Estrogen Receptor (ER ) - Clinical Cancer Research
advertisement

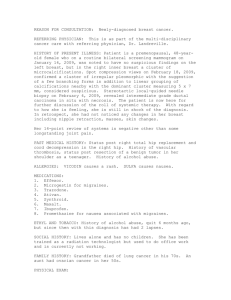
Vol. 10, 5769 –5776, September 1, 2004 Clinical Cancer Research 5769 Estrogen Receptor  (ER) Level but Not Its ERcx Variant Helps to Predict Tamoxifen Resistance in Breast Cancer Endocrinologie moléculaire et cellulaire des cancers (U 540), Institut National de la Santé et de la Recherche Médicale (INSERM), Montpellier, France; Departments of 2Pathology and 3Biostatistics, Cancer Center Val d’Aurelle, Montpellier, France; and 4Department of Medical Nutrition and Biosciences, Karolinska Institute, Novum, Huddinge, Sweden total population was positively correlated with ERcx (r ⴝ 0.63, P < 0.001), and was independent of the other parameters. In a multivariate analysis, ER expression was the most important variable (P ⴝ 0.001), followed by SBR grade (IⴙII versus III; P ⴝ 0.008), and MIB-1 (P ⴝ 0.016). To conclude, tamoxifen resistance is associated with classical variables of aggressive tumors (high SBR grade, proliferation index, and tumor size) but not with node invasiveness. Low ER level is an additional independent marker, better than ER␣ level, to predict tamoxifen resistance. ABSTRACT INTRODUCTION The antiestrogen tamoxifen, a major endocrine therapy of estrogen receptor (ER)-positive breast cancer, is nevertheless inefficient in 30 to 40% of cases for unknown reasons. We retrospectively studied 50 ER-positive primary breast carcinomas. All of the patients had received tamoxifen as the only adjuvant therapy. They were divided into two groups depending on whether they relapsed within 5 years (16 tamoxifen-resistant cases) or did not relapse within 5 years (34 tamoxifen-sensitive cases). The expression of total ER protein, and of ERcx protein, was estimated anonymously in formalin-fixed, paraffin-embedded tumor sections, by using specific antibodies and quantifiying nuclear immunostaining with a computer image analyzer. All of the tumors were found to be HER-2/neu-negative by immunohistochemistry. Univariate analysis showed that Scarff-Bloom-Richardsson grade modified by Elston (SBR grade; P < 0.001), tumor size (P ⴝ 0.042), and MIB-1 proliferation index (P ⴝ 0.02) were significantly higher in tamoxifen-resistant tumors. A low level of total ER, whether in percentage of positive cells or in quantitative immunocytochemical (QIC) score, was also associated with tamoxifen resistance (P ⴝ 0.004). ERcx expression and lymph node status were similar between the two groups. The expression of ER in the Tamoxifen is one of the first-line adjuvant therapy options in women with ER-positive breast cancer. However, in 30 to 40% of cases, these tumors relapse within 5 years of tamoxifen treatment, which requires the cessation of the regimen and the initiation of a second-line therapy. The mechanism of tamoxifen resistance in ER-positive breast cancer is unknown despite extensive studies (1–3). Tamoxifen either is inactive and unable to block the mitogenic effect of estrogen and growth factors or behaves as an agonist that stimulates the growth of cancer cells and induces growth-associated genes, as shown in different cell lines selected for their ability to grow with this antiestrogen (4, 5). This estrogenic effect of tamoxifen can be blocked by pure antiestrogens (6). It has been established, however, both in cell lines (7, 8) and in patients (9), that tamoxifen is mostly active in ERpositive breast cancer, and that the assay of ER in cytosol or in tumor section is the first predictive marker used in practice to guide the clinicians in defining systemic therapy (10). The recent discovery of a second ER, named ER (11), and of several of its variants, raised the question of the relative value of ER␣ and ER in predicting tamoxifen resistance or sensitivity in breast cancer patients. ER binds antiestrogens and their hydroxylated metabolites (12) with a higher affinity than does ER␣ (13). Both the full-length ER (ER1) and its COOHterminally truncated splice variant (ERcx or ER2), which is unable to bind tamoxifen, have been found in breast cancer (14, 15). They are able to act as dominant negative of ER␣ after heterodimerization (16), but their significance in antiestrogen resistance is controversial. It has been proposed that the action of tamoxifen on ER stimulates tumor growth via AP-1 interactions (17). Conversely, ER could inhibit the agonist activity of tamoxifen for instance on AF-1, the activating domain of transcription of ER␣ (18, 19). Finally, ER might have no value in predicting tamoxifen efficacy or resistance. To discriminate among these possibilities, we have quantified anonymously by immunohistochemistry the expression of total ER protein and its variant ERcx in 50 archival ERpositive breast carcinomas, which had been treated by tamoxifen as the only adjuvant therapy, and we have compared their value Majida Esslimani-Sahla,1,2 Joelle Simony-Lafontaine,2 Andrew Kramar,3 Roselyne Lavaill,2 Caroline Mollevi,3 Margaret Warner,4 Jan-Åke Gustafsson,4 and Henri Rochefort1 1 Received 2/27/04; revised 4/29/04; accepted 5/12/04. Grant support: Supported by INSERM, the Ligue Nationale Contre le cancer, Comité Départemental de l’Herault (to M. Esslimani-Sahla) and by grants from The Swedish Cancer Society and KaroBio AB (to J-A. Gustafsson). The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. Requests for reprints: Henri Rochefort, Endocrinologie moléculaire et cellulaire des cancers (U540) INSERM, 60 rue de Navacelles, 34090 Montpellier, France. Phone: 33-467043760; Fax: 33-467540598; Email: henri.rochefort@montp.inserm.fr. ©2004 American Association for Cancer Research. 5770 ER in Breast Cancer and Tamoxifen Resistance in tamoxifen-resistant and tamoxifen-sensitive tumors, defined according to the presence or absence of relapse within 5 years of standard tamoxifen therapy (20). MATERIALS AND METHODS Patient Selection. The files of 850 patients with primary breast carcinomas treated during 1992, at the Val d’Aurelle Cancer Center in Montpellier, France, were considered for this study. Patients were selected according to the following criteria: (a) absence of neoadjuvant therapy; (b) tumor diameter greater than 1 cm allowing biochemical assay; (c) ER-positive tumor according to cytosolic radioligand assay (ⱖ10 fmol/mg protein); (d) adjuvant therapy exclusively by tamoxifen for 5 years (20 mg/d); (e) availability of paraffin blocks for analysis; and (f) complete clinical data and sufficient follow-up. The tamoxifenresistant patients were defined as those patients who recurred while on adjuvant tamoxifen therapy (up to 5 years). The tamoxifen-sensitive patients were defined as those patients who had not recurred while on tamoxifen therapy during 5 years. Only 50 cases of 850 could be included in this study with 16 tamoxifen-resistant cases and 34 tamoxifen-sensitive cases. Histopathologic grading of tumor was obtained according to ScarffBloom-Richardsson (SBR) modified by Elston (21, 22). Nodal status was obtained by histologic analysis of at least eight axillary nodes. Menopausal status was determined by clinical and hormonal analysis. Immunohistochemical Assay. All of the tumor samples were fixed in formalin-alcohol solution and embedded in paraffin. The archived breast cancer specimens were studied by immunohistochemistry. The pathologist (ME-S) was blinded to the patient characteristics. Immunostaining was performed with ER antibodies obtained in Dr. J-Å. Gustafsson’s laboratory (Department of Medical Nutrition and Biosciences, Karolinska Institute, Novum, Huddinge, Sweden). The chicken polyclonal ER 503 IgY antibodies recognize total ER proteins (both full-length ER and its splice variants) and have been previously validated for immunohistochemistry (23, 24), including validation by protein extinction with authentic ER protein (23). The ERcx polyclonal antibodies were raised in sheep against the 14-amino-acid peptides of the COOH-terminal region: MKMETLLPEATMEQ. Analysis was also performed by ER␣ (clone 6F11, Novocastra, United Kingdom), progesterone receptor [PgR (clone PgR 636, Dako)], Ki67 (clone MIB-1, Dako), and two HER2/neu (c-ErbB2) markers [polyclonal A0485 (Dako, Denmark) and monoclonal CB11 (Novocastra)]. Adjacent sections of 5 m each were deparaffinized in xylene and rehydrated with graded EtOH concentrations. Before staining, a heat epitope retrieval procedure was performed. Sections were pretreated by pressure cooking for 15 minutes in EDTA buffer (pH 7) for ER and ERcx, and by waterbath for 40 minutes at 95° for the other markers, with citrate buffer (pH 6) for ER␣, PgR, and HER2/neu, and Tris-EDTA buffer (pH 8) for MIB-1. For ER␣ (1:50 dilution), PgR (1:100 dilution), MIB-1 (1:100 dilution), and c-ErbB2 (1:500 dilution for polyclonal antibody and 1:800 dilution for CB11 antibody), immunohistochemical labeling with the “Dako LSABR 2 System-HRP” was performed at room temperature Table 1 Comparison of clinical and histopathologic characteristics between tamoxifen-resistant and tamoxifen-sensitive patients Resistant cases Sensitive cases P value Patients Number 16 Age, median (range), y 68 (43–88) Menopausal status Pre 3 (18.8%) Post 13 (81.3%) Therapy Surgery Radical 12 (75%) Conservative 4 (25%) Radiotherapy 9 (56.3%) Tumor Histologic type IDC 14 (87.5%) ILC 2 (12.5%) SBR grading* I 0 (0%) II 3 (18.8%) III 13 (81.3%) Tumor size T1 8 (50%) T2 5 (31.3%) T3–T4 3 (18.8%) Cytosolic receptor levels, fmol/mg ER, mean 116.5 PgR, mean 107.5 Nodal status† pN0 7 (43.8%) pN1 9 (56.3%) 34 63 (36–80) ⬎0.05 4 (11.8%) 30 (88.2%) ⬎0.05 17 (50%) 17 (50%) 28 (82.2%) ⬎0.05 31 (93.9%) 2 (6.1%) ⬎0.05 0.082 0.001 11 (32.4%) 16 (47.1%) 7 (20.6%) 0.042 17 (50%) 17 (50%) 0 (%) 122.1 149.5 21 (61.8%) 13 (38.2%) ⬎0.05 ⬎0.05 ⬎0.05 NOTE. Patient and tumor characteristics are presented as percentages for categorical variables and as means and medians (range) for continuous variables. P value was obtained by Fisher’s exact test for categorical variables and by two-sample Wilcoxon test for all continuous variables; P ⬍ 0.05 was considered statistically significant (bold type). Abbreviations: IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma. * Histopathologic grading of Scarff-Bloom-Richardsson (SBR) modified by Elston. † Histopathologic nodal status: pN0, absence of nodal metastasis, pN1, metastasis of one or more nodes. with the automated Dako Autostainer (code no. K0675); and 3⬘,3⬘-diaminobenzidine tetrahydrochloride (DAB) was used as a chromogen. The immunohistochemical procedure for total ER marker was described previously (23). A similar protocol was performed for polyclonal sheep ERcx antibody (1:300 dilution), except for the use of an appropriate secondary biotinylated antisheep antibody (Santa Cruz Biotechnology, Santa Cruz, CA). Negative controls were performed by the replacement of primary antibody by IgY nonspecific serum (Nordic, Netherlands) for ER, mouse IgG1 nonspecific serum (X0931, Dako) for ER␣, PgR, and MIB-1 markers, with similar protein concentrations. Positive external controls were used in each experiment, sections of OVCAR cells, pellet-embedded in paraffin, were used for ER, and a positive breast cancer sample was used for each other marker. Adjacent normal breast tissue was also used as an internal control for ER␣, PgR, MIB-1, and ER. ERcx specificity of immunostaining was established by preincubat- Clinical Cancer Research 5771 Fig. 1 A, immunohistochemistry in adjacent serial sections of two breast invasive ductal carcinomas: the first, a to c, tamoxifen-sensitive case. A-a, a strong nuclear expression of ER total protein; A-b, nonspecific IgY serum (Nordic); A-c, a low proliferation index (Ki-67, clone MIB-1, Dako); the second, d to e, tamoxifen-resistant case, relapsing after 28 months. A-d, low nuclear ER expression; A-e, high expression of ER␣ (clone 6F11, Novocastra); A-f, high MIB-1 proliferation index. B, ERcx-staining specificity in adjacent serial sections of two invasive breast carcinomas, different from those of A. B-a and B-c, ⴱ, nuclear ERcx immunostaining in invasive cancer cells; B-c, DCIS, nuclear ERcx immunostaining in adjacent ductal carcinoma in situ. B-a, blue arrow, nuclear ERcx immunostaining in stromal cells; red arrows, nuclear ERcx immunostaining in inflammatory cells. B-b and d, staining specificity is evidenced by extinction experiment after adding a 10-fold excess of ERcx protein (b) and by using preimmune serum (d). ing the sheep polyclonal ERcx antibody with a 10-fold excess of ERcx peptide. It was also shown with pre-adsorbed ERcx antiserum (1:2100 dilution), and with preimmune sheep serum for ERcx (1:5000 dilution). In each ERcx experiment, pre-immune sheep serum was used, in addition to a positive external control (breast cancer tissue overexpressing ERcx). Archival material of mammary tumor recurrence and/or metastasis was obtained for six resistant patients and was analyzed with the same markers. Quantitative Method. Quantification was performed with a computerized image analyzer (Samba 2005 TITN, Alcatel, Grenoble, France) as described previously (23). Ten to twelve microscopic fields (G200) of invasive tumor, representative of all surface cut, were analyzed for ER␣, -, and -cx and for PgR. The highly stained fields were chosen for MIB-1 proliferation marker assessment. Results were expressed as the percentage of nuclear-stained epithelial cells, or as a quantitative immunocytochemical (QIC) score [(percentage of surface 5772 ER in Breast Cancer and Tamoxifen Resistance Table 2 Comparison of immunohistochemical variables in invasive tumors between tamoxifen-resistant and -sensitive patients ER % stained nuclei median (range)* ⱖ70% expression QIC score,† median (range) ERcx ‡ % stained nuclei median (range)* ⬎30% expression QIC score,† median (range) ER ⫺ ERcx‡ (% stained nuclei), median (range)* ER␣ (% stained nuclei) Median (range)* ⬎50% expression ER␣/ER ratio, % stained nuclei, median (range)* PgR, % stained nuclei Median (range)* ⬎20% expression MIB-1, % stained nuclei Median (range)* Proliferation index ⬍10% (low) 10–19% (moderate) ⱖ20% (high) Resistant cases Sensitive cases P value 41.8 (0–86.8) 4 (25%) 12.5 (0–39) 76.4 (7.5–98.6) 21 (62%) 29.5 (1.8–93) 0.004 0.015 0.006 30.4 (1.8–58.2) 7 (54%) 2.9 (0.2–32) 12.4 (3.3–47.3) 32.7 (6.7–67.7) 17 (52%) 4.3 (0.9–16) 33.7 (0.8–75.3) ⬎0.05 ⬎0.05 ⬎0.05 0.015 31.2 (0.4–87.2) 6 (38%) 1.01 (0–4.5) 54.5 (0–91.8) 18 (53%) 0.63 (0–12.2) ⬎0.05 ⬎0.05 ⬎0.05 13 (0–86.1) 7 (44%) 24.5 (0–79.1) 19 (56%) ⬎0.05 ⬎0.05 21.9 (0.3–45.7) 6 (37.5%) 1 (6.3%) 9 (56.3%) 7 (0–31.2) 23 (67.6%) 6 (17.6%) 5 (14.7%) 0.020 0.01 NOTE. P value was obtained by Fisher’s exact test for categorical variables and two-sample Wilcoxon test for all continuous variables; P ⬍ 0.05 was considered statistically significant (bold type). All cases were ER⫹ by radioligand and HER2neu⫺ * Percentage stained nuclei quantified by computer image analyzer. † QIC score obtained by computer image analyzer by assessment of the percentage of positive nuclei and intensity of staining. ‡ In three resistant cases and one sensitive case, tumor materials were exhausted and ERcx analysis was not realized. stained in epithelial cells) ⫻ (mean staining intensity) ⫻ 10] expressed in arbitrary units (AU). The percentage of nuclear staining of negative control was usually nil and, when weak, was subtracted. A semiquantitative method was performed for c-erbB-2 membrane staining, according to the Dako Hercept Test scoring. Statistical Methods. All of the parameters were analyzed by continuous values and by expression status. Receptor status were defined taking as cutoff points the median values observed in the 50 ER-positive cases (70% for ER, 30% for ERcx, 50% for ER␣, and 20% for PgR). Because the sensitivity of the assay may vary according to the receptors, these values may not indicate their relative level in the tumor. Univariate analysis comparing resistant and sensitive cases were performed by Fisher’s exact test for categorical variables and by the two-sample Wilcoxon test for all continuous parameters. The Wilcoxon test and the Spearman correlation coefficient were used to evaluate the relationship between ER and ERcx expression with the other parameters. P values ⬍ 0.05 were considered statistically significant. The multivariate analysis was carried out in two steps by first introducing all of the immunohistochemical variables in a stepwise backward logistic regression model (25) Significant clinical variables were then introduced to investigate the relationships with the immunohistochemical variables. Statistical significance was measured by the likelihood ratio test. Odds ratios were used to summarize the effects. Statistical analyses were performed with Stata software (StataCorp, College Station, TX; ref. 26). RESULTS Clinical and Histopathologic Characteristics of Tamoxifen-resistant and Tamoxifen-sensitive Patients. Two groups of patients were compared according to the occurrence of relapse within 5 years of tamoxifen therapy. The 16 tamoxifen resistant cases relapsed within a median of 3 years from surgery (range 14 –56 months). Among the 34 tamoxifen sensitive cases, 4 patients relapsed after 80 months, and the other 30 patients were alive and disease free at a median follow up of 9.4 years (range 60 –128 months). Most clinical and pathologic characteristics were not different in the resistant and sensitive groups (Table 1). The only differences were SBR grading and tumor size, which were more elevated in resistant cases. Immunohistochemical Staining of ER and ERcx in Resistant and Sensitive Tumors. As shown in Fig. 1A-a, ER immunoreactivity was detected in the nuclei of invasive breast cancer cells, where brown staining was totally abolished with an excess of antigen (23). Since the cytoplasmic staining was not fully abolished, only the nuclear staining was quantified. The absence of cross-reactivity between ER and ER␣ antibodies was also confirmed as shown in Fig. 1A-d and -e. Nuclear intensity and staining distribution of invasive tumors were variable according to the patient. Staining distribution was either diffuse in all of the tumor, or was focal and generally localized in tumoral islets at the periphery of the tumor. Fig. 1A shows a typical example of a tamoxifen-sensitive (Fig. 1A- a, -b, and -c) and tamoxifen-resistant (Fig. 1A-d, -e, and -f) invasive ductal breast carcinoma, with similar SBR grade (II) and size Clinical Cancer Research 5773 (pT2) and without nodal invasiveness. In the tamoxifen-sensitive case, there was a strong expression of ER (Fig. 1A-a), with a low MIB-1 proliferation rate (Fig. 1A-c). The tamoxifenresistant case showed a low ER expression (Fig. 1A-d) contrasting with a high ER␣ level (Fig. 1A-e), and high MIB-1 staining (Fig. 1A-f). ER nuclear staining was also detected in epithelial and myoepithelial cells of normal mammary glands, in stromal and inflammatory cells. ERcx immunostaining is shown in Fig. 1B. The nuclear staining mostly observed in cancer cells (Fig. 1B-a and -c) contrasted with a weak cytoplasmic staining. Nuclear staining was also observed in some stromal endothelial cells and inflammatory cells such as lymphocytes and macrophages (Fig. 1B-a). The specificity of the ERcx immunostaining was evidenced by three criteria: (a) nuclear signal was removed by adding a 10-fold excess of the antigen (Fig. 1B-b), (b) nuclear signal was removed by using an ERcx pre-adsorbed antiserum (not shown), and (c) nuclear signal was removed by using the preimmune serum (Fig. 1B-d). ERcx reactivity varied according to patients (Table 2 and Fig. 3). As shown in Table 2, total ER level was significantly higher in sensitive tumors than in resistant cases, when comparing the percentage of stained nuclei or QIC score. The same difference was found with continuous values (Fig. 2A) or status expression taking the median as a cutoff level of 70% of stained nuclei. Unlike total ER, ERcx level (either with percentage or Fig. 2 ER, ER␣ protein levels, and MIB-1 proliferation index were analyzed by immunohistochemical staining and were quantified by computer image analyzer in percentage of positive cells. Significant differences between tamoxifen-resistant (R) and tamoxifen-sensitive (S) tumors were evaluated with the two-sample Wilcoxon test. Total ER protein values were significantly higher in sensitive cases. The difference in ER␣ values between the two groups was not significant. MIB-1 was significantly higher in tamoxifen-resistant tumors. Bars, median values. Fig. 3 Total ER protein and ERcx protein levels were positively correlated (Spearman correlation, r, ⫽ 0.63; P ⬍ 0.001) in adjacent sections of the same breast cancer. The percentage of stained nuclei for ERcx was always inferior to that of total ER protein quantified in adjacent sections of the same tumors. with QIC score) did not differ between resistant and sensitive tumors. The difference between total ER and ERcx was significantly higher in sensitive tumors. The difference in ER␣ levels between the two groups was not significant (Fig. 2). However the ER␣-positive tumors (ⱖ50% of stained nuclei) were mostly seen in tamoxifen-sensitive patients. The ER␣/ER ratio, estimated in adjacent sections of each tumor, and PgR expression were not different between the two groups. The proliferation rate assessed by MIB-1 was greater in the resistant group (P ⫽ 0.01), with 63% of resistant cases expressing more than 10% of stained nuclei as compared with 32% of sensitive cases. We found no HER2/neu (c-erbB2) overexpression in any of the 50 tumors, which is consistent for ER-positive tumors. We found no significant variation in ER, ER␣, PgR, and MIB-1 levels between the primary tumor and recurrence or metastasis for the same patient, but the number (six cases) was too small to reach a conclusion. ER Correlations With the Other Variables. ER expression was independent of all parameters, including PgR (Table 3). It was correlated only with ERcx expression (Spearman correlation coefficient, r, ⫽ 0.63, P ⬍ 0.001). The percentage of ER-positive cells was always superior to the percentage of ERcx-positive cells (Fig. 3). Interestingly, MIB-1 was inversely correlated with ER␣ level (P ⫽ 0.003) but not with ER levels. A positive correlation was observed, however, between ER expression and MIB-1 proliferation index in the tamoxifen-resistant tumors (r ⫽ 0.51, P ⫽ 0.04), but no relationship was found in the tamoxifen-sensitive group. All 14 patients with a low MIB-1 proliferation index (⬍10%) and a high ER status 5774 ER in Breast Cancer and Tamoxifen Resistance (ⱖ70%) were tamoxifen sensitive (Fig. 4). ERcx expression was associated with total ER expression but was independent of all other variables. Multivariate Analysis and Predictive Variables of Resistance to Tamoxifen. In the univariate analysis (Tables 1 and 2), SBR grade was found to be the most discriminant variable between the two groups of resistant and sensitive cases (P ⫽ 0.001), followed by ER expression (P ⫽ 0.004), MIB-1 proliferation index (P ⫽ 0.02), and tumor size (P ⫽ 0.042). ER␣ expression and nodal status were not significant. In the multivariate analysis, SBR grade (I⫹II versus III), MIB-1 proliferation index, and ER␣ and ER expression were introduced in a multivariate logistic regression model (25) on a continuous scale (Table 4). Tumor size had no predictive value and was not Table 3 Distribution of ER status as a function of clinicopathologic and immunohistochemical variables Variables No. of patients Age, median (range), y Menopausal status Pre Post Therapy Surgery Radical Conservative Radiotherapy Histologic type IDC ILC SBR grading I II III Tumor size T1 T2 T3–T4 Nodal status pN0 pN1 ERcx, % Median (range) ⬎30% expression ER␣, % Median (range) ⬎50% expression PgR, % Median (range) ⬎20% expression ER, fmol/mg Median (range) ⬎100 PgR, fmol/mg Median (range) ⬎20 MIB-1, % Median (range) ⱖ10% Negative ER expression (⬍70%) Positive ER expression (ⱖ70%) P value 25 64 (43–79) 25 63 (36–88) 4 21 3 22 ⬎0.05† 13 12 18 16 9 19 ⬎0.05† 22 3 23 1 ⬎0.05† 4 10 11 7 9 9 ⬎0.05† 14 9 2 11 13 1 ⬎0.05† 15 10 13 12 ⬎0.05† 17.2 (1.8–58.2) 8 (35%) 38.0 (10.9–67.7) 16 (70%) 44.3 (0.4–91.8) 11 (44%) 53.0 (0–84.7) 13 (52%) ⬎0.05* ⬎0.05† 14.3 (0–86) 10 (40%) 25.6 (0–72) 16 (64%) ⬎0.05* ⬎0.05† 79 (28–441) 10 (43%) 111 (37–375) 12 (52%) ⬎0.05* ⬎0.05† 52 (0–442) 10 (40%) 83 (0–576) 16 (64%) ⬎0.05* ⬎0.05† 6.2 (0–35.9) 10 (40%) 9.5 (0–45.7) 11 (44%) ⬎0.05 ⬎0.05† ⬎0.05* ⬎0.05† 0.002* 0.038† Note. P ⬍ 0.05 was considered statistically significant (bold type). * Wilcoxon test † Fisher’s exact test. Fig. 4 A slight positive correlation between total ER protein and MIB-1 proliferation index in adjacent sections of the same tumors was found in resistant (R) tumors (r ⫽ 0.51; P ⫽ 0.04), but not in the sensitive (S) group nor in the overall population. The group with high ER protein levels (ⱖ70% of stained nuclei) and low MIB-1 proliferation rate (⬍10%) contains almost exclusively tamoxifen-sensitive tumors; P ⫽ 0.001, according to Fisher’s exact test. included in the model. ER expression was the most important independent variable (P ⫽ 0.001), followed by SBR grade (P ⫽ 0.008) and MIB-1 proliferation index (P ⫽ 0.016), whereas ER␣ expression was at the limit of statistical significance (P ⫽ 0.060). According to this model, 43 (86%) of the 50 patients were correctly classified. The sensitivity and specificity were 81 and 88%, respectively. The positive and negative predictive values were 76 and 91%, respectively, assuming a prevalence rate of resistance equal to 32% (16 of 50). On the basis of expression status, the logistic regression model identified SBR grade (P ⫽ 0.003), followed by ER (P ⫽ 0.013) and MIB-1 (P ⫽ 0.032). ER␣ level was not significant. In a regrouping of the four variables, grade III tumors with elevated MIB-1 proliferation index and low ER level were at a greater risk for tamoxifen-resistance. DISCUSSION In addition to classical prognostic variables associated with aggressive tumors, such as histologic SBR grade and tumor size, the level of ER determined by immunohistochemistry in a population of ER-positive tumors treated by tamoxifen was found to be the major variable in predicting tamoxifen sensitivity. ER␣ had a lower value, and ERcx had no value. This should clarify the significance of the cytosolic radioligand assay of ER (10) on which most of the clinical studies allowing introduction of this marker to predict breast cancer response to Clinical Cancer Research 5775 Table 4 Multivariate analysis of predictive factors of tamoxifen resistance Variables Odds ratio ER expression* SBR grade (I⫹II versus III) MIB-1 proliferation index* ER␣ expression* 0.949 11.881 1.108 0.968 95% confidence interval P value 0.92–0.98 1.57–89.70 1.00–1.22 0.93–1.00 0.001 0.008 0.016 0.060 NOTE. The analysis was as described in Materials and Methods according to the logistic regression model (25). P ⬍ 0.05 was considered statistically significant (bold type). * Coded as a continuous variable. antiestrogen therapy were based (9, 10). According to this pilot study, which should be confirmed prospectively on a larger scale, the assay of ER by immunohistochemistry is better than that of ER␣ in guiding the clinician, at least in HER2/neunegative tumors. The few studies on the clinical value of ER in terms of prediction of response to tamoxifen have been controversial. Our results agree with others reporting an association between ER and response to tamoxifen treatment (27, 28). They disagree. however. with the proposal that ER overexpression is associated with tamoxifen resistance (29), and that the tamoxifen/ER complex increases expression of AP-1controlled genes involved in cell proliferation (17). Whether ER actively protects breast cancer cells against tamoxifenresistance is unknown. One possible mechanism, however, could be a dominant-negative effect of ER after heterodimerization (16) inhibiting the tamoxifen agonist activity of ER␣ via the AF-1 domain (18, 19). We have not discriminated between initial and acquired tamoxifen resistance, the median time for relapse being 3 years; some resistant cases could be secondary to the selection of cancer cells stimulated for growth by tamoxifen acting as an agonist via ER␣. The four patients who recurred more than 1 year after the 5 years’ therapy were included in the tamoxifensensitive group, with the assumption that these breast cancers were initially responsive to tamoxifen. When considering these four patients as tamoxifen resistant, the multivariate analysis gave a similar significance for ER expression (P ⫽ 0.012). Among the classical markers of aggressiveness (SBR grade, tumor size, MIB-1 proliferation), only lymph node invasiveness was not associated with tamoxifen resistance. This is in agreement with studies showing that node-positive tumors respond as well as node-negative tumors to tamoxifen therapy (30) and that cancer cells, having migrated to lymph nodes, retain the same antiestrogen responsiveness as the primary tumor. The fact that ERcx expression in breast cancer is not predictive of tamoxifen resistance in our study, suggests that the full-length ER-1, or another ER variant, may be involved in tamoxifen sensitivity. It is not excluded, however, that ERcx plays a role in the initial tamoxifen resistance as suggested by studies in which tamoxifen responsiveness was evaluated after 3 months of neo-adjuvant therapy (31). The absence of correlation of ER with other classic prognostic parameters further supports its interest for breast cancer monitoring. The absence of correlation with PgR disagrees with other studies (29, 32) but was supported by a recent study on 242 breast cancers (33). The reasons for these discrepancies is unknown and could be due to different methods used for quantification and/or different sets of patients. Our results do not exclude the involvement of other entities able to induce tamoxifen resistance, such as an increased expression of HER-2/neu (34) and an altered expression of coactivator (35) or corepressor (36). However they strongly suggest that the level of ER in breast epithelial cancer cells contributes better than the level of ER␣ in predicting tamoxifen-sensitivity of breast cancer patients. This should stimulate both large-scale clinical studies before entering ER assay into clinical practice and basic studies to define the biological significance of the association between ER level and tamoxifen responsiveness of breast cancer. ACKNOWLEDGMENTS We thank Drs. Philippe Rouanet, Bernard Saint-Aubert, Jean Grenier, François Quenet, and G. Romieu (from the CRLC Val d’Aurelle, Montpellier) for supplying clinical data, and Jean-Yves Cance for preparing the figures. REFERENCES 1. Katzenellenbogen BS. Antiestrogen resistance: mechanisms by which cancer cells undermine the effectiveness of endocrine therapy. J Natl Cancer Inst (Bethesda) 1991;83:1433–5. 2. Osborne C. Tamoxifen in the treatment of breast cancer. N Engl J Med 1998;339:1609 –18. 3. Ali S, Coombs CR. Endocrine-responsive breast cancer and strategies for combatting resistance. Nat Rev Cancer 2002;2:101–12. 4. Westley B, May FEB, Brown AMC, et al. Effects of antiestrogens on the estrogen-regulated pS2 RNA, and the 52- and 160-kilodalton proteins in MCF7 cells and two tamoxifen resistant sublines. J Biol Chem 1984;259:10030 –5. 5. Nawata H, Bronzert D, Lippman ME. Isolation and characterization of tamoxifen-resistant cell line derived from MCF-7 human breast cancer cells. J Biol Chem 1981;256:5016 –21. 6. Howell A, DeFriend DJ, Robertson JF, et al. Pharmacokinetics, pharmacological and anti-tumour effects of the specific anti-estrogen ICI 182780 in women with advanced breast cancer. Br J Cancer 1996; 74:300 – 8. 7. Coezy E, Borgna JL, Rochefort H. Tamoxifen and metabolites in MCF7 cells: correlation between binding to estrogen receptor and inhibition of cell growth. Cancer Res 1982;42:317–23. 8. Bardon S, Vignon F, Derocq D, Rochefort H. The antiproliferative effect of tamoxifen in breast cancer cells: mediation by the estrogen receptor. Mol Cell Endocrinol 1984;35:89 –96. 9. Systemic treatment of early breast cancer by hormonal, cytotoxic, or immune therapy. 133 randomised trials involving 31,000 recurrences and 24,000 deaths among 75000 women. Early Breast Cancer Trialists’ Collaborative Group. Lancet 1992;339:1–15, 71– 85. 10. Mc Guire WL. Current status of estrogen receptors in human breast cancer. Cancer (Phila) 1975;36:638 – 44. 11. Gustafsson JA. Estrogen receptor -a new dimension in estrogen mechanism of action. J Endocrinol 1999;163:379 – 83. 12. Borgna JL, Rochefort H. Hydroxylated metabolites of tamoxifen are formed in vivo and bound to estrogen receptor in target tissues. J Biol Chem 1981;256:859 – 68. 13. Kuiper GGJM, Carlsson B, Grandien K, et al. Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptor ␣ and . Endocrinology 1997;138:863–70. 14. Saunders PTK, Millar MR, Williams K, Macpherson S, Bayne C, O’Sullivan C, Anderson TJ, Groome NP, Miller WR. Expression of 5776 ER in Breast Cancer and Tamoxifen Resistance oestrogen receptor beta (ER1) protein in human breast cancer biopsies. Br J Cancer 2002;86:250 –256. 15. Palmieri C, Cheng GJ, Saji S, et al. Estrogen receptor beta in breast cancer. Endocr-Rel Cancer 2002;9:1–13. 16. Pettersson K, Delaunay F, Gustafsson JA. Estrogen receptor  acts as a dominant regulator of estrogen signaling. Oncogene 2000;19: 4970 – 8. 17. Paech K, Webb P, Kuiper GGJM, et al. Differential ligand activation of estrogen receptors ER␣ and ER at AP-1 sites. Science (Wash DC) 1997;277:1508 –10. 18. Berry M, Metzger D, Chambon P. Role of the two activating domains of the estrogen receptor in the cell-type and promoter-contextdependent agonistic activity of the antiestrogen 4-hydroxytamoxifen. EMBO. J 1990;9:2811– 8. 19. Delaunay F, Pettersson K, Tujague M, Gustafsson JA. Functional differences between the amino-terminal domains of estrogen receptors ␣ and . Mol Pharmacol 2000;58:584 –90. 20. Davidson NE, Levine M. Breast cancer consensus meetings: vive la difference. J Clin Oncol 2002;20:1719 –20. 21. Bloom HJG, Richardson WW. Histological grading and prognosis in breast cancer. Br J Cancer 1957;11:359 –77. 22. Elston, C. Grading of invasive carcinoma of the breast. In: Page D, Andreson T, editors. Diagnostic histopathology of the breast. Edinburgh: Churchill Livingstone; 1987. p. 300 –11. 23. Roger P, Esslimani Sahla M, Makela S, Gustafsson JA, Baldet P, Rochefort H. Decreased expression of estrogen receptor  protein in prolliferative preinvasive mammary tumors. Cancer Res 2001;61:2537– 41. 24. Saji S, Jensen EV, Nilsson S, Rylander T, Warner M, Gustafsson JA. Estrogen receptors ␣ et  in the rodent mammary gland. Proc Natl Acad Sci USA 2000;97:337– 42. 25. Hosmer DW and Lemeshow SL. Applied logistic regression. In: John Wiley & Sons, editors. Wiley Interscience. New York; 1989. 26. StataCorp. Stata Statistical Software: release 7.0. College Station, TX: Stat Corporation; 2001. 27. Mann S, Laucirica R, Carlson N, et al. Estrogen receptor  expression in invasive breast cancer. Hum Pathol 2001;32:113– 8. 28. Murphy LC, Leygue E, Niu Y, Snell L, Ho SM, Watson PH. Relationship of coregulator and estrogen receptor isoform expression to de novo tamoxifen resistance in human breast cancer. Br J cancer 2002;87:1411– 6. 29. Speirs V, Malone C, Walton DS, Kerin MJ, Atkin SL. Increased expression of receptor  mRNA in tamoxifen-resistant breast cancer patients. Cancer Res 1999;59:5421– 4. 30. Pritchard K. Effects on breast cancer: clinical aspects. In: Lindsay R, Dempster DW, Jordan VC, editors. Estrogens and antiestrogens. Philadelphia: Lippincott-Raven Publishers; 1997. p. 175–210. 31. Saji S, Omoto Y, Shimizu C, et al. Expression of estrogen receptor (ER) cx protein in ER␣ positive breast cancer. Specific correlation with progesterone receptor. Cancer Res 2002;62:4849 –53. 32. Skrilis GP, Munot K, Bell SM, et al. Reduced expression of estrogen receptor  in invasive breast cancer and its re-expression using DNA methyltransferase inhibitors in a cell line model. J Pathol 2003; 201:213–20. 33. Fuqua SAW, Schiff R, Parra I, et al. Estrogen receptor  protein in human breast cancer: correlation with clinical tumor parameters. Cancer Res 2003;63:2434 –9. 34. Osborne CK, Bardou V, Hopp TA, et al. Role of the estrogen receptor coactivator AIB-1 (SRC-3) and HER-2/neu in tamoxifen resistance in breast cancer. J Natl Cancer Inst (Bethesda) 2003;95:353– 61. 35. Shang Y, Brown M. Molecular determinants for the tissue specificity of SERMs. Science (Wash DC) 2002;295:2465– 8. 36. Jepsen K, Hermanson O, Onami TM, et al. Combinatorial roles of the nuclear receptor corepressor in transcription and development. Cell 2000;102:753– 63.