1866
Effect of Endotoxin and Cytokines on
Lipoprotein Lipase Activity in Mice
Kenneth R. Feingold, Maureen Marshall, Rocco Gulli, Arthur H. Moser, Carl Grunfeld
Downloaded from http://atvb.ahajournals.org/ by guest on October 2, 2016
Abstract Endotoxin (lipopolysaccharide [LPS]) stimulates
the production of cytokines, which mediate many of the
metabolic effects associated with infection. In LPS-sensitive
C57B1/6 mice, LPS doses as low as 0.01 fig per mouse
decreased adipose tissue lipoprotein lipase (LPL) activity by
greater than 50%. In LPS-resistant C3H/HeJ mice, which do
not produce cytokines in response to LPS, doses of LPS as high
as 10 fig per mouse did not affect LPL activity in adipose
tissue. In muscle of C57B1/6 mice, LPL activity was decreased
by 27% after 10 fig of LPS, whereas in C3H/HeJ mice there
was no effect. These results indicate that the LPS-induced
decrease in both adipose and muscle LPL activity is mediated
by cytokines. Tumor necrosis factor (TNF), interleukin (IL)-l,
leukemia-inhibiting factor (LJF), interferon alfa, and interferon gamma all decreased adipose tissue LPL activity in
intact mice. In skeletal and cardiac muscle, only IL-1 and
interferon gamma decreased LPL activity, whereas TNF, LJF,
and interferon alfa had no effect. Inhibition of TNF activity
blocked the increase in serum triglycerides that is characteristically observed after LPS but did not affect the ability of
LPS to decrease adipose tissue LPL activity. Inhibition of IL-1
activity with IL-1 receptor antagonist partially inhibited the
increase in serum triglycerides; however, the ability of LPS to
decrease LPL activity in either adipose or muscle tissue was
not affected. These data indicate that although TNF and IL-1
play a role in mediating the increase in serum triglyceride
levels, these cytokines do not play a crucial role in the
inhibition of either adipose or muscle LPL activity. These
results also indicate that the decrease in LPL activity is not a
key event responsible for the increase in serum triglyceride
levels. In conclusion, although the inhibition of LPL activity
produced by LPS is mediated by cytokines, these effects are
not dependent on either TNF or IL-1. Changes in LPL are not
essential for the induction of hypertriglyceridemia but may
influence the distribution of nutrients. (Arteriosder Thromb.
1994;14:1866-1872.)
Key Words • tumor necrosis factor • interleukins •
interferons • serum triglycerides • leukemia inhibitory
factor
acterial, viral, and parasitic infections are frequently associated with hypertriglyceridemia
secondary to elevations in very-low-density lipoprotein (VLDL) levels.14 Endotoxin (LPS) administration, which mimics Gram-negative bacterial infections, has been shown to produce hypertriglyceridemia
by stimulating the hepatic production of VLDL and/or
by inhibiting the clearance of triglyceride-rich lipoproteins.3-5-6 The activity of lipoprotein lipase (LPL), a key
regulatory enzyme in the catabolism and clearance of
triglyceride-rich lipoproteins, is decreased after LPS
treatment in both adipose tissue and muscle.5'7'8-10 Recent studies have suggested that the decrease in adipose
tissue LPL activity is due to a posttranslational effect.11
Infection and LPS administration stimulate the production of a large number of cytokines, the hormones of
the immune system, and these cytokines are thought to
mediate many of the metabolic effects associated with
infection and LPS treatment. In adipocytes in culture,
studies by our and other laboratories have demonstrated that many cytokines, including tumor necrosis
factor (TNF), interleukin (IL)-l, IL-6, IL-11, leukemiainhibiting factor (LJF), interferon alfa (IFN-a), and
B
interferon gamma (IFN-y) inhibit LPL activity.1219
However, to date, the administration only of TNF and
IL-6 has been shown to decrease adipose tissue LPL
activity in intact animals.18-20-21 TNF decreased epididymal fat LPL activity without affecting activity in several
other sites.21 Moreover, the effect of cytokines on
muscle LPL activity in vivo and in vitro has not been
extensively explored. Our studies21 and those of Semb et
al20 have demonstrated that in rats, TNF does not
decrease muscle LPL activity.
The purpose of the present study was to determine
the following: (1) whether the LPS-induced decrease in
adipose and muscle LPL activity requires cytokine
production; to determine this we used HeJ mice, which
do not produce cytokines in response to LPS22-23; (2) the
effect of TNF, IL-1, LIF, IFN-a, and IFN-yon adipose
and muscle LPL activity in intact mice; and (3) whether
either TNF or IL-1, the major cytokines produced in
response to LPS administration, mediate the LPSinduced changes in LPL activity.
Received February 10, 1994; revision accepted July 11, 1994.
From the Department of Medicine, University of California,
San Francisco, and the Metabolism Section, Medical Service,
Department of Veterans Affairs Medical Center, San Francisco,
Calif.
Correspondence to Kenneth R. Feingold, MD, Metabolism
Section (111F), Department of Veterans Affairs Medical Center,
4150 dement St, San Francisco, CA 94121.
© 1994 American Heart Association, Inc.
Tritiated triolein was purchased from New England Nuclear.
Triolein, lecithin, and fatty acid-free bovine serum albumin were
purchased from Sigma Chemical Co. CytoScint scintillation fluid
was purchased from ICN Biochemical, Inc. Endotoxin (Escherichia coli, strain 055:B5) was purchased from Difco Laboratories. Murine TNF with a specific activity of 2.9 xlO7 U/mg,
murine IFN- y with a specific activity of 5 x 10' U/mg, and human
LJF at a concentration of 2.05 mg/mL were kindly provided by
Genentech Inc. Recombinant human IL-10 (amino acids 112 to
Methods
Materials
Feingold et al Cytokines and Lipoprolein Lipase
1867
269) with a specific activity of 5xlO7 U/mg was produced as
described previously and kindly provided by Dr Charles A.
Dinarello of Tufts University, Boston, Mass.24 Recombinant
human IFN-a (A/D) (specific activity 7.9 xlO7 U/mg) was kindly
provided by Drs M. Brunda and P. Sorter of Hoffmann-La
Roche. Human IFN-a (A/D) hybrid has been shown to regulate
mouse tissues in a manner similar to that of murine IFN-a.23
Antibodies against TNF were generated by immunization of New
Zealand White rabbits by standard techniques at Caltag Laboratories. Immunoglobulins were purified from serum by ammonium
sulfate precipitation by means of previously described procedures
to avoid LPS contamination. IL-1 receptor antagonist (IL-lra)
was kindly provided by Dr Robert C. Thompson of Synergen, Inc.
Downloaded from http://atvb.ahajournals.org/ by guest on October 2, 2016
Animal Procedures
C57BI/6 male mice (weight, 18 to 20 g) were purchased from
Simonsen Laboratories (Gilroy, Calif), and C3H/HeJ male
mice (weight, 18 to 20 g) were purchased from Jackson
Laboratories (Bar Harbor, Me). The animals were maintained
in a normal 12-hour light/dark cycle and were fed Purina
mouse chow (Ralston Purina) and water ad libitum. On the
evening before the study (16 hours before study), animals were
injected with the indicated doses of LPS (10 fig per mouse),
TNF (1 fig per mouse), IL-1 (80 ng per mouse), LIF (5 jig per
mouse), IFN-a (50 fig per mouse), or IFN-y (50 tig per
mouse), or with the appropriate vehicle alone (controls).
These doses of TNF, IL-1, IFN-a, and IFN-y have previously
been shown by our laboratory to stimulate hepatic lipid
synthesis.26 The dose of LIF used has been shown by other
investigators to be effective in vivo.27 LPS was administered
intraperitoneally in 0.9% saline solution. TNF, IL-1, LIF,
IFN-a, and rFN-y were administered intraperitoneally in 0.1%
human serum albumin solution. Food was withdrawn from the
animals after the injection because LPS and cytokines have
been shown to induce anorexia. When indicated, animals were
injected intraperitoneally with saline or anti-TNF antibodies
(quantity of antibodies sufficient to neutralize 34 ^ig of TNF)
4 hours before LPS administration. When indicated, animals
were injected subcutaneously with IL-lra (1 mg per mouse in
0.1% human serum albumin) at 0, 2, 4, and 6 hours after LPS
administration. It has been shown by several investigators that
the effect of LPS on IL-1 secretion and mRNA induction is
maximal within 60 to 90 minutes28-29; hence, the IL-lra dose
schedule used here should be able to block the effect of IL-1
induced by a single bolus of LPS.
LPL Activity
Mice were killed 16 hours after LPS or cytokine administration, and then the epididymal fat pad, quadriceps muscle, a
combination of biceps and triceps muscle, and heart were
removed and frozen in liquid nitrogen. The frozen tissue was
weighed, chopped into fine pieces, and transferred to a 15-mL
centrifuge tube. LPL was extracted with a phosphate buffer
(pH 7.5) containing 0.118 mol/L NaCl, 0.005 mol/L KC1,
0.0012 mol/L KH2PO4, 0.0012 mol/L MgSO,, 0.55 mol/L
CaCl2, and heparin (4 U/mL) for 60 minutes at 37°C. Liporytic
activity was determined as described previously.21 Briefly, the
substrate (unlabeled triolein) and 18.75 /iCi of tritiated triolein were homogenized with 3.0 mg of lecithin, 1.2 mL of 20%
fatty acid-free bovine serum albumin, 0.5 mL normal human
plasma (LPL cofactor), 0.5 mL 1% Triton X-100, 15 U
heparin, and 6.8 mL of 1 mol/L tris(hydroxymethyl)aminomethane buffer, pH 8.6. An aliquot of the resultant emulsion (0.1 mL) and 0.4 mLof the extracted medium of the tissue
were incubated in a metabolic shaker at 37°C for 60 minutes.
The reaction was stopped by addition of 4.0 mL of isopropanol-sulfuric acid reagent (10 mL 3N sulfuric acid, 400 mL
isopropanol). Subsequently, the tritiated oleic acid was separated from triolein by sequential hexane extraction and alkalinization; an aliquot of the alkaline medium was counted. One
LPS (ug / mouse)
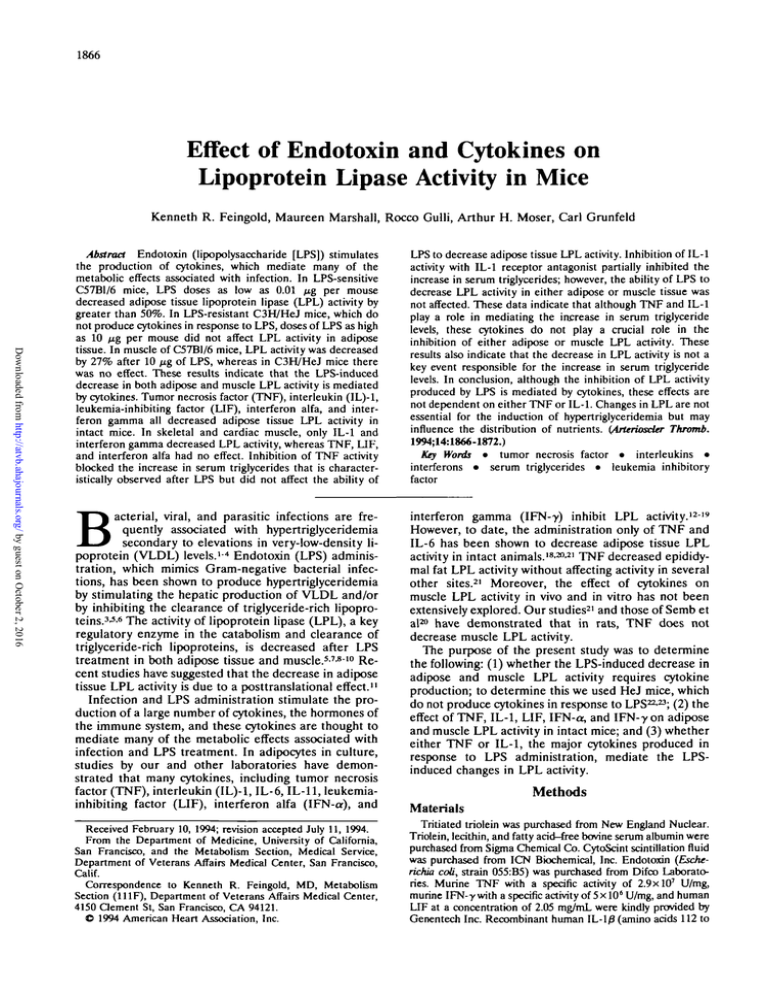
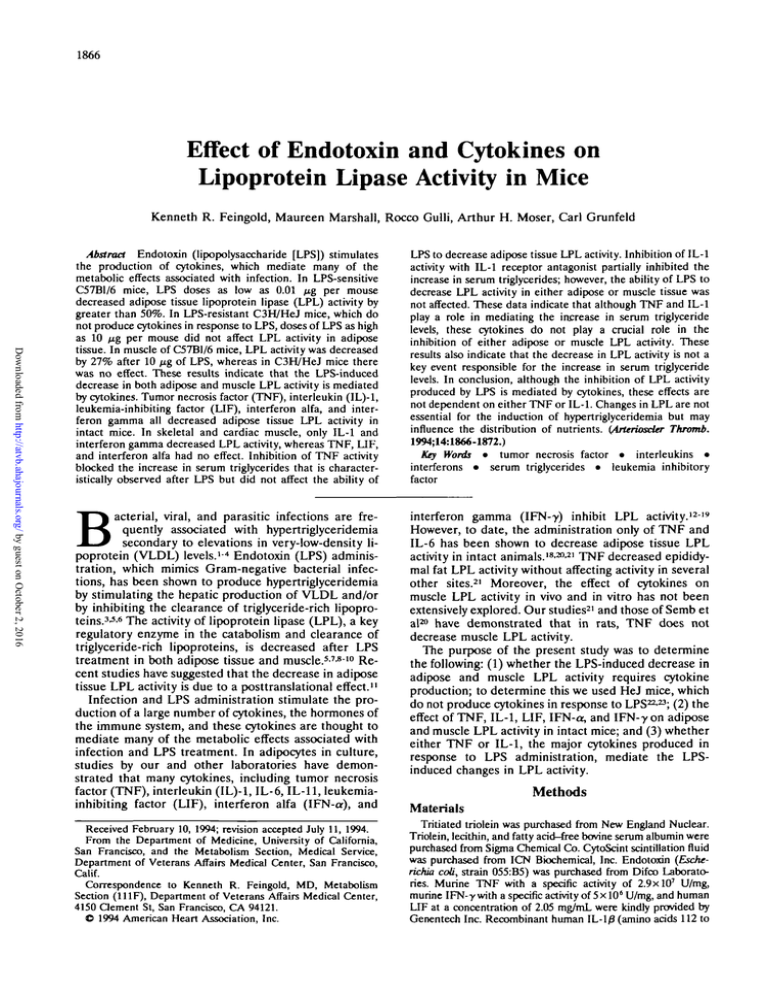
FIG 1. Une graph shows dose-response curves for the effect of
endotoxin (lipopotysaccharlde [LPS]) on adipose tissue lipoprctein lipase (LPL) activity in C57BI/6 and C3H/HeJ mice. Animals
were injected with the LPS dose indicated on the abscissa.
Sixteen hours later the animals were killed, and adipose tissue
LPL activity was determined as described in "Methods." Values
are mean±SEM; n=10 for controls and n=5 for each dose in
C57BI/6 and C3H/HeJ mice. *P<.01 compared with controls.
Control LPL activity in C57BI/6 mice was 138 and in C3H/HeJ
mice 87 nmol/h per 100 mg tissue.
unit of LPL is defined as nanoequivalents of free fatty acid
released per hour. Values are expressed per 100 mg of tissue.
Serum Triglyceride Levels
We measured serum triglyceride levels using Sigma Diagnostic Kit No. 337 (Sigma Chemical Co). Serum glycerol levels
were subtracted from total serum glyceride levels.
Statistical Analysis
Data are presented as mean±SEM. Statistical significance
between groups was calculated by Student's t test. Because
baseline LPL activity varied between experimental groups,
only animals that were studied simultaneously under identical
conditions were compared.
Results
Effects of LPS on Serum Triglyceride
and LPL Activity
The effects of LPS on serum triglyceride levels in
C57B1/6 and C3H/HeJ mice have been previously reported.30 In C57B1/6 mice serum triglyceride levels were
increased 62% and 76% by 16 hours after the administration of 1 and 10 fig of LPS, respectively.30 In contrast,
in LPS-resistant C3H/HeJ mice, serum triglyceride levels were not significantly increased by LPS doses as high
as 100 fig per mouse.30 These results indicate that the
increase in serum triglyceride levels induced by LPS is
mediated by cytokines secreted by macrophages.
The effect of LPS on adipose tissue LPL activity is
shown in Fig 1. In LPS-sensitive C57B1/6 mice, LPS
doses as low as 0.01 fig per mouse decreased LPL
activity by greater than 50%. Higher doses of LPS did
not result in a further reduction in LPS activity. In
LPS-resistant C3H/HeJ mice, doses of LPS as high as 10
Mg per mouse did not affect LPL activity in adipose
tissue. In quadriceps muscle of C57B1/6 mice, LPL
activity was decreased by 27% 16 hours after administration of 10 fig LPS (Fig 2). In cardiac muscle we
observed only a 16% decrease in LPL activity after LPS
administration, and this decrease was not statistically
significant (mean of four separate experiments; n=5 for
1868
Arteriosclerosis and Thrombosis Vol 14, No 11 November 1994
Control
Treatment
O
FIG 2. Bar graph shows effect of endotoxin (lipopolysaccharide
[LPS]) on quadriceps muscle lipoprotein lipase (LPL) activity in
C57BI/6 and C3H/HeJ mice. Animals were injected with 10 \i%
LPS, and 16 hours later muscle LPL activity was determined as
described in "Methods." Values are mean±SEM; n=5 for each
group. Control LPL activity in C57BI/6 mice was 506 and in
C3H/HeJ mice 414 nmol/h per 100 mg tissue.
Downloaded from http://atvb.ahajournals.org/ by guest on October 2, 2016
control and LPS treatment for each experiment). In
C3H/HeJ mice, 10 /xg LPS had no effect on quadriceps
muscle LPL activity (Fig 2). The lack of response of
C3H/HeJ mice indicates that the effect of LPS on both
adipose and quadriceps muscle LPL activity is mediated
by cytokines.
Effect of Cytokines on Serum Triglyceride
and LPL Activity
The effect of cytokines on serum triglyceride levels is
shown in Fig 3. As reported previously, both TNF and
IL-1 increased serum triglyceride levels (TNF, 72%;
IL-1, 11O%).30-32 LIF administration also produced an
increase in serum triglyceride levels (41%). With IFN-y
there was a trend toward an increase (35%), but this did
not reach statistical significance. IFN-a administration
did not increase serum triglyceride levels.
100
Fra 4. Bar graph shows effect of cytokines on adipose tissue
lipoprotein lipase (LPL) activity in C57BI/6 mice. Animals were
injected intraperitoneally with saline (control), tumor necrosis
factor (TNF), interieukin (IL)-1, leukemia-inhibiting factor (UF).
interferon alfa (IFN-a), or interferon gamma (IFN-y) and killed 16
hours later. LPL activity In adipose tissue was measured as
described in "Methods." Values are mean±SEM. Control and
TNF, n=5; control and IL-1, n=10; control and UF, n=10; control
and IFN-a, n=15; and control and IFN-y, n=10 and 8, respectively. Control LPL activity was 246, 485, 277, 279, and 311
nmol/h per 100 mg tissue for TNF, IL-1, UF, IFN-a, and IFN-y,
respectively.
The effect of cytokines on adipose tissue LPL activity
is shown in Fig 4. TNF, IL-1, LIF, IFN-a, and IFN--y all
decreased epididymal adipose tissue LPL activity. In
contrast, in two sites of skeletal muscle (quadriceps [Fig
5, top panel] and triceps/biceps [Fig 5, bottom panel]),
I
13
too
FIG 3. Bar graph shows effect of cytokines on serum triglyceride (TQ) levels in C57BI/6 mice. Animals were injected Intraperitoneally with saline (control), tumor necrosis factor (TNF) (1 ^g),
interieukin (1L)-1 (80 ng), leukemia-inhibiting factor (UF) (5 /tg),
interferon alfa (IFN-a) (50 HQ), or interferon gamma (IFN-y) (50
tug) and killed 16 hours later. Serum triglycerides were measured as described in "Methods." Values are mean±SEM.
Control, n=50; TNF, n=5; IL-1, n=10; UF, n=10; IFN-a, n=15;
and IFN-y, n=8. The difference between control values and TNF,
IL-1, or UF was statistically significant compared with simultaneously studied control animals. Because serum TG levels were
similar in all control groups, they were pooled for ease of
presentation.
FIG 5. Bar graphs show effect of cytokines on quadriceps (top)
or biceps and triceps (bottom) muscle lipoprotein lipase (LPL)
activity in C57BI/6 mice. Animals were injected intraperitonealiy
with saline (control), tumor necrosis factor (TNF), interieukin
(IL)-1, leukemia-inhibiting factor (UF), Interferon alfa (IFN-a), or
interferon gamma (IFN--y) and killed 16 hours later. LPL activity In
muscle tissue was measured as described in "Methods." Values
are mean±SEM. For quadriceps: control and TNF, n=5; control
and IL-1, n«=10; control and UF, n=5; control and IFN-a, n=10;
and control and IFN-y, n=5. Control LPL activity was 506, 885,
238, 671, and 405 nmol/h per 100 mg tissue for TNF, IL-1, UF,
IFN-a, and IFN--y, respectively. For biceps plus triceps: controls,
n=iO; all cytokines, n=5. Control LPL activity was 257 nmol/h
per 100 mg tissue for all cytokines.
Feingold et al
^
O
Cytokines and Lipoprotein Lipase
1869
150
5
T
150
IOC
I
FIG 6. Bar graphs show effect of cytoklnes on heart lipoprotein
lipase (LPL) activity in C57BI/6 mice. Animals were injected
intraperitoneally with saline (control), tumor necrosis factor
(TNF), interleukin (IL)-1, leukemia-inhibiting factor (LJF), interferon alfa (IFN-a), or interferon gamma (IFN->) and killed 16
hours later. LPL activity In cardiac tissue was measured as
described in "Methods." Values are mean±SEM; n=5 for controls and all cytoklnes. Control LPL activity was 1040 nmol/h per
100 mg tissue for TNF, IL-1, and IFN-a and 630 nmol/h per 100
mg tissue for IFN-y and LJF experiments.
Control
LPS
TNF-Ab LPS.TNF-Ab
Downloaded from http://atvb.ahajournals.org/ by guest on October 2, 2016
only IL-1 and IFN-y decreased LPL activity, whereas
TNF, LIF, and IFN-a had no effect. Similarly, in the
heart only IL-1 and IFN-y decreased LPL activity,
whereas TNF, LIF, and IFN-a had no effect (Fig 6).
Effect of Inhibition of TNF and IL-1 on Serum
Triglyceride Levels and LPL Activity
To inhibit TNF activity we used an antibody that we
have previously shown neutralizes TNF activity in
vivo.6-30 Pretreatment with TNF antibody blocked the
increase in serum triglyceride levels that is characteristically observed after LPS administration (Fig 7, top
panel). However, as shown in the bottom panel of Fig 7,
the ability of LPS to decrease adipose tissue LPL
activity is not affected by pretreatment with TNF antibodies. These results indicate that although TNF is an
important mediator of the increase in serum triglyceride
levels, TNF is not crucial for the LPS-induced inhibition
of adipose tissue LPL activity. Moreover, these results
suggest that a decrease in adipose tissue LPL activity is
not the key event responsible for the increase in serum
triglyceride levels.
To inhibit IL-1 activity, we used IL-lra, which we
have previously shown neutralizes IL-1 activity in
vivo.6-30 As shown in the top panel of Fig 8, administration of IL-lra partially inhibits the increase in serum
triglyceride levels induced by LPS. However, the ability
of LPS to decrease LPL activity in either adipose tissue
(Fig 8, middle panel) or muscle (Fig 8, bottom panel) is
not affected by inhibition of IL-1 activity. These data
indicate that although IL-1 plays a role in mediating the
increase in serum triglyceride levels, it does not play a
crucial role in the inhibition of either adipose or muscle
LPL activity induced by LPS.
Discussion
Low-dose LPS administration has been shown to
increase serum triglyceride levels in rats by stimulating
the secretion of VLDL by the liver, whereas high-dose
LPS inhibits the clearance of triglyceride-rich lipoproteins.6 The delay in lipoprotein clearance has been
attributed to LPS decreasing LPL activity in both
muscle and adipose tissue.3-310 Previous studies by this
laboratory and other laboratories have shown that
TNF At) LPS.TNF Ah
FIG 7. Bar graphs show effect of anti-tumor necrosis factor
antibodies (TNF-Ab) on endotoxin (lipopolysaccharide [LPS])
effect on serum triglyceride (TQ) levels (top) and adipose tissue
lipoprotein lipase (LPL) activity (bottom) in C57BI/6 mice. Animals were injected with saline or arrti-TNF-Ab followed by saline
or LPS as described in "Methods." Sixteen hours later the
animals were killed, and serum TQ levels (top) and adipose
tissue LPL activity (bottom) were determined as described In
"Methods." Values are mean±SEM; n»5 for each group.
cytokine production is required for the LPS-induced
increase in serum triglyceride levels.8-30 LPS administration to C3H/HeJ mice, which are incapable of producing cytokines in response to LPS, fails to result in an
increase in serum triglyceride levels.8-30 In the present
study we demonstrate that LPS treatment of C3H/HeJ
mice also does not decrease LPL activity in adipose
tissue. In contrast, in C57B1/6 mice, which produce
cytokines in response to LPS, treatment with LPS
decreases adipose tissue LPL activity. These results
confirm the studies of Kawakami and Cerami,8 who
previously demonstrated the failure of LPS to decrease
adipose tissue LPL activity in C3H/HeJ mice. Moreover, we now demonstrate that the LPS-induced inhibition of muscle LPL activity also requires cytokine
production. In C3H/HeJ mice, LPS treatment had no
effect on muscle LPL activity, whereas in C57B1/6 mice,
LPS treatment decreased muscle LPL activity. Thus,
the decrease in LPL activity in both adipose tissue and
muscle that occurs after LPS treatment is mediated by
cytokine production.
Previous studies have shown that a variety of different
cytokines, including TNF, IL-1, IL-6, IL-11, LIF,
IFN-a, and IFN-% inhibit the activity of LPL in cultured adipocytes.1219 However, in intact animals only
TNF and IL-6 have previously been shown to decrease
adipose tissue LPL activity.18-20-21 Interferons decrease
1870
Arteriosclerosis and Thrombosis
Vol 14, No 11 November 1994
LPS*IL-1ra
TDD
Downloaded from http://atvb.ahajournals.org/ by guest on October 2, 2016
LPS*IL-1ra
FIG 8. Bar graphs show effect of irrterieukln (ll_)-1 receptor
antagonist (ra) on endotoxin (lipopolysaccharide [LPS]) effect on
serum triglycerlde (TG) levels (top) and adipose (middle) or
quadriceps muscle (bottom) lipoprotein lipase (LPL) activity in
C57BI/6 mice. Animals were Injected with saline or IL-1 ra at 0, 2,
4, and 6 hours after LPS administration as described in "Methods." Sixteen hours after LPS the animals were killed, and serum
TG levels (top), adipose tissue LPL activity (middle), and muscle
tissue LPL activity (bottom) were determined as described In
"Methods." Values are mean±SEM; n=5 for each group.
postheparin LPL activity in plasma, but whether this is
due to a decrease in adipose tissue LPL activity is
unknown.33-34 IL-1 did not affect LPL activity in postheparin plasma of primates and caused only a small
nonsignificant decrease in LPL activity in adipose tissue
of rats.35-36 In the present study we demonstrate that the
administration of TNF, IL-1, LIF, IFN-a, and IFN-y to
intact mice decreases LPL activity in adipose tissue.
Thus, as observed in tissue culture studies, a large
number of different cytokines are capable of decreasing
adipose tissue LPL activity.
Studies in rodents have suggested that muscle LPL
activity accounts for a substantial portion of the clear-
ance of triglyceride-rich lipoproteins from the circulation.37 Moreover, during fasting, the activity of LPL in
adipose tissues decreases, and the importance of muscle
in the clearance of triglyceride-rich lipoproteins increases.38-39 Therefore, the status of muscle LPL activity
is of great importance in determining the rate of clearance and the distribution of uptake of triglyceride-rich
lipoproteins. The effect of cytokines on muscle LPL
activity in vivo and in vitro has not been extensively
explored. Studies by our laboratory21 and by Semb et
al20 have shown that in intact rats, TNF does not
decrease LPL activity in muscle. In the present study we
demonstrate that in intact mice IL-1 and IFN-y decrease skeletal muscle and heart LPL activity, whereas
TNF, LIF, and IFN-a have no effect. Thus, while many
cytokines inhibit adipose tissue LPL activity, only IL-1
and IFN-y have been shown to decrease LPL activity in
muscle. One can speculate that this selective effect on
LPL could influence the distribution of nutrients between tissues.
In the present study we measured LPL activity in
adipose and muscle tissue, which includes both intracellular and extracellular enzymes. The enzyme activity
that is important in lipoprotein metabolism is localized
to the endothelial surface. Unfortunately, at the present
time assays to specifically determine the activity of LPL
on the endothelial cell surface are not available. Nevertheless, studies have shown that LPL activity measured in whole tissue reflects the uptake by these tissues
of labeled lipid in triglyceride-rich lipoproteins.39
We next determined whether either TNF or IL-1, the
primary cytokines secreted in response to LPS, is responsible for the decrease in LPL activity in either
adipose tissue or muscle. Neutralization of TNF with
TNF antibodies markedly diminished the ability of LPS
to increase serum trigryceride levels, indicating that
TNF is an important mediator of hypertrigfyceridemia.
However, the inhibition of adipose tissue LPL activity
was not affected by the inhibition of TNF action,
indicating that TNF is not crucial for the LPS-induced
decrease in adipose tissue LPL activity. When IL-1
activity was inhibited by administration of LL-lra, there
was a partial inhibition of the LPS-induced increase in
serum triglycerides, indicating that IL-1 contributes to
hypertriglyceridemia. However, similar to our observations with TNF, the inhibition of IL-1 activity did not
affect the ability of LPS to decrease either adipose or
muscle LPL activity, indicating that IL-1 does not play
a critical role in mediating the LPS inhibition of LPL
activity. From experiments in HeJ mice it is apparent
that cytokines play a key role in mediating changes in
LPL activity. Which cytokine or combinations of cytokines are responsible for the LPS effect on LPL activity
is not clear. Based on previous studies and the experiments reported here, a large number of cytokines could
be responsible for the inhibition in adipose tissue,
whereas in muscle tissue, the number of potential
candidates uncovered thus far is small. Unfortunately,
reagents to inhibit the activity of these varied cytokines
in intact animals are not currently available to us.
It should also be recognized that while the inhibitors
of either TNF or IL-1 action had no effect on LPL
activity, these inhibitors were able to blunt the increase
in serum trigryceride levels induced by LPS. This discordant effect on LPL activity and trigryceride levels
Feingold et al
Downloaded from http://atvb.ahajournals.org/ by guest on October 2, 2016
suggests that the increase in serum triglycerides is not
related to the inhibition of LPL activity. This is in
agreement with previous studies that have demonstrated that LPS administration under certain circumstances increases serum triglyceride levels by stimulating hepatic VLDL secretion.6 Furthermore, we and
other laboratories have also shown that TNF and IL-1
increase serum triglyceride levels by increasing hepatic
VLDL secretion without affecting the clearance of
trigryceride-rich lipoproteins.21-31-32-40-41 Here we also
report that IFN-a and IFN--y can decrease LPL activity
without increasing serum trigryceride levels at 16 hours.
Thus, the present studies provide further evidence that
changes in serum trigryceride levels are not necessarily
mediated by changes in LPL activity. The changes in
LPL activity may not regulate serum triglyceride levels,
but rather they could alter the distribution of nutrients
between various tissues. It is well recognized that cytokines play a predominant role in the development of
cachexia during chronic infections and cancer, and it is
possible that cytokine-induced alterations in LPL activity could contribute to these changes.
In summary, the present study demonstrates that the
inhibition of LPL activity in adipose tissue may be
mediated by a wide variety of cytokines, whereas the
inhibition of LPL activity in muscle tissue is produced
by a more limited number of cytokines. However, the
effects of LPS on LPL activity are not mediated by TNF
or EL-1. The question of which cytokine or combinations
of cytokines mediate LPS-induced changes in LPL
activity awaits the development of additional blocking
reagents.
Acknowledgments
This study was supported by grants from the Research
Service of the Department of Veterans Affairs and the National Institutes of Health (DK-40990 and DK-07418). We
appreciate the excellent editorial assistance of P. Herranz.
References
1. Gallic JI, Kaye D, O'Leary WM. Serum lipids in infection. N Engl
J Afef.l969;281:1081-1086.
2. Fiser RH, Denniston JC, Bcisel WR. Infection with Dipiococcus
pneumoniae and Salmonella typhimurium in monkeys: changes in
plasma lipids and lipoproteins. / Infect D«.1972;125:54-60.
3. Kaufmann RL, Matson CF, Beisel WR. Hypertriglyceridemia
produced by endotoxin: role of impaired triglyceride disposal
mechanisms. J Infect Dis. 1976;133:548-555.
4. Lanza-Jacoby S, Wong SH, Tabares A, Baer D, Schneider T.
Disturbances in the composition of plasma lipoproteins during
gram negative sepsis in the rat. Biochim Biophys Acta. 1992;1124:
233-240.
5. Bagby GJ, Corll CB, Martinez RR. Triacylglycerol kinetics in
endotoxic rats with suppressed lipoprotein lipase activity. Am J
Physiol. 1987;253:E59-E64.
6. Feingold KR, Staprans I, Memon RA, Moser AH, Shigenaga JK,
Doerrler W, Dinarello CA, Grunfeld C. Endotoxin rapidly induces
changes in lipid metabolism that produce hypertriglyceridemia:
low doses stimulate hepatic trigryceride production while high
doses inhibit clearance. / Lipid Res. 1992^3:1765-1776.
7. Bagby G, Spitzer JA. Lipoprotein lipase activity in at heart and
adipose tissue during endotoxin shock. Am J Physiol. 198CH238:
H325-H330.
8. Kawakami M, Cerami A. Studies of endotoxin-induced decrease in
lipoprotein lipase activity. J Exp Med. 1981;154:631-639.
9. Bagby GJ, Spitzer JA. Decreased myocaidia] extracellulw and
muscle lipoprotein lipase activities in endotoxin treated rats. Proc
Soc Exp Biol Med. 168:395-398.
10. Scholl RA, Lang CH, Bagby GJ. Hypertriglyceridemia and its
relation to tissue lipoprotein lipase activity in endotoxemic,
Cytokines and Lipoprotein LJpase
1871
Eschcricia coh bacteremia, and porymicrobial septic rats. / Surg
Res. 1984^37:394-401.
11. Gouni I, Oka K, Etienne J, Chan L. Endotoxin-induced hypertriglyceridemia is mediated by suppression of lipoprotein lipase at a
post-transcriptional level. J Lipid Res. 199334:139-146.
12. Beutler BA, Cerami A. Recombinant interleulrin-1 suppresses
lipoprotein lipase activity in 3T3-L1 cells. J Immunol. 1985;135:
3969-3971.
13. Beutler B, Mahoney J, Le Trang, Pekala P, Cerami A. Purification
of cachectin, a lipoprotein lipase-suppressing hormone secreted by
endotoxin-induced RAW 264.7 cells./£*/7 Afaf. 1985;161:984-995.
14. Patton JS, Shepard H, Wilking H, Lewis G, Aggarwal BB, Eessalu
TE, Gavin LA, Grunfeld C. Interferons and tumor necrosis factor
have similar catabolic effects on 3T3-L1 cells. Proc Natl Acad Sci
USA. 1986;83:8313-8317.
15. Price SR, Mizel SB, Pekala P R Regulation of lipoprotein lipase
synthesis and 3T3-L1 adipocyte metabolism by recombinant
interleukin-1. Biochim Biophys Acta. 1986;889:374-381.
16. Price SR, Ohvercrona T, Pekala PH. Regulation of lipoprotein
lipase synthesis by recombinant tumor necrosis factor: the primary
regulatory role of the hormone in 3T3-L1 adipocytes. Arch
Biochem Biophys. 1986;251:738-746.
17. Mori M, Yamaguchi K, Abe K. Purification of lipoprotein lipase inhibiting protein produced by a melanoma cell line associated
with cancer cachexia. Biochem Biophys Res Common. 1989;160:
1085-1092.
18. Greenberg AS, Nordan RP, Mclntosh J, Calvo JC, Scow RO,
Jablons D. Interleultin-6 reduces lipoprotein lipase activity in
adipose tissue of mice in vivo and in 3T3-L1 adipocytes: a possible
role for interleuMn-6 in cancer cachexia. Cancer Res. 1992;52:
4113-4116.
19. Yin T, Miyazawa K, Yang YC. Characterization of interleukin-11
receptor and protein tyrosine phosphorylation induced by
interleukin-11 in mouse 3T3-L1 cells. / Biol Chem. 1992;267:
8347-8351.
20. Semb H, Peterson J, Tavernier J, Olivercrona T. Multiple effects of
tumor necrosis factor on lipoprotein lipase in vivo. / Biol Chem.
1987^262:8390-8394.
21. Grunfeld C, Gulli R, Moser AH, Gavin LA, Feingold KR. Effect
of tumor necrosis factor administration in vivo on lipoprotein
lipase activity in various tissues of the rat. / Lipid Res. 1989;30:
579-585.
22. Rosensrreich DL, Vogel SN, Jacques AR, Wahl LM, Oppenheim
JJ. Macrophage sensitivity to endotoxin: genetic control by a single
codominant gene. J Immunol. 1978.121:1664-1670.
23. Adi S, Pollock AS, Shigenaga JK, Moser AH, Feingold KR,
Grunfeld C. Role for monolrines in the metabolic effects of endotoxin: interferon gamma restores responsiveness of C3H/HeJ mice
in vivo. J Clin Invest. 1992;89:1603-1609.
24. Dinarello CA, Cannon JG, Mier JW, Bernheim H, LoPreste G,
Lynn DL, Love RN, Webb AC, Auron PE, Reuben RC, Rich A,
Wolff SM, Putney SD. Multiple biological activities of human
recombinant interleukin-1. / Clin Invest. 1986;77:1734-1739.
25. Rehberg E, Kelder B, Hoal EG, Pestka S. Specific molecular
activities of recombinant and hybrid leukocyte interferons. J Biol
Chem. 1982^257:11497-11502.
26. Feingold KR, Soued M, Serio MK, Moser AH, Dinarello CA,
Grunfeld C. Multiple cytokines stimulate hepatic lipid synthesis in
vivo. Endocrinology. 1989;125:267-274.
27. Metcalf D, Nicola NH, Gearing DP. Effects of injected leukemia
inhibitory factor on hematopoietic and other tissues in mice.
Blood. 1990;76:50-56.
28. Burchett SK, Weaver WM, Westall JA, Larsen A, Kronheim S,
Wilson CB. Regulation of tumor necrosis factor/cachectin and IL-1
secretion in human mononuclear phagocytes. / Immunol. 1988;14O:
3473-3481.
29. Ulich TR, Guo K, Irwin B, Remick DG, Davatelis GN. Endotoxininduced cytokine gene expression in vivo, II: regulation of tumor
necrosis factor and interleukin-l//3 expression and suppression. Am
JPathol. 199O;137:1173-1185.
30. Memon RA, Grunfeld C, Moser AH, Feingold KR. Tumor necrosis
factor mediates the effects of endotoxin on cholesterol and trigryceride metabolism in mice. Endocrinology. 1993;132:2246-2253.
31. Feingold KR, Grunfeld C. Tumor necrosis factor alpha stimulates
hepatic lipogenesis in the rat in vivo. J Clin Invest. 1987;80:184-190.
32. Feingold KR, Soued M, Adi S, Staprans I, Neese R, Shigenaga J,
Doerrler W, Moser AH, Dinarello CA, Grunfeld C. The effect of
interleukin-1 on lipid metabolism in the rat: similarities and differences from tumor necrosis factor. Arteriosclerosis. 1991;11:
495-500.
1872
Arteriosclerosis and Thrombosis
Vol 14, No 11 November 1994
33. Enholm C, Aho K, Huttunen JK, Kostiainen E, Mattila K, Pikkarainen J, Cantell K. Effect of interferon on plasma lipoproteins
and on the activity of postheparin plasma lipases. Arteriosclerosis.
19822:68-73.
34. Kurzrock R, Rhode MF, Quesada JR, Gianturco SH, Bradley WA,
Sherwin SA, Gutterman JU. Recombinant gamma interferon
induces hypertriglyceridemia and inhibits post-heparin lipase
activity in cancer patients. J Exp Med. 1986;164:1093-1101.
35. Ettinger WH, Miller LA, Smith TK, Parks JS. Effect of
interleukin-1 alpha on lipoprotein lipids in cynomolgus monkeys:
comparison to tumor necrosis factor. Biochim Biopbys Acta. 1992;
1128:186-192.
36. Argiles JM, Lopez-Soriano FJ, Evans RD, Williamson DH.
Interieukin-1 and lipid metabolism in the rat. Biochem J. 1989;259:
673-678.
37. Tan MH, Sata T, Havel RJ. The significance of lipoprotein lipase
in rat skeletal muscles. / Lipid Res. 1977;18:363-370.
38. Bragdon JH, Gordon RS Jr. 1958. Tissue distribution of "C after
the intravenous injection of labeled chylomicrons and unesterified
fatty acid in the rat. J Clin Invest. 1958^7:574-578.
39. Under C, Chemick SS, Fleck TR, Scow RO. Lipoprotein lipase
and uptake of chylomicron trigh/ceride by skeletal muscle of rats.
AmJ Physiol. 1976;231:860-864.
40. Chajek-Shaul T, Friedman G, Stein O, Shiloni E, Etienne J, Stein
Y. Mechanism of the hypertriglyceridemia induced by tumor
necrosis factor administration to rats. Biochim Biopbys Acta. 1989;
1001:316-324.
41. Feingold KR, Serio MK, Adi S, Moser H, Grunfeld C. Tumor
necrosis factor stimulates hepatic lipid synthesis and secretion.
Endocrinology. 1989;124:2336-2342.
Downloaded from http://atvb.ahajournals.org/ by guest on October 2, 2016
Downloaded from http://atvb.ahajournals.org/ by guest on October 2, 2016
Effect of endotoxin and cytokines on lipoprotein lipase activity in mice.
K R Feingold, M Marshall, R Gulli, A H Moser and C Grunfeld
Arterioscler Thromb Vasc Biol. 1994;14:1866-1872
doi: 10.1161/01.ATV.14.11.1866
Arteriosclerosis, Thrombosis, and Vascular Biology is published by the American Heart Association, 7272
Greenville Avenue, Dallas, TX 75231
Copyright © 1994 American Heart Association, Inc. All rights reserved.
Print ISSN: 1079-5642. Online ISSN: 1524-4636
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://atvb.ahajournals.org/content/14/11/1866
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Arteriosclerosis, Thrombosis, and Vascular Biology can be obtained via RightsLink, a service of the
Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for
which permission is being requested is located, click Request Permissions in the middle column of the Web
page under Services. Further information about this process is available in the Permissions and Rights
Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Arteriosclerosis, Thrombosis, and Vascular Biology is
online at:
http://atvb.ahajournals.org//subscriptions/