The diagnostic value of parathyroid hormone washout after
advertisement

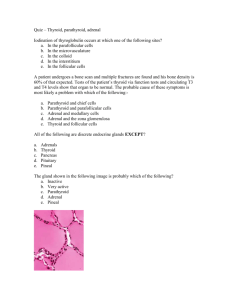
The Laryngoscope C 2013 The American Laryngological, V Rhinological and Otological Society, Inc. The Diagnostic Value of Parathyroid Hormone Washout After Fine-Needle Aspiration of Suspicious Cervical Lesions in Patients With Hyperparathyroidism Ramsy Abdelghani, MD; Salem Noureldine, MD; Ali Abbas, MD, MPH; Krzysztof Moroz, MD; Emad Kandil, MD, FACS Objectives/Hypothesis: We aimed to study the diagnostic value of parathyroid hormone (PTH) concentration in the needle washout of fine-needle aspiration (FNA) compared to cytology of suspicious lesions suggestive of culprit parathyroid glands in patients with recurrent or persistent primary hyperparathyroidism (PHPT). Study Design: Retrospective review. Methods: Patients with recurrent or persistent PHPT, who were referred to one surgeon and underwent FNA of the culprit parathyroid lesion preoperatively, were included in this study. All patients underwent comprehensive neck ultrasound, and suspicious lesions underwent ultrasound-guided FNA by the same surgeon. The aspiration cytology was read by a single dedicated cytopathologist blinded to the PTH washout results. A positive cutoff value for PTH washout concentration was defined as superior to serum PTH level obtained at the same time. The final diagnosis after reoperative surgery was confirmed by the same cytopathologist. Results: Twenty-four consecutive patients were included. The mean serum PTH and calcium were 111.5 6 106.25 pg/mL (normal: 15–65 pg/mL) and 10.8 6 0.5 mg/dL (normal: 8.6–10.2 pg/mL), respectively. Twenty-two patients (91.6%) had elevated PTH washout concentrations with a positive predictive value (PPV) of 100%. Cytopathology was successful in confirming parathyroid tissue only in seven patients (29%). An adenoma was identified in 19 patients (79.1%); however, five patients (20.8%) were found to have multiglandular disease. Conclusions: An elevated PTH washout concentration can help identify culprit parathyroid gland lesions with a high PPV in patients requiring reoperative parathyroid surgery. This diagnostic technique allows for targeted surgical approach in reoperative settings, especially in patients with negative preoperative sestamibi scans. Key Words: Hyperparathyroidism, fine-needle aspiration, parathyroid hormone, parathyroid assay, parathyroid hormone washout, recurrent hyperparathyroidism, persistent hyperparathyroidism. Level of Evidence: 4. Laryngoscope, 123:1310–1313, 2013 INTRODUCTION Primary hyperparathyroidism (PHPT) is one of the most common endocrine disorders in the United States. A single parathyroid adenoma is the cause of PHPT in 85% of cases.1 Traditionally, bilateral neck exploration with excision of hyperfunctioning parathyroid glands has been the standard in treatment of hyperparathyroid- From the Division of Endocrine and Oncologic Surgery, Department of Surgery (R.A., S.N., A.A., E.K.), and Section of Surgical Pathology and Cytopathology, Department of Pathology (K.M.), Tulane University School of Medicine, New Orleans, Louisiana, U.S.A. Editor’s Note: This Manuscript was accepted for publication October 10, 2012. Presented at the 8th International Conference on Head and Neck Cancer, Toronto, Ontario, Canada, July 21–25, 2012. The authors have no funding, financial relationships, or conflicts of interest to disclose. Send correspondence to Emad Kandil, MD, Edward G. Schlieder Chair in Surgical Oncology, Assistant Professor of Surgery, Otolaryngology and Medicine, Chief, Endocrine Surgery Section, Department of Surgery, Tulane University School of Medicine, 1430 Tulane Ave., New Orleans, LA 70124. E-mail: ekandil@tulane.edu DOI: 10.1002/lary.23863 Laryngoscope 123: May 2013 1310 ism. However, in 2% to 7% of cases, surgery is not curative at first operation, even by an experienced surgeon, and requires another surgery.2–4 Reoperations are technically difficult due to dense scarring and tissue distortion after a previous cervical operation. There is also a higher total complication rate (8.3%–13%) and risk of injury to the recurrent laryngeal nerve (0.8%–6.6%) with these reoperative surgeries.5,6 Preoperative localization of the remaining hyperfunctioning parathyroid glands in patients with previous cervical operations is helpful in minimizing surgical effort and complication rates during reoperation.7–9 Recent studies have shown multiple benefits to targeted parathyroidectomy for patients with PHPT. These include less postoperative pain, decreased need for analgesia, a lower incidence of postoperative hypocalcaemia, shorter operative times, and better cosmesis.10,11 Currently, ultrasonography and sestamibi scan are the most popular methods used to locate the culprit parathyroid gland in reoperative settings.12,13 One of the major limitations of these imaging studies is the high rate of false positives caused by other cervical pathologies and undergoing a previous surgery.14 Abdelghani et al.: PTH FNA Washout in Hyperparathyroid Patients One of the newest adjuncts to parathyroid surgery is fine-needle aspiration (FNA) with parathyroid washout. This method has been used to confirm or deny if the tissue being sampled is of parathyroid origin.15–17 There are very few studies with small numbers of patients that have shown the use of preoperative FNA to localize parathyroid adenomas and determine the eligibility of patients for minimally invasive thyroid surgery with a high sensitivity (94%), specificity (100%), and positive predictive value (PPV) (100%).16,17 We aimed to study the diagnostic value of the parathyroid hormone (PTH) concentration found in the needle washout of FNA performed preoperatively in comparison to cytological evaluation of suspicious lesions that were suggestive of enlarged parathyroid glands in patients with recurrent or persistent PHPT. TABLE I. Demographics and Biochemical Features of the Patients (n 5 24). Mean 6 SD Range Age (yr) 56 6 12 30–80 Female 87.5% 10.21 6 1.18 7.5 12.6 8.84 6 0.92 6.7 10.2 Serum calcium 6 months postoperative (mg/dL) 9.23 6 1.07 8.7 10.4 Serum albumin (g/dL) Serum PTH preoperative (pg/mL) Serum PTH postoperative (pg/mL) PTH washout (pg/mL) 3.86 6 0.57 2.6 4.5 111.5 6 106.25 31 356 45.1 6 21.3 5 74 4,393.2 6 1,074.8 743 17,413 PTH ¼ parathyroid hormone; SD ¼ standard deviation. MATERIALS AND METHODS A retrospective analysis of our endocrine surgery database was performed. Between April 2009 and September 2011, all consecutive patients with recurrent or persistent PHPT referred to a single surgeon were evaluated. The biochemical diagnosis of PHPT was arrived at through standardized criteria. Before the washout was preformed, PTH, thyroid-stimulating hormone, free thyroxin, and total calcium were evaluated in all patients. Written informed consent was obtained from all patients. In all patients, comprehensive ultrasound examination of the neck was performed by the same operating surgeon. This was compared with other imaging studies, including computed tomography scan, when available. FNA was done under ultrasound guidance on all patients with nodular lesions suspected of being enlarged parathyroid tissue. A 25-gauge needle was used for the FNA as we and others have described before.18–20 After insertion of the needle, negative pressure was applied to the suspicious lesion. Aspirated material was smeared on glass slides for cytologic examination, and then the needle was washed out with 2 mL of 0.9% normal saline. The cell block for immunohistochemical staining was performed whenever possible. The cytopathology report is usually available 1 to 2 days after the biopsy compared to several days for the PTH washout results. Nonetheless, the cytopathologist was blinded to the PTH washout results. The resulting supernatant was the source of our measured PTH concentrations. A positive cutoff value for the PTH washout was defined as being superior to the patient’s serum PTH level at the time of sampling. It was later compared to the washout results when they became available. We routinely performed intraoperative PTH level monitoring in all cases. Sensitivities of the cytology and the PTH washout were calculated. We used the Fisher exact test to compare the two sensitivities. The analysis was generated using SAS software version 9.3 for Windows (SAS Institute Inc., Cary, NC). The results were considered statistically significant if the two-tailed P value was <.05. All values are expressed as mean 6 standard deviation, range, or absolute number. Laryngoscope 123: May 2013 — Serum calcium preoperative (mg/dL) Serum calcium 1 week postoperative (mg/dL) RESULTS The study consisted of 24 consecutive patients. All patients had a history of prior neck exploration for PHPT, with persistent (n ¼ 17) or recurrent (n ¼ 7) hyperparathyroidism after the initial procedure. The average age of the patients was 55 6 12 years, with the majority of the patients being female (87.5%). The mean preoperative serum PTH level was 111.5 6 106.25 pg/mL (normal: 15–65 pg/mL). The average preoperative serum calcium level was 10.8 6 0.5 mg/dL (normal: 8.6–10.2 mg/dL). The mean PTH washout level was 4393 6 1074.8 pg/mL and ranged from 743 to 17413 pg/mL. The demographic and biochemical features of the patients are shown in Table I. The parathyroid lesions were identified by surgeonperformed ultrasound in all 24 patients. Parathyroid adenoma was found in 19 patients (79.1%), and five (20.8%) patients were found to have parathyroid hyperplasia requiring removal of additional parathyroid glands. After identifying the hyperplastic parathyroid glands, resection was performed with the goal of leaving the smallest parathyroid gland. We believe that routine intraoperative PTH monitoring is essential in identifying these patients with hyperplasia. However, the aim of the current study was to compare the diagnostic value of cytology of FNA of suspicious lesions to needle washout for PTH levels. Therefore, this did not change the accuracy of the washout in identifying the culprit lesion. Twentytwo patients had an elevated PTH washout concentration showing a PPV of 100%. Cytologic examination detected parathyroid cells in seven patients (29%). The remaining 17 negative cytological results consisted of nine (53%) follicular cell specimens and eight (47%) with a nondiagnostic or suboptimal result. We believe the reason for finding these follicular cells is due to the needle passing through the thyroid to get access to the parathyroid gland located posterior to the thyroid gland. The sensitivity of cytological examination for finding the culprit parathyroid adenoma was 29% versus 91.6% with a PPV of 100% for PTH washout (P < .001). Four (16.6%) of the cases had confirmatory immunostaining Abdelghani et al.: PTH FNA Washout in Hyperparathyroid Patients 1311 performed that revealed parathyroid cells staining with parathormone and chromogranin antibodies (Fig. 1). Preoperative sestamibi scans detected parathyroid adenoma in this select group in only nine patients (37.5%). The FNA procedure was well tolerated by all patients. There was no pain at the site of the wound, and there were no episodes of seroma or hemorrhaging. Table II shows the sensitivity of the PTH washout compared to that of cytology. The average patient follow-up time was 3.5 6 4.2 months and ranged from 9 days to 11 months. During follow-up, all patients were normocalcemic, with an average PTH value of 57 6 34.5 pg/mL and an average calcium level of 8.84 6 0.92 mg/dL, postoperatively. At the 6-month mark, the average calcium level for the patients in the study was 9.23 6 1.07 mg/dL. DISCUSSION Targeted parathyroidectomy has many advantages over other conventional methods.19 The success rate of targeted parathyroidectomy depends on accurately localizing the hyperfunctioning gland. Some popular localizing techniques currently are ultrasound, sestamibi scan, and parathyroid hormone washout. Ultrasound is easily available and performed in an office-based setting. Also, ultrasound allows for real-time visualization of the needle in relation to the lesion.21 On the other hand, ultrasound has a sensitivity of 72% to 85% in detecting parathyroid lesions22–24 and can be the only adjunct needed for a select group of patients with PHPT.25 Nonetheless, normal parathyroid glands are still rarely visible on ultrasound, depending on the skill of the person performing the ultrasound. In addition, ultrasound can show false positives secondary to thyroid pathology, blood vessels, lateral cervical lymph nodes, or the esophagus. False negatives found on ultrasound could be caused by an atypically located parathyroid gland.26 Sestamibi scan is widely used in preoperative localization of parathyroid adenomas. Sestamibi scan is especially useful in isolated and ectopic adenomas rather than in multiple adenomas.27 False negative results are due to the small size, site, and histological characteristics of such lesions.28 TABLE II. Sensitivity of PTH Washout Compared to Sensitivity of Cytology. No. of Patients True Positive False Negative Sensitivity P Value <.001* Cytology 24 7 17 29% PTH washout 24 22 2 91.6% *P value was calculated from Fisher exact tests. PTH ¼ parathyroid hormone. Our data show 29% of FNA biopsies had cytologic specimens indicative of parathyroid tissue that were later confirmed by surgical pathology. The results of our cohort compel us to agree with the opinion that the low sensitivity of cytological diagnosis decreases the reliability of this method for preoperative confirmation.29,30 PTH washout is an accurate way to localize culprit lesions in patients with findings indicating parathyroid lesions on neck ultrasound. Frasoldati and colleagues showed that a PTH washout result of more than 101 pg/mL had a 100% sensitivity and specificity for verification of parathyroid tissue.31 Marcocci and colleagues regarded a PTH washout value of >50 pg/mL as positive for sampling in parathyroid tissue,32 whereas Maser and colleagues reported that a PTH washout value of >1,000 pg/mL indicates sampling of parathyroid tissue.33 Sacks and colleagues reported 45 patients with PHPT who underwent FNA of suspected parathyroid adenomas. Thirty-seven of the 45 patients had elevated PTH levels, with a specificity of 100% at the time of operation.34 These results are consistent with our own. However, it is important to note that the PTH values from different assays are not interchangeable. Our data show that a PTH washout value above the serum PTH level is a valid indication that hyperfunctioning parathyroid tissue was sampled. A PTH washout value higher than the serum PTH should be considered diagnostic in localizing the parathyroid due to the hormone dilution in the FNA. One must consider that the aspirate is rinsed and diluted before being measured. Given this, the measured PTH level of the aspirate most likely corresponds to a much higher concentration in the original sample.32 Because a cutoff is needed, we used any value higher than the serum PTH as our cutoff point, signifying the sample was parathyroid tissue. Our data concluded that a parathyroid FNA value over the patient’s serum PTH level indicated a hyperfunctioning parathyroid was sampled. Further studies with larger numbers at different institutions are needed to determine the PTH FNA cutoff value required to confirm a hyperfunctioning parathyroid lesion. CONCLUSION Fig. 1. Parathyroid cells stained with parathormone and chromogranin antibodies. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.] Laryngoscope 123: May 2013 1312 Our study confirms the high reliability of parathyroid FNA washout in locating hyperfunctioning parathyroid tissue when the results are of a greater value than the serum PTH level. Considering its low sensitivity, cytomorphology alone is not sufficient to confirm a parathyroid lesion. PTH washouts can contribute significantly in establishing the parathyroid nature of cervical lesions. With its high specificity, an FNA with washout should be considered to confirm abnormal Abdelghani et al.: PTH FNA Washout in Hyperparathyroid Patients ultrasound findings in patients who underwent an unsuccessful parathyroidectomy. 17. 18. BIBLIOGRAPHY 1. Wang CA. Surgical management of primary hyperparathyroidism. Curr Probl Surg 1985;22:1–50. 2. Ruda JM, Hollenbeak CS, Stack BC Jr. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg 2005;132:359–372. 3. Witteveen JE, Kievit J, Morreau H, Romijn JA, Hamdy NA. No recurrence of sporadic primary hyperparathyroidism when cure is established 6 months after parathyroidectomy. Eur J Endocrinol 2010;162:399–406. 4. Westerdahl J, Bergenfelz A. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: five-year follow-up of a randomized controlled trial. Ann Surg 2007;246:976–980; discussion 980–981. 5. Thompson GB, Grant CS, Perrier ND, et al. Reoperative parathyroid surgery in the era of sestamibi scanning and intraoperative parathyroid hormone monitoring. Arch Surg 1999;134:699–704; discussion 704–705. 6. Carty SE, Norton JA. Management of patients with persistent or recurrent primary hyperparathyroidism. World J Surg 1991;15:716–723. 7. Chen H, Mack E, Starling JR. A comprehensive evaluation of perioperative adjuncts during minimally invasive parathyroidectomy: which is most reliable? Ann Surg 2005;242:375–380; discussion 380–383. 8. Jones JJ, Brunaud L, Dowd CF, Duh QY, Morita E, Clark OH. Accuracy of selective venous sampling for intact parathyroid hormone in difficult patients with recurrent or persistent hyperparathyroidism. Surgery 2002;132:944–950; discussion 950–951. 9. Seehofer D, Steinmuller T, Rayes N, et al. Parathyroid hormone venous sampling before reoperative surgery in renal hyperparathyroidism: comparison with noninvasive localization procedures and review of the literature. Arch Surg 2004;139:1331–1338. 10. Bergenfelz A, Lindblom P, Tibblin S, Westerdahl J. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: a prospective randomized controlled trial. Ann Surg 2002;236:543–551. 11. Slepavicius A, Beisa V, Janusonis V, Strupas K. Focused versus conventional parathyroidectomy for primary hyperparathyroidism: a prospective, randomized, blinded trial. Langenbecks Arch Surg 2008;393: 659–666. 12. Bhansali A, Masoodi SR, Bhadada S, Mittal BR, Behra A, Singh P. Ultrasonography in detection of single and multiple abnormal parathyroid glands in primary hyperparathyroidism: comparison with radionuclide scintigraphy and surgery. Clin Endocrinol (Oxf) 2006;65:340–345. 13. Grosso I, Sargiotto A, D’Amelio P, et al. Preoperative localization of parathyroid adenoma with sonography and 99mTc-sestamibi scintigraphy in primary hyperparathyroidism. J Clin Ultrasound 2007;35:186–190. 14. Masatsugu T, Yamashita H, Noguchi S, et al. Significant clinical differences in primary hyperparathyroidism between patients with and those without concomitant thyroid disease. Surg Today 2005;35:351–356. 15. Perrier ND, Ituarte P, Kikuchi S, et al. Intraoperative parathyroid aspiration and parathyroid hormone assay as an alternative to frozen section for tissue identification. World J Surg 2000;24:1319–1322. 16. Stephen AE, Milas M, Garner CN, Wagner KE, Siperstein AE. Use of surgeon-performed office ultrasound and parathyroid fine needle aspiration Laryngoscope 123: May 2013 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. for complex parathyroid localization. Surgery 2005;138:1143–1150; discussion 1150–1151. Doppman JL, Krudy AG, Marx SJ, et al. Aspiration of enlarged parathyroid glands for parathyroid hormone assay. Radiology 1983;148:31–35. Langer JE, Baloch ZW, McGrath C, Loevner LA, Mandel SJ. Thyroid nodule fine-needle aspiration. Semin Ultrasound CT MR 2012;33:158–165. Winters R, Friedlander P, Noureldine S, Ekaidi I, Moroz K, Kandil E. Preoperative parathyroid needle localization: a minimally invasive novel technique in reoperative settings. Minim Invasive Surg 2011;2011:487076. Kandil E, Faruqui S, Alharash J, et al. A targeted parathyroidectomy using guide wire technique in a pregnant patient with primary hyperparathyroidism. Int J Otolaryngol 2009;2009:361427. Tikkakoski T, Stenfors LE, Typpo T, Lohela P, Apaja-Sarkkinen M. Parathyroid adenomas: pre-operative localization with ultrasound combined with fine-needle biopsy. J Laryngol Otol 1993;107:543–545. Felger EA, Kandil E. Primary hyperparathyroidism. Otolaryngol Clin North Am 2010;43:417–432, x. Johnson NA, Tublin ME, Ogilvie JB. Parathyroid imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR Am J Roentgenol 2007;188:1706–1715. Meilstrup JW. Ultrasound examination of the parathyroid glands. Otolaryngol Clin North Am 2004;37:763–778, ix. Levy JM, Kandil E, Yau LC, Cuda JD, Sheth SN, Tufano RP. Can ultrasound be used as the primary screening modality for the localization of parathyroid disease prior to surgery for primary hyperparathyroidism? A review of 440 cases. ORL J Otorhinolaryngol Relat Spec 2011;73: 116–120. Solbiati L, Montali G, Croce F, Bellotti E, Giangrande A, Ravetto C. Parathyroid tumors detected by fine-needle aspiration biopsy under ultrasonic guidance. Radiology 1983;148:793–797. Allendorf J, Kim L, Chabot J, DiGiorgi M, Spanknebel K, LoGerfo P. The impact of sestamibi scanning on the outcome of parathyroid surgery. J Clin Endocrinol Metab 2003;88:3015–3018. Mihai R, Gleeson F, Buley ID, Roskell DE, Sadler GP. Negative imaging studies for primary hyperparathyroidism are unavoidable: correlation of sestamibi and high-resolution ultrasound scanning with histological analysis in 150 patients. World J Surg 2006;30:697–704. Bondeson L, Bondeson AG, Nissborg A, Thompson NW. Cytopathological variables in parathyroid lesions: a study based on 1,600 cases of hyperparathyroidism. Diagn Cytopathol 1997;16:476–482. Tseleni-Balafouta S, Gakiopoulou H, Kavantzas N, Agrogiannis G, Givalos N, Patsouris E. Parathyroid proliferations: a source of diagnostic pitfalls in FNA of thyroid. Cancer 2007;111:130–136. Frasoldati A, Pesenti M, Toschi E, Azzarito C, Zini M, Valcavi R. Detection and diagnosis of parathyroid incidentalomas during thyroid sonography. J Clin Ultrasound 1999;27:492–498. Marcocci C, Mazzeo S, Bruno-Bossio G, et al. Preoperative localization of suspicious parathyroid adenomas by assay of parathyroid hormone in needle aspirates. Eur J Endocrinol 1998;139:72–77. Maser C, Donovan P, Santos F, et al. Sonographically guided fine needle aspiration with rapid parathyroid hormone assay. Ann Surg Oncol 2006; 13:1690–1695. Sacks BA, Pallotta JA, Cole A, Hurwitz J. Diagnosis of parathyroid adenomas: efficacy of measuring parathormone levels in needle aspirates of cervical masses. AJR Am J Roentgenol 1994;163:1223–1226. Abdelghani et al.: PTH FNA Washout in Hyperparathyroid Patients 1313