Emergency Department Volunteer Handbook
advertisement

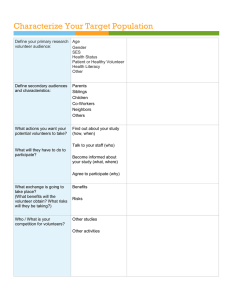
Emergency Department Volunteer Handbook Niagara Health System Thanks for being an Emergency Department Volunteer Thank you for your commitment to a great experience for our patients and their loved ones in the ED. There has been much change this past year throughout the transition to our beautiful new hospital. We know change can be hard and appreciate your support, flexibility and patience. Volunteers contributed a great deal to ensuring a smooth transition. Now that everyone has settled in our new environment, we have identified some key ways Volunteers can have an even greater impact on addressing the needs of those we serve. We have engaged Emergency Department Management, Staff and Volunteers to standardize our care delivery. Some of these initiatives include: Development of this Emergency Department Volunteer Handbook to empower current Volunteers with information that will help you deliver the best care to For All Emergency patients Volunteers New ED Volunteer Communication Binder and New Sign-In Process A bi-annual intake process for new volunteers joining the team – held in September and May each year For New An improved process for departmental orientation and Volunteers training including development of the New Volunteers’ Training Checklist and the Trainer’s Guide Please take a few minutes to review this Handbook. We know that most of this information will be familiar to you and ask for your cooperation in ensuring success of these new strategies. Thank you! 2 Table of Contents ED Volunteer Communication Binder and Sign-In………Page 4 Volunteer Position Description………………………………… Page 5 Role of Volunteers…………………………………………………….Page 7 Patient Centered Care……………………………………………….Page 9 Emergency Department Floor Plan……………………………Page 11 Emergency Department and Urgent Care Center……….Page 12 Emergency Department Overview ……………………………Page 13 Communication……………………………….……………………….Page 23 Factors Affecting Wait Times ……………………………………Page 27 Infection Prevention and Control………………………………Page 30 New Volunteer Orientation and Training Process…… Page 32 Leadership Opportunities and Questions…………………..Page 34 Our Goal: A full roster of Volunteers A full roster of who are… who are… volunteers Patient Centered Visible Skilled Confident 3 NEW PROCESS FOR SIGNING IN & OUT IMPORTANT NOTE: Emergency Volunteers will now sign-in and out at the start and end of their shift in the ED Volunteer Communication Binder. Please DO NOT sign-in or out at the Information Desk after November 22, 2013 LOCATION: ED Volunteer Communications Binder is kept on the shelf behind the Charge Nurses’ Chair at Care Station A1. (It is White with a Label on the Spine) The ED Volunteer Communication Binder contains helpful resources to assist you in your role as well as up-to-date Memo’s and Information about the Hospital and the NHS. Please be sure to spend the first five minutes of every shift reading to catch up on the news. Having up to date information will help you help patients. You are encouraged to share your ideas about additional resources and/or information that would be helpful. 4 5 6 Role of ED Volunteers Communicator Care Provider Volunteer Educator Clinical Support Communicator Directly with Patients: to comfort them, answer questions, provide information and represent the Hospital With Staff: to share information about patients, to seek guidance and direction when unsure With Volunteer Resources: to be informed and stay up to date about Hospital information, policies and procedures in an ever-changing environment. 7 Educator Share what you know from orientation, training, your experience in ED and the Hospital, your interactions with staff and from reviewing new information in the Volunteer Communication Binder at the start of each shift. Explain processes, share why things work the way they do, reasons behind wait times and other information to help patients and loved ones feel informed Care Provider Comfort Measures for Patients and their Loved Ones Warm blankets, conversation, dim the lights, adjust the bed, relay information to the Charge Nurse, assist their loved ones, get information when needed, advocate 1:1 support for patients with special needs such as anxiety, confusion, small children Clinical Support Fulfill roles requested by staff (get approval from Charge Nurse when asked to do things outside of position description scope) Retrieve items, errands to other departments etc. Escort mobile patients to general locations (Ex. Discharge support) Stock blanket warmer Disinfect wheelchairs Tidy the waiting room 8 Patient Centered Care o NRC Picker – Patient Satisfaction Surveys o A Harvard study, in partnership with NRC Picker, identified 8 behaviours that ensure a quality patient care experience o These behaviours help patients heal sooner with a decreased likelihood of re-admission POWERFUL VIDEO ON EMPATHY Could a greater miracle take place than for us to look through each other’s eyes for an instant?” ~ Henry David Thoreau http://www.youtube.com/watch?v=zh55e6U_XPM 9 Delivering Patient Centered Care o Person-centered philosophy o Consciously adopting the patients’ perspective about what matters. o Care for the patient expands to loved ones o Ask questions. Listen! Find out their story Seek to understand o Patient Involvement o “Nothing about me without me” o Patient needs vary o Whole person approach to care o Meet them where they are at o Don’t make value judgments o Focus on a Customer Service Approach o Polite, Kind, Helpful, Consistent, Needs Met, Relevant, Timely o A good patient experience is achieved by making every little interaction positive 10 The Emergency Department Floor Plan 11 Combined Emergency Department Introduction to the Department and Urgent Care Center Combined Emergency and Urgent Care Center Emergency Department • • • • • • • • Severe bleeding Difficulty breathing Chest pain or pressure Broken bones Mental health emergencies Trauma or injury to the head Sudden dizziness/difficulty seeing Severe abdominal pain Source: St.Joseph’s Healthcare Hamilton Urgent Care Center • Minor abdominal pain (nausea, vomiting, flu) • Coughs, colds, fever • Ear, nose, throat and eye problems • Cuts that may need stitches • Sprains, strains, sports injuries • Minor asthma attacks or allergic reactions Source: Niagara Health System Support for Volunteers Charge Nurse – Located at Care Station A1 - Primary contact for Volunteers on duty Triage Nurse – Located under “Start Here” and/or Triage Room 1, 2 and 3 Manager – Lisa Hildebrand TLC Volunteers – For assistance with Hospital Information Volunteer Resources 12 Overview: Emergency Department 1. Information Desk in Lobby • Please sign-in and out and read important communciation updates in the Emergency Department Volunteer Communication Binder located behind the Charge Nurse at care station A1 • ED Volunteers will no longer sign-in at the Informaiton Desk in the Lobby. 2. Volunteer Resources • Volunteer Vests are stored in the Cloak Room • Volunteers can validate Parking Passes • Volunteer cupboard located in the Activity Room near the computer 3. Waiting Room • Familiarize with the Quick Assessment - Triage Registration process. Patients enter and see Triage Nurse under START HERE • See: Factors affecting patient flow and wait times page 17. • Parking machines, wheelchair storage, washrooms and security office • Communicating with patients in the waiting room. See page 16. 13 4. Main ED Doors and Hallway • ED floor plan • Accessible washroom (on the corner) 5. Hallway to Ambulance Offload Area • Role of Registration staff - complete registration paperwork, take patient's personal information • Overview of triage/quick assessment/ambulance offload nurse role • CCAC, EMS, Police offices 6. Ambulance Offload Area • Patients come in through garage, get triaged, and moved to a room from this area • High traffic; Fire code restricts this area to paramedics, hospital personnel, and patients. Visitors should be directed to waiting room until patient is assigned a room • Water machine, washrooms and decontamination room • Ambulance garage 14 Unit A: 7. Care Station A1 • Care station, charge nurse's computer, know which nurse cares for which patients • Patients that are cared for in A (Unit A= more Acute, less stable) • Code red procedures; A1 is the meeting place for instructions (to call an emergency code- dial x 55555) • ** ED Volunteer Sign-In and Communication Binder stored on shelf behind Charge Nurses' chair 8. Resuscitation Room Hallway • A1 nurses care for these patients • Patient washroom, soiled utility, clean supply room 9. Soiled Utility Room • For disposal of items used by patients • Used food tray cart stored here 15 Unit A: 10. Blanket Warmer Corridor • Volunteers are encouraged to offer warm blankets to patients as a comfort measure with the exception of patients who have a fever • Familiarize yourself with the items on the linen carts. • Pneumatic Tube System--The Bullet 11. Clean Supply Room • Overview of commonly retrieved/seen items (from this room) • Especially; urine bottle, toilet hats, bed pans 12. Care Station A2 • Orientate volunteer to the rooms these nurses attend to 16 Unit B: Unit B: 13. Nutrition Centre 16. Blanket Warmer Give volunteer visual reference of Centre location(new the • Be •familiar with items in the Nutrition warmer is located kettle and microwave) Overview of items on linen carts • Not•patient dietary restriction procedures (Ex. Renal Diet) and always check with nurse before giving patients anything to eat or drink • Always assist loved ones/family in the Nutrition Center 17. Soiled Utility Room • Orientate volunteer to what this room is used for 15. •Clean Utility Room Important notes: Used food tray cart stored here • Be familiar with items commonly accessed in this room • Especially; urine bottles, bed pans, toothbrushes, blue 18. "Big" Storage Room shoe covers/slippers • Good place to orient volunteers toisolation cart and infection control procedures (See Page 20) • Show volunteer what equipments can be found in here 14. Nurse's Station/ Overview of Unit B • Ex. Commodes, and isolation carts •Patients are in this unit are more stable or are waiting for a bed in in-patient unit 19. Isolation/ Negative Pressure Room •See Care Station B •ENT Room (Ear, Nose, and Throat) •The three patient washrooms • Explain this room briefly • Discuss function of the pressure monitor on the wall 17 Unit C: 20. Unit Overview • Ambulance off-load patients who are waiting for an acute care bed • Offer assistance to staff - running errands, getting refreshments for patients, etc. 21. Pod D- Domestic Violence and Sexual Assault • While Volunteers do not support patients in this unit it is important to be aware of the services delivered and be able to provide directions 21. Manager's Office • Take a minute to introduce yourself to Manager, Lisa Hildebrand • Volunteer's are encouraged to approach Lisa if theres ever an issue they need assistance with 18 22. Unit E- Psychiatric Emergency • Patients being cared for Mental Health Illness are seen in this area • Not fully staffed; Currently operating with an on-call crisis nurse 23. Family Consultation Room • Space available for families to spend time away from the patient • Show volunteer how to get here from the main hallway and Pod A 24. ED Team Room • Volunteers are welcome! (Just remember we also have a generously sized team room) 25. ED Locker Room • Unlabelled lockers are available - remove locks at shift end • Volunteers can also use lockers in Volunteer Resources clock room where they pick up and return vests 19 26. Cast Room • Familiarize yourself with this room and be comfortable assisting patients with comfort measures 27. Urgent Care Center • Orient yourself to the UCC floor plan and care station • Volunteers are encouraged to assist patients and loved ones in UCC with communication and comfort measures 4. Call Bell and Code Lights • Singe solid white line= Bell is ringing • Solid red= Needs nurse's assistance • Solid yellow= Activity of daily living • Slow green flash= Volunteer/Basic assistace • Quickly flashing colour= Coordinates with the emergency code 20 Patient Room Orientation 1. Features of Treatment Rooms • Handwashing station • Linen cupboard • Overhead light controls • Call bell and console • Nurse's Cart 2. Bed Operations • Review instructions for the various functions of the bed (i.e. bed rails, incline/recline, foot pedals) • Be aware about the dangers of 'tilting' the bed by accident 3. Patient Telephone • Patients are encouraged to use their cell phones • If patient does not have access to a phone, ask nurse if a cordless phone is available-- IMPORTANT to disinfect after use and return to charger 21 7. Precautionary Measures • Always ask the nurse if the patient asks for food/and or water • Remember to ask the patient if he/she has a fever/cold before administering a warm blanket 5. Building a 'Mental Script' • Build your own mental script when first introducing yourself to patients • Ex: "Hi, my name is... I am an ED volunteer. Is there anything I can get for you?" "Is there anything I can do to make you more comfortable?" 6. Common Patient Requests • Blankets, bed incline/recline adjustments, water, food, light adjustments, commodes, urinals, particular linen • Extra pillows (Ask the aides or housekeeping) • Internet use (WIFI): Username= nhsuser Password=nhspass 22 Communicating in the Waiting Room Addressing patient concerns is very important in the waiting room as unmet concerns have a major effect on the patient experience. Volunteers in the waiting room have the potential to significantly improve the patient experience even before treatment begins. We act as a line of communication between patients and staff; we can answer pressing questions, clarify the factors behind why wait times can get long and simply provide a friendly conversation. Just listening to patients and their concerns can go a long way in making the wait more comfortable. Starting with an introduction is the best approach to interacting with patients in the waiting room: “Hello, my name is… I am a volunteer. Are there any questions I can answer? Or anything I can get for you?” The most common question being asked is with regards to the wait times. Wait times are constantly changing and are extremely difficult to estimate due to the nature of the ED. Management, clinicians and volunteers have expressed caution with regards to raising hopes unrealistically as this can contribute to elevated anxiety and frustration. Therefore, when asked about wait times or the wait list, the most appropriate communication is reassurance and advocacy. 23 Patient/Family Member Scenario 1: Can you find out how long the wait is going to be? Or how many people are ahead of me? Volunteer: First, ask the patient where they are in the triage process“Just so I understand; have you been to the Start Here window, through the brown triage doors or to the registration window yet?” –Patient informs you where they are in the triage process— Second, explain why we are unable to estimate wait times, and insist on confirming that everything is in order“I will be honest, we are unable to estimate how long the wait is going to be because it’s constantly changing. But let me go back and check the system for you to make sure everything is in order.” –Go to Triage or Quick Look Nurse— To nurse: “I just want to confirm that [name]…has been triaged and is in the system.” If asked “Why?” by the nurse, simply respond: “She is concerned and I just want to reassure her that everything is in order and she is in the system.” Third, report back to the patient“I checked with the nurse and triage is complete and you are in the system. This means that the nurses know you are here and based on their assessment, you are safe to be here for now. I know for a fact that they are trying to get you in as soon as possible but unfortunately all the beds are full.” Fourth, inquire if anything else is needed“Is there anything else I can help with? A blanket maybe? If not, my name is [name] and I will be here till around [time] so feel free to ask.” 24 Patient/Family Member Scenario 2: I have been here for 5 hours and people who came after me have already gone in! Volunteer: Guidelines for Scenario1 could be helpful for this Scenario but it’s very important to educate the patient on why this may have happened-“After you have been triaged there are many factors that can cause you to be bumped up or down the waitlist. Usually it has a lot to do with the volume and severity of patients that are coming to the ED. Also, when every bed upstairs is occupied by an admitted patient, a backlog forms in the ED. The wait can be frustrating but I can definitely tell you that everyone in there is working extremely hard to ensure you get seen ASAP and receive the best care possible. 25 Patient/Family Member Scenario 3: Can I get something to drink/eat? Technically, patients cannot ingest anything until they have been assessed by the physician. This has become a grey area since many patients are waiting hours without water or food. This is especially concerning for patients with diabetes. Depending on the nurse, some are comfortable with patients having food and/or water as long they don’t have gastrointestinal symptoms like: Abdominal pain, nausea, vomiting, etc. Volunteer: First, ask the patient if they have been triaged then ifPatient has not been triaged— “Okay, we should just hold-off for now until the nurse has seen you in the Triage Room. When you are in there check with the nurse and we can go from there.” Patient has been triaged— “Great let me just check with the nurse and I will be right back.” Second, Ask Nurse“Can [name] have [whatever patient requested]?” 26 Positive Communication Instead of saying this: That’s inaccurate or I disagree I don’t know I know the wait sucks Ambulances came in Try saying this: That’s an interesting perspective… here’s what I know I am not too sure but let me check for you I know the wait is difficult and it can be frustrating but everyone in there is working hard to get you in as soon as possible. Traumas came in Parking Information Short term Drop-Off Parking is located in front of the main hospital entrance and Emergency Department free of charge. Cars can be moved to Parking Lot A once the patient is seen by Triage. *When parking in lots with the gated system, please be sure to take your ticket with you after parking. Do not leave it in your vehicle. When you are ready to leave the hospital, please pay at one of the Precise Parklink kiosks located in the main lobby. Please note that vehicles are not permitted to park alongside the sidewalk adjacent to the main entrance. This restriction is in place to ensure the safe onboarding and offloading of patients from patient transfer vehicles. Current Parking Rates $2.00 per ½ hour $4.00 per 1 hour $8 for up to 12 hours (no in/out privileges) $16.00 Daily Pass (in/out privileges) $40.00 per 1 week (7 days) $80.00 per month (31 days, to be purchased at the St. Catharines Site) For more information, please email our parking office or call 1-888-7837275 27 Handling Complaints Use effective listening skills when someone comes forward with a complaint Apologize on behalf of the hospital for their experience Support the Hospital. Focus on the positives Encourage them to speak to their care provider or unit manager Direct them to call the Patient Relations Specialists at extension 44423 Think TEAM: Be supportive of Staff and others working hard to care for patients. It is ok to let patients know that the ED is a busy place and staff are taking care of many patients, some with critical illness or injury. Respond with HEART Hear the Story Empathize Apologize Respond and Take Action Thank them for bringing forth their concerns 28 Understanding Patient Flow at SCS ED The healthcare process begins as soon as patients walk through the sliding glass doors. Their first stop is usually the waiting room and this is where triage, registration and waiting takes place. “Start Here” Window This is the patient’s first step The triage process begins here with a “quick assessment” The nurse completes a very brief work-up on the patient to determine if the patient is stable (safe to wait) or unstable (needs to be triaged immediately) If the patient is stable, they wait to be called by the Triage Nurse. Triage Rooms 1-3 This is the patient’s second step This is where the Triage Nurses conduct a “full assessment” and determines how severe or life threatening a patient’s condition is ~FYI ~ Triage is defined as the process of categorizing patients based on the severity of their symptom. CTAS is the scale used in Canada to rank these patients Registration Desk This is the patient’s final destination before waiting to be brought into the ED The patient’s information is taken and their wristband is printed. * This new process can generate concern amongst patients so being able to explain the process and clarifying the patient’s “next step” can go a long way in alleviating stress.* 29 Factors Affecting Patient Flow and Wait Times Patient flow describes the movement of patients through the healthcare delivery process from admission to discharge. A patient may experience wait times throughout this process. Patient Triaged Waiting Patient Brought to Room or UCC Chair The wait time most commonly referred to is the time between arriving in the ED to being brought to a room. As patient flow slows, wait times increase. What are the main factors effecting patient flow? 1. Volume of patients coming through the front door and the severity of their illnesses. 2. Volume of patients coming in via ambulance and the severity of their illnesses. These patients may be rushed to a room immediately, or will be brought to Unit C (ambulance offload unit), or if ED is completely full, they will wait on stretchers. Note: If patient is stable and does not require a bed, they may be brought to the waiting room until a room is available. 30 ~FYI~ The factors listed above may result in a patient being “bumped” up or down the wait list. CTAS 1-2 patients will typically be bumped-up the list. CTAS 4-5 patients can be bumped-down the list. However, the length of time a patient has waited also factors in. Example: A CTAS 4 patient who has been waiting for four hours may get a room before a CTAS 3 patient who recently presented. 3. Number of patients in the ED waiting for a bed on the medical floors 4. Availability of rooms on inpatient units to receive patients from ED. This is affected by the number of patients on inpatient units, how many of them are being discharged and what time discharge occurs. This is also impacted by the availability of care for the patient post discharge whether that be going home, or moving to other care such as Shaver Rehabilitation, Long Term Care, Hospice and other facilities where there can also be wait times for admission. 31 Infection Control Procedures 1. Contact Precaution Signs • Familiarize yourself with IPAC signs • Understand differences between the signs 2. Personal Protective Equipment (PPE) • Be comfortable with proper wear and disposal of PPE and ask nurse to review if unsure • Reference Donning and Doffing (Page 22) • Ensure diligent hand washing practices 3. Other Information • Kindly educate family members and/or patients seen walking outside of a room with PPE • Always check for contact precaution signs before entering a room...if unsure, ASK! 32 Volunteers are permitted to enter rooms to provide comfort measures to patients with signs for Contact Precautions and Droplet/Contact Precautions. Be sure to read signs and wear the appropriate PPE. Providing care in these rooms is not mandatory and each Volunteer will make his/her own decision. Volunteers are asked NOT to enter rooms or provide care to patients in rooms marked with Airborne Precautions Signs. 33 New Volunteer Orientation & Training Process NHS Volunteer Orientation Department Shadow Shift #1 Start Regular Shifts Department Shadow Shift #2 NHS Volunteer Orientation Aim: Educate new volunteers on the mandate of volunteer resources, the policies in place to maintain safety, confidentiality, and professional conduct. Department Shadow Shift Aim: To develop a strong understanding of the department specific role, way-finding throughout the department, how volunteers communicate with patients, families and staff. Preparation of the new volunteer to commence regular shifts. 34 Shadow Shift #1 Department Orientation Where am I going during a shift in this department? Focus: Orientating the volunteer to the department’s overall layout Orientating the volunteer to department processes (Triage process, Nurse-to-patient assignment, etc.) Orientating the volunteer to policies and procedures commonly encountered (Infection control, confidentiality, NPO-food/drink restrictions, etc.) Introduction to volunteer’s role in patient care Evaluate volunteer’s understanding of material covered Shadow Shift #2 Role Orientation What is my role and how do I fulfill it? Focus: Orientating the volunteer to their role within the department Actively engage in patient and family interaction Orientating volunteer on various tasks commonly—and uncommonly—encountered during a shift Confirm volunteer’s understanding of policies and procedures (Especially: infection control and confidentiality) Evaluate volunteer’s understanding of material covered and comfort with the role 35 Interested in Leadership? Consider becoming a Trainer! At the foundation of the Emergency Department Volunteer team is a small but mighty group of individuals who provide orientation and training to new volunteers in the Emergency Department. ED Trainers have Minimum One Year experience in the Emergency Department Demonstrate success as an ED Volunteer Consistently meet commitment for weekly shifts Have a knack for teaching, role modeling, coaching Good communication and Leadership skills Please contact me at danderson@niagarahealth.on.ca for more information if you are interested in knowing more about this opportunity. 36 QUESTIONS??? Please seek out answers to any questions you may have: Rob Smith – ED Volunteer Team Lead Robert.Smith@niagarahealth.on.ca Debbie Anderson – Coordinator, Volunteer Resources danderson@niagarahealth.on.ca or… Speaking with the Charge Nurse on Duty, the Triage Nurse or Emergency Department Manager Lisa Hildebrand Thank you! Thanks for taking the time to review this important information and taking action on new initiatives to improve the experience for patients and their loved ones in the Emergency Department. We hope the information in this Handbook is valuable to you and helps you make the most of your experience as an Emergency Department Volunteer. 37