VHA Directive 2010-032 - US Department of Veterans Affairs
advertisement

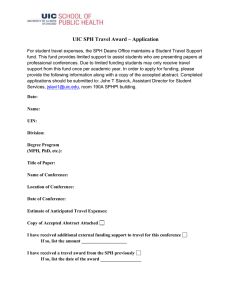
Department of Veterans Affairs Veterans Health Administration Washington, DC 20420 VHA DIRECTIVE 2010-032 June 28, 2010 SAFE PATIENT HANDLING PROGRAM AND FACILITY DESIGN 1. PURPOSE: This Veterans Health Administration (VHA) Directive provides policy for implementation of the Safe Patient Handling (SPH) Program. 2. BACKGROUND a. Work related musculoskeletal back, neck, and arm injuries in nursing staff most commonly result from patient handling tasks. Over the past 30 years, efforts to reduce these injuries included training in body mechanics and lifting techniques, elimination of “weaker” staff, and work hardening. Although these interventions have generally not improved outcomes, substantial reductions in such injuries have resulted through programs with patient handling equipment that reduce biomechanical loads of caregivers. Although SPH research has primarily been directed toward nurses, others who perform manual patient handling are also at high risk for injury and will benefit from SPH measures. Importantly, SPH Programs and the institution of patient-handling equipment have been found to enhance nursing retention and recruitment, as well as improve the quality of patient care. b. The Tampa Patient Safety Center of Inquiry developed a SPH Program as a part of an initiative that led to: markedly-increased satisfaction among patients and staff; decreased number and severity of injuries among caregivers; and improved patient quality of care. Core elements included: a risk assessment identifying unit patient handling equipment needs; introduction of appropriate equipment, training and education; utilization of unit peer leaders (UPL) (formerly Back Injury Resource Nurses) and site coordinators (currently facility champions or coordinators); implementation of a maintenance program; and once those were all in place, the development of a “minimal lift policy.” c. Implementation lessons learned in three ‘early-adopter’ Veterans Integrated Service Networks (VISNs) and results of a VISN 8 follow-up implementation research study found that UPLs are critical to the success of this SPH Program, and specifically, adequate peer leader staffing is directly related to program effectiveness and outcomes. The business case analysis of the VISN 8 data, collected from 2001 to 2003, suggests a payback of the capital investment in approximately 4 years with an internal rate of return between 0.19 and 0.37 depending on model assumptions. This SPH Program served as the basis of the Occupational Safety and Health Administration (OSHA) Ergonomics Guidelines for Healthcare Facilities and has been rolled out by the American Nurses Association as their own “Handle with Care" Program. d. Noting Tampa’s SPH Program, other VHA facilities invested funds and years of effort in SPH Program development. In July 2008, VHA leadership issued an Executive Decision Memo (EDM) supporting SPH initiatives within VHA, which provides $205,000,000 funding to SPH initiatives. Recommendations of the EDM include establishment of a SPH Program that incorporates UPLs facility champions or coordinators, and a facility SPH Committee or Task THIS VHA DIRECTIVE EXPIRES JUNE 30, 2015 VHA DIRECTIVE 2010-032 June 28, 2010 Force. Funding is provided for patient handling equipment, construction costs related to introduction of equipment, and salary monies to support the equivalent of 0.5 Full-Time Equivalent (FTE) employee as the facility patient handling champion or coordinator (see subpar. 5b). e. Consensus over the last several years suggests that ceiling lifts and their associated slings, designed for specific patient handling activities, are more effective in patient handling and safer for the patient and caregiver than portable lift devices. Nevertheless, not all patient care facilities can install ceiling-mounted lift technology without structural modifications. NOTE: Guidance on appropriate lift coverage for specific clinical areas is provided in the Patient Handling (Lifting) Equipment Coverage and Space Recommendations (see subpar. 5a). As patient dependencies vary within clinical units, formal ergonomic patient handling evaluations are necessary to implement a SPH Program. (1) Other equipment needed for SPH includes: sit-to-stand lifts, lateral-transfer devices and friction-reducing devices (often air-assisted), bed and wheelchair movers, ergonomic shower chairs, motorized beds and gurneys, and other types of devices. (2) SPH interventions include such appropriate patient handling technology determined by the evaluation of: the causes of staff injuries, service area of injuries (Community Living Centers (CLCs), Spinal Cord, Critical Care, Medical Surgical, Diagnostics, Behavioral Health, etc.), unit or area patient population characteristics, and local planning construction and renovation. f. Unit or clinical areas for inclusion in the SPH Program include all locations within a health care facility where patients or residents are moved, lifted, and handled, including, but not limited to: nursing units, CLCs, treatment areas, diagnostic areas, procedure areas, and the morgue. The SPH Program covers all patient-resident handling and movement including transport by motor vehicles, wheelchairs, stretchers, and beds. g. The Department of Veterans Affairs (VA) Office of Construction and Facilities Management includes recommendations in VA Construction Design Guidelines for the ergonomic evaluation of new construction, renovations and retrofits of existing construction as outlined in the document Patient Handling (Lifting) Equipment Coverage and Space Recommendations (see subpar. 5a) and addressed in the 2010 Guidelines for Design and Construction of Health care Facilities. This facilitates incorporation of necessary building criteria for installation of ceiling-mounted or overhead lift systems, if feasible and necessary, and for ensuring adequate and accessible storage space for portable or floor-based patient handling equipment. h. Definitions (1) Facility SPH Program. The facility SPH Program ensures required infrastructure is in place to comply with safe patient handling and movement policy. This infrastructure includes patient handling and movement equipment, program elements to support the use of such 2 VHA DIRECTIVE 2010-032 June 28, 2010 equipment, employee training, and a “Culture of Safety” approach to safety in the work environment. Program elements that support equipment use include, at a minimum: the facility champions or coordinators, the SPH facility committee, UPLs, and the use of a patient-handling assessment process that drives specific patient-handling equipment recommendations for each individual patient. (2) SPH UPLs. UPLs provide expertise in the safe patient handling and moving of patients and residents. UPLs SPH expertise is needed to advise co-workers, demonstrate equipment use, and champion the safe patient handling initiative on their units. (3) SPH Facility Champions or Coordinators. SPH facility champions or coordinators are responsible for implementing and maintaining the facility SPH Program and providing leadership, education, and training for the UPLs. (4) SPH Facility Committee. The SPH Facility Committee consists of a multidisciplinary group of clinical staff, facilities management staff, infection control staff, biomedical engineering staff, union representation, logistics staff, contracting staff, safety staff, occupational health staff, and others responsible for assisting in implementation of the SPH Program. This committee may be a sub-committee of an Environment of Care (EOC) or Safety Committee or an independently functioning committee. (5) Assessment Criteria and Care Plan for Safe Patient Handling and Movement. Assessment criteria and care plan for safe patient handling and movement is an example of an assessment process that drives specific patient handling equipment recommendations for each individual patient. (6) Patient Handling Equipment. Patient handling equipment is equipment used to decrease the risk of injury from patient handling activities and includes, but is not limited to: (a) Lifting Equipment, including ceiling-mounted, wall-mounted, portable, and floor-based designs and their accompanying slings, which function to assist in lifting and transferring patients, ambulating patients, repositioning patients, and other patient handling tasks. (b) Lateral Transfer Devices that provide assistance in moving patients horizontally from one surface to another (e.g., transfers from bed to stretcher) and include air assisted, mechanical, and friction-reducing types as well as Transfer Chairs. (c) Specific Beds that provide assistance with patient handling tasks, such as: lateral rotation therapy, transportation, percussion, bringing patients to sitting positions, etc. (d) Motorized Stretchers that provide assistance with patient-handling tasks, such as transporting patients or Hydraulic Gurneys that lift patients from the floor. (e) Repositioning Aids that provide assistance in turning patients and pulling patients up to the head of the bed and up in chairs. 3 VHA DIRECTIVE 2010-032 June 28, 2010 (f) One-way Slide Chair Cushions and other devices that prevent a patient from slipping down into chairs and beds. (g) Equipment, bed, and wheelchair transport assistive devices that assist caregivers in pushing heavy equipment and patients. (h) Powered Height-Adjustable Exam Tables that assist in the transfer of patients onto exam tables, bringing patients to sitting positions, and raising the table surface to a more ergonomically-safe working level. (i) Ergonomic Shower Chairs that are height-adjustable and have reclining features to more easily and safely clean patients. (j) Patient or Resident Transfer Aids that assist patients in moving and transferring independently. (7) Bariatric SPH Threshold. The threshold for instituting bariatric patient-handling techniques is a Body Mass Index (BMI) greater than 30 or weight in excess of 300 pounds, depending on the patient’s body size and shape, medical conditions, and physical dependency. (8) Patient Care Ergonomic Evaluation Process. A Patient Care Ergonomic Evaluation Process provides a method to determine the occurrence of ergonomic hazards in a workplace (e.g., high-risk patient handling tasks) in order to make recommendations for patient handling technology, policy, and procedures to provide musculoskeletal injury risk reduction. 3. POLICY: It is VHA policy that a SPH Program to protect caregivers and patients from injuries due to patient handling and movement must be established and maintained in all VHA facilities and that new construction and renovation projects must incorporate appropriate and necessary patient handling and moving equipment at all VHA facilities. 4. ACTION a. The Office of Public Health and Environmental Hazards (OPHEH). OPHEH is responsible for recommending SPH Program evaluation criteria for the Safety Automated Facility Evaluation (SAFE) Program to the Director Safety, Health, Environmental, and Emergency Management (10NS). b. Director, Safety, Health, Environmental, and Emergency Management (10NS). The Director, Safety, Health, Environmental, and Emergency Management is responsible for providing management support and evaluation and technical assistance to VISNs and facilities, as appropriate, to ensure compliance with this Directive. c. VISN Director. Each VISN Director is responsible for: (1) Planning, coordinating, implementing, and maintaining a SPH Program across the VISN; (2) Financial oversight across the VISN for SPH funding; and 4 VHA DIRECTIVE 2010-032 June 28, 2010 (3) Monitoring SPH program implementation by designating a VISN staff member or VISN committee to do so. d. Facility Director. Each facility Director is responsible for: (1) Planning, coordinating, implementing, and maintaining a SPH Program. NOTE: See subpar 5c for a model program implementation policy template. (2) Ensuring financial oversight of the SPH Program within the facility. (3) Supporting the equivalent of 0.5 FTE SPH Facility Champion or Coordinator position, funded for 2 years (fiscal years 2010 and 2011), to: (a) Address equipment needs; (b) Develop a facility-wide unit peer leader (UPL) program; (c) Train UPLs in their roles and responsibilities, elements of SPH policy, and equipment usage; (d) Establish an end-user equipment maintenance program; and (e) Coordinate the SPH Program within the facility. (4) Ensuring the facility champions receives privacy training as instructed in Directive 7701 for Accident Review Board (ARB) members. (5) Supporting a facility SPH UPL Program with one UPL per shift in each unit or clinical area. (6) Ensuring the facility Nursing Service and a hospital committee (Safety, EOC, Patient Safety, or other newly organized committee) maintain oversight of SPH program operations and activities. (7) Ensuring assistance from and collaboration between services and entities (such as facilities management, safety, contracting, logistics, SPD, nursing, therapy, etc.) that impact successful SPH Program implementation. (8) Ensuring utilization of the SPH expertise of facility champions when developing renovation plans, facility projects, and new construction that involve introduction or installation of patient handling equipment. (9) Ensuring that appropriate patient handling (lifting) equipment is installed during new construction and renovation construction projects in unit and clinical areas where patient handling occurs. The following is required: 5 VHA DIRECTIVE 2010-032 June 28, 2010 (a) Completion of a detailed ergonomic evaluation during the design requirements planning process to determine necessary patient lifting equipment; (b) Installation of ceiling-mounted or overhead lift systems, where necessary and feasible; and (c) Provision of adequate and accessible storage space for portable or floor-based and other patient handling equipment. NOTE: Refer to Patient Handling (Lifting) Equipment Coverage and Space Recommendation, (see subpar. 5a) and the 2010 Guidelines for Design and Construction of Health care Facilities in determining appropriate SPH design requirements. (10) Ensuring appropriate patient handling injury data is provided to facility champions by the facility Safety Officer and Human Resources, as needed, in order for them to: investigate such injuries, provide recommendations, and track these injuries by unit, area, and hospitalwide. (11) Ensuring patient handling equipment with attachment or other potential ligature points, such as ceiling lifts, are not installed in mental health units where patients are suicidal or psychiatrically unstable. In lieu of such prohibited equipment, portable lifting or moving devices may be used. Portable or floor-based and other patient handling equipment must be returned to locked storage immediately after use so that patients cannot access the equipment. (12) Ensuring that the selection and design of ceiling lift systems in CLCs use as minimally obtrusive track systems as possible in order to maintain an aesthetically pleasing appearance in the resident room. It is imperative that SPH systems fit into a home-like environment in patient and resident rooms, especially in CLC settings. NOTE: Ceiling lifts may be used in CLCs for all populations since residents must be medically and psychiatrically stable for admission and continued stay. e. SPH Facility Champions or Coordinators. SPH Facility Champions or Coordinators are responsible for: (1) Implementing and maintaining the facility SPH Program; (2) Providing leadership, education and training for UPLs; (3) Investigating as appropriate, reviewing, and tracking patient handling injuries in order to make suitable recommendations to decrease caregiver risk of injury; (4) Making patient handling equipment recommendations based on the ergonomic process and facilitating purchase of recommended equipment; and (5) Ensuring oversight of patient handling equipment. 6 VHA DIRECTIVE 2010-032 June 28, 2010 f. SPH Facility Committee. The SPH Facility Committee assists the SPH Facility Champion or Coordinator in: (1) Implementing and maintaining the SPH Program; (2) Reviewing and tracking injury data; (3) Facilitating patient handling equipment selection and purchases; (4) Ensuring awareness of patient handling issues within facility; and (5) Facilitating collaboration with various services and entities within the facility that impact the SPH Program. 5. REFERENCES a. Patient Handling (Lifting) Equipment Coverage and Space Recommendations (Find under ‘Patient Handling Equipment/Evaluation/Information Resources’ at http://www.visn8.va.gov/PatientSafetyCenter/safePtHandling/FacilityChampionResources.asp). b. EDM on Safe patient Movement and Handling Initiative, dated July 1, 2008 http://nlb.vssc.med.va.gov/EDMs/Document%20Library/EDM%20Safe%20Patient%20Moveme nt%20and%20Handling%20Initiative.pdf c. Facility Safe Patient Handling Policy Template (Find under ‘Facility Champion Materials' at: http://www.visn8.va.gov/PatientSafetyCenter/safePtHandling/FacilityChampionResources.asp). d. Bureau of Labor Statistics, 2002. Survey of occupational inquiries and illnesses, 2001. US Department of Labor (USDL) December 19, 2002. e. Collins, J.W., Wolf, L., Bell, J, & Evanoff, B (2004). An evaluation of a “best practices” musculoskeletal injury prevention program in nursing homes. Injury Prevention, 10, 206-211. f. Evanoff, B., Wolf, L., Aton, E., Canos, J., & Collins, J. (2003). Reduction in injury rates in nursing personnel through introduction of mechanical lifts in the workplace. American Journal of Industrial Medicine, 44, 451-457. g. Marras, W.S., Knapik, G.G., & Ferguson, S. (2009). Lumbar spine forces during manoeuvring of ceiling-based and floor-based patient transfer devices. Ergonomics, 52:3,384397. h. Matz, M. (2008) Analysis of VA Patient Handling and Movement Injuries and Preventive Programs. Internal VHA report to Director, VHA, Occupational Health Program. (Find under ‘Facility Champion Materials' at http://www.visn8.va.gov/PatientSafetyCenter/safePtHandling/FacilityChampionResources.asp). 7 VHA DIRECTIVE 2010-032 June 28, 2010 i. Nelson, A., Matz, M., Chen, F., Siddharthan, K., Lloyd, J., Fragala, G. Development and evaluation of a multifaceted ergonomics program to prevent injuries associated with patient handling tasks. Int J Nurs Stud. 2006 Aug;43(6):717-33. Epub 2005 Oct 25. j. Nelson, AL and Baptiste, A. (2004). Evidence-Based Practices for Safe Patient Handling and Movement. Online Journal of Issues in Nursing, 19 (3) Manuscript 3. Available at: http://www.journalofnursingstudies.com/article/S0020-7489(05)00169-0/ abstract k. U.S. Department of Labor, Occupational Safety and Health Administration. (2003). Ergonomics Guidelines for Nursing Homes. Available at: http://www.osha.gov/ergonomics/guidelines/nursinghome/ l. Department of Veterans Affairs, Deputy Under Secretary for Health for Operations and Management (10N) Memorandum dated February 26, 2008. “Clarification of Use of Mental Health Environment of Care Checklist.” m. Peer Reviewed SPH References, Matz, M. (2009) (Find under ‘Safe Patient Handling Bibliography' at http://www.visn8.va.gov/PatientSafetyCenter/safePtHandling/FacilityChampionResources.asp). n. Assessment Criteria and Care Plan for Safe Patient Handling and Movement (Find as Assessment Forms and Algorithms under ‘Resources/Websites’ at http://www.visn8.va.gov/PatientSafetyCenter/safePtHandling/FacilityChampionResources.asp). 6. FOLLOW-UP RESPONSIBILITY: The Chief Nursing Officer (108) is responsible for the contents of this Directive. Questions on implementation may be referred to OHSPSHG (13D) at (813) 558-3928 or at (202) 461-1039 and to Nursing at (813) 979-3672. 7. RECISSIONS: None. This VHA Directive expires on June 30, 2015. Robert A. Petzel, M.D. Under Secretary for Health DISTRIBUTION: 8 E-mailed to the VHA Publication Distribution List 6/29/10