. Assessment of the Pascal dynamic contour tonometer in monitoring intraocular pressure in unoperated eyes and eyes after LASIK.
J Cataract Refract Surg 2004; 30 :746–51.
37 Kaufmann C , Bachmann LM, Thiel MA. Intraocular pressure measurements using dynamic contour tonometry after laser in situ keratomileusis.
Invest
Ophthalmol Vis Sci 2003; 44 :3790–4.
38 Wolfs RC , Klaver CC, Vingerling JR, et al.
Distribution of central corneal thickness and its association with intraocular pressure: the Rotterdam Study.
Am J Ophthalmol 1997; 123 :767–72.
39 Nemesure B , Wu SY, Hennis A, et al.
Corneal thickness and intraocular pressure in the Barbados eye studies.
Arch Ophthalmol 2003; 121 :240–4.
www.bjophthalmol.com
855
EXTENDED REPORT
Ahmed valve drainage implant surgery in the management of paediatric aphakic glaucoma
C Kirwan, M O’Keefe, B Lanigan, U Mahmood
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :855–858. doi: 10.1136/bjo.2004.056143
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Professor Michael O’Keefe,
The Children’s University
Hospital, Temple Street,
Dublin 1, Republic of
Ireland; mokeefe@ materprivate.ie
Accepted for publication
2 December 2004
. . . . . . . . . . . . . . . . . . . . . . .
Background: Paediatric aphakic glaucoma presents months or years after cataract surgery in children and is a major long term complication. The results of surgical treatment are poor and many children require multiple and repeat procedures with poor visual outcomes.
Methods: 13 children (19 eyes) had Ahmed valve implantation surgery, nine of the children had previous procedures such as cycloablation or trabeculectomy. Mitomycin was used at surgery in some patients and valve needling with Healon GV and 5-fluorouracil in some blebs after surgery. SF
6 gas was also used at the time of surgery in most children to reform the anterior chamber.
Results: 12 of the children (18 eyes) achieved intraocular pressure control of 15 mm Hg or less with a valve alone or with additional medical therapy.
Conclusion: Ahmed valve implantation surgery alone or in combination with medical therapy is successful and safe in the management of paediatric aphakic glaucoma.
A phakic glaucoma is a major long term complication following congenital cataract surgery.
1–3 younger age at surgery.
4
It presents months or years after surgery and is associated with
Micro cornea and secondary membrane surgery may also play a part.
The reported frequency has ranged from 1–35%.
5 6 The variation among studies relates to difference in duration of follow up, and inclusion or exclusion of other ocular abnormalities.
The aim of this study is to record the success, complications, and visual outcome using Ahmed valve implants, and the longer term follow up.
PATIENTS AND METHODS
We conducted a retrospective chart review of all patients who underwent Ahmed valve surgery for paediatric aphakic glaucoma between 1996 and 2003. All the patients included in this study attend for regular follow up visits in our clinic.
Diagnosis of glaucoma was mainly based on changes in the optic discs and intraocular pressure. All of the surgeries were preformed by one surgeon (MO’K). Indications for valve insertion included intraocular pressure not controlled by medical therapy or other forms of surgery—namely, cycloablation and or trabeculectomy. The Ahmed valve used was model S2 from New World Medical (Rancho Cucamonga, CA,
USA).
Surgical technique involved a fornix based conjunctival flap in the superior temporal or nasal quadrant. The sclera was exposed. In 10 eyes 0.5 mg/ml mitomycin C was applied to the sclera for 3 minutes and onto the valve itself. The tube was primed using balanced salt solution. The plate was secured to the sclera with its anterior edge 6 mm posterior to the limbus using 7.0 Prolene sutures. A sclera tunnel was created starting approximately 2 mm from the limbus and, using a 23 gauge or 25 gauge needle the tunnel was advanced into the anterior chamber of the eye. The tube was trimmed bevel up and inserted through the tunnel into the anterior chamber aiming towards the centre of the pupil.
The tube was not ligated. A donor scleral patch was placed over the sclera tunnel to cover the tube. This was sutured to the sclera with 9/0 nylon sutures. The conjunctiva was reapposed using 6/0 Vicryl sutures. In most patients, a volume of 0.5 ml of 20% SF
6
(sulphur hexafluoride gas) was injected into the anterior chamber through a long corneal tunnel to maintain anterior chamber depth and prevent hypotony.
Maxitrol ointment was applied to the eye and the eye was double padded for 24 hours.
RESULTS
There were 13 patients (seven males, six females) and a total of 19 eyes in the study. Nine eyes had surgical procedures carried out before valve insertion, three had cycloblation alone, one had trabeculectomy alone, and five had both. The follow up period was between 1996 and 2003 with three patients having a follow up of more than 6 years (table 1).
There was a mean reduction in intraocular pressure of
18 mm Hg (range 8–26 mm Hg). We choose a target postoperative intraocular pressure of 15 mm Hg as the goal in all patients. To attain this some patients required additional medical treatment in addition to the valve. This was either a single medication such as betaxolol or latanoprost or a combination of these and dorzolamide or timolol (table 2).
Complete success was achieved in six eyes from four patients with valve alone with an additional 12 eyes from eight patients requiring additional medical treatment in order to
Table 1 Patient demographics
Number of patients
Male:female
Number of eyes
Age at insertion of Ahmed valve (months)
Mean
Range
Reduction in IOP (mm Hg)
Mean
Range
Previous surgical procedures
Trabeculectomy alone
Cycloablation alone
Trabeculectomy + cycloablation
Length of follow up (months)
Mean
Range
13
7:6
19
96
9–189
3
5
9
1
17.9
8–26
32
3–84 www.bjophthalmol.com
856 Kirwan, O’Keefe, Lanigan, et al
Table 2 Time of surgery, age at surgery, intraocular pressure (IOP) measurements, pre-Ahmed valve insertion, 3 months and
6 months postoperatively, and pressure drop calculated from preoperative to latest postoperative recording
Patient
DP
SP
AMC
EG
CG
SK
HN
LK
HM
SF
GD
CG
CD
Date of surgery
14 Mar 01 2
15 Jan 03 + #
20 Jul 01 +
28 May 97 2 #
5 Nov 03 +
11 Oct 02 + #
27 Mar 02 + #
8 Apr 98 2 #
3 Nov 99 2 #
26 Jun 02 + #
24 Jul 02 2 #
17 Jun 98 2 #
27 Feb 02 2
18 Jun 03 +
17 Sep 03 +
8 Oct 03 +
7 Mar 01 2
11 Aug 99 2
7 Mar 01 2
Age at surgery
(months)
17
154
18
92
104
120
34
35
28
85
9
87
125
142
114
157
188
189
130
Preop IOP
(mm Hg)
34 *
28 *
28 *
36 *
29 *
26 *
28 *
31 *
28 *
30 *
34 *
32 *
26 *
40 *
30 *
40 *
28 *
34 *
28 *
IOP 3 months postop (mm Hg)
21
12
14
10
16 *
14 *
6 *
7 *
18 *
12 *
4
12
19 *
23 *
12 *
8
14 *
14 *
16 *
IOP 6 months postop (mm Hg)
24 *
15 *
6 *
5
12
16 *
14 *
16 *
10
14 *
14 *
11
15 *
16 *
NA
NA valve removed
20 *
17 *
Latest IOP
(months postop)
15 * (35 months)
15 * (13 months)
8 (31 months)
12 (84 months)
12 (6 months)
18 * (45 months)
18 * (28 months)
16 * (71 months)
14 * (52 months)
14 * (21 months)
12 * (20 months)
10 (70 months)
13 * (28 months)
14 * (12 months)
6 * (3 months)
7 * (4 months)
NA
16 * (52 months)
14 * (15 months)
Pressure drop
(pre-latest postop)
19
13
20
26
16
12
22
24
NA
14
14
20
14
22
22
20
8
22
14
+ , with mitomycin C; 2 , without mitomycin C; # , previous trabeculectomy/cycloablation; * medical treatment, NA, not available.
achieve desired control. Only one eye was considered a failure. Mitomycin was used at surgery in 10 eyes. There was no postoperative difference in intraocular pressure measurement or complications in patients with or without mitomycin. Repeat needling of the valve using a 23 gauge needle,
Healon GV, and 5-fluorouracil was carried out in 12 eyes in the first 6 months when the intraocular pressure increased.
Healon GV was injected under the conjunctival bleb over the valve plate to free any adhesions. Fluorouracil, 5 mg/0.2 ml, was then injected into the Healon over the plate to create longer term inhibition of fibroproliferative activity. In three eyes the procedure was repeated 3 years or more after surgery. We noted a successful outcome from needling if there was an immediate drop in intraocular pressure. The visual outcome varied but was poor and seven of the eyes have visions of 6/60 or less. There was no loss of vision from this surgery (table 3).
Complications occurred in five patients (table 4). They included hypotony and choroidal detachment in two eyes of two patients. There was corneal touch in two eyes of two patients. The valve was removed in two further patients one for persistent ocular pain in a second eye. However, 3 months later a valve was re-inserted because of the recurrence of glaucoma and no further pain was experienced. The patient continues to have a successful outcome. The other, a child
Table 3 Visual outcome
Patient
CG
SK
HN
LK
DP
SP
AMC
EG
HM
SF
GD
CD
CG
Visual acuity
Right eye
6/24 *
6/36
6/24 *
6/24 *
6/36 *
6/60 *
6/36 *
6/6
3/60 *
6/9 *
6/60 *
6/60
CF *
Left eye
6/24
2/60 *
6/24
6/24 *
HM *
6/24 *
6/12 *
CF *
6/18 *
6/9 *
6/60
6/9 *
6/12
HM, hand movement visual acuity; CF, counting finger visual acuity.
* Ahmed valve in situ.
with Lowe’s syndrome dislocated a tube because of persistent aggressive rubbing of the eye and we chose not to reinsert it.
This child has uncontrolled pressure on medical therapy and has a superficial corneal scar secondary to rubbing.
DISCUSSION
The high failure rate of trabeculectomy with or without antimetabolites in children with aphakic glaucoma has led to a search for an alternative.
7 The additional use of antimetabolite increases the longer term side effects.
8 The use of medical therapy is in most cases only an adjunctive treatment and ciliary body ablative procedures such as cyclodiode laser may only have a short term benefit.
9 The poor success rate and potential complications with many of the surgical procedures may result in a delay in treatment until the glaucoma is much more advanced before intervention occurs.
In 1968 Molteno introduced the first drainage implant to treat refractory glaucoma.
10 Over the past few decades, nonvalved implants such as Molteno, Baerveldt, and Schocket and valved implants such as Krupin, Ahmed, and Opti-Med, have been used in children. The Ahmed valve was first used in 1993. The aqueous flow is directed to the posterior plate and aqueous is absorbed by orbital capillaries and lymphatics.
11 We chose the Ahmed valve because of its reduced tendency for overfiltration. It is implanted in a single stage procedure and the intraocular pressure is reduced in the immediate postoperative period.
The use of glaucoma drainage implant devices has improved the outcome in neovascular glaucoma and in glaucoma following uveitis, aphakia, and post-penetrating keratoplasty.
10 11 To achieve this many of the eyes require additional medical therapy either with one or more medications. More recently the safety and efficacy of surgery using drainage implants compared with trabeculectomy for initial surgical management of primary open angle glaucoma has
Table 4 Complications
Complication Number of eyes
Choroidal detachment/hypotony 2
Corneal touch 2
Valve removal 2 www.bjophthalmol.com
Ahmed valve drainage implant surgery in children 857 been demonstrated.
12–14 The reduction in intraocular pressure and frequency of complications was comparable between the two groups. If one takes an intraocular pressure below
21 mm Hg, then the success in the literature ranges from about 45% to 90%. Coleman et al 15 reported an overall success rate of 78% and 61%. Englert reported a success rate of 91% and 58% during a 1 year and 2 year follow up et al 17
16 Djodeyre reported an overall success rate of 70% and 63% at
12 months and 24 months respectively. More recently Morad et al highlighted a decreased success rate of 71% and 46% after 36 and 48 months after surgery.
18 Donahoe et al showed a greater success rate with drainage implants for aphakic glaucoma in those who had only one previous surgery.
19 The other surgical techniques such as trabeculectomy with mitomycin are 59% and 67% at 12 and 24 months and cycloablation 66% and 44% at 6 months and 57 months.
20 21
In a comparison of aqueous shunt devices versus trabeculectomy with mitomycin for children under 2 years of age, aqueous shunt devices offered a better chance of successful glaucoma control in the first 2 years of life.
22
Our results compare favourably with these other studies.
What is more important is we have set a lower intraocular pressure as our goal. To achieve this many of the eyes require additional medical therapy either with one or more than one medication. The mean reduction in intraocular pressure of
18 mm Hg is similar to others.
15 16 A very important observation is that the intraocular pressure remains well controlled in three eyes with more than 6 years of follow up. The success rate is not poorer in patients who have had multiple surgeries, such as cycloblation or trabeculectomy, as illustrated in nine of our patients. The success of needle revision of failed and failing trabeculectomy blebs with adjunctive
5-fluorouracil has been recently highlighted.
23 We have found a similar technique useful in our patients where there is a reduction in the control of intraocular pressure. We have used this technique 3 years or more after the initial surgery with successful outcome. A useful indicator of successful response is the finding of a drop in intraocular pressure immediately after the needling of the valve with 23 gauge needle, Healon GV and the injection of 5-fluorouracil into the
Healon. This technique was first demonstrated to the authors by Peng Khaw (personal communication).
Most of the needlings were performed in the first 6 months after valve insertion, when the rise in intraocular pressure occurred. The initial hypertensive phase was reported by
Ayyala et al 24 and Kooris et al .
25 Histological examination described the emergence of a dense layer of fibrous tissue over the plate with a consequent rise in intraocular pressure.
The hypertensive phase may be transient in some patients.
It is also claimed that its presence early in the postoperative period may be associated with an unfavourable outcome and most of these eyes may need continuing medical therapy.
25
The hypertensive phase is thought to be more frequent with the Ahmed valve because of its reduced surface area. The fact that needling and 5-fluorouracil have a beneficial effect points to congestion, oedema, inflammation, and early fibrosis as the cause.
Mitomycin is now established as an essential agent for trabeculectomies in most forms of refractory glaucoma and in other high risk patients.
26 It carries potential side effects both long and short term, such as bleb leakage and infection. Our rationale in using it in some patients is to reduce Tenon cyst and bleb encapsulation over the valve. We found no difference in intraocular pressure control or complications using this agent; it is worth stating that this was not randomised and there were 13 patients. The valve was used in other types of glaucoma with mitomycin without increased complication rate. In the largest single trial on children with
Ahmed valve drainage implants complications occurred in
50% (30 of 60 eyes).
16 Hypotony with choroidal effusion was the commonest complication in 23%. Other complications such as tube exposure, endophthalmitis, and ocular motility problems were also noted. Postoperative hypotony is a major problem with all valve implants but is less common with the
Ahmed valve because of the unidirectional flow. The special valve mechanism is designed to prevent complications of overfiltration in the immediate postoperative period.
However, we have encountered hypotony in two eyes with choroidal detachment and one required anterior chamber reformation. We have used SF
6 gas for some patients at the time of surgery and it is our view that this reduces the risk of hypotony. It remains in the eye for 72 hours, giving enough time for aqueous production and the increase of intraocular pressure to a level sufficient to prevent hypotony. Two of our earlier patients had corneal touch, which is an avoidable surgical risk and is eliminated with improved surgical technique. Our more severe complication was valve displacement caused by excess rubbing, which resulted in valve failure. It is worth highlighting this as we think that this type of valve surgery may be contraindicated in some children.
Visual outcome in many of our patients is poor, with most children achieving 6/24 best visual acuity and seven eyes achieving vision of 6/60 or less. This is not the result of valve surgery itself. These children have amblyopia.
Aphakic glaucoma is usually asymptomatic and to detect this disease adequately many require regular examinations under anaesthesia. A further dilemma is in deciding one’s criteria for diagnosing glaucoma; in particular, does one make the diagnosis on intraocular pressure alone or optic disc changes. Treatment, particularly surgery, is difficult and tedious and understandably there is sometimes a delay in performing surgery.
The complications and longer term failure of valve implants have been major obstacles to their insertion in children. There is an initial learning curve. The intraocular pressure result is impressive and is lasting at least 5 years or more in patients with longer term follow up. We confirm the success of valve needling as a useful and safe technique, both early on after surgery and in the longer term. We also recommend the use of SF
6 gas at initial surgery to reduce hypotony and choroidal detachment as it is safe, effective, and easy to administer. The complications in this series were low. This in our view is a major positive feature of the Ahmed valve. The newer B1 double plated Ahmed valves with total plate surface area of 364 mm
2
, one valve plate body, and a non-valve plate may be more effective in lowering the intraocular pressure and reducing further the need for adjunctive medical therapy.
27
Finally, we acknowledge that this study is retrospective, with a small number of patients and there is the need for longer term follow up. To date, valves have been reserved for treatment of refractory glaucoma. We believe that there is now a good case for them to be considered as first choice in surgical management of paediatric aphakic glaucoma.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
C Kirwan, M O’Keefe, B Lanigan, U Mahmood, The Children’s
University Hospital, National Children’s Eye Centre, Temple Street,
Dublin, and University College Dublin, Republic of Ireland
REFERENCES
1 Phelps CD , Arafat NI. Open angle glaucoma following surgery for congenital cataracts.
Arch Ophthalmol 1977; 95 :1985–7.
2 Mills MD , Robb RM. Glaucoma following childhood cataract surgery.
J Pediatr
Ophthalmol Strabismus 1994; 31 :355–60.
3 Russell Eggitt I , Zamiri P. Review of aphakic glaucoma after surgery for congenital cataract.
J Cataract Refract Surg 1997; 23 :664–8.
4 Vishwarath M , Cheong Leen R, Taylor D, et al.
Is early surgery for congenital cataracts a risk for glaucoma ?
Br J Ophthalmol 2004; 88 :905–10.
www.bjophthalmol.com
858 Kirwan, O’Keefe, Lanigan, et al
5 Rabiah P . Frequency and predictors of glaucoma after pediatric cataract surgery.
Am J Ophthalmol 2004; 137 :30–7.
6 Simon JD , Mehta N, Simmons ST, et al.
Glaucoma after pediatric lensectomy/ vitrectomy.
Ophthalmology 1991; 98 :670–4.
7 Mandal AK , Bagga H, Nutteti R, et al.
Trabeculectomy with or without mitomycin C for pediatric glaucoma in aphakia and pseudophakia following congenital cataract surgery.
Eye 2003; 17 :53–62.
8 Wells AP , Cordeiro F, Bunie C, et al.
Cystic bleb formation and related complications in limbic versus formix based conjunctival flaps in paediatric and young adult trabeculectomy with mitomycin C.
Ophthalmology
2003; 110 :2192–7.
9 Phelan MJ , Higginbottam EJ. Contact transcleral Nd:Yag laser cyclophoria coagulation for refractory paediatric glaucoma.
Ophthalmic Surg Lasers
1995; 26 :401–3.
10 Molteno ACB . New implant for drainage in glaucoma: clinical trial.
Br J Ophthalmol 1979; 53 :606–15.
11 Rosenberg LF , Krupin T. Implants in glaucoma surgery. In: Peter R, Shields MB,
Krupin T, eds.
The glaucomas.
2nd ed. Philadelphia: Mosby,
1996:1783–807.
12 Heuer DK , Lloyd MA, Abrams DA. Which is better ?
A randomized clinical trial of single plate versus double plate Molteno implantation for glaucoma in aphakia and pseudophakia.
Ophthalmology 1992; 99 :1512–19.
13 Mills RP , Reynolds A, Edmond MJ. Long term survival of Molteno glaucoma drainage devices.
Ophthalmology 1996; 103 :299–305.
14 Wilson R , Mendis IL, Smith SD, et al.
Ahmed glaucoma valve implant vs trabeculectomy in the surgical treatment of glaucoma a randomized clinical trial.
Am J Ophthalmol 2000; 130 :267–73.
15 Coleman AL , Smyth RJ, Wilson MR, et al.
Initial clinical experience with the
Ahmed glaucoma valve implant in pediatric patients.
Arch Ophthalmol
1997; 115 :186–91.
16 Englert JA , Freedman SF, Cox TA. The Ahmed valve in refractory pediatric glaucoma.
Am J Ophthalmol 1999; 127 :34–42.
17 Djodeyre MR , Calvo JP, Gomez JA. Clinical evaluation and risk factors of time to failure of Ahmed glaucoma valve implant in pediatric patients.
Ophthalmology 2001; 108 :614–20.
18 Morad Y , Donaldson C, Fraco F, et al.
The Ahmed drainage implant in the treatment of pediatric glaucoma.
Am J Ophthalmol 2003; 135 :821–9.
19 Donahoe SP , Keech RV, Munden P, et al.
Baerveldt implant surgery in the treatment of advanced childhood glaucoma.
J AAPOS 1997; 1 :41–5.
20 Beck AD , Wilson WR, Lynch MG. Trabeculectomy with adjunctive mitomycin
C in pediatric glaucoma.
Am J Ophthalmol 1998; 126 :648–57.
21 Freedman SF , McCormick K, Cox TA. Mitomycin C—augmented trabeculectomy with postoperative modulation in pediatric glaucoma.
J AAPOS 1999; 3 :117–24.
22 Beck AD , Freedman S, Kammer J, et al.
Queous shunt devices compared with trabeculectomy with mitomycin-C for children in the first two years of life.
Am J Ophthalmol 2003; 136 :994–1000.
23 Broadway D , Bloom P, Bunee C, et al.
Needle revision of failing and failed trabeculectomy blebs with adjunctive 5 fluorouracil.
Ophthalmology
2004; 111 :665–73.
24 Ayyala RS , Zurakowski D, Smith JA, et al.
A clinical study of the Ahmed glaucoma valve implant in advanced glaucoma.
Ophthalmology
1998; 105 :1968–76.
25 Kouros Nouri-Mahdavi , Caprioli J. Evaluation of the hypertensive phase after insertion of the Ahmed glaucoma valve.
Am J Ophthalmol 2003; 136 :1001–8.
26 Katz GI , Higginbottam EJ, Lihter PR. Mitomycin C vs 5-fluorouracil in high risk glaucoma filtering surgery. Extended follow up.
Ophthalmology
1995; 102 :1263–9.
27 Miele DL , Herndon L, Leep. Early clinical experience with Ahmed glaucoma bilateral plate.
ARVO 2002:6.
www.bjophthalmol.com
859
EXTENDED REPORT
Outcomes in persistent hyperplastic primary vitreous
A Hunt, N Rowe, A Lam, F Martin
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :859–863. doi: 10.1136/bjo.2004.053595
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Dr Adrian Robert Hunt,
Sydney Eye Hospital, 8
Macquarie Street, Sydney,
Australia 2000; hunt_adrian@bigpond.
com
Accepted for publication
5 October 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aims: To report outcomes in cases of persistent hyperplastic primary vitreous (PHPV) and examine factors predictive of visual acuity in patients selected for surgery.
Methods: Retrospective case series of 55 eyes in 50 patients presenting between 1990 and 2001 at the
Children’s Hospital, Westmead. 33 eyes underwent surgery aimed at visual rehabilitation.
Results: In surgical patients, median age at surgery was 77 days, and median age at final follow up was
28 months. Six (18%) achieved a visual acuity at final follow up of 6/60 or better and eight (24%) achieved acuity of less than 6/60 to counting finger vision inclusive. Those undergoing surgery before
77 days were approximately 13 times more likely to obtain a visual acuity of counting fingers or better than those operated later (p = 0.01). Neither posterior segment PHPV nor post-surgical glaucoma was a significant predictor of outcome in this selected group.
Conclusion: Early surgery aimed at rehabilitation markedly improves the likelihood of useful visual outcome in selected eyes with PHPV.
P ersistent hyperplastic primary vitreous (PHPV) causes considerable visual morbidity in affected eyes. Previous surgical series have documented variable visual and anatomical outcomes even with highly selected cases.
1–13 Poor visual outcomes temper the decision to pursue surgery and ongoing visual rehabilitation.
We report on a series of 55 eyes diagnosed with PHPV managed surgically and conservatively over a 10 year period at the Children’s Hospital at Westmead, Sydney. Data were analysed to determine factors predictive of visual outcome in eyes receiving surgical intervention aimed at visual rehabilitation.
PATIENTS AND METHODS
The medical records of patients with PHPV diagnosed by consultant paediatric ophthalmologists between January
1990 and March 2001 were reviewed retrospectively. The ethics committee of the Children’s Hospital, Westmead, approved the research protocol. Departmental and hospital records were screened for potential PHPV, including cases coded as congenital cataract, microphthalmia, and congenital vitreous disorders. The inclusion criteria for this study involved documentation of typical anterior and/or posterior segment features of PHPV.
phthalmia, 16
1–3 12–15 These included microcataract, retrolental plaque, shallow anterior chamber, elongated ciliary processes, persistent hyaloid artery, retinal dysplasia, and retinal detachment. Diagnosis was made based on a combination of clinical, examination under general anaesthesia, and ultrasound findings. The difficult distinction between bilateral PHPV and Norrie disease was not defined by molecular genetic analysis.
17
Preoperative ancillary tests including B-scan ultrasound with
Doppler, computed tomography (CT), magnetic resonance imaging (MRI), and visual evoked potentials (VEP) were performed as directed by the treating ophthalmologist. Four surgeons performed or supervised all procedures.
In this study PHPV was categorised as anterior if a retrolental opacity, elongated ciliary processes, or cataract was present on clinical examination. PHPV was categorised as posterior when one or more of the following features was associated with an elevated vitreous membrane or stalk from the optic nerve: a retinal fold or retinal dysplasia, retinal detachment, or optic nerve hypoplasia.
Surgical interventions aimed at visual rehabilitation included lensectomy with or without anterior or total vitrectomy, and trabeculectomy. Cases with isolated anterior involvement or glaucoma were routinely selected for early surgery. Cases with minimal posterior involvement were selected upon the treating surgeon’s discretion. Occlusion therapy combined with aphakic correction (contact lens, or spectacle if bilateral) followed surgery.
Visual acuity was assessed with age appropriate tests including Kays picture tests, Teller cards, Sheridan-Gardner, and Snellen tests.
18 Age at surgery was calculated in days, and cases categorised into early and late surgery groups using the median value.
For patients receiving surgical intervention aimed at visual rehabilitation, final visual acuity was categorised into
‘‘useful’’ (counting finger vision or better) and ‘‘poor’’(worse than counting fingers). Associations between clinical factors
(age at surgery, sex, presence of posterior PHPV, and late glaucoma) and visual outcome were examined using 2 6 2 tables and logistic regression modelling. Statistical analyses were performed using SPSS, and significance defined as p , 0.05.
RESULTS
Fifty five eyes of 50 patients were included in the study, with 31
(62%) males and 19 (38%) females. Five (10%) of the patients were diagnosed with bilateral PHPV and were assigned a single case number; 25 right eyes (45%) and 30 left eyes (55%) were included. Median age at diagnosis was 44 days. Three quarters were diagnosed within 90 days. PHPV was an isolated abnormality in most of the patients (76%). Twelve patients had systemic abnormalities, seven of which were neurological and one case of Walker-Warburg syndrome (table 1). Fifteen eyes (27%) had anterior segment involvement only. Thirty three (60%) eyes had combined involvement. Seven (13%) had purely posterior involvement, including hyaloid remnants (two eyes) with disc atrophy (one eye), large retrolental/central vitreous masses (five eyes) with vitreous haemorrhage (one eye), and retinal detachment (three eyes). Five (71%) of the
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; PFV, persistent fetal vasculature; PHPV, persistent hyperplastic primary vitreous; VEP, visual evoked potentials www.bjophthalmol.com
860 Hunt, Rowe, Lam, et al
Table 1 Additional diagnoses in 12 patients
Case No
18
21
32
38
41
45
48
23
24
28
30
50
Condition
Bilateral deafness, behavioural abnormalities
Ipsilateral retinopathy of prematurity
Ipsilateral facial asymmetry
Tracheomalacia, polymicrogyria with seizures
Walker-Warburg syndrome, hydrocephaly, polycythaemia
Patent ductus arteriosus
Microcephaly
Developmental delay, syndactyly, ear/nose abnormalities
Microcephaly
Ipsilateral hemifacial dysmorphism
Ipsilateral hypoplasia of right optic nerve, chiasm, carotid artery and cerebrum
Bilateral deafness eyes with pure posterior PHPV had neurological abnormalities listed in table 1.
Early surgical intervention aimed at visual rehabilitation
Thirty three (60%) eyes underwent early surgery directed at visual rehabilitation (table 2). Median age at diagnosis was
40 days. Median age at surgery was 77 days, and one quarter underwent surgery in the first month of life. Median age at final follow up was 28 months.
Signs of incipient or actual angle closure glaucoma complicated the clinical course in seven (23%) eyes of this group. Two eyes in one patient underwent initial trabeculectomy because of congenital glaucoma with cloudy corneas.
Subsequent visualisation of the extent of bilateral disease in this patient combined with significant co-morbidities led the clinician to pursue a more conservative approach. Five eyes were complicated by glaucoma after lensectomy. Late trabeculectomy was performed on two eyes (final VA: 1/24,
NLP), medical management undertaken in two eyes (1/60,
NLP), and photocycloablation performed in one eye (NLP).
Strabismus was documented in 22 (67%) patients and six of these underwent eye muscle surgery. Retinal detachment was documented in three (9%) eyes and phthisis documented in another four (12%) eyes in this group.
Subsequent interventions in this group included pupilloplasty in two eyes, YAG laser capsulotomy (one eye), surgical capsulotomy (one eye), and secondary intraocular lens implantation (two eyes). Two eyes were enucleated and three eyes had socket moulding for fitting of prostheses.
Visual acuity data were available for 31 eyes (94%) in this group at final follow up. Six (18%) achieved a visual acuity at final follow up of 6/60 or better. Eight (24%) achieved acuity of less than 6/60 to counting finger vision inclusive. Seven
(21%) had hand movement to light perception vision inclusive, and 11 (33%) had no light perception or had undergone enucleation.
Cases 21, 24, and 28 were excluded from statistical analysis, as visual outcome may have been affected by ocular or neurological conditions in addition to PHPV. There was no significant correlation between ‘‘useful’’ vision (defined as counting fingers at 1 metre or better acuity) at final follow up, and sex, eye, location of PHPV, or post-surgical glaucoma in regression analyses. After adjustment for post-surgical glaucoma and posterior segment PHPV, surgery before 77 days of age was found to strongly predict ‘‘useful’’ vision (OR
13.0, p = 0.01).
Conservative management
Twenty two eyes were managed without early surgical intervention aimed at visual rehabilitation (table 3).
Median age at diagnosis was 55 days. Median age at final follow up was 13 months.
Retinal detachment was documented in six (28%) eyes in this group. Angle closure glaucoma was documented in one eye. Strabismus was documented in six (28%) patients in this group. Strabismus surgery was performed in one patient in this group. Moulding for prosthesis fitting was performed on three eyes. Probing was performed for nasolacrimal duct obstruction for one patient.
Final visual acuity was available for 20 of these patients.
One (4%) achieved a visual acuity at final follow up of 6/48 or better. One (4%) achieved acuity of 6/60 to counting finger vision inclusive. Six (28%) had hand movement to light perception vision inclusive. Ten (45%) had no light perception and one had undergone enucleation as a primary procedure.
DISCUSSION
Persistent hyperplastic primary vitreous was first described by Reese in 1955 in his Jackson Memorial Lecture.
14
Representing a form of persistent fetal vasculature (PFV),
Goldberg has suggested the terminology change to better reflect the pathology.
1 18 The exact aetiology remains unknown. Characteristically PHPV presents as unilateral leucocoria with variably severe microcornea or microphthalmia.
1 3 PHPV is usually found in otherwise healthy full term infants, however, it has been described in association with systemic and, in particular, neurological abnormalities.
19
Severity can range from pupillary strands or an isolated
Mittendorf dot, to more severe forms with retrolenticular membranes, retinal dysplasia, or detachment.
1 3 15 18 20 21
PHPV management is based on the extent of anterior and posterior segment involvement. Posterior PHPV has been associated with a poor visual outcome in previous studies.
1–13
Including all patients in our study, the absence of posterior involvement predicted counting finger or better vision but this failed to reach statistical significance (OR 1.6, p = 0.44).
For patients receiving visual rehabilitation surgery, presence of posterior segment involvement was found not to be associated with visual acuity at final follow up (p = 0.46).
This failure to achieve statistical significance may be due to small patient numbers, short follow up time, and/or a selection for surgery of patients with only minimal posterior segment disease.
Pollard stated that age at presentation is a major predictor of visual outcome.
3 Karr and Scott found surgical patients achieving 20/200 or better acuity presented at a mean age of
2.4 months, whereas those that achieved 20/300 or worse presented at a mean age of 4.3 months.
5 Our study showed surgery before 77 days was associated with useful vision (OR
13, p = 0.01). This provides a useful prognostic factor in case selection that concurs with previous anecdotal reports.
Comparing results with Karr and Scott’s series, eyes achieving 6/60 or better in our study had mean age at surgery of 41 days (1.3 months), excluding one patient operated at age 15 months who achieved 6/48. Mean age at surgery for patients achieving worse than 6/60 was 121 days
(4.0 months).
Other factors examined in the statistical analysis (sex, laterality, and late glaucoma) were found not to be significantly associated with visual outcomes, although a possible trend for poor final acuity in males was found after multivariate adjustment (odds ratio 0.08, p = 0.09)).
However, the limited size of our series means all calculated associations are unstable to small changes in frequencies in any category of predictor or outcome factor. These low frequencies are also reflected in the large confidence intervals obtained for significant associations. The authors also recognise other factors such as compliance with occlusion www.bjophthalmol.com
Outcomes in PHPV 861
Table 2 Surgical rehabilitation patient data
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
22
23
24
1
2
Case
No Sex Eye
Age at diagnosis
(months)
M RE 2
F LE 2
18
19
20
21
25
26
27
28R
28L
M RE 3
M RE 1
M LE 0
F RE 0
F
M
M
RE 0
LE 1
RE 14
F LE 2
F RE 10
M
M
M
M
F
F
M
M
F
M
F
M
M
M
F
M
F
F
LE 2
LE 4
LE 1
RE 0
LE 4
LE 2
LE 0
RE 1
LE 7
LE 2
LE 4
RE 1
RE 0
LE 0
RE 3
LE 0
RE 0
LE 0
29L F LE 1
29R F RE 1
30R F RE 2
Best preoperative visual acuity
Vague LP
Vague LP
Poorly F&F
Vague LP
NA
Poorly F&F
NA
NA
Poorly F&F
NA
Poorly F&F
No F&F
No F&F
Poorly F&F
Poorly F&F
6/480 Teller
NA
Poorly F&F
NA
Poorly F&F
NA
NA
NA
NA
6/240 Teller
NA
NA
NA
NA
Poorly F&F
Poorly F&F
NA
PHPV type
A
A/P
A/P
A/P
A
A
A/P
A/P
A/P
A/P
A/P
A/P
A/P
A/P
A
A/P
A
A
A
A/P
A/P
A/P
A/P
A
A/P
A
A/P
A/P
A/P
A/P
A/P
A/P
Indications for surgery
C RP
C RP
C
C G
C RP
C RP
C RP
C RP
C RP
C
C RP
C RP
C RP AC
C
C RP
C RP
C
C RP
C RP
C
C
C RP
C RP AC
C
C
C RP
C
G
G
C RP
C RP
C RP
L/V
L/V
L/V
L
L/V
L/V
L/V
L
L/V
L/V
L
Surgery
Age at surgery
(months)
L/V
L/V
4
3
L
L
L/V
L/V
9
13
0
1
Sequelae and clinical course
Indrawing of ciliary processes, LXT small
Post-PHPV noted postoperatively, RET
Glaucoma, trab, RD
L/V
L/V
L
L
L/V
L/V
L
L
L/V
L
Trab.
Trab.
L/V
L/V
L/V
1
1
15
2
10
2
4
2
2
5
2
4
1
6
6
4
1
1
10
5
1
NA
NA
1
1
4
RXT variable, CL compliance poor
Pupil closure, pupilloplasty, RET
RD, CL compliance poor
CL compliance poor, secondary IOL
RET
Pupil closure, pupilloplasty, RET
Phthisis
Glaucoma, phthisis
LET small
RXT
LET, squint surgery
LXT, CL compliance poor, secondary IOL
LXT, enucleation
YAG laser capsulotomy
LET, CL compliance poor
LET, squint surgery, threshold ROP, cryotherapy, glaucoma
LET variable
Glaucoma, photocycloablation
RET, squint surgery, capsulotomy
RET, RD
RHT/XT, squint surgery
Dead (PUO) at age
14 months
Presented with glaucoma
Presented with glaucoma
AET, squint surgery
AET, squint surgery, glaucoma, trab age
4
RD, phthisis, enucleation
L 2
Age at final follow up
(months)
30
14
8
16
42
43
12
116
25
107
42
23
22
32
1
95
54
20
22
123
17
1
28
13
44
104
8
8
8
52
52
80
Visual acuity at final follow up
F&F
Vague LP
Poorly fixes
NLP
3/18 Kays
1/60 SGSL
6/570Teller
LP
6/48 Teller
6/48 Snellen
LP
Prosthesis
NLP
6/36 Teller
F&F
3/36 Snellen
3/36 Kays
NLP
6/36 Teller
LP
1.5/60 Teller
NA
NLP
NLP
NLP
NA
6/120 Teller
NLP
NLP
1/18 SGSL
1/24 SGSL
NLP
31L F LE 1 LP A C 63 3/24 SGSL
LP, light perception; NLP, no light perception; F&F, fixing and following; A, anterior PHPV; P, posterior; C, cataract; RP, retrolental plaque; G, glaucoma; AC, shallow anterior chamber; Trab, trabeculectomy; L, lensectomy; V, vitrectomy; RET, right esotropia; LET, left esotropia; RXT, right exotropia; RHT, right hypertropia;
AET, alternating esotropia; RD, retinal detachment; ROP, retinopathy of prematurity; CL, contact lens; secondary IOL, secondary intraocular lens; SGSL, Sheridan-
Gardner single letters.
and correction of refractive errors may influence outcome, but precise measurement of all potential confounders was limited by the retrospective nature of the study. Caution must be exercised in interpreting results given treatment groups
(early versus late surgery) were not randomly allocated.
The difficult task of managing anisometropic amblyopia in neonatal aphakia is cited as a major factor contributing to poor visual outcome.
22 Anteby et al concluded that intraocular lens implantation may be a favourable and beneficial option for the management of children with unilateral PHPV in their series of 89 children.
23 Thirty of the 61 eyes in that study underwent cataract extraction/vitrectomy with intraocular lens implantation. High intraocular pressure and glaucomatous changes were observed less commonly with pseudophakia (8%) compared to aphakia (23%), and the incidence of NLP was 10% and 43% respectively. Our predominantly aphakic experience has been similar with a
23% incidence of glaucoma, and final VA of NLP in 32%. The two secondary pseudophakic cases in our series were not complicated by glaucoma and achieved 3/36 Kays and 6/48
Teller VA.
Surgical intervention has previously been recommended for globe preservation in PHPV complicated by progressive retinal detachment, angle closure glaucoma, and recurrent intraocular haemorrhage.
1–4 14 15 24 In the surgical group eight eyes were complicated by glaucoma or retinal detachment, and seven of these had no light perception at final follow up.
Four eyes underwent trabeculectomy with three having no www.bjophthalmol.com
862 Hunt, Rowe, Lam, et al
39
40
41
42
43
44
45
46
47
48
49
50
36
37
38
31R
32L
32R
33
34
35
Table 3 Conservative management patient data
Case Sex Eye
30L F LE
Age at diagnosis
(months)
2
Visual acuity at presentation
NLP
PHPV type
Contraindications to early surgery
A/P SA SP
M
M
M
M
M
M
F
M
M
M
M
M
M
F
F
F
M
M
F
F
M
1
0
3
3
0
4
NA
0
8
1
4
2
LE
LE
LE
LE
RE
LE
RE
LE
LE
RE
LE
RE
0
5
0
1
2
2
0
2
0
RE
LE
RE
RE
LE
RE
LE
RE
RE
NA
NA
LP
NA
Good F&F
NA
NA
Poorly F&F
NA
Roving
NA
Poorly F&F
LP
LP
Vague LP
NLP
Vague LP
NLP
NLP
Poorly F&F
NA
SP
SP
SP
SA
SA SP
SA SP
SP
SP
MP
SA
SA
SA SP
P
P
P
A
A/P
A/P
A
A/P
A
P
P
A/P
A
A/P
A/P
A
P
P
A/P
A/P
A/P
G SA SP
SP
SP
SA SP
SP
SA SP
SA
SP
SA SP
Miscellaneous
Corneal diameter 7 mm, patent hyaloid artery
Glaucoma at presentation, phthisis, prosthesis
Large retrolental mass, rsmicrocephaly
RD, microcephaly
Microphthalmos, prosthesis
Patent hyaloid artery to disc
Shallow anterior chamber, AP
14 mm
Shallow anterior chamber, late lensectomy for glaucoma
Patent hyaloid artery to disc, nystagmus
Ectopia lentis, retinal dysplasia,
L-ptosis and duct blockage requiring probing.
Corneal diameter 8 mm, AP rs14 mm
Corneal diameter 8 mm, AP rs13 mm
Hyaloid artery, hypoplastic disc, roving nystagmus, microcephaly
Progressive phthisis, enucleation
Hyaloid artery only, developmental delay
Shallow anterior chamber with pupil bound down
Prosthesis
Retrolental mass, AP 12 mm and left ptosis, roving nystagmus
Retrolental mass
Vitreous haemorrhage, RD
Hyaloid artery and retrolental mass,
Shallow anterior chamber, strabismus surgery
11
3
9
37
11
3
13
56
8
14
9
59
17
47
22
63
2
2
1
2
95
Age final follow up
(months)
80
NA
NLP
NLP
NLP
NLP
NLP
LP
NLP
6/18
NLP
NLP
LP
Visual acuity at final follow up
NLP
NLP
LP
Vague LP
NLP
Vague LP
NLP
NA
3/60
NLP
LP, light perception; NLP, no light perception; F&F, fixing and following; A, anterior PHPV; P, posterior; MP, minimal posterior PHPV; SP, severe posterior PHPV not amenable to surgery; SA, severe anterior PHPV not amenable to surgery; G, glaucoma; RD, retinal detachment; AP, globe anteroposterior diameter; MRI, magnetic resonance imaging.
light perception at final follow up; none of these eyes went on to develop phthisis or required enucleation.
Mild PHPV can run a relatively benign natural course without surgery.
1 25 Two patients in our series with an isolated hyaloid artery the only manifestation of PHPV achieved , 6/18 (Teller) at age 11 months and 3/60
(Sheridan-Gardner) at 4 years with conservative management. Surgery may be avoided if the visual axis is clear, anatomical anomalies are not progressive, and the anterior chamber angle is not compromised.
1 26
Optimal timing of surgery aimed at visual rehabilitation is presumably governed by the early critical periods of visual development.
27 28 The study findings support the value of early diagnosis and early intervention to maximise visual potential in selected patients.
ACKNOWLEDGEMENTS
We are grateful to the orthoptic staff at the Children’s Hospital,
Westmead, and also Professor Frank Billson, Dr Jeremy Smith, and
Dr Michael Giblin, for their contribution to this article through patient care and management.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
A Hunt, N Rowe, F Martin, Department of Ophthalmology, The
University of Sydney, New South Wales, Australia
A Lam, Department of Radiology, The Children’s Hospital, Westmead,
Sydney, Australia
REFERENCES
1 Goldberg MF . Persistent fetal vasculature (PFV): an integration of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). LIV
Edward Jackson Memorial Lecture.
Am J Ophthalmol 1997; 124 :587–626.
2 Pollard Z . Results of treatment of persistent hyperplastic primary vitreous.
Ophthalmic Surg 1991; 22 :48–52.
3 Pollard Z . Persistent hyperplastic primary vitreous: diagnosis, treatment and results.
Trans Am Ophthalmol Soc 1997; 95 :487–549.
4 Smith RE , Maumenee AE. Persistent hyperplastic primary vitreous: results of surgery.
Trans Am Acad Ophthalmol Otolaryngol 1974; 78 :911–25.
5 Karr DJ , Scott WE. Visual acuity results following treatment of persistent hyperplastic primary vitreous.
Arch Ophthalmol 1986; 104 :662–7.
6 Acers TE , Coston TO. Persistent hyperplastic primary vitreous. Early surgical management.
Am J Ophthalmol 1967; 64 :734–5.
7 Scott WE , Drummond GT, Keech RV, et al.
Management and visual acuity results of monocular congenital cataracts and persistent hyperplastic primary vitreous.
Aust N Z J Ophthalmol 1989; 17 :143–51.
8 Federman JL , Shields JA, Altman B, et al.
The surgical and non surgical management of persistent hyperplastic primary vitreous.
Ophthalmology
1982; 89 :20–4.
9 Alexandrakis G , Scott IU, Flynn HW, et al.
Visual acuity outcomes with and without surgery in patients with persistent fetal vasculature.
Ophthalmology
2000; 107 :1068–72.
10 Mittra RA , Huynh LT, Ruttum MS, et al.
Visual outcomes following lensectomy and vitrectomy for combined anterior and posterior persistent hyperplastic primary vitreous.
Arch Ophthalmol 1998; 116 :1190–4.
11 Reynolds JD . Visual acuity after treatment of persistent hyperplastic primary vitreous [letter].
Arch Ophthalmol 1986; 104 :1274–1277.
12 Dass AB , Trese MT. Persistent hyperplastic primary vitreous results.
Ophthalmology 1999; 106 :280–4.
13 Hadda R , Font RL, Reeser F. Persistent hyperplastic primary vitreous. A clinicopathologic study of 62 cases and review of the literature.
Surv
Ophthalmol 1978; 23 :123–34.
14 Reese AB . Persistent hyperplastic primary vitreous. Jackson Memorial Lecture.
Trans Am Acad Ophthalmol Otolaryngol 1955; 59 :271–86.
www.bjophthalmol.com
Outcomes in PHPV 863
15 Reese AB . Persistent hyperplastic primary vitreous.
Am J Ophthalmol
1955; 40 :317–31.
16 Grignolo A , Riviera A. Biometry of the human eye from the sixth month of pregnancy to the tenth year of life. In: Vanysek J, ed.
Diagnostica Ultrasonica in Ophthalmologia 1968:251–7.
17 Pendergast SD , Trese MT, Liu X, et al.
Study of the Norrie disease gene in 2 patients with bilateral PHPV.
Arch Ophthalmol 1998; 116 :381–2.
18 Taylor D , ed. History, examination and further investigation. In: Practical paediatric ophthalmology . 1st ed. Oxford: Blackwell Science,
1997:31–3.
19 Marshman WE , Jan JE, Lyons CJ. Neurologic abnormalities associated with persistent hyperplastic primary vitreous.
Can J Ophthalmol
1999; 34 :17–22.
20 Duke-Elder SS , Cook C. The ocular vascular system. In: Duke-Elder SS, ed.
System of ophthalmology, Vol III. Normal and abnormal development. Part I.
Embryology . London: Henry Kimpton, 1963:179–209.
21 Pruett RC . The pleomorphism and complications of posterior primary vitreous.
Am J Ophthalmol 1975; 80 :625–9.
22 Parks MM , Johnson DA, Reed GW. Long-term visual results and complications in children with aphakia.
Ophthalmology 1993; 100 :826–41.
23 Anteby I , Cohen E, Karshai I, et al.
Unilateral persistent hyperplastic primary vitreous: course and outcome.
J AAPOS 2002; 6 :92–6.
24 Nankin SJ , Scott WE. Persistent hyperplastic primary vitreous. RotoExtraction and other surgical experience.
Arch Ophthalmol 1977; 95 :240–3.
25 Maurer PA , Hiles DA. Unoperated persistent hyperplastic primary vitreous.
Trans Am Acad Ophthalmol Otolaryngol 1987; 38 :518–22.
26 Gulati N , Eagle RC Jr, Tasman W. Unoperated eyes with persistent fetal vasculature.
Trans Am Ophthalmol Soc 2003; 101 :59–64.
27 Raskind R . Persistent hyperplastic primary vitreous: necessity of early recognition and treatment.
Am J Ophthalmol 1966; 62 :1072–6.
28 Von Noorden GK . Histological studies of the visual system in monkeys with experimental amblyopia.
Invest Ophthalmol 1973; 12 :727–38.
Video reports
To view the video reports in full visit our website www.bjophthalmol.com and click on the link to the video reports.
N
Zero Phaco Microincision Cataract Surgey: The Hacc Technique.
K Vaitheeswaran,
S Gars, R Grover, M Nadar, S Sharma
N
The presenting features of multiple sclerosis.
VJM Barrett, J Walker, JS Elton
N
Removal of INTACS: Stepped surgical complexity demonstrated with three cases.
L Ilari, J C McAlister, D S Gartry
N
The Nuclear Slide: A novel approach for unleashing the potential of the hydrodissection wave.
A Naseri
N
Giant pleomorphic adenoma of the lacrimal gland: pre- and post-operative function.
A Jain, V I Nehru, U N Saikia, C E E Reddy
N
Limbal-sparing lamellar keratoplasty.
S L Watson, S Rauz, J Dart
N
Bilateral Abducens Neuromyotonia.
L H Ospina, N Aui-aree, D P Anderson
N
Light to dark physiological variation in irido-trabecular angle width.
G M Gazzard,
P J Foster, D S Friedman, P T Khaw, S K L Seah
Video Suite: Triamcinolone-assisted vitrectomy
N
Triamcinolone-assisted removal of the posterior hyaloid to repair retinal detachment due to macular hole in high myopia.
A Ueno, H Enaida, Y Hata, T Nakamura, T Hisatomi,
K Fujisawa, T Kubota, T Sakamoto, T Ishibashi
N
Triamcinolone acetonide-assisted Epiretinal Membrane Peeling.
S D M Chen, C K Patel
N
A suture technique to manage a case of severe early flap displacement after laser in situ keratomileusis.
L Spadea, P Pantaleoni, G Bianco
N
Reconstruction of the Ocular Surface in LOGIC Syndrome.
E Moore, V Kumar,
J R Ainsworth, S Shah
N
Laser Photocoagulation for Posterior Segment Intraocular Parasites.
T Prabriputaloong,
S Asawaphureekorn
N
Feeder Vessel Treatment with High Speed ICG Angiography.
D Stanescu-Segall,
G Coscas, F Coscas, G Soubrane
N
Endoscopy to aid anterior segment surgery.
J E Moore, A Sharm
N
Penetrating ocular injury due to a fish hook: Surgical removal.
S D M Chen,D Chiu,
C K Patel
N
Retinal Ganglion Cell Axon Response to Guidance Molecules.
S F Oster and DW Sretavan
N
Marin-Amat Syndrome.
A Jogiya, C Sandy
N
Excision of subcutaneous Dirofilariasis of the eyelid.
D Mallick, TP Ittyerah
N
Thixotropy: a novel explanation for the cause of lagophthalmos after peripheral facial nerve palsy.
M Aramideh, J H T M Koelman, P P Devriese, F VanderWerf, JD Speelman
N
Surgical revision of leaking filtering blebs with an autologous conjunctival graft.
K Taherian, A Azuara-Blanco
N
Dipetalonema Reconditum in the human eye.
T Huynh, J Thean, R Maini www.bjophthalmol.com
864
EXTENDED REPORT
‘‘Light’’ versus ‘‘classic’’ laser treatment for clinically significant diabetic macular oedema
F Bandello, A Polito, M Del Borrello, N Zemella, M Isola
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :864–870. doi: 10.1136/bjo.2004.051060
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Francesco Bandello, MD,
Department of
Ophthalmology, University of Udine, P le S Maria della Misericordia, 33100
Udine, Italy; francesco.bandello@ uniud.it
Accepted for publication
1 October 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aim: To compare the effectiveness of ‘‘light’’ versus ‘‘classic’’ laser photocoagulation in diabetic patients with clinically significant macular oedema (CSMO).
Methods: A prospective randomised pilot clinical trial in which 29 eyes of 24 diabetic patients with mild to moderate non-proliferative diabetic retinopathy (NPDR) and CSMO were randomised to either ‘‘classic’’ or ‘‘light’’ Nd:YAG 532 nm (frequency doubled) green laser. ‘‘Light’’ laser treatment differed from conventional (‘‘classic’’) photocoagulation in that the energy employed was the lowest capable to produce barely visible burns at the level of the retinal pigment epithelium. Primary outcome measure was the change in foveal retinal thickness as measured by optical coherence tomography (OCT); secondary outcomes were the reduction/elimination of macular oedema on contact lens biomicroscopy and fluorescein angiography, change in visual acuity, contrast sensitivity, and mean deviation in the central
10 ˚ visual field. Examiners were masked to patients’ treatment.
Results: 14 eyes were assigned to ‘‘classic’’ and 15 were assigned to ‘‘light’’ laser treatment. At
12 months, seven (50%) of 14 eyes treated with ‘‘classic’’ and six (43%) of 14 eyes treated with ‘‘light’’ laser had a decrease of foveal retinal thickness on OCT (p = 0.79). A comparison of reduction/elimination of oedema, visual improvement, visual loss, change in contrast sensitivity, and mean deviation in the central 10 ˚ showed no statistical difference between the groups at 12 months (p .
0.05 for all groups).
Conclusions: This study suggests that ‘‘light’’ photocoagulation for CSMO may be as effective as ‘‘classic’’ laser treatment, thus supporting the rationale for a larger equivalence trial.
M acular oedema is the most common cause of visual loss in patients with diabetic retinopathy and its prevalence in the diabetic population has increased approximately fivefold over the past 10 years, from 0.4% to
2.1%.
1
The Early Treatment Diabetic Retinopathy Study (ETDRS) demonstrated the benefit of a specific strategy of laser treatment on reducing the risk of moderate visual loss in eyes with clinically significant macular oedema (CSMO).
2
Treatment with a grid pattern in the parafoveal region up to and including the edge of the foveal avascular zone in case of diffuse thickening has also been advocated in non-randomised series.
3 4 However, the beneficial effect of laser photocoagulation is associated with severe destruction of retinal photoreceptors and considerable side effects, such as post-treatment atrophic scarring causing paracentral dense scotomas, generalised loss of the central 10 ˚ threshold sensitivity, choroidal neovascularisation, and subfoveal fibrosis.
5–11 Moreover, a significant lateral spread of retinal pigment epithelium (RPE) atrophy may occur over time thus impairing visual function even if visual acuity (VA) is relatively preserved.
8 12 These potential complications may also negatively affect the decision to apply additional laser treatments whenever required.
Recently, some authors have shown that barely perceivable very light threshold treatment and non-visible end point subthreshold treatment promoted resolution of CSMO in small uncontrolled series.
13–15 This therapeutic effect has been correlated with the selective treatment of the RPE and subsequent restoration of its barrier function and production of growth factors.
16–20 Among these, the pigment epithelium derived factor (PEDF) has been shown to have a strong antiangiogenic activity and to be upregulated after photocoagulation.
21–22 Based on these data, conventional
ETDRS-like laser burns may not be necessary in the treatment of CSMO.
When treating or re-treating eyes with CSMO and leaking abnormalities close to the foveal centre or diffuse macular thickening, very light laser burns may have the theoretic advantage of producing less invalidating paracentral scotomata or significant reduction in the central sensitivity. We present here results of a prospective, randomised pilot trial comparing the effectiveness of barely visible or ‘‘light’’ laser treatment versus conventional or ‘‘classic’’ laser photocoagulation in CSMO.
METHODS
Patients were enrolled from 1 September 2001 to 30
November 2002. Eligibility criteria included a diagnosis of either type 1 or type 2 diabetes mellitus and non-proliferative diabetic retinopathy with CSMO documented by slit lamp contact lens biomicroscopy, as defined by the ETDRS, 3 and confirmed by optical coherence tomography (OCT). Increased macular thickness was established if the foveal thickness
(FTH), defined as the mean thickness of the central 1 mm diameter disc of the retinal map, exceeded two SD the mean normal value (that is, .
210 m m).
23 24 Other inclusion criteria were haemoglobin A
1c equal or less than 10%, diastolic blood pressure less than 90 mm Hg, and visual acuity of at least 20/200 on the ETDRS chart. Patients with previous laser treatment, proliferative diabetic retinopathy, history of retinal detachment, glaucoma or any other clinically relevant
Abbreviations: CSMO, clinically significant macular oedema; ETDRS,
Early Treatment Diabetic Retinopathy Study; FA, fluorescein angiography; FTH, foveal thickness; MD, mean deviation; NPDR, nonproliferative diabetic retinopathy; OCT, optical coherence tomography;
PEDF, pigment epithelium derived factor; RPE, retinal pigment epithelium; VA, visual acuity www.bjophthalmol.com
‘‘Light’’ v ‘‘classic’’ laser treatment for CSMO 865 ocular disease, cataract extraction or lens implantation within the past 12 months, or significant media opacities were excluded. The study was conducted according to the tenets of the Declaration of Helsinki and all subjects gave informed consent after the intent of the study had been explained.
At the baseline examination, an independent examiner refracted both eyes, measured distance visual acuity and contrast threshold using ETDRS visual acuity chart at
4 metres and Pelli-Robson charts at 1 metre, respectively.
Best corrected visual acuity was scored based on the total number of correct letters identified at 4 metres plus 30.
25 The first examination also included automated static threshold perimetry, stereo fundus photography, fluorescein angiography (FA), and OCT. If FA disclosed a macular area of nonperfusion at least twice as large as the foveal avascular zone, patients were excluded from the study. Automated static threshold perimetry was performed using the Humphrey field analyser (Humphrey-Allergan Medical Instruments, Irvine,
CA, USA) 10-2 program. The mean deviation (MD) over the central 10 ˚ was recorded. OCT scans were obtained using the
OCT 2000 scanner (Zeiss Humphrey Instruments, Dublin, CA,
USA) with the A5 version software. OCT scanning was performed by selecting the ‘‘radial lines’’ scan pattern, which acquires six linear scans 6 mm long centred on the fovea at equally spaced angular orientation. Acceptable scans were automatically analysed by the OCT computer software and retinal thickness maps were generated. Images were judged to be ‘‘acceptable’’ on the basis of the following acceptance criteria: good demarcation of the vitreoretinal and chorioretinal interface allowing for a correct identification of the two interfaces by the software and absence of artefacts caused by eye motion or unstable fixation. The FTH was recorded for analysis from the retinal thickness maps.
Patients who were believed to satisfy all eligibility criteria were assigned randomly at enrolment to receive ‘‘classic’’ or
‘‘light’’ laser treatment. If a patient had both eyes simultaneously eligible for the study, the right eye was assigned randomly to ‘‘classic’’ or ‘‘light’’ laser treatment and the left
Table 1 Baseline characteristics *
Characteristics
Age (mean (SD))
Sex
Female (%)
Male (%)
Visual acuity
Mean No (SD) of letters read
(approximate Snellen equivalent)
.
20/32
20/32-20/40
, 20/40
History of hypertension
Present
Not present
Systemic vascular disease
Present
Not present
Type of diabetes
1
2
Duration of diabetes (SD) (years)
Insulin treatment
HbA
1c
(SD) (%)
Mean deviation of central 10-2 test
(SD) (dB)
Foveal thickness on OCT (SD) ( m m)
Mean contrast sensitivity, No (SD) of letters
* Data are given as number (%) of patients
‘‘Classic’’ treatment
(n = 14)
63.71 (6.53)
5 (36)
9 (64)
74.64 (9.79)
(20/32)
7 (50)
4 (29)
3 (21)
8 (57)
6 (43)
1 (7)
13 (93)
0 (0)
14 (100)
9.36 (5.86)
5
7.5 (1.4)
2 3.23 (2.96)
360.36 (115)
31.71 (3.97) eye received the opposite assignment. All the visits and tests were performed by the same masked examiners (AP, MDB).
Photocoagulation was performed by the same surgeon
(FB) using a Nd:YAG 532 nm (frequency doubled) green laser. ‘‘Light’’ laser treatment differed from ‘‘classic’’ in that the energy employed was the lowest capable to produce barely visible burns at the level of the retinal pigment epithelium. For primary treatment with ‘‘classic’’ photocoagulation, 47 (SD 26) spots were applied with power ranging between 100 mW and 250 mW (median 140 mW), and for primary treatment with ‘‘light’’ photocoagulation, 92 (SD 36) spots were applied with power ranging between 50 mW and
100 mW (median 50 mW). Follow up visits were performed every 3 months after treatment and included a protocol refraction, best corrected visual acuity and contrast threshold measurement, fundus biomicroscopy, FA, and OCT.
Automatic static threshold perimetry of the central 10 ˚ was performed at the 3 month and 12 month follow up visit.
Supplemental treatment with the same protocol of the primary treatment was considered at each visit in those eyes with treatable lesions on FA and either increased foveal thickening on fundus examination or persistent foveal thickening and decreased vision. For supplemental treatment, 45 (SD 10) spots were applied in ‘‘classic’’ group, and
106 (SD 44) spots were applied in the ‘‘light’’ group. The study included all patients who completed the 12 month follow up examination.
The primary efficacy outcome was the proportion of patients with significant decrease in FTH on OCT retina thickness maps. A significant change in FTH was defined as a change greater than 10%, which is slightly higher than the reproducibility of the instrument (that is, reproducibility of plus or minus 6%) 26 in an attempt to exclude changes caused by spontaneous inter-visit variability. Secondary efficacy outcomes included the proportion of patients with reduction elimination of CSMO on biomicroscopy and fluorescein leakage on FA compared with baseline examination at 3, 6, and 12 months after study entry, the proportion of eyes that experienced a visual gain or loss of five or more letters
‘‘Light’’ treatment
(n = 15)
63.40 (7.26)
5 (33)
10 (67)
76.73 (5.80) (20/32)
6 (40)
8 (53)
1 (7)
9 (60)
6 (40)
1 (7)
14 (93)
0 (0)
15 (100)
10.00 (5.79)
4
7.7 (2.1)
2 3.51 (1.83)
322.93 (96)
33.36 (2.24) p Value
0.90
1
0.81
0.31
0.88
1
0.77
0.60
0.79
0.76
0.54
0.98
www.bjophthalmol.com
866 Bandello
(approximately one line) on the ETDRS chart, mean changes in visual acuity, contrast threshold, MD of the central 10 ˚ sensitivity, and number of local losses greater than 5 dB at each test point of the central 10 ˚ , suggestive of posttreatment scotomata.
Comparison between groups for categorical variables was performed with x 2 test; when assumptions for x 2 test were not verified, Fisher’s exact test was used. The normality of continuous variables distributions was checked by the
Shapiro-Wilk test. Comparisons between groups for continuous variables were performed with t test or the Mann-
Whitney U test depending on Shapiro-Wilk test results.
Comparisons within groups for continuous variables on differences from baseline were performed with paired t test or Wilcoxon test also depending on Shapiro-Wilk test results.
All analyses were performed using the statistical software
SPSS version 11.1.
RESULTS
A total of 29 eyes of 24 patients were assigned randomly to
‘‘classic’’ or ‘‘light’’ laser photocoagulation; 14 eyes were assigned to ‘‘classic’’ and 15 to ‘‘light’’ laser treatment. Five patients were treated bilaterally and 19 patients were treated unilaterally. OCT data were not available for one eye in the
‘‘light’’ group; therefore it was excluded from OCT data analysis. Baseline variables for each group are given in table 1.
Systemic, functional, and morphological characteristics were similar and not statistically different between the two groups.
Table 2 summarises the results at 12 months for individual patients. Table 3 compares the outcome measurements at 3,
6, and 12 months between the two study groups. No statistically significant differences could be found for any of the outcome measurements except for the proportions of eyes that experienced a visual gain of five or more letters at
6 months, which was larger in the ‘‘light’’ group. The average
FTH in both groups did not change significantly from baseline at any follow up visit. The initial median visual acuity of 20/32 in both groups remained unchanged at
12 months. At the 3, 6, and 12 month follow up, five (36%), seven (50%), and seven (50%) of 14 eyes treated with
‘‘classic’’ and four (29%), six (43%), and six (43%) of 14 eyes treated with ‘‘light’’ laser had a decrease of FTH on OCT
(p = 1, 0.50 and 0.79, respectively, Fisher’s exact test). At
12 month follow up, five (36%) of 14 eyes treated with
‘‘classic’’ and five (33%) of 15 eyes treated with ‘‘light’’ laser showed one line or more improvement in the visual acuity and two (14%) in the ‘‘classic’’ group and two (13%) eyes in the ‘‘light’’ group showed one line or more decrease in the visual acuity (p = 1, Fisher’s exact test). The average MD decrease over the central 10 ˚ at 12 months after ‘‘classic’’ and
‘‘light’’ laser treatment was 0.04 (SD 1.39) dB and 0.03 (SD
1.84) dB, respectively (p = 0.99, independent samples test).
The number of local losses greater than 5 dB at each test point of the central 10 ˚ , suggestive of post-treatment paracentral scotomata, was 5.00 and 4.78 in the ‘‘classic’’ and ‘‘light’’ laser treatment group, respectively, at 12 months
(p = 0.40, Mann-Whitney U test). One and three eyes were retreated at 3 months and four and three eyes at 6 months in the ‘‘classic’’ and ‘‘light’’ treatment group, respectively
(p = 0.60 and 0.68, respectively, Fisher’s exact test).
CASE REPORT
A 55 year old man presented with a 8 year history of type 2 diabetes mellitus and non-proliferative diabetic retinopathy in both eyes. On examination, his visual acuity was 20/50 in the right eye and 20/64 in the left eye. Fundus biomicroscopy revealed diffuse retinal thickening in both eyes (figs 1A, 2A).
FA showed extensive perifoveal leaking microaneurysms
Table 2 Details of the patients who underwent ‘‘classic’’ and ‘‘light’’ treatment
Patient Age Sex
Initial visual acuity
10
11
8
9
12
13
6
7
4
5
(A) ‘‘Classic’’ treatment group
1 61 M 20/100
2
3
75
54
F
M
20/32
20/25
68
60
66
68
F
M
F
F
20/62.5
20/32
20/25
20/25
55
61
64
76
58
62
M
M
M
M
M
M
20/50
20/20
20/25
20/25
20/40
20/40
9
10
7
8
11
12
13
5
6
3
4
14 64 F 20/25
(B) ‘‘Light’’ treatment group
1
2
61
59
M
M
20/32
20/20
56
60
60
63
F
M
M
M
20/40
20/25
20/32
20/20
56
68
63
55
74
76
77
M
F
F
M
F
M
M
20/20
20/25
20/32
20/62.5
20/40
20/32
20/32
14
15
58
65
F
M
20/40
20/25
No of letters gained/lost
Initial foveal thickness
Final foveal thickness
9
2 8
2 2
2 9
15
2 1
1
14
2
10
2
2
0
2
0
0
2 4
2 1
1
2 8
6
0
2
5
10
6
1
2 15
1
11
1
510
400
236
384
275
324
216
555
292
241
322
291
500
499
449
266
278
356
306
NA
237
345
258
588
305
371
301
211
320
367
433
290
298
237
306
340
306
284
240
406
237
218
412
173
268
501
579
271
550
400
253
278
240
NA
234
428
183
322
Change in foveal thickness on OCT
Reduction/ resolution of
CSMO on slit lamp
Increased
Increased
No
Decreased
Decreased
NA
No
Increased
Decreased
Decreased
Increased
Increased
Decreased
Decreased
No
Decreased
No
Increased
Decreased
Decreased
No
Increased
Decreased
No
No
Increased
Decreased
Decreased
Decreased
Yes
No
Yes
No
No
No
No
No
Yes
Yes
No
No
No
Yes
No
Yes
Yes
No
Yes
Yes
No
No
Yes
Yes
Yes
No
Yes
Yes
Yes
CSMO, clinically significant macular oedema ; FA, fluorescein angiography.
No
No
Yes
No
Yes
No
Yes
Yes
Yes
Yes
No
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
No
Yes
No
No
Reduction/ resolution of leakage on FA Re-treatment
Yes (1 year)
Yes (1 year)
Yes (6 months)
Yes (1 year)
Yes (1 year)
Yes (6 months)
Yes (1 year)
Yes (6 months)
Yes (6 months)
Yes (1 year)
Yes (1 year) www.bjophthalmol.com
‘‘Light’’ v ‘‘classic’’ laser treatment for CSMO 867
Table 3 Outcome measurements by time and treatment group *
Characteristics
Change in FTH on OCT
Decreased
Unchanged
Increased p Value
Mean (SD) change in FTH ( m m)
(post-treatment value minus pretreatment value) p Value `
Change in CSMO on biomicroscopy
Reduced/eliminated
Increased p Value
Reduction/resolution of leakage on FA p Value
Change in visual acuity
> 5 letters increase
No change
> 5 letters decrease p Value
Mean (SD) change in No of letters
(post-treatment value minus pre-treatment value) p Value `
Mean (SD) change in mean deviation of central 10 ˚ sensitivity (post-treatment value minus pretreatment value) p Value `
Mean No (SD) of scotomata p Value 1
Change (SD) in contrast sensitivity
(No of letters) p Value 1
No of eyes retreated p Value
3 months
‘‘Classic’’
(n = 14)
5 (36)
7 (50)
2 (14)
8 (57)
0 (0)
8 (57)
4 (29)
8 (57)
2 (14)
1
2 48.21 (88)
2.00 (5.22)
0.232
‘‘Light’’
(n = 15)
Light (n = 14)
4 (29)
8 (57)
2 (14)
2 15.86 (46)
4 (26)
1 (7)
0.19
0.96
#
9 (56)
0.29
3 (20)
12 (80)
0 (0)
0.46
2 0.81 (1.61)
0.80 (3.36)
2 0.66 (1.39)
7.92 (6.76)
0.82
0.63
2 0.36 (2.50)
0.75
0
7.28 (6.63)
2 0.07 (1.62)
0
6 months
‘‘Classic’’
(n = 14)
7 (50)
5 (43)
2 (14)
2 63.78 (105)
7 (50)
0 (0)
11 (79)
2 (14)
12 (86)
0 (0)
0.50
0.189
0.54
0.68
0.03
1.93 (4.56)
0.86
2 0.71 (2.84)
0.85
1 (7)
0.60
* Data are given as number (%) of patients except where noted.
Calculated with the Fisher’s exact test.
` Calculated with the t test.
1
Calculated with the U-Mann Whitney test.
‘‘Light’’
(n = 15)
Light (n = 14)
6 (43)
3 (21)
5 (36)
2 14.86 (85)
5 (33)
2 (13)
10 (63)
7 (47)
6 (40)
2 (12)
2.27 (5.75)
2 0.40 (2.67)
3 (20)
12 months
‘‘Classic’’
(n = 14)
7 (50)
4 (29)
3 (21)
0.79
2 47.86 (121)
0.274
‘‘Light’’
(n = 15)
Light (n = 14)
6 (43)
3 (21)
5 (36)
6.36 (135)
10 (71)
2 (14)
10 (71)
0.09
0.70
5 (36)
7 (50)
2 (14)
1
3.07 (6.50)
5 (33)
2 (13)
9 (56)
5 (33)
8 (53)
2 (13)
0.80 (6.82)
0.37
2 0.04 (1.39) 2 0.03 (1.84)
0.99
5.00 (4.96)
0.40
2 1.21 (3.51)
0.56
4 (29)
0.68
4.78 (5.87)
2 0.27 (2.76)
3 (20) bilaterally (figs 1B, 2B). OCT retina thickness maps were similar in both eyes and displayed severe diffuse macular thickening (figs 1C, 2C). Two sessions of ‘‘classic’’ and
‘‘light’’ laser treatment were applied to the right and left eye, respectively, at study entry and after 6 months. The degree and extent of retinal and RPE whitening produced by laser burns, which were greater in the right eye, were documented immediately after the first laser session by red-free photographs (figs 1D, 2D). One year later his visual acuity had decreased to 20/80 in the right eye and improved to 20/50 in the left eye. The fundus examination disclosed marked decrease in foveal thickness in both eyes and multiple laser scars, which where more prominent and partly hyperpigmented in the right eye (fig 1E). FA disclosed a significant reduction of late leakage in both eyes (figs 1F, 2F). The OCT retinal thickness map documented a marked decrease of foveal thickening bilaterally (figs 1G, 2G). The central 10 ˚ MD decreased from 2 5.4 dB to 2 3.45 dB in the right eye and from 2 5.9 dB to 2 3.60 dB in the left eye (figs 1H, 2H). The number of paracentral scotomata was six and two in the right and left eye, respectively.
DISCUSSION
Recent reports have suggested that the energy employed by the ETDRS in patients with CSMO may not be necessary to obtain a therapeutic effect and that these patients may be overtreated.
13–15 We designed this prospective, randomised pilot trial specifically to determine whether a significant difference existed between ‘‘classic’’ and ‘‘light’’ laser photocoagulation for CSMO and to assess the feasibility of a definite trial. Since visual acuity remains stable for a rather long time in the majority of patients with CSMO, regardless of treatment, the detection of small differences in the proportions of eyes losing vision requires large sample sizes and a long follow up time. Therefore, we used as our primary outcome a morphological parameter, which has been shown by the ETDRS to be useful in demonstrating a beneficial treatment effect. Biomicroscopic/photographic evaluation of macular oedema is semi-quantitative at best, while OCT retinal thickness measurements are objective, quantitative, and reproducible.
26–29 In our study, OCT examinations were performed at every visit by an experienced independent examiner who accepted only scans fulfilling well defined acceptance criteria. Since it has been shown that in eyes undergoing grid laser photocoagulation the average threshold sensitivity across the central 10 ˚ significantly decreases, 5 we also measured the perimetric central sensitivity in order to identify theoretical differences of the effect of the two treatments on the central visual field.
The results of this randomised trial suggest that there is no significant difference between eyes with CSMO treated with either ‘‘classic’’ or ‘‘light’’ laser treatment within the first year.
However, it is possible that significant differences might have been identified if a larger sample was used or follow up was continued beyond 1 year. In particular, the greater gain in mean number of letters, larger decrease in mean FTH, and greater proportion of eyes with reduction in CSMO on biomicroscopy in the ‘‘classic’’ group at 1 year, though not www.bjophthalmol.com
868 Bandello
Figure 1 Case report, right eye.
Clinically significant macular oedema before and after ‘‘classic’’ laser treatment. (A) Fundus photograph.
(B) Fluorescein angiography shows late leakage surrounding the fovea.
(C) OCT retina thickness map shows severe diffuse macular thickening.
(D) Red-free photograph immediately after ‘‘classic’’ laser treatment demonstrates multiple, ETDRS level grey-white burns applied to the areas of fluorescein leakage. (E) Fundus photograph 1 year after treatment shows multiple laser scars associated with several areas of hyperpigmentation. (F) Late phase fluorescein angiogram obtained 1 year after treatment demonstrates only minimal residual leakage temporal to the fovea.
(G) OCT retina thickness map at 1 year shows a significant decrease in foveal thickening with minimal residual thickening temporal to the fovea.
(H) ‘‘Total deviation’’ display of the central 10
˚
visual field before (left) and
1 year after laser treatment (right). A mean deviation (MD) decrease from
2 5.4 dB to 2 3.45 dB and six scotomata (focal losses greater than
5 dB, indicated by circles) mostly located on the nasal hemifield can be observed at 1 year.
reaching statistical significance, may suggest a trend towards a larger beneficial effect from ‘‘classic’’ treatment. On the other hand, a significantly larger number of patients experiencing a visual gain in the ‘‘light’’ group at 6 months may suggest an earlier benefit from this treatment, which might decrease after
6 months. Also, the failure to detect a significant difference in change in MD from baseline and in number of scotomata between the two treatment groups at 1 year could depend upon the fact that the central 10 ˚ sensitivity showed no significant decrease following ‘‘both’’ laser treatments, in contrast with the findings reported by Striph et al.
5 This may be because of the application of ‘‘lighter’’ intensity and fewer burns even in the
‘‘classic’’ group either because of a different technique or because fewer eyes with diffuse CSMO requiring extensive treatment were included in our study. Moreover, a more sensitive test, such as the microperimetry, might have been better in identifying differences between treatments in terms of focal losses on the visual field, since the point density of the central 10-2 test may not be sufficient to detect all the localised defects.
We also found a discrepancy between the number of eyes with reduction of CSMO based on biomicroscopic examination and OCT in the ‘‘classic’’ group. This finding was the result of the resolution of paracentral oedema and persistence of central foveal thickening in three patients (patients 6, 9,
10, in table 2), as confirmed by reviewing their retinal www.bjophthalmol.com
‘‘Light’’ v ‘‘classic’’ laser treatment for CSMO 869
Figure 2 Case report, left eye.
Clinically significant macular oedema before and after ‘‘light’’ laser treatment.
(A) Fundus photograph. (B) Fluorescein angiography reveals areas of focal and diffuse leakage. (C) OCT retina map demonstrates severe diffuse macular thickening. The topographic pattern of retinal thickening was very similar to the other eye. (D) Immediate post-‘‘light’’ laser treatment photograph demonstrates barely visible laser lesions. (E) and (F) Fundus photograph and late phase fluorescein angiogram obtained 1 year after treatment show very faint laser scar and significant reduction in fluorescein leakage.
(G) 1 year after ‘‘light’’ laser treatment the oedema is almost completely resolved in the central fovea and residual thickening temporal to the fovea is present. (H) ‘‘Total deviation’’ display of the central 10
˚
visual field before (left) and 1 year after laser treatment (right). A mean deviation
(MD) decrease from 2 5.9 dB to
2 3.6 dB and two scotomata (focal losses greater than 5 dB, indicated by circles) both located on the nasal hemifield can be seen at 1 year.
thickness maps, which revealed a marked decrease in the paracentral areas of the map but not in the central region.
In conclusion, this study, although underpowered and unlikely to yield definite conclusions as most pilot trials, seems to rule out large differences between the two treatments. Given the potential complications from the
‘‘classic’’ ETDRS level treatment, in particular the relatively high risk of invalidating paracentral scotomata, lighter intensity laser modalities should be investigated. Our preliminary data, suggesting a similar therapeutic effect between ‘‘classic’’ and ‘‘light’’ laser treatment, supports the further investigation of ‘‘light’’ laser photocoagulation with a larger equivalence trial.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
F Bandello, A Polito, M Del Borrello, N Zemella, Department of
Ophthalmology, University of Udine, Udine, Italy
M Isola, Department of Medical and Morphological Research, University of Udine, Udine, Italy
REFERENCES
1 Lee PP , Feldman ZW, Ostermann J, et al.
Longitudinal prevalence of major eye diseases.
Arch Ophthalmol 2003; 121 :1303–10.
2 Early Treatment Diabetic Retinopathy Study Research Group .
Photocoagulation for diabetic macular edema. Early Treatment Diabetic
Retinopathy Study report number 1.
Arch Ophthalmol 1985; 103 :1796–806.
3 Lee CM , Olk RJ. Modified grid laser photocoagulation for diffuse diabetic macular edema. Long-term visual results.
Ophthalmology
1991; 98 :1594–602.
www.bjophthalmol.com
870 Bandello
4 Akduman L , Olk RJ. Diode laser (810 nm) versus argon green (514 nm) modified grid photocoagulation for diffuse diabetic macular edema.
Ophthalmology 1997; 104 :1433–41.
5 Striph GG , Hart WM Jr, Olk RJ. Modified grid laser photocoagulation for diabetic macular edema. The effect on the central visual field.
Ophthalmology
1988; 95 :1673–9.
6 Sinclair SH , Alaniz R, Presti P. Laser treatment of diabetic macular edema: comparison of ETDRS-level treatment with threshold-level treatment by using high-contrast discriminant central visual field testing.
Sem Ophthalmol
1999; 4 :214–22.
7 Hudson C , Flanagan JG, Turner GS, et al.
Influence of laser photocoagulation for clinically significant diabetic macular edema (DMO) on short-wavelenght and conventional automated perimetry.
Diabetologia 1998; 41 :1283–92.
8 Schatz H , Madeira D, McDonald HR, et al.
Progressive enlargement of laser scars following grid laser photocoagulation for diffuse diabetic macular edema.
Arch Ophthalmol 1991; 109 :1549–51.
9 Lewis H , Schachat AP, Haimann MH, et al.
Choroidal neovascularization after laser photocoagulation for diabetic macular edema.
Ophthalmology
1990; 97 :503–10.
10 Guyer DR , D’Amico DJ, Smith CW. Subretinal fibrosis after laser photocoagulation for diabetic macular edema.
Am J Ophthalmol
1992; 113 :652–6.
11 Han DP , Mieler WF, Burton TC. Submacular fibrosis after photocoagulation for diabetic macular edema.
Am J Ophthalmol 1992; 113 :513–21.
12 Mainster MA , White TJ, Tips JH, et al.
Retinal-temperature increases produced by intense light sources.
J Opt Soc Am 1970; 60 :264–70.
13 Friberg TR , Karatza EC. The treatment of macular disease using a micropulsed and continuous wave 810-nm diode laser.
Ophthalmology
1997; 104 :20–30-8.
14 Roider J , Brinkmann R, Wirbelauer C, et al.
Subthreshold (retinal pigment epithelium) photocoagulation in macular diseases: a pilot study.
Br J Ophthalmol 2000; 84 :40–7.
15 Moorman CM , Hamilton AM. Clinical applications of the MicroPulse diode laser.
Eye 1999; 13 :145–150.
16 Bresnick GH . Diabetic maculopathy. A critical review highlighting diffuse macular edema.
Ophthalmology 1983; 90 :1301–17.
17 Wallow IH , Bindley CD. Focal photocoagulation of diabetic macular edema.
A clinicopathologic case report.
Retina 1988; 8 :261–9.
18 Del Priore LV , Glaser BM, Quigley HA, et al.
Response of retinal pigment epithelium to laser photocoagulation in organ culture.
Arch Ophthalmol
1989; 107 :119–22.
19 Marshall J , Clover G, Rothtery S. Some new findings of retinal irradiation by krypton and argon lasers. In: Birngruber R, Gabel V-P, eds. Laser treatment and photocoagulation of the eye.
Doc Ophthalmol Proc Series 36 . The Hague:
Junk, 1984:21–37.
20 Roider J , Michaud N, Flotte T, et al.
Response of the RPE to selective photocoagulation of the RPE by repetitive short laser pulses.
Arch Ophthalmol
1992; 110 :1786–92.
21 Dowson DW , Volpert OV, Gillis P, et al.
Pigment epithelium-derived factor: a potent inhibitor of angiogenesis.
Science 1999; 285 :245–8.
22 Ogata N , Tombran-Tink J, Jo N, et al.
Upregulation of pigment epitheliumderived factor after laser photocoagulation.
23 Hee MR , Puliafito C, Duker JS, et al.
Topography of diabetic macular edema with optical coherence tomography.
Ophthalmology 1998; 105 :360–70.
24 Massin P , Erginay A, Haouchine B, et al.
Retinal thickness in healthy and diabetic subjects measured using optical coherence tomogroaphy mapping software.
Eur J Ophthalmol 2002; 12 :102–8.
25 Ferris FL 3rd , Kassoff A, Bresnick GH, et al.
New visual acuity charts for clinical research.
Am J Ophthalmol 1982; 94 :91–6.
26 Massin P , Vicaut E, Haouchine B, et al.
Reproducibility of retinal mapping using optical coherence tomography.
Arch Ophthalmol 2001; 119 :1135–42.
27 Chauhan DS , Marshall J. The interpretation of optical coherence tomography images of the retina.
Invest Ophthalmol Vis Sci 1999; 40 :2332–42.
28 Polito A , Shah SM, Haller JA, et al.
Comparison between retinal thickness analyzer and optical coherence tomography for assessment of foveal thickness in eyes with macular disease.
Am J Ophthalmol 2002; 134 :240–51.
29 Browning DJ , McOwen MD, Bowen R, et al.
Comparison of the clinical diagnosis of diabetic macular edema with diagnosis by optical coherence tomography.
Ophthalmology 2004; 111 :712–15.
www.bjophthalmol.com
871
EXTENDED REPORT
Serum prorenin levels and diabetic retinopathy in type 2 diabetes: new method to measure serum level of prorenin using antibody activating direct kinetic assay
H Yokota, F Mori, K Kai, T Nagaoka, N Izumi, A Takahashi, T Hikichi, A Yoshida, F Suzuki,
Y Ishida
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :871–873. doi: 10.1136/bjo.2004.056580
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Harumasa Yokota, MD,
Department of
Ophthalmology,
Asahikawa Medical
College, 2-1-1-1
Midorigaoka Higashi,
Asahikawa, 078-8510
Japan; atokoy18@ asahikawa-med.ac.jp
Accepted for publication
1 December 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aim: To investigate the serum levels of prorenin and its correlation with the severity of diabetic retinopathy
(DR).
Methods: 248 patients with diabetes and 108 control subjects were divided into four groups: no-DR
(n = 146), no proliferative diabetic retinopathy (no-PDR) (n = 78), PDR (n = 24), and controls (n = 108).
Serum levels of prorenin from all subjects were measured using the new antibody activating direct kinetic
(AAD-PR) assay. The serum prorenin levels were compared among the groups.
Results: The serum levels of prorenin in the control, no-DR, no-PDR, and PDR groups, respectively, were
109.1 (66.1), 194.6 (160.4), 271.5 (220.3), and 428.4 (358.4) pg/ml (mean (SD)). Prorenin in the PDR group was remarkably high compared with the control and no-DR groups (p , 0.0001) and with the no-
PDR group (p = 0.002). Serum levels of prorenin increased with increasingly severe retinopathy. No correlation was found between the prorenin level and the duration of disease or HbA
1c
.
Conclusions: The serum levels of prorenin in patients with PDR were found to be markedly high using the
AAD-PR assay. Increased levels of prorenin in diabetes may have an important role in the pathogenesis of
DR.
D iabetic retinopathy (DR) is a major cause of blindness worldwide. Although strict glycaemic control is thought to be essential to prevent the occurrence of DR, 1 some cases unfortunately develop advanced proliferative diabetic retinopathy (PDR).
2 In fact, because it is difficult to confirm if diabetic microangiopathy including retinopathy is progressive or not, a useful predictor that is well correlated with the occurrence of diabetic microangiopathy is needed to prevent the development of diabetic microvascular complications.
Prorenin is an inactive precursor of renin. The circulating prorenin level is five to 10 times higher than the active form of renin. Although little is known about the biological function of prorenin, it reportedly increases in diabetes and is associated with the occurrence of DR and nephropathy.
3–5
Furthermore, in adolescents with diabetes, higher serum levels of prorenin occur several years before diabetic nephropathy 6–8 and retinopathy.
9 This modulation of prorenin in diabetes indicates that prorenin is involved in the occurrence and the progression of diabetic microangiopathy.
Although measuring prorenin seems to be a good method to determine if diabetic microangiopathy is present or not, the method of measuring prorenin in previous reports has been complicated. Until recently, the level of prorenin was determined by measuring the total renin level and subtracting the active rennin level.
10–12 Total renin was measured after activating inactive prorenin by trypsin or non-proteolytically.
At the same time, active renin was measured independently, and the difference in the levels between total renin and active renin was defined as the prorenin level.
A new method called the antibody activating direct prorenin (AAD-PR) assay, developed by Suzuki et al , 13 enables direct measurement of the concentration of prorenin using an antibody to the prorenin profragment, which detects prorenin in serum and confirms the complex to the prorenin.
This complex has renin-like activity—that is, the ability to convert angiotensinogen to angiotensin I. The generated angiotensin I is measured with the enzyme linked immunosorbent assay. The prorenin level can be calculated by the amount of generated angiotensin I. The AAD-PR assay was reported to have higher sensitivity than previous methods.
14
In this study, we focused on the relation between the serum levels of prorenin and the severity of DR. We measured serum levels of prorenin in patients with type 2 diabetes and estimated the clinical implication of prorenin in DR using the
AAD-PR assay.
PATIENTS AND METHODS
In all, 248 patients with diabetes and 108 control subjects from Asahikawa Medical College Hospital were included. The control subjects had a normal examination that included urinalysis, blood chemistry, and blood pressure measurement and had never had type 2 diabetes. Patients with diabetes who were followed by physicians at Asahikawa Medical
College Hospital all satisfied the criteria for diagnosis of diabetes by the World Health Organization. The subjects received a detailed explanation of the aims of the study and provided informed consent. This study protocol was reviewed by the ethics committee of our institution. All procedures adhered to the tenets of the Declaration of Helsinki.
The subjects were divided into four groups: patients without DR (no-DR group), those with retinopathy but no proliferative DR (no-PDR group), patients with proliferative
DR (PDR group), and controls. The characteristics of these groups are shown in table 1. Sera were obtained from all subjects and then treated as described by Kawazu et al to measure the serum levels of prorenin.
14 The distribution of serum prorenin levels in the four groups was compared using one way of analysis variance and Scheffe’s test. A p value of
Abbreviations: AAD-PR, antibody activating direct prorenin; DR, diabetic retinopathy; PDR, proliferative diabetic retinopathy; RAS, reninangiotensin system www.bjophthalmol.com
872
Table 1 Characteristics of the study groups (SD)
Number (male/female)
Age (years)
Duration of diabetes (years)
HbA
1c
(%)
Systolic blood pressure (mm Hg)
Diastolic blood pressure (mm Hg)
Control
108 (62/46)
55.9 (15.5)
124.0 (11.5)
75.8 (3.7)
No-DR
146 (70/76)
58 (13.3)
8.1 (6.9)
7.5 (1.7)
123.2 (15.3)
72.5 (4.6)
No-PDR
78 (42/36)
60.0 (13.3)
13.3 (7.2)
8.2 (1.8)
131.2 (16.0)
70.9 (9.7)
PDR
24 (13/11)
56.1 (10.1)
14.5 (8.4)
7.6 (1.3)
134.0 (14.2)
75.5 (9.9)
Yokota, Mori, Kai, et al
0.05 or lower was considered significant. The Pearson correlation coefficient ( r ) was calculated to determine whether there were close associations among the variables.
RESULTS
The characteristics of the subjects are shown in table 1. There is no statistical difference between males and females, which has been reported to affect the serum levels of prorenin.
14
Systolic blood pressure and diastolic blood pressure were not significantly different among the four groups. The distribution of the serum levels of prorenin in the four groups is shown in figure 1. The serum levels of prorenin in the control, no-DR, no-PDR, and PDR groups were 109.1 (66.1), 194.6
(160.4), 271.5 (220.3), and 428.4 (358.4) pg/ml (mean (SD)), respectively. The serum levels of prorenin were markedly higher in the PDR group than in the control and no-DR groups (p , 0.0001, Scheffe’s test) and the no-PDR
(p = 0.002) group. The serum levels of prorenin were higher with increasingly severe retinopathy. No significant correlation was found between the serum prorenin level and disease duration ( p = 0.56).
r = 0.17, p = 0.04) or the HbA
1c level ( r = 0.05,
DISCUSSION
In this study, we evaluated the serum levels of prorenin in patients with diabetes using the newly developed AAD-PR assay. This study showed that the serum levels of prorenin in patients with diabetes with PDR were remarkably higher than in the normal healthy subjects, patients without DR, and those with no PDR. The serum concentration of prorenin in patients with diabetes was higher than in control subjects, and a high serum concentration of prorenin in patients with diabetes increased with increasingly severe retinopathy.
These results supported previous reports that had shown the clinical implication of prorenin in the occurrence and the development of diabetic microangiopathy.
3–9 15
Recent studies investigated the relation between the concentration of prorenin and the occurrence or the development
1800
1600
1400
1200
1000
800
600
400
200
0
Control no-DR no-PDR PDR
Figure 1 The distribution of serum levels of prorenin; * p , 0.05,
** p , 0.01.
of DR.
3–9 15 Franken et al reported that a high plasma prorenin level is associated with DR, particularly PDR.
4 Makimattila et al reported that the serum total renin level increased and was a useful marker of activity and the severity of DR.
15 Total renin is composed of renin and prorenin, and 90% of total renin is prorenin.
16 The active renin level in diabetes does not increase.
17 18 An increase in the total renin level was thought to be the result of the increased level of prorenin in diabetes.
These reports showed the close relation between the concentration of prorenin and the severity of DR 4 15 and supported our results. Although those previous reports showed higher levels of prorenin in diabetes with retinopathy, the conventional measurement method was more complicated and less sensitive for determining the concentration of prorenin than the AAD-
PR assay.
14
In the present study, we showed that there was no close relation between the serum levels of prorenin and HbA
1c or duration of diabetes. Franken et al reported that the plasma concentration of prorenin was not correlated with HbA
1c the duration of diabetes.
5 and
On the other hand, Makimattila et al reported that the serum concentration of total renin was correlated with HbA
1c
.
15 Luetscher et al also demonstrated a positive correlation between HbA
1c tration of prorenin.
3 HbA
1c and the plasma concenand the duration of diabetes are key risk factors for diabetic microangiopathy and are thought to be associated with the occurrence of DR.
1 19 Although
HbA
1c is an important indicator for determining the degree of glycaemic control in diabetes, this is not sufficient to be associated with the occurrence and the severity of DR.
20
Higher serum levels of prorenin in diabetes might be more appropriate for estimating the occurrence and the severity of
DR than HbA
1c
. In this study, the duration of diabetes was longer in patients with PDR than other patients who had no retinopathy or in whom retinopathy was not proliferative; however, there was no close relation between the serum levels of prorenin and the duration of diabetes. Duration, as mentioned previously, is also an important key factor for the occurrence of DR, 19 but it does not seem to affect the serum concentration of prorenin.
In this study, we did not measure renin at the same time to determine if the serum level of renin in diabetes increased or not. Renin is well known to be a key enzyme in the cleavage of angiotensinogen to angiotensin I, and this reaction is a rate limiting step to generate angiotensin II in the reninangiotensin system (RAS). Previous reports showed that the concentration of renin in diabetes does not increase, 21 although RAS has been implicated in the pathogenesis of
DR.
3–5 15 22–25 The fact that renin does not increase in diabetes seems to be a discrepancy, but RAS is activated in diabetes.
Our study, as other previous reports showed, 3–5 13 26 might indicate the involvement of increased prorenin in the development of DR. In addition, as mentioned previously, the plasma concentration of prorenin precedes the occurrence of diabetic nephropathy by several years.
7 8 Increasing prorenin in diabetes may trigger microangiopathy and promote the development of diabetic microangiopathy through the activation of RAS.
www.bjophthalmol.com
Prorenin levels in diabetes mellitus 873
Recently, prorenin was reported to have enzymatic activity that generated angiotensin I and activated the RAS thorough the generation of angiotensin II.
26–28 Prorenin is composed of two components, the profragment of prorenin and mature renin. Suzuki et al demonstrated that prorenin has a key region in its profragment for non-proteolytic activation with protein interaction.
26 Furthermore, Nguyen et al , who investigated the renin/prorenin receptor, showed that the prorenin binding this receptor activated the conversion of angiotensinogen to angiotensin I. High levels of this receptor mRNA were detected in the heart, brain, and placenta and lower levels in the kidney and liver.
27 Recently, Ichihara et al proved the non-proteolytic activation of prorenin and the presence of renin/prorenin receptor in the kidney using streptozotocin induced diabetic rats. They reported that the interference of prorenin with peptide which inhibits an interaction of prorenin with renin/prorenin receptor, inhibited the local generation of angiotensin II and improved diabetic nephropathy in streptozotocin induced diabetic rats.
18 Angiotensin I generated with non-proteolytic activation of prorenin is transformed to angiotensin II by soluble or endothelium specific angiotensin converting enzyme.
Angiotensin II exhibits pathological effects in the retina in diabetes through binding angiotensin II type 1 receptor, which is thought to be the most important receptor of all subtypes to exhibit the physiological and pathological effects.
Angiotensin II is associated with overexpression of some angiogenic factors—that is, vascular endothelial growth factor (VEGF), 29–33 and angiopoietin 2.
34 VEGF and angiopoietin 2 have a crucial role in the development of retinal neovascularisation, 35–38 a main feature of PDR. Taken together, it is possible that a high concentration of prorenin in patients with diabetes activates the local RAS in the eyes through its binding renin/prorenin receptor and promotes the pathogenesis of DR through the generation of angiotensin II.
In this study, we evaluated the serum levels of prorenin in patients with type 2 diabetes with a newly developed method, the AAD-PR assay. The serum levels of prorenin in patients with PDR were markedly high. High levels of prorenin in diabetes increase with increasingly severe retinopathy. We showed that a high concentration of circulating prorenin may be involved in the pathogenesis of DR. Further prospective study is needed to investigate the relation between modulation of the serum levels of prorenin and the severity of DR, and in turn, whether patients without DR with a higher level of prorenin will develop retinopathy.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
H Yokota, F Mori, K Kai, T Nagaoka, N Izumi, A Takahashi, T Hikichi,
A Yoshida, Department of Ophthalmology, Asahikawa Medical College,
Asahikawa, Japan
F Suzuki, Faculty of Applied Biological Science, Gifu University, Gifu,
Japan
Y Ishida, Preveqol Co, Tokyo, Japan
The authors have no proprietary interest in any aspect of this report.
REFERENCES
1 The Diabetes Control and Complications Trial Research Group . The effect of intensive treatment of diabetes on the development and progression of longterm complications in insulin-dependent diabetes mellitus.
N Engl J Med
1993; 329 :977–86.
2 Mattock MB , Cronin N, Cavallo-Perin P, et al.
Plasma lipids and urinary albumin excretion rate in Type 1 diabetes mellitus: the EURODIAB IDDM
Complications Study.
Diabet Med 2001; 18 :59–67.
3 Luetscher JA , Kraemer FB, Wilson DM, et al.
Increased plasma inactive renin in diabetes mellitus. A marker of microvascular complications.
N Engl J Med
1985; 312 :1412–17.
4 Franken AA , Derkx FH, Schalekamp MA, et al.
Association of high plasma prorenin with diabetic retinopathy.
J Hypertens Suppl 1988; 6 :S461–3.
5 Franken AA , Derkx FH, Blankestijn PJ, et al.
Plasma prorenin as an early marker of microvascular disease in patients with diabetes mellitus.
Diabete
Metab 1992; 18 :137–43.
6 Allen TJ , Cooper ME, Gilbert RE, et al.
Serum total renin is increased before microalbuminuria in diabetes.
Kidney Int 1996; 50 :902–7.
7 Deinum J , Ronn B, Mathiesen E, et al.
Increase in serum prorenin precedes onset of microalbuminuria in patients with insulin-dependent diabetes mellitus.
Diabetologia 1999; 42 :1006–10.
8 Chiarelli F , Pomilio M, De Luca FA, et al.
Plasma prorenin levels may predict persistent microalbuminuria in children with diabetes.
Pediatr Nephrol
2001; 16 :116–20.
9 Kordonouri O , Wladimirowa A, Danne T. High total serum renin concentrations are associated with the development of background retinopathy in adolescents with type 1 diabetes.
Diabetes Care 2000; 23 :1025–6.
10 Sealey JE . Plasma renin activity and plasma prorenin assays.
Clin Chem
1991; 37 :1811–19.
11 Cooper RM , Murray GE, Osmond DH. Trypsin-induced activation of renin precursor in plasma of normal and anephric man.
Circ Res 1977; 40 :I171–9.
12 Derkx FH , de Bruin RJ, van Gool JM, et al.
Clinical validation of renin monoclonal antibody-based sandwich assays of renin and prorenin, and use of renin inhibitor to enhance prorenin immunoreactivity.
Clin Chem
1996; 42 :1051–63.
13 Suzuki F , Hatano Y, Nakagawa T, et al.
Non-proteolytic activation of human prorenin by anti-prorenin prosegment (pf # 1: 1P-15P) antiserum.
Biosci
Biotechnol Biochem 1999; 63 :550–4.
14 Kawazu S , Minagawa S, Yazawa M, et al.
Sex difference and possible relationship to microvascular complications of serum prorenin levels in type 2 diabetic patients, measured by a novel antibody-activating direct enzyme kinetic assay.
Journal of Diabetes and Its Complications 2004; 18 :275–81.
15 Makimattila S , Summanen P, Matinlauri I, et al.
Serum total renin, an independent marker of the activity and severity of retinopathy in patients with
IDDM.
Br J Ophthalmol 1998; 82 :939–44.
16 Sealey JE , Glorioso N, Itskovitz J, et al.
Prorenin as a reproductive hormone.
New form of the renin system.
Am J Med 1986; 81 :1041–6.
17 Ubeda M , Hernandez I, Fenoy F, et al.
Vascular and adrenal reninlike activity in chronically diabetic rats.
Hypertension 1988; 11 :339–43.
18 Ichihara A , Hayashi M, Kaneshiro Y, et al.
Inhibition of diabetic nephropathy by a decoy peptide corresponding to the ‘‘handle’’ region for nonproteolytic activation of prorenin.
J Clin Invest 2004; 114 :1128–35.
19 Chaturvedi N , Sjoelie AK, Porta M, et al.
Markers of insulin resistance are strong risk factors for retinopathy incidence in type 1 diabetes.
Diabetes Care
2001; 24 :284–9.
20 Kohner EM , Aldington SJ, Stratton IM, et al.
United Kingdom Prospective
Diabetes Study, 30: diabetic retinopathy at diagnosis of non-insulindependent diabetes mellitus and associated risk factors.
Arch Ophthalmol
1998; 116 :297–303.
21 Derkx FH , Schalekamp MA. Human prorenin: pathophysiology and clinical implications.
Clin Exp Hypertens A 1988; 10 :1213–25.
22 Drury PL , Bodansky HJ, Oddie CJ, et al.
Increased plasma renin activity in type
1 diabetes with microvascular disease.
Clin Endocrinol 1982; 16 :453–61.
23 Moravski CJ , Skinner SL, Stubbs AJ, et al.
The renin-angiotensin system influences ocular endothelial cell proliferation in diabetes: transgenic and interventional studies.
Am J Pathol 2003; 162 :151–60.
24 Funatsu H , Yamashita H. Pathogenesis of diabetic retinopathy and the reninangiotensin system.
Ophthalmic Physiol Opt 2003; 23 :495–501.
25 Sjolie AK , Chaturvedi N. The retinal renin-angiotensin system: implications for therapy in diabetic retinopathy.
J Hum Hypertens 2002; 16 (Suppl 3):S42–6.
26 Suzuki F , Hayakawa M, Nakagawa T, et al.
Human prorenin has ‘‘gate and handle’’ regions for its non-proteolytic activation.
J Biol Chem
2003; 278 :22217–22.
27 Nguyen G , Delarue F, Burckle C, et al.
Pivotal role of the renin/prorenin receptor in angiotensin II production and cellular responses to renin.
J Clin
Invest 2002; 109 :1417–27.
28 Prescott G , Silversides DW, Reudelhuber TL. Tissue activity of circulating prorenin.
Am J Hypertens 2002; 15 :280–5.
29 Wilkinson-Berka JL , Kelly DJ, Gilbert RE. The interaction between the reninangiotensin system and vascular endothelial growth factor in the pathogenesis of retinal neovascularization in diabetes.
J Vasc Res 2001; 38 :527–35.
30 Sarlos S , Rizkalla B, Moravski CJ, et al.
Retinal angiogenesis is mediated by an interaction between the angiotensin type 2 receptor, VEGF, and angiopoietin.
Am J Pathol 2003; 163 :879–87.
31 Otani A , Takagi H, Suzuma K, et al.
Angiotensin II potentiates vascular endothelial growth factor-induced angiogenic activity in retinal microcapillary endothelial cells.
Circ Res 1998; 82 :619–28.
32 Moravski CJ , Kelly DJ, Cooper ME, et al.
Retinal neovascularization is prevented by blockade of the renin-angiotensin system.
Hypertension 2000; 36 :1099–104.
33 Williams B . A potential role for angiotensin II-induced vascular endothelial growth factor expression in the pathogenesis of diabetic nephropathy ?
Miner
Electrolyte Metab 1998; 24 :400–5.
34 Otani A , Takagi H, Oh H, et al.
Angiotensin II induces expression of the Tie2 receptor ligand, angiopoietin-2, in bovine retinal endothelial cells.
Diabetes
2001; 50 :867–75.
35 Oh H , Takagi H, Suzuma K, et al.
Hypoxia and vascular endothelial growth factor selectively up-regulate angiopoietin-2 in bovine microvascular endothelial cells.
J Biol Chem 1999; 274 :15732–9.
36 Takagi H , Koyama S, Seike H, et al.
Potential role of the angiopoietin/tie2 system in ischemia-induced retinal neovascularization.
Invest Ophthalmol Vis
Sci 2003; 44 :393–402.
37 Umeda N , Ozaki H, Hayashi H, et al.
Colocalization of Tie2, angiopoietin 2 and vascular endothelial growth factor in fibrovascular membrane from patients with retinopathy of prematurity.
Ophthalmic Res 2003; 35 :217–23.
38 Oshima Y , Deering T, Oshima S, et al.
Angiopoietin-2 enhances retinal vessel sensitivity to vascular endothelial growth factor.
J Cell Physiol
2004; 199 :412–17.
www.bjophthalmol.com
874
EXTENDED REPORT
Classification of abnormal fundus autofluorescence patterns in the junctional zone of geographic atrophy in patients with age related macular degeneration
A Bindewald, S Schmitz-Valckenberg, J J Jorzik, J Dolar-Szczasny, H Sieber, C Keilhauer,
A W A Weinberger, S Dithmar, D Pauleikhoff, U Mansmann, S Wolf, F G Holz, for the FAM
Study Group *
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :874–878. doi: 10.1136/bjo.2004.057794
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Professor Frank G Holz,
Department of
Ophthalmology, University of Bonn, Ernst-Abbe-
Strasse 2, D-53127 Bonn,
Germany; frank.holz@ ukb.uni-bonn.de
* Fundus Autofluorescence in Age-related Macular
Degeneration Group. See appendix for list of participants.
Accepted for publication
2 December 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aim: To describe and classify patterns of abnormal fundus autofluorescence (FAF) in the junctional zone of geographic atrophy (GA) in patients with age related macular degeneration.
Methods: Digital FAF images were recorded in 164 eyes of 107 patients using a confocal scanning laser ophthalmoscope (cSLO; excitation 488 nm, detection above 500 nm) as part of a prospective multicentre natural history study (FAM Study). FAF images were obtained in accordance with a standardised protocol for digital image acquisition and generation of mean images after automated alignment.
Results: Image quality was sufficient for classification of FAF patterns in 149 eyes (90.9%) with lens opacities being the most common reason for insufficient image quality. Abnormal FAF outside GA in 149 eyes was classified into four patterns: focal (12.1%), banded (12.8%), patchy (2.0%), and diffuse (57.0%), whereby 12.1% had normal background FAF in the junctional zone. In 4% there was no predominant pattern. The diffuse pattern was subdivided into four groups including reticular (4.7%), branching (27.5%), fine granular (18.1%), and fine granular with peripheral punctate spots (6.7%).
Conclusions: Different phenotypic patterns of abnormal FAF in the junctional zone of GA can be identified with cSLO FAF imaging. These distinct patterns may reflect heterogeneity at a cellular and molecular level in contrast with a non-specific ageing process. A refined phenotypic classification may be helpful to identify prognostic determinants for the spread of atrophy and visual loss, for identification of genetic risk factors as well as for the design of future interventional trials.
I n developed countries age related macular degeneration
(AMD) has become the most common cause for registered blindness. Severe visual loss results from choroidal neovascularisation (CNV), pigment epithelial detachment or geographic atrophy (GA) of the retinal pigment epithelium
(RPE).
1 GA is thought to be the natural end stage of the atrophic AMD process when CNV does not develop.
2 While
CNV is the more common cause for visual loss, GA is responsible for approximately 20% of the severe visual impairment from AMD.
3 4 While extensive research in recent years has been attributed to the pathomechanisms of CNV formation and its inhibition, relatively little attention has been focused on GA as a common disorder.
With the advent of confocal scanning laser ophthalmoscopy (cSLO) it has become possible to visualise fundus autofluorescence (FAF) and its spatial distribution in vivo.
5–8
It represents a tool to evaluate the RPE during ageing and in retinal disease.
9 As shown by spectrometric investigations by
Delori and associates FAF is mainly derived from lipofuscin
(LF) in the RPE.
10 Excessive accumulation of LF represents a common pathogenetic pathway in various monogenetic and complex retinal diseases and may precede photoreceptor degeneration.
11–13 Recent studies described FAF changes in early and advanced atrophic AMD.
7 14 Hereby, excessive LF accumulation in the junctional zone precedes the development of GA and the enlargement of pre-existing GA.
15
Preliminary observations using FAF imaging suggested that there may be distinct phenotypes with regard to changes in
FAF in the junctional zone of GA.
7 Based on these findings a prospective, multicentre, natural history study was initiated to more precisely identify FAF variations in patients with
AMD. Here we report on a refined classification of FAF patterns in the junctional zone of GA in patients with AMD.
METHODS
Digital FAF images were obtained as part of the prospective, multicentre Fundus Autofluorescence in Age-related Macular
Degeneration (FAM) Study using a cSLO (Heidelberg retina angiograph, HRA classic, and HRA 2, Heidelberg Engineering,
Dossenheim, Germany), the optical and technical principles of which have been described previously.
7 15
For FAF imaging, an argon blue laser (HRA classic) or an optically pumped solid state laser (HRA2) (both 488 nm) was used for excitation. Emitted light was detected above 500 nm
(barrier filter). With an interference filter, the green share of the argon laser light was reduced to the extent that the ratio of the intensities of green and blue is below 10
2 7
. The above mentioned cut-off filter suppressed blue argon excitation light at 488 nm by a factor of 10 2 6 . Consequently, it was assumed that reflectance signals do not contribute to the FAF image obtained from the posterior pole of the examined eye.
This blockage even suppressed reflexes on the optical surface of the lens.
Maximal retinal irradiance using the HRA was approximately 2 mW/cm
2 for a 10 ˚ 6 10 ˚ frame and was therefore well below the limits established by the American National
Abbreviations: AMD, age related macular degeneration; cSLO, confocal scanning laser ophthalmoscope; ETDRS, Early Treatment
Diabetic Retinopathy Study; FAF, fundus autofluorescence; GA, geographic atrophy; HRA, Heidelberg retina angiograph; LF, lipofuscin;
RPE, retinal pigment epithelium; VA, visual acuity www.bjophthalmol.com
Abnormal fundus autofluorescence patterns in AMD 875
Table 1 Variations in fundus autofluorescence (FAF) in the junctional zone of geographic atrophy (GA) of 149 eyes * with atrophic AMD
Pattern of increased FAF in the junctional zone of GA
None
Focal
Banded
Patchy
Diffuse
Reticular
Branching
Fine granular
Fine granular with peripheral punctate
No
85
7
41
27
10
18
18
19
3
%
12.1
12.1
12.8
2.0
57.0
4.7
27.5
18.1
6.7
* In 15 eyes of the initially included 164 eyes insufficient FAF image quality did not allow for evaluation of the FAF pattern outside the atrophic patch; frequency data therefore refer to 149 eyes.
Six eyes (4.0%) were not grouped into one of these types, because there was no predominant FAF pattern in the junctional zone of GA.
Figure 1 Normal background fundus autofluorescence outside the central patch of geographic atrophy (66 year old patient, left eye, VA
5/80). The atrophic area is associated with a markedly decreased fundus autofluorescence because of the absence of retinal pigment epithelial cells, and, thus, autofluorescent lipofuscin.
Standards Institute (ANSI) and other international standards
(ANSI Z136.1; 1993). Images were immediately digitised and processed using a flexible frame processor and subsequently displayed on a computer screen. The digital images were saved on hard disc for further analysis and processing.
For acquisition of FAF images a standard operation procedure was developed which included focusing of the retinal image in reflection and red-free mode, sensitivity adjustment and acquisition of at least 15 single 30 ˚ 6 30 ˚ FAF images which encompassed the entire macular area and at least part of the optic disc. In order to amplify the FAF signal the best nine single images were aligned and a mean image was calculated after detection and correction of eye movements using image analysis software (Heidelberg Eye
Explorer, Heidelberg Engineering, Dossenheim, Germany).
Patients with unilateral or bilateral GA caused by AMD were included into the study. Any sign of exudation or choroidal neovascularisation as well as previous drug, surgical, or laser therapy were exclusion criteria. The study followed the tenets of the Declaration of Helsinki and was approved by the local ethics committees. Informed consent was obtained from each patient after explanation of the nature and possible consequences of the study. Best corrected central visual acuity (VA) was determined using Early
Treatment Diabetic Retinopathy Study (ETDRS) charts.
EDTA blood samples were taken for future molecular genetic analyses. The pupil of the study eye was dilated with 1% tropicamide and FAF images were obtained from each patient.
FAF images were evaluated by two independent readers. In case of discrepancy a third reader was involved to arbitrate.
Abnormal FAF was defined as an increased or decreased FAF signal compared with the FAF outside such lesions, the latter being referred to as normal FAF, which shows an even distribution, with a typical lower intensity in the macula caused by absorption of macular pigment in the neurosensory retina and lower LF levels in central RPE cells.
5 6 There is also a lower signal along large retinal vessels (absorption) and at the optic disc (absence of autofluorescent material).
RESULTS
Digital FAF images were obtained from a total of 164 eyes from 107 patients (mean age 72.96 (SD 7.43) years; 44 male and 63 female patients) with unilateral or bilateral GA caused by AMD.
Sixty eyes (36.6%) had multifocal areas of atrophy whereas
103 eyes (62.8%) presented with an unifocal patch of GA. In one eye (0.6%) delineation of the GA was not clear and the distinction between unifocal and multiple confluent areas of atrophy therefore impossible. An extrafoveolar location of the atrophic areas was observed in 86 eyes (52.4%); GA involved the foveola in 77 eyes (47.0%). In one eye (0.6%) the atrophic patch seemed to reach the fovea, but an exact demarcation was not possible. Because VA was 10/25 the foveola probably was not involved in the atrophic process. The total area of atrophy ranged from 0.4–39.8 mm 2 (mean 6.6 mm 2 ). Mean
VA in eyes with extrafoveolar GA was 10/20 (range 5/200–20/
16), and 10/50 (range 5/200–20/20) in eyes with subfoveal
GA.
GA as well as retinal vessels and the optic disc typically showed a markedly decreased FAF signal as previously described.
15–17 Evaluation of the FAF pattern outside GA requires good image quality and was performed in FAF images with sufficient image quality regarding contrast and sharpness. FAF image quality was sufficient for evaluation in
149 (90.9%) out of 164 eyes. Cataract and inability of proper fixation during the image recordings represented the most common reasons for insufficient image quality. Frequency data therefore refer to 149 eyes. In 18 eyes (12.1%) there was
Figure 2 Multiple patches of markedly focal increased fundus autofluorescence at the margin of the atrophic patch (77 year old patient, right eye, VA 5/80).
www.bjophthalmol.com
876 Bindewald, Schmitz-Valckenberg, Jorzik, et al no abnormal FAF noted in the junctional zone. The FAF outside the GA (fig 1) showed a normal even distribution.
The following patterns of abnormal FAF in the junctional zone of GA were identified (table 1).
Focal increased autofluorescence
In 18 eyes (12.1%) single or multiple small spots of markedly focal increased FAF were present at the margin of the atrophic patch (fig 2).
Band of increased autofluorescence
In 19 eyes (12.8%) there was a continuous stippled band of increased FAF surrounding the entire atrophic area (fig 3).
Patchy increased autofluorescence
Three eyes (2.0%) showed larger areas of patchy increased
FAF outside the area of GA. FAF intensity of these patches tended to be of lesser degree compared with the focal pattern described above (fig 4).
Diffuse increase of autofluorescence
The most frequent pattern of increased FAF in eyes with GA was a pattern referred to as diffuse, which was noted in 85 eyes (57.0%). Hereby, FAF changes were not confined to the margin of the atrophic areas but showed a larger spread at the posterior pole. These diffuse changes showed again interindividual differences that were classified into four subtypes.
Reticular
A so called reticular pattern (seven eyes, 4.7%) was characterised by various lines of increased FAF with a preferred radial orientation (fig 5A).
Branching
In 41 eyes (27.5%) there was a diffuse increased FAF with a fine branching pattern of an increased FAF signal (fig 5B).
Fine granular
This pattern was characterised by a larger area of increased
FAF with a granular-like appearance surrounding the GA, and was present in 27 eyes (18.1%) (fig 5C). There was a clear border between the granular increased FAF and the surrounding normal background FAF.
Figure 3 Band of increased fundus autofluorescence surrounding the geographic atrophy (69 year old patient, right eye, VA 10/40).
Figure 4 Larger areas of patchy increased fundus autofluorescence outside the area of geographic atrophy (66 year old patient, right eye,
VA 10/20).
Fine granular with peripheral punctate spots
In 10 eyes (6.7%) with a diffuse FAF change surrounding the atrophic area there were elongated small lesions with increased FAF signal (fig 5D).
Six eyes (4.0%) were not grouped to one of these types.
There was no predominant FAF pattern in the junctional zone of GA which led to discrepancy between the different readers. Frequency data of table 1 therefore show the results of 143 eyes of 97 patients. Bilateral GA was present in 46 patients. In 41 patients (89.13%) the pattern of abnormal
FAF outside the GA was identical reflecting a high degree of intraindividual symmetry.
DISCUSSION
With the advent of confocal scanning laser ophthalmoscopy it is possible to visualise FAF in vivo. While preliminary reports indicated interindividual variations in association with GA in patients with AMD 7 a refined classification of FAF changes in the junctional zone of GA is reported here. Refined phenotyping is not only important to identify prognostic determinants, it appears also as a prerequisite to determine specific genetic factors in a complex, multifactorial disease such as AMD.
18 19 We propose that the FAF classification system presented here may be used in other studies on GA caused by AMD.
RPE LF contains the dominant fluorophores responsible for
FAF.
20 Excessive LF accumulation represents a common final pathogenetic pathway in various monogenetic and complex retinal disorders. LF granules also accumulate with age.
21
Recent experimental studies have addressed possible molecular mechanisms of how excessive LF may interact with normal cellular functions of RPE cells. Hereby, A2-E has been identified as a main autofluorescent compound of LF.
22 Toxic properties of A2-E include phototoxic and detergent effects as well as inhibitory effects on lysosomal function.
23–26
Identification of other molecular species besides the LF proteome is in progress.
27 Recently developed animal models that share phenotypic characteristics of AMD including excessive LF and A2-E accumulation in the RPE, add to the understanding of potential underlying molecular mechanisms.
28 29 Clinical evidence of adverse LF effects comes from
FAF investigations and psychophysical studies. Scholl et al have demonstrated impaired photoreceptor function in association with increased FAF by fine matrix mapping in patients with AMD including GA.
30 We have shown that increased FAF in the junctional zone of GA and, thus, www.bjophthalmol.com
Abnormal fundus autofluorescence patterns in AMD 877
Figure 5 Diffuse types of increased fundus autofluorescence in the junctional zone of geographic atrophy. (A) Reticular pattern of increased fundus autofluorescence with a preferred radial orientation (69 year old patient, left eye, VA 10/32). (B) Diffuse pattern of increased fundus autofluorescence with relatively short branching linear features (79 year old patient, left eye, VA 10/32). (C) Diffusely increased fundus autofluorescence with a granular-like appearance surrounding the well defined area of geographic atrophy (55 year old patient, right eye, VA 10/20). (D) Peripheral elongated small lesions with increased fundus autofluorescence signal (62 year old patient, right eye, VA 10/100).
excessive LF accumulation precede the development of new areas of GA or the enlargement of pre-existing atrophic patches, 7 and is associated with impaired retinal sensitivity on microperimetry testing.
31
Various limitations have to be considered for FAF imaging.
Media opacities including lens opacifications may result in FAF images that cannot be analysed adequately.
Furthermore, this system currently does not allow for absolute quantitation of the FAF signal. However, this is not a prerequisite to delineate topographic patterns of abnormal FAF and, therefore, it might not be required to detect absolute levels of FAF. The accurate delineation of atrophic areas is facilitated in FAF imaging compared to fundus photographs as a result of the absence of the RPE containing the dominant fluorophores.
32 33
Ru et al initially described the presence of elevated
FAF surrounding GA.
14 Different abnormal FAF patterns in the junctional zone of GA in association with AMD have been identified previously in a smaller cohort.
7 Based on these findings the hypothesis was raised that there may be marked interindividual variation in the presence of high intraindividual symmetry with distinct phenotypic patterns in FAF.
33
Here we examined patients using FAF imaging. Particular features of FAF changes allowed for classification into various patterns.
GA in association with AMD has been shown to gradually enlarge over time.
34–37 Schatz and McDonald determined the yearly spread of atrophy in fundus photographs.
36 Medium sized areas of atrophy grew faster than smaller areas.
Sunness et al determined rates of spread in a cohort of 123 patients and identified interindividual variaton.
2 37 So far, prognostic determinants for the individual progression of atrophic AMD, and, therefore, additional visual loss, are unknown. Since there is both experimental and clinical evidence of toxic properties of LF 23–26 we hypothesise that different phenotypes of FAF changes in the junctional zone of
GA are associated with different rates of spread of preexisting atrophy. Our preliminary analyses indicate that progression is smaller in eyes with no or minimal FAF alteration in the junctional zone as opposed to eyes with widespread diffuse changes (Bindewald et al ARVO 2004;
# 2960). As different patterns of increased FAF might reflect heterogeneity at a cellular and molecular level, this classification might be helpful to identify genetic factors. The high degree of symmetry of abnormal FAF in patients with bilateral GA points rather towards specific genetic contributions than non-specific ageing processes.
33
In summary, based on a cross sectional analysis of patients with GA associated with AMD a classification system is presented to distinguish phenotypic patterns of FAF alterations in the junctional zone of atrophic areas. The observations implicate excessive RPE LF accumulation in atrophic AMD and are useful to test hypotheses in this respect. Non-invasive
FAF imaging obviously gives information over and above conventional imaging methods. Expanding the ongoing FAM study with longitudinal analyses it may be useful to identify prognostic determinants for the progression of atrophic
AMD, to monitor future interventional trials and to determine genetic factors.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
A Bindewald, S Schmitz-Valckenberg, F G Holz, Department of
Ophthalmology, University of Bonn, Ernst-Abbe-Strasse 2, 53127 Bonn,
Germany
J J Jorzik, H Sieber, S Dithmar, Department of Ophthalmology,
University of Heidelberg, INF 400, 69120 Heidelberg, Germany
J Dolar-Szczasny, First Eye Hospital of Medical University of Lublin,
Chmielna 1, 20-079 Lublin, Poland
C Keilhauer, Department of Ophthalmology, University of Wuerzburg,
Josef-Schneider-Strasse 11, 97080 Wuerzburg, Germany
A W A Weinberger, Department of Ophthalmology, University of
Aachen, Pauwelsstrasse 30, 52074 Aachen, Germany
D Pauleikhoff, Department of Ophthalmology, St Franziskus Hospital,
Domagkstrasse15, 48149 Muenster, Germany
U Mansmann, Institute for Medical Biometrics and Epidemiology,
University of Munich LMU, Marchioninistrasse 15, 81377 Munich,
Germany
S Wolf, Department of Ophthalmology, University of Bern Inselspital,
3010 Bern, Switzerland
Supported by Deutsche Forschungsgemeinschaft DFG Ho 1926/2-1,
1926/2-2 DFG Research Priority Program AMD SPP 1088.
APPENDIX
Centres and members participating in the Fundus
Autofluorescence in Age-Related Macular Degeneration
(FAM) Study: Department of Ophthalmology, University of
Bonn, Germany: investigators: Almut Bindewald, Hans-
Martin Helb, Felix Roth, Steffen Schmitz-Valckenberg,
Johannes N Witten, Frank G Holz study nurse: Martina
Hofmann; Department of Ophthalmology, University of Heidelberg,
Germany: investigators: Jork J Jorzik, Daniel W Miller,
Helena Sieber, Stefan Dithmar study nurse: Maria Herrmann
Institute for Medical Statistics and Biometry, University of
Heidelberg, Germany: Jens Dreyhaupt, Manuela Herzig, Maria
Pritsch, Anja Schuldt; Ulrich Mansmann Coordination Center for
Clinical Trials, University of Heidelberg: Marcus Schwabedissen,
Kristina Unnebrink; Department of Ophthalmology, University of Aachen, Germany: investigator: Andreas Weinberger;
Department of Ophthalmology, University of Leipzig, Germany: investigators: Wilma Einbock, Andreas Moessner, Ute
Schnurrbusch-Wolf, Henrike Wustemeyer, Sebastian Wolf; www.bjophthalmol.com
878 Bindewald, Schmitz-Valckenberg, Jorzik, et al
Department of Ophthalmology, University of Wuerzburg, Germany: investigators: Juliane Mlynski, Claudia Keilhauer; St
Franziskus Hospital Muenster, Germany: investigators: Georg
Spital, Astrid Meister, Daniel Pauleikhoff.
REFERENCES
1 Klein R , Klein BE, Jensen SC, et al.
The five-year incidence and progression of age-related maculopathy: the Beaver Dam Eye Study.
Ophthalmology
1997; 104 :7–21.
2 Sunness JS . The natural history of geographic atrophy, the advanced atrophic form of age-related macular degeneration.
Mol Vis 1999; 5 :25–9.
3 Ferris FL 3rd , Fine SL, Hyman L. ge-related macular degeneration and blindness due to neovascular maculopathy.
Arch Ophthalmol
1984; 102 :1640–2.
4 Hyman LG , Lilienfeld AM, Ferris FL 3rd, et al.
enile macular degeneration: a case-control study.
Am J Epidemiol 1983; 118 :213–27.
5 Von Ru¨ckmann A , Fitzke FW, Bird AC. Distribution of fundus autofluorescence with a scanning laser ophthalmoscope.
Br J Ophthalmol 1995; 79 :407–12.
6 Bellmann C , Holz FG, Schapp O, et al.
Topographie der
Fundusautofluoreszenz mit einem neuen konfokalen Laser-Scanning-
Ophthalmoskop.
Ophthalmologe 1997; 94 :385–91.
7 Holz FG , Bellmann C, Margaritidis M, et al.
Patterns of increased in vivo fundus autofluorescence in the junctional zone of geographic atrophy of the retinal pigment epithelium associated with age-related macular degeneration.
Graefes Arch Clin Exp Ophthalmol 1999; 237 :145–52.
8 Bindewald A , Jorzik JJ, Loesch A, et al.
Visualisation of retinal pigment epithelial (RPE) cells in vivo using digital high resolution confocal scanning laser ophthalmoscopy.
Am J Ophthalmol 2004; 137 :556–8.
9 Delori FC , Fleckner MR, Goger DG, et al.
Autofluorescence distribution associated with drusen in age-related macular degeneration.
Invest
Ophthalmol Vis Sci 2000; 41 :496–504.
10 Delori FC , Dorey CK, Staurenghi G, et al.
In vivo fluorescence of the ocular fundus exhibits retinal pigment epithelium lipofuscin characteristics.
Invest
Ophthalmol Vis Sci 1995; 36 :718–29.
11 Wing GL , Blanchard GC, Weiter JJ. The topography and age relationship of lipofuscin concentration in the retinal pigment epithelium.
Invest Ophthalmol
Vis Sci 1978; 17 :601–7.
12 Weiter JJ , Delori FC, Wing GL, et al.
Retinal pigment epithelial lipofuscin and melanin and choroidal melanin in human eyes.
Invest Ophthalmol Vis Sci
1986; 27 :145–52.
13 Dorey CK , Wu G, Ebenstein D, et al.
Cell loss in the aging retina. Relationship to lipofuscin accumulation and macular degeneration.
Invest Ophthalmol Vis
Sci 1989; 30 :1691–9.
14 Von Ru¨ckmann AV , Fitzke FW, Bird AC. Fundus autofluorescence in agerelated macular disease imaged with a laser scanning ophthalmoscope.
Invest
Ophthalmol Vis Sci 1997; 38 :478–86.
15 Holz FG , Bellmann C, Staudt S, et al.
Fundus autofluorescence and development of geographic atrophy in age-related macular degeneration.
Invest Ophthalmol Vis Sci 2001; 42 :1051–6.
16 Von Ru¨ckmann A , Fitzke FW, Bird AC. Distribution of pigment epithelium autofluorescence in retinal disease state recorded in vivo and its change over time.
Graefes Arch Clin Exp Ophthalmol 1999; 237 :1–9.
17 Spaide RF . Fundus autofluorescence and age-related macular degeneration.
Ophthalmology 2003; 110 :392–9.
18 Elkin PL . Primer on medical genomics part V: bioinformatics.
Mayo Clin Proc
2003; 78 :57–64.
19 Gerlai R . Phenomics: fiction or the future ?
Trends Neurosci 2002; 25 :506–9.
20 Delori FC , Goger DG, Dorey CK. Age-related accumulation and spatial distribution of lipofuscin in RPE of normal subjects.
Invest Ophthalmol Vis Sci
2001; 42 :1855–66.
21 Feeney-Burns L , Hilderbrand ES, Eldridge S. Aging human RPE: morphometric analysis of macular, equatorial, and peripheral cells.
Invest
Ophthalmol Vis Sci 1984; 25 :195–200.
22 Eldred GE , Lasky MR. Retinal age-pigments generated by self-assembling lysosomotropic detergents.
Nature 1993; 361 :724–6.
23 Holz FG , Schutt F, Kopitz J, et al.
Inhibition of lysosomal degradative functions in RPE cells by a retinoid component of lipofuscin.
Invest Ophthalmol Vis Sci
1999; 40 :737–43.
24 Schutt F , Davies S, Kopitz J, et al.
Photodamage to human RPE cells by A2-E, a retinoid component of lipofuscin.
Invest Ophthalmol Vis Sci 2000; 41 :2303–8.
25 Sparrow JR , Nakanishi K, Parish CA. The lipofuscin fluorophore A2E mediates blue light-induced damage to retinal pigmented epithelial cells.
Invest Ophthalmol Vis Sci 2000; 41 :1981–9.
26 Bergmann M , Schu¨tt F, Holz FG, et al.
Inhibition of the ATP-driven proton pump in RPE lysosomes by the major lipofuscin fluorophore A2-E may contribute to the pathogenesis of age-related macular degeneration.
FASEB J
2004; 18 :562–4.
27 Schutt F , Ueberle B, Schnolzer M, et al.
Proteome analysis of lipofuscin in human retinal pigment epithelial cells.
FEBS Lett 2002; 528 :217–21.
28 Mata NL , Tzekov RT, Liu X, et al.
Delayed dark-adaptation and lipofuscin accumulation in abcr + / 2 mice: Implications for involvement of ABCR in agerelated macular degeneration 2001; 42 :1685–90.
29 Ambati J , Anand A, Fernandez S, et al.
An animal model of age-related macular degeneration in senescent Ccl-2- or Ccr-2-deficient mice.
Nat Med
2003; 9 :1390–7.
30 Scholl HPN , Bellmann C, Luong V, et al.
Photopic and scotopic fine matrix mapping of retinal areas of increased fundus autofluorescence in patients with age-related maculopathy.
Invest Ophthalmol Vis Sci
2004; 45 :574–83.
31 Schmitz-Valckenberg S , Bu¨ltmann S, Bindewald A, et al.
Fundus autofluorescence and fundus perimetry in the junctional zone of geographic atrophy in patients with age-related macular degeneration.
Invest Ophthalmol
Vis Sci 2005; 45 :4470–6.
32 Schmitz-Valckenberg S , Jorzik JJ, et al.
FAM Study Group. Analysis of digital scanning laser ophthalmoscopy fundus autofluorescence images of geographic atrophy in advanced age-related macular degeneration.
Graefes
Arch Clin Exp Ophthalmol 2002; 240 :73–8.
33 Bellmann C , Jorzik J, Spital G, et al.
Symmetry of bilateral lesions in geographic atrophy in patients with age-related macular degeneration.
Arch
Ophthalmol 2002; 120 :579–84.
34 Maguire P , Vine AK. Geographic atrophy of the retinal pigment epithelium.
Am J Ophthalmol 1986; 102 :621–5.
35 Sarks JP , Sarks SH, Killingsworth MC. Evolution of geographic atrophy of the retinal pigment epithelium.
Eye 1988; 2 :552–77.
36 Schatz H , McDonald HR. Atrophic macular degeneration. Rate of spread of geographic atrophy and visual loss.
Ophthalmology 1989; 96 :1541–51.
37 Sunness JS , Gonzalez-Baron J, Applegate CA, et al.
Enlargement of atrophy and visual acuity loss in the geographic atrophy form of age-related macular degeneration.
Ophthalmology 1999; 106 :1768–79.
www.bjophthalmol.com
879
EXTENDED REPORT
Digital imaging of the optic nerve head: monoscopic and stereoscopic analysis
J E Morgan, N J L Sheen, R V North, Y Choong, E Ansari
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :879–884. doi: 10.1136/bjo.2004.046169
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
J E Morgan, Department of
Ophthalmology, University
Hospital of Wales, Heath
Park, Cardiff CF4 4XW,
UK; morganje3@cardiff.
ac.uk
Accepted for publication
11 November 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aims: To compare monoscopic and stereoscopic assessment of the optic disc using novel software for the digital stereoscopic analysis of optic disc stereopairs.
Methods: Software was developed for the stereoscopic display of digital optic disc images using an interlaced display method. Neuroretinal rim width was determined at 10 degree intervals around the optic disc using a custom (stereoscopic) cursor whose depth was adjusted to that of Elschnig’s rim.
Measurements were taken, first viewing the disc monoscopically and at a separate sitting, stereoscopically.
Results: Measurements were made in 35 eyes from 35 patients (1260 estimates for each observer) using three observers. The mean cup to disc ratio (CDR) ranged from 0.57 to 0.66 (SD 0.13–0.14) for monoscopic viewing compared with 0.64 to 0.69 (SD 0.12–0.14) for stereoscopic viewing. Stereoscopic assessments gave higher CDRs in temporal, superior, nasal, and inferior aspects of the optic disc
(p , 0.001, Mann-Whitney U test). Agreement between observers in estimating CDR was high for monoscopic assessment (intraclass correlation coefficient 0.74 (CI 0.72 to 0.76) increasing to 0.80 (0.78
to 0.82) for stereoscopic assessment.
Conclusion: Digital stereoscopic optic disc assessment provides lower estimates of neuroretinal rim width and higher levels of interobserver agreement compared with monoscopic assessments.
A ccurate and reproducible assessment of the optic disc has a key role in the management of the glaucoma patient. Since considerable axon loss can precede the development of clinically detectable visual field loss, the early detection of structural retinal damage should facilitate earlier disease diagnosis and improve the clinical prognosis.
Similarly, close monitoring of the optic disc can detect progressive glaucomatous damage before changes appearing in the visual field.
1
The poor agreement, even among expert observers for subjective assessment of the optic disc, 2 3 has driven the development of clinical imaging devices such as scanning laser tomography, 4 polarimetry, 5 and optic coherence tomography.
6 These devices show great promise in the diagnosis of glaucoma and in the detection of progressive disease. For example, scanning laser tomography has been reported to detect early glaucomatous optic nerve damage with a sensitivity and specificity approaching 84% and 96%, respectively, 7 and can identify eyes with progressive damage before the onset of visual field loss.
1
By contrast, stereoscopic analysis of the optic disc images in glaucoma has not been developed as a routine clinical technique even though it remains the ‘‘gold standard’’ by which newer diagnostic technologies continue to be evaluated 8 and has provided valuable insights into the nature of glaucomatous pathophysiology.
9 Studies comparing the efficacy of stereoscopic imaging for the diagnosis of early glaucoma have shown that in expert hands, it can detect early glaucomatous damage with a sensitivity and specificity 8 10 that compares favourably with that obtained with scanning laser ophthalmoscopic devices.
11
Several factors have limited the clinical analysis of stereoscopic images. Firstly, the viewing of stereoscopic images can be impractical in the clinical setting where mirror based stereoscopes are required.
12 Secondly, the analysis of the optic discs is usually subjective, and the high diagnostic precision that has been reported with this technique has come from groups with considerable expertise in the clinical assessment of the optic disc 8 ; these results may not be applicable in less specialised units. Finally, there is little evidence to show that stereoscopic imaging per se provides sufficient additional clinical information to justify its use when compared with the monoscopic evaluation of optic nerve head images. This issue was highlighted recently by a study analysing sequential stereoscopic images, which suggests that stereoscopic imaging conveys little additional benefit 13 for the assessment of the optic disc.
This study employs software that has been developed for the digital, computer based assessment of stereoscopic optic disc images 14 15 to address many of the difficulties that have hindered the clinical analysis of these images.
16 We describe the application of this technique, in which we have developed tools for the precise delineation of the pathological features of stereoscopic optic disc images in space. The present study was designed to determine, firstly, whether digital stereoscopic analysis provided different estimate of neuroretinal rim width compared with monoscopic assessment and secondly, whether acceptable levels of interobserver agreement could be obtained for the assessment of neuroretinal rim width.
These are important questions that should be addressed before a new imaging modality such as digital stereoscopy is considered for clinical use in the diagnosis of glaucomatous optic neuropathy.
METHODS
The study is based on 35 optic disc images from patients with either glaucomatous or normal discs which were selected from our database of clinical images to provide a range of cup to disc ratios (CDRs). Patients were diagnosed as glaucomatous on the basis of visual field examination (Humphrey 24–2
SITA fast) and the existence of characteristic cupping of the optic disc indicating either diffuse or focal damage to the neuroretinal rim as identified by stereoscopic biomicroscopy
Abbreviations: CDR, cup to disc ratio; ICC, intraclass correlation coefficient; IOP, intraocular pressure; LC, liquid crystal www.bjophthalmol.com
880 Morgan, Sheen, North, et al
R h h/2
L
Original
Compressed
60 Hz
Sync doubled
120 Hz stereoscopic
Figure 1 Diagram showing the image manipulation required to display stereoscopic images in the above and below format using a synchronous doubling emitter.
h , image height.
and, if required, by stereoscopic examination of the optic nerve head images (colour slides). Ocular hypertensive patients had normal optic nerve and visual field examinations with intraocular pressures (IOPs) that were consistently above 22 mm Hg. Patients were classified as normal if they had IOPs of 21 mm Hg or below with normal visual field and optic disc examination. Stereoscopic images were taken in the course of routine patient care following informed and signed consent in accordance with requirements for the use of images in clinical research at the University Hospital of
Wales, Cardiff, UK. The observers, who were clinically trained and experienced in optic disc analysis were masked to the diagnosis of the optic discs, which were examined in random order. Sequential high quality stereofundus images were obtained using a Nikon F505 fundus camera using
Kodachrome EPN Ektachrome 35 mm slide film (ISO 100).
In every case, the pupil was dilated to more than 5 mm using one drop of tropicamide 1% and phenylephrine hydrochloride
2.5%. Stereoscopic images were taken using established techniques in which the illumination beam of the camera was set at the one part of the corneal limbus before being displaced horizontally to produce a standardised offset.
8 All patients had clear media with a visual acuity of 20/40 or better with correction.
Stereoimages were digitised using a Nikon Coolscan slide scanner to produce 24 bit true colour (1021 6 844 pixel) bit maps. The images were displayed in above and below format on a Sony 400 PS 19 inch monitor with a refresh rate of
75 Hz and were viewed stereoscopically using liquid crystal shutter glasses (Stereographics Corporation, San Rafael, CA,
USA). With this display format, the images that comprise the stereopair are compressed to 50% of their original height
(fig 1) and arranged so that one image occupies the top half of the display screen (‘‘frame’’) and the other image occupies the lower half. At the usual refresh rate of 60 Hz the images would be displayed one above the other in their compressed format. When the synchronous emitter (Stereographics Corp) which is connected to the VGA output of the computer is enabled the monitor refreshes at 120 Hz, showing first the upper field, which is now stretched to occupy the entire screen followed then by the lower field. The fields occupy the same point in space on the screen and are each refreshed, one after the other, at 60 Hz to give a flicker free stereoscopic image. The liquid crystal (LC) shutter glasses are triggered by an infrared emitter so that the LC lenses alternately opacify in synchronicity with the field displayed on the screen so that the correct image is seen by either eye. The images are restored to their original height at this refresh rate, but with
50% of the original vertical resolution. At the start of each session, the operator adjusts the vertical and horizontal offset of the images to ensure the highest quality stereoview. All observers received training in the use of the stereoscopic imaging software before starting the study.
Stereoimages were analysed using a mouse controlled cursor whose depth in stereoscopic viewing space could be adjusted to that of the optic disc margin (inner border of
Elschnig’s rim). A second line was then drawn within this boundary to demarcate the inner border of the neuroretinal rim. Both the disc margin and the neuroretinal rim inner boundary were drawn with the cursor set to the depth of the scleral rim (fig 2).
Once these contour lines were accepted, the program determined the width of the neuroretinal rim at 10 degree intervals around the optic disc. These widths were displayed as a series of lines at the depth of the scleral rim and were seen to lie within the tissue of the neuroretinal rim (fig 2).
The length of each line could be adjusted at each 10 degree interval so that the inner and outer ends of the line coincided with the inner and outer margins of the optic disc, respectively. Once the user had completed this adjustment,
CDRs were computed automatically and saved for further analysis.
In order to determine whether stereoscopic or monoscopic viewing affected the reproducibility of CDR assessment, the observers first viewed the optic disc monoscopically by viewing the right hand image of the stereoscopic pair. The image was displayed using the same software package and using the stereoscopic viewing glasses (Stereographics) to control for the effects of viewing through LC lenses. Not less than 1 week later, the images were viewed stereoscopically and the CDRs recalculated. Images were analysed in this order so that stereoscopic cues could not influence grading of the monoscopic images.
Neuroretinal rim
Cup
Scleral rim
Figure 2 Schematic diagram showing the criterion used for measurement of neuroretinal rim width. The cursor bar is set to the level of the neuroretinal rim (Elschnig’s rim). The inset diagram of the optic disc shows how the bar can be located to any given sector of the disc and adjusted in length to match the width of the neuroretinal rim.
500
450
400
350
300
250
200
150
100
50
0
0 0.1
0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9
CDR stereoscopic
1.0
Figure 3 Distribution of cup to disc ratios (CDR) for the three observers for stereoscopic assessments. Results from the three observers are represented by different symbols. Each observer made 1260 stereoscopic neuroretinal rim assessments over 35 discs.
www.bjophthalmol.com
Digital imaging of the optic nerve head 881
Comparison between normally distributed variables was by
Student’s t test. Non-parametric comparisons were made using the Mann-Whitney test. Differences between CDR estimates were expressed as means and standard deviations.
The measure of agreement between the observers was quantified using the intraclass correlation coefficient 17 (two way mixed effect model 18 ), which was determined for both monoscopic and stereoscopic images. In each case, statistical analysis was performed using SPSS 10.0.
RESULTS
High quality stereopairs were obtained from 35 eyes in 35 patients. Only one image was taken from each individual with 17 images from glaucomatous eyes, three from ocular hypertensive eyes, and 15 from healthy eyes. The mean age of the patients was 64 years (range 44–83 years). Each observer made 36 estimates of CDR in 35 eyes giving a total of 1260
CDR values. The distribution of stereoscopic CDR estimates for the three observers is shown in figure 3.
For monoscopic assessments, the mean CDRs for the three observers ranged from 0.57 to 0.66 (SD 0.13–0.14) compared with a 0.64 to 0.69 (SD 0.12–0.14) for the stereoscopic assessments. In figure 4 the mean stereoscopic CDRs (all observers, all locations around the disc, 35 discs) have been plotted against the corresponding monoscopic score showing that in the majority of cases the stereoscopic optic disc assessment provided a greater estimate of the CDR.
Comparison within each observer showed this difference to be statistically significant at the 0.001 level (Mann Whitney test).
In figure 5 the difference in stereoscopic and monoscopic assessment has been plotted against the mean of the stereoscopic and monoscopic assessment for each sector around the optic disc (Altman and Bland plots, 19 temporal, superior, nasal, and inferior). Positive differences in CDR estimate indicate a greater CDR estimate with stereoscopic compared with monoscopic viewing. It can be seen that for most assessments, the CDR estimate was greater when viewed stereoscopically compared with the monoscopic assessment. Although the monoscopic and stereoscopic assessment were statistically different for each segment
(p , 0.001, Mann Whitney), we did not find a significant difference between segments (ANOVA p = 0.40). Linear regression analysis suggests that the CDR assessment
(stereoscopic) had minimal effect on the magnitude of the difference between stereoscopic and monoscopic assessment
( r
2
= 0.06, p , 0.001, standardised coefficient beta = 0.27).
The levels of intraobserver and interobserver differences and agreement for monoscopic and stereoscopic observations
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
0.0
0.2
0.4
0.6
Monoscopic CDR
0.8
1.0
Figure 4 Plot of mean stereoscopic neuroretinal rim assessment (as cup to disc ratio, CDR) against the mean monoscopic CDR assessment. Data from 35 eyes averaged for the three observers to give 35 data points.
are shown in tables 1 and 2, respectively. For both monoscopic and stereoscopic assessments, intraobserver variation tended to be less than interobserver variation but this was not a marked effect. The intraclass correlation coefficient (ICC) for intraobserver agreements was calculated by comparison of measurements at the first and second examination sessions. The ICCs for interobserver agreements were based on observations made at the second examination session. For both monoscopic and stereoscopic observations the level of intraobserver agreement tended to be higher than interobserver agreement. One notable exception was that observer 3 had a lower level of intraobserver agreement for monoscopic observations compared with interobserver agreement with observer 2 (table 1). The level of interobserver agreement was greater with stereoscopic compared with monoscopic observations. This effect was also seen for the level of agreement between all three observers; for monoscopic assessments the ICC between all three observers was
0.63 (CI 0.35 to 0.77) compared with 0.74 (CI 0.65 to 0.80) for stereoscopic assessments, indicating good agreement with monoscopic assessment and substantial agreement with stereoscopic assessment.
20
DISCUSSION
We have described the use of digital stereoscopic optic disc assessment or the estimation of neuroretinal rim width in normal and glaucomatous eyes. The principal findings of the study are, firstly, that we found high levels of interobserver agreement for neuroretinal rim width for both monoscopic and stereoscopic assessments—with agreement being higher for stereoscopic assessment. Secondly, we found that stereoscopic optic disc assessment provided higher estimates of
CDR (and therefore a lower estimate of neuroretinal rim width) compared with monoscopic assessment.
The level of agreement for both monoscopic and stereoscopic assessment compares favourably with that obtained by expert observers 21 22 similar grade staff.
3 and exceeds that previously reported for
We found that intraobserver agreement was greater than interobserver agreement and in both cases this improved with stereoscopic observations. Several factors may account for the high level of agreement. The stereoscopic cursor enables the precise delineation of the inner margin of the neuroretinal rim with reference to the plane of Elschnig’s rim. The inner border of the neuroretinal rim has conventionally been defined as the point at which the retina surface steepens or changes slope at the margin of the optic disc 22–25 which is highly subjective. To our knowledge, ours is the first study in which software has been developed so that the cursor can be used at the level of interest within a stereoscopic image. As such, our software allowed the observers to minimise parallax errors in the measurement of neuroretinal rim width. Previous reports of digital stereoscopic disc analysis 14 did not describe the use of stereoscopic cursors. With the Discam system a single cursor is used, which is projected on one of the stereoscopic images 13 and cannot be adjusted to lie within the correct measurement plane. It is possible that the presentation of the cursor to a single eye may introduce effects such as rivalry, 26 which could complicate further accurate stereoscopic measurements.
These technical differences may account for the findings of
Parkin et al , 13 who did not report significant difference between monoscopic and stereoscopic assessments of neuroretinal rim width using the Discam stereoscopic disc imaging system but did note a trend for monoscopic rather than stereoscopic measurements to provide a higher estimate of CDR.
Another factor accounting for the high level of agreement between observers is that the observers could adjust their estimate of neuroretinal rim width using cursor bars whose www.bjophthalmol.com
882
A
0
40
Temporal
Superior
130
Nasal
310
Inferior
220
180
Morgan, Sheen, North, et al
Figure 5 Plot of the difference between stereoscopic and monoscopic optic disc assessments against the mean of the monoscopic and stereoscopic assessment. Symbols indicate the data from each observer. (A) Diagram showing angular subtense for each sector around the disc. (B) Temporal segment. (C) Superior segment.
(D) Nasal segment. (E) Inferior segment.
0.40
B
Temporal
0.30
0.20
0.10
0.00
–0.10
–0.20
–0.30
–0.40
0.0
0.1
0.2
0.3
0.4
0.5
0.6
Mean mono stereo
0.7
0.8
0.9
1.0
0.40
D
Nasal
0.30
0.20
0.10
0.00
–0.10
–0.20
–0.30
–0.40
0.0
0.1
0.2
0.3
0.4
0.5
0.6
Mean mono stereo
0.7
0.8
0.9
1.0
0.40
C
Superior
0.30
0.20
0.10
0.00
–0.10
–0.20
–0.30
–0.40
0.0
0.1
0.2
0.3
0.4
0.5
0.6
Mean mono stereo
0.7
0.8
0.9
1.0
0.40
E
Inferior
0.30
0.20
0.10
0.00
–0.10
–0.20
–0.30
–0.40
0.0
0.1
0.2
0.3
0.4
0.5
0.6
Mean mono stereo
0.7
0.8
0.9
1.0
length matched the width of the rim. The CDR value was generated by the computer and was not, therefore, a factor in intraobserver or interobserver variation.
The tendency for stereoscopic optic disc imaging to provide higher estimates of CDR (and therefore lower estimates of neuroretinal rim area) has previously been reported.
22 These findings are consistent with the relation between the shape of the optic nerve and the underlying optic nerve head colour.
A recent analysis of digital stereoscopic imaging revealed different results with monoscopic estimates for the CDR being greater than stereoscopic estimates 13 is not consistent with this view. It is possible that it relates to the use of monochromatic images (Discam uses a 256 grey scale compared with 24 bit colour resolution used in the present study) which may have obscured subtle variations in optic nerve head pallor at the margin of the neuroretinal rim.
Although the clinical relevance of the differences between monoscopic and stereoscopic assessment has yet to be established, it is likely that it will influence the sensitivity with which progressive glaucomatous damage can be detected; for eyes with a CDR of 0.7 a 0.1 difference represents 30% of the remaining neuroretinal rim. Our findings suggest that stereoscopic imaging will permit earlier detection of neuroretinal rim changes compared with monoscopic viewing.
Technical improvements in the quality of the stereoscopic display may also improve sensitivity for the detection of progressive damage. As with others 14 15 we have employed a synchronised doubled digital stereoscopic system to develop our prototype display because software development is straightforward, does not require specialised graphics cards, and can be implemented on computers and monitors with low specification. Unfortunately, the vertical resolution of the stereoscopic pair images is reduced by 50% and the images www.bjophthalmol.com
Digital imaging of the optic nerve head
Table 1 Monoscopic observations
Observer 1
Observer 1
Mean diffs *
SD diff *
Range *
ICC *
Observer 2
Observer 3
Mean diffs
SD diff
Range
ICC
Mean diffs
SD diff
Range
ICC
0.01
0.09
0.77
0.78
2 0.10
0.08
0.62
0.63
2 0.10
0.11
0.73
0.53
Observer 2
Mean diffs *
SD diff *
Range *
ICC *
Mean diffs
SD diff
Range
ICC
0.04
0.05
0.62
0.85
0.00
0.09
0.62
0.77
Observer 3
Mean diffs *
SD diff *
Range *
ICC *
0.12
0.08
0.61
0.55
Summary of the difference between the observers for the estimation of CDR by monoscopic viewing. Mean diffs: mean differences are shown for CDR assessments at matched 10 degree intervals. SD diff: standard deviation of the difference between measurements. ICC: intraclass correlation coefficient.
* Intraobserver comparison.
Interobserver comparisons.
883
Table 2 Stereoscopic observations
Observer 1
Observer 1
Mean diffs *
SD diff *
Range *
ICC *
Observer 2
Observer 3
Mean diffs
SD diff
Range
ICC
Mean diffs
SD diff
Range
ICC
2
2
0.05
0.08
0.78
0.88
0.05
0.09
0.80
0.71
0.04
0.09
0.80
0.72
Observer 2
Mean diffs *
SD diff *
Range *
ICC *
Mean diffs
SD diff
Range
ICC
0.03
0.06
0.70
0.83
0.01
0.07
0.66
0.81
Observer 3
Mean diffs *
SD diff *
Range *
ICC *
Summary of the difference between the observers for the estimation of CDR by stereoscopic viewing. Table layout as for table 1.
0.06
0.07
0.66
0.74
are vertically offset by one scan line on the video monitor which results in a subtle degradation of the quality of the stereoscopic image. Higher resolution systems for the analysis of stereoscopic images are now available and are likely to supersede the above and below stereoscopic display format.
With a suitable graphics card and a monitor with a refresh rate exceeding 100 Hz, it is possible to display right and left stereoscopic image pairs so that they occupy the same point in visual space on the monitor (so called quad buffered or page flipping technique) without the need for a small vertical offset. Image compression is not required so that images can be displayed at a higher resolution compared with interlaced displays. Another advantage of this technology is that it lends itself to the sequential analysis of aligned stereopairs for the detection progressive damage and will facilitate the clinical application of techniques such as stereochronoscopy.
27 28
The final consideration in the assessment of the stereoscopic images is that we used sequential rather than simultaneous stereoscopic images. We selected this option since sequentially acquired views are those that are available in most clinics since they do not require specialised cameras or additional hardware. Our results should, therefore be applicable to routine clinical practice. Since simultaneous stereoscopic images generally provide higher quality stereoviews 29 we predict that these would highlight greater differences between monoscopic and stereoscopic analysis.
We anticipate that developments in digital stereoscopy could have a valuable role in the refinement of the diagnosis of glaucomatous optic neuropathy and in the detection of the progressive glaucomatous damage. Given the advances that have been made in other digital imaging modalities, it is likely that digital stereoscopy can be used as a useful adjunctive diagnostic tool.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
J E Morgan, Y Choong, E Ansari, Department of Ophthalmology,
University Hospital of Wales, Heath Park, Cardiff CF4 4XW, UK
J E Morgan, N J L Sheen, R V North, Department of Optometry and
Vision Sciences, Cardiff University, Redwood Building, Edward VII
Avenue, Cardiff CF10 3NB, UK
Support: Welsh Office for Research and Development (WORD, UK).
Presented in part at the Association for Research in Vision and
Ophthalmology, Fort Lauderdale, FL, USA, May 2000.
REFERENCES
1 Kamal DS , Viswanathan AC, Garway-Heath DF, et al.
Detection of optic disc change with the Heidelberg retina tomograph before confirmed visual field change in ocular hypertensives converting to early glaucoma.
Br J Ophthalmol
1999; 83 :290–4.
2 Lichter PR . Variability of expert observers in evaluating the optic disc.
Trans
Am Ophthalmol Soc 1976; 74 :532–72.
3 Harper R , Reeves B, Smith G. Observer variability in optic disc assessment: implications for glaucoma shared care.
Ophthalmic Physiol Opt
2000; 20 :265–73.
4 Weinreb R , Dreher A. Reproducibility and accuracy of topographic measurement of the optic nerve head with the laser tomographic scanner. In:
Nasemann H, Burk R, eds.
Scanning laser ophthalmoscopy and tomography .
Munich: Quintessenz Verlags, 1990:177–82.
www.bjophthalmol.com
884 Morgan, Sheen, North, et al
5 Dreher A , Reiter K. Retinal laser ellipsometry: a new method for measuring the retinal nerve fiber layer thickness distribution.
Clin Vis Sci 1992; 7 :481–8.
6 Swanson EA , Izatt JA, Hee MR, et al.
In vivo retinal imaging by optical coherence tomography.
Optics Lett 1993; 18 :1864–6.
7 Wollstein G , Garway-Heath D, Hitchings R. Identification of early glaucoma cases with the scanning laser ophthalmoscope.
Ophthalmology
1998; 105 :1557–63.
8 Caprioli J . Clinical evaluation of the optic nerve in glaucoma. Trans.
Am
Ophthalmol Soc 1994; XCII :590–641.
9 Jonas JB , Budde WM, Panda-Jonas S. Ophthalmoscopic evaluation of the optic nerve head.
Surv Ophthalmol 1999; 43 :293–320.
10 Caprioli J . Discrimination between normal and glaucomatous eyes.
Invest
Ophthalmol Vis Sci 1992; 33 :153–9.
11 Greaney MJ , Hoffman DC, Garway-Heath DF, et al.
Comparison of optic nerve imaging methods to distinguish normal eyes from those with glaucoma.
Invest Ophthalmol Vis Sci 2002; 43 :140–5.
12 Gloster J , Parry DG. Use of photographs for measuring cupping in the optic disc.
Br J Ophthalmol 1974; 58 :850–62.
13 Parkin B , Shuttleworth G, Costen M, et al.
A comparison of stereoscopic and monoscopic evaluation of optic disc topography using a digital optic disc stereo camera.
Br J Ophthalmol 2001; 85 :1347–51.
14 Yogesan K , Barry CJ, Jitskaia L, et al.
Software for 3-D visualization/analysis of optic-disc images.
IEEE Eng Med Biol Mag 1999; 18 :43–9.
15 Eikelboom RH , Barry CJ, Jitskaia L, et al.
Neuroretinal rim measurement error using PC-based stereo software.
Clin Experiment Ophthalmol
2000; 28 :178–80.
16 Shuttleworth GN , Khong CH, Diamond JP. A new digital optic disc stereo camera: intraobserver and interobserver repeatability of optic disc measurements.
Br J Ophthalmol 2000; 84 :403–7.
17 McGraw K , Wong SP. Forming inferences about some intraclass correlation coefficients.
Psychological Methods 1996; 1 :30–46.
18 Shrout P , Fleiss J. Intraclass correlations: uses in assessing rater reliability.
Psychological Bulletin 1979; 86 :420–8.
19 Bland M , Altman D. Statistical methods for assessing agreement between two methods of clinical measurement.
Lancet 1986; 1 :307–10.
20 Landis JR , Koch GG. The measurement of observer agreement for categorical data.
Biometrics 1977; 33 :159–74.
21 Tielsch JM , Katz J, Quigley HA, et al.
Intraobserver and interobserver agreement in measurement of optic disc characteristics.
Ophthalmology
1988; 95 :350–6.
22 Varma R , Steinmann WC, Scott IU. Expert agreement in evaluating the optic disc for glaucoma.
Ophthalmology 1992; 99 :215–21.
23 Britton RJ , Drance SM, Schulzer M, et al.
The area of the neuroretinal rim of the optic nerve in normal eyes.
Am J Ophthalmol 1987; 103 :497–504.
24 Garway-Heath D , Ruben S, Viswanathan A, et al.
Vertical cup/disc ratio in relation to optic disc size: its value in the assessment of the glaucoma suspect.
Br J Ophthalmol 1998; 82 :1118–24.
25 Garway-Heath DF , Hitchings RA. Quantitative evaluation of the optic nerve head in early glaucoma.
Br J Ophthalmol 1998; 82 :352–61.
26 Harrad RA , McKee SP, Blake R, et al.
Binocular rivalry disrupts stereopsis.
Perception 1994; 23 :15–28.
27 Heijl A , Bengtsson B. Diagnosis of early glaucoma with flicker comparisons of serial disc photographs.
Invest Ophthalmol Vis Sci 1989; 30 :2376–84.
28 Berger JW , Patel TR, Shin DS, et al.
Computerized stereochronoscopy and alternation flicker to detect optic nerve head contour change.
Ophthalmology
2000; 107 :1316–20.
29 Boes D , Spaeth G, Mills R, et al.
Relative optic cup depth assessments using three stereo photograph viewing methods.
J Glaucoma 1996; 5 :9–14.
www.bjophthalmol.com
885
EXTENDED REPORT
Expression of growth differentiation factor-5 and bone morphogenic protein-7 in intraocular osseous metaplasia
S Toyran, A Y Lin, D P Edward
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :885–890. doi: 10.1136/bjo.2004.056374
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Deepak P Edward, MD,
Department of
Ophthalmology, University of Illinois at Chicago, 1905
W Taylor Street, L217,
Chicago, IL 60612, USA; deepedwa@uic.edu
Accepted for publication
1 December 2004
. . . . . . . . . . . . . . . . . . . . . . .
Background/aims: Intraocular bone is seen in a wide spectrum of ocular disorders. The pathogenetic mechanisms of bone formation in the eye are unclear. Growth differentiation factor-5 (GDF-5), bone morphogenic protein-7 (BMP-7), and transforming growth factor beta-1 (TGF b 1) are multifunctional cytokines that have important roles in bone formation. Immunohistochemistry was used to localise GDF-5,
BMP-7, and TGF b 1 in the human eye to determine their role in intraocular bone formation.
Methods: Paraffin embedded sections from human eyes included fetal eyes (n = 5), normal adult eyes
(n = 4), eyes with osseous metaplasia (n = 8), and eyes with focal fibrous metaplasia of the retinal pigment epithelium (RPE) without osseous metaplasia (n = 2). Immunohistochemistry was performed using indirect immunofluorescence with antibodies to GDF-5, BMP-7, and TGF b 1. The staining intensity was evaluated semiquantitatively in the RPE, retina, ciliary epithelium, and cornea; and analysed statistically.
Results: When compared with normal adult eyes, which showed no RPE immunoreactivity, the RPE metaplasia surrounding areas of osseous metaplasia showed mild GDF-5 and moderate BMP-7
(p = 0.004) intracytoplasmic immunoreactivity. In contrast, trace GDF-5 and mild BMP-7 staining was seen in zones of RPE fibrous metaplasia in areas not associated with osseous metaplasia. Mild intracytoplasmic
TGF b 1 expression was seen in the RPE metaplasia surrounding the bone when compared with adult eyes.
Both fetal and adult eyes showed trace to mild GDF-5 and BMP-7 labelling of the non-pigmented ciliary epithelium which was increased in the eyes with osseous metaplasia. In eyes with osseous metaplasia, a significant decrease in GDF-5 and BMP-7 labelling was noted in fetal keratocytes (p = 0.0159 for both antibodies) when compared to adult eyes. Also, a significant decrease in BMP-7 labelling was seen in keratocytes in eyes with osseous metaplasia (p = 0.0162).
Conclusions: The increase in GDF-5, BMP-7, and TGF b 1 immunoreactivity in zones of RPE metaplasia in eyes with osseous metaplasia suggests that these proteins have an important role in intraocular ectopic bone formation.
I ntraocular bone is seen in a many ocular disorders, including longstanding retinal detachment, chronic inflammation, and phthisis bulbi.
1–4 Bone morphogenic proteins (BMPs) are multifunctional cytokines, members of the transforming growth factor beta (TGF b ) superfamily of growth factors that have a wide range of effects that include regulation of cell growth, differentiation, and apoptosis.
5 6 In the eye they are expressed in the cornea, ciliary epithelium, lens epithelium, retina, and blood vessels.
7 These proteins act as autocrine and/or paracrine factors regulating bone growth and remodelling.
8
Ectopic ossification originates from osteoprogenitor stem cells lying dormant within the affected soft tissues. With the proper stimulus, the stem cells differentiate into osteoblasts and lead to osteoid formation, eventually leading to mature ectopic bone.
Although many isoforms of BMP induce bone formation,
BMP-7 is a potent osteoprogenitor. Growth differentiation factor-5 (GDF-5) has an important role in long bone development in humans, and has been shown to induce differentiation of mesenchymal cells into osteoblast lineages.
9
Both BMP-7 and cartilage derived morphogenetic protein-1
(also known as GDF-5) are overexpressed in pleomorphic adenomas of the salivary gland where heterotopic bone formation may be seen.
10 11 These findings suggest GDF-5 and
BMP-7 may have important roles in extraosseous bone formation. To evaluate this hypothesis in the eye, we examined the expression of GDF-5 and BMP-7 by immunohistochemistry in normal adult and fetal human eyes, and in eyes with intraocular osseous and fibrous metaplasia.
MATERIALS AND METHODS
Sections from enucleated specimens were obtained from the archives of the pathology laboratory of the University of
Illinois at Chicago, IL, USA. The project was approved by the institutional review board at the University of Illinois at
Chicago and complied with the Declaration of Helsinki.
Sections from human eyes included fetal eyes (n = 5) (range of age 57–72 days), normal adult eyes (n = 4), eyes with osseous metaplasia in the posterior pole (n = 8), and eyes with focal fibrous metaplasia of the retinal pigment epithelium (RPE) without osseous metaplasia (n = 2). Eyes with RPE fibrous metaplasia and tumour were excluded. A hip bone tissue specimen was used as a positive control. The specimens were fixed in 10% buffered formalin, processed, and embedded in paraffin wax. The tissue with bone had been previously decalcified.
Immunohistochemistry
Immunohistochemistry was performed on deparaffinised slides using indirect immunofluorescence technique. Before incubation with primary antibody, antigen retrieval with sodium citrate buffer (pH 6.0) was performed. The primary antibodies used are described in table 1. The reaction product was visualised using Cy3 conjugated streptavidin solution and the nuclei counterstained with DAPI.
Abbreviations: BMP-7, bone morphogenic protein-7; GDF-5, growth differentiation factor-5; RPE, retinal pigment epithelium; TGF b 1, transforming growth factor beta-1 www.bjophthalmol.com
886
Table 1 Primary antibodies
Antibody
GDF-5
Type
Polyclonal
Dilution
1:100
BMP-7
TGFb 1-G
Polyclonal
Polyclonal
1:100
1:25
Catalogue No
Sc-6901
Sc-6899
Sc-146-G
Source
Santa Cruz Biotechnology, Inc (Santa Cruz,
CA, USA)
Santa Cruz Biotechnology, Inc
Santa Cruz Biotechnology, Inc
Toyran, Lin, Edward
Data analysis
The immunolabelled specimens were examined under a Zeiss microscope, using Axioskop 2 Plus software. Two independent observers assigned a semiquantitative score to each slide based on the intensity of staining: negative = 0, 1 + (trace) =
1–25, 2 + (mild) = 26–50, 3 + (moderate) = 51–75, 4 +
(intense) = 76–100. A Mann-Whitney non-parametric test was used to compare the staining intensity between normal adult, fetal, and osseous eyes.
RESULTS
The results of staining for GDF-5 and BMP-7 in the normal adult, fetal and osseous eyes are shown in figures 1 and 2.
Adjacent sections stained with haematoxylin and eosin are presented for orientation. Figure 3 shows TGF b 1 immunoreactivity in an eye with osseous metaplasia.
Figure 4 shows the staining intensity of normal adult, fetal, and osseous eyes in the RPE, retina, ciliary epithelium, and cornea.
Retina and retinal pigment epithelium (RPE)
GDF-5 and BMP-7 immunoreactivity was absent in the normal adult sensory retina and RPE (figures not shown). In fetal eyes mild GDF-5 (fig 1A, B) and BMP-7 (fig 1C, D) labelling was present in Muller cell processes. In eyes with osseous metaplasia, mild GDF-5 (fig 1E, F) and moderate
BMP-7 (fig 1G, H) intracytoplasmic immunoreactivity was seen, especially in areas of RPE fibrous metaplasia surrounding bone. Staining was less intense in the osteoblasts. Trace
GDF-5 and BMP-7 immunoreactivity was seen in the retina.
Figure 1 Immunostaining of the retina and RPE. Cy3 is the fluorophore (red) and DAPI is the nuclear counterstain (blue). (A) Fetal retina (haematoxylin and eosin; magnification 6 40). (B) Mild GDF-5 staining of Muller cell processes of the retina in (A) (arrow) (magnification 6 40). (C) Mild stippled BMP-7 staining of Muller cell processes of the fetal retina in (D) (arrow) (magnification 6 40). (D) Fetal retina (haematoxylin and eosin; magnification 6 40).
(E) Area of osseous metaplasia surrounded by a zone of RPE fibrous metaplasia (arrowhead) (haematoxylin and eosin; magnification 6 20).
(F) Mild to moderate stippled GDF-5 staining of RPE fibrous metaplasia around the bone in (E) (arrowheads). Bruch’s membrane is indicated by the arrow (magnification 6 20). (G) Moderate stippled BMP-7 staining of RPE metaplasia (arrowheads) in (H) around the bone. Bruch’s membrane is indicated by the arrow (magnification 6 20). (H) Area of osseous metaplasia surrounded by RPE fibrous metaplasia (arrowheads)
(haematoxylin and eosin; magnification 6 20). (I) RPE fibrous metaplasia distant from the area of bone formation (haematoxylin and eosin; magnification 6 20). (J) Trace GDF-5 staining of RPE fibrous metaplasia in (I) (arrowheads) (magnification 6 20). (K) Mild BMP-7 staining of
RPE fibrous metaplasia in (L) (arrowheads) (magnification 6 20). (L) RPE fibrous metaplasia distant from the area of bone formation
(haematoxylin and eosin; magnification 6 20). (M) RPE fibrous metaplasia in an eye without bone formation. (haematoxylin and eosin; magnification 6 20). (N) Trace to mild GDF-5 staining of RPE fibrous metaplasia in (M) (arrowhead) (magnification 6 20). (O) Trace to mild
BMP-7 staining of RPE fibrous metaplasia in (P) (arrowheads) (magnification 6 20). (P) RPE fibrous metaplasia in an eye without bone formation
(haematoxylin and eosin; magnification 6 20).
www.bjophthalmol.com
GDF-5 and BMP-7 in intraocular osseous metaplasia 887
Figure 2 Immunostaining of the non-pigmented ciliary epithelium. (A) Ciliary epithelium of the normal adult eye (haematoxylin and eosin; magnification 6 40). (B) Mild stippled GDF-5 staining of the non-pigmented ciliary epithelium in (A) (arrows) (magnification 6 40). (C) Mild stippled
BMP-7 staining of the non-pigmented ciliary epithelium in (D) (arrows) (magnification 6 40). (D) Ciliary epithelium of the normal adult eye
(haematoxylin and eosin; magnification 6 40). (E) Ciliary epithelium of the fetal eye (haematoxylin and eosin; magnification 6 40). (F) Trace stippled
GDF-5 staining of the non-pigmented ciliary epithelium in (E) (arrow) (magnification 6 40). (G) Moderate BMP-7 staining of the non-pigmented ciliary epithelium in (H) (arrows) (magnification 6 40). (H) Ciliary epithelium of the fetal eye (haematoxylin and eosin; magnification 6 40). (I) Ciliary epithelium of the eye with osseous metaplasia (haematoxylin and eosin; magnification 6 20). (J) Mild to moderate diffuse GDF-5 staining of the nonpigmented ciliary epithelium in the eye with the osseous metaplasia in (I) (arrows) (magnification 6 20). (K) Moderate diffuse BMP-7 staining of the nonpigmented ciliary epithelium in the eye with the osseous metaplasia in (L) (arrows) (magnification 6 40). (L) Ciliary epithelium of the osseous metaplasia eye (haematoxylin and eosin; magnification 6 40).
In addition, trace GDF-5 (fig 1I, J) and mild BMP-7 (fig 1K,
L) immunoreactivity was seen in zones of RPE fibrous metaplasia not associated with osseous metaplasia. Trace
GDF-5 (fig 1M, N) and BMP-7 (fig 1O, P) immunoreactivity was seen in zones of RPE fibrous metaplasia of the eye without osseous metaplasia.
TGF b 1 immunoreactivity was absent in normal adult and fetal eyes. Mild intracytoplasmic TGF b 1 (fig 3) immunoreactivity was seen in the RPE surrounding the bone. TGF b 1 immunoreactivity was only evaluated in the RPE and areas of
RPE metaplasia.
Only the increased intensity of BMP-7 labelling in eyes with osseous metaplasia was statistically significant (significance versus normal; p = 0.004) (fig 4A, B).
Ciliary epithelium
There was mild intracytoplasmic staining of GDF-5 and BMP-
7 in the non-pigmented ciliary epithelium of normal adult eyes (fig 2A, B and 2C, D). GDF-5 staining in the fetal eye was less intense than in normal non-pigmented ciliary epithelium (fig 2E, F). However, BMP-7 immunoreactivity was more intense than in normal adult eyes (fig 2G, H). In eyes with osseous metaplasia, moderate GDF-5 (fig 2I, J) and
BMP-7 (fig 2K, L) expression was noted in the nonpigmented ciliary epithelium and faint BMP-7 immunoreactivity was seen in the pigmented ciliary epithelium. Moderate
GDF-5 immunoreactivity was seen in the stromal cells of the ciliary body.
The differences in expression of GDF-5 and BMP-7 in fetal
(p = 0.4127, p = 0.5556, GDF-5 and BMP-7 respectively) and osseous eyes (p = 0.3677) compared to normal eyes did not reach statistical significance (fig 4C).
Cornea
Moderate GDF-5 and BMP-7 staining was noted in keratocytes of normal adult eyes (figures not shown). Fetal keratocytes showed trace labelling with both antibodies.
The decreased GDF-5 and BMP-7 immunoreactivity in fetal keratocytes when compared to normal eyes was statistically significant (p = 0.0159 for both antibodies). Mild staining of
Figure 3 Immunostaining of the RPE with TGF b 1. (A) RPE fibrous metaplasia surrounding bone (haematoxylin and eosin; magnification 6 20).
(B) Mild to moderate stippled TGF b 1 staining of RPE metaplasia (arrowheads) around the bone in (A). Bruch’s membrane is indicated by the arrow
(magnification 6 20).
www.bjophthalmol.com
888
70
A
20
10
0
60
50
40
30
GDF5
BMP7
TGF-b1
Normal Fetal eye Osseous Fib met with bone
Fib met without bone
70
C
60
50
40
30
20
10
0
Normal
GDF5
BMP7
Fetal eye Osseous
80
D
70
60
50
40
30
20
10
0
Normal
GDF5
BMP7
Fetal eye Osseous
Toyran, Lin, Edward
70
B
20
10
0
60
50
40
30
Normal Fetal eye
GDF5
BMP7
Figure 4 Staining intensity of GDF-5 and BMP-7 in (A) RPE; (B) retina;
(C) ciliary epithelium; and (D) cornea of normal adult and fetal eyes, and eyes with osseous metaplasia. The staining intensity of TGF b 1 is only evaluated in the RPE (A), and includes eyes with RPE fibrous metaplasia without bone formation.
Osseous
GDF-5 and BMP-7 was observed in keratocytes of eyes with osseous metaplasia. Only the decrease in BMP-7 expression was significantly compared to normal eyes (p = 0.0162)
(fig 4D).
DISCUSSION
Ectopic ossification is the abnormal formation of bone within extraskeletal soft tissues. Some BMPs (BMP-2–8, 13, 14) are potent inducers that aid in transforming undifferentiated mesenchymal cells into cartilage and bone forming elements.
Of these, BMP-7 is a potent and well described osteoprogenitor and it is theorised that cytokines like BMP-7 induce ectopic ossification by inducing differentiation of pluripotential cells, mesenchymal cells, or fibroblasts into osteoprogenitor cells.
11–13
Intraocular bone formation usually occurs in the setting of a chronically diseased eye. Ectopic ossification may occur as a result of local or systemic inflammation. Local pathology like chronic retinal detachment, hyperplasia, and transdifferentiation of RPE appear to be a few of the prerequisites for intraocular osseous metaplasia.
14
Furthermore, pathological studies have shown that ocular inflammation is a common finding in eyes with bone formation.
14 The inflammatory infiltrate usually consists of chronic inflammatory cells including monocytes and macrophages, which produce cytokines such as interleukin-1 (IL-1) and tumour necrosis factor alpha (TNFa ).
15
Although the presence of IL-1 or TNFa was not directly investigated in the current study, it may have an indirect role in bone formation through activation of other cytokines.
TNFa and IL-1 are reported to stimulate activated cells to produce TGF b 1 16 and BMP-7.
17 18 It is possible that in the presence of inflammation, similar events may occur in the
RPE, which is known to express TGF b 1.
19 TGF b 1 promotes the transformation of epithelial cells to mesenchymal cells in the kidney 20 and possibly promotes the transformation of normal RPE into fibroblasts (RPE fibrous metaplasia), which is a common finding in eyes with osseous metaplasia. In our study eyes with osseous metaplasia had increased TGF b 1 expression in areas of RPE metaplasia when compared to normal eyes. Bosse et al demonstrated TGF b 1 mRNA in areas of mesenchymal tissue proliferation, and proposed that TGF b 1 was a local cellular regulator of ectopic bone formation.
21
Although the increase in TGF b 1 immunoreactivity was not statistically significant because of small numbers, the study in general supports its role in ectopic bone formation.
BMP-7 stimulates the transformation of mesenchymal cells into osteoblasts. In the eye, ectopic bone formation is mainly seen in areas of RPE fibrous metaplasia.
14 In our study there was significant BMP-7 immunoreactivity in areas of
RPE fibrous metaplasia surrounding bone. In contrast, eyes with RPE fibrous metaplasia without osseous metaplasia showed a mild increase in BMP-7 staining compared to normal eyes. This suggests that the expression of BMP-7 needs to reach a threshold level before the fibrous metaplasia cells transform into osteoblasts, which might explain the fact that all chronic ocular inflammatory disorders do not result in bone formation.
Additionally, BMP-7 inhibits the transformation of epithelial cells into fibroblasts.
20 Since BMP-7 was detected in metaplastic RPE cells and not in normal RPE, the metaplastic
RPE may be inhibiting the transformation of normal retinal pigment epithelial cells into fibrous cells, a process that was promoted by TGF b 1. Co-localisation of BMP-7 and TGF b 1 to areas of fibrous metaplasia suggests that these cytokines have an important role in regulating the transformation of RPE into fibrous cells and bone.
We therefore propose the following model for bone formation inside the eye (fig 5). Chronic end stage eye disease is often accompanied by intraocular inflammation.
The inflammatory cells release IL-1 or TNFa , stimulating the
RPE to produce TGF b 1 and BMP-7. TGF b 1 triggers epithelial-mesenchymal transformation of RPE cells into
RPE fibrous metaplasia. BMP-7 inhibits this transformation by counteracting the effect of TGF b 1. Additionally, BMP-7 promotes the transformation of metaplastic RPE into osteoblasts. It is likely that GDF-5, which was co-localised with BMP-7 in areas of RPE metaplasia, also stimulates osseous metaplasia. In rats, GDF-5 has been shown to induce the formation of cartilaginous tissue as well as bone.
22 GDF-5 was found in osteoblast-like cells from the primary ossification centres of long bones.
23 www.bjophthalmol.com
GDF-5 and BMP-7 in intraocular osseous metaplasia 889
Intraocular inflammation
Monocytes
Macrophages
IL-1
TNF α
+
TGF β
1
+
RPE
TGF β
1
BMP-7
Epithelial mesenchymal transformation
+
–
+
RPE
Metaplasia
Transdifferentiation
Osteoprogenitor cells
(osteoblasts)
Collagen matrix protein
Ectopic ossification
Ectopic bone tissue
Figure 5 Schematic diagram with proposal pathways of intraocular bone formation. Inflammatory cells synthesise interleukin (IL-1), tumour necrosis factor (TNFa ), and transforming growth factor beta-1 (TGF b 1). IL-1 and TNFa stimulate retinal pigment epithelium (RPE) to produce TGF b 1 and bone morphogenic protein-7 (BMP-7). Both TGF b 1 released from RPE and inflammatory cells trigger epithelial-mesenchymal transformation (from RPE cells to RPE metaplastic cells). BMP-7 balances these effects by inhibiting this process. On the other hand, increased BMP-7, if excessive, can cause transdifferentiation from RPE metaplasia to osteoblasts.
It is likely that these cytokines exercise their effects on target cells through ligand receptors. In rat eyes, TGF-beta type I and II receptors and BMP type IA, IB, and II receptors are expressed in the RPE, and other ocular structures.
24
BMP-7 binds predominantly to BMP type IB receptor in the rat osteoprogenitor-like cell line.
25 Also receptor binding studies of GDF-5 revealed that GDF-5 has affinity for the
BMP receptor type IA, IB, and II.
26
Though this model of intraocular ossification focused on inflammatory stimuli causing bone formation, intraocular bone formation has been well recognised in non-inflammatory proliferations such as teratomas, medulloepitheliomas, and choroidal osteomas. Our study did not specifically address these conditions; however, overexpression of cytokines such as GDF-5 and BMP-7 are reported in other neoplasias such as pleomorphic adenomas of the salivary gland, which are sites for heterotopic bone formation.
10 11
Although the expression of BMP-7 in adult and fetal human eyes has not been previously studied, focal mRNA expression has been detected in animal embryos.
27 28 BMP-7 has been shown in chick embryo RPE 29 and developing mouse RPE.
30 In our study fetal and normal adult RPE failed to show BMP-7 immunoreactivity. BMP-7 and GDF-5 immunoreactivity was absent in the normal adult sensory retina. BMP-7 has been shown to induce dendritic growth in rat sympathetic neurons.
31 However, since dendritic growth presumably is not a prominent feature of normal, mature human retina, one would expect that BMP-7 is not highly expressed.
In animal embryos, BMP-7 is abundantly expressed at the junction between the neuroepithelium and
RPE (likely Muller cell processes).
27–29 Our findings confirm this expression pattern in human tissue.
The expression of BMP-7 in the non-pigmented ciliary epithelium of human fetal eyes confirms previous studies that showed moderate BMP-7 expression in the nonpigmented ciliary epithelium of late stage mouse embryos and postnatal mice.
32 It was postulated that BMP-7 was required for ciliary body development. In contrast, there was decreased expression of GDF-5 compared to normal eyes, suggesting that GDF-5 may not have a role in ciliary body development. These changes are not statistically significant, probably because of the small sample size. Although not statistically significant, there was a trend towards increased expression of BMP-7 and GDF-5 in the non-pigmented ciliary epithelium of eyes with osseous metaplasia. This may result from inflammation in the ciliary body or diffusion of cytokines (for example, IL-1) from the posterior pole through the vitreous, stimulating the ciliary epithelium to produce
BMP-7 and GDF-5.
Moderate BMP-7 and GDF-5 immunoreactivity was seen in keratocytes of normal adult corneas. BMP-7 and GDF-5 are expressed in human keratocytes 32 and may be important regulators of corneal epithelial cell proliferation.
33 A significant decrease in the expression of GDF-5 and BMP-7 was observed in the corneas of fetal eyes. GDF-5 inhibits the proliferation of corneal epithelial and stromal cells.
33 It may need to be downregulated for proper corneal development.
Alternatively, factors required for corneal development might downregulate GDF-5 and BMP-7. Or, perhaps these proteins are not important for corneal development.
Decreased expression of GDF-5 and BMP-7 was also observed in corneas with osseous metaplasia compared to normal eyes; however, the decrease was only significant for
BMP-7. The reason for the decreased expression of BMP-7 in the cornea is not clear, since the cornea is not directly affected by the ossification.
In summary, we propose a potential pathway for the formation of bone within the eye that suggests that BMP-7 has an important role in this process. It is possible that other
BMPs and cytokines not investigated in this study also have a role in this complex process. GDF-5 also appears to have a role in osseous metaplasia but further studies may help understand the signalling pathway for bone formation and better define the role of GDF-5. In addition, this study confirmed in human tissue some of the previously published expression patterns of BMP-7 and GDF-5 in animals.
ACKNOWLEDGEMENTS
A gift from William Pendill Glaucoma Research Foundation.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
S Toyran, D P Edward, Department of Ophthalmology and Visual
Sciences, University of Illinois at Chicago, Chicago, IL, USA
A Y Lin, D P Edward, Department of Pathology, University of Illinois at
Chicago, Chicago, IL, USA
This work was supported by NEI Core Grant for Vision Research (EY
01792) supported by Research to Prevent Blindness, Bethesda, MD,
USA.
Competing interests: none declared www.bjophthalmol.com
890 Toyran, Lin, Edward
REFERENCES
1 Finkelstein EM , Boniuk M. Intraocular calcification and hematopoesis.
Am J Ophthalmol 1969; 68 :683–90.
2 Monselise M , Rapaport I, Romem M, et al.
Intraocular ossification.
Ophthalmologica 1985; 190 :225–9.
3 Evans NM . Ocular ossification—a case report and review of literature.
Trans
Ophthalmol Soc U K 1986; 105 :330–6.
4 Shields CL , Shields JA, Augsburger JJ. Choroidal osteoma.
Surv Ophthalmol
1988; 33 :17–27.
5 Wordinger RJ , Agarwahl R, Talati M, et al.
Expression of bone morphogenetic proteins (BMP), BMP receptors and BMP associated proteins in human trabecular meshwork and optic nerve head cells and tissues.
Mol Vis
2002; 8 :241–50.
6 Reddi AH . Bone and cartilage differentiation.
Curr Opin Genet
1994; 4 :737–44.
7 Yamashita H , Tobari I, Sawa M, et al.
Functions of the transforming growth factor-beta superfamily in eyes.
Nippon Ganka Gakkai Zasshi
1997; 101 :927–47.
8 Centrella M , Horowitz MC, Wozney JM, et al.
Transforming growth factor family members and bone.
Endocr Rev 1994; 15 :27–39.
9 Yamaguchi A , Komori T, Suda T. Regulation of osteoblast differentiation mediated by bone morphognetic proteins, hedgehogs, and Cbfa1.
Endocr Rev
2000; 21 :393–411.
10 Kusafuka K , Yamaguchi A, Kayano T, et al.
Expression of bone morphogenetic proteins in salivary pleomorphic adenomas.
Virchows Arch
1998; 432 :247–53.
11 Kusafuka K , Luyten FP, De Bondt R, et al.
Immunohistochemical evaluation of cartilage-derived morphogenic protein-1 and -2 in normal human salivary glands and pleomorphic adenomas.
Virchows Arch 2003; 442 :482–90.
12 Gruber R , Kandler B, Fuerst G, et al.
Porcine sinus mucosa holds cells that respond to Bone morphogenetic protein (BMP)-6 and BMP-7 with increased osteogenic differentiation in vitro.
Clin Oral Implants Res 2004; 15 :575–80.
13 Rutherford RB , Moalli M, Franceschi RT, et al.
Bone morphogenetic proteintransduced human fibroblasts convert to osteoblasts and form bone in vivo.
Tissue Eng 2002; 8 :441–52.
14 Vemuganti GK , Honavar SG, Jalali S. Intraocular osseous metaplasia. A clinico-pathological study.
Indian J Ophthalmol 2002; 50 :183–8.
15 Dayer JM . Evidence for the biological modulation of IL-1 activity: the role of
IL-1 Ra.
Clin Exp Rheumatol 2002; 20 (5 Suppl 27):14–20.
16 Chao CC , Hu S, Sheng WS, et al.
Tumor necrosis factor-alpha mediates the release of bioactive transforming growth factor-beta in murin microglial cell cultures.
Clin Immunol Immunopathol 1995; 77 :358–65.
17 Merrihew C , Soeder S, Rueger DC, et al.
Modulation of endogenous osteogenic protein -1 (OP-1) by interleukin-1 in adult human articular cartilage.
J Bone Joint Surg Am 2003; 85-A (Suppl 3):67–74.
18 Yoshida S , Kubota Y, Toba T, et al.
Induction of osteogenic protein-1 expression by interleukin-1beta in cultured rabbit articular chondrocytes.
Tohoku J Exp Med 2002; 197 :101–9.
19 Tanihara H , Yoshida M, Matsumoto M, et al.
Identification of transforming growth factorb expressed in cultured human retinal pigment epithelial cells.
Invest Ophthalmol Vis Sci 1993; 34 :413–19.
20 Zeisberg M , Kalluri R. The role of epithelial to mesenchymal transition in renal fibrosis.
J Mol Med 2004; 82 :175–81.
21 Bosse A , Wulf M, Wiethege T, et al.
Collagens and growth factors in heterotopic ossification.
Pathologe 1994; 15 :216–25.
22 Hotten GC , Matsumoto T, Kimura M, et al.
Recombinant human growth/ differentiation factor 5 stimulates mesenchyme aggregation and chondrogenesis responsible for the skeletal development of limbs.
Growth
Factors 1996; 13 :65–74.
23 Chang SC , Hoang B, Thomas JT, et al.
Cartilage derived morphogenetic proteins. New members of the transforming growth factor beta superfamily predominantly expressed in long bones during human embryonic development.
J Biol Chem 1994; 269 :28227–34.
24 Obata H , Kaji Y, Yamada H, et al.
Expression of transforming growth factorbeta superfamily receptors in rat eyes.
Acta Ophthalmol Scand
1999; 77 :151–6.
25 Tamaki K , Souchelnytskyi S, Itoh S, et al.
Intracellular signaling of osteogenic protein-1 through Smad5 activation.
J Cell Physiol 1998; 177 :355–63.
26 Erlacher L , McCartney J, Piek E, et al.
Cartilage-derived morphogenetic proteins and osteogenic protein-1 differentially regulate osteogenesis.
J Bone
Miner Res 1998; 13 :383–92.
27 Dudley AT , Lyons KM, Robertson EJ. A requirement for bone morphogenetic protein-7 during development of the mammalian kidney and eye.
Genes Dev
1995; 9 :2795–807.
28 Trousse F , Esteve P, Bovolenta P. BMP4 mediates apoptotic cell death in the developing chick eye.
J Neurosci 2001; 21 :1292–301.
29 Vogel-Hopker A , Momose T, Rohrer H, et al.
Multiple functions of fibroblast growth factor-8 in chick eye development.
Mech Dev
2000; 94 :25–36.
30 Hung FC , Zhao S, Chen Q. Retinal ablation and altered lens differentiation induced by ocular overexpression of BMP-7.
Vis Res 2000; 42 :427–38.
31 Horbinski C , Stachowiak EK, Chandrasekaran V, et al.
Bone morphogenetic protein-7 stimulates initial dendritic growth in sympathetic neurons through an intracellular fibroblast growth factor signaling pathway.
J Neurochem
2002; 80 :54–63.
32 Zhao S , Chen Q, Hung FC, et al.
BMP signaling is required for development of the ciliary body.
Development 2002; 129 :4435–42.
33 You L , Kruse FE, Pohl J, et al.
Bone morphogenetic proteins and growth and differentiation factors in the human cornea.
Invest Ophthalmol Vis Sci
1999; 40 :296–311.
www.bjophthalmol.com
891
EXTENDED REPORT
The impact of the Health Technology Board for Scotland’s grading model on referrals to ophthalmology services
S Philip, L M Cowie, J A Olson
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :891–896. doi: 10.1136/bjo.2004.051334
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Dr John Olson, Grampian
Diabetes Retinal Screening
Programme, Woolmanhill,
Aberdeen AB25 1LD, UK
Accepted for publication
11 November 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aim: To ascertain the impact of the Health Technology Board for Scotland’s grading model on referrals to ophthalmology services.
Methods: An analysis was performed of the screening outcomes of 5575 consecutive patients, who were screened by the Grampian Diabetic Retinopathy Screening Programme between March and September
2003 according to the recommendations of the Health Technology Board and the Scottish Diabetic
Retinopathy Grading Scheme 2003.
Results: 3066 (55%) were male. The median age was 65 years. 5.4% were passed on to the level 3 grader and 3.4% were finally referred to ophthalmology services. 2.3% required re-screening in 6 months; 85% were screened without mydriasis; 11.9% had ungradeable images despite a staged mydriasis protocol.
Time to complete grading was 32 days (22–45).
Conclusion: The impact of the Health Technology Board for Scotland’s recommendations on referrals to ophthalmology services is modest and should be containable within existing resources.
D iabetic retinopathy is still the commonest cause of blindness in people of a working age in the United
Kingdom but there is a long latent period between the onset of diabetic retinopathy and its progression to sight threatening eye disease and blindness.
1 2 The Diabetic
Retinopathy Study and the Early Treatment Diabetic
Retinopathy Study showed that photocoagulation can reduce the risk of severe visual loss by 50% or more.
3 4 Systematic screening for retinopathy among patients with diabetes has been shown to be cost effective.
5–7 All nations within the
United Kingdom are embarking on national screening programmes for diabetic retinopathy.
8 9 The most effective and pragmatic model for diabetic retinopathy has yet to be ascertained.
9–11 The Scottish Executive Health Department has decided that in Scotland the national diabetic retinopathy screening programme should be implemented according to the recommendations of the Health Technology Board for
Scotland.
12
The Health Technology Board for Scotland’s model attempted to optimise ‘‘clinical effectiveness and cost effectiveness while respecting patient preference.’’ After applying a rigorous health technology assessment process it recommended a digital photography based screening programme based on single 45 degree disc/macula using a staged mydriasis protocol.
12 The Health Technology Board for
Scotland recommended a three level grading process (fig 1) to enable screening programmes to become quickly established while still protecting patients.
The Scottish Executive Health Department’s Diabetic
Retinopathy Screening Implementation Group predicted that the impact of this model on referrals to ophthalmology services would be modest based on early experience from
Grampian, Lanarkshire and Tayside.
8 The aim of this study was to assess whether or not this prediction was accurate.
METHODS
Study population
The Grampian Diabetes Retinal Screening Programme commenced in April 2002. Grampian’s population of 525 859 is served by 89 general practices. All patients over the age of
10 years with diabetes mellitus were referred to the retinal screening programme by their general practitioner. Patients could opt out of the screening programme only if they were attending ophthalmology services on a regular basis and the consultant ophthalmologist was willing to continue screening for diabetic retinopathy. In this scenario, the hospital patient administration system was used to confirm the presence of an ophthalmology appointment and whether they attended a specialist medical retina clinic or not. The retinal screening programme had one fixed non-mydriatic
45 degree retinal Canon CR5–45NM camera (Canon Inc,
Medical Equipment Business Group, Kanagawa, Japan) based at the Diabetes Centre, Woolmanhill Hospital,
Aberdeen, and two mobile Canon CR6–45NM cameras
(Canon Inc, Medical Equipment Business Group,
Kanagawa, Japan) housed in mobile vans. All cameras were attached to high resolution (2160 6 1440 pixels) Canon D30 digital cameras. At the time of the study there were 15 700 patients on the register. Grading and outcome data on all
5575 patients who underwent screening between March 2003 and September 2003 were collated and analysed.
Staffing
The screening programme employed three level 1 graders/ retinal photographers, two part-time level 2 graders, and one part-time level 3 grader during the period of the study. Whole time equivalents were 1.0 for level 1 grading, 0.1 for level 2 grading, 0.1 for level 3 grading, and 3.0 for photography. The level 1 graders/retinal photographers had no previous experience in retinal screening before recruitment in
January 2003 and underwent a 5 day intensive practical training programme run over 2 weeks. The level 2 graders, all of whom had previous experience in retinal screening, undertook the grading component of the same training programme. The level 3 grader was a consultant in medical ophthalmology.
Screening examination
Patients had their best visual acuity, with pinhole correction if required, measured by Bailey-Lovie logMAR charts.
13 Then, www.bjophthalmol.com
892
Level 1 grader
All pictures graded for all features of retinopathy. Software calculates grade of retinopathy
R0
R1, R2, R3, R4, M1, M2
Level 2 grader
Pictures regraded for all features of retinopathy. Software calculates grade of retinopathy
R0, R1
R2, M1
R6
M2, R3, R4
Level 3 grader
Pictures regraded for all features of retinopathy by ophthalmologist.
Software calculates grade of retinopathy
R0, R1
R2, M1
R6
Refer to ophthalmology
M2, R3, R4
Recall in 12 months
Recall in 12 months
Recall in 6 months
Refer for slit lamp examination
Recall in 12 months
Recall in 6 months
Refer for slit lamp examination
Philip, Cowie, Olson
Figure 1 Outline of the Health
Technology Board for Scotland grading model.
a single 45 ˚ disc/macular field digital image was taken for each eye using a high resolution non-mydriatic digital fundus camera in a darkened room. If the pupils failed physiologically to dilate sufficiently to enable an acceptable image to be obtained, the photograph was repeated at the same visit following mydriasis with tropicamide 1%.
After the grading process, those patients identified as having ungradeable images were invited to attend an additional appointment at the Diabetes Centre, Woolmanhill
Hospital, Aberdeen. There, slit lamp examination, following mydriasis with tropicamide 1%, was undertaken by a level 2 grader.
Table 1 Levels of retinopathy according to the Scottish Diabetic Retinopathy Grading
Scheme 2003
Retinopathy
R0
R1 (mild)
R2 (moderate)
Description
No diabetic retinopathy anywhere
Background diabetic retinopathy (BDR), mild
At least one dot haemorrhage or microaneurysm with or without hard exudates
BDR, moderate
Outcome
Re-screen in 12 months
Re-screen in 12 months
Re-screen in 6 months (or refer to ophthalmology if this is not feasible)
R3 (severe)
Four or more blot haemorrhages (ie, > AH * standard photograph 2a) in one hemifield only. (Inferior and superior hemifields are delineated by a line passing through the centre of the fovea and the optic disc)
BDR, severe
Any of the following features
Four or more blot haemorrhages (ie, > AH * standard photograph 2a) in both inferior and superior hemifields
Venous beading (ie, > AH * standard photograph 6a)
IRMA (ie, > AH * standard photograph 8a)
Refer to ophthalmology
R4 (proliferative) Refer to ophthalmology
R5 (enucleated)
R6
Proliferative diabetic retinopathy
PDR
Any of the following features
New vessel
Vitreous haemorrhage
Enucleated eye
Not adequately visualised
Re-screen 12 months
(other eye)
Technical failure
AH * , Airlie house standard photographs.
14 www.bjophthalmol.com
Impact of HTBS grading model
Table 2 Levels of maculopathy according to Scottish Diabetic Retinopathy Grading
Scheme 2003
Maculopathy
M1 (observable)
M2 (referable)
Description
Lesions within a radius of .
1 but ( 2 disc diameters of the centre of the fovea
Any hard exudates
Lesions within a radius of ( 1 disc diameters of the centre of the fovea
Any blot haemorrhages
Any hard exudates
Outcome
Re-screen in 6 months
(or refer to ophthalmology if this is not feasible)
Refer to ophthalmology
893
Grading
Commercial software (Digital Healthcare, UK) was used for image grading and report generation. All graders identified individual features of retinopathy on the images. The retinopathy grade was automatically calculated according to the Scottish Diabetic Retinopathy Grading System 2003.
8 This was a revised version of the grading scheme recommended by the Health Technology Board for Scotland (tables 1–3).
Level 1 graders graded all images first for image quality and then for retinopathy according to the Scottish Diabetes
Retinopathy Grading System 2003 (table 1–3). Images with any retinopathy or those that were of insufficient quality for grading (technical failure) were passed on to a level 2 grader.
These images were then re-graded and those deemed to have features of referable retinopathy were passed on to a level 3 grader, a consultant in medical ophthalmology. Both level 2 and level 3 graders could final grade ungradeable images
(technical failures). Level 1 and level 2 graders also passed on patients with other significant retinal findings such as retinal vein occlusions and suspicious optic discs. The level 3 grader made the final assessment, confirming or refuting the need for referral to ophthalmology. The level 3 grader also reviewed any images with abnormal features of concern not related to diabetic retinopathy.
Patients with gradeable images stayed within the screening programme unless referred by the level 3 grader to ophthalmology. The final arbiter of referral for patients with ungradeable images was the slit lamp examiner. Patients with coincidental findings of concern were referred to the primary care clinic at the ophthalmology department.
Statistical analysis
Data were analysed using Statistical Package for Social
Sciences (version 11.5.0, SPSS, Chicago, IL, USA). Descriptive data are expressed as mean (SD) or median with 25th and 75th quartiles. The proportions of patients with different outcomes and different grades of retinopathy were calculated with 95% confidence intervals. If a patient had assessment by more than one level of grader then the grade assigned by the highest level of grader was taken as the final result.
Level 2
2124 (38%)
Level 1
3149 (57%)
Figure 2 The grading level at which images were assigned the final grade.
RESULTS
Patient characteristics
Level 3
302 (5%)
Of the 5575 patients, 3066 (55%) were male. The median age of patients screened was 65 (54–73) years. Eighty five per cent of the patients were over the age of 45 and 48.2% over
65. These demographics were almost identical to those of the
Scottish Diabetes Survey 2002.
15
In all, 4742 (85%) patients had screening without mydriasis. Patients whose images were classed as technical failures were then invited for slit lamp examination were older (mean 74.3 (SD 11.2) years) than those with gradeable images (mean 60.5 (15.5) years, p , 0.01). Thirteen patients had only one functioning eye (0.2%).
Grading process and screening outcomes
All 5575 patients had their images reviewed by the level 1 grader. Figure 2 shows the number and proportion of images passed on to the level 2 and level 3 graders. Patients assigned their final screening outcome at each grading level are outlined in tables 4 and 5. Fifty seven per cent of patients were assigned their final grade by the level 1 grader. The
Table 3 Coincidental findings according to Scottish Diabetic Retinopathy Grading
Scheme 2003
Coincidental findings
Photocoagulation
Other
Description
Laser photocoagulation scars present
Other non-diabetic lesion present
Pigmented lesion (naevus)
Age related macular degeneration
Drusen maculopathy
Myelinated nerve fibres
Asteroid hyalosis
Retinal vein thrombosis
Outcome
Not applicable
Refer according to local guidelines www.bjophthalmol.com
894
Table 4 Final screening outcomes at each grading level
Screening outcome Level 1
Re-screening in 12 months
Re-screening in 6 months
3149 (56.5%)
NA
Referral for slit lamp biomicroscopy NA
Referral to ophthalmology NA
Level 2
1368 (24.5%)
107 (1.9%)
649 (11.6%)
NA
NA, not applicable as these outcomes could not be assigned at this level.
Level 3
79 (1.4%)
21 (0.4%)
12 (0.2%)
190 (3.4%)
Total No (%) (95% CI )
4596 (82.4) (81.5 to 83.4)
128 (2.3) (1.9 to 2.7)
661 (11.9) (11.0 to 12.7)
190 (3.4) (3.0 to 3.9)
Philip, Cowie, Olson median time for complete grading was 32 days (22–45). The main delay in grading appeared to occur at the level 1 stage
(median 28 days (21–40)).
The level 1 grader passed on images of 2426 (43.5%) patients to the level 2 grader. Only 302 (5.4%) were subsequently passed on to the level 3 grader, a consultant in medical ophthalmology, for final assessment. At final assessment, the level 3 grader agreed that 190 patients should be referred to ophthalmology services including five patients who had significant non-diabetes pathology (retinal vein occlusions, two; glaucoma, two; large naevus, one). However, for 112 patients the level 3 grader disagreed, recommending that 21 should be re-screened in 6 months, 33 should be rescreened in 12 months, 46 did not have significant nondiabetes pathology, and 12 were ungradeable requiring slit lamp examination. Only 331 (5.9%) patients passed on by the level 1 grader as having any retinopathy were finally downgraded by a higher level grader as having no retinopathy
After final grading, 3485 patients (62.5%) had no retinopathy, while 18 patients (0.3%) had proliferative retinopathy
(table 5). The most frequent cause for referral to ophthalmology services was referable maculopathy (131 patients,
2.3%).
DISCUSSION
This study provides outcome data on the impact of the Health
Technology Board for Scotland’s grading model on referrals to ophthalmology from a primary care based diabetic retinopathy screening programme using digital photography that meets the recommended resolution agreed by both the
Health Technology Board for Scotland and the National
Screening Committee for England.
9 12
The Health Technology Board for Scotland’s grading model appears to be effective in triaging patients needing review by the third level grader. Only 302 (5.4%) patients’ images needed review by the third level grader and, of those, 190
(3.4%) were finally referred to ophthalmology services. Only
10% of the images passed to the level 3 grader were downgraded for review in 12 months. Most errors were caused by the misclassification of referable maculopathy such as misjudging the position of blot haemorrhages or exudates, incorrectly classifying drusen as exudates or mistaking dot haemorrhages for blots haemorrhages.
A major difference between the recommendations for
Scotland and those for England is that in Scotland, patients with ungradeable images requiring slit lamp examination are to be contained within the screening programme, whereas in
England they are to be referred to ophthalmology services. In our study 661 patients (11.9%) required re-invitation for examination by slit lamp biomicroscopy. The reported rates for technical failures in other studies vary from 3.7% to
19.7%.
16–21 In the study by Scanlon et al , the technical failure rate for mydriatic photography was reported as 3.7%; however, a further 15.5% of patients had only ‘‘partially assessable images.’’ 18 Comparisons of technical failure figures are difficult because of a lack of standard image quality assessment protocols; however, our high technical failure rate might be explained by the presence of two new photographers during the study period who were still in their learning phase. Patients were also in their first systematic screening cycle when those who had undiagnosed cataract or other permanent media opacities, might first be encountered. In the second screening cycle these patients would be offered slit lamp examination, if cataract surgery was inappropriate, rather than digital photography, which should lead to a lower photographic technical failure rate.
Furthermore, although high resolution cameras, as recommended by the Health Technology Board for Scotland, have diagnostic advantages, their use of a higher intensity flash compared to that used by lower resolution cameras may result in increased reflections from media opacities increasing the technical failure rate. In addition, the relative quality of the good photographs obtained by high resolution cameras is also better, thus the threshold for rejecting photographs may be higher. Though our technical failure rates are higher than others have documented we think they are realistic for newly established screening programmes. Regardless, provision must be made for those patients with ungradeable images.
In Scotland it has been recommended that this resource be provided within the screening programme, an alternative would be to set up a dedicated clinic within ophthalmology.
Which is more effective has yet to be determined.
Another difference between the Health Technology Board for Scotland and the National Screening Committee recommendations for England is the presence of a 6 monthly rescreening interval for borderline patients (table 4).
9 The
Health Technology Board for Scotland recommended that
Table 5 Overall grades of retinopathy assigned for patients screened
Overall level of retinopathy or maculopathy
R0: No diabetic retinopathy
R1: Mild diabetic retinopathy
R2: Moderate diabetic retinopathy
M1: Observable maculopathy
M2: Referable maculopathy
R3: Severe diabetic retinopathy
R4: Proliferative diabetic retinopathy
R6: Image is of a quality inadequate for grading
Number of patients (%) (95% CI)
3485 (62.5) (61.2 to 63.7)
1116 (20.0) (18.9 to 21.0)
17 (0.3) (0.2 to 0.5)
111 (2) (1.7 to 2.4)
131 (2.3) (2.0 to 2.8)
36 (0.6) (0.5 to 0.9)
18 (0.3) (0.2 to 0.5)
661 (11.9) (11.0 to 12.7) www.bjophthalmol.com
Impact of HTBS grading model 895 patients with ‘‘moderate background retinopathy’’ or ‘‘observable maculopathy’’ could be re-screened at 6 months or referred to ophthalmology services if the screening programme lacked the capacity to contain them within the programme.
12 In our study 128 patients (2.3% (1.9–2.7)) fell into these borderline categories and were re-screened at
6 months thus reducing the impact of the screening programme on ophthalmology services.
There are also differences with respect to classification of diabetic maculopathy. The National Screening Committee for
England recommends that patients with a dot or blot haemorrhage at the macula are referred if they have a visual acuity of worse than or equal to 6/12. Using the National
Screening Committee for England’s criteria this would have resulted in an additional 159 (2.8%) referrals.
The number of patients in our study who needed referral to ophthalmology services was lower than others have suggested and has not yet led to the requirement for any additional resources within ophthalmology services. Using a low resolution digital mydriatic photographic screening method, Scanlon et al had a 12.2% referral rate for patients not already under the care of an ophthalmologist.
18 However, this figure included patients with technical failures in either eye as these patients were not contained within the screening programme. In Liverpool between 1991 and 1999, using colour slide mydriatic photography, a ‘‘high resolution’’ technique, a referral rate of 7.1% was obtained.
22 In
Newcastle using combined mydriatic Polaroid photography and mydriatic direct ophthalmoscopy a referral rate of 4.5% was documented.
23 Our lower referral rate of 3.4% may reflect the effectiveness of previous retinal screening performed at hospital diabetes clinics in Grampian or, alternatively, may reflect different population demographics compared to other studied populations. The population of Grampian is relatively affluent and predominantly white.
24 25 Other ethnic groups are known to be at a higher risk of developing diabetic retinopathy and to have a higher rate of cataract formation.
26–28
It is possible that higher rates of untreated cataract formation will be found in a less affluent population.
29
If all patients with ungradeable pictures are to be referred to ophthalmology, and in addition there is not a 6 month review group, then the National Screening Committee for
England’s prediction of an 8% initial referral rate to ophthalmology services seems low. Furthermore, as the
National Screening Committee for England recommends a two field photographic schedule then it is likely that the technical failure rate will be higher if both photographs need to meet image quality standards.
Ophthalmology time will be required to train retinal screeners to grade before any screening programme can commence. The exact amount and level of training needed is still being debated throughout the four nations. Our experience, based on internal quality assurance by the level
3 grader, suggests that newly appointed level 1 graders with no previous experience of retinal screening can be quickly trained to accurately identify images with no features of retinopathy.
Finally, grading for quality assurance may place a significant burden on ophthalmology services. National
Health Service Quality Improvement Scotland has published diabetic retinopathy screening standards for Scotland that state that ‘‘the images from a minimum of 500 randomly selected patients (or all images graded if less than 500 patients) per grader per annum not otherwise referred to a third level grader are reviewed by a third level grader.’’ 30 As the Grampian Diabetes Retinal Screening Programme has five graders, this equates to 2500 patients (1250 over
6 months) per annum. The National Screening Committee for England recommends that 10% of the normal patients
(348 patients in our study) should be regraded by a second level grader rather than an ophthalmologist.
31 In addition, it recommends that ideally each grader should read a minimum of 1500 and maximum of 4000 patients per annum. National
Health Service Quality Improvement Scotland took the view that until diabetic retinopathy screening programmes had become established and that there were proved training programmes for retinal screeners then this quality assurance would have to be performed by medical retina specialists. In time, however, it is hoped that this burden could be shared by other healthcare professionals.
In conclusion, the Health Technology Board for Scotland’s three level grading model appears to be effective in both triaging patients needing review by the level 3 grader and in minimising the numbers of unnecessary referrals to ophthalmology services. Thus, the impact of the Health Technology
Board for Scotland’s recommendations should be modest, enabling referrals to be contained within existing ophthalmology resources in Scotland.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the invaluable assistance of the retinal screening nurses and the administrative staff of the Grampian
Diabetes Retinal Screening Programme.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
S Philip, L M Cowie, J A Olson, Grampian Diabetes Retinal Screening
Programme, Woolmanhill, Aberdeen AB25 1LD, UK
REFERENCES
1 Bamashmus MA , Matlhaga B, Dutton GN. Causes of blindness and visual impairment in the west of Scotland.
Eye 2004; 18 :257–61.
2 Evans J , Rooney C, Ashwood F, et al.
Blindness and partial sight in England and Wales: April 1990-March 1991.
Health Trends 1996; 28 :5–12.
3 Early Treatment Diabetic Retinopathy Study Research Group .
Photocoagulation for diabetic macular edema. Early Treatment
Diabetic Retinopathy Study report number 1.
Arch Ophthalmol
1985; 103 :1796–806.
4 The Diabetic Retinopathy Study Research Group . Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic
Retinopathy Study (DRS) findings, DRS Report Number 8.
Ophthalmology
1981; 88 :583–600.
5 Foulds WS , McCuish A, Barrie T, et al.
Diabetic retinopathy in the west of Scotland: its detection and prevalence, and the cost-effectiveness of a proposed screening programme.
Health Bull (Edinb)
1983; 41 :318–26.
6 Sculpher MJ , Buxton MJ, Ferguson BA, et al.
Screening for diabetic retinopathy: a relative cost-effectiveness analysis of alternative modalities and strategies.
Health Econ 1992; 1 :39–51.
7 James M , Turner DA, Broadbent DM, et al.
Cost effectiveness analysis of screening for sight threatening diabetic eye disease.
BMJ
2000; 320 :1627–31.
8 Diabetic Retinopathy Screening Implementation Group .
Diabetic retinopathy screening services in scotland: recommendations for implementation .
Edinburgh: Scottish Executive, 2003:69–70.
9 Harding S , Greenwood R, Aldington S, et al.
Grading and disease management in national screening for diabetic retinopathy in England and
Wales.
Diabet Med 2003; 20 :965–971.
10 Lau HC , Voo YO, Yeo KT, et al.
Mass screening for diabetic retinopathy—a report on diabetic retinal screening in primary care clinics in Singapore.
Singapore Med J 1995; 36 :510–13.
11 Peters AL , Davidson MB, Ziel FH. Cost-effective screening for diabetic retinopathy using a nonmydriatic retinal camera in a prepaid health-care setting.
Diabetes Care 1993; 16 :1193–5.
12 Facey K , Cummins E, Macpherson K, et al. Organisation of services for diabetic retinopathy screening , Health Technology Assessment Report 1.
Glasgow: Health Technology Board for Scotland, 2002.
13 Lovie-Kitchin JE . Validity and reliability of visual acuity measurements.
Ophthalmic Physiol Opt 1988; 8 :363–70.
14 Davis MD , Norton EWD, Myers FL. The Airlie classification of diabetic retinopathy. In: Goldberg MF, Fine SL, eds.
Symposium on the treatment of diabetic retinopathy .US Dept of Health, Education and Welfare,
1968:7–37.
15 Scottish Diabetes Survey Monitoring Group .
Scottish Diabetes Survey 2002 .
Edinburgh: Scottish Executive Health Department, 2002:18–19.
16 Olson JA , Strachan FM, Hipwell JH, et al.
A comparative evaluation of digital imaging, retinal photography and optometrist examination in screening for diabetic retinopathy.
Diabet Med 2003; 20 :528–34.
www.bjophthalmol.com
896 Philip, Cowie, Olson
17 Massin P , Erginay A, Ben Mehidi A, et al.
Evaluation of a new non-mydriatic digital camera for detection of diabetic retinopathy.
Diabet Med
2003; 20 :635–41.
18 Scanlon PH , Malhotra R, Thomas G, et al.
The effectiveness of screening for diabetic retinopathy by digital imaging photography and technician ophthalmoscopy.
Diabet Med 2003; 20 :467–74.
19 Herbert HM , Jordan K, Flanagan DW. Is screening with digital imaging using one retinal view adequate ?
Eye 2003; 17 :497–500.
20 Boucher MC , Gresset JA, Angioi K, et al.
Effectiveness and safety of screening for diabetic retinopathy with two nonmydriatic digital images compared with the seven standard stereoscopic photographic fields.
Can J Ophthalmol
2003; 38 :557–68.
21 Agrawal A , McKibbin MA. Technical failure in photographic screening for diabetic retinopathy.
Diabet Med 2003; 20 :777.
22 Younis N , Broadbent DM, Vora JR, et al.
Prevalence of diabetic eye disease in patients entering a systematic primary care-based eye screening programme.
Diabet Med 2002; 19 :1014–21.
23 Pandit RJ , Taylor R. Quality assurance in screening for sight-threatening diabetic retinopathy.
Diabet Med 2002; 19 :285–91.
24 Social Disadvantage Research Centre .
Scottish indices of deprivation index
2003 . Edinburgh: Scottish Executive, 2003:21–28.
25 Office of Chief Statistician .
Analysis of ethnicity in the 2001 census .
Edinburgh: Scottish Executive, 2004:26.
26 Pardhan S , Gilchrist J, Mahomed I. Impact of age and duration on sightthreatening retinopathy in South Asians and Caucasians attending a diabetic clinic.
Eye 2004; 18 :233–40.
27 Mather HM , Chaturvedi N, Kehely AM. Comparison of prevalence and risk factors for microalbuminuria in South Asians and Europeans with type 2 diabetes mellitus.
Diabet Med 1998; 15 :672–7.
28 Das BN , Thompson JR, Patel R, et al.
The prevalence of eye disease in
Leicester: a comparison of adults of Asian and European descent.
J R Soc Med
1994; 87 :219–22.
29 Klein BE , Klein R, Lee KE, et al.
Socioeconomic and lifestyle factors and the 10year incidence of age-related cataracts.
Am J Ophthalmol
2003; 136 :506–12.
30 NHS Quality Improvement Scotland .
Diabetic retinopathy screening clinical standards—March 2004 . Edinburgh: Scottish Executive Health Department,
2004:31.
31 UK National Screening Committee . Essential elements in developing a diabetic retinopathy screening programme. 2004:43
(www.nscretinopathy.org.uk/ resources/FinalWorkbook2doc, accessed 27
May 2004.).
www.bjophthalmol.com
897
SCIENTIFIC REPORT
The effects of indocyanine green and endoillumination on rabbit retina: an electroretinographic and histological study
A K H Kwok, T Y Y Lai, C-K Yeung, Y-S Yeung, W W Y Li, S W Chiang
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :897–900. doi: 10.1136/bjo.2004.061093
Aim: To evaluate the functional and morphological retinal toxicity associated with intravitreal injection of indocyanine green (ICG) dye in rabbit eyes during vitrectomy with endoillumination.
Methods: 20 eyes of 10 New Zealand pigmented rabbits were used in the study. All eyes underwent pars plana vitrectomy and removal of posterior vitreous cortex under endoillumination. In one eye of each rabbit, intravitreal injection of 0.1 ml of 2.5 mg/ml ICG was applied for
30 seconds followed by 10 minutes of endoillumination. The control eye had endoillumination only without ICG injection.
Dark adapted and light adapted electroretinograms (ERGs) were performed before the surgery and 1 week after surgery for serial comparisons. Rabbits were killed 1 week after surgery and eyes were enucleated for histological examination.
Results: Serial ERG comparisons showed significant reduction in the light adapted a-wave amplitude (p = 0.037) and significant delays in the dark adapted and light adapted b-wave latencies (p = 0.020 and p = 0.038, respectively) in the ICG treated eyes. Histological examinations demonstrated loss of photoreceptor outer segments with focal absence of photoreceptors in some areas in the ICG injected eyes.
Conclusions: Vitrectomy followed by intravitreal injection of
2.5 mg/ml ICG for 30 seconds with endoillumination may result in retinal toxicity causing functional and morphological retinal damages in rabbit eyes. The lowest concentration of
ICG should be used if necessary for intraocular use to prevent potential retinal toxicity.
T he use of indocyanine green (ICG) dye to stain the internal limiting membrane (ILM) for its removal during macular hole surgery has been demonstrated to improve the anatomical success rate in macular hole surgery.
1–5
However, clinical studies have also reported adverse effects associated with ICG assisted ILM peeling, resulting in visual field defects and visual impairment.
6–8 Several experimental studies have used cell cultures to investigate the potential retinal toxicity caused by ICG.
9–12 We have previously demonstrated that ICG resulted in a concentration dependent reduction in cell viability and increased expressions of apoptosis related genes p53 and bax as well as the cell cycle arrest protein p21 in human cultured retinal pigment epithelial (RPE) cells.
10 Further studies have similarly shown that high concentrations of ICG caused more reductions in
RPE cell viability.
11 12
Using in vitro cell culture models to study the potential ICG toxicity has the disadvantage of being unable to reproduce the functional and morphological retinal toxicity in vivo.
Animal experiments were therefore performed to evaluate the in vivo retinal toxicity caused by ICG.
13–17 Since ICG related retinal toxicity may be caused by endoillumination during surgery resulting in a photosensitising effect, 18 animals studies on ICG toxicity should include the use of endoillumination in the experiment. The purpose of our study is to investigate the retinal toxicity in rabbit eyes after the application of ICG during vitrectomy with endoillumination through retinal electroretinography and histology.
MATERIALS AND METHODS
Animals
Twenty eyes of 10 New Zealand pigmented rabbits were used in the study. All animals were treated in accordance with the
ARVO statement for the use of animals in ophthalmic and vision research and the protocol was approved by the committee on animal research of The Chinese University of
Hong Kong.
Surgical procedure
The rabbits were anaesthetised with an intramuscular injection of 15 mg/kg xylazine hydrochloride, 50 mg/kg ketamine hydrochloride, and 60 mg/kg sodium pentobarbital.
Both pupils were dilated with 0.5% tropicamide and 0.5% phenylephrine eye drops. Following disinfection with 5% povidone-iodine and draping of the surgical field, standard three port pars plana vitrectomy with removal of the posterior vitreous cortex under endoillumination was performed in all eyes. In the eyes receiving ICG injection, 0.1 ml of 2.5 mg/ml
ICG solution was applied gently over the optic disc with the infusion temporarily stopped. ICG was prepared by diluting
25 mg of commercially available stock ICG powder with the
10 ml solution provided (Diagnogreen Injection, Daiichi
Pharmaceutical, Tokyo, Japan). After 30 seconds, the intravitreal ICG solution was aspirated out with resumption of the infusion solution. Endoillumination was then applied for
10 minutes in eyes with or without ICG injection using a surgical light pipe connected to a tungsten halogen light source (Premiere, Storz Inc, USA). The light pipe was put in the mid-vitreous in order to provide an even illumination to the posterior pole. The sclerotomies and conjunctival wounds were then closed and subconjunctival injection of 5 mg gentamicin was given. Postoperatively, all rabbits received tobramycin ointment twice daily for 1 week.
Electroretinogram recording
Full field electroretinogram (ERG) was performed on all eyes before surgery and 1 week after surgery. All eyes were dilated with 0.5% phenylephrine and 0.5% tropicamide drops and dark adapted for 30 minutes before recordings. Stimuli were delivered by a xenon strobe light mounted on a Ganzfeld dome. Responses were recorded with a computerised recording unit with amplifier filtered at frequencies from 0.5 Hz to
1 kHz (Nicolet Biomedicals, Madison, WI, USA). The rabbits were positioned in front of the dome and Burian-Allen
Abbreviations: ERG, electroretinogram; ICG, indocyanine green; ILM, internal limiting membrane; RPE, retinal pigment epithelium www.bjophthalmol.com
898
A
Control
B
2.5 mg/ml ICG
50 µ V
0 20 40 60 80 100
Time (ms)
120 140 160 180
Control
Kwok, Lai, Yeung, et al
2.5 mg/ml ICG
50 µ V
0 20 40 60 80 100
Time (ms)
120 140 160 180
Figure 1 (A) The dark adapted ERG waveforms and (B) light adapted
ERG waveforms of 2.5 mg/ml ICG treated and control rabbit eyes.
bipolar contact lens electrodes (Hansen Laboratory, Iowa
City, IA, USA) and grounding earclip electrodes were used for recordings. Dark adapted ERG was performed with a white stimulus and a total of eight responses were averaged and light adapted ERG was recorded after light adapting the rabbit for 5 minutes. The responses to 20 bright white flashes at 1 Hz were recorded. The average of the control eyes was taken as 100% and the average of the treated eyes was calculated as the relative percentage of the control eye.
19 To avoid diurnal variation in ERG responses, all ERGs were performed at the same time of day. ERG were analysed by measuring the latency and amplitude of the a-waves and b-waves. The preoperative ERGs and the ERG performed
1 week after surgery were compared using the paired two tailed t test. A p value of > 0.05 was considered statistically significant.
Specimen preparation for light microscopy
Rabbits were killed by an intravenous injection of 120 mg/kg sodium pentobarbital 1 week after surgery and the eyes were enucleated. All eyes were sectioned in half and fixed in 4 ˚ C mixture of 2.5% glutaraldehyde and 4% paraformaldehyde in
0.1 M phosphate buffer at pH 7.4. After fixation, the specimens were stained en bloc with lead citrate, washed three times in 0.1 M phosphate buffer, and serially dehydrated with ethyl alcohol. The specimens were embedded and stained with haematoxylin and eosin for light microscopy.
RESULTS
Electroretinography analysis
Figure 1 shows the dark adapted and light adapted ERG waveforms of the rabbits at 1 week after surgery. There was
Figure 2 (A) Light microscopy of eyes without ICG injection showing preservation of retinal morphology in all layers. (B) Light microscopy of eyes treated with 2.5 mg/ml ICG showing loss of the outer segments of the photoreceptors, focal absence of photoreceptors, and localised areas of RPE irregularities. Focal areas of cellular oedema were also seen in the outer nuclear and inner nuclear layers. (RPE, retinal pigment epithelium; OS, outer segment; IS, inner segment; ONL, outer nuclear layer; OPL, outer plexiform layer; INL, inner nuclear layer; IPL, inner plexiform layer; GCL, ganglion cell layer; NFL, nerve fibre layer.
Haematoxylin and eosin stain, original magnification 6 400.) no difference in the shape of the waveforms recorded in the eyes treated with ICG compared with control eyes. Table 1 demonstrates the ERG results expressed as relative ratios of the ICG treated eyes compared with control eyes. For the dark adapted ERG, no significant changes were observed in the ratios of the a-wave latency, a-wave amplitude, and b-wave amplitude compared with the baseline ERG. However, there was a significant delay in the dark adapted b-wave ERG latency for the ICG treated eyes compared with control after surgery (two tailed t test, p = 0.020). For the light adapted
ERG, there was a significant reduction in the a-wave amplitude and significant increase in the b-wave latency for the ICG treated eyes after surgery (two tailed t test, p = 0.037 and p = 0.038 respectively). No significant changes in the a-wave latency and the b-wave amplitude after surgery were observed.
Light microscopic analysis
In the control eyes without ICG injection, the normal structure of the retina was preserved (fig 2A). However, in eyes that were treated with ICG, localised areas of RPE irregularities could be seen. There were also losses of the outer segments of the photoreceptors together with focal www.bjophthalmol.com
Intravitreal ICG injection in rabbit
Table 1 Results of the dark adapted and light adapted ERG
Baseline
(mean (SEM))
1 week after surgery
(mean (SEM)) ERG component
Dark adapted a-wave latency a-wave amplitude b-wave latency b-wave amplitude
Light adapted a-wave latency a-wave amplitude b-wave latency b-wave amplitude
1.05 (0.01)
1.20 (0.23)
0.98 (0.02)
0.93 (0.03)
0.99 (0.03)
1.35 (0.34)
0.97 (0.02)
1.00 (0.04)
1.01 (0.03)
1.47 (0.37)
1.05 (0.01)
1.00 (0.04)
0.98 (0.04)
0.69 (0.10)
1.05 (0.03)
0.96 (0.10)
* Statistically significant, two tailed t test (n = 20).
p Value
0.18
0.54
0.020
*
0.11
0.87
0.037
*
0.038
*
0.40
899 absence of photoreceptors in some areas (fig 2B). In the outer nuclear and inner nuclear layers, focal areas of cellular oedema with irregularities were detected.
DISCUSSION
Several animal studies have evaluated the potential retinal toxicity of subretinal and intravitreal ICG injections and most studies showed there is a concentration dependent retinal toxicity associated with ICG.
13–17 Maia et al demonstrated that
ERG and histology were normal 1 week after intravitreal injection of 0.5 mg/ml ICG in rabbit eyes, whereas injections of higher concentrations of 5 mg/ml and 25 mg/ml ICG resulted in dark adapted ERG abnormalities.
17 Histological examination also revealed morphological changes in eyes injected with these ICG concentrations. In another experiment, Enaida et al performed gas vitrectomy using 100% SF
6 gas followed by intravitreal ICG injection to evaluate the morphological and functional damage caused by ICG in rat eyes, which showed that ICG injection resulted in functional changes detected on dark adapted b-wave even at a low dose of 0.25 mg/ml.
16 However, since no endoillumination was used in these experiments, the retinal toxicity caused by the potential photosensitising effects of ICG may not be adequately assessed. Furthermore, the injection of ICG in these experiments was not aspirated from the vitreous cavity and the retained ICG might have therefore caused prolonged contact with the retina resulting in toxicity. In the experiment by Maia et al , 17 the concentrations of 5 mg/ml and
25 mg/ml ICG used may also be too high, as the maximum concentration of ICG that is commonly used for macular surgery is 2.5 mg/ml. We therefore decided to investigate the effects of intravitreal injection of 2.5 mg/ml ICG for a short duration of 30 seconds after pars plana vitrectomy, followed by endoillumination in order to reproduce the clinical situation more realistically.
This study demonstrated that intravitreal application of
2.5 mg/ml ICG with endoillumination resulted in significant reduction in the light adapted a-wave amplitude and significant delays in both dark adapted and light adapted b-wave latency compared with control eyes. Morphological changes with loss of photoreceptor outer segments were also seen in ICG treated eyes upon histological examinations.
Both functional and morphological toxicity occurred despite having an ICG contact time of only 30 seconds. Since the light adapted a-wave ERG response mainly originates from the cone photoreceptors, the results suggest that cone photoreceptors may be more susceptible to ICG toxicity. The observed delays in b-wave latencies also suggest that ICG cells. Although, it is unclear whether the ERG changes are reversible, these changes may be transient as Maia et al showed that some of the ERG changes were no longer significant 1 month after intravitreal ICG injection.
17
These results should be interpreted with caution as despite the replication of the surgical method with the use of endoillumination, the experiments still could not mimic the
ICG use in humans during vitrectomy as the vitreous cavity of rabbit eyes is smaller than that of humans, which means a higher concentration of ICG might accumulate in the rabbit eye.
17 This study also has the limitation of investigating only one concentration of ICG and thus is unable to demonstrate the concentration dependent toxicity caused by ICG. Another limitation is the relatively short follow up duration with only one time interval studied after surgery. None the less, in view of the potential retinal toxicity, the minimal concentration of
ICG should be used during surgery if required. Diluting the
ICG solution with balanced salt solution for iso-osmolarity or with dextrose for preparing infracyanine green solution can also reduce the toxicity.
9 Moreover, surgeons may also consider using lower light levels, shorter light exposure, as well as using different wavelengths of light in order to avoid potential clinical toxicity.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
A K H Kwok, T Y Y Lai, C-K Yeung, Y-S Yeung, W W Y Li, S W Chiang,
Department of Ophthalmology and Visual Sciences, The Chinese
University of Hong Kong, Hong Kong Eye Hospital, Hong Kong, People’s
Republic of China
A K H Kwok, Department of Ophthalmology, Hong Kong Sanatorium and Hospital, Hong Kong, People’s Republic of China
Correspondence to: Dr Timothy Y Y Lai, Department of Ophthalmology and Visual Sciences, The Chinese University of Hong Kong, Hong Kong
Eye Hospital, 147K Argyle Street, Kowloon, Hong Kong; tyylai@netvigator.com
Accepted for publication 1 January 2005
REFERENCES
1 Kadonosono K , Itoh N, Uchio E, et al.
Staining of internal limiting membrane in macular hole surgery.
Arch Ophthalmol 2000; 118 :1116–18.
2 Da Mata AP , Burk SE, Riemann CD, et al.
Indocyanine green-assisted peeling of the retinal internal limiting membrane during vitrectomy surgery for macular hole repair.
Ophthalmology 2001; 108 :1187–92.
3 Kwok AK , Lai TY, Man-Chan W, et al.
Indocyanine green staining and removal of retinal internal limiting membrane in stage 3 or 4 macular hole surgery.
Br J Ophthalmol 2003; 87 :71–4.
4 Kwok AK , Lai TY, Yuen KS, et al.
Macular hole surgery with or without indocyanine green stained internal limiting membrane peeling.
Clin
Experiment Ophthalmol 2003; 31 :470–5.
5 Slaughter K , Lee IL. Macular hole surgery with and without indocyanine green assistance.
Eye 2004; 18 :376–8.
6 Haritoglou C , Gandorfer A, Gass CA, et al.
Indocyanine green-assisted peeling of the internal limiting membrane in macular hole surgery affects visual outcome: a clinicopathologic correlation.
Am J Ophthalmol
2002; 134 :836–41.
www.bjophthalmol.com
900 Kwok, Lai, Yeung, et al
7 Uemura A , Kanda S, Sakamoto Y, et al.
Visual field defects after uneventful vitrectomy for epiretinal membrane with indocyanine greenassisted internal limiting membrane peeling.
Am J Ophthalmol
2003; 136 :252–7.
8 Ando F , Sasano K, Ohba N, et al.
Anatomic and visual outcomes after indocyanine green-assisted peeling of retinal internal limiting membrane in idiopathic macular hole surgery.
Am J Ophthalmol
2004; 137 :609–14.
9 Stalmans P , Van Aken EH, Veckeneer M, et al.
Toxic effect of indocyanine green on retinal pigment epithelium related to osmotic effects of the solvent.
Am J Ophthalmol 2002; 134 :282–5.
10 Yam HF , Kwok AK, Chan KP, et al.
Effect of indocyanine green and illumination on gene expression in human retinal pigment epithelial cells.
Invest Ophthalmol Vis Sci 2003; 44 :370–7.
11 Ho JD , Tsai RJ, Chen SN, et al.
Cytotoxicity of indocyanine green on retinal pigment epithelium: implications for macular hole surgery.
Arch Ophthalmol
2003; 121 :1423–9.
12 Rezai KA , Farrokh-Siar L, Ernest JT, et al.
Indocyanine green induces apoptosis in human retinal pigment epithelial cells.
Am J Ophthalmol
2004; 137 :931–3.
13 Lee JE , Yoon TJ, Oum BS, et al.
Toxicity of indocyanine green injected into the subretinal space: subretinal toxicity of indocyanine green.
Retina
2003; 23 :675–81.
14 Kawaji T , Hirata A, Inomata Y, et al.
Morphological damage in rabbit retina caused by subretinal injection of indocyanine green.
Graefes Arch Clin Exp
Ophthalmol 2004; 242 :158–64.
15 Maia M , Kellner L, de Juan E Jr, et al.
Effects of indocyanine green injection on the retinal surface and into the subretinal space in rabbits.
Retina
2004; 24 :80–91.
16 Enaida H , Sakamoto T, Hisatomi T, et al.
Morphological and functional damage of the retina caused by intravitreous indocyanine green in rat eyes.
Graefes Arch Clin Exp Ophthalmol 2002; 240 :209–13.
17 Maia M , Margalit E, Lakhanpal R, et al.
Effects of intravitreal indocyanine green injection in rabbits.
Retina 2004; 24 :69–79.
18 Haritoglou C , Gandorfer A, Schaumberger M, et al.
Light-absorbing properties and osmolarity of indocyanine-green depending on concentration and solvent medium.
Invest Ophthalmol Vis Sci 2003; 44 :2722–9.
19 Jaffe GJ , Yang CH, Guo H, et al.
Safety and pharmacokinetics of an intraocular fluocinolone acetonide sustained delivery device.
Invest
Ophthalmol Vis Sci 2000; 41 :3569–75.
www.bjophthalmol.com
901
SCIENTIFIC REPORT
Microglial stability and repopulation in the retina
T A Albini, R C Wang, B Reiser, E Zamir, G S Wu, N A Rao
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :901–903. doi: 10.1136/bjo.2004.060293
Background/aims: Parenchymal central nervous system microglia are repopulated by bone marrow derived monocytes more slowly than any other reticuloendothelial cells. The contribution of bone marrow derived monocytes to the uninflammed retina has not been studied. The present study sought to determine repopulation of retinal microglia in uniflammed retina by bone marrow derived monocytes in bone marrow chimeric rats.
Methods: Chimeric (Y R X) Lewis rats were constructed by transplanting 5 6 10 7 male bone marrow cells into lethally irradiated female recipient rats. The chimeras were sacrificed
8, 10, 12, 30, and 52 weeks after bone marrow transplant, and retina, brain, lung, and spleen samples were collected.
DNA was extracted and quantified. Y positive infiltrating cells in the collected samples were detected by polymerase chain reaction amplification of a Y chromosome specific 104 bp fragment.
Results: There was a rapid repopulation of haematopoietic tissues in the spleen (at 8 weeks), confirming the establishment of chimerism, and to a lesser extent, of lung (at
30 weeks). This repopulation was absent in the brain parenchyma and retina until 52 weeks after transplantation.
Conclusions: These data indicate that resident microglia in the retina, much like those in the brain, are stable in number in the retinal compartment (up to 1 year), and repopulation by bone marrow derived cells may be delayed for a year.
M icroglia are resident monocytes in the retina and central nervous system (CNS), functionally similar to macrophages. In retinal tissue, microglia can be distinguished from macrophages primarily by morphological features and perivascular distribution. These cells have long been known to have a reactive role in response to local tissue injury or degeneration. Growing evidence suggests an active proinmflammatory role for microglia as well. Resident microglia play an active proinflammatory part in the CNS in several experimental and clinical diseases, including experimental autoimmune encephalomyelitis, cerebrovascular disease, Alzheimer’s disease, HIV encephalopathy, and multiple sclerosis.
1–4 Although there is no direct evidence that retinal microglia are potent antigen presenting cells in vivo, retinal microglia express phenotypic markers of antigen presenting cells in vitro.
5 In experimental autoimmune uveitis (EAU) microglia migrate to the photoreceptor cell layer and generate TNF a and peroxynitrite early in the course of disease, before macrophage infiltration.
6
Monocyte precursor cells are thought to move to the CNS and the retina during embryonic life and the early postnatal period. There, these precursor cells transform into mature resting microglia of normal CNS and retinal tissue.
7 8 As a consequence of inflammation or other tissue damage, bone marrow derived monocytes commonly invade the CNS or retina. In healthy CNS and retina, renewal of microglial populations may be accomplished by in situ proliferation of resident microglia. Alternatively, bone marrow derived macrophages may slowly migrate to healthy CNS or retinal tissue and transform into resident microglia. The mechanism of microglial renewal is not clearly understood in the CNS.
Some CNS monocytes, primarily meningeal microglia and perivascular dendritic cells, may be slowly replaced by bone marrow derived monocytes.
9 10 In contrast, parenychymal
CNS microglia have been thought to be renewed predominantly by in situ proliferation of resident microglia. However, one recent study of CNS parenchymal microglia found that these cells may also be repopulated by bloodborne monocytes after peripheral nerve axotomy.
11 The authors conclude that parenchymal microglia are wanderers between the peripheral immune system and the CNS. The mechanism of microglial renewal in the retina is not well described.
To test the hypothesis that retinal microglia are predominantly derived from resident microglia and not from bone marrow derived monocytes, we used a chimeric model of male Lewis rat bone marrow transplanted to lethally irradiated female Lewis rats. Immunohistochemistry or in situ hybridisation of Y chromosome gene product from serial sections may not be sufficiently sensitive to detect small numbers of bone marrow derived cells in this chimeric model. Therefore we assayed retinas, brain, lung and spleen by polymerase chain reaction (PCR) for a Y chromosome gene product at various time intervals after transplantation to determine if any bone marrow derived cells had established residence in these organs. Since monocytes would be the principal—if not only—infiltrating bone marrow derived cells in the uninflamed retina and CNS, the presence of Y chromosome gene product indicates infiltration of bone marrow derived monocytes into the retina. In a previous experiment, 6 we found that Y chromosome gene product could not be detected in the retinas of bone marrow chimeric
Lewis rats. Here, we expand these data in animals surviving for 1 year after bone marrow transplant.
MATERIALS AND METHODS
Lewis rats weighing 150—175 g (Charles River Laboratory,
Wilmington, MA, USA) were used in all studies. Ten chimeric
(Y R X) rats were constructed according to a previously described protocol.
6 Briefly, bone marrow removed from the tibia, femur, and humerus of the male donor rats was passed through a density gradient medium (Ficoll-Paque Plus;
Amersham Pharmacia Biotech, Piscataway, NJ, USA) to remove red blood cells and cell debris. The cells were washed with RPMI 1640 (Gibco BRL, Rockville, MD, USA) supplemented with 10% fetal bovine serum. Female rats were irradiated with 1000 rads by a caesium-135 gamma irradiator
(Gamma Cell-40; Atomic Energy of Canada, Ltd, Ottawa,
Ontario, Canada) and then given intracardiac injections of
5 6 10
7 bone marrow cells in 1.0 ml Hanks’ balanced salt solution.
Abbreviations: CNS, central nervous system; EAU, experimental autoimmune uveitis www.bjophthalmol.com
902 Albini, Wang, Reiser, et al
Table 1 Detection of Sry (Y chromosome) gene product by PCR in solid organs harvested from two bone marrow chimeric
(Y R X) Lewis rats for each of five time points after bone marrow transplant
Spleen
Lung
Right retina
Left retina
Brain
8 weeks
+ / +
2 / 2
2 / 2
2 / 2
2 / 2
12 weeks
+ / +
2 / 2
2 / 2
2 / 2
2 / 2
15 weeks
+ / +
2 / 2
2 / 2
2 / 2
2 / 2
30 weeks
+ / +
+ / +
2 / 2
2 / 2
2 / 2
52 weeks
+ / +
+ / +
2 / 2
+ / +
+ / +
Detection of gene product by PCR is denoted with a plus or minus for each animal. Thus, ‘‘ + / 2 ’’ denotes detection of Sry in the first animal, but not the second.
There was a rapid repopulation of the spleen (at 8 weeks) and, to a lesser extent, lung (at 30 weeks) in Y R X bone marrow transplantation. This repopulation was absent in the brain parenchyma and retina until 52 weeks after transplantation.
Two rats were killed at each time point: 8, 10, 12, 30, and
52 weeks after bone marrow transplantation. The animals were perfused with normal saline to remove any intravascular circulating cells. The retinas from each animal were used independently, yielding two retinal samples from each animal.
Retinal DNA was extracted (Easy-DNA kit;
Invitrogen, Carlsbad, CA, USA), and the pellet was dissolved in 50 m l TRIS EDTA and quantified by 260 nm absorption.
Exactly 1 m g DNA was used for polymerase chain reaction
(PCR). Similarly, DNA samples from the spleen, lungs, and brain were obtained and quantified.
As previously decribed, 6 PCR amplification for 35 cycles of a 104 bp segment of the murine Sry gene (the sex determining region of the Y chromosome) encoded by genomic DNA isolated from harvested organs was performed using the following pair of primers: 5 9 -CATCGAAGGGTTAAAGTGCCA-
3 9 (5 9 primer) and 5 9 -ATAGTGTGTAGGTTGTTGTCC-3 9 (3 9 primer). A previously published experiment established the sensitivity of this method for detecting the presence of 104 bp fragments of male DNA: this PCR protocol detected 1 ng of male DNA in 1 m g of female DNA (0.1%) and could detect
0.01% male cells (1:10 000) in the mixture of male and female cells.
6
RESULTS
Confirming the establishment of chimerism, PCR showed the presence of Y chromosome murine Sry gene product in spleens harvested from chimeric (Y R X) Lewis rats 8 weeks after bone marrow transplantation, as well as at every time point thereafter (table 1).
Sry was not detected in the lungs of chimeric rats 8, 10, or 12 weeks after establishment of chimerism; but Sry was detected in the lungs of chimeric rats at 30 weeks and 52 weeks.
Sry could not be detected in retinas and brains of chimeric rats 8, 10, 12, or 30 weeks after bone marrow transplantation. However, the retina of one eye from each animal did show the presence of Sry at 52 weeks, as did the brain (fig 1)
2
O (– control)
Male Lewis DNA (+ control)
Figure 1 PCR amplification for 35 cycles of a 104 bp segment of the murine Sry gene (the sex determining region of the Y chromosome) from
DNA extracted from organs of a bone marrow chimeric (Y R X) Lewis rat
52 weeks after bone marrow transplant. The 104 bp product is detected in the lung, spleen, brain, and left retina.
DISCUSSION
The origin of microglia in the CNS has been a focus of debate.
However, the current prevailing view is that macrophage-like cells, presumably derived from mesodermal cells belonging to haematopoietic lineage, invade the brain parenchyma during embryonic development.
12–14 Similarly, retinal microglia are the only bone marrow derived cells in the healthy retina when there is no infiltration or extravasation of bloodborne cells. Bone marrow chimeric (Y R X) animals make it possible to use PCR for Y chromosome gene product to detect bone marrow derived cells in the retina with great sensitivity. This study shows that in the absence of inflammation, the retina and brain in bone marrow chimeric rats remains free of bone marrow derived cells for up to one year. This fact could be exploited to better characterise infiltrating cells in inflammatory reactions such as EAU.
PCR is a highly sensitive technique with some limitations.
We have demonstrated that PCR allows for detection of Y chromosome gene product of a single XY cell in 10 000 XX cells.
6 Assuming that 2% of retinal cells are microglia, we should be able to detect Y chromosome gene product when as few as 0.5% of the microglia in the retina carry Y chromosomes. Not all positive amplification for Y gene product represents microglia; the presence of passenger leucocytes cannot be absolutely excluded despite saline perfusion of the animals before harvest of organs. Retinal stem cells or other mesenchymal cells are known migrate into the retina during embryonic development and may migrate into the adult uninflamed retina, although to the best of our knowledge adult migration has not been shown. Also, we cannot conclude that absolutely no bloodborne cells are present in retina and brain before 52 weeks; we may miss fewer than one bloodborne cell in 10 000 cells. Nevertheless, we conclude that for at least 30 weeks after the establishment of chimerism, less than 0.5% of microglia are newly derived from the bone marrow. Interestingly, the retina of only one eye from each animal showed the presence of Sry at
52 weeks (fig 1) Since unilateral detection of Sry was seen in two animals and confirmed for both animals on two repeat runs of PCR, we do not think this represents a false positive.
Alternatively, this may reflect numbers of infiltrating bloodborne cells in the retina at the threshold of yielding positive
PCR.
Bone marrow chimera models are particularly useful for distinguishing resident microglia from newly infiltrating macrophages in retinal inflammation since there are no generally accepted helpful immunohistochemical markers to make this distinction. PCR technology and in situ hybridisation may make it possible to quantify and localise infiltrating cells; however this study sought to describe the relative rate of migration of bloodborne cells into the uninflammed retina, and therefore only the most sensitive technique was used— that is, PCR. Confirmatory in situ hybridisation was likely to yield a false negative result because of the probable low www.bjophthalmol.com
Microglial stability in the retina 903 number of bloodborne cells present in any given tissue section.
Finally, this study confirms the similarity in stability of microglial populations in the brain and retina. In previous studies using bone marrow chimeric rats to characterise CNS microglial turnover, parenchymal microglia were found to be stable 1 year after bone marrow transplantation. In these studies, meningeal monocytes, and to a lesser extent perivascular CNS microglia, were replaced by bone marrow derived cells more quickly.
9 This was quantified in a study by
Kennedy and Abkowitz 15 : 1 month after transplantation, 89% of the donor cells were detected in the spleen; after 1 year,
61% were detected in lung and 30% in perivascular and leptomeningeal sites, but not in the parenchyma of the brain.
The retinal microglia were not studied. Since there are fewer parenchymal microglia in the retina than in the brain, it was unclear how quickly the predominantly perivascular retinal microglia would be replaced by bone marrow derived monocytes. This study shows that retinal microglia do not turn over quickly and suggests that, like CNS microglia, retinal microglia remain inactivated behind the blood-retina barrier for long periods of time and are uniquely adapted, in contradistinction to other tissue resident macrophages. This study also confirms that as in the CNS, bone marrow derived cells do not typically cross the blood-retina barrier in the healthy retina.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
T A Albini, R C Wang, B Reiser, E Zamir, G S Wu, N A Rao, Doheny Eye
Institute, Keck School of Medicine, University of Southern California, Los
Angeles, CA, USA
Supported in part by National Eye Institute Grant EY013253 and core grant 3040 from the National Institutes of Health, Bethesda, Maryland, and unrestistricted grant from Research to Prevent Blindness, New York,
NY, USA.
Correspondence to: Narsing A Rao, Doheny Eye Institute, DVRC 211,
1450 San Pablo Street, Los Angeles, CA 90033, USA; nrao@usc.edu
Accepted for publication 14 December 2004
REFERENCES
1 Barger SW , Harmon AD. Microglial activation by Alzheimer amyloid precursor protein and modulation by apolipoprotein E.
Nature
1997; 388 :878–81.
2 McGeer PL , Itagaki S, Boyes BE, et al.
Reactive microglia are positive for HLA-
DR in the substantia nigra of Parkinson’s and Alzheimer’s disease brains.
Neurology 1988; 38 :1285–91.
3 Price RW , Brew B, Sidtis J, et al.
The brain in AIDS: central nervous system
HIV-1 infection and AIDS dementia complex.
Science 1988; 239 :586–92.
4 Sriram S , Rodriguez M. Indictment of the microglia as the villain in multiple sclerosis.
Neurology 1997; 48 :464–70.
5 Matsubara T , Pararajasegaram G, Wu GS, et al.
Retinal microglia differentially express phenotypic markers of antigen-presenting cells in vitro.
Invest Ophthalmol Vis Sci 1999; 40 :3186–93.
6 Rao NA , Kimoto T, Zamir E, et al.
Pathogenic role of retinal microglia in experimental uveoretinitis.
Invest Ophthalmol Vis Sci 2003; 44 :22–31.
7 Barron KD . The microglial cell. A historical review.
J Neurol Sci
1995; 134 (Suppl):57–68.
8 Chen L , Yang P, Kijlstra A. Distribution, markers, and functions of retinal microglia.
Ocul Immunol Inflamm 2002; 10 :27–39.
9 Lassmann H , Hickey WF. Radiation bone marrow chimeras as a tool to study microglia turnover in normal brain and inflammation.
Clin Neuropathol
1993; 12 :284–5.
10 Lassmann H , Schmied M, Vass K, et al.
Bone marrow derived elements and resident microglia in brain inflammation.
Glia 1993; 7 :19–24.
11 Flugel A , Bradl M, Kreutzberg GW, et al.
Transformation of donor-derived bone marrow precursors into host microglia during autoimmune CNS inflammation and during the retrograde response to axotomy.
J Neurosci Res
2001; 66 :74–82.
12 Eglitis MA , Mezey E. Hematopoietic cells differentiate into both microglia and macroglia in the brains of adult mice.
Proc Natl Acad Sci USA
1997; 94 :4080–5.
13 Ling EA , Wong WC. The origin and nature of ramied and amoeboid microglia: a historical review and current concepts.
Glia 1993; 7 :9–18.
14 Santambrogio L , Belyanskaya SL, Fischer FR, et al.
Developmental plasticity of
CNS microglia.
Proc Natl Acad Sci USA , 2001; 98 :6295–300.
15 Kennedy DW , Abkowitz JL. Kinetics of central nervous system microglial and macrophage engraftment: analysis using a transgenic bone marrow transplantation model.
Blood 1997; 90 :986–93.
www.bjophthalmol.com
904
EXTENDED REPORT
TLRs and NODs mRNA expression pattern in healthy mouse eye
S Rodrı´guez-Martı´nez, M E Cancino-Dı´az, L Jime´nez-Zamudio, E Garcı´a-Latorre, J C Cancino-Dı´az
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :904–910. doi: 10.1136/bjo.2004.056218
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Dr Juan Carlos Cancino-
Dı´az, Departamento de
Microbiologı´a,
Laboratorio de
Microbiologı´a General,
Escuela Nacional de
Ciencias Biolo´gicas,
Carpio y Plan de Ayala s/n, Me´xico, DF, 11340,
Me´xico; jccancinodiaz@ hotmail.com
Accepted for publication
1 December 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aims: To look for TLR and NOD mRNA expression in the healthy eye and in other immune privileged and non-immune privileged mouse organs.
Methods: Semiquantitative RT-PCR was performed to look for TLR1–9 and NOD1 and NOD2 mRNA expressions in the whole eye, in the anterior (AP) and posterior (PP) portions of the eye, in corneal fibroblasts (CF) and in ovary, brain, testis, heart, lung, and spleen.
Results: All the TLR mRNAs were expressed in the whole eye of Balb/c mice. NIH and C57BL/6 did not express TLR9 and TLR8, respectively. NIH expressed higher levels of TLR1, 2, 3, and 6 than the other strains. C57BL/6 expressed the lowest levels of all TLRs. TLR9, 5, and 4 were the less expressed in all strains. All TLRs were expressed in Balb/c PP and TLR1 was not expressed in AP. In NIH and Balb/c CF the majority of TLRs were overexpressed with LPS. In testis, expression of most TLRs was absent. Non-immune privileged organs expressed most of the TLRs. All the organs expressed NOD1 and NOD2. In PP NOD2 was not expressed.
Conclusion: TLRs and NODs are expressed in the eye, and could have an important role in the innate immunity.
T he eye is considered an immunologically privileged organ because it can accept corneal transplantation and by the presence of immunosuppressors. This means that intraocular inflammation, which could interfere with the transparency needed to preserve the vision, is self limited. The immune privilege is in part the result of what has been called anterior chamber immune deviation (ACAID).
1 It has been demonstrated that the aqueous humour contains immunosuppressors and immunomodulators 2 3 that inhibit T cell activation. It has been suggested that transforming growth factor (TGF) b 2 is the main agent in this process, with interleukin 6 (IL-6) as an antagonist and modulator.
4–6 In experimental ocular inflammation induced by LPS, the immune suppressive properties of the aqueous humour are lost.
7
The innate immunity is the first line of defence in the host and limits the infection during the first hours after the exposure to micro-organisms. Innate immunity recognises molecular structures of the micro-organism called ‘‘pathogen associated molecular patterns’’ (PAMPs) through the pattern recognition receptors (PRRs). The PRRs are expressed in cells of the innate immune system, including those that function as antigen presenting cells (APC) in the adaptive immunity.
8
The toll-like receptors (TLRs) and the nucleotide binding oligomerisation domain (NOD) proteins are PRRs involved in the recognition of multiple microbial products.
9 10 The TLRs are transmembrane receptors with an extracellular domain, involved in the recognition of the PAMP ligand and with an intracellular domain called TLR/IL-1 receptor (TIR), essential for the signal transduction that drives the activation of the nuclear factor kappa B (NFk B).
11 12 The NOD proteins is a family of cytosolic proteins that also has been implicated in the recognition of bacteria and in the induction of inflammatory response.
10 13
The expression of the TLRs and NODs in the eye has been scarcely studied. Recent reports only indicate that TLR4 is expressed in human cornea 14 and in APC of uvea, 15 and that
TLR5 binds Pseudomonas aeruginosa flagellin in corneal epithelium.
16 We propose that these molecules could be expressed in the eye and could have an important role in its innate immunity. In this work, we studied the expression of the TLR and NOD molecules in the healthy eye and other organs from three different mouse strains.
METHODS
Animals
Balb/c, C57BL/6, and NIH mice were used. All the mice were healthy, 4–6 weeks old, and did not present any ophthalmological alterations. The experimental protocols were performed in accordance to the Instituto de Oftalmologı´a, animals in ophthalmic and vision research.
Organs
Mice were killed by cervical dislocation. Eyes, testis, ovary, brain (immune privileged organs), and spleen, lung, and heart (non-immune privileged organs) were obtained from each mouse.
To analyse different portions of ocular tissues we obtained the eyes by enucleation and the eye was cut in two portions.
The anterior portion (AP) contained corneal tissues and the posterior portion (PP) contained all the other tissues of the eye.
Culture of primary corneal fibroblasts
NIH and Balb/c corneas were digested with 24 U of dispase solution (Invitrogen, Carlsbad, CA, USA) at 37 ˚ C for 4 hours, followed by 10 minutes of digestion with trypsin-EDTA
(Invitrogen) at 37 ˚ C. After being washed with DMEM, the cells were resuspended in DMEM (150 000 cells/ml) containing 5% of FBS (Gibco, Rockville, MD, USA), gentamicin, and
Abbreviations: ACAID, anterior chamber immune deviation; AP, anterior portion; APC, antigen presenting cells; CF, corneal fibroblasts;
IL, interleukin; LPS, lipopolysaccharide; NOD, nucleotide binding oligomerisation domain protein; PAMPs, pathogen associated molecular patterns; PP, posterior portion; PRRs, pattern recognition receptors; RT-
PCR, reverse transcriptase polymerase chain reaction; TGF, transforming growth factor; TIR, TLR/IL-1 receptor; TLRs, toll-like receptors www.bjophthalmol.com
TLRs and NODs mRNA expression pattern in healthy mouse eye
Table 1 Primer sequence
TLR5
TLR6
TLR7
TLR8
TLR9
TLR1
TLR2
TLR3
TLR4
NOD1
NOD2 b actin
Primer sequence
Sense: 5 9 -GGACTTCCACATGTCTCCACTATCC-3 9
Anti-sense: 5 9 -TCCATGCTTGTTCTTCTCTGTGG-3 9
Sense: 5 9 -GTGGTACCTGAGAATGATGTGGG-3 9
Anti-sense: 5 9 -GTTAAGGAAGTCAGGAACTGGGTG-3 9
Sense: 5 9 -AGGTACCTGAGTTTGAAGCGAGC-3 9
Anti-sense: 5 9 -GAGCATCAGTCTTTGAAGGCTGG-3 9
Sense: 5 9 -CTGGGTGAGAAATGAGCTGG-3 9
Anti-sense: 5 9 -GATACAATTCCACCTGCTGCC-3 9
Sense: 5 9 -TATCTCCCTGTTCTTCAGACGGC-3 9
Anti-sense: 5 9 -TGGTTGCCAGATAGGTCTAAGCG-3 9
Sense: 5 9 -TTAACTGACCTTCCTGGGTGTGG-3 9
Anti-sense: 5 9 -GCAGAACAGTATCACAGGACAGTGG-3 9
Sense: 5 9 -CAAACTTCTGTAGACCGTCATGGG-3 9
Anti-sense 5 9 -AAGTACCGCAACTCTCTCAACGG-3 9
Sense: 5 9 -GTTATGTTGGCTGCTCTGGTTCAC-3 9
Anti-sense: 5 9 -TCACTCTCTTCAAGGTGGTAGC-3 9
Sense: 5 9 -GACTTACTGTTGGAGGTGCAGACC-3 9
Anti-sense: 5 9 -GAACACCACGAAGGCATCATAGG-3 9
Sense: 5 9 -AGCTGCAGCCTTGCTTTAGCC-3 9
Anti-sense: 5 9 -TCAGCCATAAATGCCGTAGCG-3 9
Sense: 5 9 -CCGAAGCCCTAGCACTGATGC-3 9
Anti-sense: 5 9 -CAACCATCACGACTCCTCGGG-3 9
Sense: 5 9 -TGGAATCCTGTGGCATCCATGAAAC-3 9
Anti-sense: 5 9 -TAAAACGCAGCTCAGTAACAGTCCG-3 9
547
476
324
249
410
308
300
Amplified segment
(pb)
596
541
489
203
313
905 fungizone. The corneal fibroblasts (CF) were cultured overnight in 25 cm
2 flasks; the medium with non-attached cells was discarded and the incubation was continued in new medium, which was changed every 3 days, until 90% of confluence was achieved.
17 The CF were treated with LPS
(10 m g/ml) in fresh DMEM medium for 3 or 6 hours. The total RNA was obtained with TRIzol reagent (Invitrogen).
RNA isolation and RT-PCR analysis
All the organs were washed in D-PBS to eliminate blood contamination. Total RNA extraction was performed with
TRIzol reagent. Total RNA was treated with free RNAse-
DNAse I and RNA was re-extracted with TRIzol reagent. For the reverse transcriptase (RT) reaction, total RNA (3 m g) with
0.5
m g of oligo-(dT)
15-18
(Invitrogen) was denatured at 70 ˚ C for 10 minutes. Then, 1X single strand buffer, 0.5 mM DTT,
500 m M of each dNTPs and 200U of MMLV reverse transcriptase (Invitrogen) were added. The RT reactions were performed at 42 ˚ C for 1 hour. The polymerase chain reactions
(PCR) were performed with 1 m l of the cDNA, 1X buffer,
1 mM MgCl
2
, 200 m M of each dNTPs, and 0.2
m M of each
TLR, NOD, and b actin specific primers (table 1). Optimal
PCR conditions were 30 cycles of 30 seconds at 92 ˚ C,
30 seconds at 60 ˚ C, and 30 seconds at 72 ˚ C.
Semiquantitative PCR
The intensity of the amplified bands was analysed with the
Alpha Imager software. The band intensities were normalised with the corresponding b actin signal (TLR/ b actin or NOD/ b actin rate). These results were analysed by the Kruskal-Wallis statistical test.
RESULTS
Expression of TLRs mRNA in the eye of Balb/c, C57BL/
6, and NIH mice
Expression analysis of each TLR (TLR1–9) mRNA in the healthy eye of the studied mouse strains was performed.
Balb/c mice expressed all the TLRs, whereas NIH and C57BL/6 mice did not express the TLR9 and TLR8, respectively, and
TLR5 was only expressed in 20% of the NIH mice (fig 1). In
500
400
300
200 bp
500
400
300
200
500
400
300
200
M 1 2 3 4 5 6 7 8 9 A
NIH
Balb/c
C57B/6
Figure 1 Expression of TLR mRNAs in the healthy eye of three mouse strains. RT-PCRs were performed in the eyes of NIH, Balb/c and C57BL/
6 mice. Lane M corresponds to 100 bp molecular ladder; lanes 1–9 correspond to mRNA expression of TLRs1-9, respectively, and lane A to b actin expression.
order to quantify the expression of the TLRs, we performed a semiquantitative analysis of the RT-PCR products using the b actin as housekeeping gene. Figure 2 shows the median (SD) of the TLRs expression levels (TLR/ b actin expression) in the three mouse strains studied. We found that in the eye of the
NIH mice, levels of TLR1, 2, 3, and 6 were higher than in
Balb/c and C57BL/6 (p , 0.05). C57BL/6 mice always presented the lowest expression levels of TLRs. Among all the
TLRs, TLR9, 5, and 4, were the less expressed, and TLR2, 6, 1, and 3 were highly expressed in the eye of the three mouse strains studied.
www.bjophthalmol.com
906 Rodrı´guez-Martı´nez, Cancino-Dı´az, Jime´nez-Zamudio, et al
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
NIH
NIH
TLR1
Balb/c
TLR4
Balb/c
TLR7
C57
C57
NIH Balb/c C57
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
NIH
NIH
TLR2
Balb/c
TLR5
Balb/c
TLR8
C57
C57
NIH Balb/c C57
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
NIH
NIH
TLR3
Balb/c
TLR6
C57
Balb/c
TLR9
C57
NIH Balb/c C57
Figure 2 Intensity of mRNA expression of TLRs in the eye of mice.
The intensity of each band of figure 1 was measured in an Alpha Imager system. Each bar corresponds to the median value (SD) of the relation TLR/ b actin mRNA expression in the whole eye of 10 NIH mice, five Balb/c mice, and five C57BL/6 mice, respectively.
Horizontal lines show statistical difference (p , 0.05) according to the
Kruskal-Wallis test.
To explore the TLR expression in the eye regions that could be considered with and without immune privilege we worked with the AP and PP of Balb/c mice, respectively. All the TLRs were expressed in both portions, except for TLR1 in the AP
(fig 3A).
Expression of TLRs mRNA in corneal fibroblast from
Balb/c and NIH mice
In CF from Balb/c mice only TLR1 and TLR3 were not expressed and in CF from NIH mice no TLR was expressed, but the LPS induced the overexpression of all TLRs in CF
A
500
400
300
200
500
400
300
200
500
400
300
200
M 1 2 3 4 5 6 7 8 9 A
AP
PP
CF
B
β act
TLR1
TLR2
TLR3
TLR4
TLR5
TLR6
TLR7
TLR8
TLR9
0
Balb/c
3 6 0
NIH
3 6
Figure 3 Expression of TLR mRNAs in different compartments of the eye.
(A) RT-PCRs were performed in anterior portion (AP), posterior portion (PP), and corneal fibroblasts (CF) from a pool of
16 Balb/c mice eyes. In each gel image, lane M corresponds to 100 bp molecular ladder, lanes 1–9 correspond to mRNA expression of
TLRs1-9, respectively, and lane A to b actin expression. (B) RT-PCRs were performed on TLR1-9 in corneal fibroblast of Balb/c and NIH mice treated at 0, 3, and 6 hours with LPS
(10 m g/ml).
www.bjophthalmol.com
TLRs and NODs mRNA expression pattern in healthy mouse eye 907 from Balb/c and TLR1, 2, 3, 4, 5, 6, and 7 in NIH mice.
C57BL/6 CF were not assayed (fig 3B).
Expression of TLRs mRNA in immune privileged and non-immune privileged organs
TLR expression was analysed in other organs: immune privileged (brain, testis, and ovary) and in non-immune privileged (spleen, lung, and heart). As can be seen in figure 4, all the TLRs were expressed in the ovary of the three strains studied. In contrast, in the testis of the three strains studied; only TLR2 and 8 were found. TLR2, 3, 6, and 9 were expressed in Balb/c mice brain; C57BL/6 mice brain also expressed TLR2, 3, 6 and 9, as well as TLR5. NIH mice brain expressed most of the TLRs except TLR3, TLR8, and TLR9.
In the non-immune privileged organs, all the TLRs were expressed in at least one of the strains, except TLR1 which was absent in the heart of the three strains (fig 4).
Expression of NODs mRNA
The mRNAs of the NOD1 and NOD2 molecules were found in the whole eye of the three studied strains, but NOD1 expression was higher than NOD2 in NIH and Balb/c mice.
In C57BL/6 mice, NOD1 and NOD2 were expressed with similar intensity (fig 5A and 5B). In the AP and in the CF from Balb/c mice, NOD1, and NOD2 were expressed, and again, NOD1 with higher intensity. However in the PP, NOD2 was not expressed (fig 5C). NOD1 and NOD2 were expressed in all the immune privileged and non-immune privileged organs assayed, and as in the eye, NOD1 expression was higher than NOD2 (fig 6).
DISCUSSION
In this work, we studied the mRNA expression of TLRs and
NODs in the eyes of three different mouse strains, as we suppose that the innate immunity molecules could be playing an important part in the ocular transparency, providing protection against pathogenic agents, thus avoiding inflammation.
We found all the TLRs were expressed in the healthy eye of
Balb/c mice; only TLR9 and TLR8 were not expressed in NIH and C57BL/6 mice, respectively. These results suggest that these molecules may have a protecting role in the healthy eye by limiting a possible ocular inflammation through the recognition of different PAMPs. Although it is well known that TLRs can induce the expression of endogenous signals, as inflammatory cytokines and chemokines, 11 Lemaitre et al have reported that the activation of Toll leads to the production of antimicrobial peptides in Drosophila , a phenomenon that has also been demonstrated in mammalian cells.
18
Paulsen et al detected, by RNA expression of the antimicrobial molecules bactericidal-permeability-increasing protein (BPI), heparin binding protein (CAP37), and b defensin 1, in samples of healthy nasolacrimal duct epithelium.
19 The expression of b defensin 1 was also detected constitutively in human corneal epithelial cell cultures and the expression of b defensin 2 was induced by IL-1 b in the same cells type.
20 21 Human b defensin 1 and the inducible b defensin 2 have been detected also in cilliary body and retinal pigment epithelial cells.
22 We suggest that these antimicrobial peptides could also be induced by PAMPs through the TLRs that we have found in both portions of the eye. Human corneal and conjunctiva epithelial cells express b defensin 2 mRNA, and this expression is upregulated by heat killed Pseudomonas aeruginosa and its LPS.
23 24 LPS, a PAMP binding to TLR4, has been involved in the induction of b defensin 2 in human tracheobronchial epithelium and astrocytes.
25 26 This could occur in the eye, as in our study we found expression of TLR4 in the eye of the three studied strains. Saint et al , have recently demonstrated, in a murine model, that river blindness is the result of a TLR4 dependent inflammatory response against the endosymbiotic bacterium Wolbachia .
27
In this work we observed that in NIH, a non-syngenic strain of mice, the expression of TLR and NOD mRNA molecules was higher than in the syngenic strains Balb/c and C57BL/6 mice,
(p , 0.05). The growth environment for NIH mice is less strict than that required for syngenic mice. Then, these results could suggest that the exposure to an agent induces an overexpression of the TLR in this strain. Song et al reported that human corneal epithelial cells expressed CD14 and TLR4, and that these molecules were overexpressed after the induction
Eye
Spleen
Lung
Heart
Brain
Ovary
Testis bp
500
400
300
200
500
400
300
200
500
400
300
200
500
400
300
200
500
400
300
200
500
400
300
200
500
400
300
200
M 1 2 3 4
NIH
5 6 7 8 9 A M 1 2 3
Balb/c
4 5 6 7 8 9 A M 1 2 3
C57/BL6
4 5 6 7 8 9 A
Figure 4 Expression of TLR mRNAs in non-immune privileged and immune privileged organs. RT-PCR was performed on whole eye, brain, testis, ovary, spleen, lung, and heart of NIH,
Balb/c and C57BL/6 mice. In every gel image, lane M corresponds to 100 bp molecular ladder, lanes 1–9 correspond to mRNA expression of
TLRs1-9, respectively, and lane A to b actin expression.
www.bjophthalmol.com
908 Rodrı´guez-Martı´nez, Cancino-Dı´az, Jime´nez-Zamudio, et al
A bp
500
400
300
200
500
400
300
200
500
400
300
200
M NOD1 NOD2 β act
NIH
Balb/c
C57BL/6
B
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
NOD 1
NIH Balb/c C57
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
NOD 2
NIH Balb/c C57
Figure 5 Expression of NOD1 and
NOD2 mRNAs in the eye. (A) RT-PCR in whole eye of NIH, Balb/c, and C57BL/
6 mice. Lane M corresponds to 100 bp molecular ladder. (B) Intensity of mRNA expression of NODs in the eye. Each bar shows the median (SD) of the relation NOD/ b actin mRNA expression in the whole eye of 10 NIH, five Balb/c, and five C57BL/6 mice, respectively. Horizontal lines show statistical difference (p , 0.05) by
Kruskal-Wallis test. (C) mRNA expression of NODs in different eye compartments of Balb/c mice. AP, anterior portion; PP, posterior portion;
CF, corneal fibroblasts.
C bp
600
500
400
300
NOD1 NOD2 β act
NOD1 NOD2 β act
NOD1 NOD2 β act
M AP PP CF
600
500
400
300
600
500
400
300 bp
600
500
400
300 with Pseudomonas aeruginosa LPS.
14 Moreover, Jan-Michel et al reported the overexpression of TLR2, 3, 4, 6, and 7 in intestinal myofibroblast cells after LPS stimulation.
28 We found similar results in the treatment of CF with LPS. Nevertheless, the response of the CF to LPS was different in each strain.
Our results show that TLR2, TRL1, and TLR6 expression are the strongest in the eye of the three strains of mice studied.
These results are in accordance with several reports, which described the required co-expression of TLR2 and TLR6.
29
Besides, it is known that TLR2 forms heterodimeric complexes with TLR1.
30 The co-function of these TLRs increases the ability to recognise a wide variety of PAMPs and could explain the highest expression of these three TLRs in the eye.
The co-function TLR1-TLR2 cannot occur in the AP, as TLR1 was not detected in this compartment.
M NOD1NOD2 act act act act
TLR3 and TLR7 were also expressed in the three strains.
These results suggest that the healthy eye is able to respond to viral infections because the TLR3 recognises viral double stranded RNA, 11 agent R-848.
31 and TLR7 and TLR8 can bind to the antiviral
TLR5 is involved in the recognition of the bacterial flagellin of pathogenic bacteria like Salmonella .
32 In the eye of the studied mice we found a low expression of TLR5. However, in the report by Zhang et al , flagellin of Pseudomonas aeruginosa was shown to contribute to the inflammatory responses of corneal epithelium in a TLR-5-NFk B signalling pathway dependent manner, suggesting that the expression of TLR5 can be induced.
16 We found that TLR5 was induced by LPS in CFs of both strains.
There are no reports about TLR9 in the eye. We found low expression of TLR9, that recognises the non-methylated act act act
A
Figure 6 Expression of NOD mRNA in non-immune privileged and immune privileged organs. RT-PCR from the whole eye, brain, testis, ovary, spleen, lung, and heart of NIH (A), Balb/c (B), and C57BL/6 (C) mice. Lane M:
100 bp molecular ladder.
B
C
Eye Brain Testis Ovary Spleen Lung Heart www.bjophthalmol.com
TLRs and NODs mRNA expression pattern in healthy mouse eye 909 sequence CpG of bacterial DNA, 33 in the eye of Balb/c and
C57BL/6 mice, and was absent in the eye of NIH mice, even in its CF treated with the LPS.
In the eye, the TLRs could have an important role in the rapid elimination of microbial pathogens through antimicrobial peptide induction. When the microbial pathogens invade ocular tissues the TLRs also can induce pro-inflammatory cytokines and chemokines and trigger the adaptive immune response. Song et al reported that the human corneal epithelial and stromal cells secreted IL-6 and IL-8 when treated with LPS.
14 Oakes et al reported that the IL-8 gene expression is associated with herpes simplex virus infection of human keratocytes but not in human corneal epithelial cells.
34 We found expression of TLR7 and TLR8, which are associated with the recognition of antiviral products in CF of
Balb/c mice.
We found a differential expression of TLRs between the eye and the other immune privileged organs, such as testis and brain, where some TLRs were absent. According to our results, the eye has a TLRs expression pattern as that seen in the non-immune privileged organs.
NOD1 and NOD2 are intracellular molecules, which have a role in the regulation of pro-inflammatory pathways through
NFk B induced by bacterial ligands.
10 NOD2 recognises a specific peptidoglycan motif from bacteria, the muramyl dipeptide, 35 and NOD1 is able to detect a bacterial motif brought into the cytosolic compartment, as gammaD glutamylmesodiaminopimelate.
36 So far, reports about the expression of NOD1 and NOD2 in the eye do not exist.
We found expression of NOD2 in the AP and in the Balb/c
CF, but not in the PP. NOD1 is present in both portions and in Balb/c CF. The expression of NOD molecules in the eye suggests that the eye is also able to respond to intracellular
PAMPs. Recently, mutations in NOD2 have been associated with inflammatory diseases as Blau syndrome, a rare autosomic dominant disorder, in which the patient presents diverse ailments, such as arthritis, uveitis, skin rashes, and granuloma.
37
Several reports indicate that there are different susceptibilities to infections in the three strains studied. For example, C57BL/6 is resistant to simplex virus 1, 39
Toxoplasma gondii , 38 and to Trypanosoma congolense , to herpes
40 but is susceptible to
3, 42
Salmonella typhimurium whereas Balb/c is resistant to P
, 41 to hepatitis virus type seudomona aeruginosa , 43 to adenovirus type 1,
Yersinia , 46 and to
44 and susceptible to cytomegalovirus,
Mycobacterium.
47
45 to
We think that in these differences could be involved the different expression patterns of TLRs and NODs seen in the strains.
ACKNOWLEDGEMENTS
(CGPI20040430) and by the Patronato del Instituto de Oftalmologı´a received scholarships from CONACYT and PIFI-IPN for her post-
Latorre, and Mario E Cancino-Dı´az are fellows of COFAA-IPN, EDI-
IPN, and SNI-CONACYT. Juan C Cancino-Dı´az is a fellow of EDI-IPN and SNI-CONACYT.
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
S Rodrı´guez-Martı´nez, J C Cancino-Dı´az, Laboratorio de Microbiologı´a
General, Departamento de Microbiologı´a de la Escuela Nacional de
Ciencias Biolo´gicas del Instituto Politecnico Nacional, Carpio y Plan de
Ayala, Me´xico DF 11340, Me´xico
M E Cancino-Dı´az, L Jime´nez-Zamudio, E Garcı´a-Latorre, Laboratorio de Inmunoquı´mica I, Departamento de Inmunologı´a de la Escuela
Nacional de Ciencias Biolo´gicas del Instituto Politecnico Nacional,
Carpio y Plan de Ayala, Me´xico DF 11340, Me´xico
S Rodrı´guez-Martı´nez, Laboratorio de Inmunologı´a Ocular del Instituto de Oftalmologı´a, Fundacio´n Conde de Valenciana, Me´xico DF, Me´xico
REFERENCES
1 Wenkel H , Streilein JW. Analysis of immune deviation elicited by antigens injected into the subretinal space.
Invest Ophthalmol Vis Sci
1998; 39 :1823–34.
2 Cousins SW , McCabe MM, Danielpour D, et al.
Identification of transforming growth factor-beta as immunosuppressive factor in aqueous humor.
Invest
Ophthalmol Vis Sci 1991; 32 :2201–11.
3 Apte RS , Sinha D, Mayhew E, et al.
Role of macrophage migration inhibitory factor in inhibiting NK cell activity and preserving immune privilege.
J Immunol
1998; 160 :5693–6.
4 Hooper P , Bora NS, Kaplan HJ, et al.
Inhibition of lymphocyte proliferation by resident ocular cells.
Curr Eye Res 1991; 10 :363–72.
5 Ohta K , Wiggert B, Taylor AW, et al.
Effects of experimental ocular inflammation on ocular immune privilege.
Invest Ophtalmol Vis Sci
1999; 40 :2010–18.
6 Ohta K , Yamagami S, Taylor AW, et al.
IL-6 antagonizes TGF-b and abolishes immuneprivilege in eyes with endotoxin-induced uveitis.
Invest Ophthalmol Vis
Sci 2000; 41 :2591–9.
7 Peng B , Li Q, Roberge FG, et al.
Effect of transforming growth factor beta-1 in endotoxin-induced uveitis.
Invest Ophthalmol Vis Sci 1997; 38 :257–60.
8 Janeway CA Jr . The immune system evolved to discriminate infectious nonself from noninfectious self.
Immunol Today 1992; 13 :11–16.
9 Rock FL , Hardman G, Timans JC, et al.
A family of human receptors structurally related to Drosophila toll.
Proc Natl Acad Sci USA
1998; 95 :588–93.
10 Inohara N , Nu´n˜ez G. Nods: intracellular proteins involved in inflammation and apoptosis.
Nature Rev Immunol 2003; 3 :371–82.
11 Medzhitov R . Toll like receptors and innate immunity.
Nature Rev Immunol
2001; 1 :135–45.
12 Medzhitov R , Preston-Hurlburt P, Kopp E, et al.
MyD88 is an adaptor protein in the hToll/IL-1 signaling.
Science 1997; 279 :1612–15.
13 Chamaillard M , Girardin SE, Viala J, et al.
Nods, Nalps and Naip: intracellular regulators of bacterial-induced inflammation.
Cell Microbiol
2003; 5 :581–92.
14 Song PI , Abraham TA, Park Y, et al.
The expression of functional LPS receptor proteins CD14 and toll-like receptor 4 in human corneal cells . Invest
Ophthalmol Vis Sci 2001; 42 :2867–77.
15 Chang JH , McCluskey P, Wakefield D. Expression of toll-like receptor 4 and its associated lipopolysaccharide receptor complex by resident antigenpresenting cells in the human uvea.
Invest Ophthalmol Vis Sci
2004; 45 :1871–8.
16 Zhang J , Xu K, Ambati B, et al.
Toll-like receptor 5-mediated corneal epithelial inflammatory response to Pseudomonas aeruginosa flagelin.
Invest
Ophthalmol Vis Sci 2003; 44 :4247–54.
17 Berryhill BL , Kader R, Kane B, et al.
Partial restoration of the keratocyte phenotype to bovine keratocytes made fibroblastic by serum.
Invest
Ophthalmol Vis Sci 2002; 43 :3416–21.
18 Lemaitre B , Nicolas E, Michaut L, et al.
The dorseventral regulatory gene cassette spa¨tzle/Toll/cactus controls the potent antifungal response in
Drosophila adults.
Cell 1996; 86 :973–83.
19 Paulsen FP , Pufe T, Schaudig U, et al.
Detection of natural peptide antibiotics in human nasolacrimal ducts.
Invest Ophthalmol Vis Sci
2001; 42 :2157–63.
20 Haynes RJ , Tighe PJ, Dua S. Antimicrobial defensin peptides of the human ocular surface.
Br J Ophtalmol 1999; 83 :737–41.
21 McDermott AM , Redfern RL, Zhang B, et al.
Defensin expression by the cornea: multiple signaling pathways mediate IL-1B stimulation of hBD-2 expression by human corneal epithelial cells.
Invest Ophthalmol Vis Sci
2003; 44 :1859–65.
22 Haynes RJ , McElveen JE, Dua HS, et al.
Expression of human beta-defensins in intraocular tissues.
Invest Ophthalmol Vis Sci 2000; 41 :3026–31.
23 McNamara NA , Van R, Tuchin OS, et al.
Ocular surface epithelia express mRNA for human beta defensin 2.
Exp Eye Res 1999; 69 :483–90.
24 Narayanan S , Miller WL, McDermott AM. Expression of human beta-
Defensisn in conjunctival epithelium: relevance to dry eye disease.
Invest
Ophthalmol Vis Sci 2003; 44 :3795–801.
25 Becker MN , Diamond G, Verghese MW, et al.
CD14-dependent lipopolysaccharide-induced beta-defensin-2 expression in human tracheobronchial epithelium.
J Biol Chem 2000; 275 :29731–6.
26 Hao HN , Zhao J, Lotoczky G, et al.
Induction of human beta-defensin-2 expression in human astrocytes by lipopolysaccharide and cytokines.
J Neurochem 2001; 77 :1027–35.
27 Saint AA , Blackwell NM, Hall LR, et al.
The role of endosymbiotic Wolbachia bacteria in the pathogenesis of river blindness.
Science 2002; 295 :1892–5.
28 Jan-Michel O , Rosenberg IM, Podolsky DK. Intestinal myofibroblasts in innate immune responses of the intestine.
Gastroenterology 2003; 124 :1866–78.
29 Hajjar AM , O’Mahony DS, Ozinsky A, et al.
Cutting edge: functional interactions between toll-like receptor (TLR) 2 and TLR1 or TLR6 in response to phenol-soluble modulin.
J Immunol 2001; 166 :15–19.
30 Tapping RI , Tobias PS. Mycobacterial lipoarabinomannan mediates physical interactions between TLR1 and TLR2 to induce signaling.
J Endotoxin Res
2003; 9 :264–8.
31 Jurk M , Heil F, Vollmer J, et al.
Human TLR7 or TLR8 independently confer responsiveness to the antiviral compound R-848.
Nat Immunol 2002; 3 :499.
32 Hayashi F , Smith KD, Ozinsky A, et al.
The innate immune response to bacterial flagellin is mediated by Toll-like receptor 5.
Nature
2001; 410 :1099–103.
33 Hemmi H , Takeuchi O, Kawai T, et al.
A Toll-like receptor recognizes bacterial
DNA.
Nature 2000; 408 :740–5.
www.bjophthalmol.com
910 Rodrı´guez-Martı´nez, Cancino-Dı´az, Jime´nez-Zamudio, et al
34 Oakes JE , Monteiro CA, Cubitt CL, et al.
Induction of interleukin-8 gene expression is associated with herpes simplex virus infection of human corneal keratocytes but not human corneal epithelial cells.
J Virol 1993; 67 :4777–84.
35 Girardin SE , Boneca IG, Viala J, et al.
Nod2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection.
J Biol Chem
2003; 278 :8869–72.
36 Chamaillard M , Hashimoto M, Horie Y, et al.
An essential role for NOD1 in host recognition of bacterial peptidoglycan containing diaminopimelic acid.
Nat Immunol 2003; 4 :702–7.
37 Miceli-Richard C , Lesage S, Rybojad M, et al.
CARD15 mutations in Blau syndrome.
Nat Genet 2001; 29 :19–20.
38 Macario AJL , Stahl W, Miller RM. Lymphocyte subpopulations and function in chronic murine toxaplasmosis. II. Cyclic immunosuppression in genetic-lowresponder mice.
Cell Immunol 1980; 56 :235–9.
39 Brenner GJ , Cohen N, Moynihan JA. Similar immune response to nonlethal infection with herpes simplex virus-1 in sensitive (BALB/c) and resistant
(C57BL/6) strains of mice.
Cell Immunol 1994; 157 :510–24.
40 Ogunremi O , Tabel H. Genetics of resistance to Trypanosoma congolense in inbred mice: Efficiency of apparent clearance of parasites correlates with long-term survival.
J Parasitol 1995; 81 :876–81.
41 Robson HG , Vas SI. Resistance of mice to Salmonella typhimurium.
J Infect Dis
1972; 126 :378–80.
42 Le Prevost C , Virelizier JL, Dupuy JM. Immunopathology of mouse hepatitis virus type 3 infection. III. Clinical and virologic observation of a persistent viral infection.
J Immunol 1975; 115 :640–3.
43 Morissette C , Skamene E, Gervais F. Endobronchial inflammation following
Pseudomonas aeruginosa infection in resistant and susceptible strains of mice.
Infect Immun 1995; 63 :1718–24.
44 Guida JD , Fejer G, Pirofski LA, et al.
Mouse adenovirus type 1 causes a fatal hemorrhagic encephalomyelitis in adult C57BL/6 but not BALB/c mice.
J Virol
1995; 69 :7674–81.
45 Price P , Eddy KS, Papadimitriou JM, et al.
Genetic determination of cytomegalovirus-induced and age-related cardiopathy in inbred mice.
Characterization of infiltrating cells.
Am J Pathol 1991; 138 :59–67.
46 Autenrieth IB , Beer M, Bohn E, et al.
Immune responses to Yersinia enterocolitica in susceptible BALB/c and resistant C57BL/6 mice: an essential role for gamma interferon.
Infect Immun 1994; 62 :2590–9.
47 Chiodini RJ , Buergelt CD. Susceptibility of Balb/c, C57/B6 and C57/B10 mice to infection with Mycobacterium paratuberculosis.
J Comp Pathol
1993; 109 :309–19.
www.bjophthalmol.com
911
EXTENDED REPORT
Generation of transgenic mice with mild and severe retinal neovascularisation
C-M Lai, S A Dunlop, L A May, M Gorbatov, M Brankov, W-Y Shen, N Binz, Y KY Lai, C E Graham,
C J Barry, I J Constable, L D Beazley, E P Rakoczy
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Ophthalmol 2005; 89 :911–916. doi: 10.1136/bjo.2004.059089
See end of article for authors’ affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Associate Professor Chooi-
May Lai, Lions Eye Institute,
2 Verdun Street,
Nedlands, Western
Australia, 6009, Australia; mlai@cyllene.uwa.edu.au
Accepted for publication
1 December 2004
. . . . . . . . . . . . . . . . . . . . . . .
Aim: To generate a mouse model for slow progressive retinal neovascularisation through vascular endothelial growth factor (VEGF) upregulation.
Methods: Transgenic mice were generated via microinjection of a DNA construct containing the human
VEGF
165
(hVEGF) gene driven by a truncated mouse rhodopsin promoter. Mouse eyes were characterised clinically and histologically and ocular hVEGF levels assayed by ELISA.
Results: One transgenic line expressing low hVEGF levels showed mild clinical changes such as focal fluorescein leakage, microaneurysms, venous tortuosity, capillary non-perfusion and minor neovascularisation, which remained stable up to 3 months postnatal. Histologically, there were some disturbance and thinning of inner and outer nuclear layers, with occasional focal areas of neovascularisation. By contrast, three other lines expressing high hVEGF levels presented with concomitantly severe phenotypes. In addition to the above, clinical features included extensive neovascularisation, haemorrhage, and retinal detachment; histologically, focal to extensive areas of neovascularisation associated with retinal folds, cell loss in the inner and outer nuclear layers, and partial retinal detachment were common.
Conclusions: The authors generated four hVEGF overexpressing transgenic mouse lines with phenotypes ranging from mild to severe neovascularisation. These models are a valuable research tool to study excess
VEGF related molecular and cellular changes and provide additional opportunities to test anti-angiogenic therapies.
R etinal neovascularisation, a major cause of blindness in the developed world, is characteristic of many eye diseases including retinopathy of prematurity (ROP), retinal vein occlusion, and diabetic retinopathy (DR).
1–3
Retinal neovascularisation is thus an issue of major clinical importance, and for this reason, a variety of animal models have been developed.
The precise mechanisms underlying retinal neovascularisation have not been fully elucidated but have been linked to hypoxia and are thought to be mediated by various growth factors including vascular endothelial growth factor (VEGF).
4
VEGF has been a favoured molecule for study since it is hypoxia induced, 5 is one of the most potent angiogenic factors known, 6 and has a pivotal role during normal retinal vasculature development.
7 Furthermore, intravitreal VEGF injections or implants have induced neovascularisation in adult animals.
8 9 However, a major shortcoming of these models has been the lack of consistent phenotype and reproducibility.
9–12
The development of transgenic mouse models with early retinal neovascularisation 13 14 provides an approach to study the damaging phase of retinal neovascularisation and an opportunity for therapeutic evaluation.
15–19 However, most of the current ocular neovascularisation models are hampered by both extensive and rapid neovascularisation which result in severe retinal damage.
14
The rhodopsin promoter used in existing transgenic mouse models contains regulatory regions known to enhance expression of the associated transgene. In addition, the rhodopsin promoter length has been correlated to the transgene’s expression level.
20–22 As our aim was to produce a transgenic mouse model expressing low VEGF levels which would lead to a slow progression of retinal neovascularisation akin to vascular changes observed in DR, we constructed a transgene cassette using the 1.4 kb mouse rhodopsin promoter fragment known to lack transcriptional enhancers 23 to drive human VEGF (hVEGF) expression in the transgenic mice.
METHODS
Animal husbandry
All animal procedures were performed in accordance with the
ARVO statement for the use of animals in ophthalmic and vision research and with approval from the animal ethics committee at the University of Western Australia, Australia.
Mice were housed in cages at a constant temperature of 22 ˚ C, with a 12:12 hour light/dark cycle, and food and water were available ad libitum.
Transgenic mice generation
The previously described hVEGF
165 mouse rhodopsin promoter 23 isoform 24 and truncated were used to generate the pcDNA.opsin.VEGF construct (fig 1A). The 2.89 kb Ase I/
Sac II fragment containing the truncated mouse rhodopsin promoter, hVEGF
165 and bovine growth hormone polyadenylation signal sequence was used for transgenic mice generation.
Pups were first screened by Southern blot analysis.
Presence of the 2.1 kb fragment containing the truncated
Abbreviations: CFP, colour fundus photography; CNV, choroidal neovascularisation; DR, diabetic retinopathy; ELISA, enzyme linked immunosorbent assay; FFA, fluorescein fundus angiography; FITC, fluorescein isothiocyanate; hVEGF, human vascular endothelial growth factor; INL, inner nuclear layer; NFL, nerve fibre layer; NPDR, nonproliferative diabetic retinopathy; ONL, outer nuclear layer; PBS, phosphate buffered saline; PCR, polymerase chain reaction; PDR, proliferative diabetic retinopathy; RPE, retinal pigment epithelium; ROP, retinopathy of prematurity; VEGF, vascular endothelial growth factor www.bjophthalmol.com
912 Lai, Dunlop, May, et al
Ase
Ampicillin
I (6072)
Sac II (232)
VEGFR
A
Mouse opsin promoter pMB1 origin pcDNA.opsin.VEGF
Ase I (4840)
Ase I (4781)
SV40 polyA
8 kb
Neo resistance
MW 029 tg wt
6822 bp human VEGF
MuOpPF
BGH polyA f1 origin
Ase I (3120)
SV40 promoter
050 tg wt
056 tg wt
086 tg wt
090 tg wt
094 tg wt
B
C
2 kb
Figure 1 In vitro characterisation of transgenic mice. (A) Diagrammatic representation of the pcDNA.opsin.VEGF construct used for transgenic mice generation. (B) Southern blot analysis showing the banding profiles from the different lines. Pups were screened by Southern blot analysis of Eco RI digested tail DNA and probed with a 1.1 kb [ a – 32 P]dCTP labelled Eco RI fragment of the mouse rhodopsin promoter from pcDNA.opsin.VEGF (A). Lane 1, lambda DNA control; lanes 2 and 3, no DNA control. (C) Agarose gel electrophoresis of PCR products from the different lines. Lane 1, no primer control; lane 2, no DNA control; lane 3, positive control. The PCR conditions consisted of denaturation at
95
˚
C for 15 minutes, 40 cycles of 95
1 minute, and 72
˚
˚
C for 30 seconds, 58
˚
C for
C for 4 minutes, followed by a final extension at 72
˚
for 7 minutes. MW, molecular weight marker; tg, transgenic mice; wt, non-transgenic littermate.
C mouse rhodopsin promoter and hVEGF
165 fragments in the transgenic mice was then confirmed by polymerase chain reaction (PCR) amplification of tail DNA using the primer pair 5 9 CGA GGC TCA GAG AGG AAT ACT T3 9 and
5 9 CAC CGC CTC GGC TTG TCA C3 9 . First generation heterozygote transgenic offspring from backcrossing founders with
C57Bl/6J mice were characterised clinically, by colour fundus photography (CFP) and fluorescein fundus angiography
(FFA), and histologically with age matched, non-transgenic littermates and C57Bl/6J mice as controls.
Quantification of ocular hVEGF protein
To circumvent complications presented by differences in onset and severity of retinopathy at later time points, 10 day old mouse eyes, an age where the retinopathy was still mild and retinas intact in all the lines, were enucleated for hVEGF quantification using an enzyme linked immunosorbent assay
(ELISA; Quantikine, R & D Systems, Minneapolis, MN, USA).
Intact mouse eyes were disrupted with a pestle in 50 m l of phosphate buffered saline (PBS) containing protease inhibitor cocktail (Roche, Indianapolis, IN, USA). Total protein in the eye homogenate was quantified by the Bradford method
(Protein Assay dye; Bio-Rad, Richmond, CA, USA) with bovine serum albumin as the standard. Ocular hVEGF levels were normalised to 1 mg total protein.
Fluorescein labelled dextran perfusion and retina flat mount preparation
Six week old deeply anaesthetised mice were perfused with
PBS (pH 7.4) followed by 2 ml fluorescein isothiocynate labelled dextran (FITC-dextran, 50 mg/ml, MW 2.0
6 10 6 ;
Sigma, St Louis, MO, USA). Eyes were enucleated, fixed in
2% paraformaldehyde for 30 minutes, and flat mounted for fluorescence microscopy.
25
Histology
Eyes from each transgenic line were enucleated at between
1 week and 12 weeks postnatal following euthanasia with pentobarbital (Lethabarb; Virbac, NSW, Australia) and fixed for 4 hours in 4% neutral buffered formalin before paraffin embedding. Five m m thick paraffin sections were stained with haematoxylin and eosin (H & E) for light microscopy.
RESULTS
Characterisation of transgenic mice
Six founders, designated 029, 050, 056, 086, 090, and 094
(fig 1B), were identified by Southern blot analysis.
Subsequent PCR amplification showed that the 2.1 kb DNA fragment was present in all but line 090 (fig 1C). Of these, lines 029, 050, 056, and 094 showed varying degrees of neovascularisation and pathology (see below). Lines 086 and
090 appeared normal even at 10 months postnatal and hence are not discussed further.
Features of diabetic retinopathy
The most prevalent disease associated with retinal neovascularisation is DR.
3 In this study, we used classic clinical features of DR 26 to determine whether retinal vascular changes observed in DR also occurred in our transgenic lines
(table 1). Representative images showing pathological features associated with non-proliferative diabetic retinopathy (NPDR; microaneurysm, exudates, haemorrhage, venous abnormalities) and proliferative diabetic retinopathy
(PDR; neovascularisation, preretinal haemorrhage, fibrovascular proliferation) are summarised and documented in figure 2.
Evaluation of mouse eyes and comparison with human
DR eyes
CFP and FFA demonstrated the fundus and retinal vasculature of C57Bl/6J mice (fig 3A and B) and non-transgenic littermates (data not shown) to be normal at all ages examined. The C57Bl/6J mouse eye has even calibre vessels radiating from a well defined optic nerve head. FITC-dextran perfusion and histological examination of control eyes showed intact retinal vessels (fig 3C) and normal retinal morphology (fig 3D).
The four transgenic lines were distinguished by the onset and severity of neovascular changes (table 1). When examined by CFP, FFA, FITC-dextran perfusion, and histology, line 029 eyes showed consistently milder changes at early stages (3–4 weeks). Using CFP, the fundus had pale lesions (fig 3E); some were flat at the level of the outer retina and some were raised when examined stereoscopically. The optic nerve head and retinal vasculature appeared similar to the controls. FFA demonstrated multiple areas of focal hyperfluorescence (fig 3F, arrowhead). Upon stereoscopic examination, these lesions were seen at the level of the capillary bed in the inner retina (fig 3F, arrows), resembling microaneurysms. In the FITC-dextran perfused eyes the retinal vasculature appeared normal, except for some hyperfluorescent spots, focally dilated vessels (fig 3G, arrow) and occasional saccular structures resembling microaneurysms.
Although line 029 transgenic mouse eyes had distinct, full thickness and normal appearing inner nuclear (INL), outer nuclear (ONL) and nerve fibre layers (NFL), there were focal areas of disturbance in the retina (fig 3H, arrow).
Clinically (CFP and FFA), changes in line 029 transgenic mice remained relatively stable with some increases in size and numbers of hyperfluorescent spots in follow up examinations at 10–12 weeks postnatal (fig 3I and J). By www.bjophthalmol.com
Transgenic mouse model for retinal neovascularisation 913
Figure 2 Colour fundus photography (CFP) and fluorescein fundus angiography (FFA) showing different features of diabetic retinopathy (DR). (A) An eye with mild non-proliferative diabetic retinopathy (NPDR) presented with microaneurysms (short arrows), haemorrhages (long arrows), as well as hard and soft exudates (arrowhead). (B) An eye with severe NPDR showing a greater number of microaneurysms (short arrows), haemorrhages (long arrows), and also venous abnormalities such as venous dilatation (white arrow) and tortuosity (arrowheads). (C) and (D) Eyes with high risk proliferative diabetic retinopathy (PDR). Haemorrhages (long arrows), hard exudates (small arrowhead), venous beading on the inferior arcade, new vessels (hallmark for PDR) and preretinal haemorrhage (large arrowheads) are present in (C) and new vessels at the disc (long arrows) are seen in (D).
(E) A late phase FFA of an eye with PDR showing leakage from the new vessels (arrowheads) and small spots of hyperfluorescence representing microaneurysms (arrows). Dark patches near the right edge are zones of capillary non-perfusion. (F) Eye with advanced PDR showing extensive fibrovascular proliferation (arrows).
this age, the presence of dilated, tortuous capillaries with hyperfluorescent saccular structures resembling microaneurysms (fig 3K, arrows) and areas of capillary non-perfusion were evident from FITC-dextran perfusion. Histologically, there was significant disturbance in the ONL and INL which also appeared thinner compared to control eyes (compare fig 3D and 3L). Frequent focal areas of neovascularisation were present in the ONL and INL (fig 3L arrow). These vascular changes, such as microaneurysms, fluorescein leakage, and tortuous vessels, were similar to those observed in NPDR (fig 2A and B) and very early stages of PDR (fig 2C and D).
By 3–4 weeks postnatal, lines 050 and 056 demonstrated severe neovascularisation (fig 3M–P) and line 094 presented with retinal changes (fig 3Q–T) ranging from mild to severe.
CFP revealed broad opaque sheets of pale tissue (fig 3M, arrows), venous dilatation (fig 3Q, arrowhead), and tortuosity (fig 3Q, arrow). In addition, FFA revealed intensely hyperfluorescent lesions (fig 3N, arrows and 3R, arrows) associated with haemorrhage.
FITC-dextran perfusion showed tortuous vessels and glomerular tufts of hyperfluorescence in the central and peripheral retina that varied in size and morphology (fig 3O and 3S, arrows). In addition, lines
050, 056, and 094 presented with extensive areas of capillary non-perfusion (fig 3O and 3S, dark regions). The presence of extensive subretinal and intraretinal neovascularisation
(fig 3P, arrowheads) was associated with the formation of folds and cell loss in the INL and ONL. Partial retinal detachment with subretinal exudate was also present.
Preretinal haemorrhage (fig 3T inset, arrow) was observed in line 094 eyes with severe retinopathy. The above described features are similar to changes associated with severe neovascularisation in patients with PDR (fig 2C and 2E, arrowheads).
Although neovascular changes were present in all four lines examined, their choroidal vasculature appeared normal.
In addition, their progression to the end stage of the disease, represented by severe fundal depigmentation, retinal vessel narrowing with abnormal capillary bed, scarring or retinal detachment varied between the lines. The disease progression was slow in line 029 (8 months) but was rapid in lines 050
(3 months), 056 (3 months), and 094 (4 months).
Quantification of hVEGF protein
A correlation between VEGF levels and the severity of neovascularisation was seen. hVEGF levels in line 029 (35.5
(SD 13.8) pg VEGF/mg total protein) were significantly lower
(p , 0.05) than those in lines 050 and 094 (410.6 (52.6) pg
Table 1 Characterisation of retinal vasculature in the transgenic mouse lines
Retinal vasculature characteristics
Capillary non-perfusion
Microaneurysms
Venous dilatation
Tortuosity of blood vessels
Haemorrhages
Neovascularisation
Preretinal haemorrhage
Vitreous haemorrhage
Fibrovascular proliferation
Cataracts *
Retinal detachment
Line 029
+
+
–
+
¡
–
–
+
–
–
–
Line 050/056
+
+
++
++
+
+
+
+
–
+++
+++
Line 094
++
++
++
++
+
+
+
+
+
+
++
* Other pathological features observed through clinical and histological examinations.
www.bjophthalmol.com
914 Lai, Dunlop, May, et al
Figure 3 Characterisation of the different transgenic mouse lines by colour fundus photography (CFP) (A, E, I, M, and Q), fluorescein fundus angiography (FFA) (B, F, J, N, and R), fluorescence micrographs of flat mounted, fluorescein labelled dextran perfused eyes (C, G, K, O, and S), and light micrographs (LM) of haematoxylin and eosin stained paraffin sections (D, H, L, P, and T). C57Bl/6 control mouse eye at 4 weeks (A–C) and at
3 weeks postnatal (D). Line 029 transgenic mouse eye at 4 weeks (E–G) and at 3 weeks (H) postnatal. Line 029 transgenic mouse eyes at 12 weeks
(I–J) and at 10 weeks (K–L) postnatal. Line 050/056 transgenic mouse eye at 4 weeks (M–O) and at 3 weeks (P) postnatal. Line 094 transgenic mouse eyes at 4 weeks (Q–S) and at 3 weeks (T) postnatal. Arrowhead in (F) demonstrates focal hyperfluorescence which corresponds to pale lesions in (E).
Arrows in (N) and (R) point to intense and extensive fluorescein leakage. The arrows in (G), (K), (O), and (S) point to focally dilated vessels (G), microaneurysm (K), and glomerular tufts of hyperfluorescence (O and S). The arrows in (H), (L), (P), and (T) point to new vessels. Arrowhead and arrow in (Q) show venous dilatation and tortuosity, respectively.
and 375.8 (49.0) pg VEGF/mg total protein, respectively).
hVEGF protein was not detected in eyes of age matched, nontransgenic littermates or C57Bl/6J eyes (n = 4 for each line).
DISCUSSION
We generated a mouse model that clearly demonstrated that relatively low hVEGF protein levels were sufficient to produce clinical and pathological changes consistent with slowly developing retinal neovascularisation. We used the mouse rhodopsin promoter to ensure inclusion of intrinsic regulatory elements to drive transgene expression. In addition, this promoter was truncated to exclude the enhancer region
( 2 1575 to 2 1477) with the aim of driving lower hVEGF levels to induce less severe neovascular changes compared to those in previously described transgenic mice.
14 Indeed, using the truncated proximal promoter region, we generated one transgenic line (029) with almost 10-fold lower hVEGF expression than in the other three transgenic lines. The fact that only one out of four lines demonstrated moderate hVEGF expression suggested that as long as transgene construct integration remained random, the use of truncated species specific promoters was not sufficient to strictly control transgene expression levels. Fortunately, variability in transgene expression associated with random chromosomal integration can now be circumvented using the more expensive knock-in technologies.
27
Line 029 clearly demonstrated that relatively low hVEGF protein levels were sufficient to produce clinical and pathological changes consistent with those seen in NPDR and very early stages of PDR, as well as other ocular neovascular disorders. The ability of exogenous VEGF to induce retinal ischaemia and neovascularisation had previously been reported in monkeys.
8 28 It was hypothesised that VEGF may trigger retinal ischaemia since it upregulates retinal ICAM-1 (intercellular adhesion molecule) expression, which in turn may lead to retinal leucosis and death of endothelial cells and pericytes.
29
The presence of areas of capillary non-perfusion in the eyes of our transgenic lines may be the result of VEGF triggered retinal ischaemia. It is possible that, once ischaemia is initiated, a cycle begins whereby VEGF induced neovascularisation is outstripped by VEGF induced ischaemia. It has been shown that, in addition to microaneurysm and microvessel obliteration, the earliest clinical manifestation of NPDR arises directly or indirectly as a result of VEGF upregulation.
30 cells, astrocytes, and some endothelial cells in retinas of diabetics with NPDR 31 and in Goto-Kakisaki rats before observable vascular changes.
32 Taken together, line 029 demonstrated several changes that have been observed in the retinal vasculature of patients with NPDR, such as microaneurysms, venous abnormalities (dilatation, tortuosity, and www.bjophthalmol.com
Transgenic mouse model for retinal neovascularisation focal constrictions) and, at later stages, capillary nonperfusion (fig 2B and C). Further studies on line 029 will be necessary to elucidate the possible role of moderate hVEGF levels on a variety of retinal cell types and how such expression leads to sequelae such as capillary occlusion, hypoxia, microaneurysms, and venous dilatation.
We anticipated that, following moderate photoreceptor specific hVEGF upregulation, the principal pathological change would be neovascularisation restricted to the outer retina. This was observed in line 029 where neovascularisation was mild and may represent the very early stages of PDR.
However, in the other lines, severe neovascularisation occurred in the outer retina as well as in the inner retina and at subretinal and preretinal locations. Our observation of preretinal neovascularisation in these lines contrasts with other mouse models with severe retinopathy, 13 14 but which lacked preretinal haemorrhage, a hallmark of PDR.
26
The photoreceptor specific hVEGF upregulation did not induce choroidal neovascularisation (CNV) in our and other transgenic mouse models.
13 14 Similarly, transgenic mouse models with retinal pigment epithelial (RPE) cell specific
VEGF upregulation did not develop CNV.
33 34 It was suggested that the intact RPE cells and Bruch’s membrane may act as barriers and unless they are perturbed, as through subretinal injection, 35 36 the upregulated hVEGF is not sufficient to cause CNV. In our transgenic mice, the RPE and Bruch’s membrane were intact even in lines showing severe retinal neovascularisation. In addition, in spite of the severe retinal neovascularisation present at 3–4 weeks postnatal, the changes in lines 050, 056, and 094 did not in any way resemble the regression and massive overgrowth of abnormal vessels across the surface of the retina, as characterised in
ROP.
37
The relatively mild degree of neovascularisation and its slow onset in line 029, as well as stable retinopathy for at least 3 months provide a valuable model for the development and evaluation of therapeutic treatments for retinal neovascularisation. The gradual changes observed in line 029 were similar to our previous mouse model in which VEGF upregulation was mediated by a recombinant adeno associated virus vector.
38 However, it differed from an existing
VEGF transgenic mouse model, 13 which demonstrated earlier onset and more severe retinopathy. Likewise, a previously reported inducible VEGF transgenic model 39 had variable pathology even when using the same doxycyclin dosage and neovascularisation was rapid and severe with complete retinal detachment.
14
Although photoreceptors are not the main VEGF expression site during DR, many resultant pathological changes observed in our transgenic mice, particularly line 029, resembled NPDR or very early stages of PDR. Similar to other VEGF models, our transgenics are not hyperglycaemic but rather target the most damaging end stage of DR— namely, retinal neovascularisation. Transgenic VEGF models therefore may not provide information on the sequence of events leading to VEGF upregulation in DR and other diseases. However, the regulatory sequelae of excess VEGF production are a potential area for further study which may provide valuable information relevant to DR, as well as a wide variety of other ocular diseases in which retinal neovascularisation is a major feature.
ACKNOWLEDGEMENTS
The authors acknowledge OzGene Pty Ltd, Western Australia, for generating the transgenic colony, and the Animal Resource Centre,
Western Australia, and the Sir Charles Gairdner Hospital Animal
Resource Centre, Western Australia, for maintenance of the transgenic mice. This project was the research effort of the Diabetic
Retinopathy Consortium, Perth, Australia.
915
. . . . . . . . . . . . . . . . . . . . .
Authors’ affiliations
C-M Lai, L A May, M Brankov, W-Y Shen, N Binz, Y K Lai, C E Graham,
C J Barry, I J Constable, E P Rakoczy, Centre for Ophthalmology and
Visual Science, The University of Western Australia, Nedlands, Australia
S A Dunlop, L D Beazley, School of Animal Biology, The University of
Western Australia, Nedlands, Australia
S A Dunlop, L D Beazley, Western Australian Institute for Medical
Research, The University of Western Australia, Nedlands, Australia
M Gorbatov, M Brankov, W-Y Shen, N Binz, Y K Lai, C E Graham,
C J Barry, Lions Eye Institute, Molecular Ophthalmology Department,
Nedlands, Australia
Sponsor details. This study was supported by the Juvenile Diabetes
Research Foundation International (USA), National Health and Medical
Research Council (Australia) and Westpac Foundation (Australia).
Ethical approval. Ethical approval (AEC 03/300/016 and 03/100/
107) for breeding of and experimentation on animals has been granted by the Animal Ethics Committee at the University of Western Australia,
Australia.
REFERENCES
1 Battaglia Parodi M , Iacono P, Di Crecchio L, et al.
Clinical and angiographic features in nasal branch retinal vein occlusion.
Ophthalmologica
2004; 218 :210–13.
2 Recchia FM , Baumal CR, Sivalingam A, et al.
Endophthalmitis after pediatric strabismus surgery.
Arch Ophthalmol 2000; 118 :939–44.
3 Klein R , Klein BE, Moss SE, et al.
The Wisconsin epidemiologic study of diabetic retinopathy. III. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years.
Arch Ophthalmol 1984; 102 :527–32.
4 Witmer AN , Vrensen GF, Van Noorden CJ, et al.
Vascular endothelial growth factors and angiogenesis in eye disease.
Prog Retin Eye Res 2003; 22 :1–29.
5 Forsythe JA , Jiang BH, Iyer NV, et al.
Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1.
Mol Cell Biol
1996; 16 :4604–13.
6 Senger DR , Connolly DT, Van de Water L, et al.
Purification and NH2-terminal amino acid sequence of guinea pig tumor-secreted vascular permeability factor.
Cancer Res 1990; 50 :1774–8.
7 Feeney SA , Simpson DA, Gardiner TA, et al.
Role of vascular endothelial growth factor and placental growth factors during retinal vascular development and hyaloid regression.
Invest Ophthalmol Vis Sci
2003; 44 :839–47.
8 Tolentino MJ , Miller JW, Gragoudas ES, et al.
Intravitreous injections of vascular endothelial growth factor produce retinal ischemia and microangiopathy in an adult primate.
Ophthalmology 1996; 103 :1820–8.
9 Ozaki H , Hayashi H, Vinores SA, et al.
Intravitreal sustained release of VEGF causes retinal neovascularization in rabbits and breakdown of the bloodretinal barrier in rabbits and primates.
Exp Eye Res 1997; 64 :505–17.
10 Chakrabarti S , Sima AA, Tze WJ, et al.
Prevention of diabetic retinal capillary pericyte degeneration and loss by pancreatic islet allograft.
Curr Eye Res
1987; 6 :649–58.
11 Kobayashi T , Kubo E, Takahashi Y, et al.
Retinal vessel changes in galactosefed dogs.
Arch Ophthalmol 1998; 116 :785–9.
12 Su EN , Alder VA, Yu DY, et al.
Continued progression of retinopathy despite spontaneous recovery to normoglycemia in a long-term study of streptozotocin-induced diabetes in rats.
Graefes Arch Clin Exp Ophthalmol
2000; 238 :163–73.
13 Okamoto N , Tobe T, Hackett SF, et al.
Transgenic mice with increased expression of vascular endothelial growth factor in the retina: a new model of intraretinal and subretinal neovascularization.
Am J Pathol
1997; 151 :281–91.
14 Ohno-Matsui K , Hirose A, Yamamoto S, et al.
Inducible expression of vascular endothelial growth factor in adult mice causes severe proliferative retinopathy and retinal detachment.
Am J Pathol 2002; 160 :711–9.
15 Takahashi K , Saishin Y, Silva RL, et al.
Intraocular expression of endostatin reduces VEGF-induced retinal vascular permeability, neovascularization, and retinal detachment.
Faseb J 2003; 17 :896–8.
16 Takahashi K , Saishin Y, Mori K, et al.
Topical nepafenac inhibits ocular neovascularization.
Invest Ophthalmol Vis Sci 2003; 44 :409–15.
17 Oshima Y , Deering T, Oshima S, et al.
Angiopoietin-2 enhances retinal vessel sensitivity to vascular endothelial growth factor.
J Cell Physiol
2004; 199 :412–17.
18 Nambu H , Nambu R, Oshima Y, et al.
Angiopoietin 1 inhibits ocular neovascularization and breakdown of the blood-retinal barrier.
Gene Ther
2004; 11 :865–73.
19 Saishin Y , Takahashi K, Seo MS, et al.
The kinase inhibitor PKC412 suppresses epiretinal membrane formation and retinal detachment in mice with proliferative retinopathies.
Invest Ophthalmol Vis Sci 2003; 44 :3656–62.
20 Nie Z , Chen S, Kumar R, et al.
RER, an evolutionarily conserved sequence upstream of the rhodopsin gene, has enhancer activity.
J Biol Chem
1996; 271 :2667–75.
21 Fortini ME , Rubin GM. Analysis of cis-acting requirements of the Rh3 and Rh4 genes reveals a bipartite organization to rhodopsin promoters in Drosophila melanogaster.
Genes Dev 1990; 4 :444–63.
22 Zack DJ , Bennett J, Wang Y, et al.
Unusual topography of bovine rhodopsin promoter-lacZ fusion gene expression in transgenic mouse retinas.
Neuron
1991; 6 :187–99.
www.bjophthalmol.com
916 Lai, Dunlop, May, et al
23 May LA , Lai CM, Rakoczy PE. In vitro comparison studies of truncated rhodopsin promoter fragments from various species in human cell lines.
Clin
Experiment Ophthalmol 2003; 31 :445–50.
24 Chavand O , Spilsbury K, Rakoczy PE. Addition of a c-myc epitope tag within the VEGF protein does not affect in vitro biological activity.
Biochem Cell Biol
2001; 79 :107–12.
25 Shen WY , Garrett KL, da Cruz L, et al.
Dynamics of phosphorothioate oligonucleotides in normal and laser photocoagulated retina.
Br J Ophthalmol
1999; 83 :852–61.
26 Diabetic Retinopathy Study . Report Number 6. Design, methods, and baseline results. Report Number 7. A modification of the Airlie House classification of diabetic retinopathy.
Invest Ophthalmol Vis Sci
1981; 21 :1–226.
27 Hamanaka H , Katoh-Fukui Y, Suzuki K, et al.
Altered cholesterol metabolism in human apolipoprotein E4 knock-in mice.
Hum Mol Genet 2000; 9 :353–61.
28 Tolentino MJ , McLeod DS, Taomoto M, et al.
Pathologic features of vascular endothelial growth factor-induced retinopathy in the nonhuman primate.
Am J Ophthalmol 2002; 133 :373–85.
29 Lu M , Perez VL, Ma N, et al.
VEGF increases retinal vascular ICAM-1 expression in vivo.
Invest Ophthalmol Vis Sci 1999; 40 :1808–12.
30 Robison WG Jr , Laver NM, Lou MF. The role of aldose reductase in diabetic retinopathy: prevention and intervention studies. In: NN O, Chader GJ, eds.
Progress in retinal and eye research . Oxford: Pergammon, 1995:593–640.
31 Amin RH , Frank RN, Kennedy A, et al.
Vascular endothelial growth factor is present in glial cells of the retina and optic nerve of human subjects with nonproliferative diabetic retinopathy.
Invest Ophthalmol Vis Sci
1997; 38 :36–47.
32 Sone H , Kawakami Y, Okuda Y, et al.
Ocular vascular endothelial growth factor levels in diabetic rats are elevated before observable retinal proliferative changes.
Diabetologia 1997; 40 :726–30.
33 Schwesinger C , Yee C, Rohan RM, et al.
Intrachoroidal neovascularization in transgenic mice overexpressing vascular endothelial growth factor in the retinal pigment epithelium.
Am J Pathol 2001; 158 :1161–72.
34 Oshima Y , Oshima S, Nambu H, et al.
Increased expression of VEGF in retinal pigmented epithelial cells is not sufficient to cause choroidal neovascularization.
J Cell Physiol 2004; 201 :393–400.
35 Spilsbury K , Garrett KL, Shen WY, et al.
Overexpression of vascular endothelial growth factor (VEGF) in the retinal pigment epithelium leads to the development of choroidal neovascularization.
Am J Pathol
2000; 157 :135–44.
36 Wang F , Rendahl KG, Manning WC, et al.
AAV-mediated expression of vascular endothelial growth factor induces choroidal neovascularization in rat.
Invest Ophthalmol Vis Sci 2003; 44 :781–90.
37 Reynaud X , Dorey CK. Extraretinal neovascularization induced by hypoxic episodes in the neonatal rat.
Invest Ophthalmol Vis Sci 1994; 35 :3169–77.
38 Rakoczy PE , Brankov M, Fonceca A, et al.
Enhanced recombinant adenoassociated virus-mediated vascular endothelial growth factor expression in the adult mouse retina: a potential model for diabetic retinopathy.
Diabetes
2003; 52 :857–63.
39 Mori K , Duh E, Gehlbach P, et al.
Pigment epithelium-derived factor inhibits retinal and choroidal neovascularization.
J Cell Physiol 2001; 188 :253–63.
www.bjophthalmol.com
Br J Ophthalmol 2005; 89 :917–929
PostScript
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
917
LETTERS
Subconjunctival corticosteroid injection for the treatment of nonnecrotising anterior scleritis
Scleritis commonly is a recurrent disease that requires long term immunosuppressive treatment that can be associated with significant adverse effects.
1 Although topical and periorbital steroids are accepted therapeutic options for treatment of scleritis, subconjunctival administration of depot corticosteroids has been considered unsafe owing to the risk of scleral thinning and perforation.
2–4
Recently, this has been challenged by reports describing the safe and effective use of subconjunctival depot steroid injections in patients with non-necrotising scleritis.
5–7
Based on these reports we reviewed our experience using subconjunctival corticosteroid injections (SCI) in the management of non-infectious, non-necrotising anterior scleritis.
Case reports
A retrospective, non-comparative review of the clinical records of patients with scleritis evaluated at the National Eye Institute was performed and four patients treated with SCI were identified. Subconjunctival triamcinolone acetonide (Kenalog 40 mg/ml, Westwood
Squibb Pharmaceuticals, Buffalo, NY, USA)
(2–12 mg per injection) was given to an area of active scleritis through a 30 gauge needle following topical anaesthesia in one quadrant of the eye at one time. The initial indication for SCI in all cases was unilaterally active non-necrotising scleritis with adverse effects from systemic immunosuppressive therapy in patients with no known history of ocular hypertension associated with steroids and no underlying disease requiring additional systemic immunosuppressive therapy.
Patients were evaluated within 1–2 weeks
Figure 1 Active diffuse anterior scleritis in the temporal quadrant of the left eye (patient 4, left eye directed nasally) (A), immediately after SCI (B), and 3 months following the SCI (C) is illustrated.
after injection and, 2–4 weeks thereafter.
Mean follow up time was 15.75 (SD 7.5) months (range 5–22 months).
In all cases the scleral inflammation was controlled within 2–9 days of SCI without a concurrent increase in systemic immunosuppression. Although effective, each patient subsequently required additional injections because of recurrent disease activity in the treated or the fellow eye within an average time of 7.4 months. However, with one exception, all recurrences developed in a previously untreated quadrant of the eye.
Only one patient showed a recurrence of active scleritis in a previously treated quadrant 21 months following the initial SCI. The maximum number of injections given in one eye was four. Following the initiation of the
SCI each patient’s prednisone dose was tapered by .
50% over an average of
5 months. Complications included subconjunctival haemorrhage and transient elevations in IOP that was managed with topical antiglaucoma medications and systemic acetazolamide (table 1). No patient showed enhanced scleral thinning or progression to necrotising scleritis.
Comment
Approximately 37% of patients with scleritis have associated systemic diseases.
8 A seminal review of scleritis cases showed that 26.1% of patients with scleritis require systemic immunosuppressive therapy and, of these,
37.5% experience a treatment complication.
1
Although associated with cataract and increased intraocular pressure, local steroid therapy offers the benefit of anti-inflammatory control without the side effects of systemic immunosuppressive drugs. However, because of the potential risk of scleral thinning and perforation subconjunctival steroid injections have been avoided for the treatment of scleritis.
Recently, two retrospective studies demonstrated rapid clinical improvement with SCI with no evidence of scleral thinning or serious side effects in non-necrotising scleritis during follow up extending to 23 years.
6 7 However, recurrences occurred in both studies requiring repeated injections. In a prospective study, patients with recalcitrant scleritis were able to discontinue all immunosuppressive therapy after treatment with SCI.
5
Although SCIs were effective in rapidly controlling the active scleritis in our series, two patients developed steroid response and all developed recurrent scleritis requiring repeated injections. The major benefit of the
SCI in this series was that they facilitated
.
50% reduction in each patient’s prednisone dose which could not be achieved or sustained before their use.
This study confirms the existing literature that SCI may be an effective adjunct for the treatment of active non-necrotising anterior
Table 1 Clinical characteristics, treatment regimens, and adverse events with subconjunctival steroid injection
Patient age, sex
1, 57, F
2, 41, M
3, 56, F
4, 11, M
Scleritis type
Nodular anterior both eyes
Diffuse anterior both eyes
Diffuse anterior both eyes
Diffuse anterior both eyes +
Posterior left eye
Associated disease
Mixed connective tissue disease
(inactive)
None *
Sjogren’s syndrome
(inactive)
None
Systemic treatment before
SCI
Pred 15 mg
MTX 12.5 mg
Pred 9 mg
MMF 2 g
Pred 20 mg
MTX 20 mg
Pred 50 mg
CsA 150 mg
Side effects from systemic treatment
Osteoporosis
Weight gain
Pneumonia
Weight gain
Myopathy
Recurrent UTI
GERD
Weight gain
Persistent headache
Prednisone dose followed by relapse before SCI
7.5 mg
9 mg
15 mg
50 mg
Duration of scleritis before SCI
(months)
63
14
36
11
Systemic treatment after SCI (last follow up)
None
Pred 4 mg
MMF 2 g
Pred 5 mg
MTX 25 mg
Pred 10 mg
Follow up
(months)
22
19
17
5
Side effects from SCI
None
Transient IOP increase LE
None
Subconjunctival haemorrhage,
Transient IOP increase LE
SCI, subconjunctival injection of triamcinolone acetonide; CsA, cyclosporine; MMF, mycophenolate mofetil; Pred, prednisone; UTI, urinary tract infection; GERD, gastrooesophageal reflux disease.
Doses in the table indicate daily oral dose for Prednisone and CsA and weekly dose for methotrexate.
* The patient was HLAB27 positive but did not have any associated systemic manifestations.
www.bjophthalmol.com
918 PostScript scleritis in appropriately selected patients and that this therapy is not unequivocally associated with the risk of scleral thinning or perforation. Local treatment with steroid injections may help reduce potential side effects from systemic therapy in patients with active scleritis in the absence of active systemic disease. As with all retrospective small case series our results should be interpreted with caution.
H N Sen, R Ursea, R B Nussenblatt,
R R Buggage
Laboratory of Immunology, National Eye Institute,
National Institutes of Health, Bethesda, MD, USA
Correspondence to: H Nida Sen, MD, National Eye
Institute, National Institutes of Health, Bldg 10, Room
10N112, Bethesda, MD 20892, USA; nidamd@yahoo.com
doi: 10.1136/bjo.2004.052738
Accepted for publication 1 November 2004
No financial support has been received for this study and the authors do not have any proprietary interest in any of the materials mentioned in the study.
References
1 Jabs DA , Mudun A, Dunn JP, et al.
Episcleritis and scleritis: clinical features and treatment results.
Am J Ophthalmol 2000; 130 :469–76.
2 Sainz de la Maza M , Jabbur NS, Foster CS. An analysis of therapeutic decision for scleritis.
Ophthalmology 1993; 100 :1372–6.
3 Watson PG . Treatment of scleritis and episcleritis.
Trans Ophthalmol Soc UK 1974; 94 :76–9.
4 Fraunfelder FT , Watson PG. Evaluation of eyes enucleated for scleritis.
Br J Ophthalmol
1976; 60 :227–30.
5 Zamir E , Read RW, Smith RE, et al.
A prospective evaluation of subconjunctival injection of triamcinolone acetonide for resistant anterior scleritis.
Ophthalmology 2002; 109 :798–805.
6 Croasdale CR , Brightbill FS. Subconjunctival corticosteroid injections for nonnecrotizing anterior scleritis.
Arch Ophthalmol 1999; 117 :966–8.
7 Tu EY , Culbertson WW, Pflugfelder SC, et al.
Therapy of nonnecrotizing anterior scleritis with subconjunctival corticosteroid injection.
Ophthalmology 1995; 102 :718–24.
8 Akpek EK , Thorne JE, Qazi FA, et al.
Evaluation of patients with scleritis for systemic disease.
Ophthalmology 2004; 111 :501–6.
Figure 1 (A) Temporal hemianopia of the right eye. Visual acuity was 20/20. (B) The optic disc of the left eye shows atrophy and glaucomatous damage, the cup-disc ratio is 1.0. Note the reflex on the retinal surface, caused by the silicone oil tamponade. (C) Axial T1 weighted MRI scans demonstrate intraocular silicone oil (S) which is hyperintensive compared to the normal vitreous (V).
Note the hyperintensive signal in the area of the intracranial portion of the optic nerve and the chiasm (arrow). (D) T2 weighted scans demonstrate hypointensive signals in the silicone filled eye
(S) as well as in the area of the optic nerve and chiasm.
Visual field defect in association with chiasmal migration of intraocular silicone oil
Silicone oil is used as a long term intraocular tamponade in vitreoretinal surgery for conditions such as rhegmatogenous retinal detachments. Complications such as silicone oil associated keratopathy, cataract formation, or emulsification with secondary glaucoma have been reported.
1 We report the unusual case of intracranial silicone oil migration with subsequent visual field defect in the fellow eye and the results of neurosurgical intervention
Case report
A 66 year old male patient had undergone cataract surgery and lens implantation on both eyes 20 months earlier. Six months after cataract surgery a retinal detachment was seen in the left eye which was first treated with pars plana vitrectomy and gas tamponade (15%
C
2
F
6
). After a period of 4 months, a redetachment occurred and silicone oil (Acri.Sil-ol 5000,
5000 cps, Acri.Tec, Hennigsdorf, Germany)
Figure 2 (A) Left optic nerve (ON) before incision. Arrows point at translucent thinned perineural sheath with silicone oil beneath. OC, entrance to optic canal; ICA, internal carotid artery. (B)
Silicone oil (arrow) evading from left optic nerve after incision of perineural sheath. (C) View into left optic nerve after complete removal of the silicone oil. The nerve has been hollowed out by the oil with just thin nerve walls remaining. (D) After intracranial surgery, a regression of the visual field defect was observed.
www.bjophthalmol.com
PostScript 919 was used as a permanent tamponade.
Postoperative visual acuity was 20/500 in the left eye. Twelve months later, the patient was referred to our institution for further evaluation of a temporal hemianopia of sudden onset in the right eye
(fig 1A) and for treatment of elevated intraocular pressure in the left eye. At presentation, visual acuity was 20/20 in the right eye and light perception in the left eye. Intraocular pressure was in a normal range in the right eye and elevated to
35 mm Hg in the left eye despite local antiglaucomatous monotherapy using latanoprost (Xalatan). Emulsified silicone oil was detected in the anterior chamber angle during gonioscopy of the left eye.
Funduscopy revealed a glaucomatous excavation and atrophy of the optic nerve in the left eye with a cup-disc ratio of 1.0
(fig 1B); the retina was attached, with the silicone oil filling of the globe being incomplete. Magnetic resonance imaging
(MRI) of the brain was then performed for further evaluation. T1 weighted MRI scan revealed a hyperintensive signal in the left vitreous cavity characteristic for silicone oil.
2 An identical hyperintensive signal was also observed in the left optic nerve and the left half of the optic chiasm (fig 1C); in contrast, in T2 weighted sections the silicone located in the optical system and in the vitreous cavity appeared hypointensive
(fig 1D). In order to prevent a further progression of the visual field defect of the right eye, a decompression of the optic nerve seemed prudent. After informed consent, the patient underwent left subfrontal craniotomy and the left optic nerve and the optic chiasm were explored. No oil was found in the subarachnoid space or in the brain tissue.
Therefore, the left optic nerve at the transition to the optic chiasma was slit open and the intrachiasmatic and intranerval silicone oil was removed by smooth suction and irrigation.
The nerve was completely hollowed out by the oil with only thin perineural structures remaining (fig 2A, B, C). At the end the small opening in the nerve was covered with a collagen fleece coated with fibrin glue
(Tachocomb H, Nycomed Pharma GmbH,
Unterschleissheim, Germany). The neurosurgical intervention was performed without intraoperative or postoperative complications.
In addition, a re-vitrectomy with gas tamponade was performed to remove the silicone oil from the vitreous cavity of the left eye. One month later, a regression of the visual field defect in the right eye was observed (fig 2D) and best corrected visual acuity was 20/32.
Intraocular pressure in the left eye was normal without treatment after surgery.
case reports. However, a histopathological study 4 previously demonstrated silicone cavities posterior to the lamina cribrosa in an silicone filled eye with glaucomatous nerve damage. The case presented in this report is unique because of the additional affection of the fellow eye as a result of optic nerve compression caused by silicone oil within the optic nerve sheath and its close proximity to the chiasm and the regression of the visual field defect after neurosurgical intervention.
D Eckle, A Kampik, C Hintschich, C Haritoglou
Department of Ophthalmology, Ludwig-Maximilians-
University, Mathildenstrasse 8, 80336 Munich,
Germany
J-C Tonn, E Uhl
Department of Neurosurgery, Klinikum Großhadern,
Ludwig-Maximilians-University, Marchioninistrasse
15, 81377 Munich, Germany
A Lienemann
Department of Diagnostic Radiology, Klinikum
Innenstadt, Ludwig-Maximilians-University,
Ziemssenstrasse 1, 81377 Munich, Germany
Correspondence to: Christos Haritoglou, MD,
Department of Ophthalmology, Ludwig-Maximilians-
University, Mathildenstrasse 8, 80336 Munich,
Germany; christos.haritoglou@med.uni-muenchen.de
doi: 10.1136/bjo.2004.062893
Accepted for publication 29 November 2004
References
1 Ni C , Wang WJ, Albert DM, et al.
Intravitreous silicone injection. Histopathologic findings in a human eye after 12 years.
Arch Ophthalmol
1983; 101 :1399–401.
2 Williams RL , Beatty RL, Kanal E, et al.
MR imaging of intraventricular silicone: case report.
Radiology
1999; 212 :151–4.
Comment
This case indicates that silicone oil can migrate intracranially under certain, yet unknown, conditions. Referring to the literature, there is only one case by Eller and co-authors 3 describing the intracranial migration of silicone oil in a patient with AIDS who had undergone vitrectomy with silicone oil tamponade for treatment of retinal detachment secondary to cytomegalovirus infection of the retina. As in our patient, there was a coincidence of uncontrolled high intraocular pressure associated with atrophy and glaucomatous damage of the optic nerve. It seems likely that elevated intraocular pressure and optic nerve atrophy allowed intraocular silicone oil to migrate intracranially, although a definite conclusion cannot be drawn from two
Figure 1 (A) Fundus photograph of the left eye showing an elliptical area of congenital retinal pigment epithelial (RPE) lesion temporal to the foveola. The lesion is depigmented in the nasal aspect with scalloped hyperpigmentation temporally. (B) Normal RPE cells, with prominent apical melanosomes and basal nuclei. Normal Bruch’s membrane and choriocapillaris (haematoxylin and eosin 6 330). (C) Hypertrophic, thickened retinal pigment epithelial cells from pigmented area of
CHRPE. These are thickened, and packed with melanosomes, in both apical and basal areas
(haematoxylin and eosin, 6 500). (D) Atrophic, thinned RPE cells from depigmented areas of CHRPE lesion. Almost no melanosomes remain in these cells (haematoxylin and eosin, 6 500). (E) Electron micrograph from hypertrophic RPE cells from pigmented areas of CHRPE. Nuclei are both apical and basal. Melanosomes are dense and rounded. Bruch’s membrane is normal (electron microscopy 6 2000). (F) Electron microscopy from the depigmented area of the CHRPE. RPE cells are atrophic and vacuolated, with very few small melanosomes. Bruch’s membrane consists of the
RPE basement membrane (arrow), a lucent thickened inner collagenous layer (below) extending to the elastic layer (middle dark layer). Note the RPE cell ( * ) within the outer collagenous layer of
Bruch’s membrane. The choriocapillaris (C) is separated from this by a thickened lucent outer collagenous layer (right), but choriocapillaris (and endothelial cell basement membrane) are missing from most areas (central and left) (electron microscopy 6 2000).
www.bjophthalmol.com
920 PostScript
Table 1 Summary of previously published histopathological findings in congenital hypertrophy of retinal pigment epithelium
(RPE)
Author
Kurz 6
Buettner 5
Shields 11
Wirz 12
Champion 7
Lloyd 8
Traboulsi 10
Parker 13
Kasner 14
Regillo 9
Present case
Year
1962
1975
1975
1982
1989
1990
1990
1990
1992
1993
2005
Age
(years)
19
62, 23
4
60
, 1
59
51
37,46
61
2
62
Type
Solitary
Solitary
Grouped
Solitary
Solitary
Solitary
FAP
FAP
FAP
Grouped
Solitary
Main histopathological findings
RPE cells Pigment granules
Size
–
Density
–
Size
Large
Hypertrophy
Normal
Hypertrophy
Hyperplasia
Hypertrophy
Hypertrophy
Hyperplasia
Hypertrophy
Hyperplasia
Hypertrophy
Hypertrophy
Hyperplasia
Normal
Hypertrophy
Atrophy
–
Normal
–
Increased Macromelanosomes
–
–
Normal
Normal
Large
Large
Large
Macromelanosomes
Large
–
Large
Large
Large
Density Shape Others
Increased Spherical Hypigmented RPE
(lacunae)
Normal overlying photoreceptors
Increased Spherical Thickened Bruch’s membrane
Atrophic RPE (lacunae)
Increased Ellipsoid
Absent overlying photoreceptors
Normal overlying photoreceptors
Increased Irregular Atrophic outer retina
Absence of lipofuscin
Increased Spherical Small microvilli
Abnormal melanogenesis
Increased Spherical Absence of lipofuscin
Abnormal phagocytosis
Increased Spherical RPE hamartoma
Increased –
Increased Spherical RPE hamartoma
Increased Ellipsoid
Choristoma
Abnormal melanogenesis
Absent RPE hypertrophy
Absent RPE hyperplasia
Increased Spherical Thickened Bruch’s membrane
FAP, familial adenomatous polyposis with or without extracolonic manifestations (Gardner’s syndrome).
3 Eller AW , Friberg TR, Mah F. Migration of silicone oil into the brain: a complication of intraocular silicone oil for retinal tamponade.
Am J Ophthalmol 2000; 129 :685–8.
4 Manschot WA . Intravitreal silicone injection.
Adv
Ophthalmol 1978; 36 :197–207.
Congenital hypertrophy of retinal pigment epithelium: a clinicopathological case report
Congenital hypertrophy of retinal pigment epithelium (CHRPE) is a peculiar congenital anomaly of the retinal pigment epithelium
(RPE) diagnosed by its characteristic ophthalmoscopic appearance.
1 It is now realised that sporadic CHRPE is distinct from the similar appearing retinal lesions described in patients with Gardner’s syndrome.
2–4 We recently enucleated an eye with a choroidal melanoma that also had a distinct area of solitary CHRPE with lacunae formation. This provided us with a unique opportunity to correlate clinical and histopathological features of a solitary CHRPE.
pigmentation. Highly pigmented temporal areas showed hypertrophic RPE cells with loss of nuclear basal polarity and variable numbers melanosomes (fig 1C). By contrast, RPE cells were thinned and atrophic in depigmented areas (fig 1D), with a marked reduction in (or loss of) melanosomes and decreased melanosome size. Between these areas, ‘‘transitional zones’’ showed variable changes. Electron microscopy confirmed that, in pigmented areas of CHRPE, hypertrophic RPE cells had dense rounded intact melanosomes, but little or no lipofuscin (fig 1E). In these areas, Bruch’s membrane was normal. Depigmented areas had thin atrophic RPE cells, with cytoplasmic vacuoles and very few, much smaller melanosomes (fig 1F). Here, Bruch’s membrane thickening (of the inner and outer collagenous layers) was most marked, with occasional insertion of RPE cells through the RPE basement membrane into the inner collagenous layer, but not beyond the elastic layer.
Case report
A 62 year old woman with a large ciliochoroidal melanoma was observed to have an elliptical retinal pigment epithelial lesion about 1 mm temporal to the foveola
(fig 1A). The lesion was about 3 mm 6 2 mm in basal dimension and appeared flat. The lesion was depigmented in the nasal aspect with scalloped hyperpigmentation temporally. The eye was enucleated and processed routinely for histological examination.
On histopathological evaluation, cilio-choroidal melanoma was confirmed. In areas just outside the CHRPE lesion, the retinal pigment epithelium (RPE) was normal (fig 1B). The pathology of the ‘‘CHRPE’’ lesion varied across the lesion, correlating with the level of
Comment
Only few reports exist regarding the histopathological findings of CHRPE and its variants (table 1). In solitary CHRPE, hypertrophic RPE cells with hyperpigmention have been reported.
5–8 Additional findings have included presence of macromelanosomes 7 and absence of lipofuscin.
8 In contrast, the grouped CHPRE is composed of normal sized
RPE cells with hyperpigmentation.
9 The
CHRPE-like lesions seen in Gardner’s syndrome show evidence of RPE hyperplasia and even hamartomatous changes in addition to
RPE hypertrophy and hyperpigmentation.
10
Our case shows many of the features previously described in CHRPE. Pathologically in our case, there appears to be gradation of changes from the pigmented areas to the non-pigmented areas. Depigmentation and atrophy of RPE cells, starting with fragmentation of melanosomes progresses to gradual loss of melanosomes and RPE atrophy. Both the fragmentation of melanosomes and eventual atrophy appear to correlate with increasing changes in Bruch’s membrane—namely, an increased thickness of the inner and outer collagenous layers, by electron lucent material may represent water, lipid or proteinaceous deposit. To our knowledge, this has not been reported previously, although review of an electron micrograph from the 23 year old patient of Buettner suggests that this feature may be present in a depigmented area of
CHRPE.
5
A close inter-reaction between the functions of RPE cells and Bruch’s membrane is well recognised. It remains possible that the depigmentation of RPE cells caused the changes in the Bruch’s membrane (‘‘ancient’’ CHRPE). It is also possible that, in our patient, changes affecting Bruch’s membrane are non-specific and are unrelated to CHRPE.
Acknowledgements
We are grateful to Mr Bart Wagner for assistance with electron microscopy and Mr Robin Farr with the graphics.
M A Parsons
Ophthalmic Sciences Unit, University of Sheffield,
Sheffield, UK
I G Rennie
Department of Ophthalmology and Orthoptics,
University of Sheffield, Sheffield, UK
P A Rundle, I G Rennie, S Dhingra
Department of Ophthalmology, Royal Hallamshire
Hospital, Sheffield, UK
H Mudhar
Department of Histopathology, Royal Hallamshire
Hospital, Sheffield, UK www.bjophthalmol.com
PostScript 921
A D Singh
Cole Eye Institute, Cleveland Clinic Foundation,
Cleveland, OH, USA
Correspondence to: Arun D Singh, MD, Department of Ophthalmic Oncology, Cole Eye Institute, Cleveland
Clinic Foundation, 9500 Euclid Avenue, Cleveland,
OH 44195, USA; singha@ccf.org
doi: 10.1136/bjo.2004.061887
Accepted for publication 29 November 2004
References
1 Gass JD . Focal congenital anomalies of the retinal pigment epithelium.
Eye 1989; 3 :1–18.
2 Blair NP , Trempe CL. Hypertrophy of the retinal pigment epithelium associated with Gardner’s syndrome.
Am J Ophthalmol 1980; 90 :661–7.
3 Traboulsi EI , Maumenee IH, Krush AJ, et al.
Pigmented ocular fundus lesions in the inherited gastrointestinal polyposis syndromes and in hereditary nonpolyposis colorectal cancer.
Ophthalmology 1988; 95 :964–9.
4 Shields JA , Shields CL, Shah PG, et al.
Lack of association among typical congenital hypertrophy of the retinal pigment epithelium, adenomatous polyposis, and Gardner syndrome.
Ophthalmology 1992; 99 :1709–13.
5 Buettner H . Congenital hypertrophy of the retinal pigment epithelium.
Am J Ophthalmol
1975; 79 :177–89.
6 Kurz GH , Zimmerman LE. Vagaries of the retinal pigment epithelium.
Int Ophthalmol Clin
1962; 2 :441–64.
7 Champion R , Daicker BC. Congenital hypertrophy of the pigment epithelium: light microscopic and ultrastructural findings in young children.
Retina
1989; 9 :44–8.
8 Lloyd WC 3rd , Eagle RC Jr, Shields JA.
Congenital hypertrophy of the retinal pigment epithelium. Electron microscopic and morphometric observations.
Ophthalmology
1990; 97 :1052–60.
9 Regillo CD , Eagle RC Jr, Shields JA, et al.
Histopathologic findings in congenital grouped pigmentation of the retina.
Ophthalmology
1993; 100 :400–5.
10 Traboulsi EI , Murphy SF, de la Cruz ZC, et al.
A clinicopathologic study of the eyes in familial adenomatous polyposis with extracolonic manifestations (Gardner’s syndrome).
Am J Ophthalmol 1990; 110 :550–61.
11 Shields JA , Tso MO. Congenital grouped pigmentation of the retina. Histopathologic description and report of a case.
Arch
Ophthalmol 1975; 93 :1153.
12 Wirz K , Lee WR, Coaker T. Progressive changes in congenital hypertrophy of the retinal pigment epithelium.
Graefes Arch Clin Exp Ophthalmol
1982; 219 :214–21.
13 Parker JA , Kalnins VI, Deck JH, et al.
Histopathological features of congenital fundus lesions in familial adenomatous polyposis.
Can J Ophthalmol 1990; 25 :159–63.
14 Kasner L , Traboulsi EI, Delacruz Z, et al.
A histopathologic study of the pigmented fundus lesions in familial adenomatous polyposis.
Retina
1992; 12 :35–42.
Figure 1 (A) B-scan ultrasound demonstrated a large intraocular tumour with scleral thickening and retrobulbar oedema. There was almost no intrinsic vascularity noted within the tumour.
No extrascleral tumour extension was noted.
(B) A-scan ultrasonography of the right eye showed relative low internal reflectivity. (C) MRI of the orbits was significant for an intraocular tumour that displayed high signal intensity on
T1 weighted images. On T2 weighted images it displayed low signal intensity. Note the small eccentric collar-button (arrow). There was no evidence of extraocular tumour extension.
showed no light perception, a relative afferent pupillary defect, a shallow anterior chamber, and an intraocular pressure of 58 mm Hg.
Dense vitreous haemorrhage and tumour obscured her fundus.
Three dimensional ultrasonography revealed vitreous haemorrhage, a total retinal detachment, and a large choroidal mass
(fig 1A, B). Computed tomography and magnetic resonance imaging (MRI) of the orbits showed a 2 cm intraocular mass with a collar-button extension (arrow) consistent with a choroidal melanoma (fig 1C).
The patient participated in a discussion of the risks and benefits of treatment, found primary enucleation unacceptable, and preferred fine needle aspiration biopsy (FNAB) before treatment.
Cytology
Transvitreal FNAB showed small, well preserved, spindle-shaped, dendritic, and epithelioid cells with evenly distributed melanin pigmentation (fig 2A) and no evidence of malignancy. Both cytology and subsequent immunohistochemistry were consistent with melanocytoma.
Though a combination of topical glaucoma medications and oral prednisone decreased her ocular pain, the patient consented to enucleation.
Macroscopic examination
A large evenly pigmented choroidal mass measuring 12 mm in height and 17 6 18 mm in greatest dimension was noted. The tumour extended from the ciliary body to the optic disc.
Light microscopy
Extensive infarction of the tumour was present. The cell outlines revealed a tumour composed of uniform large and heavily pigmented cells with round, small central nuclei. Many of these cells were magnocellular and histopathologically consistent with melanocytoma. However, distinct cells with larger nuclei and prominent nucleoli were present singly and in small clusters. In these areas, rare atypical mitoses were noted. These features were diagnostic of malignant transformation of a large melanocytoma (fig 2B).
At 6 months post-enucleation there is no evidence of metastatic disease.
Finding malignant change in a necrotic choroidal melanocytoma: a clinical challenge
Melanocytic intraocular tumours can grow as to exceed their vascular supply, become necrotic, and induce inflammation. They present with atypical signs and become a diagnostic challenge. We present a case of a large melanocytic intraocular tumour that offered an atypical presentation, unexpected cytology, and finally diagnostic histopathology.
Case report
A 37 year old white woman presented with a painful right eye and vision loss. Examination
Figure 2 (A) The cytological preparations from FNAB showed very small, pigmented dendritic and epithelioid cells with small dark oblong nuclei. No mitoses or necrosis was present. Some of the very deeply pigmented cells seen were melanophages. These cells were naevus-like, there were no cells that were large enough or that had appropriate nuclear morphology to be called melanoma
(original magnification 6 100). (B) Histopathology of the enucleated eye showed a necrotic tumour
(left inset; original magnification 6 100). Histopathology demonstrated spindle and small epithelioid melanoma cells (right inset; original magnification 6 100) and a melanoma with a mitotic figure in the centre (arrow). These findings suggested malignant change (original magnification 6 100).
www.bjophthalmol.com
922 PostScript
Comment
Melanocytomas are darkly pigmented tumours that commonly arise at the optic nerve margin.
They also occur in the iris, ciliary body, and the choroid. Though largely benign and stationary, melanocytomas can (albeit rarely) undergo malignant transformation.
1–8 When this occurs, it can be difficult to differentiate between melanocytomas and malignant melanomas by ultrasonography or fluorescein angiography.
Adenoma and adenocarcinoma of the retinal pigment epithelium should also be considered.
In this case, FNAB did not establish the diagnosis of a malignant melanocytoma and clearly demonstrates the potential danger of relying on FNAB (alone) for the diagnosis in atypical and necrotic intraocular tumours.
Foci of malignant change were missed, leading to the diagnosis of melanocytoma.
Fortunately, enucleation was performed.
This case also demonstrates that melanocytomas can undergo necrosis resulting in atypical features such as opaque media, pain and inflammation. They can induce vasoocclusive disease within the optic nerve, ischaemic necrosis of the tumour, ischaemic retinopathy, neovascular glaucoma, and melanocytic glaucoma.
9 Since both necrotic melanocytomas and necrotic malignant uveal melanomas can present with the same acute symptoms (pain, inflammation, and an elevated intraocular pressure), these findings can detract the clinician’s ability to differentiate between these tumours.
Malignant change in a melanocytoma is a rare event. It is actually more common for a uveal melanoma to undergo spontaneous necrosis and present with intraocular inflammation, haemorrhage, secondary neovascularisation, and orbital inflammation. Such necrotising tumours have an increased incidence of penetration through the Bruch’s membrane, scleral invasion, and extrascleral extension.
10 Clearly, large necrotic intraocular tumours can be a diagnostic challenge for both clinician and pathologist.
M Kurli, P T Finger, T Manor
New York Eye Cancer Center, New York, USA
M Kurli, S A McCormick
The New York Eye and Ear Infirmary, New York, USA
P T Finger
New York University School of Medicine, and New
York Eye and Ear Infirmary, New York, USA
H E Grossniklaus
Emory University School of Medicine, Atlanta, GA,
USA
Correspondence to: Paul T Finger, MD, The New York
Eye Cancer Center, 115 East 61st Street, New York
City, NY 10021, USA; pfinger@eyecancer.com
doi: 10.1136/bjo.2004.060038
Accepted for publication 28 November 2004
This work is supported by The Eye Care Foundation,
Inc, and Research to Prevent Blindness, New York
City, NY, USA.
The authors have no proprietary interest in the products mentioned in this study.
References
1 Zimmerman LE . Melanocytic tumors of interest to the ophthalmologist.
Ophthalmology
1980; 87 :497–502.
2 Reidy JJ , Apple DJ, Steinmetz RL, et al.
Melanocytoma: nomenclature, pathogenesis, natural history and treatment.
Surv Ophthalmol
1985; 29 :319–27.
3 Roth AM . Malignant change in melanocytomas of the uveal tract.
Surv Ophthalmol
1978; 22 :404–12.
4 Apple DJ , Craythorn JM, Reidy JJ, et al.
Malignant transformation of an optic nerve melanocytoma.
Can J Ophthalmol
1984; 19 :320–5.
5 Barker-Griffith AE , McDonald RP, Green WR.
Malignant melanoma arising in a choroidal magnocellular nevus (melanocytoma).
Can J Ophthalmol 1976; 11 :140–6.
6 Heitman KF , Kincaid MC, Steahly L. Diffuse malignant change in a ciliochoroidal melanocytoma in a patient of mixed racial background.
Retina 1988; 8 :67–72.
7 Leidinix M , Mamalis N, Goodart R, et al.
Malignant transformation of a necrotic melanocytoma of the choroid in an amblyopic eye.
Ann Ophthalmol 1994; 26 :42–6.
8 Shetlar DJ , Folberg R, Gass JDM. Choroidal malignant melanoma associated with a melanocytoma.
Retina 1999; 19 :346–9.
9 Teichmann KD , Karcioglu ZA. Melanocytoma of the iris with rapidly developing secondary glaucoma.
Surv Ophthalmol 1995; 40 :136–44.
10 Moshari A , Cheeseman EW, McLean IW.
Totally necrotic choroidal and ciliary body melanomas: associations with prognosis, episcleritis and scleritis.
Am J Ophthalmol 2001; 131 :232–6.
Improvement after transvitreal limited arteriovenous crossing manipulation without vitrectomy for complicated branch retinal vein occlusion using 25 gauge instrumentation
Although arteriovenous adventitial sheathotomy (AAS) has been proposed as an alternative treatment for patients with branch retinal vein occlusion (BRVO) complicated by macular haemorrhage, persistent macular oedema after grid laser photocoagulation, and macular ischaemia, the inner retinal incision may increase the risk of retinal detachment and spontaneous vitreous haemorrhage.
1–3 Han et al.
2 recently proposed that incomplete separation of the common adventitial sheath without lysis may achieve comparable results. Thus, we propose transvitreal limited arteriovenous crossing manipulation
(LAM) without vitrectomy as an alternative to
AAS.
Case report
A 70 year old man with a medical history of hypertension, presented with BRVO of
14 weeks’ duration, visual acuity of 7/200, intraretinal macular haemorrhages, macular oedema assessed by ocular coherence tomography, and capillary non-perfusion on fluorescein angiography (fig 1). After informed consent and institutional review board approval was obtained, the patient underwent LAM without vitrectomy using the
25 gauge transconjunctival standard vitrectomy system (MADLAB, Bausch & Lomb, St
Louis, MO, USA). Next, the blunt, flexible extendable pick (MADLAB) was introduced into the vitreous, and, once extended, makes a slit in the internal limiting membrane approximately 1.5 mm next to the pathological arteriovenous crossing. Then, LAM was initiated by first lifting the proximal portion of the artery followed by the portion distal to the crossing. Then, the artery was lifted at the crossing site, stretching but not severing the common adventitial sheath. Visualisation of clot dislodgement and reperfusion were noted. No vitrectomy was performed and no vitreous cutter was used during the procedure. There was no evidence of posterior vitreous detachment.
Figure 1 Preoperative fundus photography, fluorescein angiography, and optical coherence tomography. (A) Fundus photography of the left eye exhibiting severe intraretinal haemorrhage and macular oedema secondary to superotemporal secondary order branch retinal vein occlusion.
Arrowhead denotes site of occlusion. The course of the vein is outlined by the white dots underneath and points towards 2 o’clock from the optic disc. (B) Fluorescein angiography of the left eye at
12 seconds exhibiting widespread blocked fluorescence secondary to haemorrhage, hyperfluorescence of the vessel wall, and extensive capillary dropout estimated at 10 disc diameters with vessel ‘‘pruning.’’ Arrowhead denotes site of occlusion. The course of the occluded vein is better outlined in this angiogram by the underlying white dots. (C) Fluorescein angiography of the left eye at 4 minutes exhibiting consistent capillary dropout, blocked fluorescence secondary to haemorrhage, and extensive leakage along capillary vessel walls. Arrowhead denotes site of occlusion. (D) Optical coherence tomography of the left eye exhibiting extensive macular oedema with large cystic spaces in the foveal region. Foveal thickness was calculated to be 512 m m.
www.bjophthalmol.com
PostScript 923
2 Han DP , Bennett SR, Williams DF, et al.
Arteriovenous crossing dissection without separation of the retina vessels for treatment of branch retinal vein occlusion.
Retina
2003; 23 :145–51.
3 Mason J 3rd , Feist R, White M Jr, et al . S.
eathotomy to decompress branch retinal vein occlusion: a matched control study.
Ophthalmology 2004; 111 :540–5.
4 Fujii GY , de Juan E Jr, Humayun MS.
Improvements after sheathotomy for branch retinal vein occlusion documented by optical coherence tomography and scanning laser ophthalmoscope.
Ophthalmic Surg Lasers
Imaging 2003; 34 :49–52.
‘‘Ecstasy’’ induced immunosuppression and herpes zoster ophthalmicus
It is uncommon for younger patients to develop herpes zoster ophthalmicus (HZO) without underlying immunocompromise.
3,4-Methylenedioxymethamphetamine
(MDMA, ‘‘ecstasy’’) is a widely abused psychomotor stimulant shown to cause a transient immunosuppression.
1–4 In this report, we present the relation between MDMA induced immune dysfunction and the development of
HZO in a previously healthy young male.
Figure 2 Postoperative fundus photography, fluorescein angiography, and optical coherence tomography. (A) Fundus photography of the left eye exhibiting marked resolution of intraretinal haemorrhage and macular oedema, particularly in the foveal region. Arrowhead denotes site of previously complete occlusion. The course of the now ghost vessel is outlined by the white dots underneath. (B) Fluorescein angiography of the left eye at 10 seconds exhibiting noticeably decreased blocked fluorescence secondary to haemorrhage, continued hyperfluorescence of the vessel wall, and extensive but decreased capillary dropout estimated at approximately 5 disc diameters. Persistent, but less severe, vessel ‘‘pruning’’ was also evident. Arrowhead denotes site of previously complete occlusion. (C) Fluorescein angiography of the left eye at 6 minutes exhibiting decreased capillary dropout, persistent blocked fluorescence secondary to haemorrhage, and decreased leakage along capillary vessel walls. Decreased leakage is particularly noted in the foveal region. Arrowhead denotes site of occlusion. The course of the occluded vein is outlined in this angiogram by the underlying white dots. (D) Optical coherence tomography of the left eye exhibiting markedly decreased macular oedema and the absence of cystic spaces. Foveal thickness was calculated to be 133 m m.
At the 2 month postoperative visit, the patient’s visual acuity was 20/40. Fundus photography and fluorescein angiography revealed markedly decreased intraretinal haemorrhages and good macular perfusion, respectively. Macular thickness decreased from 512 m m to 133 m m on optical coherence tomography (fig 2). No cataract progression was noted and intraocular pressure remained stable throughout the postoperative course.
The patient has remained stable for over
12 months.
Comment
Our group has previously published a case report of 25 gauge AAS with vitrectomy where improvement was noted in visual acuity, macular thickness (as measured by optical coherence tomography), and refixation (as shown by scanning laser ophthalmoscopy).
4 Han et al 2 postulated that incomplete separation of the common adventitial sheath may be an alternative to AAS. The LAM without vitrectomy procedure may provide a minimally invasive way of clot dislodgment and reperfusion without need for large retinal incisions near retinal vessels as with AAS.
Although this intervention may suggest benefit, it is certainly possible that the macular oedema spontaneously resolved as a result of reperfusion from recanalisation. We are uncertain as to which of these factors (LAM or recanalisation) resulted in significant improvement. It is our belief that the reperfusion after the procedure was mainly responsible for the dramatic clearing of haemorrhage and the resolution of the macular oedema. A prospective, randomised trial examining the potential benefits of 25 gauge without vitrectomy and
20 gauge AAS with vitrectomy procedures for
BRVO is warranted.
R R Lakhanpal, M Javaheri, R A Equi,
M S Humayun
Microsurgery Advanced Design Laboratory
(MADLAB), Doheny Retina Institute, Doheny Eye
Institute, Department of Ophthalmology, Keck School of Medicine, University of Southern California, Los
Angeles, CA, USA
Correspondence to: Mark S Humayun, MD, PhD,
Doheny Retina Institute, Doheny Eye Institute,
Department of Ophthalmology, Keck School of
Medicine, University of Southern California, 1450 San
Pablo Street (Room 3600), Los Angeles, CA 90033,
USA; humayun@usc.edu
doi: 10.1136/bjo.2004.061739
Supported in part by NIH grant for vision research
EY03040 and by an unrestricted grant from Research to Prevent Blindness.
The blunt 25 gauge nitinol flexible extendable retinal pick and the transconjunctival standard vitrectomy system (TSV) are disclosed to Bausch & Lomb Surgical,
St Louis, MO, USA. The Microsurgery Advanced
Design Laboratory (MADLAB) at the Doheny Retina
Institute may receive royalties related to the sale of these instruments mentioned in this article to defray operating costs. The authors have no proprietary interests in any instrumentation in this article.
References
1 Opremcak EM , Bruce RA. Surgical decompression of branch retinal vein occlusion via arteriovenous crossing sheathotomy: a prospective review of 15 cases.
Retina
1999; 19 :1–5.
Case report
A 24 year old African-American male without significant past medical history presented with an eruptive, vesicular rash on his left forehead and eyelid consistent with the diagnosis of herpes zoster ophthalmicus
(fig 1). Although he reported using safe sexual practice and denied injecting drug use, he admitted using an oral drug, ecstasy, three times a day for 4 days before the development of his symptoms. He tested negative for HIV and underlying malignancy, and slowly improved on intravenous aciclovir during his admission
Varicella zoster reactivation is a potential complication of immunosuppression. Predisposing factors to reactivation include increasing age, neoplastic diseases, HIV, immunosuppressive therapy, or debilitating systemic disease.
5 Since zoster in patients under
50 years old is uncommon, a search for predisposing factors is indicated. It has been shown, in short term studies, that ecstasy use results in immune suppression.
1–4 Therefore, we believe that our patient’s prolonged use of ecstasy facilitated the development of HZO.
3,4-Methylenedioxymethamphetamine is a widely abused psychomotor stimulant with behavioural effects similar to those elicited by amphetamines and hallucinogens. MDMA has become a popular drug of abuse over the past two decades.
3 A study in 1988 found that 39% of students on a college campus admitted to having taken the drug at least once in the previous year.
6 Surveys have also shown a steady increase in MDMA use in 8th, 10th, and
12th graders.
7 MDMA produces a profound euphoria, heightened feelings of empathy, emotional warmth, and self acceptance.
7
Adverse effects include hyperthermia, seizures, cardiac arrhythmias, hepatotoxicity, and many psychiatric disorders.
8 There has been an increase in reports of presumed ecstasy related fatalities and severe adverse effects such as aortic dissection and myocardial infarction.
9 10
Connor et al 1 3 4 demonstrated that acute
MDMA administration produced a variety of time dependent neurochemical, endocrine, and immune alterations in rats. Their studies www.bjophthalmol.com
924 PostScript
Figure 1 A 24 year old patient developed herpes zoster ophthalmicus after using the drug
‘‘ecstasy.’’ provided evidence that a single administration of MDMA induces a rapid and sustained suppression of induced lymphocyte proliferation and a decrease in circulating lymphocytes. The alterations in immune function were accompanied by a significant increase in plasma corticosterone concentrations. They hypothesised that users of MDMA may have reduced immunocompetence and therefore display increased susceptibility to both infectious and neoplastic disease.
1
In a study by Pacifici et al 2 it was shown that MDMA administered to humans at doses compatible with its recreational use caused rapid changes in certain immunological parameters. They demonstrated that
1 hour after administration, there was a significant reduction in CD4 T cell count and an increase in natural killer cell count.
These changes in immune function were also linked to increased cortisol concentration.
2
Comment
The studies discussed above provide evidence for the relation between MDMA and immune dysfunction. We have demonstrated a case where MDMA abuse led to the development of herpes zoster ophthalmicus. This relation has important implications for the examination of an atypical infectious process. Given the rising use of MDMA, especially among high school and college students, this consequence is a significant public health concern. Not only is it important to gather history regarding the use of illicit drugs, but also to stress the negative impact this drug can have on potential users. We anticipate more reports of infectious diseases related to
MDMA use. Further studies are necessary to define the mechanisms by which MDMA causes immune dysfunction and to determine long term effects in humans.
O M Zwick
UCSF-Department of Ophthalmology, 400 Parnassus
Avenue, A-750, San Francisco, CA 94143–0344,
USA
D H Fischer, J C Flanagan
Wills Eye Hospital, 840 Walnut Street, Philadelphia,
PA 19107, USA
Correspondence to: Orin M Zwick, MD, UCSF-
Department of Ophthalmology, 400 Parnassus
Avenue, A-750, San Francisco, CA 94143–0344,
USA; ozwickmd@yahoo.com
doi: 10.1136/bjo.2004.061150
Accepted for publication 2 November 2004
References
1 Connor TJ , McNamara MG, Finn D, et al.
Acute
3,4-methylenedioxymethamphetamine (MDMA) administration produces a rapid and sustained suppression of immune function in the rat.
Immunopharmacology 1998; 38 :253–60.
2 Pacifici R , Zuccaro P, Lopez H, et al.
Acute effects of 3,4-methylenedioxymethamphetamine alone and in combination with ethanol on the immune system in humans.
J Pharmacol Exp Ther
2001; 296 :207–15.
3 Connor TJ . Methylenedioxymethamphetamine
(MDMA, ‘‘Ecstasy’’): a stressor on the immune system.
Immunology 2004; 111 :357–67.
4 Connor TJ , Kelly JP, Leonard BE. An assessment of the acute effects of the serotonin releasers methylenedioxymethamphetamine, methylenedioxyamphetamine and fenfluramine on immunity in rats.
Immunopharmacology
2000; 46 :223–35.
5 Gnann JW Jr , Whitley RJ. Clinical practice.
Herpes zoster.
N Engl J Med 2002; 347 :340–6.
6 Peroutka SJ . Incidence of recreational use of 3,4methylenedimethoxymethamphetamine (MDMA,
‘‘ecstasy’’) on an undergraduate campus.
N Engl J Med 1987; 317 :1542–3.
7 Koesters SC , Rogers PD, Rajasingham CR.
MDMA (‘‘ecstasy’’) and other ‘‘club drugs’’: the new epidemic.
Pediatr Clin North Am
2002; 49 :415–33.
8 Burgess C , O’Donohoe A, Gill M. Agony and ecstasy: a review of MDMA effects and toxicity.
Eur Psychiatry 2000; 15 :287–94.
9 Qasim A , Townend J, Davies MK. Ecstasy induced acute myocardial infarction.
Heart 2001; 85 :e10.
10 Duflou J , Mark A. Aortic dissection after ingestion of ‘‘ecstasy’’ (MDMA).
Am J Forensic Med Pathol
2000; 21 :261–3.
Reversible posterior leucoencephalopathy syndrome: a cause of temporary cortical blindness
Reversible posterior leucoencephalopathy
(RPLS) describes a syndrome of headaches, confusion, seizures, and visual disturbances associated with transient characteristic lesions on neuroimaging, predominantly affecting the posterior region of the brain.
1 RPLS affects patients with hypertension, eclampsia, renal failure, and those on immunosuppressants and chemotherapeutic agents. We discuss a case of
RPLS that presented primarily with visual symptoms.
the white matter of the occipital and parietal regions (fig 1).
Cerebral arteriography revealed a normal intracranial circulation.
Nifedipine was prescribed to control the patient’s mean arterial blood pressure to approximately 90 mm Hg. The chemotherapy regimen was not changed because he was between courses. His GCS score and speech improved. Two weeks later, his visual acuity had improved to 6/12 in both eyes. A repeat
MRI scan, 23 days after the first study, showed a dramatic improvement with slight residual signal change in the parieto-occipital region on T
2 weighted images (fig 2). Nine months after the onset of symptoms, and having completed his chemotherapy, he maintains a visual acuity of 6/6 in the right eye and 6/9 in the left eye, with full visual fields and normal colour vision.
Comment
RPLS is characterised by altered mental status, headache, seizures, and visual disturbance, often occurring in patients receiving chemotherapy. Seventy six per cent of children with RPLS have at least three of these four signs.
2 The most common visual abnormality is cortical blindness but homonymous hemianopia, visual neglect, and blurred vision can also occur. Patients are commonly hypertensive at presentation, but this may be mild.
As illustrated, areas of temporarily increased signal intensity (representing white matter oedema) in the posterior regions of the cerebral hemispheres on T
2 sequences are characteristic.
3 weighted MRI
Sparing of the calcarine fissure and paramedian occipital lobe structures aids in the differentiation of RPLS from bilateral infarction of the posterior cerebral artery territory.
4 Although the parietooccipital region is principally affected, the syndrome may affect the frontal lobes, basal ganglia, brainstem, or cerebellum.
1
While not completely understood, the cerebral oedema is thought to result from increased vascular permeability and cerebral hyperperfusion as a result of a combination of autoregulatory failure in the cerebral vessels and hypertension.
4 This patient was treated with methotrexate and cytarabine,
Case report
A 10 year old boy with B cell acute lymphoblastic leukaemia affecting his maxilla was commenced on chemotherapy with intravenous vincristine and cyclophosphamide, oral prednisolone and folinic acid, together with intrathecal methotrexate, cytarabine, and hydrocortisone for central nervous system extension.
Ten days after the onset of chemotherapy he complained of sudden bilateral visual loss.
On examination his visual acuity was perception of light in both eyes. His pupils were equal and reactive to light and funduscopy was normal; there was no other neurological deficit. His blood pressure was elevated at
150/102 mm Hg. Over the next 24 hours his speech and conscious state became disturbed, his Glasgow coma scale (GCS) score dropped to 7/15 and he developed increased tone and clonus on his left side. A computed tomography (CT) scan showed symmetrical areas of low density involving both occipital and parietal regions associated with mild swelling. A magnetic resonance imaging (MRI) scan, 24 hours after the onset of symptoms, revealed extensive high signal intensity changes on T
2 weighted sequence involving
Figure 1 Axial T
2 weighted magnetic resonance imaging scan, 24 hours after the onset of symptoms, showing high signal intensity involving the white matter of both occipital lobes (arrows).
www.bjophthalmol.com
PostScript 925
Figure 2 Axial T
2 weighted magnetic resonance imaging scan, 23 days later, showing a reduction in signal intensity at the occipital lobes.
both of which have been reported to cause
RPLS.
5 6 These drugs may have a direct cytotoxic effect on vascular endothelial cells, may induce and exacerbate hypertension and may lower seizure threshold.
7 Intrathecal chemotherapy may cause cerebral vasospasm, contributing to cerebral vascular autoregulation impairment.
8 The parieto-occipital region may be preferentially involved because of less extensive sympathetic innervation of the posterior cerebral circulation compared to other intracranial arteries, 9 which reduces the ability of an already impaired cerebral autoregulation to compensate.
This case illustrates that the neurological impairment from RPLS is substantially reversible with prompt treatment of the associated hypertension and the dose reduction or discontinuation of inciting drugs.
1 It highlights the importance of the recognition of
RPLS and the prompt start of appropriate treatment to prevent irreversible brain injury.
N Niyadurupola, C A M Burnett, L E Allen
Department of Ophthalmology, Addenbrooke’s
Hospital, Hills Road, Cambridge, CB2 2QQ, UK
Correspondence to: Nuwan Niyadurupola,
Department of Ophthalmology, Addenbrooke’s
Hospital, Hills Road, Cambridge, CB2 2QQ, UK; nuwan.niya@doctors.org.uk
Consent: Full written consent was obtained.
doi: 10.1136/bjo.2004.060400
Accepted for publication 16 November 2004
Competing interests: none declared
4 Singhi P , Subramanian C, Jain V, et al.
Reversible brain lesions in childhood hypertension.
Acta
Paediatr 2002; 91 :1005–7.
5 Gay CT , Bodensteiner JB, Nitschke R, et al.
Reversible treatment-related leukoencephalopathy.
J Child Neurol
1989; 4 :208–13.
6 Vaughn DJ , Jarvik JG, Hackney D, et al.
High dose cytarabine neurotoxicity: MR findings during the acute phase.
Am J Neuroradiol
1993; 14 :1014–16.
7 Shin RK , Stern JW, Janss AJ, et al.
Reversible posterior leukoencephalopathy during the treatment of acute lymphoblastic leukaemia.
Neurology 2001; 56 :388–91.
8 Henderson RD , Rajah T, Nicol AJ, et al.
Posterior leukoencephalopathy following intrathecal chemotherapy with MRA-documented vasospasm.
Neurology 2003; 60 :326–8.
9 Edvinsson L , Owman C, Sjoberg NO. Autonomic nerves, mast cells and amine receptors in human brain vessels: histochemical and pharmacologic study.
Brain Res 1976; 115 :377–93.
Morquio syndrome: electron microscopic findings
Mucopolysaccharidoses (MPS) are a group of hereditary storage diseases secondary to deficiencies of lysosomal enzymes. MPS type
IV is known as Morquio syndrome.
1 In
‘‘classic’’ or type A Morquio syndrome the deficient enzyme is N-acetylgalactosamine-6sulphate-sulphatase.
2 Morquio syndrome has been associated with cataract, 3 optic atrophy, 4 tapetoretinal pigmentary degeneration, 4 5 and corneal clouding.
4 6–8 We report a case of type
A Morquio syndrome with electron microscopic findings.
Case report
A 38 year old man was referred for consideration of left corneal grafting for progressive corneal haziness of several years’ duration.
He was diagnosed with Morquio syndrome in childhood on the basis of severe growth retardation, skeletal dysplasia, and facial dysmorphism. Subsequently, a diagnosis of type A Morquio syndrome was confirmed on enzyme assay of skin fibroblasts. On examination visual acuities were 6/12 right eye and
6/18 left eye. There was bilateral corneal oedema and stromal haze, greater on the left, precluding fundal examination. His intraocular pressures were normal and his angles, although poorly visualised, appeared open.
Following an uneventful left penetrating keratoplasty the host cornea was examined by light, transmission and scanning electron microscopy.
On light microscopy, the basal cells of the epithelium were swollen as a result of oedema but both the epithelium and
Bowman’s membrane were of uniform thickness. In paraffin sections the spaces around the keratocytes were enlarged, but this was because of fixation artefact and this abnormality was not seen in the toluidine blue sections. The stroma around the enlarged spaces contained a thin dense border which stained with Alcian blue but not with colloidal iron/periodic acid Schiff or mucicarmine. Descemet’s membrane and the endothelial monolayer were of uniform thickness.
In the toluidine blue sections the stroma appeared hypercellular and had a disorderly lamellar pattern. Both the keratocytes and the endothelium contained numerous intracytoplasmic bodies.
At the ultrastructural level, the epithelium contained abnormal inclusion bodies. In areas of the epithelium, the apical portion of the basal cells was packed with small clear membrane-bound vacuoles which decreased in numbers in the wing cell and superficial cell layers. In other sectors the epithelium appeared normal. There were sectors where the basement membrane was markedly thickened and Bowman’s membrane was discontinuous in small areas where fibrocytic and/or inflammatory cells were invading beneath the basal layer. Numerous small unmyelinated nerves were distributed throughout the basal cell layer.
References
1 Hinchey J , Chaves C, Appignani B, et al.
A reversible posterior leukoencephalopathy syndrome.
N Engl J Med 1996; 334 :494–500.
2 Pavlakis SG , Frank Y, Chusid R. Hypertensive encephalopathy, reversible occipitoparietal encephalopathy, or reversible posterior leukoencephalopathy: three names for an old syndrome.
J Child Neurol 1999; 14 :277–81.
3 Suminoe A , Matsuzaki A, Kira R, et al.
Reversible posterior leukoencephalopathy syndrome in children with cancers.
J Paed Haem Oncol
2003; 25 :236–9.
Figure 1 (A) Within the cytoplasm an irregular electron dense mass (arrowhead) is surrounded by concentric membranes (arrow). A granular deposit is present in the stroma around the cell membrane ( * ) ( 6 120 000). (B) Normal keratocytes were absent from the stroma—the cytoplasm of each cell contained inclusions although the content was variable. Some cells were disrupted by the volume of the inclusions (arrow): many of the cells were surrounded by a layer of electron dense granular material (arrowheads). The corneal lamellae were distorted by the swollen cells ( 6 3800).
www.bjophthalmol.com
926 PostScript
Correspondence to: T Leslie, Department of
Ophthalmology, Grampian University Teaching
Hospitals, Aberdeen AB25 2ZN, UK; thorfinnleslie@ hotmail.com
doi: 10.1136/bjo.2004.055400
Accepted for publication 12 November 2004
Competing interests: none declared
Figure 2 (A) In some sectors Bowman’s layer was absent and the epithelium was in contact with fibrous tissue over a thick basement membrane (arrow). Intracytoplasmic bodies were absent from the fibroblasts within the fibrous tissue (arrowheads) ( 6 3800). (B) At lower magnification the inclusions appear to be amorphous in parts, but this represents the concentric lamellar material. The lamellae contain spindle-shaped strips of wide banded collagen (arrowhead). The cell with preserved cytoplasm containing inclusions is surrounded by a layer of electron dense granular material (arrows) ( 6 9600). (C) Descemet’s membrane is of normal thickness. The endothelium contains membranous inclusions, which accumulate to such a level that the cells are cystic (arrow)
( 6 4500). (D) When examined by scanning electron microscopy, the posterior endothelial surface is nodular as a result of the accumulation of intracytoplasmic inclusions. Linear areas of cell disruption are present ( 6 850).
Every keratocyte, to a varying degree, appeared to be involved in the overproduction of mucopolysaccharide and glycolipids.
Intracytoplasmic inclusions in the form of multilaminar bodies, fingerprint whorl patterns, fibrillogranular inclusions, small lipid vacuoles, and clear vacuoles were all observed
(figs 1 and 2). The collagen bundles in the stromal lamellae appeared normally aligned but scattered throughout the stroma were distended spaces or lacunae occupied by disrupted keratocytes and these distorted the lamellae. In the stromal lamellae around the keratocyte lacunae, there was deposition of an encircling layer of granular material and bundles of wide banded collagen fibres were present in the surrounding corneal stroma (fig 2).
The endothelial cell cytoplasm contained similar abnormalities to those described in the keratocytes with small clear membrane bound vacuoles which had fused to form large empty cytoplasmic spaces causing the cell membranes to collapse. By scanning electron microscopy the endothelial cells possessed a cobblestone appearance because of numerous small nodular bulges on the apical surface but the majority were of normal size and shape and the hexagonal integrity groups of degenerate cells with cytoplasmic disruption were scattered throughout the monolayer. The graft remained clear with no evidence of recurrence 2 years postoperatively with a best corrected visual acuity of 6/6.
Comment was maintained.
Small linear
This patient had corneal opacification but none of the other common ocular associations of Morquio syndrome.
3–8 As with the two previous studies which investigated the corneal opacification type A Morquio syndrome with electron microscopy.
7 8 We found the most obvious abnormality to be mocopolysaccharide inclusions in the form of intracytoplasmic, multilaminar concentric bodies particularly within keratocytes but also affecting the epithelium and endothelium. The degree of keratocyte disruption was striking and possibly related to the late stage of the disease in this case. We confirmed the previous findings of bundles of abnormal collagen fibres, which were present in the corneal stroma around the lacunae 6 8 and of areas of epithelial membrane bound vacuoles.
7
We identified areas of basement membrane thickening and areas where Bowman’s layer was discontinuous with fibrocytic and/or inflammatory cells invading beneath the basal layer. Numerous small unmyelinated nerves were distributed throughout the basal cell layer. These epithelial changes have not been commented on previously and are possibly secondary to the epithelial oedema which had been identified in this case by light microscopy.
Although early recurrence of opacification has been reported 4 the corneal graft in this case remains clear at the 2 year follow up.
T Leslie, M A R Siddiqui
Department of Ophthalmology, Grampian University
Teaching Hospitals, Aberdeen, UK
D A Aitken, C M Kirkness, W R Lee
Department of Ophthalmology, Gartnavel General
Hospital, Glasgow, UK
A I Fern
Department of Ophthalmology, Hairmyres General
Hospital, East Kilbride, UK
References
1 Morquio L . Sur une forme de dystrophie osseusse familiale.
Arch Med Enfants 1929; 32 :129–40.
2 Matalon R , Arbogast B, Jusice P, et al.
Morquio’s syndrome: deficiency of a chondroitin sulphate Nacetylhexosamine sulfate sulfatase.
Biochem
Biophys Res Commun 1974; 61 :759–65.
3 Olsen H , Baggesen K, Sjolie AK. Cataracts in
Morquio syndrome (mucopolysaccharidosis IV A).
Ophthalmic Paediatr Genet 1993; 14 :87–9.
4 Kassmann-Kellner B , Weindler J, Pfau B, et al.
Ocular changes in mucopolysaccharidosis IVA
(Morquio A syndrome) and long-term results of perforating keratoplasty.
Ophthalmologica
1999; 213 :200–5.
5 Dangel ME , Tsou BH. Retinal involvement in
Morquio’s syndrome (MPS IV).
Ann Ophthalmol
1985; 17 :349–54.
6 Ghosh M , McCulloch C. The Morquio syndrome light and electron microscopic findings from two corneas.
Canad J Ophthal 1974; 9 :445–52.
7 Iwamoto M , Nawa Y, Maumenee IH, et al.
Ocular histopathology and ultrastructure of
Morquio syndrome (systemic mucopolysaccharidosis IVA).
Graefes Arch Clin
Exp Ophthalmol 1990; 228 :342–9.
8 Rawe IM , Leonard DW, Meek KM, et al.
X-ray diffraction and transmission electron microscopy of Morquio syndrome type A cornea: a structural analysis.
Cornea 1997; 16 :369–76.
Importance of early morning intraocular pressure recording for measurement of diurnal variation of intraocular pressure
Intraocular pressure (IOP) is subject to cyclic fluctuations through the day. Diurnal variation in glaucoma was first reported in 1898.
1
Duke-Elder and others reported high IOP on awakening.
2–6 There is therefore a chance of missing a pressure elevation with single readings.
Phasing is mainly carried out from 0900 to
1800 hours, thereby missing any early morning spikes of IOP. Any delay in the first measurement will miss variations in IOP that are present immediately on wakening.
4 7 We carried out a retrospective study, where patients under the care of the senior author
(CL) are routinely admitted for phasing in order to obtain an early morning recording of
IOP immediately on awakening.
Report
A total of 93 patients (mean age 73.2 years) were admitted for phasing under the care of the senior author between December 1997 and August 2002. The first measurement of
IOP took place between 0800–1000 hours.
Further measurements were taken every
2 hours until 2000 hours. The final measurement was taken early morning (between
0600–0800 hours) immediately on awakening. Goldmann applanation tonometry was carried out by experienced staff.
In all, 17 patients requiring treatment or change in management for their glaucoma were identified. Of these, 13 were identified as having POAG. Four patients out of 13
(30.8%) showed peak IOP (23–28 mm Hg, www.bjophthalmol.com
PostScript 927
15
12
9
6
27
24
21
18
3
0
16.24 16.47
17.96
15.24
16.12
17.21
15.12
0600–0800
Time intervals
Figure 1 Mean IOP during phasing in our unit at different intervals.
mean 24.5) in the early morning (0600–
0800 hours) immediately on awakening
(fig 2). These cases would have been missed if routine outpatient measurements of diurnal variation only had been carried out.
Comment
The evaluation of IOP is usually based on measurements performed during office hours.
As IOP is considered a major risk factor for glaucoma, an undetected IOP spike could be the missing link that has not been taken into account.
8 Various investigators have shown that IOP just after awakening is increased.
4 7
Phasing during routine office hours only would miss this. In our series we detected four patients with high IOPs in the early morning.
Goldmann tonometry was done in the sitting position, which might have reduced our chance to detect more cases, as IOP could be higher in the supine position.
9 We did our best to take measurements immediately on awakening although there was a time delay in some patients because of reduced mobility.
These limitations could have been avoided to some extent by using a portable tonometer such as the Perkins tonometer.
The disadvantages of our study were its retrospective nature, small population of study, and different members of staff involved in IOP measurements, thereby introducing variability. Staff members were not blind to the results but they do not have any vested interest in whether the early morning result is important. IOP could be overestimated in patients with thicker corneas, which we have not controlled for. We believe this factor, and its own diurnal variation, should be taken into consideration in future studies.
15
12
9
6
27
24
21
18
3
0
24.5
17
18 18.12 19 17.12
16
–1000 –1200
1000
Time intervals
–1800 –2000
1800
Figure 2 Mean IOP variation in the four patients detected with early morning IOP spikes.
Based on our study we believe that more cases of glaucoma could be identified by early morning measurement of IOP during phasing.
Acknowledgements
The authors gratefully acknowledge the assistance of Clare Jenkins, clinical audit coordinator, Queen
Victoria Hospital, East Grinstead, and Matthew
Hankins, senior lecturer, Post Graduate Medical
School, University of Brighton, Brighton, UK.
No proprietary interest or research funding.
P P Syam, I Mavrikakis, C Liu
Sussex Eye Hospital, Eastern Road, Brighton BN2 5BF,
UK
Correspondence to: Mr C S C Liu, Sussex Eye
Hospital, Eastern Road, Brighton BN2 5BF, UK;
CSCLiu@aol.com
Ethics committee approval: As this was a retrospective study, ethics committee approval was not required.
doi: 10.1136/bjo.2004.052787
Accepted for publication 11 November 2004
References
1 Sidler-Huguenin . Die Spa¨terfolge der
Glaukombehandlung bei 76 Privatpatienten von
Prof Haab, Zurich.
Beitr Augenheilkd
1898; 32 :96.
2 Duke-Elder S .
System of ophthalmology , Vol IV—
The physiology of eye and vision. Ch IV . London:
Henry Kimpton, 1968:276–80.
3 Frampton P , Da Rin D, Brown B. Diurnal variation of intraocular pressure and the overriding effects of sleep.
Am J Optom Physiol Opt
1987; 64 :54–61.
4 Brown B , Burton P, Mann S, et al.
Fluctuation in intraocular pressure with sleep: II. Time course of
IOP decrease after waking from sleep.
Ophthal
Physiol Opt 1988; 8 :249–52.
5 Drance SM . Diurnal variation of intraocular pressure in treated glaucoma.
Arch Ophthalmol
1963; 70 :302–11.
6 Sacca SC , Rolando M, Marletta A, et al.
Fluctuations of intraocular pressure during the day in open angle glaucoma, normal tension glaucoma and normal subjects.
Ophthalmologica
1998; 212 :115–9.
7 Zeimer RC , Wilensky JT, Gieser DK. Presence and rapid decline of early morning intraocular pressure peaks in glaucoma.
Ophthalmology
1990; 97 :547–50.
8 Brubaker RF . Delayed functional loss in glaucoma. LII Edward Jackson memorial lecture.
Am J Ophthalmol 1996; 121 :473–83.
9 Liu JH , Kripke DF, Twa MD, et al.
Twenty-fourhour pattern of intraocular pressure in the aging population.
Invest Ophthalmol Vis Sci
1999; 40 :2912–7.
Autoimmune retinopathy associated with intravesical BCG therapy
Intravesical BCG is used as adjunctive immunotherapy for superficial carcinomas of the urinary bladder. Endophthalmitis and uveitis are the reported ocular complications.
1–3 We report an unusual case of autoimmune retinopathy in a 58 year old man treated with intravesical BCG. The clinical features resembled CAR (cancer associated retinopathy) but there was no serum reaction to the CAR autoantigen.
1 We believe that this is the first reported case of autoimmune retinopathy caused by BCG treatment.
Case report
A 58 year old white man was referred with reduced vision and photophobia for 4 months following a 6 week (one instillation per week) course of intravesical BCG immunotherapy for recurrent transitional cell bladder carcinoma.
On examination, after 4 months of complaints, the visual acuity was 6/24 in each eye and N18 for near. Anterior segment evaluation revealed bilateral early nuclear cataracts. The anterior chamber and vitreous were quiet. The fundus examination showed mildly attenuated arterioles (RE .
LE) with a mild pigmentary disturbance in the mid-periphery. Intraocular pressure was normal. Colour vision showed a protan-deutan axis in both eyes. There was no family history of colour blindness. Full field electroretinogram (ERG) amplitudes were subnormal for photopic and scotopic conditions in both eyes. Latency was normal. An electrooculogram (EOG) was borderline normal in both eyes. Automated perimetry revealed bilaterally enlarged blind spots. Fundus fluorescein angiography showed narrowed arterioles. The choroid was normal. Serum analysis revealed no reaction to 23 kD CAR autoantigen.
1
However, an unusual reaction which may represent a form of autoimmune degeneration was reported by the laboratory.
The photophobia increased over the next
2 months. A repeat full field ERG revealed that photopic responses were indistinguishable from noise in the right eye and just detectable in the left eye. On examination, visual acuity in each eye was 6/24. Oral prednisolone 20 mg daily was commenced.
After a year it was decided to stop it as there was no improvement in vision. On his last follow up visit, the visual acuity was counting fingers in each eye and N36 at 10 cm. This had remained stable for 3 years. The photophobia was stable owing to dense cataracts and was well controlled with dark glasses.
The fundus remained unchanged. The primary bladder carcinoma was unchanged and no secondaries were found.
Comment
BCG has been used for the treatment of bladder cancers for many years. Ocular toxicity caused by BCG resulting in granulomatous uveitis with vitiligo has been reported.
1 The first case of endogenous endophthalmitis after use of BCG for metastatic bladder carcinoma was reported in
1988. The patient developed bilateral infiltrative retinitis and vitritis.
Vitrectomy revealed Mycobacterium bovis .
2
CAR is associated with melanomas, cancers of lung, cervix, colon, bladder, prostate, and breast. Progressive visual loss, night blindness with ring scotoma, and markedly abnormal
ERG findings were described. Fundus revealed mild retinal pigmentation.
2 Histopathology of
CAR affected eyes revealed loss of retinal receptors and atrophic changes in the retinal pigment epithelium (RPE), most marked in the macula. An abnormal state of RPE hypersensitivity contributing to retinal degeneration has been reported. Grunwald et al ,
Kornguth et al and Keltner et al found antibodies to normal retina in serum of cancer patients with associated retinopathies.
1 3 One key autoantigen was identified as a 23 kD photoreceptor component ‘‘recoverin,’’ later found to be expressed by small cell carcinomas.
Other CAR antigens have also since been identified.
3 4 Corticosteroids, gamma globulin, and plasmapheresis do help in some cases.
1
Induction of autoimmune reactions within the eye by extraocular diseases brings into question the possibility of a sensitisation involving the M bovis component of the BCG vaccine. The live attenuated mycobacterium of intravesical BCG infects normal and cancerous www.bjophthalmol.com
928 PostScript bladder epithelial cells. The infection then initiates a cascade of immune events including a rapid influx of CD4 + T cells, cytokine release
(IL2, IFN-gamma and alpha) with an increase of gamma/delta T cells. These cells are not
MHC type II restricted.
5 We propose this is how activation of cellular immunity may lead to autoimmune phenomena in the eye.
Our case demonstrated the clinical features of an autoimmune retinopathy but the reaction to CAR antigen was absent. However, the unusual reaction reported suggests the presence of an immune mechanism which has the potential to cause a progressive type of retinopathy, the prognosis of which is unknown and which does not respond to steroids.
We may not have presented enough evidence to link the use of intravesical BCG with the ocular changes, although the temporal relation to the BCG therapy suggests that BCG is the most likely trigger of the autoimmunity.
We suggest the bladder neoplasm is also a possibility. Ophthalmologists need to be aware of this rare possibility in order to improve their diagnostic yield in investigations of patients with similar clinical profiles. Patients also need to be warned of this rare but serious complication. This ocular complication in a previously normal patient necessitates regular ophthalmic screening in potential patients.
S Sharan
Save Sight Institute, University of Sydney, Department of Ophthalmology, Sydney Eye Hospital, 8 Macquarie
Street, Sydney 2000, Australia
C E Thirkill
Department of Ophthalmology, UC Davis Health
System, University of California, Sacramento, CA
95817, USA
J R Grigg
Save Sight Institute, University of Sydney, Department of Ophthalmology, Sydney Eye Hospital, 8,
Macquarie Street, Sydney 2000, Australia
Correspondence to: Sapna Sharan, Save Sight
Institute, University of Sydney, Department of
Ophthalmology, Sydney Eye Hospital, 8 Macquarie
Street, Sydney 2000, Australia; sapnasd@ yahoo.co.uk
doi: 10.1136/bjo.2004.065359
Accepted for publication 1 January 2005
References
1 Ryan SJ . In: Retina , 2nd ed. St Louis: Mosby,
1994:894–6.
2 Lester H , Erdey RA, Fastenberg DM, et al.
Bacillus
Calmette-Guerin (BCG) endophthalmitis.
Retina
1988; 8 :182–4.
3 Thirkill CE , Tait RC, Tyler NK, et al.
The cancer associated retinopathy antigen is a recoverin-like protein.
Invest Ophthalmol Vis Sci
1992; 33 :2768–72.
4 Thirkill CE . RPE hypersensitivity complicating paraneoplastic retinopathies.
Ocul Immunol
Inflamm 2000; 8 :25–37.
5 Bohle A , Brandau S. Immune mechanisms in bacillus Calmette-Guerin immunotherapy for superficial bladder cancer.
Urol
2003; 170 :964–9.
MAILBOX
Preoperative videotape sessions and patient satisfaction with cataract surgery
We read with interest the article by Pager.
1
The study showed that a preoperative videotape session describing the experience of day stay cataract surgery resulted in a significant increase in overall satisfaction during the immediate postoperative period.
Patient satisfaction has drawn increasing attentions in all field of medicine for medical, financial, and litigation reasons. Age, types of aphakic correction, information received by patients, ocular co-morbidity, and postoperative visual acuity have been identified as important factors affecting the overall satisfaction in patients undergoing cataract surgery.
2 While this study addressed the psychosomatic response in the perioperative period, it would be interesting to know how the videotape session can affect the perception of surgical outcome. It would be even more worthwhile to assess how such a videotape session can modify the patient response to unfavourable outcomes when surgical complications occur. Further information on patient satisfaction in either group during the follow up period would be relevant.
It was shown that the majority of patients could not recall relevant information after verbal consent.
3 Remembering the information deteriorated significantly after the operation, even more so in those of an advanced age and with less than high school education.
3 Videotape has been used in the informed consent process in other medical fields. Patients having gastrointestinal endoscopy were found to be more satisfied with videotape followed by physician discussion than either method alone.
4 It has also been demonstrated to lead to higher knowledge scores, especially in patients with lower education levels.
5 Since cataract patients are usually old and come with very high expectations, we think that further research is required to explore the use of videotape in order to achieve a better informed consent.
K S C Yuen, A C K Cheng, W-M Chan
The Chinese University of Hong Kong, Department of
Ophthalmology and Visual Sciences, Prince of Wales
Hospital, Shatin, Hong Kong, China
Correspondence to: Dr Kenneth S C Yuen, The
Chinese University of Hong Kong, Department of
Ophthalmology and Visual Sciences, Prince of Wales
Hospital, Shatin, Hong Kong, China; ksyuen@gmail.com
doi: 10.1136/bjo.2005.072835
Accepted for publication 8 April 2005
References
1 Pager CK . Randomised controlled trial of preoperative information to improve satisfaction with cataract surgery.
Br J Ophthalmol
2005; 89 :10–13.
2 Legro MW . Quality of life and cataracts: a review of patient-centered studies of cataract surgery outcomes.
Ophthalmic Surg 1991; 22 :431–43.
3 Morgan LW , Schwab IR. Informed consent in senile cataract extraction.
Arch Ophthalmol
1986; 104 :42–5.
4 Agre P , McKee K, Gargon N, et al.
Patient satisfaction with an informed consent process.
Cancer Pract 1997; 5 :162–7.
5 Rossi M , McClellan R, Chou L, et al.
Informed consent for ankle fracture surgery: patient comprehension of verbal and videotaped information.
Foot Ankle Int 2004; 25 :756–62.
Optical coherence tomography in photodynamic therapy
Sahni et al presented a new terminology to validate the reliability of optical coherence tomography (OCT) and studied the effect of photodynamic therapy (PDT) in patients with subfoveal, predominantly classic choroidal neovascularisation (CNV) secondary to age related macular degeneration (AMD).
1 The new terminology introduced neuroretinal foveal thickness (NFT), bilaminar foveal thickness (BFT), outer high reflectivity band thickness (OHRBT), intraretinal fluid (IRF), subretinal fluid (SRF), and vitreomacular hyaloid attachment. A heterogeneous group of patients were included. Whereas in three patients OCT scanning was performed before
PDT, 53 had already undergone up to seven treatment sessions. The results showed a significant correlation of mean neuroretinal foveal thickness and intraretinal fluid.
Additionally, there was a high correlation between bilaminar foveal thickness and visual acuity (VA). The authors also reported a poor agreement between OCT and clinical examination in the detection of cystoid macular oedema (CMO) and subretinal fluid, indicating the usefulness of OCT.
We congratulate the authors and want to add two aspects from our clinical experience.
In a previous study we reported the presence of CMO and increased foveal thickness to correlate with a poorer visual outcome in non-treated neovascular AMD.
2 Sahni et al demonstrated no correlation between VA and
IRF and SRF in patients undergoing PDT, giving evidence that a beneficial effect of
PDT, especially for the group with exudative
AMD associated with CMO, arises. OCT seems to be valuable in predicting functional outcome following PDT.
The current study presented no data on the actual time when the OCT evaluation has been performed, although several authors described remarkable OCT findings following
PDT. In a prospective study we evaluated 24 patients (53 PDT sessions) before PDT as well as 2 days and 1 week after PDT by VA and
OCT.
3 Here, a transient hyperopic shift corresponded with a consecutive increased retinal thickness up to 680 m m on OCT. The cross sectional OCT scan in the macular area revealed a retinal detachment, whereas the anatomy of the neurosensory retina maintained intact, no relevant thickening or schisis-like changes were observed. Previous examinations by Costa et al , determined a few hours after PDT, indicated an increased subretinal leakage on indocyanine green angiography (ICG) and consecutive retinal elevation on OCT, confirming our functional and OCT findings.
4 Long term OCT findings presented by Rogers et al demonstrated structural alterations in terms of persistent retinal thinning 3 months after PDT.
5 Therefore, OCT findings before the first PDT are necessary to determine predictable signs for functional outcome. OCT is a useful technique describing morphologal findings of the retina and choroid. Nevertheless, a higher number of patients before the first PDT application have to be evaluated by OCT to define predictable signs elucidating visual outcome.
S Mennel, F Liu, C H Meyer
Department of Ophthalmology, Philipps-University,
Robert-Koch- Strasse 4, Marburg, Germany
Correspondence to: Dr Stefan Mennel, Department of
Ophthalmology, Philipps-University, Robert-Koch-
Strasse 4, Marburg, Germany; stefan.mennel@lycos.com
doi: 10.1136/bjo.2005.071092
Accepted for publication 14 March 2005 www.bjophthalmol.com
Downloaded from bjo.bmjjournals.com
on 11 October 2005
‘‘Monin chooses his target, the governor, and Malraux his, the editor of L’Impartial ,
Monin offers Cognacq a job at the
L’Indochine in the propaganda department…. I shall buy you a nice cap: on it, like on a little boy’s Sunday best sailor’s beret…. The three words that sum up your administration: Disorder, Inequality,
Anarchy. Malraux portrays Lachevrotiere as a specialist in ‘‘pistol duels with the shortsighted, and sword duels with the one armed.’’ He builds up a hefty dossier on Lachevrotiere’s military non career.
Monin willingly countersigns as a voluntary consort for the duration of the war.
(Todd, Olivier.
Malraux. A Life . New York:
Alfred A Knopf, 2005:49) also improved insulin resistance as measured by glucose tolerance testing. This was not the case with white chocolate.
( Am J Clin Nutr 2005; 81 :611–14)
The controversy surrounding vitamin E continues. In the laboratory this potent anti-oxidant appears to have a protective effect against cancer and cardiovascular disease but clinical trials have failed to show any benefit from its use. Now in a study of 5000 patients with diabetes or cardiovascular disease, nearly 4000 of whom agreed to take vitamin E or placebo, no protective effect on heart disease or cancer was demonstrated in the group that took prophylactic vitamin E. The only positive finding was an increased risk of heart failure among patients who took vitamin E. ( JAMA 2005; 293 :1338–47)
The stress of marathon running is well known.
Dehydration and electrolyte imbalance are two of the recognised complications of this sport. In a study of collapsed marathon runners, however, investigators noted that hypernatraemia with hyperosmolality was equally common as hypernatraemia with hypo-osmolaity.
In some circumstances, therefore, the administration of fluids to collapsed marathon runners may exacerbate hypernatraemia and result in fatal cerebral oedema.
( Arch Pathol Lab Med 2005; 129 :227-30)
Recently C reactive protein (CRP) has emerged as a possible potent risk marker for cardiovascular disease. The B type natriuretic peptides have also received interest as potential risk markers. In a population based prospective study of 764 adults older than 50 years of age in
Copenhagen, investigators studied the risk of mortality and first major cardiovascular event in relation to baseline levels of CRP, urinary albumin, and N-terminal probrain natriuretic peptide. In this study measurement of N-terminal pro-brain natriuretic peptide provided prognostic information about mortality and risk factor for first major cardiovascular event.
It was a stronger risk biomarker for cardiovascular disease and death than
CRP. ( JAMA 2005; 293 :1609–16)
The lack of refrigeration remains a problem in providing vaccinations for the world’s poor since these drugs often lose their efficacy in the heat. Two hundred years ago a solution for this was to vaccinate orphaned children to propagate the vaccine. The ethical dilemmas involved in such a programme are obvious.
However, investigators at Arizona State
University now suggest that genetically engineered potatoes may be used to produce a vaccine against hepatitis B virus.
This so called edible vaccine proved to be effective in 60% of volunteers who ate raw chunks of the potato. Shifting the strategy from edible vaccines from food to process pills may be the next step in this development. ( Scientific American 2005; 292 :25)
Considerable concern has been raised about reporting bias as the result of selective reporting of results from clinical trials. In a study of all journal articles of randomised trials indexed in PubMed, investigators from Toronto concluded that incomplete reporting of outcomes within published articles of randomised trials is common.
Medical of study outcomes and trial protocols should be made publicly available. ( BMJ
2005; 330 :753–6) literature therefore represents a selective and biased subset
There is more good evidence for chocolate lovers. Dark but not white chocolate seems to have a blood pressure lowering effect. In a study of 15 healthy volunteers dark chocolate was shown to produce a significant drop in systolic blood pressure and
There is considerable interest in biofilm production in relation to bacterial infections and the development of therapeutic strategies to interfere with it. The importance of this is further emphasised by a study of patients with prosthetic heart valves. In this study Staphylococcus epidermidis , usually a benign bacterium became pathogenic on the heart valve.
This appears to be because the bacterium secretes an extracellular polymer polygamma-
DL
-glutamic acid. This in turn forms a biofilm that protects it from the host’s normal innate defences. Targeting this extracellular polymer may be a way to develop new antibacterial therapies. ( J Clin
Invest 2005; 115 :688–94)
It now appears clear that genetic factors are important in the development of age related macular degeneration (AMD). It is less clear what environmental factors may also have an important role. Results from the Age Related Eye Disease Study
Research Group suggest that patients with early intermediate AMD who smoke or have an increase in body mass index are more likely to progress to advanced AMD.
The question of whether the use of antacids and anti-inflammatory medications affected progression of AMD could not be ascertained from this study but the authors suggest further study is warranted. ( Ophthalmology 2005; 112 :533–9)
Malaria continues to be a worldwide health concern. In certain areas of the world it remains endemic. In a study from
Kenya of children who had been infected with falciparum malaria some children developed neurocognitive impairments that were evident as long as 9 years after initial infection. The long term consequences of malaria in children can be profound. Learning disabilities may persist for many years.
( J Neurol Neurosurg
Psychiatry 2005; 76 :476–81)
Among older men there is some interest in testosterone supplements for the effects of so called male menopause. In a randomised controlled trial older men who received supplemental testosterone did not appear to fare better than those who did not when evaluated by a symptom score on androgen deficiency in the ageing male. However, the group that received the supplement appeared to be less sad and grumpy. ( Age and Aging 2005; 34 :125–30) www.bjophthalmol.com
Downloaded from bjo.bmjjournals.com
on 11 October 2005
‘‘Monin chooses his target, the governor, and Malraux his, the editor of L’Impartial ,
Monin offers Cognacq a job at the
L’Indochine in the propaganda department…. I shall buy you a nice cap: on it, like on a little boy’s Sunday best sailor’s beret…. The three words that sum up your administration: Disorder, Inequality,
Anarchy. Malraux portrays Lachevrotiere as a specialist in ‘‘pistol duels with the shortsighted, and sword duels with the one armed.’’ He builds up a hefty dossier on Lachevrotiere’s military non career.
Monin willingly countersigns as a voluntary consort for the duration of the war.
(Todd, Olivier.
Malraux. A Life . New York:
Alfred A Knopf, 2005:49) also improved insulin resistance as measured by glucose tolerance testing. This was not the case with white chocolate.
( Am J Clin Nutr 2005; 81 :611–14)
The controversy surrounding vitamin E continues. In the laboratory this potent anti-oxidant appears to have a protective effect against cancer and cardiovascular disease but clinical trials have failed to show any benefit from its use. Now in a study of 5000 patients with diabetes or cardiovascular disease, nearly 4000 of whom agreed to take vitamin E or placebo, no protective effect on heart disease or cancer was demonstrated in the group that took prophylactic vitamin E. The only positive finding was an increased risk of heart failure among patients who took vitamin E. ( JAMA 2005; 293 :1338–47)
The stress of marathon running is well known.
Dehydration and electrolyte imbalance are two of the recognised complications of this sport. In a study of collapsed marathon runners, however, investigators noted that hypernatraemia with hyperosmolality was equally common as hypernatraemia with hypo-osmolaity.
In some circumstances, therefore, the administration of fluids to collapsed marathon runners may exacerbate hypernatraemia and result in fatal cerebral oedema.
( Arch Pathol Lab Med 2005; 129 :227-30)
Recently C reactive protein (CRP) has emerged as a possible potent risk marker for cardiovascular disease. The B type natriuretic peptides have also received interest as potential risk markers. In a population based prospective study of 764 adults older than 50 years of age in
Copenhagen, investigators studied the risk of mortality and first major cardiovascular event in relation to baseline levels of CRP, urinary albumin, and N-terminal probrain natriuretic peptide. In this study measurement of N-terminal pro-brain natriuretic peptide provided prognostic information about mortality and risk factor for first major cardiovascular event.
It was a stronger risk biomarker for cardiovascular disease and death than
CRP. ( JAMA 2005; 293 :1609–16)
The lack of refrigeration remains a problem in providing vaccinations for the world’s poor since these drugs often lose their efficacy in the heat. Two hundred years ago a solution for this was to vaccinate orphaned children to propagate the vaccine. The ethical dilemmas involved in such a programme are obvious.
However, investigators at Arizona State
University now suggest that genetically engineered potatoes may be used to produce a vaccine against hepatitis B virus.
This so called edible vaccine proved to be effective in 60% of volunteers who ate raw chunks of the potato. Shifting the strategy from edible vaccines from food to process pills may be the next step in this development. ( Scientific American 2005; 292 :25)
Considerable concern has been raised about reporting bias as the result of selective reporting of results from clinical trials. In a study of all journal articles of randomised trials indexed in PubMed, investigators from Toronto concluded that incomplete reporting of outcomes within published articles of randomised trials is common.
Medical of study outcomes and trial protocols should be made publicly available. ( BMJ
2005; 330 :753–6) literature therefore represents a selective and biased subset
There is more good evidence for chocolate lovers. Dark but not white chocolate seems to have a blood pressure lowering effect. In a study of 15 healthy volunteers dark chocolate was shown to produce a significant drop in systolic blood pressure and
There is considerable interest in biofilm production in relation to bacterial infections and the development of therapeutic strategies to interfere with it. The importance of this is further emphasised by a study of patients with prosthetic heart valves. In this study Staphylococcus epidermidis , usually a benign bacterium became pathogenic on the heart valve.
This appears to be because the bacterium secretes an extracellular polymer polygamma-
DL
-glutamic acid. This in turn forms a biofilm that protects it from the host’s normal innate defences. Targeting this extracellular polymer may be a way to develop new antibacterial therapies. ( J Clin
Invest 2005; 115 :688–94)
It now appears clear that genetic factors are important in the development of age related macular degeneration (AMD). It is less clear what environmental factors may also have an important role. Results from the Age Related Eye Disease Study
Research Group suggest that patients with early intermediate AMD who smoke or have an increase in body mass index are more likely to progress to advanced AMD.
The question of whether the use of antacids and anti-inflammatory medications affected progression of AMD could not be ascertained from this study but the authors suggest further study is warranted. ( Ophthalmology 2005; 112 :533–9)
Malaria continues to be a worldwide health concern. In certain areas of the world it remains endemic. In a study from
Kenya of children who had been infected with falciparum malaria some children developed neurocognitive impairments that were evident as long as 9 years after initial infection. The long term consequences of malaria in children can be profound. Learning disabilities may persist for many years.
( J Neurol Neurosurg
Psychiatry 2005; 76 :476–81)
Among older men there is some interest in testosterone supplements for the effects of so called male menopause. In a randomised controlled trial older men who received supplemental testosterone did not appear to fare better than those who did not when evaluated by a symptom score on androgen deficiency in the ageing male. However, the group that received the supplement appeared to be less sad and grumpy. ( Age and Aging 2005; 34 :125–30) www.bjophthalmol.com