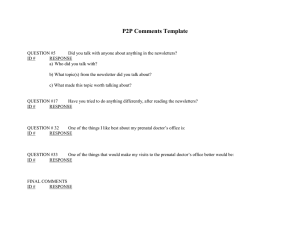
provider manual
advertisement

2015 PROVIDER MANUAL LAST UPDATED: JANUARY 2015 MCD_PV_PMREV_0115_01/21/2015_WZ Total Care, A Today’s Options of New York Health Plan is a member of the Universal American family of companies. WELCOME Welcome to the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. Thank you for your commitment and dedication to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and our members. As a participating provider, you play an instrumental role in the delivery of quality health services. ABOUT THIS MANUAL This manual will provide you with the necessary information to facilitate the delivery of health care for TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN members, such as: Member identification Claim procedures Verification of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN coverage TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Quality Improvement, Utilization Management, and Case Management Programs. YOUR CALL TO ACTION We encourage you to carefully read this manual Contact your Provider Relations Representative with any questions or comments regarding this manual, or to discuss any aspects of being a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Participating Provider Call our Member Service Department with comments or to obtain any general information HOW YOU CAN REACH US Representatives are available 8:00 a.m. through 5:00 p.m. Monday through Thursday, 9:00 a.m. through 5:00 p.m. Friday. After these hours, an answering service is available. Member Services Provider Services (Quality Assurance/Utilization Review & Provider Relations) Toll Free Number for all of the above FAX Number (800) 223-7242 (315) 234-5901 (877) 872-4716 (800) 223-7242 (315) 425-5502 When writing to us or for claim submission: TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN P O Box 11507 Syracuse, New York 13218-1507 Again, welcome to the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. We are looking forward to a long lasting working relationship. MCD_PV_PMREV_0115_01/21/2015 TABLE OF CONTENTS Welcome About This Manual Your Call To Action How You Can Reach Us SECTION 1 MEMBERSHIP AND ELIGIBILITY How to Identify TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member .............................................................................................................................................1 Determining Eligibility of Members ..................................................................................................1 SECTION 2 PROVIDER RESPONSIBILITIES Primary Care Provider (PCP) Selection by Member .........................................................................1 Expectations of Primary Care Providers ...........................................................................................1-3 Child/Teen Health Program (C/THP) ................................................................................................3 Adult Preventive Guidelines ..............................................................................................................4 Prenatal Guidelines ............................................................................................................................5 Appointment Availability Guidelines ................................................................................................5 Duty to Report ....................................................................................................................................6 24 Hour, 7 Days a Week Access to Clinical Care..............................................................................7 Standards of Care ...............................................................................................................................7 Transfer of Mental Health and Substance Abuse Information...........................................................7 Health Care Professional Performance Evaluation ............................................................................8 Attachments 2-3……………………………………………………………………………………..9-26 SECTION 3 STANDARDS OF CARE/PERFORMANCE EVALUATION Standards for Medical Records .........................................................................................................1-2 Medical Record Review ....................................................................................................................2-3 SECTION 4 UTILIZATION MANAGEMENT AND CASE MANAGEMENT Preauthorization ..............................................................................................................................1-10 Notification Methods and Time Frames of Utilization Decisions ..................................................... 11 Emergency Admissions....................................................................................................................12 Referrals/Referral Form Required....................................................................................................13 Standing Referrals ............................................................................................................................. 13 Specialist or Specialty Center as PCP ............................................................................................... 14 Access to Specialty Care ................................................................................................................... 14 Continuity of Care ............................................................................................................................. 15 Continuity upon Provider Leaving Network ..................................................................................... 15 Case Management ............................................................................................................................. 16-17 SECTION 5 BILLING AND CLAIMS Contractor Requirements .................................................................................................................. 1 Electronic Submissions ..................................................................................................................... 1 Manual Submission of Claims .......................................................................................................... 1-2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Critical UB04 Data Elements ............................................................................................................................................ 2 Claims Should Be Completed Per CMS 1500 or UB04 Billing Manuals ......................................... 3 Explanation of Payment .................................................................................................................... 3 Inclusive and Multiple Services ........................................................................................................ 3 Identification of the Primary Payer ................................................................................................... 3-4 Non-Covered Services ...................................................................................................................... 4 Hold Harmless .................................................................................................................................. 4-5 Post Payment Audits ......................................................................................................................... 5 Requests for Services of Claim Payment Issues ............................................................................... 6 SECTION 6 QUALITY IMPROVEMENT PROGRAM SECTION 7 BENEFIT SUMMARIES TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Medicaid Managed Care ................................................................................................................................................... 1-3 Benefits Using a Medicaid Card Only .............................................................................................. 4 Services Not Covered by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or Medicaid……………………………………………………………………………….4-5 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Child Health Plus (CHIP) Benefits................................................................................................................................. 5-7 Services Not Covered Under CHIP .................................................................................................. 7 Family Health Plus (FHPlus) ............................................................................................................ 8-9 Services Not Covered Under FHPlus................................................................................................ 10 FHPlus Co-Payments ........................................................................................................................ 10-11 SECTION 8 MEMBERS RIGHTS/RESPONSIBILITIES Members Rights ................................................................................................................................ 1 Member Responsibilities .................................................................................................................. 2 SECTION 9 ACTION/GRIEVANCES/APPEAL SYSTEMS Definitions......................................................................................................................................... 1-3 Upon Receipt of a Service Authorization Request ........................................................................... 3-4 Prior Authorization Determinations .................................................................................................. 4 Concurrent Review Determinations .................................................................................................. 5 Extension of Service Authorization Timeframes .............................................................................. 6 Retrospective Review ....................................................................................................................... 6 Notice of Actions (Adverse Determinations).................................................................................... 7 Formats and Content of Notices........................................................................................................ 7-9 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Obligation to Notify ................................................................................................................................................ 9-10 Action Appeals Process .................................................................................................................... 10-12 Timeframes for Resolution of Action Appeals ................................................................................. 12-13 Appeal Requests................................................................................................................................ 13 Action Appeal Notices ...................................................................................................................... 13-14 External Appeals ............................................................................................................................... 14-15 Response to External Appeal Requests ............................................................................................. 15 Provider Request for External Appeal .............................................................................................. 16 Results of External Appeal ............................................................................................................... 16 Grievances......................................................................................................................................... 16-17 Timeframes for Grievance Resolution by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN ................................................................................................................... 17 Grievance Determination Notices ..................................................................................................... 17-18 Grievance Appeals ............................................................................................................................ 18-19 Important Telephone Numbers And Addresses ................................................................................ 19 SECTION 10 EXTERNAL APPEALS External Appeals ............................................................................................................................... 1 Response to External Appeal Requests ............................................................................................. 1-2 Provider Request for External Appeal .............................................................................................. 2 Results of External Appeal ............................................................................................................... 2-3 SECTION 11 PHARMACY Pharmacy........................................................................................................................................... 1 SECTION 12 TERMINATION OF CONTRACT Procedures for Termination of Contract between TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and Health Care .............................................................................. 1 Hearing.............................................................................................................................................. 2 Non-Renewal .................................................................................................................................... 3 SECTION 13 FRAUD AND ABUSE Fraud and Abuse Contact Information .............................................................................................. 1 SECTION 14 HIV Guidelines Guidelines ......................................................................................................................................... 1-8 SECTION 15 Transportation Policy Policy ................................................................................................................................................ 1 SECTION 16 DEFINITIONS Definitions......................................................................................................................................... 1-3 SECTION 17 CREDENTIALING PROCEDURES……………………………………………………………………………………1-9 SECTION 18 TUBERCULOSIS………………………………………………………………....1-3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 1 MEMBERSHIP AND ELIGIBILITY HOW TO IDENTIFY A TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MEMBER Each TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN member is issued a membership card upon enrollment and is instructed to produce this card when presenting for any health care services covered under a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Managed Care Benefit Package. The member’s identification card will identify their Primary Care Provider and their effective date of coverage. If a member does not have their identification card, or you have any questions on membership, contact Member Services at (800) 223-7242 or toll free at (800) 223-7242. DETERMINING ELIGIBILITY OF MEMBERS TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Medicaid/Family Health Plus: Prior to rendering care, it is the responsibility of each service provider to verify a member’s Medicaid Managed Care or Family Health Plus coverage through the eMedNY (ePaces) website www.emedny.org. The ePaces website is designed to provide an accurate and timely verification of a recipient’s eligibility for Medicaid Managed Care or Family Health Plus services. A Medicaid Managed Care or Family Health Plus enrollee covered under TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will appear on the Eligibility Screen as: Eligible PCP…Insurance Coverage Code “TO” Both “PCP” and “TO” must appear for coverage to be in effect. Confirmation of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN coverage can also be obtained using either a touch-tone or rotary dial telephone by calling 1-800-997-1111. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Child Health Plus All Child Health Plus members receive an identification card. Members should be requested to present their card at each visit. Eligibility cannot be confirmed using ePaces. If you have any questions on eligibility, do not hesitate to contact TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Member Services Department at (800) 223-7242 or toll free at (800) 223-7242. Revised January 2015 Section 1 Page1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 2 PROVIDER RESPONSIBILITIES PRIMARY CARE PROVIDER SELECTION BY MEMBER The Primary Care Provider (PCP) is responsible for coordinating the member’s health care. Each TOTAL CARE, A TODAY’s OPTIONS OF NEW YORK HEALTH PLAN’s Member is encouraged to select a PCP from TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Network Directory. If a provider is not accepting new patients, there will be an asterisk (*) next to the provider’s name in the directory. If a member does not select a PCP, the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member Service Department contacts the member to assist them with making a selection (A Primary Care Provider is a Pediatrician, Family Practitioner or Internist). If all attempts to contact the member are unsuccessful, the member is notified by mail of a selection made by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. At this time, the member is again afforded the opportunity to select his or her own PCP. A member can change their PCP at any time by calling the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member Services Department toll free at (800) 223-7242. The effective date of the change will be the first of the month following the month of the request unless there are special circumstances. EXPECTATIONS OF PARTICIPATING PROVIDERS Participating Providers are expected to: • • • • • • • Perform duties in their area of specialty. Provide preventive care services, including well child, adolescent, and adult preventive services (e.g., pap smears, HIV counseling, immunizations). See Attachments 1. Provide complete current information concerning a diagnosis, treatment, treatment options and prognosis from a physician or other provider in terms the patient can be reasonably expected to understand. When it is not advisable to give such information to the patient, the information will be made available to an appropriate person on the patient’s behalf. Provide information from a physician or other provider necessary to give informed consent prior to the start of any procedure or treatment. Afford the patient the opportunity to refuse treatment to the extent permitted by law and to be informed of the medical consequences of that action. Be responsible for the supervision of patient care if a mid-level practitioner or resident renders care. Be responsible for patient care twenty-four hours a day or make arrangements with an alternate participating provider who must be available by telephone and can be available for coverage. If you use an answering machine, the message must direct the enrollee to a live voice. Work closely with the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Quality Assurance/Utilization Review (QA/UR) Department to assure patient compliance with follow-up. Revised January 2015 Section 2 Page1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL • Comply with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s credentialing criteria and policies (see Section 17) • Primary Care Providers (PCP) will coordinate care when the patient is referred to a specialist. • Comply with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s procedures on referrals and preauthorization (See Section 4) • Refer patients to the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN QA/UR Department who require Case Management Services. • Maintain confidentiality of medical information. For patients who have AIDS or who have been tested for the HIV virus, please see NYS Public Health Law Article 27.F, Section 2782. • Comply with New York State Department of Health Communicable Disease Reporting Requirements (e.g. HIV, Tuberculosis, Hepatitis C etc.). These requirements are found at http://www.health.ny.gov/professionals/diseases/reporting/communicable/ • Communicate with patients regarding areas of needs, and concerns requiring immediate attention. • Comply with Federal and state requirements for informed consent for hysterectomies and sterilization. Requirements are found on http://www.health.state.ny.us. • Utilize formal Mental Health and Substance Abuse Assessment Tools. • Adhere to the Express Script/TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Pharmacy Formulary. See our website at www.totalcareny.com for detailed information. • Refer patients needing urgent evaluation or emergency care to a participating emergency department or urgent care site whenever possible. • Adhere to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Appointment Availability Guidelines (See page 4 of this Section). Ensure that members with appointments are not routinely made to wait longer than one hour. • Adhere to Child/Teen Health Guidelines (See Attachment 1). • Comply with the Adult Preventive Care Guidelines (See Attachment 2). • Make available records and medical information for Quality Improvement/Utilization Review activities (See Sections 4 and 6). • Follow TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Standards for Medical Records (See Section 3). Revised January 2015 Section 2 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL • Receive signed acknowledgment from the member prior to rendering non-covered services. Signed acknowledgments confirm the member’s knowledge of non-covered services under their Benefit Plan. • Participate in TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Health Advisory Committees if possible. • Adhere to adopted clinical practice guidelines. Listed on the next page are the reference sources for the guidelines adopted by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN: TB What the Clinician Should Know, US Department of HHS, Public Health Service 4th Edition STD Guidelines for Treatment of Sexually Transmitted Diseases, US Department of Health and Human Services, Centers for Disease Control and Prevention www.cdc.gov/std/treatment Lead Screening and Follow-Up Requirements New York State Department of Health, DOH Subpart 67-1 Screening and Follow-Up HIV Practice Guidelines New York State Department of Health AIDS Institute. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has adopted the clinical practice guidelines of the New York State Department of Health AIDS Institute. Clinical Guidelines pertain to HIV prevention and medical management of adults, children and adolescents with HIV infection. Clinical guidelines can be accessed at www.hivguidelines.org. HIV Counseling and Testing of Pregnant Women Department of Health Memorandum A1 99-01. All pregnant women must receive counseling on HIV. The medical record must show written documentation when the counseling was given. The obstetrical provider is expected to encourage all pregnant women to have serological blood test for HIV. In New York State all newborns are screened for HIV after birth. However, if the mother’s positive HIV status is known prior to birth there is the window of opportunity to significantly reduce the vertical transmission of virus if the mother took anti-retroviral medications during the pregnancy. Pneumococcal Conjugate Vaccine New York State Department of Health CHILD/TEEN HEALTH PROGRAM (C/THP) The Child/Teen Health Program (C/THP) is a program of early and periodic screening, including periodic diagnostic and treatment services for children and adolescents up to 21 years of age. Care and services are provided in accordance with the periodicity schedule and guidelines developed by the American Academy of Pediatrics (See Attachment 1). Primary Care Providers will make every effort to ensure that the C/THP Guidelines are followed when providing services to TOTAL CARE, A TODAY’S OPTIONS OF NEW Revised January 2015 Section 2 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL YORK HEALTH PLAN members. The PCP’s medical record must document services, referrals for services and follow up as required by C/THP (See Attachment 1). ADULT PREVENTIVE CARE GUIDELINE Attachment 2 of this section outlines the Adult Preventive Care Guideline that has been adopted by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. Revised January 2015 Section 2 Page 4 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL PRENATAL GUIDELINES All providers are required to follow the New York State Prenatal Guidelines (See Attachment 3). Members can receive prenatal care from their choice of OB/GYN providers within the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Network. No referral from the PCP is necessary. APPOINTMENT AVAILABILITY GUIDELINES All providers in the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN network will comply with the following appointment availability guidelines. • Emergency Care: Immediately upon presentation at a service delivery site. • Urgent Care: Within twenty-four (24) hours of request. • Non-Urgent “Sick” Visit: Within forty-eight (48) to seventy-two (72) hours of request. • Routine Appointments: Within four (4) weeks of request. • Specialist Referrals (not urgent): Within four (4) to six (6) weeks of request. • Initial Prenatal Visit: Within three (3) weeks during first trimester, two weeks during the second trimester, and one week thereafter. • Adult Baseline and Routine Physicals: Within twelve (12) weeks from enrollment. • Well Child Care: Within four (4) weeks of request. • Initial Family Planning Visits: Within two weeks of request. • In-Plan Mental Health or Substance Abuse Follow-Up Visits (pursuant to an emergency or hospital discharge): within five (5) days of request, or sooner as clinically indicated. • In-Plan, Non-Urgent Mental Health or Substance Abuse Visits: Within two (2) weeks of request. • Initial PCP Office Visit for Newborns: Within two (2) weeks of hospital discharge. • Provider Visits To Make Health, Mental Health and Substance Abuse Assessments for the purpose of making recommendations regarding a recipient’s ability to perform work when requested by a LDSS: within ten (10) days of request by an Enrollee, in accordance with Benefit Agreement. These guidelines are based on New York State Department of Health requirements and may be changed by the Department of Health. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will annually complete appointment availability and accessibility surveys of providers. The TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Medical Director will communicate outcomes of those surveys to the provider. Revised January 2015 Section 2 Page 5 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL In the event that there is a problem identified, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will work with the provider to determine and implement a corrective action plan. DUTY TO REPORT TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is obligated under New York State Public Health Law (Article 4405-b) to make a report to the appropriate professional disciplinary agency within thirty days of obtaining knowledge of any information that reasonably appears to show that a health professional is guilty of professional misconduct as defined in Article One Hundred Thirty One Section 6530. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will report the following to the Office of Medical Misconduct: The termination of a health care provider contract pursuant to New York State Public Health Law (4406-d) for reasons relating to alleged mental or physical impairment, misconduct or impairment of patient safety or welfare; 2 The voluntary or involuntary termination of a contract or employment or other affiliation with such organization to avoid the imposition of disciplinary measures; or 3 The termination of a health care provider contract in the case of a determination of fraud or in a case of imminent harm to patient health. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will submit the information, in writing to : 1 Director, Central Intake Operations Office of Professional Medical Conduct New York State Department of Health 433 River Street, Suite 303 Troy, New York 12180-2299 The report will include the MD’s full name, license number, address, account/date of event/incident, of actions taken by the health plan (including date of termination of contract or withdrawal), and contact persons at the managed care organization (MCO). TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will seek an “advisory opinion” if TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is reasonably unable to determine whether a report must be made. These advisory opinions will be sought by written request to the Director of OPMC at the address listed above. Any report or information furnished to an appropriate professional discipline agency in accordance with the provisions of Section 4405-b will be deemed a confidential communication and will not be subject to inspection or disclosure in any manner except upon formal written request by a duly authorized public agency or pursuant to a judicial subpoena issue in a pending action or proceeding. Revised January 2015 Section 2 Page 6 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 24-HOUR, 7-DAYS A WEEK ACCESS TO CLINICAL CARE TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN provides access to medical services to its enrollees 24-hours a day seven days a week through the network of Primary Care Providers who supervise and coordinate their care. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s contracts with Primary Care Providers require that each PCP assure the availability of covered health services to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN members on a 24-hour a day, 365 days per year basis, including periods after normal business hours, on weekends, or at any other time. The PCP must arrange for complete back up coverage from other participating providers in the event the PCP is unable to be available. Coverage and availability must allow a member to reach a live voice with one phone call. In the event the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member is calling from a pay phone, or cannot receive a return call, adequate arrangements must be in place to connect the Member to his/her provider. In the event the PCP is temporarily unavailable or unable to provide patient care or referral services to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Members, the PCP must arrange for another TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN participating physician to provide such services. In the rare event a PCP has a non-contracted physician covering, the PCP must have prior approval of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. The covering provider must sign an agreement to accept the PCP’s negotiated rate and agree not to balance bill TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Members. STANDARDS OF CARE Participating providers are required to comply with all applicable federal and state laws, licensing requirements and professional standards. Additionally, they are required to provide covered services in accordance with general practice guidelines. By signing the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Participating Provider Agreement, the provider agrees that, he/she will comply with all federal, state and local laws in the conduct of his/her profession, including those prohibiting discrimination against the disabled. TRANSFER OF MENTAL HEALTH AND SUBSTANCE ABUSE INFORMATION It is the policy of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to promote continuity of care and ensure adequate communication of all services received by a member to the Plan PCP. Revised January 2015 Section 2 Page 7 Mental Health and Substance Abuse Specialists will obtain signed patient release of information forms at initial visits to ensure consistent communication between Mental Health and Substance Abuse Specialists and the Plan PCP. HEALTH CARE PROFESSIONAL PERFORMANCE EVALUATION TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will ensure that health care professionals are regularly informed of information maintained by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to evaluate the performance or practice of the health care professional. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will consult with health care professionals in developing methodologies to collect and analyze health care professional profiling data. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will use its Quality Assurance Committee to define the methodologies and review the outcome of analysis. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN also reviews Quality Assurance outcomes with the Board of Directors. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide any such information and profiling data and analysis to health care professionals. Such information, data or analysis shall be provided on a periodic basis appropriate to the nature and amount of data and the volume and scope of services provided. The information will also be made available upon request of the health care professional. Any profiling data used to evaluate the performance or practice of a health care professional will be measured against stated criteria and an appropriate group of health care professionals using similar treatment modalities serving a comparable patient population. Upon presentation of such information or data, each health care professional will be given the opportunity to discuss the unique nature of the health care professional’s patient population which may have a bearing on the health care professional’s profile and to work cooperatively with the managed care organization to improve performance. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN CREDENTIALING TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will complete credentialing activities and notify the provider within 90 days of completed application. The notification will inform you as to whether you are credentialed, whether additional time is needed or that TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is not in need of additional providers. If additional information is needed by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, we will notify you as soon as possible, but no more than 90 days from the receipt of the application. See Section 17 for Credentialing Policy and Procedure. Revised July 2014 Section 2 Page 9 Attachment 2 MEMBER NAME PROVIDER DATE OF BIRTH FACILITY TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN ADULT PREVENTIVE GUIDELINES REVIEW (Ages 21 – 75 Years) STANDARD YES NO N/A DATE Has member had PCP visit during review year? Initial History Completed at First Visit? (All) B/P (All) Height (All) Weight (All) BMI Dental Screening? (All) Pap every year? (All Women) [May be less frequent if 3 consecutive neg. results]. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 Chlamydia? (Women under 25 and sexually active, women over 26 if at risk or symptomatic.) Rubella serology or Vac. History? (Women of child bearing age). Blood Cholesterol? (Men every 5 years from age 35 – Women every 5 years from age 45). Colon Ca. Screening?(Yearly after age 50 for all). Mammography? (Yearly for women over 40). Vision Screening? (All over age 65). Assess for Hearing Impairment? (All over 65). Assess for Problem Drinking? (All) Tobacco and Substance Abuse Screening? (All) Substance use counseling? (All) Injury Prevention counseling? (All) Sexual Behavior counseling? (All) HIV testing offered (All) Annual Diet and Exercise counseling? (All) Dental Health counseling? (All) Tobacco use counseling? (All) Td Booster? (All, every 10 years) Hepatitis B Vac.? (All at increased risk) MMR Vac.? (All born after 1956 w/o proof of immunity) Varicella Vac.? (All non-immune adults) Pneumococcal? (All over age of 65) Influenza? (All over age of 50) Reviewed By: Date Reviewed: Revised January 2015 WAS MENTAL HEALTH SCREEN DONE? WAS SUB. ABUSE SCREEN DONE? Section 2 Page 10 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 Medicaid Prenatal Care Standards Prenatal care standards in New York State (10 NYCRR, Part 85.40) were developed in early 1990 in response to the creation of the Prenatal Care Assistance Program (PCAP), a prenatal care program developed to provide for comprehensive perinatal care to low income, high risk pregnant women. The most recent revision of these standards occurred in 2000. Changes in the clinical standards of prenatal care since that time necessitate a review of Part 85.40 standards to compare them to current professional standards of practice which address new challenges and concepts in prenatal care. In order to accomplish this task, the Department partnered with the Island Peer Review Organization (IPRO) to review the existing PCAP standards and compare them to current American College of Obstetricians and Gynecologists (ACOG) guidelines 1 new recommendations in prenatal care, as well as other national guidelines of obstetric practice to determine the need to modify the prenatal standards as they become applied to all Medicaid prenatal providers. The Office of Health Insurance Programs, in collaboration with the Division of Family Health, IPRO and a statewide advisory workgroup made up of key stakeholders in the field of prenatal care were charged with the responsibility for developing this revised set of Medicaid Prenatal Care Standards for New York State. Steps in the process included: • Literature review and comparison of Part 85.40 with current ACOG guidelines and other evidence-based literature; • Stakeholder meetings to discuss current standards of practice; • Summary proposal with recommendations for revised standards; • Revisions to Article 25, New York State Public Health Law; and • Draft Medicaid Prenatal Care Standards for review and subsequent adoption. The Department would like to express its appreciation to all the external stakeholders who gave of their time and shared their expertise in the field of prenatal care to assist us in the development of prenatal care standards for the NYS Medicaid Program. A. Requirements 1. General requirements: a. Prenatal care providers shall create and maintain records and reports that are complete, legible, retrievable and available for review by representatives of the Commissioner of Health upon request. Such records and reports shall include the following: i. a comprehensive prenatal care record for each pregnant woman which documents the provision of care and services received and which is maintained in a manner consistent with medical confidentiality requirements; TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL ii. special reports and data submissions as necessary for the Commissioner of Health; iii. records of internal quality assurance; iv. all written policies and procedures required by this section; and v. data submissions in electronic form as requested by the Commissioner of Health in compliance with the most current Department of Health policies for health information exchange in New York State. b. Prenatal care providers shall comply with all federal, state and local laws and regulations regarding the disclosure of protected medical information when sharing or transferring medical information with other healthcare providers or facilities. Providers shall therefore obtain written informed consent from patients prior to transfer of medical records or information where required by law. c. Prenatal care providers shall comply with the requirements to obtain informed consent for all services described herein, in accordance with all applicable laws and regulations. d. Any subcontracts between the prenatal care providers and other agents or agencies providing care and services shall: e. 2. Attachment 3 i. be available for review and inspection by the Department of Health; and ii. require that subcontractors provide contracted care and services that meet the minimum standards established in this section and are provided in accordance with generally accepted standards of practice and patient care services. Prenatal care providers shall participate in quality improvement initiatives as requested by the Commissioner of Health. Provider/Staff requirements: a. Prenatal care services, including prenatal diagnostic and treatment services, provided to pregnant women and postpartum women shall meet generally accepted standards of care as described by the most current American Academy of Pediatrics (AAP) and American College of Obstetricans and Gynecologists (ACOG) guidelines for perinatal care and shall be provided by a qualified provider practicing as: i. a licensed physician practicing in accordance with Article 131 of the New York State Education Law and must be either an obstetrical care physician (MD/DO), Board Certified or Board Eligible in their area of specialty, or have completed an accredited residency program in Family Practice or Obstetrics/Gynecology; TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 3. Attachment 3 ii. a nurse practitioner practicing in accordance with Article 139 of the New York State Education Law; iii. a licensed Midwife practicing in accordance with Article 140 of the New York State Education Law; or iv. a registered physician's assistant practicing in accordance with Part 94 of this Title, Article 37 of the NYS PHL and article 131 of the NYS Education Law. b. Prenatal care providers shall promote the delivery of prenatal care services in a culturally sensitive/competent manner to all pregnant women including those with limited English proficiency and diverse cultural and ethnic backgrounds. Interpretation services must be offered to patients whose primary language is not English, in person when practical, or via telephone if a translator is not immediately available. c. Prenatal care providers must either have admitting privileges at one or more hospitals or shall develop agreements with planned delivery sites including a system for sharing patient information for continuity and follow-up care. Provider/Specialist/Consultation Requirements: Prenatal care providers shall provide pregnant women timely access and referral to appropriate levels of prenatal care, (basic, specialty, and subspecialty), based on her assessed risk status in order to prevent, recognize and treat conditions associated with maternal and infant mortality and morbidity.2 a. Management of pre-existing medical conditions Providers shall provide or arrange for the provision of care for the specific needs of a pregnant woman with a pre-existing medical condition, according to current standards of practice. b. Transfer of care - Practices shall develop criteria requiring transfer of primary responsibility for patient care from a family medicine practice physician, physician's assistant, licensed midwife or nurse practitioner to an obstetrician and/or maternal-fetal medicine specialist (high risk obstetrician or perinatologist). c. Specialty physician consultation/referral - Prenatal care providers shall develop criteria for consultation and referral for care to a maternal-fetal medicine specialist, perinatalogist, high risk obstetrician, specialty physician, behavioral health specialist, including licensed social worker or other health care specialist as necessary based on the identification of specific risk factors or medical conditions requiring additional specialty monitoring and management. Prenatal care providers should follow AAP/ACOG's early and on-going pregnancy risk specific TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 recommendations for consultation3. Referrals for specialty provider consultations should include: i. description of the indication for the consult, ii. the role of the consultant during the initial consult iii. the role of the consultant during the followup care throughout the stages of pregnancy, and iv. the sharing of patient/clinical information between the primary care obstetrical provider and the special care consultant.4 B. Access to Care 1. Any pregnant woman who presents for prenatal care should begin receiving care as quickly as possible, preferably the same day. All prenatal care service providers must provide prenatal care services to recipients determined to be presumptively eligible for medical assistance but are not yet enrolled in Medicaid. 2. Prenatal care providers shall assist or refer women for assistance with application for medical assistance and managed care plan selection in accordance with procedures established by the Commissioner. 3. Prenatal care practices must provide or arrange for the provision of 24 hour/7 day week coverage (after hours and weekend/vacation number to call that leads to a person or message that can be returned by a health care professional within one hour). Pregnant women shall have access to unscheduled or emergency visits on a 24 hour basis5. 4. Prenatal care providers must develop systems, or arrange for reminder/call backs to patients needing continued or followup services, and for visits requiring follow-up for abnormal test results. Prenatal care providers shall outreach to patients to reschedule missed appointments in a manner that maintains patient confidentiality. 5. Prenatal care providers shall schedule prenatal care visits for an uncomplicated pregnancy consistent with AAP/ACOG recommendations. Pregnant women with medical, obstetrical and/or psychosocial problems may require more frequent visits. The need for increased surveillance is best determined by the prenatal care provider based on the individual needs of the woman, and the nature and severity of her problems. C. Prenatal Risk Assessment, Screening and Referral for Care Prenatal care (PNC) providers shall conduct a comprehensive prenatal care risk assessment for both maternal and fetal risks, at the earliest prenatal care visit, on all pregnant women. 1. The risk assessment shall include but not be limited to an analysis of individual characteristics affecting pregnancy, such as genetic, nutritional, environmental, behavioral health, psychosocial and history of previous and current obstetrical/fetal and medical/surgical risk factors. Historical TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 obstretric risk assessment shall include an evaluation of prior preterm birth, risk for recurrent preterm birth and eligibility for progesterone supplementation as per ACOG recommendations.6 Prenatal care providers are encouraged to use a standardized written risk assessment tool, such as the ACOG, Hollister or POPRAS form. Using established criteria for determining high risk pregnancies, the prenatal care provider shall determine the woman's risk status based on generally accepted standards of practice. The risk assessment shall be: a. reviewed at each visit; b. repeated formally early in the third trimester; c. used to form the basis for the development of the care plan and; d. documented clearly in the medical record. 2. Based on results of the risk assessment and the individual woman's increased risk for a poor pregnancy outcome, the prenatal care provider shall refer the pregnant woman for follow-up care. Referrals for such care may include but are not limited to: prenatal case management programs provided by managed care plans, other case management programs, home visitation agencies, or community-based programs for prenatal care coordination. 3. In accordance with Public Health Law section 2530-a 2.3. Prenatal care providers shall complete a standardized New York State Prenatal Care Risk Screening Form, which summarizes the results of the comprehensive risk assessment (as described in C.1.) for each new pregnancy. The completion of this risk screening form once during the pregnancy and reporting of the information shall be with the pregnant woman's informed written consent and shall be in a format to be developed by the Commissioner. If consent and voluntary participation is obtained, prenatal care providers shall complete the New York State Prenatal Care Risk Screening Form at the earliest prenatal care visit and transmit the information in a confidential manner to be determined by the Commissioner. D. Psychosocial Risk Assessment, Screening, Counseling And Referral For Care Prenatal care providers shall conduct a psychosocial risk assessment of all pregnant women during the first prenatal care visit. The assessment should be reviewed at each visit and formally repeated early in the third trimester and postpartum to identify important issues that may have developed over time. The assessment shall include a broad range of social, economic, psychological and emotional problems. Screening should include but not be limited to assessment of barriers to care, unstable housing, communication barriers (i.e. language and /or cultural barriers), nutrition, tobacco use, substance use, depression or other psychiatric illness, safety, domestic abuse, sexual abuse, and stress. Based on the results of this assessment the providers shall identify areas of concern, validate major issues with the patient, provide information, and if indicated, provide treatment or make appropriate referral(s). TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 The psychosocial risk assessment shall include but not be limited to screening for the following7 1. Tobacco Use-Prenatal care providers shall assess all pregnant women about their past and present use of tobacco and exposure to second hand smoke. All pregnant women should be advised to avoid or minimize time spent in the presence of tobacco smoke. The patient who smokes should be strongly advised to stop smoking and be provided with tailored counseling to assist in smoking cessation. Patients who smoke shall be offered a referral to an appropriate smoking cessation education and/or treatment program.8 2. Substance Use-Prenatal care providers shall assess all pregnant women about their past and present use of all substances, including drugs, alcohol, or the use of any prescription or nonprescription medications, including herbal supplements. The possible effects of any substances used before or during pregnancy should be discussed. A woman who acknowledges the use of any substances should be counseled about the implications of their use during pregnancy, and strongly encouraged to refrain from use of any substances that may negatively affect her or her fetus. If appropriate the woman should be offered a referral to a treatment program. 3. Domestic Violence-Prenatal care providers shall screen all pregnant women for domestic violence. Descriptions of domestic abuse from the patient should be documented in the patient's medical record, safety of the patient and family shall be ascertained and referrals made to appropriate counseling, legal and social-service advocacy programs. 4. Depression-Prenatal care providers shall screen pregnant and postpartum women for depression utilizing an appropriate screening tool, and should have a system in place to ensure that positive screening results are followed by accurate diagnosis, implementation of treatment, and follow-up either within the practice or through referral. Prenatal care providers should refer to information on maternal depression, including current evidence and guidelines, evidence-based screening tools and available follow-up support resources provided on the Department's website9 E. Nutritional Screening, Counseling and Referral for Care Prenatal care providers shall provide or arrange for the provision of nutritional and physical activity screening, counseling and referral which includes: 1. Individual nutritional risk assessment including an assessment of pre-pregnancy BMI, weight gain to date, if any, and specific nutritional risks at the initial prenatal care visit and continuing reassessments as needed; 2. Documentation of the nutritional assessment, risk status and the plan of care in the patient's medical record; 3. Referral of pregnant women identified as being at nutritional risk for specific nutritional counseling, monitoring and followup; TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 4. F. Health Education Attachment 3 Provision of basic nutrition education and counseling for each pregnant woman which includes: a. appropriate dietary intake and recommended dietary allowances during normal pregnancy; b. recording of height and weight at the initial prenatal visit to allow for the calculation of the BMI and sequential weight monitoring at each visit. Parameters of appropriate weight gain should be made based on the pre-pregnancy BMI categories recommended in the 2009 Institute of Medicine (IOM) guidelines 10 c. focused approach to nutrition counseling based on AAP/ACOG guidelines which includes exercise and lifestyle changes for all women, but particularly for women with a BMI in the obese (BMI>30) or underweight (BMI<18.5)11 range; and d. counseling and education regarding infant feeding choices discussed with the woman during prenatal visits and immediately postpartum. Prenatal care providers should support breast feeding by counseling the patient regarding the nutritional advantages of human breast milk and should provide her with information regarding the benefits of breast feeding for both the mother and infant. Exclusive breastfeeding is recommended for the first 6 months of life and should be continued along with supplemental foods through the second half of the first year of life and for as long as desired thereafter. Breastfeeding is not recommended for HIV positive women and may be medically contraindicated in other situations. Income eligible women considering breastfeeding should be referred to the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) for breastfeeding education and support. 5. Referral of pregnant women identified as needing to access proper nutrition and assistance in obtaining supplemental food to programs such as the Supplemental Nutritional Assistance Program (SNAP) or the Special Supplemental Nutrition Program for Women, Infants and Children (WIC). 6. Special considerations for underweight and/or overweight/obese women: a. Prenatal care providers shall assess and counsel underweight and overweight/obese women regarding the increased risk for pregnancy complications related to their weight and encourage these women to participate in a lifestyle improvement program, including diet, exercise, and behavior modification. b. Prenatal care providers shall consider screening obese patients for gestational diabetes upon presentation or in the first trimester, and repeat screening later in the pregnancy if results are initially negative 12. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 Prenatal care providers shall provide or arrange for the provision of health and childbirth education based on an assessment of the pregnant woman's individual needs. Prenatal care providers should focus on the pregnant woman's ability to comprehend the information and use materials appropriate to the educational, cultural and language needs of the patient as well as her gestational history. Such services shall be provided by professional staff, documented in the medical record and shall include but not be limited to the following: 1. Rights and responsibilities of the pregnant woman; 2. Signs and symptoms of complications of pregnancy; 3. Physical activity, exercise and recommended weight gain during pregnancy; 4. Avoidance of harmful behaviors including the use of alcohol, drugs, non-prescribed medications and nicotine; 5. Sexuality during pregnancy; 6. Occupational and environmental concerns including lead exposure; 7. Risks of HIV infection and risk reduction behaviors; 8. Signs of labor; 9. Labor and delivery process and availability of various delivery options; 10. Relaxation techniques in labor; 11. Obstetrical anesthesia and analgesia; 12. Preparation for parenting including infant development and care, options for feeding and the benefits of breast feeding; 13. Newborn screening program, including the distribution of newborn screening literature; 14. Family planning and optimum inter-pregnancy interval. G. Development of a Care Plan and Care Coordination Prenatal care providers shall develop a care plan jointly with each pregnant woman which addresses the problems identified as a result of the initial and ongoing risk assessments. The care plan shall describe the implementation and coordination of all services required by the pregnant woman, be routinely updated and implemented jointly by the pregnant woman, her family and the appropriate members of the health care team. 1. Care shall be coordinated to: a. Ensure that relevant information is exchanged between the prenatal care provider and other providers, health plan case managers or sites of care including the anticipated delivery site. b. Ensure that the pregnant woman and her family or other designated representative, with her consent, have continued access to information resources and are encouraged to participate in the decisions involving the care and services being provided. c. Encourage and assist the pregnant woman in obtaining necessary medical, dental, nutritional, psychosocial, drug and substance abuse services appropriate to her identified needs. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 2. 3. Attachment 3 d. Provide the pregnant woman with an opportunity to receive prenatal and postpartum home visitation when medical and/or psychosocial benefits may be derived from the visits. e. Provide to or refer the pregnant woman for needed services as identified in the risk assessment. f. Obtain special tests and services that may be recommended or required by the Commissioner of Health, when necessary to protect maternal and/or fetal health. Pregnant women shall be provided appropriate medical care, counseling and education based on test results. The prenatal care provider shall coordinate labor and delivery services by developing agreements with planned delivery sites which address, at a minimum, the following: a. a system for sharing prenatal medical records, including HIV test results; b. pre-booking of women for delivery by 36 weeks gestation for low risk pregnancies and by 24 weeks gestation for high risk pregnancies; c. scope of services; and d. sharing of delivery/birth outcome information. The prenatal care provider shall arrange for postpartum home visitation care as necessary and available when the mother and/or newborn may derive medical, physical and/or psychosocial benefits from such visits. H. Prenatal Care Services Prenatal care providers shall provide or make arrangements for the provision of comprehensive prenatal care services in accordance with generally accepted standards of professional practice, as outlined by the AAP and ACOG.13 1. Prenatal diagnostic and treatment services shall include but not be limited to the following: a. Comprehensive assessment - An initial comprehensive assessment including history, review of systems, and physical examination. b. Standard and special laboratory tests - Based on AAP/ACOG recommendations, standard and special laboratory tests and procedures should be performed at the recommended gestational age. c. Follow-up, evaluation of results and referral - Followup shall be conducted as indicated based on abnormal findings from the comprehensive assessment, results of preliminary abnormal laboratory test findings and repeat testing of women considered to be at high risk. Prenatal care providers shall discuss the following with the pregnant woman: i. findings from the comprehensive assessment, ii. results of all laboratory tests, iii. recommendations for additional testing, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 2. Attachment 3 iv. treatment options and obtaining informed consent for treatment, v. technological support and referrals as necessary. HIV Services a. Prenatal HIV Counseling and Testing Prenatal care providers shall provide HIV counseling to all pregnant women as early as possible in the pregnancy without regard to risk. Counseling shall be provided and informed consent obtained prior to HIV testing and shall be consistent with the requirements described in Article 27F of the Public Health Law and NYCRR Title 10 Section 63.3. A repeat third trimester test, preferably at 34 - 36 weeks should be routinely recommended to all pregnant women who tested negative early in prenatal care to identify seroconversion after an initial negative prenatal HIV test.14 The New York State Department of Health Informed Consent to Perform HIV Testing (DOH Form - 2556), allows the pregnant woman to receive counseling for both tests at the initial counseling and to sign for both tests at that time. The pregnant woman should be counseled about benefits to knowing her HIV status, specifically the significant reduction in risk of mother-to-child HIV transmission with the provision of antiretroviral (ARV) prophylaxis to HIV-positive women during pregnancy, at delivery and to the newborn. The pregnant woman should be informed that if she does not have a prenatal test, she will be HIV-counseled again when she presents for delivery, and that expedited testing will be done on her, with her consent, or on the newborn, without her consent. She should also be told that all newborns are routinely screened for HIV as part of the Newborn Screening Program, as a final safety net to identify exposed infants. Pregnant women who receive negative test results should be provided with their results and if at continued risk for developing HIV, encouraged to access HIV prevention programs and services appropriate to their risk(s). Pregnant women who receive positive HIV test results should be provided with post-test counseling consistent with Public TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 Health Law section 2781 and Part 63 regulations and will be provided necessary care and/or appropriate referrals for services.15 Prenatal care providers should transfer information regarding a prenatal patient's HIV counseling and testing status, including a copy of the result, if one exists, to the delivery setting. Routine consent procedures for the transfer of medical records are sufficient to authorize the transfer of HIV-related information to health care providers. b. Care of an HIV-Positive Pregnant Woman Management of antiretroviral (ARV) medications during pregnancy should be done by, or in consultation with, an experienced HIV specialist familiar with state and federal clinical guidelines for the care of HIV-positive pregnant women and the prevention of mother-to-child HIV transmission. Breastfeeding is not recommended for HIV-positive women where there are good alternatives. 3. Dental care The prenatal care provider shall conduct an assessment of the woman's oral health care needs at the first prenatal care visit. The assessment shall include but not be limited to interviewing the patient regarding current oral health problems, previous dental problems, and the availability of a dental provider. Pregnant women identified as having a current oral health problem or not having a dental visit in the past six months should be referred to a dentist as soon as possible, preferably before 20 weeks gestation. The prenatal care provider shall educate the pregnant woman about the importance of oral health and that dental care is safe during pregnancy. Oral health care should be coordinated between the prenatal care provider and the dentist.16 4. Immunizations Pregnancy is not an absolute contraindication to any vaccination. Some vaccines are strongly recommended for pregnant women during the prenatal period. Many women will not be up-to-date and each pregnant woman should be evaluated for immunization status. Prenatal care providers should reference current guidelines for immunizations and be TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 alert for updated recommendations. Guides for immunizing during and after pregnancy are available from the Centers for Disease Control and Prevention (CDC)17 and the New York State Department of Health Bureau of Immunization.18 a. All pregnant women shall be evaluated for serologic evidence of immunity to rubella at their first prenatal visit, unless known to be immune by documentation of a previous test. Varicella immunity shall also be assessed by either a reliable history of disease, laboratory evidence of previous disease or documented receipt of two doses of vaccine. b. Influenza vaccine is strongly recommended for all pregnant women due to the increased risk of influenza-related complications among pregnant women. Providers should advocate for influenza vaccination and provide the influenza vaccine to their pregnant patients.19Pregnant women should only receive the trivalent inactivated influenza vaccine (TIV), and not the live attenuated influenza vaccine (LAIV), the nasal spray. c. The following immunizations are recommended for women at risk for these diseases and who do not have a history of immunity: i. Hepatitis B - A pregnant woman's risk of acquiring Hepatitis B Virus (HBV) should be assessed along with her risk of acquiring other sexually-transmitted infections. Pregnant women who have been identified as being at risk for HBV infection should be vaccinated. Pregnancy is not a contraindication for HBV vaccination, and limited evidence does not suggest any fetal harm from the HBV vaccine. ii. Tetanus, Diphtheria/Tetanus, Diphtheria, Pertussis booster (Td/Tdap) - Pregnant women who have not received a Td booster within the last 10 years and require immediate protection against tetanus and diphtheria (ie. wound prophylaxis) should be vaccinated with Td based on the severity of the risk of tetanus and the need to be immunized. Immunization with Td during pregnancy is preferred in the 2nd or 3rd trimester. iii. Due to the burden of pertussis disease in vulnerable newborns, pregnant women should receive a dose of Tdap during each pregnancy, regardless of prior immunization history, optimally between 27 weeks and 36 weeks gestation. Tdap may be given at any time during pregnancy and there is no evidence of adverse fetal effects from administrating inactivated viral or bacterial vaccines or toxoids during pregnancy.20 For women who have not previously received TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 Tdap, if Tdap was not administered during pregnancy, Tdap should be administered immediately postpartum. By providing Tdap vaccine to women during pregnancy, infants will gain pertussis antibodies during the time they are most vulnerable-before three months of age. The infant's immune response to DTap may not be as strong; however, based on a recent study looking at this issue, this interference does not seem to cause any problems when it comes to protecting infants.21 Researchers are still working to better understand this issue. The benefits of vaccinating during pregnancy and protecting a newborn during the most vulnerable time outweigh the potential risk of blunting an infant's response to DTaP vaccine.22 d. e. Other pregnancy related immunization issues: i. New York State Public Health Law 2500-e requires that every pregnant woman be tested for the presence of hepatitis B surface antigen (HBsAg) and that the test results and the date are documented in the prenatal record. It also requires that infants of women who are hepatitis B surface antigen positive or whose test results are unknown receive treatment at birth with hepatitis B vaccine and hepatitis B immunoglobulin (HBIG). ii. New York State Public Health Law 2112 (effective July 1, 2008) prohibits the administration of vaccines containing more than trace amounts of thimerosal, a mercury-containing preservative, to pregnant women, unless the supply is insufficient. There is no evidence that thimerosal causes harm to the pregnant woman or her fetus. Postpartum Period - The following vaccinations or a history of immunity are recommended for all postpartum women: influenza, MMR (measles, mumps, rubella), Tdap, varicella and human papilloma virus. An adult schedule should be checked for appropriate indications in regard to age, previous history of disease or prior history of vaccination. 23 Women who plan to breastfeed can and should receive vaccinations as no evidence exists of any risk to a mother or her infant if she is vaccinated while breastfeeding. Breastfeeding is not a contraindication to any vaccination, with the exception of vaccinia vaccine. 5. Lead Poisoning Prevention, Testing and Management TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 As required by NYS Public Health Law and Regulations (NYCRR Subpart 67-1.5), prenatal health care providers shall provide all pregnant women with anticipatory guidance on preventing lead poisoning, information on the major sources of lead and the means to prevent exposure. At the initial prenatal visit, each pregnant woman shall be assessed for exposure to lead by using a risk assessment questionnaire recommended by the State Commissioner of Health.24 If the pregnant woman responds "yes" to even one of the questions, she is considered to be at risk, and should have a blood lead test and be counseled on how to eliminate lead exposure. Pregnant women found to have a confirmed blood lead level of 10 micrograms per deciliter (mcg/dL) or greater should be provided with risk reduction counseling and followup testing in accordance with NYS Department of Health guidelines. In addition, all pregnant women with a confirmed blood lead level of 10 mcg/dL or greater who may have been occupationally exposed to lead should be referred to an occupational health clinic for individual guidance. All women should receive anticipatory guidance on the prevention of childhood lead poisoning at their postpartum visits. Consultation for medical management of a lead poisoned pregnant woman is available from the Regional Lead Resource Centers (RLRC).25 Prenatal care providers are required to adhere to the most current New York State Department of Health guidelines for the prevention, identification and management of lead poisoning in pregnancy, as described in Lead Poisoning Prevention Guidelines for Prenatal Care Providers - NYSDOH & ACOG District II, June, 2009.26 6. Use of Ultrasound Prenatal care providers must document the medical indication for performing an ultrasound examination of a pregnant patient based on identified need. Ultrasound for gestational dating is recommended, especially before 20 weeks, if there is a size-date discrepancy or imprecise menstrual dates.27Ultrasonography shall be provided only by physicians or technologists who have undergone training and only when there is a valid medical indication for the examination documented in the woman's medical record by a qualified prenatal care provider.28 AAP/ACOG guidelines should be followed when recommending an ultrasound exam. Common indications for ultrasound include but are not TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 limited to evaluation for gestational age; fetal number, viability, placenta location, abnormal amniotic fluid volume, fetal growth disturbances, fetal anomolies and aneuploidy screening.29 7. Screening for Genetic Disorders Prenatal care providers shall offer all pregnant women additional maternal/fetal screenings to identify fetal abnormalities/genetic problems as follows: 8. a. Birth defects - Prenatal care providers shall offer all pregnant women screening tests to identify birth defects at specific times throughout the prenatal period based on AAP/ACOG recommendations. b. invasive diagnostic testing for aneuploidy should be available to all women regardless of maternal age. Early amniocentesis (at less than 15 weeks gestation) should not be performed.30 c. Pregnant women should be counseled regarding the differences between screening and invasive diagnostic testing for aneuploidy including a discussion of the risks and benefits of the invasive test compared with other available screening tests. Pregnant women who choose not to undergo invasive diagnostic testing for aneuploidy shall be offered aneuploidy screening before 20 weeks gestation regardless of maternal age.31 d. Prenatal care providers should offer information on cystic fibrosis screening to all couples and cystic fibrosis carrier screening should be offered to all couples regardless of race or ethnicity.32 e. Prenatal genetic screening or diagnosis should be offered to pregnant women based on personal and family history. Genetic screening and counseling criteria should be based on AAP/ACOG recommendations. This includes screening for genetic disorders based on racial and ethnic background, such as hemoglobinopathies (sickle cell, αthalassemia, β-thalassemia), Tay-Sachs disease, Canavans disease and familial dysautonomia, cystic fibrosis and other genetic disorders based on family history.33 Fetal Well- Being Tests of fetal well- being are indicated in the presence of specific maternal and pregnancy-related conditions and shall be performed based on the judgment of a qualified prenatal care provider according to individual patient need.34 There are several tests used in clinical practice to assess fetal status, each test has advantages, disadvantages as well as risks. The prenatal care provider, based on clinical judgment TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3 and recommended AAP/ACOG guidelines should choose the test that best meets the needs of the pregnant woman and her fetus and initiate testing at the appropriate gestational age. The test results and the interpretation shall be discussed with the pregnant woman, documented in the medical record and appropriate referrals initiated as soon as possible. I. Postpartum Services The prenatal care provider shall schedule a postpartum visit based on the woman's identified needs and in accordance with AAP/ACOG's recommended schedule, (approximately 4 - 6 weeks after delivery but no later than eight weeks after delivery; women with a complicated gestation or delivery by cesarean section should have a visit scheduled within 7 - 14 days of delivery). The visit should include an interval history and a physical examination to evaluate the patient's current status and her adaptation to the newborn. 1. The visit shall include but not be limited to the following: a. identify whether any medical, dental, psychosocial (including depression), nutritional (including breastfeeding), tobacco/smoking cessation needs, alcohol and drug treatment needs of the mother or infant are being met; b. provide anticipatory guidance on the prevention of childhood lead poisoning; c. refer the mother or other infant caregiver to resources available for meeting identified needs and provide assistance in meeting such needs where appropriate; d. assess family planning/contraceptive needs and provide advice and services or referral when indicated; e. provide appropriate inter-conception counseling including information such as recommended preconception daily intake of folic acid (400 mcg) as per CDC and ACOG guidelines and encourage a preconception visit prior to subsequent pregnancies; f. refer the infant to preventive and special care services appropriate to his/her needs; g. advise the mother/caregiver of the availability of Medicaid eligibility for infants; and h. advise or refer the mother for assistance with an application for on-going medical care assistance for herself, in accordance with her financial status, health assistance program eligibility and the policies and procedures established by the Commissioner of Health and the State of New York. i. recommend that overweight/obese women continue a nutrition and exercise regimen after pregnancy to encourage weight loss before attempting another pregnancy.35 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 3 STANDARDS OF CARE/PERFORMANCE EVALUATION STANDARDS FOR MEDICAL RECORDS To ensure complete, quality documentation of patient records, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has established the following standards for medical records: • • • • • • • • • • • • • • • • • • • • Patient identification must be contained on each page of the record (Name, DOB, ID) Provider signature and professional title must be identified on each entry. All entries in the record must be dated Personal biographical data including address, employer, home and work telephone numbers, and marital status must be included in the medical record. The medical record must be legible Past medical history must be contained within the medical record The record will contain a family history An ongoing problem list must be maintained to monitor a member’s health status Allergies and/or adverse reactions must be clearly and easily identified on the record, or NKA must be noted The record for members 12 and older must contain documentation of screening and counseling for: Tobacco Alcohol Drugs/Substances HIV The record will contain pertinent history and physical information, i.e. appropriate subjective and objective information relevant to the patient’s presenting complaints. Laboratory and other studies will be ordered according to established guidelines Working diagnoses must be consistent with findings Plans of action and treatment must be consistent with finding The care delivered must be medically appropriate Problems from previous visits must be addressed A date of return or follow-up plan for each encounter must be done Use of specialists according to established guidelines Lab work, special studies, hospitalizations, emergency room, outpatient surgery/procedure and consult summaries will be in the record and initialed by member’s PCP or addressed upon review in progress notes The record will demonstrate evidence of continuity and coordination of care between primary and specialty providers Evidence that preventive screening and services are offered according to established guidelines Revised January Section 3 Page 1 • • • • • • • Immunization records will be complete and current. Refusal of immunizations by reason of genuine and sincere religious beliefs or medical contradictions should be clearly documented Documentation that information on the Patient Self-Determination Act has been provided to the member and that competent consenting adults (including a person who is under 18 years of age who is either married or has a child) either have or have not executed an oral or written Advance Directive Timely screening for STD’s will be documented Education about risk and prevention of STD’s will be documented Reporting of STD’s to the County Health Department Lead levels of 20 micrograms or above must be reported to the local County Health Departments and will be documented Screening for HIV per NYS Guidelines Each enrollee should have a separate medical record and the record should verify that the PCP coordinates and manages care. In addition, the OB record must include all relevant information that may impact a pregnancy (See Medicaid Prenatal Guidelines, Attachment 3). The MEDICAL RECORD REVIEW As part of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Quality Improvement Program (See Section 6), a review of medical records and clinical documentation will be done to evaluate compliance with minimum standards for medical record documentation and maintenance. Periodically, a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN representative will schedule visits with the provider's office to review the medical records of members or they will request copies of records. All participating providers are expected to comply with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s requirements for access to medical records, with reasonable notice, during the term and upon termination of the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Provider Agreement, including but not limited to: • Parties who should have access to records: TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN representatives or their delegates (for UR or QA), TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN physician(s), any duly authorized third party. This would include: NYSDOH by CMS and the LDSS • Maintenance period: A minimum of six (6) years from the date of service, six (6) years past the majority of the patient or cession of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN operation and/or any time thereafter that such access is required in Revised January 2015 Section 3 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL connection with a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN covered person’s medical care. • • Revised January 2015 Copies: TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is entitled to obtain copies of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN member’s medical records without charge to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or the member. Other disclosure: Participating providers are required to disclose medical records as required by law. This extends to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN members. Section 3 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 4 UTILIZATION MANAGEMENT AND CASE MANAGEMENT PREAUTHORIZATION TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has a system for Precertification of designated services. When calling the Utilization Management Department for Precertification, the physician’s office should have the following information available (as applicable): • • • • • • • • • PCP’s name Patient’s name, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN ID number, and date of birth Reason for authorization or need for service Admitting physician’s name Facility/Provider, address, and telephone number Anticipated length of stay Number of visits Diagnosis and procedure (including CPT-4 and ICD-9 codes) Member Specific clinical information Pre Certifications are required for the following Services: • • • • • • • • • • • All Inpatient admissions to hospitals and facilities (includes maternity, NICU, skilled nursing, hospice, birthing centers, rehabilitation facilities; Inpatient Mental Health and/or Chemical Dependency Services;) Home care, including home infusion services and physical therapy performed in the home Private duty nursing Long term support services including personal care services, consumer directed personal assistance and adult day care Referrals to non-participating Providers Sleep Studies Genetic testing CPAP/BIPAP/Oxygen/TENS Units DME with Purchase Price allowance >$500* Certain surgeries not performed in the doctor’s office** Specific Radiology Procedures (MRI, Selected CT Scans and Nuclear Medicine Studies )** *See fee schedule at https://www.emedny.org/ProviderManuals/DME/index.aspx click on Fee Schedule **See attached listing of outpatient surgeries not requiring preauthorization and Radiology Procedures requiring an auth. List and Prior Authorization form can also be found at http://www.totalcareny.com/documents/177.pdf Revised January 2015 Section 4 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Surgery No Prior Authorization Required 1/1/2015 CPT Description ADENOIDECTOMY/ TONSILLECTOMY & ADENOIDECTOMY AMPUTATION CPT Code Range 42820, 42821, 42830;42831;42835;42836 ANY AMPUTATION CPT CODE ARTERIOVENOUS ANASTOMOSIS FOR DIALYSIS ARTHROCENTESIS/ASPIRATION AND OR INJECTION, MAJOR JOINT OR BURSA BIOPSY (ANY TYPE) BRONCHOSCOPY CATARACT REMOVAL, INSERTION OF LENS 66920, 66982-66984, 66830, 66840, 66850, 66852, 66930, 66940 CERUMEN REMOVAL 69210 CIRCUMCISION 54150, 54160, 54161 COLONOSCOPY (ANY TYPE),INCLUDING SIGMOIDOSCOPY 45330,45378;45380;45384,45385-45392 CERVICAL CERCLAGE 57000, 59320, 59325, 59871 COLPOSCOPY OF CERVIX (INCLUDING LEEP AND ECC) 57452-57461;57505, 57520,57522 CYSTOURETHROSCOPY 52000 DILITATION OF THE ESOPHAGUS 43450 36821 20610 ANY BIOPSY CPT CODE 31622-31656 ESOPHAGOSCOPY EXCISION/INCISION OF LINGUAL FRENULUM 43200 41010;41115 EXCISION OF CYST, BREAST 19000;19001;19020;19030;19120; 19125;19126 MC_CO_SURPR_1214_12/29/2014 Revised January 2015 Section 4 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL MC_CO_SURPR_1214_12/29/2014 Surgery No Prior Authorization Required 1/1/2015 MC_CO_SURPR_1214_12/29/2014 EXCISION OF HEMORRHOID 46260,46261,46262,46250,46221,4694546946,46255,46257-46258 EXCISION OF PILIONIDAL CYST 11770-11772 EXCISION OF VARICOCELE OR LIGATION OF SPERM VEINS EYE REMOVAL HERNIA REPAIR (UMBILICAL,INGUINAL, VENTRAL/INCISIONAL ) 55530 HYPOSPADIUS AND/OR CHORDEE REPAIR INCISION AND DRAINAGE INJECTION PROCEDURE FOR CYSTOGRAPHY WITH VOIDING CYSTOGRAPHY KNEE ARTHROSCOPY DEBRIDEMENT/SHAVING (CHONDROPLASTY) KNEE ARTHROSOCPY WITH MENISCECTOMY 65091,65093,65101,65103,65105,65110,65112,65114 49491-49525,49580-49587,49560-49566,4956049566,49570,49652 54300,54304,54308,543412,54316,54318,54322,54324, 54326,54328,54332,54336,54340,54344,54348,54352,54360, 54380,54385,54390 10060-10180 51600 29877 29870,29873,29875;29880,29881-29887, 29888 LAPAROSCOPIC CHOLECYSTECTOMY 47562-47570 LARYNGOSCOPY (ANY TYPE) 31505,31510,31511,31512,31513,31515, 31520,31525,31526,31527, 31528,31529,31530,31531,31535,31536, 31540,31541,31545,31546, 31560,31561,31570,31571,31575,31576, 31577,31578 LUMBAR PUNCTURE;DIAGNOSTIC OR THERAPEUTIC 62270, 62272 MEATOTOMY 53025,52285,53020 NASAL CAUTERIZATION 30901,30903,30905,30906 MC_CO_SURPR_1214_12/29/2014 Revised January 2015 Section 4 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL RADIOLOGY PROCEDURES AUTHORIZATION REQUIRED 1/1/2015 NEUROLYSIS ULNAR NERVE NEUROPLASTY MEDIAN NERVE CARPAL OR ULNAR Open reduction internal fixation ORIF (ANY TYPE) ORCHIECTOMY PARACENTESIS 64718 29848;64721 ANY ORIF CPT CODE 54520,54690,54522,54535,54530 49080-49082 PORT PLACEMENT/EVALUATION,REMOVAL 36570-36571; 36576;36578;36590;36598 PREOPERATIVE PLACEMENT OF NEEDLE LOCALIZATION WIRE; PERCUTANEOUS, DURING BREAST BIOPSY 19290-19295 PROBING OF NASOLACRIMAL DUCT 68810-68840 REMOVAL OF IMPLANT; (WIRE, PIN, SCREW, ROD/PLATE) 20670; 20680 REMOVAL OF CV CATHETER W/O PORT/PUMP 36589 STRABISMUS REPAIR (PEDIATRIC) 67311;67312;67314;67316;67348;67320;67332; 67334;67335;67340;67343 TAMIS PROCEDURE (TRANSANAL MINIMALLY INVASIVE SURGERY) TONSILLECTOMY, PRIMARY OR SECONDARY TRANSFUSION, BLOOD OR BLOOD COMPONENTS TRIGGER FINGER RELEASE TUBAL LIGATION 45171 42825; 42826 36430 26055 58565, 58600-58615; 58670, 58671 TYMPANOSTOMY/MYRINGOTOMY 69420-69450, 69610,69631 TERMINATION OF PREGNANCY UPPER ENDOSCOPY DIAGNOSTIC OR WITH BIOPSY 59840 59841 59850 59851 59852 59855 59856 43235; 43236; 43237; 43238; 43239; 43240; 43241; 4324243259 URETERAL STENT PLACEMENT 52332 67005,57010,67108,67112-67113,67036-67043,6703967040,67039,67027,66852 VITRECTOMY Revised January 2015 Section 4 Page 4 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL RADIOLOGY PROCEDURES AUTHORIZATION REQUIRED 1/1/2015 CPT Description 70496 CTA HEAD WITH CONTRAST 70498 CTA OF THE NECK WITH CONTRAST 70540 MRI ORBIT FACE AND NECK WITHOUT CONTRAST 70542 MRI ORBIT FACE AND NECK WITH CONTRAST 70543 MRI ORBIT FACE AND NECK WITHOUT CONTRAST; FOLLOWED BY WITH CONTRAST 70544 MRA HEAD WITHOUT CONTRAST 70545 MRA HEAD WITH CONTRAST 70546 MRA HEAD WITH AND WITHOUT CONTRAST 70547 MRA NECK WITHOUT CONTRAST 70549 MRA NECK WITH AND WITHOUT CONTRAST 70551 MRI BRAIN (INCLUDING BRAIN STEM); WITHOUT CONTRAST 70552 MRI BRAIN (INCLUDING BRAIN STEM); WITH CONTRAST 70553 MRI BRAIN (INCLUDING BRAIN STEM) 71275 CT ANGIOGRAPHY CHEST; NON-CORONARY 71551 MRI CHEST WITH CONTRAST 71552 MRI CHEST WITH OR WITHOUT CONTRAST 71555 MRA CHEST; WITH OR WITHOUT CONTRAST 72141 MRI CERVICAL SPINE WITHOUT CONTRAST 72142 MRI CERVICAL SPINE WITH CONTRAST 72146 MRI THORACIC SPINE WITHOUT CONTRAST 72147 MRI THORACIC SPINE WITH CONTRAST 72148 MRI LUMBAR SPINE WITHOUT CONTRAST 72149 MRI LUMBAR SPINE WITH CONTRAST 72156 MRI CERVICAL SPINE WITH AND WITHOUT CONTRAST 72157 MRI THORACIC SPINE WITH AND WITHOUT CONTRAST 72158 MRI LUMBAR SPINE WITH AND WITHOUT CONTRAST 72159 MRA SPINAL CANAL AND CONTENTS MC_CO_RADPR_1214_12/29/2014 Revised January 2015 Section 4 Page 5 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL RADIOLOGY PROCEDURES AUTHORIZATION REQUIRED 1/1/2015 72191 CTA PELVIS WITH CONTRAST 72195 MRI PELVIS WITHOUT CONTRAST 72196 MRI PELVIS WITH CONTRAST 72197 MRI PELVIS; WITH AND WITHOUT CONTRAST 72198 MRA PELVIS 73206 CTA UPPER EXTREMITY WITH CONTRAST 73218 MRI UPPER EXTREMITY OTHER THAN JOINT WITHOUT CONTRAST 73219 MRI UPPER EXTREMITY OTHER THAN JOINT WITH CONTRAST 73220 MRI UPPER EXTREMITY OTHER THAN JOINT; WITH AND WITHOUT CONTRAST 73221 MRI UPPER EXTREMITY JOINT WITHOUT CONTRAST 73222 MRI UPPER EXTREMITY JOINT WITH CONTRAST 73223 MRI UPPER EXTREMITY JOINT WITH AND WITHOUT CONTRAST 73225 MRA UPPER EXTREMITY 73706 CTA LOWERE EXTREMITY WITH CONTRAST 73718 MRI LOWER EXTREMITY OTHER THAN JOINT; WITHOUT CONTRAST 73719 MRI LOWER EXTREMITY OTHER THAN JOINT; WITH CONTRAST 73720 MRI LOWER EXTREMITY OTHER THAN JOINT WITH AND WITHOUT CONTRAST 73721 MRI LOWER EXTREMITY JOINT WITHOUT CONTRAST 73722 MRI LOWER EXTREMITY JOINT WITH CONTRAST 73723 MRI LOWER EXTREMITY JOINT WITH AND WITHOUT CONTRAST 73725 MRA UPPER EXTREMITY 74175 CTA OF THE ABDOMEN WITH CONTRAST 74181 MRI ABDOMEN WITHOUT CONTRAST 74182 MRI ABDOMEN WITH CONTRAST 74183 MRI ABDOMEN WITH AND WITHOUT CONTRAST 74185 MRA ABDOMEN 74740 HYSTEROSALPINGOGRAM 75557 CARDIAC MRI FOR MORPHOLOGY AND FUNCTION W/O CONTRAST MC_CO_RADPR_1214_12/29/2014 Revised January 2015 Section 4 Page 6 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL RADIOLOGY PROCEDURES AUTHORIZATION REQUIRED 1/1/2015 76377 CARDIAC MRI FOR MORPHOLOGY AND FUNCTION W/O CONTRAST; WITH FLOW/VELOCITY QUANTIFICATION CARDIAC MRI FOR MORPHOLOGY AND FUNCTION W/O CONTRAST; WITH STRESS IMAGING CARDIAC MRI FOR MORPHOLOGY AND FUNCTION W/O CONTRAST; WITH FLOW/VELOCITY QUANTIFICATION AND STRESS CARDIAC MRI FOR MORPHOLOGY AND FUNCTION W/O CONTRAST MATERIAL FOLLOWED BY CONTRAST MATERIAL AND FURTHER SEQUENCES CARDIAC MRI FOR MORPHOLOGY AND FUNCTION W/O CONTRAST MATERIAL FOLLOWED BY CONTRAST MATERIAL AND FURTHER SEQUENCES; WITH FLOW /VELOCITY QUANTIFICATION CARDIAC MRI FOR MORPHOLOGY AND FUNCTION W/O CONTRAST MATERIAL FOLLOWED BY CONTRAST MATERIAL AND FURTHER SEQUENCES; WITH STRESS IMAGING CARDIAC MRI FOR MORPHOLOGY AND FUNCTION W/O CONTRAST MATERIAL FOLLOWED BY CONTRAST MATERIAL AND FURTHER SEQUENCES; WITH FLOW/VELOCITY QUANTIFICATION AND STRESS CTA ABDOMINAL AORTA AND BILAT. ILIOFEMORAL LOWER EXTREMITY RUNOFF WITH CONTRAST 3D RENDERING WITH INTERPRETATION AND REPORTING OF COMPUTED TOMOGRAPHY, MRI, ULTRASOUND OR OTHER TOMOGRAPHIC MODALITY; NOT REQUIRING IMAGE POST PROCESSING ON AN INDEPENDENT WORKSTATION. 3D RENDERING WITH INTERACTION AND REPORTING OF COMPUTED TOMOGRAPHY, MRI, ULTRASOUND OR OTHER TOMOGRAPHIC MODALITY; REQUIRING IMAGE POST PROCESSING ON AN INDEPENDENT WORKSTATION. 76496 CARDIAC BLOOD POOL IMAGING, SINGLE AT REST 76497 UNLISTED COMPUTED TOMOGRAPHY PROCEDURE 76498 UNLISTED MRI PROCEDURE 77058 MRI BREAST UNILATERAL 77059 MRI BREAST BILATERAL 78451 MYOCARDIAL SPECT SINGLE STUDY AT REST 78452 MYOCARDIAL SPECT MULTIPLE STUDIES 78453 MYOCARDIAL PERFUSION PLANAR 1 STUDY REST/STRESS 78454 78459 MYOCARDIAL PERFUSION PLANAR MULTIPLE STUDIES MYOCARDIAL IMAGING, POSITRON EMISSION TOMOGRAPHY (PET) METABOLIC EVALUATION 78481 CARDIAC BLOOD POOL IMAGING (PLANAR) FIRST PASS TECHNIQUE SINGLE STUDY, AT REST OR WITH STRESS; PLUS EJECTION FRACTION 78483 CARDIAC BLOOD POOL IMAGING; MULTI 75558 75559 75560 75561 75562 75563 75564 75635 76376 MC_CO_RADPR_1214_12/29/2014 Revised January 2015 Section 4 Page 7 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL MC_CO_RADPR_1214_12/29/2014 RADIOLOGY PROCEDURES AUTHORIZATION REQUIRED 1/1/2015 78492 MYOCARDIAL IMAGING, POSITRON EMISSION TOMOGRAPHY (PET), PERFUSION; SINGLE STUDY AT REST OR STRESS MYOCARDIAL IMAGING, POSITRON EMISSION TOMOGRAPHY (PET), PERFUSION; MULTIPLE STUDIES AT REST OR STRESS 78494 CARDIAC BLOOD POOL IMAGING, SPECT 78496 CARDIAC BLOOD POOL IMAGING-SINGLE STUDY 78608 BRAIN IMAGING, POSITRON EMISSION TOMOGRAPHY (PET) METABOLIC EVALUATION 78609 78812 BRAIN IMAGING, POSITRON EMISSION TOMOGRAPHY (PET) PERFUSION EVALUATION TUMOR IMAGING, POSITRON EMISSION TOMOGRAPHY (PET); LIMITED AREA (EG, CHEST, HEAD/NECK) TUMOR IMAGING, POSITRON EMISSION TOMOGRAPHY (PET); SKULL BASE TO MID THIGH 78813 TUMOR IMAGING, POSITRON EMISSION TOMOGRAPHY (PET); WHOLE BODY 78814 TUMOR IMAGING, POSITRON EMISSION TOMOGRAPHY (PET) WITH CONCURRENTLY ACQUIRED COMPUTER TOMOGRAPHY (CT) FOR ATTENUATION CORRECTION AND ANATOMICAL LOCALIZATION; LIMITED AREA (EG CHEST, HEAD/NECK) 78491 78811 78816 TUMOR IMAGING, POSITRON EMISSION TOMOGRAPHY (PET) WITH CONCURRENTLY ACQUIRED COMPUTER TOMOGRAPHY (CT) FOR ATTENUATION CORRECTION AND ANATOMICAL LOCALIZATION; SKULL BASE TO MID THIGH TUMOR IMAGING, POSITRON EMISSION TOMOGRAPHY (PET) WITH CONCURRENTLY ACQUIRED COMPUTER TOMOGRAPHY (CT) FOR ATTENUATION CORRECTION AND ANATOMICAL LOCALIZATION; WHOLE BODY 91035 PH PROBE - PH ELECTRODE PLACEMENT WITH MUCOSAL ATTATCHED TELEMETRY 0066T VIRTUAL COLONOSCOPY - SCREENING 0067T VIRTUAL COLONSOCOPY - DIAGNOSTIC CTA HEART WITHOUT CONTRAST INCLUDING POSTPROCESSING AND QUANTITATIVE EVAL. OF CORONARY CALCIUM 78815 0144T 0145T 0147T COMPUTED TOMOGRAPHY, HEART WITH CONTRAST MATERIAL CT ANGIOGRAPHY OF CORONARY ARTERIES; WITHOUT QUANTITATIVE EVALUATION OF CORONARY CALCIUM CT ANGIOGRAPHY OF CORONARY ARTERIES; WITH QUANTITATIVE EVALUATION OF CORONARY CALCIUM 0148T CARDIAC STRUCTURE AND MORPHOLOGY AND CT ANGIOGRAPHY OF CORONARY ARTERIES; WITHOUT QUANTITATIVE EVALUATION OF CORONARY CALCIUM 0149T CARDIAC STRUCTURE AND MORPHOLOGY AND CT ANGIOGRAPHY OF CORONARY ARTERIES WITH QUANTITATIVE EVALUATION OF CORONARY CALCIUM 0150T CARDIAC STRUCTURE / MORPHOLOGY FOR CHD 0146T MC_CO_RADPR_1214_12/29/2014 Revised January 2015 Section 4 Page 8 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL RADIOLOGY PROCEDURES AUTHORIZATION REQUIRED 1/1/2015 0151T CT HEART WITH CONTRAST MATERIAL, INCLUDING NON CONTRAST IMAGES, IF PERFORMED, CARDIAC GATING AND 3D IMAGE POST PROCESSING, FUNCTION EVALUATION S8085 FLUORINE-18 FLUORODEOXYGLUCOSE (F-18 FDG) IMAGING USING DUAL-HEAD COINCIDENCE DETECTION SYSTEM (NON DEDICATED PET SCAN) G0219 PET IMAGING WHOLE BONE; MELANOMA FOR NON COVERED INDICATIONS G0235 PET IMAGING ANY SITE NOT OTHERWISE SPECIFIED PET IMAGING, FULL AND PARTIAL-RING PET SCANNERS ONLY, FOR INITIAL DIAGNOSIS OF BREAST CANCER AND/OR SURGICAL PLANNING FOR BREAST CANCER (E.G. INITIAL STAGING OF AXILLARY LYMPH NODES) G0252 MC_CO_RADPR_1214_12/29/2014 Revised January 2015 Section 4 Page 9 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Prior Authorization Request Form This form and any supporting clinical information (office notes, Laboratory and Radiology Reports, Brief Medical History, or Treatment Plan) must be faxed to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Utilization Review Department BEFORE services are rendered. Fax Numbers 315-425-5502 OR 315-234-5928 For Emergent Requests, please call the Utilization Review Department at 1-800-223-7242 Member Last Name Date of Birth / Member First Name / ID# Requesting Physician Address Office Contact Name Fax Number ( Phone Number ( ) ) Referred to Provider Name Address Phone Number ( ) Fax Number ( ) Diagnosis ICD-9 Codes CPT Codes Services Requested This form can also be found on the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN website at totalcareny.com Revised January 2015 Section 4 Page 10 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL NOTIFICATION METHODS UTILIZATION DECISIONS AND TIME FRAMES OF Upon receipt of necessary information for a Utilization Management (UM) decision to be made, the following timeframes and methods will be followed by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN: A. Pre-authorization TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must make decision and notify enrollee/ enrollee designee and provider, by phone and in writing, within 3 business days of receipt of necessary information. Enrollee/enrollee designee notification may be delegated to the provider by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN via this manual. B. Concurrent TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must make decision and notify enrollee/enrollee designee and provider by phone and writing within 1 business day of receipt of necessary information. (Note: this requirement may be satisfied by notice to the provider, by telephone and in writing, within one (1) business day of receipt of necessary information). C. Retrospective TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must make decision within 30 days of receipt of necessary information. Revised January 2015 Section 4 Page 11 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL EMERGENCY SERVICES Emergency services are not subject to prior approval. EMERGENCY ADMISSIONS TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Utilization Management Department must be contacted by telephone as soon as possible regarding emergency inpatient hospital admissions and/or maternity admissions of a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN enrollee at (877) 872-4716. Either the admitting physician or the hospital makes contact. If the admission occurs after TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s normal business hours of 8:00 a.m. through 5:00 p.m. Monday through Thursday, 9:00 a.m. through 5:00 p.m. Friday, contact must be made as soon as possible the first normal business day. Revised January 2015 Section 4 Page 12 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL REFERRALS ARE VALID FOR 90 DAYS FROM THE DATE REFERRED UNLESS OTHERWISE NOTED ON THE REFERRAL FORM. Precertification is not required for the following services: • • • • • • • • • • Emergency Care. Emergency services are not subject to referral or prior approval. An emergency is a medical or behavioral condition, the onset of which is sudden, that manifests itself by symptoms of sufficient severity, including severe pain, that a prudent layperson possessing an average knowledge of medicine and health, could reasonably expect the absence of immediate medical attention to result: 1) in placing the health of the person afflicted with such condition in serious jeopardy, or in the case of a behavioral condition, placing the health of the person or others in jeopardy or 2) serious impairment to such person’s bodily functions or 3) serious dysfunction of any bodily organ or part of such person, or serious disfigurement of such person. Laboratory and radiology services. Exams of well newborns in hospital performed by pediatrician Routine vision exams, eyeglass lenses and frames issued by participating provider GYN services by a participating provider. Referrals are never required for OB/GYN services and are unlimited Family planning and reproductive health services provided by a participating or Medicaid provider Prenatal and postpartum services by a participating provider HIV counseling and testing services by participating or non-participating provider One (1) mental health and one (1) alcohol/substance abuse assessment from an in-plan provider during a 12 month period initiated by selfreferral of Medicaid enrollee (excludes Child Health Plus Enrollees) Members may self-refer to Counties for TB testing and treatment STANDING REFERRALS In order to provide continuity of services, a standing referral may be utilized for an enrollee with a condition requiring on going care from a specialist (such as cardiology, oncology) or an enrollee with a life threatening condition or disease. . • Requests for standing referrals must be submitted either verbally or in writing by enrollee or designee to the Utilization Management Department (UM) • A review of the case by the Medical Director in consultation with the Primary Care Provider and a specialist in the same field will determine whether a standing referral is appropriate. • If the review determines that the request is appropriate, a treatment plan will be initiated and reviewed in consultation with the Primary Care Provider, the specialist, and the enrollee or his/her designee. • The Medical Director or her/his designee will then determine maximum/minimum visits to provide continuation of care at the same time allowing updates between specialist and PCP without interruption of visits. • If there is not an appropriate specialist in the Network, a standing referral will be authorized with the non-participating specialist. The specialist will agree to follow TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN policies including quality requirements. This service should add no additional cost Revised January 2015 Section 4 Page 13 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL beyond what enrollees pay for in network services. SPECIALIST OR SPECIALTY CENTER AS PCP For enrollees with a degenerative and disabling condition or disease, the enrollee/enrollee’s designee or a PCP may request a specialist or specialty center as PCP. The Medical Director will, in consultation with the Primary Care Provider and the specialist or specialty center, review the enrollees medical record and determine whether, based on existing clinical standards, the enrollee’s disease or condition is degenerative and disabling. An enrollee cannot elect to use a non-participating specialist or center as PCP unless the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN network does not include an appropriate provider. If a non-participating specialist or specialty center is chosen, services will be provided at no additional cost to the enrollee. ACCESS TO SPECIALTY CARE Specialty Provider or Specialty Center Outside Of The TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Network • The enrollee will not be allowed to elect a non-participating specialist, unless the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN network does not include an appropriate provider. • If the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Network does not • have a health care provider with appropriate training and experience, an authorization can be made to an appropriate accredited specialty center or to an appropriate provider outside of the Network. • If an enrollee with a life threatening or degenerative and disabling condition or disease requires specialized medical care over a prolonged period of time, an enrollee may receive a referral to an accredited or designated specialty care center with expertise in the field. • The referral will be made pursuant to a treatment plan approved by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN in consultation with the PCP, non-participating provider, specialty center and enrollee or enrollee’s designee. • The services from a non-participating specialist will add no additional cost beyond what enrollees pay for in network services. NOTE: It is expected that Network Specialist will update the Primary Care Physician with their findings. This applies to all Network Specialist including Mental Health and Substance Abuse providers. Revised January 2015 Section 4 Page 14 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL CONTINUITY OF CARE TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s goal is to provide continuity of care for all new enrollees when: • The enrollee has a life threatening disease at the time of enrollment, the enrollee may continue with the services of a non-participating physician for up to 60 days • The enrollee is receiving prenatal care and is past the first trimester, the enrollee may continue with their physician until delivery and follow up care. • All new TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN enrollees o with diagnosis of a life threatening or degenerative and disabling disease will be allowed to continue ongoing course of treatment with the current provider up to 60 days from the effective date of enrollment. • All requests for continuity of care referrals must be submitted either orally or in writing by enrollee or designee to the Member Service Department at (800) 223-7242 or addressed to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, o Member Service Dept, PO Box 11507 Syracuse, NY 13218-1507. • A determination of appropriateness will include a review of medical records with consultation of outside provider in same specialty area to assure that enrollee is receiving care from accredited, licensed or designated specialty area with expertise in the field. • During the period of review to determine appropriateness, a minimum/maximum number of visits will be authorized preventing disruption of services. • After completion of 60 days, enrollee’s PCP (Primary Care Provider) will work closely with the out of plan provider to approve a treatment plan or to transition care. • If the enrollee has entered their second trimester of pregnancy at the time of the effective date of enrollment, the transitional period will include the provision of follow up care directly related to the delivery. CONTINUITY UPON PROVIDER LEAVING NETWORK If an enrollee’s health care provider leaves the managed care organization’s network of providers for reasons other than imminent harm to patient care, a determination of fraud, or a final disciplinary action by a state licensing board that impairs the health professional’s ability to practice, the managed care organization will permit the enrollee to continue an ongoing course of treatment with the enrollee’s current health care provider during a transitional period. The transitional period date begins the date the provider’s contractual obligation to provide services to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN terminates and ends no later than 90 days, or if health care professional is providing obstetric care and the member has entered her second trimester of pregnancy at the time of the provider’s termination, the transitional period includes post-partum care directly related to the delivery. The care will be authorized by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN for the transitional period only if the health care provider agrees to accept reimbursement at the rates applicable prior to the start of the transitional period as payment in full; to adhere to quality assurance requirements and to provide medical information related to such care; and to adhere to the organization’s policies and procedures including referrals and obtaining pre-authorization and a treatment plan approved by the organization. In no event will this paragraph be construed to require TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to provide coverage for benefits not otherwise covered or to diminish or impair preexisting condition limitations contained within the enrollee’s benefit plan. Revised January 2015 Section 4 Page 15 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL CASE MANAGEMENT TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN recognizes that its members have unique needs that may interfere with their compliance with services recommended by their Primary Care Providers. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Case Management Program is available to assist providers with Case Management services when these individuals are identified. To refer a member to Case Management, please call the Case Management Department at 1-800-223-7242. CRITERIA FOR REFERRAL Members with the following are conditions should be referred to our Case Management Department: 1. Hospitalizations (Primary Diagnoses): A. Psychiatric B. Substance Abuse C. Admissions for Controllable Diseases, for example—diabetes, asthma, hypertension 2. Social Issues: A. Medical Child Neglect 3. Life Threatening Chronic Diseases: A. HIV/AIDS B. Cancer C. Tuberculosis 4. 5. Members with Three Or More Consecutive Missed Appointments. Members with Significant Impairments. A. Hearing Impaired B. Vision Impaired C. Mobility Impaired D. Cognitively/Mentally Impaired 6. 7. Pregnant Patients Members That Failed To Meet Health Prevention Guidelines: A. Delayed Immunizations Three (3) Months Or More. (Ages 0-18 Years) B. Absence Or Delayed Lead Screening Of More Than Six (6) Months. (Ages 1-6 Years) C. Mammograms Delayed For Two (2) Years. (40 Years And Older) D. Pap Smears Delayed Two (2) Years. (From Onset Sexual Activity Or 18 Years And Older) E. Inability to have member patient return for follow-up of an abnormal lab or condition which may result in significant morbidity or mortality, for example—TB test, suspected cancer, etc. 8. Newly Diagnosed Patients With: A. Asthma B. Diabetes C. HIV/AIDS D. Mental Illness E. Substance Abuse F. Failure to Thrive G. Low Birth Weight Infants H. Critically Ill Newborn I. Newborns with NICU stay greater than 24 hours 9. Identify through claims data high risk populations that would benefit from Case Management Services. High risk populations will include Members who meet the following criteria: A. Members with at least on ER/hospitalization for diabetes B. Members with inpatient admission for asthma C. Members with more than one admission for mental health/chemical dependency within 6 months D. Members with inpatient admissions for acute MI, Coronary Artery Bypass Graft (CABQ), or Percutaneous Transluminal Coronary Angioplasty (PTCA) High risk populations will be discussed quarterly at Case Management and QI Committee meetings. Categories for review may be modified depending on the needs of the membership. Revised January 2015 Section 4 Page 16 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 10. Cases Identified By: A. Primary Care Provider B. Quality Improvement Program C. Complaint or Grievance Procedure D. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Medical Director E. Member F. Hospital Discharge Planner G. Quarterly Administrative Claims Review Revised January 2015 Section 4 Page 17 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 5 BILLING AND CLAIMS TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN as a State Department of Health contractor is required to: TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must maintain a health information system that collects, analyzes, integrates, and reports data. The system must provide information on areas, including but not limited to, utilization, Complaints and Appeals, and Disenrollments for other than loss of Medicaid or Family Health Plus eligibility. The system must be sufficient to provide the data necessary to comply with the requirement of our Agreement with the State Department of Health. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must take the following steps to ensure that data received from Participating Providers is accurate and complete: verify the accuracy and timeliness of reported data; screen the data for completeness, logic and consistency; and collect utilization data in standardized formats as requested by the State Department of Health. ELECTRONIC SUBMISSIONS TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is affiliated with Claimsnet, an electronic claims clearinghouse. As a participating provider office, you may submit your TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN claims electronically through Claimsnet. We are providing this service, at no cost to you, as part of our claims processing enhancement program. Claimsnet offers accurate and rapid submission of your TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN claims (HCFA 1500 or UB-92) as well as electronic claims submission to *other Payers. Best of all, it is an easy to use system which operates via the Internet. Once you complete the simple registration process, you will find the Claimsnet system highly automated, reliable and secure. Please contact our Provider Relations Department for direction on how to proceed at (877) 872-4716. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN can also be found on the WebMD payer list under Payer ID of 16146. Please contact TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Provider Relations Department at the number indicated above prior to submission through WebMD. Training to obtain Returned Claims Reports will be provided to you by Claimsnet. • Fees apply for payers other than TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL SUBMISSION OF CLAIMS All claims are to be submitted on the appropriate claim form, HCFA 1500 or the UB 92 FORM to: Revised January 2015 Section 5 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN 5232 Witz Drive North Syracuse, New York 13212-6501 The following information should be included on claims to expedite reimbursement: • Member's name, address and TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN ID Number. The TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK • HEALTH PLAN is the enrollee’s Social Security Number for CHIP and the Medicaid Number or CIN for Medicaid members • Name, address & signature of service provider • TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK • HEALTH PLAN assigned provider number (HCFA 1500 field 10d, UB 92 box 2 or 51). Beginning May 23, 2007 this number must be the provider’s National Provider Identification (NPT) number. • Tax Identification Number (TIN) in field 25 of the HCFA 1500 Form or in field 5 of the UB92 Claim Form • Date of service • Place of Service • CPT—4 Procedure Code • ICD—9 Diagnosis Code • Provider’s Charge • Name of referring physician (if applicable) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN CRITICAL UB04 DATA ELEMENTS NYS Diagnosis Related Group – Acute Care ; Skilled Nursing Facilities Zero Fill Type of Bill Code Statement Covers Period Type of Admission Source of Admission Patient Status Neonate Birth Weight Value Code - When Appropriate Neonate Birth Weight in Grams – When Appropriate Revenue Codes/HCPSC Codes Quantity of Units Submitted– Electronic Claims Zero Fill When Units Are Needed Dollar Charge Amount Principal/Primary Diagnosis Code Inpatient Admit Diagnosis Principal Procedure Code Surgeon Identification Number (NPI) – For Inpatient & Outpatient Surgical Claims Admission Date/Start of Care Date Attending Provider Identification Number (NPI) Medical Number/Health Record Number Present On Admission (POA) Discharge Status Revised January 2015 Section 5 Page 2 • • • • • • • • • • • • • • • • • • • • TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Claims Should Be Completed Per CMS 1500 or UB 92 Billing Manuals. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN claims should be submitted to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN within 90 days from date of service. Please notify TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN of any changes in your tax ID number, billing address or office address. Failure to do so will result in delay in reimbursements. Providers are responsible for determining if another insurer has primary responsibility for payment of services rendered. If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN determines that another payer is primarily responsible for payment, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will pay difference in accordance with our agreement. EXPLANATION OF PAYMENT: TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide an Explanation of Payment (EOP) statement with each reimbursement check. Each claim that is being reimbursed will be listed on the check’s accompanying EOP statement. This will include: • • • • Member's name and identification number Patient account number if provided on claims Explanation of Payment Code CPT-4 Code Total amount paid by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN ICD - 9 Code INCLUSIVE AND MULTIPLE SERVICES: • • Any office visits occurring the same day of surgery will be included in a global fee TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will adjust reimbursement for multiple procedures billed according to accepted medical policy. IDENTIFICATION OF THE PRIMARY PAYER: The identification of the primary payer prior to claim submission will improve the efficiency and accuracy of the claim payment process. Revised January 2015 Section 5 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL If a condition is related to the member's employment or is the result of an automobile or other accident, worker's compensation or no-fault carrier may apply. For worker's compensation claims, the employer should be contacted. For accident claims, the accident or no fault carrier should be billed as the primary payer. When a balance is due after payment by primary insurers, you may then submit a claim for that balance including the following information: • • The amount received from the primary plan A copy of the other plan's explanation of benefits In the event that the primary insurer’s reimbursement is greater than the established TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN rate, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will make no supplemental payments. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s original reimbursement amount must be returned to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN if it is determined that another payer is primary. NON-COVERED SERVICES: If the patient’s enrollment in TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or the Medicaid Program cannot be proven at the time of service, the patient may be directly billed. If it is later determined that the patient is enrolled with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and has paid for services rendered, the provider must refund the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN member any amounts collected in excess of applicable co-payments, co-insurance or deductibles. You may bill TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN members for non-covered services, such as items that are for personal convenience. You must advise the enrollee prior to providing the service that it is not covered and you must advise member of the cost of the service. Please see following entitled “Hold Harmless.” HOLD HARMLESS As a condition of participation in TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, PROVIDER agrees not to bill, charge, collect a deposit from, seek compensation, remuneration or reimbursement from, or have recourse against, Members of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or persons acting on their behalf, for health care services which are rendered to such Members by PROVIDER and which are Covered Services in accordance with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN benefits. This Agreement extends to all Covered Services furnished to the Member during the time he/she is enrolled in, or otherwise entitled to benefits promised by, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. The foregoing applies in all Revised January 2015 Section 5 Page 4 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL circumstances including, but not limited to non-payment or other breach of this Agreement by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and insolvency of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN ceases to operate due to insolvency or any other reason, the PROVIDER will abide by provisions of 2.10. This Agreement shall not prohibit collection of co-payments or payments for non-covered services from Members by PROVIDER in accordance with the terms of coverage issued by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, provided that PROVIDER shall have advised the Member that the service is subject to copayments or uncovered and of the Member’s liability prior to providing the service. Where the PROVIDER is uncertain as to whether a service is covered, PROVIDER shall make reasonable efforts to contact TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and obtain coverage determination prior to advising a Member as to coverage and liability for payment and prior to providing the service. Additionally, in the case of Medicaid Managed Care enrollees, PROVIDER agrees that, during the time an enrollee is enrolled in TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, PROVIDER will not bill the County Department of Social Services or the New York State Department of Health for covered services within the Medicaid Managed Care Benefit Package as set forth in the agreement between TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and the County Department of Social Services. The PROVIDER further agrees that the foregoing shall be construed to be for the benefit of Members of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN; shall survive the Termination of this Agreement; and shall supersede any oral or written contrary agreement now existing or hereafter entered into between the PROVIDER and such agents or persons acting on their behalf. POST PAYMENT AUDITS Periodically, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN representative may conduct post-payment audits. In such cases, an independent audit firm may be employed by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to conduct the audit. Participating providers are expected to make the necessary documentation available, (e.g. the patient's medical records) to ensure a successful audit. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or its representatives may request a refund for any overpayments, which may be found, or the amount of the overpayments may be deducted from future claim submissions. Revised January 2015 Section 5 Page 5 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL REQUESTS FOR REVIEW OF CLAIM PAYMENT ISSUES Listed below are payment issues that may be addressed to the Provider Relations Department: • Provider reimbursement methodology • Contract/benefit plan limitations • Any non medical issue Requests must be submitted to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN within sixty (60) days from the date of denial or payment on the EOP. Verbal requests should be followed with a brief written request as to why the original denial should be overturned. The following information should be included in the written request: • • • • • • • Date of service Member's name/TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN ID# or Child Health Plus Social Security Number Provider name and name of referring physician ICD-9 diagnosis TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Claim Number Reason for the review of payment request Any other pertinent information that would have impact on the review TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will review the request within thirty working days upon receipt of all necessary information. Additional information may be requested to make a determination regarding an appropriate adjustment. After review, a written or phone call will be made to the provider. Revised January 2015 Section 5 Page 6 TOTAL CARE QUALITY IMPROVEMENT PLAN 2014 TOTAL CARE QUALITY IMPROVEMENT PROGRAM PURPOSE: The Total Care Quality Improvement (QI) Program constitutes a systematic process for the identification, evaluation, resolution, and monitoring of potential and/or actual problems in the health care management of its members. The program’s design allows for proactive planning for ongoing improvement of the health care status and health outcomes of its members. The Medical Director oversees the program and ensures that the QI committee along with its subcommittees implements planned activities. This includes chairing of the credentialing committee to ensure the process documents services are being provided by properly qualified providers. BOARD AUTHORITY AND RESPONSIBILITY: The QI Program is accountable to the Total Care Board of Directors. Accordingly, this QI Program has been established and fully supported by the Total Care Board of Directors who will direct the Total Care Staff to implement the program. The Board of Directors will exercise its ultimate responsibility as overseer by receiving and reviewing quality improvement reports from the QI Program on a monthly basis. It will be the responsibility of the Plan’s Medical Director to ensure this reporting occurs. MEDICAL DIRECTOR RESPONSIBILITY: The Plan Medical Director will supervise the QI Program. As the Program supervisor, the TOTAL CARE Medical Director is responsible for the following: 1. To ensure that the QI Committee reviews the basic activities as outlined in the Quality Improvement Program. 2. To ensure that identified problems are prioritized with clear action plans; are monitored; and are re-evaluated. 3. To ensure the minutes of the QI Committee and all subcommittees are significantly detailed to reflect the Committee’s activities. 4. To ensure that the QI Program activities are presented and reviewed with the Board of Directors, President, Chief Operating Officer, and contracted clinical/medical staff. 2 Attachment 1 QUALITY IMPROVEMENT COMMITTEE: TOTAL CARE maintains and supports a Quality Improvement Committee for the purpose of providing clinical oversight within the QI Program. Membership: • TOTAL CARE Medical Director • TOTAL CARE Chief Operating Officer • TOTAL CARE Quality Assurance Director • TOTAL CARE Utilization Review Director • TOTAL CARE Member Services Representative • TOTAL CARE Provider Relations Representative • TOTAL CARE QA Nurse(s) • TOTAL CARE Case Managers • TOTAL CARE Director of Audit and Cost Containment • Behavioral Health Provider • Pharmacist • Dentist • Network Physician The Medical Director chairs the Quality Improvement Committee. Committee members will be appointed by the Medical Director. The Committee will meet at least eight times per year and submit quarterly reports to the Board of Directors. Quality Improvement Reports will be presented using NCQA reporting format when applicable. Reports will be enhanced using a variety of techniques including bar graphs, pie charts, and color alerts (i.e. dashboard reporting). Minutes and records will be maintained to document committee activity, studies, action plans and follow-up of established quality improvement plans. Objectives: The QI Committee will: 1. Ensure that preventive health services and educational services are provided to members in accordance with Total Care’s accepted guidelines. 2. Review recommendations for resolution of presented problems. 3 Attachment 1 3. Ensure the appropriate assignment for resolution of identified problems. 4. Be responsible for monitoring and re-evaluating identified problems, the effectiveness of resolutions, and the timeliness of planned implementations. 5. Make recommendations for quality improvement to the TOTAL CARE Board of Directors. 6. Promote opportunities to improve the health status and health outcome of members. Responsibilities: The QI Committee will determine and prioritize meaningful activities and/or problems based on the following: 1. High risk procedures or diagnoses 2. Frequency of occurrence 3. Major adverse consequences on health of patients 4. Cost effectiveness 5. Compliance with accepted or standard protocols of care 6. Continuity/Coordination of care 7. Improving health outcomes 8. Prenatal Services 9. Annual QARR/HEDIS information 10. Plan response to NYSDOH Quality Matrix issues The Committee will ensure: 1. Specific plans of action are generated for the resolution of problems identified as needing improvement; 2. Identification of the key responsible persons for carrying out action plans; 4 Attachment 1 3. Identification of time tables for implementation of action plans for improvement; 4. Documentation of the methodology for monitoring and re-evaluation of the problem, inclusive of time table and responsible person(s); 5. Planned interventions are conducted in a timely manner. Scope and Content: Identification of Benchmarks and Goals: Benchmarks and goals are determined through multiple sources including: Healthy People 2020, New York State’s Managed Care Plan Performance results, New York State Medicaid Averages, county health department data and National benchmarks where available. Identification of Clinical and Administrative Problems (Meaningful Activities): The QI Committee will utilize clinical and administrative data sources to identify meaningful activities that will be reviewed by the QI Committee. These data sources will minimally include: 1. 2. 3. 4. 5. 6. 7. Medical Record Reviews (Retrospective and Concurrent) Incident and/or Sentinel Events Member and/or provider complaints/comments Satisfaction surveys Utilization Information Case Management Information MIS Reports inclusive of member demographics, disease prevalence and utilization patterns In determining the manner by which potential clinical and administrative problems are examined, the plan will ensure: 1. The existence of procedures for the analysis 2. The acquisition of sufficient data to perform a meaningful analysis 3. Involvement of appropriate clinical personnel, including physicians and other providers for peer review The following components will be routinely monitored: 5 Attachment 1 Clinical Care: 1. General Medical Record Review A sampling of enrolled members will have their medical records reviewed utilizing Total Care’s Medical Record Documentation Standards. (Attachment 1) The reviews will be conducted by the Plan’s QA Nurses on an annual basis. The Quality Improvement Program will receive and review individual and aggregate data of its network providers to monitor the compliance with medical record standards. A provider having less than 80% compliance with the Medical Record Documentation Standards will trigger the need for an individual corrective action plan by the provider. Steps will be taken to ensure that a statistically valid sample of medical records is reviewed based on administrative claims data. The Medical Director will send the review tool, its results and any requests for a corrective action plan to the provider. In cases in which there is a needed action, the provider will be requested to respond to the Medical Director within 30 days. The Medical Director is responsible to review the appropriateness of the action plan and determine the time frame for follow up by the Quality Assurance/Utilization Management Department. The information from the audits will be presented in aggregate to the Quality Improvement Committee. The QA office will maintain individual results as part of the provider’s profile. These results will be available to the Credentialing/Provider Network Committee. 2. Preventive Health Services The Committee will review medical records and claims data of a random sample of TOTAL CARE members to determine adherence to preventive services protocols, e.g., Adult Preventive Guidelines (Attachment 2), Child/Teen Health Program Guidelines (Attachment 3) The Plan’s QA Director will be responsible for the coordination of these reviews on an annual basis. Non-users will be queried by member services. This information will be utilized to determine access of care issues of TOTAL CARE members (through Lack of Services Review). 7 Attachment 1 3. Prenatal Care The Committee will monitor prenatal care services received by a random sample of members through medical record and claims data reviews to determine compliance with established prenatal guidelines of the New York State Department of Health (Attachment 4). The Plan’s QA Director will be responsible for coordination of these reviews on an annual basis. 4. Acute and Chronic Diseases The Committee will review cases based on minimally one (1) clinical diagnosis annually. The diagnosis that will be reviewed will be reflective of the conditions seen in the membership, such as: • • • • • • • Hypertension Sexually Transmitted Diseases Asthma Diabetes HIV TB Anemia 5. Focused Clinical Study (Performance Improvement Project) The QI Program will minimally conduct one Performance Improvement Project on an annual basis. The study will be based on an area identified by the QI Committee as meaningful to the Plan and its membership. The focus study will be done in mutual agreement of the NYSDOH external review agent such as IPRO. 2013-2014 Topic”Improving Performance in Chronic Disease Prevention and Management“ The QA Director will be responsible for coordinating the study. 8 Attachment 1 6.Morbidity/Mortality Review The QI Committee will review on an annual basis a summary of mortalities. The QA Director will be responsible for coordinating the review. 7.Newborn Tracking (including Low birth weight Infants) On an annual basis, the QI Committee will review all infants on plan to monitor introduction into Primary Care within 4 weeks of birth. Report will include a review of infants with a birth weight under 2500 grams for birth outcome The QA Director will be responsible for coordinating the review 8. Informed Consent On an annual basis, the QI Committee will review a random sample of members receiving hysterectomies or tubal ligations to determine whether proper consent has been obtained prior to surgery. The QA Director will be responsible for coordinating the review Network Management: Access/Availability 1. Access to Services: The Committee will monitor accessibility to services through such methods as patient surveys, provider office surveys, and member complaints. Results will be reviewed using the Plan’s established access to care standards. (Attachment 5) The reviews will be submitted annually to the QI Committee and coordinated by the Director of Audit and Cost Recovery. Non-users will be queried by member services. This information will be utilized to determine access of care issues of TOTAL CARE members. 8 Attachment 1 2. Provider Satisfaction Surveys: The QI Committee will review data from provider surveys conducted on an annual basis by the Provider Relations Department. The surveys will be coordinated by the Director of Audit and Cost Recovery. (Attachment 6) 3. Appointment and Reappointment of Providers: The Credentialing/Provider Committee is incorporated as a subcommittee of the QI Committee. Reports of the committee will be submitted quarterly to the QI Committee and more often if necessary (Attachment 7). Customer Service 1. Member Satisfaction: Surveys completed periodically by the Local Department of Social Services an d the bi annual New York State Member Satisfaction Survey will be presented as received. The surveys will be coordinated by theMember Services Manager. 2. Complaint Report: Quarterly Report detailing number and category of complaints and identifying trends including complaints that result in physician transfers. The quarterly reviews will be coordinated by the and the Director of Audit and Cost Recovery. 3. Wait Time Study On an annual basis, a review is conducted to determine length of time experienced by members in the waiting room while in the office of participating PCP and OB/GYN providers TOTAL CARE Director of Audit and Cost Containment will coordinate the review 11 Attachment 1 Utilization Management The QI Committee will review data relevant to utilization activities to promote high quality cost effective care for all members. 1. Lack of Service Utilization On an annual basis, review of members who did not utilize plan services within 6 months of enrollment will be performed on non-use of services. The Director of QA will coordinate the review. 2. Emergent Care Visits per Member: On an annual basis, the utilization of emergency services will be analyzed to determine most common diagnoses and high users. The review will be coordinated by the QA Director. 3. Most Frequent Diagnosis by Member: On an annual basis, a review of claims data will be done to determine most frequently used diagnosis by members for primary care and most frequently used diagnosis by specialty services. The review will be coordinated by the QA Director. 4. Hospital Admissions per Member: On an annual basis, a review will be presented to the Committee indicating number of members with more than two (2) hospitalizations, length of stay and reasons for admission. The review will be coordinated by the QA Director. 5. Pharmacy Report The QI reports submitted to TOTAL CARE by its pharmacy manager will be presented to the QI Committee minimally on a quarterly basis. The review will be coordinated by the QA Director. 12 Attachment 1 6. Preauthorization Review A random sample of authorizations will be reviewed to determine compliance with NYSDOH standards. Reports will be presented to the QI Committee annually. The review will be coordinated by the Utilization Review Director. Provider Specific Reviews: Random provider specific reviews will be conducted in regard to: • • • • General chart documentation Health prevention Specific diagnosis Prenatal Care Any patient issues of concern will be referred to the Medical Director. The plan will contact the patient and the provider, for example, need for pap smear, immunization delay, etc. Information on the quality improvement reports and expected actions will be provided to the applicable provider. 13 Attachment 1 Quality Improvement Committee Subcommittees: Subcommittees that report to the Quality Improvement Committee include: 1. Credentialing/Provider Network Committee 2. Case Management Committee 3. Peer Review Committee ANNUAL REVIEW The QI Program description will be evaluated annually and updated as necessary. The program evaluation will be written and include: 1. A description of completed and ongoing QI activities 2. A trending of measures to assess performance in the quality of clinical care and quality of service 3. An analysis of whether there have been demonstrated improvements in the quality of clinical care and quality of service to members 4. An evaluation of the overall effectiveness of the QI Program. CONFIDENTIALITY Information or data leading to identification of a specific person or the status of a specific patient will be maintained in strict confidence. The quality of care of members of the plan will be discussed to improve quality but not in a manner that will jeopardize Total Care, its patients or its employees. The written Quality Assurance Program will be provided to all members of the Board of Directors, providers and staff and will be available to all enrollees in Total Care. 12 Attachment 1 ATTACHMENTS TO QUALITY IMPROVEMENT PROGRAM 13 Attachment 1 Standards for General Medical Documentation 1.Patient identification must be contained on each page of the record (Name, DOB, ID) 2. Provider signature and professional title should be identified on each entry. 3.All entries in the record should be dated. 4.Personal biographical data including address, employer, home and work telephone numbers, and marital status will be included in the medical record. 5.The medical record must be legible. 6.Past medical history should be contained within the medical record. 7.The record will contain a family history. 8.An ongoing problem list will be maintained to monitor a member’s health status. 9.Allergies and/or adverse reactions shall be clearly and easily identified on the record, or NKA will be noted. 10.The record for members 12 and older will contain documentation of screening and counseling for: § Tobacco § Alcohol § Drugs/Substances § HIV 11.The record will contain pertinent history and physical information, IE: appropriate subjective and objective information relevant to the patient’s presenting complaints. 12. Laboratory and other studies will be ordered according to established guidelines. 13.Working diagnoses are consistent with findings. 14.Plans of action and treatment are consistent with findings. 15.Problems from previous visits are addressed. 16.There will be a date of return or follow-up plan for each encounter. 17.There is use of specialists according to established guidelines. 18.Lab work, special studies, hospitalizations, emergency room, outpatient surgery / procedure and consult summaries will be initialed by member’s PCP or addressed upon review in progress notes. 19.The record will demonstrate evidence of continuity and coordination of care between primary and specialty providers. 20.There is evidence that preventive screening and services are offered according to established guidelines. 21.Immunization records will be complete and current. Refusal of immunizations by reason of personal beliefs should be clearly documented. Medical contraindications also must be clearly documented. 14 Attachment 1 22.There is documentation that information on the Patient SelfDetermination Act has been provided to the member and that competent consenting adults (including a person who is under 18 years of age who is either married or has a child) either have or have not executed an oral or written Advance Directive. 23.There is documentation that timely screening for STD’s is documented. 24.There is documentation that education about risk and prevention of STD’s is documented. 25.There is documentation that reporting of STD’s to the local County Health Department has occurred. 26.There is documentation that lead levels of 20 or above are reported to local County Health Departments. SCORING N/A = NOT APPLICABLE 2 = FULL COMPLIANCE 1 = PARTIAL COMPLIANCE 0 = NO COMPLIANCE 15 Attachment 1 _ MEMBER NAME PROVIDER TOTAL CARE 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 _ _ ADULT PREVENTIVE GUIDELINES REVIEW (Ages 21 – 75 Years) STANDARD Has member had PCP visit during review year? Initial History Completed at First Visit? (All) B/P (All) Height (All) Weight (All) BMI Dental Screening? (All) Pap every year? (All Women) [May be less frequent if 3 consecutive neg. results]. Chlamydia? (Women under 25 and sexually active, women over 26 if at risk or symptomatic.) Rubella serology or Vac. History? (Women of child bearing age). Blood Cholesterol? (Men every 5 years from age 35 – Women every 5 years from age 45). Colon Ca. Screening?(Yearly after age 50 for all). Mammography? (Yearly for women over 40). Vision Screening? (All over age 65). Assess for Hearing Impairment? (All over 65). Assess for Problem Drinking? (All) Tobacco and Substance Abuse Screening? (All) Substance use counseling? (All) Injury Prevention counseling? (All) Sexual Behavior counseling? (All) HIV testing offered (All) Annual Diet and Exercise counseling? (All) Dental Health counseling? (All) Tobacco use counseling? (All) Td Booster? (All, every 10 years) Hepatitis B Vac.? (All at increased risk) MMR Vac.? (All born after 1956 w/o proof of immunity) Varicella Vac.? (All non-immune adults) Pneumococcal? (All over age of 65) Influenza? (All over age of 50) Reviewed By: Date Reviewed: DATE OF BIRTH FACILITY YES NO N/A DATE WAS MENTAL HEALTH SCREEN DONE? WAS SUB. ABUSE SCREEN DONE? Attachment 2 Attachment 3 New York State Medicaid Prenatal Care Standards November, 2009 Prenatal care standards in New York State (10 NYCRR, Part 85.40) were developed in early 1990 in response to the creation of the Prenatal Care Assistance Program (PCAP), a prenatal care program developed to provide for comprehensive perinatal care to low income, high risk pregnant women. The most recent revision of these standards occurred in 2000. Changes in the clinical standards of prenatal care since that time necessitate a review of Part 85.40 standards to compare them to current professional standards of practice which address new challenges and concepts in prenatal care. In order to accomplish this task, the Department partnered with the Island Peer Review Organization (IPRO) to review the existing PCAP standards and compare them to current American College of Obstetricians and Gynecologists (ACOG) guidelines1, new recommendations in prenatal care, as well as other national guidelines of obstetric practice to determine the need to modify the prenatal standards as they become applied to all Medicaid prenatal providers. The Office of Health Insurance Programs, in collaboration with the Division of Family Health, IPRO and a statewide advisory workgroup made up of key stakeholders in the field of prenatal care were charged with the responsibility for developing this revised set of Medicaid Prenatal Care Standards for New York State. Steps in the process included: Literature review and comparison of Part 85.40 with current ACOG guidelines and other evidencebased literature; Stakeholder meetings to discuss current standards of practice; Summary proposal with recommendations for revised standards; Revisions to Article 25, New York State Public Health Law; and Draft Medicaid Prenatal Care Standards for review and subsequent adoption. The Department would like to express its appreciation to all the external stakeholders who gave of their time and shared their expertise in the field of prenatal care to assist us in the development of prenatal care standards for the NYS Medicaid Program. 1 New York State Medicaid Prenatal Care Standards November, 2009 Attachment 4 A. REQUIREMENTS 1. General requirements: a) Prenatal care providers shall create and maintain records and reports that are complete, legible, retrievable and available for review by representatives of the Commissioner of Health upon request. Such records and reports shall include the following: • a comprehensive prenatal care record for each pregnant woman which documents the provision of care and services received and which is maintained in a manner consistent with medical confidentiality requirements; • special reports and data submissions as necessary for the Commissioner of Health; • records of internal quality assurance; • all written policies and procedures required by this section; and • data submissions in electronic form as requested by the Commissioner of Health in compliance with the most current Department of Health policies for health information exchange in New York State. b) Prenatal care providers shall comply with all federal, state and local laws and regulations regarding the disclosure of protected medical information when sharing or transferring medical information with other healthcare providers or facilities. Providers shall therefore obtain written informed consent from patients prior to transfer of medical records or information where required by law. c) Prenatal care providers shall comply with the requirements to obtain informed consent for all services described herein, in accordance with all applicable laws and regulations. d) Any subcontracts between the prenatal care providers and other agents or agencies providing care and services shall: i) be available for review and inspection by the Department of Health; and ii) require that subcontractors provide contracted care and services that meet the minimum standards established in this section and are provided in accordance with generally accepted standards of practice and patient care services. e) Prenatal care providers shall participate in quality improvement initiatives as requested by the Commissioner of Health. 2. Provider/Staff requirements: a) Prenatal care services, including prenatal diagnostic and treatment services, provided to pregnant women and postpartum women shall meet generally accepted standards of care as described by the most current American Academy of Pediatrics (AAP) and ACOG guidelines for perinatal care and shall be provided by a qualified provider practicing as: a licensed physician practicing in accordance with Article 131 of the New York State Education Law and must be either an obstetrical care physician (MD/DO), Board Certified or Board Eligible in their area of specialty, or have completed an accredited residency program in Family Practice or Obstetrics/Gynecology; ii) a nurse practitioner practicing in accordance with Article 139 of the New York State Education Law and certified in the specialty of obstetrics/gynecology; iii) a licensed Midwife practicing in accordance with Article 140 of the New York State Education Law; or iv) registered physician’s assistant practicing in accordance with Part 94 of this Title, Article 37 of the NYS PHL and article 131 of the NYS Education Law. Attachment 4 b) Prenatal care providers shall promote the delivery of prenatal care services in a culturally sensitive/competent manner to all pregnant women including those with limited English proficiency and diverse cultural and ethnic backgrounds. Interpretation services must be offered to patients whose primary language is not English, in person when practical, or via telephone if a translator is not immediately available. c) Prenatal care providers must either have admitting privileges at one or more hospitals or shall develop agreements with planned delivery sites including a system for sharing patient information for continuity and follow-up care. 3. Provider/Specialist/Consultation Requirements: Prenatal care providers shall provide pregnant women timely access and referral to appropriate levels of prenatal care, (basic, specialty, and subspecialty), based on her assessed risk status in order to prevent, recognize and treat conditions associated with maternal and infant mortality and morbidity.2 a) Management of pre-existing medical conditions - Providers shall provide or arrange for the provision of care for the specific needs of a pregnant woman with a pre-existing medical condition, according to current standards of practice. b) Transfer of care - Practices shall develop criteria requiring transfer of primary responsibility for patient care from a family medicine practice physician, physician’s assistant, licensed midwife or nurse practitioner to an obstetrician and/or maternal-fetal medicine specialist (high risk obstetrician or perinatologist). c) Specialty physician consultation/referral – Prenatal care providers shall develop criteria for consultation and referral for care to a maternal-fetal medicine specialist, perinatalogist, high risk obstetrician, specialty physician, behavioral health specialist, including licensed social worker or other health care specialist as necessary based on the identification of specific risk factors or medical conditions requiring additional specialty monitoring and management. Prenatal care providers should follow AAP/ACOG’s early and on-going pregnancy risk specific recommendations for consultation.3 Referrals for specialty provider consultations should include: i) a description of the indication for the consult, ii) the role of the consultant during the initial consult iii) the role of the consultant during the follow-up care throughout the stages of pregnancy, and iv) he sharing of patient/clinical information between the primary care obstetrical provider and the special care consultant. 4 Attachment 4 B. ACCESS TO CARE 1. Any pregnant woman who presents for prenatal care should begin receiving care as quickly as possible, preferably the same day. All prenatal care service providers must provide prenatal care services to recipients determined to be presumptively eligible for medical assistance but are not yet enrolled in Medicaid. 2. Prenatal care providers shall assist or refer women for assistance with application for medical assistance and managed care plan selection in accordance with procedures established by the Commissioner. 3. Prenatal care practices must provide or arrange for the provision of 24 hour/7 day week coverage (after hours and weekend/vacation number to call that leads to a person or message that can be returned by a health care professional within one hour). Pregnant women shall have access to unscheduled or emergency visits on a 24 hour basis.5 4. Prenatal care providers must develop systems, or arrange for reminder/call backs to patients needing continued or follow-up services, and for visits requiring follow-up for abnormal test results. Prenatal care providers shall outreach to patients to reschedule missed appointments in a manner that maintains patient confidentiality. 5. Prenatal care providers shall schedule prenatal care visits for an uncomplicated pregnancy consistent with AAP/ACOG recommendations. Pregnant women with medical, obstetrical and/or psychosocial problems may require more frequent visits. The need for increased surveillance is best determined by the prenatal care provider based on the individual needs of the woman, and the nature and severity of her problems. C. PRENATAL RISK ASSESSMENT, SCREENING AND REFERRAL FOR CARE Prenatal care (PNC) providers shall conduct a comprehensive prenatal care risk assessment for both maternal and fetal risks, at the earliest prenatal care visit, on all pregnant women. 1. The risk assessment shall include but not be limited to an analysis of individual characteristics affecting pregnancy, such as genetic, nutritional, environmental, behavioral health, psychosocial and history of previous and current obstetrical/fetal and medical/surgical risk factors. Prenatal care providers are encouraged to use a standardized written risk assessment tool, such as the ACOG, Hollister or POPRAS form. Using established criteria for determining high risk pregnancies, the prenatal care provider shall determine the woman’s risk status based on generally accepted standards of practice. The risk assessment shall be: a) reviewed at each visit; b) repeated formally early in the third trimester; c) used to form the basis for the development of the care plan and; d) documented clearly in the medical record. Attachment 4 2. Based on results of the risk assessment and the individual woman’s increased risk for a poor pregnancy outcome, the prenatal care provider shall refer the pregnant woman for follow-up care. Referrals for such care may include but are not limited to: prenatal case management programs provided by managed care plans, other case management programs, home visitation agencies, or community-based programs for prenatal care coordination. 3. In accordance with Public Health Law section 2530-a 2.3. Prenatal care providers shall complete a standardized New York State Prenatal Care Risk Screening Form, which summarizes the results of the comprehensive risk assessment (as described in C.1.) for each new pregnancy. The completion of this risk screening form once during the pregnancy and reporting of the information shall be with the pregnant woman’s informed written consent and shall be in a format to be developed by the Commissioner. If consent and voluntary participation is obtained, prenatal care providers shall complete the New York State Prenatal Care Risk Screening Form at the earliest prenatal care visit and transmit the information in a confidential manner to be determined by the Commissioner. D. PSYCHOSOCIAL RISK ASSESSMENT, SCREENING, COUNSELING AND REFERRAL FOR CARE Prenatal care providers shall conduct a psychosocial risk assessment of all pregnant women during the first prenatal care visit. The assessment should be reviewed at each visit and formally repeated early in the third trimester and postpartum to identify important issues that may have developed over time. The assessment shall include a broad range of social, economic, psychological and emotional problems. Screening should include but not be limited to assessment of barriers to care, unstable housing, communication barriers (i.e. language and /or cultural barriers), nutrition, tobacco use, substance use, depression or other psychiatric illness, safety, domestic abuse, sexual abuse, and stress. Based on the results of this assessment the providers shall identify areas of concern, validate major issues with the patient, provide information, and if indicated, provide treatment or make appropriate referral(s). The psychosocial risk assessment shall include but not be limited to screening for the following6: 1. Tobacco Use – Prenatal care providers shall assess all pregnant women about their past and present use of tobacco and exposure to second hand smoke. All pregnant women should be advised to avoid or minimize time spent in the presence of tobacco smoke. The patient who smokes should be strongly advised to stop smoking and be provided with tailored counseling to assist in smoking cessation. Patients who smoke shall be offered a referral to an appropriate smoking cessation education and/or treatment program. 7 2. Substance Use – Prenatal care providers shall assess all pregnant women about their past and present use of all substances, including drugs, alcohol, or the use of any prescription or nonprescription medications, including herbal supplements. The possible effects of any substances used before or during pregnancy should be discussed. A woman who acknowledges the use of any substances should be counseled about the implications of their use during pregnancy, and strongly encouraged to refrain from use of any substances that may negatively affect her or her fetus. If appropriate the woman should be offered a referral to a treatment program. Attachment 4 3. Domestic Violence – Prenatal care providers shall screen all pregnant women for domestic violence. Descriptions of domestic abuse from the patient should be documented in the patient’s medical record, safety of the patient and family shall be ascertained and referrals made to appropriate counseling, legal and socialservice advocacy programs. 4. Depression – Prenatal care providers shall screen pregnant and postpartum women for depression utilizing an appropriate screening tool, and should have a system in place to ensure that positive screening results are followed by accurate diagnosis, implementation of treatment, and follow-up either within the practice or through referral. E. NUTRITIONAL SCREENING, COUNSELING AND REFERRAL FOR CARE Prenatal care providers shall provide or arrange for the provision of nutritional and physical activity screening, counseling and referral which includes: 1. Individual nutritional risk assessment including an assessment of pre-pregnancy BMI, weight gain to date, if any, and specific nutritional risks at the initial prenatal care visit and continuing reassessments as needed; 2. Documentation of the nutritional assessment, risk status and the plan of care in the patient’s medical record; 3. Referral of pregnant women identified as being at nutritional risk for specific nutritional counseling, monitoring and follow-up; 4. Provision of basic nutrition education and counseling for each pregnant woman which includes: a) appropriate dietary intake and recommended dietary allowances during normal pregnancy; b) recording of height and weight at the initial prenatal visit to allow for the calculation of the BMI and sequential weight monitoring at each visit. Parameters of appropriate weight gain should be made based on the pre-pregnancy BMI categories recommended in the 2009 Institute of Medicine (IOM) guidelines8; c) a focused approach to nutrition counseling based on AAP/ACOG guidelines which includes exercise and lifestyle changes for all women, but particularly for women with a BMI in the obese (BMI>30) or underweight (BMI<18.5)9 range; and d) counseling and education regarding infant feeding choices discussed with the woman during prenatal visits and immediately postpartum. Prenatal care providers should support breast feeding by counseling the patient regarding the nutritional advantages of human breast milk and should provide her with information regarding the benefits of breast feeding for both the mother and infant. Exclusive breastfeeding is recommended for the first 6 months of life and should be continued along with supplemental foods through the second half of the first year of life and for as long as desired thereafter. Breastfeeding is not recommended for HIV positive women and may be medically contraindicated in other situations. Income eligible women considering breastfeeding should be referred to the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) for breastfeeding education and support. Attachment 4 5. Referral of pregnant women identified as needing to access proper nutrition and assistance in obtaining supplemental food to programs such as the Supplemental Nutritional Assistance Program (SNAP) or the Special Supplemental Nutrition Program for Women, Infants and Children (WIC). 6. Special considerations for underweight and/or overweight/obese women: a) Prenatal care providers shall assess and counsel underweight and overweight/obese women regarding the increased risk for pregnancy complications related to their weight and encourage these women to participate in a lifestyle improvement program, including diet, exercise, and behavior modification. b) Prenatal care providers shall consider screening obese patients for gestational diabetes upon presentation or in the first trimester, and repeat screening later in the pregnancy if results are initially negative.10 F. HEALTH EDUCATION Prenatal care providers shall provide or arrange for the provision of health and childbirth education based on an assessment of the pregnant woman’s individual needs. Prenatal care providers should focus on the pregnant woman’s ability to comprehend the information and use materials appropriate to the educational, cultural and language needs of the patient as well as her gestational history. Such services shall be provided by professional staff, documented in the medical record and shall include but not be limited to the following: 1. Rights and responsibilities of the pregnant woman; 2. Signs and symptoms of complications of pregnancy; 3. Physical activity, exercise and recommended weight gain during pregnancy; 4. Avoidance of harmful behaviors including the use of alcohol, drugs, non-prescribed medications and nicotine; 5. Sexuality during pregnancy; 6. Occupational and environmental concerns including lead exposure; 7. Risks of HIV infection and risk reduction behaviors; 8. Signs of labor; 9. Labor and delivery process and availability of various delivery options; 10. Relaxation techniques in labor; 11. Obstetrical anesthesia and analgesia; 12. Preparation for parenting including infant development and care, options for feeding and the benefits of breast feeding; 13. Newborn screening program, including the distribution of newborn screening literature; 14. Family planning and optimum inter-pregnancy interval. Attachment 4 G. DEVELOPMENT OF A CARE PLAN AND CARE COORDINATION Prenatal care providers shall develop a care plan jointly with each pregnant woman which addresses the problems identified as a result of the initial and ongoing risk assessments. The care plan shall describe the implementation and coordination of all services required by the pregnant woman, be routinely updated and implemented jointly by the pregnant woman, her family and the appropriate members of the health care team. 1. Care shall be coordinated to: a) Ensure that relevant information is exchanged between the prenatal care provider and other providers, health plan case managers or sites of care including the anticipated delivery site. b) Ensure that the pregnant woman and her family or other designated representative, with her consent, have continued access to information resources and are encouraged to participate in the decisions involving the care and services being provided. c) Encourage and assist the pregnant woman in obtaining necessary medical, dental, nutritional, psychosocial, drug and substance abuse services appropriate to her identified needs. d) Provide the pregnant woman with an opportunity to receive prenatal and postpartum home visitation when medical and/or psychosocial benefits may be derived from the visits. e) Provide to or refer the pregnant woman for needed services as identified in the risk assessment. f) Obtain special tests and services that may be recommended or required by the Commissioner of Health, when necessary to protect maternal and/or fetal health. Pregnant women shall be provided appropriate medical care, counseling and education based on test results. 2. The prenatal care provider shall coordinate labor and delivery services by developing agreements with planned delivery sites which address, at a minimum, the following: a) a system for sharing prenatal medical records, including HIV test results; b) pre-booking of women for delivery by 36 weeks gestation for low risk pregnancies and by 24 weeks gestation for high risk pregnancies; c) scope of services; and d) sharing of delivery/birth outcome information. 3. The prenatal care provider shall arrange for postpartum home visitation care as necessary and available when the mother and/or newborn may derive medical, physical and/or psychosocial benefits from such visits. Attachment 4 H. PRENATAL CARE SERVICES Prenatal care providers shall provide or make arrangements for the provision of comprehensive prenatal care services in accordance with generally accepted standards of professional practice, as outlined by the AAP and ACOG.11 1. Prenatal diagnostic and treatment services shall include but not be limited to the following: a) Comprehensive assessment – An initial comprehensive assessment including history, review of systems, and physical examination. b) Standard and special laboratory tests – Based on AAP/ACOG recommendations, standard and special laboratory tests and procedures should be performed at the recommended gestational age. c) Follow-up, evaluation of results and referral – Follow-up shall be conducted as indicated based on abnormal findings from the comprehensive assessment, results of preliminary abnormal laboratory test findings and repeat testing of women considered to be at high risk. Prenatal care providers shall discuss the following with the pregnant woman: i) findings from the comprehensive assessment, ii) results of all laboratory tests, iii) recommendations for additional testing, iv) reatment options and obtaining informed consent for treatment, v) technological support and referrals as necessary. 2. HIV Services a) Prenatal HIV Counseling and Testing Prenatal care providers shall provide HIV counseling to all pregnant women as early as possible in the pregnancy without regard to risk. Counseling shall be provided and informed consent obtained prior to HIV testing and shall be consistent with the requirements described in Article 27F of the Public Health Law and NYCRR Title 10 Section 63.3. A repeat third trimester test, preferably at 34 – 36 weeks should be routinely recommended to all pregnant women who tested negative early in prenatal care to identify sero-conversion after an initial negative prenatal HIV test.12 The New York State Department of Health Informed Consent to Perform HIV Testing (DOH Form – 2556), allows the pregnant woman to receive counseling for both tests at the initial counseling and to sign for both tests at that time. The pregnant woman should be counseled about benefits to knowing her HIV status, specifically the significant reduction in risk of mother-to-child HIV transmission with the provision of antiretroviral (ARV) prophylaxis to HIV-positive women during pregnancy, at delivery and to the newborn. The pregnant woman should be informed that if she does not have a prenatal test, she will be HIVcounseled again when she presents for delivery, and that expedited testing will be done on her, with her consent, or on the newborn, without her consent. She should also be told that all newborns are routinely screened for HIV as part of the Newborn Screening Program, as a final safety net to identify exposed infants. Pregnant women who receive negative test results should be provided with their results and if at continued risk for developing HIV, encouraged to access HIV prevention programs and services appropriate to their risk(s). Pregnant women who receive positive HIV test results should be provided with post-test counseling consistent with Public Health Law section 2781 and Part 63 regulations and will be provided necessary care and/or appropriate referrals for services.13 Attachment 4 Prenatal care providers should transfer information regarding a prenatal patient’s HIV counseling and testing status, including a copy of the result, if one exists, to the delivery setting. Routine consent procedures for the transfer of medical records are sufficient to authorize the transfer of HIV-related information to health care providers. b) Care of an HIV-Positive Pregnant Woman Management of antiretroviral (ARV) medications during pregnancy should be done by, or in consultation with, an experienced HIV specialist familiar with state and federal clinical guidelines for the care of HIV-positive pregnant women and the prevention of mother-to-child HIV transmission. Breastfeeding is not recommended for HIV-positive women where there are good alternatives. 3. Dental care The prenatal care provider shall conduct an assessment of the woman’s oral health care needs at the first prenatal care visit. The assessment shall include but not be limited to interviewing the patient regarding current oral health problems, previous dental problems, and the availability of a dental provider. Pregnant women identified as having a current oral health problem or not having a dental visit in the past six months should be referred to a dentist as soon as possible, preferably before 20 weeks gestation. The prenatal care provider shall educate the pregnant woman about the importance of oral health and that dental care is safe during pregnancy. Oral health care should be coordinated between the prenatal care provider and the dentist.14 4. Immunizations Pregnancy is not an absolute contraindication to any vaccination. Some vaccines are strongly recommended for pregnant women during the prenatal period. Many women will not be up-to-date and each pregnant woman should be evaluated for immunization status. Guides for immunizing during and after pregnancy are available from the Centers for Disease Control and Prevention (CDC)15 and the New York State Department of Health Bureau of Immunization.16 a) All pregnant women shall be evaluated for serologic evidence of immunity to rubella at their first prenatal visit, unless known to be immune by documentation of a previous test. Varicella immunity shall also be assessed by either a reliable history of disease, laboratory evidence of previous disease or documented receipt of two doses of vaccine. b) Influenza vaccine is strongly recommended for all pregnant women due to the increased risk of influenza-related complications among pregnant women. Pregnant women should only receive the trivalent inactivated influenza vaccine (TIV), and not the live attenuated influenza vaccine (LAIV), the nasal spray. c) The following immunizations are recommended for women at risk for these diseases and who do not have a history of immunity: Hepatitis B - A pregnant woman’s risk of acquiring Hepatitis B Virus (HBV) should be assessed along with her risk of acquiring other sexually-transmitted infections. Pregnant women who have been identified as being at risk for HBV infection should be vaccinated. Pregnancy is not a contraindication for HBV vaccination, and limited evidence does not suggest any fetal harm from the HBV vaccine. ii) Tetanus, Diptheria/Tetanus, Diptheria, Pertussis booster (Td/Tdap) - Pregnant women who have not received a Td booster within the last 10 years and require immediate protection against tetanus and diphtheria (ie. wound prophylaxis) should be vaccinated with Td based on the severity of the risk of tetanus and the need to be immunized. Immunization with Td during pregnancy is preferred in the 2nd or 3rd trimester. Attachment 4 iii) Tdap may be administered during pregnancy if the woman requires protection from pertussis. Tdap is not contraindicated during pregnancy; however, data on its safety and effect on newborn immune response to the primary DTaP series is limited. d) Other pregnancy related immunization issues: New York State Public Health Law 2500-e requires that every pregnant woman be tested for the presence of hepatitis B surface antigen (HBsAg) and that the test results and the date are documented in the prenatal record. It also requires that infants of women who are hepatitis B surface antigen positive or whose test results are unknown receive treatment at birth with hepatitis B vaccine and hepatitis B immunoglobulin (HBIG). New York State Public Health Law 2112 (effective July 1, 2008) prohibits the administration of vaccines containing more than trace amounts of thimerosal, a mercury-containing preservative, to pregnant women, unless the supply is insufficient. There is no evidence that thimerosal causes harm to the pregnant woman or her fetus. e) Postpartum Period – The following vaccinations or a history of immunity are recommended for all postpartum women: influenza, MMR (measles, mumps, rubella), Tdap, varicella and human papilloma virus. An adult schedule should be checked for appropriate indications in regard to age, previous history of disease or prior history of vaccination.17 Women who plan to breastfeed can and should receive vaccinations as no evidence exists of any risk to a mother or her infant if she is vaccinated while breastfeeding. Breastfeeding is not a contraindication to any vaccination, with the exception of vaccinia vaccine. 5. Lead Poisoning Prevention, Testing and Management As required by NYS Public Health Law and Regulations (NYCRR Subpart 67-1.5), prenatal health care providers shall provide all pregnant women with anticipatory guidance on preventing lead poisoning, information on the major sources of lead and the means to prevent exposure. At the initial prenatal visit, each pregnant woman shall be assessed for exposure to lead by using a risk assessment questionnaire recommended by the State Commissioner of Health.18 If the pregnant woman responds “yes” to even one of the questions, she is considered to be at risk, and should have a blood lead test and be counseled on how to eliminate lead exposure. Pregnant women found to have a confirmed blood lead level of 10 micrograms per deciliter (mcg/dL) or greater should be provided with risk reduction counseling and follow-up testing in accordance with NYS Department of Health guidelines. In addition, all pregnant women with a confirmed blood lead level of 10 mcg/dL or greater who may have been occupationally exposed to lead should be referred to an occupational health clinic for individual guidance. All women should receive anticipatory guidance on the prevention of childhood lead poisoning at their postpartum visits. Consultation for medical management of a lead poisoned pregnant woman is available from the Regional Lead Resource Centers (RLRC).19 Prenatal care providers are required to adhere to the most current New York State Department of Health guidelines for the prevention, identification and management of lead poisoning in pregnancy, as described in Lead Poisoning Prevention Guidelines for Prenatal Care Providers – NYSDOH & ACOG District II, June, 2009.20 Attachment 4 6. Use of Ultrasound Prenatal care providers must document the medical indication for performing an ultrasound examination of a pregnant patient based on identified need. Ultrasound for gestational dating is recommended, especially before 20 weeks, if there is a size-date discrepancy or imprecise menstrual dates.21 Ultrasonography shall be provided only by physicians or technologists who have undergone training and only when there is a valid medical indication for the examination documented in the woman’s medical record by a qualified prenatal care provider.22 AAP/ACOG guidelines should be followed when recommending an ultrasound exam. Commonindications for ultrasound include but are not limited to evaluation for gestational age; fetnumber, viability, placenta location, abnormal amniotic fluid volume, fetal growth disturbancfetal anomolies and aneuploidy screenin23 7. Screening for Genetic Disorders Prenatal care providers shall offer all pregnant women additional maternal/fetal screenings to identify fetal abnormalities/genetic problems as follows: a) Birth defects – Prenatal care providers shall offer all pregnant women screening tests to identify birth defects at specific times throughout the prenatal period based on AAP/ACOG recommendations. b) Invasive diagnostic testing for aneuploidy should be available to all women regardless of maternal age. Early amniocentesis (at less than 15 weeks gestation) should not be performed.24 c) Pregnant women should be counseled regarding the differences between screening and invasive diagnostic testing for aneuploidy including a discussion of the risks and benefits of the invasive test compared with other available screening tests. Pregnant women who choose not to undergo invasive diagnostic testing for aneuploidy shall be offered aneuploidy screening before 20 weeks gestation regardless of maternal age. 25 d) Prenatal care providers should offer information on cystic fibrosis screening to all couples and cystic fibrosis carrier screening should be offered to all couples regardless of race or ethnicity.26 e) Prenatal genetic screening or diagnosis should be offered to pregnant women based on personal and family history. Genetic screening and counseling criteriea should be based on AAP/ACOG recommendations. This includes screening for genetic disorders based on racial and ethnic background, such as hemoglobinopathies (sickle cell, α-thalassemia, β-thalassemia), Tay-Sachs disease, Canavans disease and familial dysautonomia, cystic fibrosis and other genetic disorders based on family history.27 1. Fetal Well-Being Tests of fetal well-being are indicated in the presence of specific maternal and pregnancy-related conditions and shall be performed based on the judgment of a qualified prenatal care provider according to individual patient need.28 There are several tests used in clinical practice to assess fetal status, each test has advantages, disadvantages as well as risks. The prenatal care provider, based on clinical judgment and recommended AAP/ACOG guidelines should choose the test that best meets the needs of the pregnant woman and her fetus and initiate testing at the appropriate gestational age. The test results and the interpretation shall be discussed with the pregnant woman, documented in the medical record and appropriate referrals initiated as soon as possible. Attachment 4 I. POSTPARTUM SERVICES The prenatal care provider shall schedule a postpartum visit based on the woman’s identified needs and in accordance with AAP/ACOG’s recommended schedule, (approximately 4 – 6 weeks after delivery but no later than eight weeks after delivery; women with a complicated gestation or delivery by cesarean section should have a visit scheduled within 7 – 14 days of delivery). The visit should include an interval history and a physical examination to evaluate the patient’s current status and her adaptation to the newborn. 1. The visit shall include but not be limited to the following: a) identify whether any medical, dental, psychosocial (including depression), nutritional (including breastfeeding), tobacco/smoking cessation needs, alcohol and drug treatment needs of the mother or infant are being met; b) provide anticipatory guidance on the prevention of childhood lead poisoning; c) refer the mother or other infant caregiver to resources available for meeting identified needs and provide assistance in meeting such needs where appropriate; d) assess family planning/contraceptive needs and provide advice and services or referral when indicated; e) provide appropriate inter-conception counseling including information such as recommended preconception daily intake of folic acid (400 mcg) as per CDC and ACOG guidelines and encourage a preconception visit prior to subsequent pregnancies; f) refer the infant to preventive and special care services appropriate to his/her needs; g) advise the mother/caregiver of the availability of Medicaid eligibility for infants; and h) advise or refer the mother for assistance with an application for on-going medical care assistance for herself, in accordance with her financial status, health assistance program eligibility and the policies and procedures established by the Commissioner of Health and the State of New York. i) recommend that overweight/obese women continue a nutrition and exercise regimen after pregnancy to encourage weight loss before attempting another pregnancy.29 2. The prenatal care provider shall arrange for postpartum home visitation as necessary when the mother and/or newborn may derive medical, physical and/or psychosocial benefits from such visits. 3. Postpartum documentation by the prenatal provider shall include: delivery outcome, maternal physical exam, health status of the mother/infant including medical, nutritional, psychosocial needs with referrals. Attachment 4 References 1 American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (AAP/ACOG). Guidelines for Perinatal Care, Sixth Edition. October, 2007. Chapter 2, pgs. 2 and 8. 3 ACOG Guidelines Appendix B and C pages 385 -388. 4 Maternal Fetal Medicine Society. Recommendations to Address Documentation Guidelines for level of Involvement in Consultation/co-management of Obstetric Patients, pgs. 1 – 3. 5 AAP/ACOG Guidelines, pg. 87. 6 ACOG Committee on Health Care for Underserved Women. Committee Opinion. Psychosocial Risk Factors: Perinatal Screening and Intervention, Vol. 108 (2), August, 2006; pgs. 469 – 477. 7 Medicaid currently covers up to six (6) smoking cessation counseling sessions within a 12-month period. Effective January 1, 2010, Medicaid will cover smoking cessation counseling for up to 180 days postpartum. 8 Institute of Medicine (IOM). Weight Gain During Pregnancy: Reexamining the Guidelines. Washington, DC: The National Academies Press. Posted online May 28, 2009. 9 IOM. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington, DC: The National Academies Press. Posted online May 28, 2009. 10 ACOG Committee on Obstetric Obesity. Committee Opinion. Obesity in Pregnancy, Vol. 106 (3), September, 2005; pgs. 671 – 675. 11 American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (AAP/ACOG). Guidelines for Perinatal Care, Sixth Edition. October, 2007. 12 NYSDOH 2007 Health Alert: Steps to Further Reduce Mother-to-Child HIV Transmission in New York State at: http://www.health.state.ny.us/diseases/aids/testing/healthalert.htm 13 NYSDOH 2005 Guidance for HIV Counseling and Testing and New Laboratory Reporting Requirements, Rev. 2006 14 NYS Oral Health Guidelines August 2006. http://www.health.state.ny.us/prevention/dental/oral_health_care_pregnancy_early_childhood.htm 15 Centers for Disease Control and Prevention (CDC) http://www.cdc.gov/vaccines/pubs/preg-guide.htm 16 New York State Department of Health Bureau of Immunization.at http://www.health.state.ny.us/prevention/immunization/providers/. 17 New York State Department of Health, Adult Immunization Schedule. http://www.health.state.ny.us/publications/2391.pdf 18 New York State Department of Health, Lead Exposure Risk Assessment Questionnaire. http://www.health.state.ny.us/environmental/lead/exposure/childhood/risk_assessment.htm 19 Regional Lead Resource Centers (RLRC). Contact information for RLRC can be found at http://www.health.state.ny.us/environmental/lead/regional_lead_resource_centers.htm. 20 New York State Department of Health, Lead Poisoning Prevention Guidelines for Prenatal Care Provider – NYSDOH & ACOG District II, June, 2009. Access online at: http://www.health.state.ny.us/environmental/lead/ 21 AAP/ACOG, pgs. 110-112. 22 AAP/ACOG, pg. 102. 23 ACOG Practice Bulletin, Clinical Management Guidelines for Obstetrician-Gynecologists, Ultrasonography in Pregnancy, Number 101, February, 2009. 24 ACOG Practice Bulletin, Clinical Management Guidelines for Obstetrician-Gynecologists, Invasive Prenatal Testing for Aneuploidy, Number 88, December, 2007. 25 ACOG Practice Bulletin, Clinical Management Guidelines for Obstetrician-Gynecologists. Screening for Fetal Chromosomal Abnormalities. Number 77, January, 2007. 26 ACOG Committee on Genetics. Committee Opinion. Update on Carrier Screening for Cystic Fibrosis, Vol. 106 (6), December, 2005; pgs. 1465-1468. 27 AAP/ACOG. pgs. 84-85. 28 AAP/ACOG, pgs. 111-112. 29 ACOG Committee Opinion Number 315. September, 2005, Vol. 106 (3), pg. 673. 2 AAP/ACOG, 17 Attachment 4 APPOINTMENT AVAILABILITY GUIDELINES All providers in the TOTAL CARE network will comply with the following appointment availability guidelines. • Emergency Care: Immediately upon presentation at a service delivery site. • Urgent Care. Within twenty-four (24) hours of request. • Non-Urgent “Sick” Visit: Within forty-eight (48) to seventy-two (72) hours of request. • Routine Appointments: Within four (4) weeks of request. • Specialist Referrals (not urgent): Within four (4) weeks of request. • Initial Prenatal Visit: Within three (3) weeks during first trimester, two weeks during the second trimester, and one week thereafter. • Adult Baseline and Routine Physicals: Within twelve (12) weeks from enrollment. • Well Child Care: Within four (4) weeks of request. • Initial Family Planning Visits: Within two weeks of request. • In-Plan Mental Health or Substance Abuse Follow-Up (pursuant to an emergency or hospital discharge): within five (5) days of request, or sooner as clinically indicated. • In-Plan, Non-Urgent Mental Health or Substance Abuse Visits: Within two (2) weeks of request. • Initial PCP Office Visit for Newborns: Within two (2) weeks of hospital discharge. • Provider Visits to Make Health, Mental Health and Substance Abuse Assessments for the purpose of making recommendations regarding a recipient’s ability to perform work when requested by a LDSS: within ten (10) days of request by an Enrollee, in accordance with Benefit Agreement Attachment 5 24-HOUR, 7-DAYS A WEEK ACCESS TO CLINICAL CARE TOTAL CARE provides access to medical services to its enrollees 24-hours a day, seven days a week through the network primary care providers. TOTAL CARE’s contracts with primary care providers require that each PCP assure the availability of covered health services to TOTAL CARE members on a 24-hour a day, 365 days per year basis, including periods after normal business hours, on weekends, or at any other time. The PCP must arrange for complete back up coverage from other participating providers in the event the PCP is unable to be available. Coverage and availability must allow a member to reach a live voice with one phone call. In the event the TOTAL CARE member is calling from a pay phone, or cannot receive a return call, adequate arrangements must be in place to connect the member to his/her provider. In the event the PCP is temporarily unavailable or unable to provide patient care or referral services to TOTAL CARE members, the PCP must arrange for another TOTAL CARE participating physician to provide such services. In the rate event a PCP has a non-contracted physician covering, the PCP must have prior approval of TOTAL CARE. The covering provider must sign an agreement to accept the PCP’s negotiated rate and agree not to balance bill TOTAL CARE members Attachment 5 Provider Satisfaction Survey 2013 Member Service 1. I am promptly directed to the appropriate person when I call TOTAL CARE? Yes Sometimes No 2. My issues are resolved in a timely manner? Yes Sometimes No 3. My issues are resolved accurately? Yes Sometimes No 4. The Member Service Representative is professional? Yes Sometimes No 5. The Member Service Representative is knowledgeable? Yes Sometimes No 6. The Member Service Representative understands my issue(s)? Yes Sometimes No 7. I am satisfied with the phone wait time to speak with a Member Service Representative Yes Sometimes No Authorization 8. TOTAL CARE provided authorization in a timely manner? o Yes o Sometimes o No 9. Overall satisfaction with TOTAL CARE’S authorization process o Very satisfied o Satisfied o Dissatisfied o N/A 11. Does TOTAL CARE process paid claims in a timely manner? o Yes o Sometimes o No 11. Does TOTAL CARE process paid claims accurately? o Yes o Sometimes o No Claims Processing 12. TOTAL CARE’S explanation of payment summary i ? o Easy to read and understandable o Unclear o Hard to read and unable to understand Survey Continues on the Back Pa ge Attachment 6 Provider Relations 14. My issues are resolved in a timely manner? o Yes o Sometimes o No 13. When speaking with the Provider Relations Department were you satisfied with the results of your call? o Very satisfied o Satisfied o Dissatisfied o N/A 15. My issues are resolved accurately? o Yes o Sometimes o No 16. Has TOTAL CARE provided you with timely information that affects your practice? o Yes o Sometimes o No o N/A Communication 17. Has TOTAL CARE provided you with accurate information that affects your practice? o Yes o Sometimes o No o N/A 18. Preferred method of receiving information from TOTAL CARE o Email updates o Office visits by a Provider Representative o Newsletter mailed to your office o Informational forums 19. Overall satisfaction with communication between your office and TOTAL CARE o Very satisfied o Satisfied o Dissatisfied 20. Has a TOTAL CARE Marketing Representative visited your office in the past 6 months? o Yes o No 21. Is TOTAL CARE present in your office (brochures)? o Yes o No Marketing 22 Overall satisfactions with TOTAL CARE’S Marketing Representative o Very satisfied o Satisfied o Dissatisfied Health Plex (Dental Vendor) 23. In the past year did you have to contact Health Plex? o Yes o No 25. Does Health Plex process paid claims accurately? o Yes o Sometimes o No 24. Does Health Plex process paid claims in a timely manner? o Yes o Sometimes o No 26. Overall satisfaction with Health Plex o Very satisfied o Satisfied o Dissatisfied Express Scripts (Pharmacy Vendor) 27. In the past year did you have to contact Express cripts? o Yes o No 29. Does Express Scripts process paid claims accurately? o Yes o Sometimes o No 28. Does Express Scripts process paid claims in a timely manner? o Yes o Sometimes o No 30. Overall satisfaction with Express Scripts o Very satisfied o Satisfied o Dissatisfied Med Review (Hospitals Only) 31. In the past year did you have to contact Med Review? o Yes o No 33. Overall satisfaction with Med Review o Very satisfied o Satisfied o Dissatisfied 32. Does Med Review respond in a timely manner? o Yes o Sometimes o No Attachment 6 Overall Evaluation 34. Overall does TOTAL CARE staff treat you in a professional and respectful manner? o All of the time o Sometimes o Never 35. On a scale from 1 to 5 where 1 is the “worst” health plan and 5 is the “best” health plan, how would you rate your experience with TOTAL CARE o 1- Worst health plan o 2 o 3 o 4 o 5- Best health plan TOTAL CARE would appreciate any additional comments/ suggestions you may have to improve the way we serve you and our members. About Your Office Provider Name: Specialty: Individual Responding: Title: Email: Total Care Credentialing Process Revision 12-3-12 Quality Assurance Nurse Role- Quality Assurance Nurse receives all credentialing files weekly and reviews against criteria. Nurse will note whether provider meets criteria under each criteria point. Nurse will indicate if all criteria is met or whether it requires additional review. Nurse forwards files for Medical Director Review. Medical Director reviews the initial credentialing and re-credentialing files and signs off on “clean “files. Clean files are defined as those in which no additional review is required. Medical Director roleThe Medical Director is responsible to present the credential findings to the Credentialing Committee . The Credentialing Committee has the delegated authority to approve, or approve with conditions and/or deny/terminate participation in Total Care’s network. The Medical Director will at a minimum refer for full Credentials Committee review the following: Primary Care Provider with more than 3 malpractice awards/settlements within the past 10 years Primary Care Provider with more than $1,000,000 in aggregate malpractice awards/settlements within the past 10 years Specialists with more than 5 malpractice awards/settlements >$20,000 within the past 10 years Specialists with more than $2 million in malpractice awards /settlements within the past 10 years . For the purposes of this calculation any one malpractice award/settlement is capped at $1,000,000 Any disciplinary action by NYSDOH, Medicare of Medicaid. Any criminal conviction or pending prosecution within the past 15 years. Board of Directors’ role- Delegate approval process to the Medical Director and the Credentialing Committee. The Medical Director is responsible to provide quarterly reports to the Board of Directors on the results of the credentialing process. Attachment 7 QUALITY IMPROVEMENT PROGRAM TOTAL CARE, INC. POLICY AND PROCEDURE DATE ISSUED: October 22, 2002 NUMBER: SUPERSEDES: PAGE: 051 1 OF DATED: DEPARTMENT: QA/UR AUTHORIZED BY Medical Director SUBJECT: VALID SAMPLING METHODS POLICY: It is the policy of TOTAL CARE to utilize a systematic sampling scheme to assure ongoing integrity of reports. PROCEDURE: 1. Determine the eligible member (EM) population. Develop a list including the first and last name and date of birth of the member. 2. Determine the minimum required sample size (MRSS). This will be 30 or 5% of the EM, whichever is greater. This becomes the denominator for the review. If the EM is less than the MRSS, all eligible members are included in the study. 3. Determine the final sample size (FSS). This includes the MRSS plus an adequate number of substitutions. The over sampling size is 5%. The FSS is calculated by the following formula: FSS = MRSS + (MRSS x over sampling rate) Rounding up to the next whole number. 4. Sort the list of eligible members in alphabetical order by the last name, first name and date of birth. 5. Calculate N by EM/FSS, rounding down to a whole number. 6. Calculate START=(RAND x N). Rand will always be 1. The sample will be selected from a single pass through the member list. 7. Select the sample, choosing every ith member using the formula: ith member = START + [(i-1) x (EM/FSS), rounding down to a whole number. Attachment 8 1 TOTAL CARE QUALITY IMPROVEMENT PROGRAM ORGANIZATIONAL STRUCTURE TOTAL CARE BOARD OF DIRECTORS TOTAL CARE QUALITY IMPROVEMENT COMMITTEE CASE MANAGEMENT PEER REVIEW COMMITTEE CREDENTIAL / PROVIDER NETWORKS QUALITY IMPROVEMENT PROGRAM SUBCOMMITTEES The Subcommittees listed below report to the TOTAL CARE Quality Improvement Committee. CASE MANAGEMENT/UTILIZATION REVIEW The Case Management/Utilization Review Committee is responsible to provide oversight that the Case Management Program is meeting its objectives of identifying patients with special needs. The Committee is responsible to make recommendations to the Case Management Program. The Committee is also responsible to monitor utilization trends of members on accordance with established standards, developing and implementing action plans as appropriate. The membership of the Case Management Committee is made up of the following: Certified Case Manger (Chairperson) Case Management Staff The Medical Director will present a Case Management/Utilization report to the Quality Improvement Committee on a quarterly basis. Meeting Frequency: Quarterly PEER REVIEW COMMITTEE The Peer Review Committee is responsible for monitoring provider performance. The Committee will review provider profiling and fraud & abuse data that specifically involves provider issues. The Committee is responsible for reviewing the impact of clinical policies and procedures for providers and the members. The Committee will serve as clinical resource to the Medical Director. The Committee membership may vary based on the protocols under review. The Medical Director will present a Peer Review Committee report to the Board of Directors minimally on a quarterly basis. The membership of the Peer Review Committee is made up of the following: TOTAL CARE Medical Director/Assistant Medical Director (Chairperson) Primary Care Providers OB/GYN Provider TOTAL CARE Director of Audit/Cost Containment Senior Director Health Care Services Meeting Frequency: Quarterly. May be called to meet more frequently on an ad hoc basis. CREDENTIAL/PROVIDER NETWORK This Committee is chaired by the Medical Director/Assistant Medical Director. The Committee is responsible to provide oversight of the credentialing and re-credentialing procedures for the Plan. The Committee is responsible to approve the delegated and/or outsourced programs engaged by the Plan. The Committee reviews and comments on the tools and procedures used to monitor any delegated or outsource agreements. The Committee is responsible to approve recommended providers consistent with the defined criteria as applicable (i.e., NYSDOH, NCQA). The Committee will review provider grievances in regard to performance and/or credentials. The Medical Director will provide the Board of Directors with reports of this Committee minimally on a quarterly basis. The membership of the Credential/Provider Network Committee is made up of the following: TOTAL CARE Medical Director TOTAL CARE QA Director TOTAL CARE UR Director Provider Relations /Contracting Coordinator Chief Operating Officer Designated Physicians Meeting Frequency: Quarterly. May be called to meet more frequently on an ad hoc basis. QUALITY IMPROVEMENT PROGRAM 2014 QUALITY IMPROVEMENT COMMITTEE CALENDAR JANUARY MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT FEBRUARY MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT 2011 QI PLAN REVIEW STATUS REPORT UPDATE CASE MANAGEMENT COMMITTEE REPORT MARCH MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT FOCUSED CLINICAL STUDY ER REVIEW SCHC/TC COLLABORATIVE REPORT APRIL MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT MOST FREQUENT DIAGNOSIS BY MEMBER PHARMACY REPORT CASE MANAGEMENT COMMITTEE REPORT MAY MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT MORBIDITY/MORTALITY REPORT JUNE MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT FOCUSED CLINICAL STUDY HOSPITAL ADMISSIONS PER MEMBER JULY MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT LACK OF SERVICE UTILIZATION PHARMACY REPORT PREAUTHORIZATION REVIEW CASE MANAGEMENT COMMITTEE REPORT PROVIDER SATIFACTION SURVEY AUGUST MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT HIV REVIEW FOCUSED CLINICAL STUDY MEDICAID PRENATAL GUIDELINES REVIEW (INCLUDING CHECKUPS AFTER DELIVERY) HPN REPORT (2ND QUARTER 2014) SEPTEMBER MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT CHILD/TEEN GUIDELINES REPORT ADULT PREVENTIVE GUIDELINES STD FOLLOW UP OCTOBER MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT PHARMACY REVIEW NEWBORN TRACKING (INCLUDING LOW BIRTH WEIGHT) INFORMED CONSENT REPORT CASE MANAGEMENT COMMITTEE REPORT ACCESS AND AVAILABILITY NOVEMBER MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT FOCUSED CLINICAL STUDY REVIEW OF CLINICAL GUIDELINES SCHC / TC COLLABORATIVE REPORT MEDICAL RECORD DOCUMENTATION HPN REPORT (3RD QUARTER 2014) DECEMBER MEMBER SERVICES REPORT CREDENTIALING COMMITTEE REPORT 2013 QI CALENDAR WAIT TIME STUDY QARR UTILIZATION REPORT/QARR RESULTS REPORTED ON AS RECEIVED NYSDOH ANNUAL SITE SURVEY REPORT (ANNUAL) ROOT CAUSE ANALYSIS UPDATES (AS RECEIVED FROM NYSDOH) MEMBER SATISFACTION SURVEYS (AS RECEVIED BY LDSS/NYSDOH) NYSDOH CAHPS SURVEY (BIANNUAL) HPN/CREDENTIALING REPORT (QUARTERLY REPORT FROM DOH) QUALITY IMPROVEMENT COMMITTEE CALENDAR EXPLANATION SHEET 2014 ACCESS AND AVAILABILITY (ACCESS TO SERVICES) Provider Relations staff (using IPRO Guidelines for Access and Availability Surveys) will do telephone surveys of provider offices. Report will be presented to QI Committee annually. (Attachment 6) Medicaid Contract Section 15-Access Requirements Medicaid Contract Section 18-Appointment Availability ADULT PREVENTIVE SERVICES: A random sample (Attachment 8) of members greater than 21 years of age who have been continuously enrolled for one year, and have had a preventive care visit, will be reviewed using TOTAL CARE’s Adult Preventive Guidelines as criteria of care. Reporting to the QI Committee will be annual. (Attachment 2) Medicaid Contract Section 16.2 CASE MANAGEMENT COMMITTEE REPORT: On a quarterly basis a summary of the Case Management Committee activities will be presented to the QI Committee. Medicaid Contract Section 10.19 CHILD TEEN HEALTH GUIDELINES: A random sample of members ages 0 through 21 years of age who have been continuously enrolled for one year, and have had a well visit, will be reviewed using Child Teen Health Guidelines as criteria for care. Reporting to the QI Committee will be annually. (Attachment 3) Medicaid Contract Section 10.4-Child Teen Health Program/Adolescent Preventive Services CREDENTIALING COMMITTEE REPORT: Minimally, on a quarterly basis a summary of the Credentialing Committee activities will be presented to the QI Committee. Medicaid Contract Section 21.4a ER REVIEW: Administrative data will be reviewed to determine emergency room utilization including most common diagnosis and high users of Emergency Room Services. Data will be presented to the Quality Improvement (QI) Committee annually. Medicaid Contract Section 10.19 FOCUS STUDY (PERFORMANCE IMPROVEMENT PROJECT) 20132014:Improving Performance in Chronic Disease Prevention and Management: Total Care is participating in the statewide Initiative. Updates will be provided to the QI Committee quarterly. Medicaid Contract Section 18.6 HIV REVIEW: Data will be reviewed for members identified with HIV (+) diagnosis to determine if member is receiving care from PCP or specialty clinic per established guidelines. A report will be submitted to the QI Committee on an annual basis. Medicaid Contract Section 10.22 Medicaid Contract Section 15.8 – Specialist as Coordinator of Primary Care HOSPITAL ADMISSIONS PER MEMBER: On an annual basis, a review of claims data will be presented indicating number of members with more than 2 hospitalizations, length of stay and reasons for admission. Medicaid Contract Section 10.19 HPN REPORT-Quarterly report discussing NYSDOH evaluation of Total Care Provider Network Adequacy Medicaid Contract Section 21.1 Network Requirements INFORMED CONSENT FOR TUBALS AND HYSTERECTOMIES: A random sample of members receiving hysterectomies or tubal ligations will be reviewed to determine whether proper consent has been obtained prior to surgery. A report will be submitted to the QI Committee on an annual basis. Medicaid Contract Section 35.7- Informed Consent for Hysterectomy and Sterilization LACK OF SERVICE UTILIZATION: On an annual basis, review of members who did not utilize plan services within 6 months of enrollment will be performed on non-use of services. Medicaid Contract 13.6 LOW BIRTHWEIGHT (see Newborn Tracking) MEDICAL RECORDS DOCUMENTATION: PCPs, with 6 or more members, will each have six (6) records reviewed at random to determine compliance with Medical Record Documentation Standards. This review may occur at the time chart reviews for other criteria are occurring, or if necessary from a separately selected random sample. Reporting to the QI Committee will be annual. (Attachment 1) As reviews are conducted, results will be communicated to providers and issues reported to Medical Director NYCRR10 Part 98-1.13f MEMBER SATISFACTION: Surveys completed periodically by the Local Department of Social Services and the bi annual New York State Member Satisfaction Survey will be presented as received. NYCRR10 Part 98- 1.12 MEMBER SERVICES REPORT: On a quarterly basis, member complaints, including those resulting in Physician transfers, (with identified trends, both numerical aggregates and appropriate details of complaints) will be presented to the QI Committee after the complaint report to the state. Quarterly, the enrollment report, no contact report and phone statistics will be presented on a rotating basis. Results of the member services satisfaction survey will be presented monthly. Medicaid Contract Section 14 (Grievance) Medicaid Contract Section 13.6 NYCRR10 Part 98- 1.12 MORBIDITY AND MORTALITY REVIEW: A summary of mortalities will be presented to the QI Committee minimally on an annual basis. NYCRR10 Part 98-1.12(d) (e) MOST FREQUENT DIAGNOSIS BY MEMBER: On an annual basis, a review of claims data will be done to determine most frequently used diagnosis by members for primary care and specialty services. Medicaid Contract Section 10.19 NEW ENROLLEE HEALTH SCREENING REPORT – On a quarterly basis, a summary of new enrollee health screenings that result in an addition of a member to case management will be reported to the committee. Medicaid Contract Section 13.6a NEWBORN TRACKING- Annual review to monitor introduction into Primary Care within 4 weeks of birth. Report will include the total number of infants with a birth weight under 2500 grams for birth outcome as well as mother’ prenatal record TOTAL CARE AREA OF CONCERN-Identified as High Volume Population NUMBER OF VISITS PER MEMBER ACCORDING TO BASIC AGE CATEGORIES: On an annual basis, charts will be audited as indicated for at least 5%, or 30, whichever is more of members generating more than projected visits by age group (using Department of Health age guidelines). The review will be coordinated by the QA/UR Director. NYSDOH Requirement NYSDOH CAHPS SURVEY- Report as received from NYSDOH Part of QARR Reporting PHARMACY REVIEW: The QI reports submitted to TOTAL CARE by its pharmacy manager will be presented to the QI Committee minimally on a quarterly basis. Vendor Oversight REAUTHORIZATION REVIEW: A random sample of authorizations will be reviewed to determine compliance with NYSDOH standards. Reports will be presented to the QI Committee annually. Medicaid Contract Section 16-Utilization Management Guidelines Medicaid Contract Appendix F- Action and Grievance System Requirements PROVIDER SATISFACTION SURVEY: The Provider Relations staff will conduct a satisfaction survey of providers on an annual basis. The report will be submitted to the QI Committee on an annual basis. (Attachment 7) Medicaid Contract Section 22.5g QARR 2013 ROOT CAUSE ANALYSIS UPDATE: Summary reports of activities to improve rates for Lead Screening, Adult BMI and Breast Cancer Screening will be presented to the QI Committee during the year as reviews are done by NYSDOH Medicaid Contract Section 16.1b QARR 2014: The QARR results will be presented to the QI Committee on an annual basis. Medicaid Contract Section 18.6 QARR UTILIZATION REPORT – Administrative data will reviewed to determine inpatient, outpatient, Emergency Room Utilization and Frequency of Selected Procedures including trends. Reporting will be annual Medicaid Contract Section 18.6 QI PLAN ANNUAL REVIEW: The TOTAL CARE QI plan will be reviewed minimally on an annual basis to determine effectiveness of plan. Medicaid Contract Section 16- Quality Assurance NYCRR Part 98-1.12 SCHC / TC COLLABORATIVE REPORT: A specifically identified area of study agreed upon between Total Care and Syracuse Community Health Center will be reviewed and reported on monthly. Targeted reporting will center around QARR indicators and interventions implemented to maximize overall Quality of Care TOTAL CARE AREA OF CONCERN-Identified as High Volume Population STD FOLLOWUP: A sample using random sampling methodology of members treated or screened for STD’s will be reviewed annually. Medicaid Contract Section 10.18c- Prevention and Treatment of STD’s USE OF MENTAL HEATLH AND SUBSTANCE ABUSE SCREENING TOOL: Using the samples for Adult Preventive Services and Child Teen Health Guidelines or Medical Record Documentation, charts will be reviewed for Mental Health and Substance Abuse Screening and use of any specific tools for such screening. Reporting to the QI Committee will be annually. Medicaid Contract Section 10.21 WAIT TIME SURVEY: On an annual basis, a review is conducted to determine length of time experienced by members in the waiting room while in the office of participating PCP and OB/GYN providers. Medicaid Contract Section 15-Access Requirements MEDICAID PRENATAL GUIDELINES COMPLIANCE (including Checkups after Delivery): A random sample of members delivering in 2012-2013 who were continuously enrolled 4 months prior to delivery and two months post-delivery will be reviewed using the Medicaid prenatal guidelines as criteria of care. Reporting to the QI Committee will be annual (Attachment 4). Medicaid Contract Section 10.11 2015 QI CALENDAR: The TOTAL CARE QI calendar will be reviewed minimally on an annual basis to determine effectiveness and frequency of QI activities. Medicaid Contract Section 16-Quality Assurance QARR ACTIVITIES MONITORING 2014 BY MEASURE 1. Adult BMI HYBRID MEASURE-MEDICAL RECORD REVIEW REQUIRED 2013 Performance 82.70 % (increase from last reported rate in 2012-50.12 %) 2013 Statewide Average 79.00% GOAL- 90th Percentile of 2013 Average: 71.10% Member Outreach Not planned Provider Outreach • Providers will receive a targeted mailing which will describe this measure and include a case study of SCHC’s improvement. This mailing will include additional information on how Total Care providers can access tools and resources from the health plan to operationalize the program SCHC put in place. The article will also provide codes which capture BMI Assessment. • Monitoring of Provider patterns in May, June, and July 2014 to review sample of records for all Adult Preventive Health guidelines • Targeted weekly group meeting with Large Provider Group. Members of the committee include Site Medical Director, Director of Nursing, Quality Director, Reimbursement Specialist, Total Care Medical Director, Total Care VP/COO and Total Care QA Director. Performed analysis of what the barriers are. Adult Flow Sheets revised to include BMI as part of vital signs measurement. BMI added to GYN visit note for documentation by GYN staff. Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre- QA Nurse Monitoring Mechanism: Sample of 100 Medical Records Monitoring Frequency: Monthly beginning August 2014 2. Annual Monitoring for Patients on Persistent Medications 2013 Performance-89.97% (improved from 2012 Performance 89.00%) 2013 State Average – 90.00% Goal – 90th Percentile of State Average: 81.00% Member Outreach • Quarterly Member Mailing - Member letter to all affected members encouraging compliance sent quarterly. Mailing will be sent again during 2014 end of year push. • Case Management - Members will be entered into case management in which they will receive education on their medications and importance of compliance. Case managers will monitor individuals with history of non-compliance closely. Case Managers will send out mailings to all members in this group to inform them about compliance and remind them about refilling their prescriptions on time. • Quarterly Outbound Calling - Televox outbound calling (May, July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • End of Year Outbound Calling - Member Services will begin making live telephone contact with members during end-of-year push in September 2013 to stress importance of labs. Will assist in scheduling appointments if needed. • Healthy Rewards Incentive Program – Members will be notified of incentive program and eligibility through targeted member mailing at end of year as well as birthday card mailings throughout the year. Provider Outreach • Mailing to all providers and onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. • Provider Gap in Care Reports - Notification to providers of all members (May 2014 and July 2014) in their panel who are in need of service by end of measurement year (December 31, 2014). List will be revised in October 2014. List will be provided more frequently between July and October 2014. Incentive (member) $ 25 Gift Card for successful completion of required Lab Studies at Large Provider Site Incentive (Provider) $15 Provider Incentive Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntryre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 3. Antidepressant Medication Management 2013 Performance - 51.11% (Acute Phase, up from 2012 – 49.00%) 2013 State Average – 51.00% (Acute Phase) 2013 Performance – 37.00% (Continuing Phase, up from 2012 – 32.00%) 2013 State Average – 37.00% (Continuing Phase) Goal- 90th Percentile 2013 Acute Phase: 45.90%, Continuing Phase: 33.30% Member Outreach • Case Management – All eligible members will be offered case management. Case Managers will conduct a Behavioral Health Assessment and develop a care plan. Case Managers will assure member has access to PCP and medications. • Targeted Member Mailing - All members on acute phase medications will be sent a letter from the case manager reminding them about refilling their medications on a timely basis. This letter will include education about their antidepressant medications and will also include contact information for their case manager. Provider Outreach • Collaboration effort with large provide provider groups to use Pharmacy data for member identification. • Identify behavioral health vendor and delegate this function and measure responsibility. • Description of measure included in Provider Tip Sheet. Incentive (member) Not Planned Incentive (Provider) Not Planned Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning September 2014 4. Use of Appropriate Medications for People with Asthma Measure rotated in in 2014 Goal – 90th Percentile Member Outreach • Case Management – Case Managers will outreach to members who have visited the ER with diagnosis of asthma, inpatient admission with asthma, or multiple clinic visits with asthma. • Case Management – Case Managers will open cases and outreach to all members with asthma. Case manager will provide education on asthma and discuss asthma medications. • Year Round Outbound Calling - Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. Provider Outreach • Questionnaire sent to PCP asking if the member has a follow up visit and medication history. Provider is asked if member is appropriate for Case Management services. • Provider Gap in Care Reports - Notification to providers of all members (May 2014 and July 2014) in their panel who are in need of service by end of measurement year (December 31, 2014). List will be revised in October 2014. List will be provided more frequently between July and October 2014. Incentive (member) none Incentive (Provider) $100 Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 5. Appropriate Testing for Pharyngitis 2013 Rate-70.85% (decrease from 76.00% in 2012) 2013 State Average – 87.00% Goal- 90th Percentile – 78.30% Member Outreach Provider Outreach Not Planned • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. This nurse will ask providers and determine if Point of Care testing is available, being used and appropriately coded for. • Community Quality Nurse Consultant will perform retrospective medical record review at Urgent Care sites to determine if measure specifications are being followed. Once review is complete, provider sites will be visited to reinforce expectations. • Provider education through newsletter articles to reinforce the judicious use of antibiotics. Incentive (member) Not Planned Incentive (Provider) Not Planned Comments: Use of Supplemental Database Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning May 2014 6. Appropriate Treatment for Upper Respiratory Infection (URI) 2013 Rate 87.13%, increase from 84.00% in 2011 2013 State Average 93.00% Goal-90th Percentile: 83.70% Member Outreach Not Planned Provider Outreach • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. Provider education to reinforce the judicious use of antibiotics including patient education is also provided regarding supportive care for viral infections. • Encounter reconciliation done at large provider group to include appropriate coding for URI Incentive (member) Not Planned Incentive (Provider) Not Planned Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning May 2014 7. Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis 2013 Rate-33.95%-increase from 18.00% in 2012 2013 Statewide Average – 24.00% Goal-90th Percentile – 21.60% Member Outreach Not Planned Provider Outreach • Provider education regarding the viral etiology of greater than 90% of uncomplicated acute bronchitis. • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. The nurse will also discuss appropriate coding of all and any additional diagnoses to justify antibiotic therapy Incentive (member) Not Planned Incentive (Provider) Not Planned Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning July 2014 8. Breast Cancer Screening 2013 Rate- 71.21%, increase from 2011 rate of 63.78% 2013 Statewide Average – 68.00% Goal 90th Percentile – 61.20% Member Outreach • Quarterly Outbound Calling - Televox outbound calling in May and July 2014 encouraging members to make an appointment. • Total Rewards Incentive Program – Members will be notified of incentive program and eligibility through targeted member mailings throughout the year. • End of Year Mailing - Mailings to members to encourage mammography screening. Letter for 2014 lists all sites for mammography screenings including phone numbers and hours of operation so member can easily make appointment. Additionally, a joint letter will be sent from Total Care and SCHC for SCHC members. • End of Year Outbound Calling - Member Services Department will begin outbound calling in September 2014 to encourage screening and assist in making appointments or other barriers to care. Provider Outreach • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. The Consultant will share list of sites patients can receive screening with providers. • Targeted article in Provider newsletter to reinforce TOTAL CARE’s policy and expectations regarding mammography (Fall 2014) • Provider Gap in Care Reports - Notification to providers of all members (May 2014 and July 2014) in their panel who are in need of service by end of measurement year (December 31, 2014). List will be revised in October 2014. List will be provided more frequently between July and October 2014. • SCHC - SCHC dedicates at least one day per month in which Total Care members can come for mammography services. Members are called by SCHC prior to appointment. Incentive (member) $25 gift card for members timely receiving service Incentive (Provider) Not Planned Comments $ amount for member incentive was raised from $10$25 in 2012. Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 9. Cervical Cancer Screening 2013 Rate-69.47%, similar from 2012 Rate (69.00%) 2013 Statewide Average – 71.00% Goal 90th Percentile – 63.90% Member Outreach • Mailings to members to encourage cervical cancer screening. Additionally, a joint letter will be sent from Total Care and SCHC for SCHC members. • End of Year Member Mailing - Member letter to all affected members encouraging compliance sent during end of year push in 2013. Mailing will be sent again during 2014 end of year push. • Quarterly Outbound Calling - Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • End of Year Outbound Calling - Member Services will begin making live telephone contact with members during end-of-year push in September 2014 to stress importance of screening. Will assist in scheduling appointments if needed. Provider Outreach • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure and discuss women’s health preventive care gaps in care. Incentive (member) Not Planned Incentive (Provider) Not Planned Comments Use of Supplemental Database Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 10. Chlamydia Screening 2012 Reported Rate-69.54 (combined) % -increase from 62.00% in 2011 Goal -90th Percentile 2011-74.81% Member Outreach • Mailings to members (age >20 years) to encourage chlamydia screening. Additionally, a joint letter will be sent from Total Care and SCHC for SCHC members. • End of Year Member Mailing - Member letter to all affected members encouraging compliance sent during end of year push in 2013. Mailing will be sent again during 2014 end of year push. • Year Round Outbound Calling - Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • End of Year Outbound Calling - Member Services will begin making live telephone contact with members during end-of-year push in September 2014 to stress importance of screening. Will assist in scheduling appointments if needed. Provider Outreach • Provider Gap in Care Reports - Notification to providers of all members (May 2014 and July 2014) in their panel who are in need of service by end of measurement year (December 31, 2014). List will be revised in October 2014. List will be provided more frequently between July and October 2014. • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. • Provider Incentive Program – Total Care providers are incentivized to conduct chlamydia screening for eligible members through a $25 payment per member. • SCHC- Urine GC/ Chlamydia NAAT ordered at age appropriate adolescent preventive care visit. Urine Chlamydia NAAT ordered at all reproductive health visits inclusive of GYN, SBHC, WIC, Adult Medicine & Family Medicine clinical areas. Incentive (member) Incentive (Provider) Comments Not Planned $ 20 Use of Supplemental Database 11. Comprehensive Diabetes Rotated Measure in 2012 Indicators-Last Reported Rates in 2011 HgbA1c-91.42% Poorly Controlled 33.21% <8-56.75% LDL Screening-82.66% <100 42.15% Retinal Eye Exam-61.13% Nephropathy Testing-79.74% Blood Pressure Control- <140/80-47.45% <140/90-75.73% Composite- All 4 Tests (HgbA1c, LDL Screening, Retinal Eye Exam and Nephropathy Testing)-44 % Indicators-90th Percentile in 2011 Composite- All 4 Tests (HgbA1c, LDL Screening, Retinal Eye Exam and Nephropathy Testing)-56.54% Blood Pressure Control-<140/90-75.70% Member Outreach • Case Management - All diabetic members will be entered into case management and receive two phone calls a year, at a minimum. The case management program will include a review of other chronic conditions and screen for behavioral issues. Case managers will provide disease management education and will mail educational pamphlets about controlling diabetes. • Targeted Member Mailing - Mailings to members to encourage all screenings in July 2014. Letter also lists all sites for Eye Exams including phone numbers and hours of operation so member can easily make appointment • Quarterly Outbound Calling - Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • End of Year Member Mailing - Member letter to all affected members encouraging compliance sent during end of year push in 2013. Mailing will be sent again during 2014 end of year push. • End of Year Outbound Calling - Member Services will begin making live telephone contact with members during end-of-year push in September 2014 to stress importance of labs. Will assist in scheduling appointments if needed. • Total Rewards Incentive Program - Members will be notified of Total Rewards Incentive Program and $25 incentive for completing all four components of this measure. Provider Outreach • Provider Gap in Care Reports - Notification to providers of all members (May 2014 and July 2014) in their panel who are in need of service by end of measurement year (December 31, 2014). List will be revised in October 2014. • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure (completion of all four components) and review coding concerns. Incentive (member) $25 gift card for members timely receiving service Incentive (Provider) all 4 tests-$100 HgbA1c <8.0-8.9-add’l $50 HgbA1c <8-add’l $50 LDL <100-add’l $ 50 Comments Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 12. Controlling High Blood Pressure HYBRID MEASURE-MEDICAL RECORD REVIEW REQUIRED 2013 Rate – 70.32%, increased since 2012 at 68.00% 2013 Statewide Average – 63.00% Goal – 90th Percentile 2013 – 56.70% Member Outreach • Targeted Member Mailing - Mailings will be sent to members with high blood pressure to encourage screening in July 2014. The mailing will encourage Patients ages 18 – 85 years with documented hypertension to have their blood pressure rechecked appropriately prior to end of PCP visit; follow up visits will be scheduled to reassess blood pressure measurements. • Quarterly Outbound Calling - Televox outbound calling (May 2014 and July 2014) to remind members about this screening. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • End of Year Member Mailing - Member letter to all affected members encouraging compliance sent during end of year push in 2013. Mailing will be sent again during 2014 end of year push. • End of Year Outbound Calling - Member Services will begin making live telephone contact with members during end-of-year push in September 2014 to stress importance of labs. Will assist in scheduling appointments if needed. Provider Outreach • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. This nurse will ask providers and determine if screening is available, being used and appropriately coded for. Incentive (member) Incentive (Provider) Not Planned Not Planned Key Responsible Person: Cathy Brigden Assigned Person: Lisa McIntyre Monitoring Mechanism: Sample of 100 Medical Records Monitoring Frequency: Monthly beginning September 2014 13.Drug Therapy for Rheumatoid Arthritis 2013 Rate-71.93%, increased from 68.00% in 2012 2013 Statewide Average – 78.00% Goal 90th Percentile 2013 – 70.20% Member Outreach • Case Management - All members in this population will be entered into case management. Case Managers will conduct an assessment, assure members understand importance of the appropriate use of their medications, and resolve any barriers to refilling their drug therapy. • Targeted Member Mailing - Mailings to members to encourage compliance to medications and treatment in June 2014 and August 2014. • Quarterly Outbound Calling - Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • End of Year Member Mailing - Member letter to all affected members encouraging compliance will be sent during end of year push in 2014 • End of Year Outbound Calling - Member Services will begin making live telephone contact with members during end-of-year push in September 2014 to stress importance of their treatment plan. Will assist in scheduling appointments if needed. Provider Outreach • Onsite follow up by Community Quality Nurse Consultant to providers to encourage proper DMARD medications for Rheumatoid Arthritis to review specifications of the measure. • Quarterly list to providers of members with gaps in care. • Collaboration effort with large provide provider groups to use Pharmacy data for member identification. Incentive (member) Not Planned Incentive (Provider) $100 Provider Incentive Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 14. Follow-up After Hospitalization for Mental Illness 2013 Rate-44.44%(7 day follow up)- Decrease from 2012 rate-66.33% 2013 Statewide Average – 48.00% Goal – 90th Percentile 2013 – 43.20% Member Outreach • Case Management - Case Managers will reach member prior to or upon discharge to assure contact, assure follow-up appointment has been made, facilitate transportation, and ensure PCP is aware of the discharge plan. Provider Outreach • Request confirmation from facility that member has an outpatient appointment scheduled within 7 days. Member needs to have appointment made before discharge. • Outreach to facilities who have inpatient Mental Health units. Reinforce the appointment needs to be kept no later than 7 days from discharge. If a timely appointment cannot be made, the facility must call Total Care to redirect the appointment to a provider who can accommodate the patient within 7 days. Incentive (member) Incentive (Provider) Comments Not Planned Not Planned Use of Supplemental Database 15. Follow-Up Care for Children Prescribed ADHD Medication 2013 Rate- 55.00% (Initiation Phase), down from 61.00% in 2012 2013 Statewide Average – 57.00% Goal- 90th Percentile 2013 – 51.30% Member Outreach • Case management – All children prescribed ADHD medications will be offered case management. Case Managers shall monitor understanding of child as well as supervising parental and help receive refills. Provider Outreach • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. • Collaboration effort with large provide provider groups to use Pharmacy data for member identification. SCHC Initiation phase- schedule follow up after initial prescription within 2 – 3 weeks. Monitor compliance and reschedule non-compliant patients by 4 weeks. Maintenance phase – Ensure follow up ADHD patients following initiation and stabilization of therapy every 2 – 3 months. Adjunctive support for this measure includes Provider, nursing and ancillary staff education. Incentive (member) Not Planned Incentive (Provider) Not Planned Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 16. HIV/AIDS Comprehensive Care 2013 Rate-Engaged In Care 94.12%, Increase from 2012 rate 83.08% 2013 Statewide Average – 72.00% Goal-90th Percentile 2013-64.80% Member Outreach • Case Management – All eligible members are offered case management. Coordinate outreach efforts through Case Management provided by HIV clinics. Track member every 4 -6 months via form to 4 ID Clinics: SCHC, St. Joe’s, SUNY and Ivy Clinic at Arnot–Ogden Hospital. Information is requested regarding dates of PCP visits, Viral Load monitoring tests and Syphilis Screening. • Targeted Member Mailing - Mailings to members to encourage compliance to medications and treatment in June 2014 and August 2014. • End of Year Member Mailing - Member letter to all affected members encouraging compliance sent during end of year push in 2013. Mailing will be sent again during 2014 end of year push. • End of Year Outbound Calling - Member Services will begin making live telephone contact with members during end-of-year push in September 2014 to stress importance of labs. Will assist in scheduling appointments if needed. • Total Rewards Incentive Program - Members will be notified of Healthy Rewards Incentive Program and $25 incentive for completing test. Provider Outreach • Outreach to providers caring for HIV members regarding specifications of measure. Outreach to providers and members by May 15, 2014 to ensure members have had the first visit in 2013 by June 30, 2013. This initiative will be repeated in 2014. • Notification to providers of all members (July 2014) in their panel who are in need of service by end of measurement year (December 31, 2014). List will be revised in October 2014. Incentive (member) $25 for Viral Load Monitoring Incentive (Provider) Not Planned Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 17. Immunizations for Adolescents HYBRID MEASURE-MEDICAL RECORD REVIEW REQUIRED 2012 Reported Rate-Combined-71.53% increase from 2011 rate of 57.91% Statewide Average 2011 (New measure in 2011) - 67% Goal – Member Outreach • Outreach efforts will be coupled with efforts for adolescent well care visit. Provider Outreach • Notification to providers of all members in their panel who are in need of service. List will be revised in October 2014. SCHC Procedure: Provider education regarding ACIP/CDC/AAP immunization schedules & SCHC Preventive Care Recommendations. Administer Tdap at 6th grade entry or 10 – 13 years .Meningococcal conjugate#1 at 11-12 yrs. Incentive (member) Incentive (Provider) Comments Not Planned Not Planned New Measure. Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Sample of 100 Medical Records Monitoring Frequency: Monthly beginning July 2014 18. Pharmacotherapy Management of COPD Exacerbation 2012 Reported Rate- Bronchodilator 80%-increase from 2011 rate of 70.97% Goal-90th Percentile 2011-89.72% Member Outreach • Case Management - Members will be entered into Case Management where they will receive an assessment, education on disease process, and a review of the treatment plan. • Targeted Member Mailing - Mailings to members to encourage compliance to medications and treatment in June 2014 and August 2014. • Quarterly Outbound Calling - Televox outbound calling (May 2014 and July 2014) to remind members about this screening. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • End of Year Member Mailing - Member letter to all affected members encouraging compliance sent during end of year push in 2013. Mailing will be sent again during 2014 end of year push. • End of Year Outbound Calling - Member Services will begin making live telephone contact with members during end-of-year push in September 2014 to stress importance of labs. Will assist in scheduling appointments if needed. • Total Rewards Incentive Program - Members will be notified of Total Rewards Incentive Program and $25 incentive for completing test. Provider Outreach • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant reviewing specifications of the measure, prescribing patterns, and coding. • Quarterly notification of members with gaps in care. • Collaboration effort with large provide provider groups to use Pharmacy data for member identification. Incentive (member) Not Planned Incentive (Provider) $100 Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning September 2014 19. Use of Imaging Studies for Low Back Pain 2013 Rate-71.69%, decrease from 2012 rate of 73.72% 2013 Statewide Average – 78.00% Goal 90th Percentile 2013 – 70.20% Member Outreach Not Planned Provider Outreach • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. Provider education to reinforce the judicious use of radiology procedure for diagnosis of Low Back Pain in the first 30 days after diagnosis including patient education is provided regarding supportive care Encounter reconciliation done at large provider group to include appropriate coding for Low Back Pain Incentive (member) Not Planned Incentive (Provider) Not Planned • Key Responsible Person: Jennifer Skotniski Assigned Person: Faith Timerson Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning July 2014 20. Use of Spirometry Testing in the Assessment and Diagnosis of COPD 2013 Rate-43.61%, increase from 2012 rate of 31.79% 2013 Statewide Average – 53.00% Goal – 90th Percentile 2013 – 47.70% Member Outreach • Mailing to all members eligible for measure educating members about importance of visit and availability of incentive program (August 2014). Mailing will be improved in 2014 to include an image of the type of test so as not to confuse from other noneligible breathing tests. • Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • Member Services will begin making telephone contact with members directly during end-of-year push in September 2014. Will assist in scheduling appointments if needed. • Members in this population will be entered in Case Management. Case Managers will conduct an assessment, provide education on disease process, and review the treatment plan with the member. Provider Outreach • Onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure. • Notification to providers of all members (July 2014) in their panel who are in need of service by end of measurement year (December 31, 2014). List will be revised in October 2014. • Article in provider newsletter reminding providers of measure requirements and coding. Incentive (Member) Incentive (Provider) $25 $100 Comments Small Eligible Population (133 in 2012) Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 21. Annual Dental Visit 2013 Rate-33.33% (age 19-21), decreased from 2012 Rate of 44.00% 2013 Statewide Average – 44.00% Goal-90th Percentile 2013-39.60% Member Outreach Outreach by Dental Benefit Manager (HealthPlex) to members in need of visit to Primary Care Dentist. They have implemented a member incentive effective June 2013. Provider Outreach Onsite follow up at top 10 high volume providers reviewing specifications of the measure. Reminders to PCP to encourage annual dental visit beginning at age 2. See Healthplex Provider Incentive Program Supplement. SCHC Procedure: Referrals for annual dental visits starting at 12 months of age by medical providers. QI reports to monitor compliance by age groups. Incentive (member) Through HealthPlex program Incentive (Provider) Not Planned Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning October 2014 22. Timeliness of Prenatal Care HYBRID MEASURE-MEDICAL RECORD REVIEW REQUIRED 2013 Rate- 86.86%, 2011 Rate – 87.00% Rotated Measure 2011 2013 Statewide Average – 88.00% GOAL – 90th Percentile 2013 – 79.20% Member Outreach • Case management will be offered to all pregnant women. Case manager will conduct a prenatal care assessment, provide prenatal education, and conduct ongoing assessment to detect any changes in the course of the pregnancy. Case manager will assure appropriate referral to perinatology or Maternal-Fetal Medicine (MFM) for pregnancies which become high-risk. • Member education will include information on the importance of gestational diabetes, appropriate and inappropriate weight gain, nutrition, preeclampsia, and signs and symptoms of preterm labor as well as the importance of initial well child visits and lead safety upon child birth. Materials and handouts will be shared with members as needed. • Case Managers will call all members upon notification of delivery. Case Managers will notify hospital discharge planners to schedule an initial well child visit for the newborn as well as a postpartum visit for the mother. Provider Outreach • Onsite follow up at top 10 high volume PCP and OB/GYN providers by Community Quality Nurse Consultant reviewing specifications of the measure. • Provider relationship with OB/GYN specialists to foster strong communication about the member’s care. • Notification of delivery from hospitals prior to discharge. • Encourage Expedited initial assessment within 7 days of confirmation of pregnancy. Aggressive patient education regarding the importance early entry to prenatal care at PCP or OB/GYN visits. • Increase identification of newly diagnosed pregnancy by using DOH roster indicator Incentive (member) Incentive (Provider) Not Planned Not Planned Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Sample of 100 Medical Records Monitoring Frequency: Monthly beginning July 2014 23. Postpartum Care HYBRID MEASURE-MEDICAL RECORD REVIEW REQUIRED 2013 Rate-72.51%-Increase from 2010 rate of 70.07% (Rotated Measure in 2012) 2013 Statewide Average – 70.00% Goal-90th Percentile 2013 Average – 63.00% Member Outreach • Case Managers conduct outreach telephone call to all members within 2 weeks of delivery. During the outreach call, Case Managers will stress the importance of the postpartum visit and help members identify and provide access to community resources. • Case Managers send a letter to all eligible members (upon notification of delivery) informing them about the importance of the visit as well as the Healthy Rewards Incentive Program. Provider Outreach • • • Onsite follow up at top 10 high volume PCP and OB/GYN providers reviewing specifications of the measure. Case Managers share documentation of delivery with members PCP or OB/GYN Work with Discharge staff at facilities to ensure member has OB/GYN appointment prior to discharge SCHC Post partum visit appointments within 21-42 days provided to patients prior to hospital discharge. Post partum appointments are checked and scheduled by the Pediatric staff during the newborn visits. Pediatric Health Care Providers focus on maternal health and well being, encouraging maternal compliance with care. Outreach from OB charge nurse or designee, closely monitoring compliance and rescheduling appointments as needed. Outreach through pregnancy care case management staff. Incentive (member) Incentive (Provider) $25 Grocery Gift Card for completion of timely visit $25 Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Sample of 100 Medical Records Monitoring Frequency: Monthly beginning July 2014 Frequency of Ongoing Prenatal Care 24. HYBRID MEASURE-MEDICAL RECORD REVIEW REQUIRED 2013 Rate- 76.64% Rotated Measure in 2011 2013 Statewide Average – 70.00% Goal – 90th Percentile 2013 Average – 63.00% Member Outreach • Case management will be offered to all pregnant women. Case manager will conduct a prenatal care assessment, provide prenatal education, and conduct ongoing assessment to detect any changes in the course of the pregnancy. Case manager will assure appropriate referral to perinatology or Maternal-Fetal Medicine (MFM) for pregnancies which become high-risk. • Upon notification of pregnancy, Case Managers will mail each eligible member, a brochure listing when the member should schedule a prenatal care visit. The Case Manager will follow-up with a phone call to assure a visit has been scheduled and will follow-up prior to next appointment to assure all prenatal care visits have been made and the member has attended each one. Provider Outreach • Case Manager will work in conjunction with large OB/GYN offices to assure member access to appointments. Incentive (member) Incentive (Provider) Not Planned Not Planned Key Responsible Person: Cathy Brigden Assigned Person: Lisa McIntyre Monitoring Mechanism: Sample of 100 Medical Records Monitoring Frequency: Monthly beginning July 2014 Well-Child and Preventive Care Visits in the First 15 Months of life 25. 2013 Rate-84.34%, improved from 2012 Rate of 81.00% 2013 Statewide Average – 83.00% Goal-90th Percentile State Average – 74.70% Member Outreach • Letter to caregiver of all eligible members encouraging compliance sent during end of year push in 2013. Mailing will be sent again during 2014 end of year push. • Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Caregiver will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • Member Services will begin making live telephone contact with members during endof-year push in September 2013 to stress importance of Well Child Visit. Will assist in scheduling appointments if needed. • Prenatal Case Management program includes education of Well Child Visit for members who have had deliveries. • Prenatal Case Managers submit notification of member delivery to newborn’s PCP. Provider Outreach • Onsite follow up at top 10 high volume PCP and OB/GYN providers by Community Quality Nurse Consultant to review specifications of the measure. • Article in provider newsletter reminding providers of the appropriate well child visit coding. Article will include ICD-9 and CPT-4 codes so providers are aware of the correct coding schemes for QARR reporting (Summer 2014) • Prenatal Case Manager will work in conjunction with pediatric offices to assure all newborn member files are communicated to PCP and that appointments are made by the PCP. Incentive (member) Not Planned Incentive (Provider) Not Planned Key Responsible Person: Cathy Brigden Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning July 2014 26. Well-Child and Preventive Care Visits During the 3rd, 4th, 5th and 6th Years 2013 Rate- 81.61%, 2012 Rate – 78.00% 2013 Statewide Average – 82.00% Goal-90th Percentile 2013 Average – 73.80% Member Outreach • Letter to caregiver of all eligible members encouraging compliance sent during end of year push in 2013. Mailing will be sent again during 2014 end of year push. • Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Caregiver will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • Member Services will begin making live telephone contact with members during endof-year push in September 2013 to stress importance of Well Child Visit. Will assist in scheduling appointments if needed.. Provider Outreach • Mailing to all providers and onsite follow up at top 10 high volume providers by Community Quality Nurse Consultant to review specifications of the measure • Notification to providers of all members (July 2014) in their panel who are in need of service by end of measurement year (December 31, 2014). List will be revised in October 2014. • Seasonal Mailing prior to school commencing, encouraging members to complete school physical, educating members about importance of visit, and informing members about the Total Rewards incentive program (August 2014.) • Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • Member Services will begin making telephone contact with members directly during end-of-year push in September 2014. Will assist in scheduling appointments if needed. • Article in provider newsletter reminding providers of the appropriate well child visit coding. Article will include ICD-9 and CPT-4 codes so providers are aware of the correct coding schemes for QARR reporting (SUMMER 2014). Article encouraged providers to take advantage of opportunities to convert a follow up visit to a well child and American Academy of Pediatrics recommendation for annual visit. Incentive (member) $25 Incentive (Provider) $25 Provider Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning July 2014 27. Adolescent Well Care and Preventive Visits 2013 Rate-58.90%, increase from 2012 rate of 55.00% 2013 Statewide Average-59.00% Goal- 90th Percentile 2013 Average – 53.10% Member Outreach • Member letter encouraging compliance sent during end of year push in 2013. Mailing will be sent again during 2014 end of year push. • Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • Member Services will begin making live telephone contact with members during endof-year push in September 2013 to stress importance of labs. Will assist in scheduling appointments if needed. • Seasonal Mailing prior to school commencing, encouraging members to complete school physical, educating members about importance of visit, and informing members about the Healthy Rewards incentive program (August 2014.) Provider Outreach • Mailing to all providers and onsite follow up at top 10 high volume providers reviewing specifications of the measure • Mailing to all members eligible for measure educating members about importance of visit and availability of incentive program (August 2014) • Notification to providers of all members (July 2014) in their panel who are in need of service by end of measurement year (December 31, 2014). List will be revised in October 2014. • Article in provider newsletter reminding providers of the appropriate well child visit coding. Article will include ICD-9 and CPT-4 codes so providers are aware of the correct coding schemes for QARR reporting (SUMMER 2014). Article encouraged providers to take advantage of opportunities to convert a follow up visit to a well child and American Academy of Pediatrics recommendation for annual visit. Emphasized that when members present for summer camp physicals and school employment physicals this would be an opportune time for their annual well visit. • Televox outbound calling (May 2014 and July 2014) to remind members about this gap in care. Members will have option to speak with a member services representative and can get more information about gap in care as well as information to make an appointment. • Member Services will begin making telephone contact with members directly during end-of-year push in September 2014. Will assist in scheduling appointments if needed. Incentive (member) $25 Incentive (Provider) $25 Comments : Supplemental Database Key Responsible Person: Jennifer Skotniski Assigned Person: Lisa McIntyre Monitoring Mechanism: Review of Administrative Data compared to targeted goal Monitoring Frequency: Monthly beginning July 2014 Revised 4/16/14 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 7 BENEFIT SUMMARIES TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN , MEDICAID MANAGED CARE The member must receive these services from providers who are in the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Provider Network. All services must be medically necessary and provided or referred by the Member’s Primary Care Provider (PCP). Regular Medical Care Office visits with the Member’s PCP Referrals to specialists Eye/hearing exams Preventive Care Well baby care Well-child care Regular check-ups Shots for children from birth through childhood Maternity Care Pregnancy care Doctors/midwife and hospital services Newborn nursery care Home Health Care (must be medically needed and arranged by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN ) At least 2 visits to high-risk infants (newborns) Visit to women who stay in the hospital less than 48 hours after birth Visit to women who stay in hospital less than 96 hours after a Cesarean birth Other home health care visits as needed and ordered by the PCP/specialist Vision Care Services of an ophthalmic dispenser and optometrist, and coverage for contact lenses, polycarbonate lenses, artificial eyes, and or replacement of lost or destroyed glasses, including repairs, when medically necessary. Artificial eyes are covered as ordered by a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN provider Eye exams, generally every two years, unless medically needed more often Glasses (new pair of Medicaid approved frames every two years, or more often if medically needed) Low vision exam and vision aids ordered by your doctor Specialist referrals for eye diseases or defects Revised January 2015 Section 7 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Hospital Care Inpatient Care Outpatient Care Lab, x-ray, other tests Emergency Care - An emergency is defined as a medical or behavioral condition, the onset of which is sudden, that manifests itself by symptoms of sufficient severity, including severe pain, that a prudent lay person possessing an average knowledge of medicine and health, could reasonably expect the absence of immediate medical attention to result: • • • • In placing the health of the person afflicted with such condition in serious jeopardy, or in the case of a behavioral condition, placing the health of the person or others in jeopardy: or Serious impairment to such person’s bodily functions; or Serious dysfunction of any bodily organ or part of such person; or serious disfigurement of such person Mental Health/Alcohol and Substance Abuse All inpatient mental health and alcohol/substance abuse services Most outpatient mental health services (contact plan for specifics) SSI recipients can get these services only from any Medicaid provider by using their Medicaid Card. Inpatient detoxification services, however, are covered by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN as an inpatient hospital benefit Specialty Care - Includes the services of other practitioners, including Medical and nursing staffs Occupational, physical and speech therapists and audiologists Midwives Other Covered Services Pharmacy – Express Scripts is the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Benefit Manager Dental – Healthplex is the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Benefit Manger Transportation All Counties- Emergency transportation only. Non-emergency transportation is covered by Medicaid Durable Medical Equipment (DME) Hearing Aids/Prosthetics/Orthotics Court Ordered Services Case Management Social Support Services (help in getting community services) FQHC services Family Planning Podiatry for children and persons with special problems (i.e., diabetes, etc.) Revised January 2015 Section 7 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Personal Care Services There are some services that a Member can choose where to get the care. The Member can get these by using their TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Membership Card. The Member may also go to providers who will take their Medicaid Benefit Card. They do not need a referral from their PCP to obtain these services: Family Planning - The Member may go to any doctor or clinic that takes Medicaid and offers family planning services. The Member is welcome to visit one of the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN family planning providers as well HIV Testing and Counseling – The Member may obtain these services from TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN doctors or from doctors or clinics that take Medicaid. The Member does not need a referral when they get this service as part of a family planning visit. The Member can also get HIV testing and counseling services any time from TOTALC CARE providers, if they talk to their PCP first. Revised January 2015 Section 7 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL BENEFITS USING A MEDICAID CARD ONLY There are some services TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN does not provide. The Member can receive these services from any provider who takes Medicaid by using their Medicaid Benefit Card: Mental Health Intensive psychiatric rehab treatment Day treatment Intensive case management Partial hospital care Rehab services to those in community homes or family-based treatment Clinic services for children with SED (Serious Emotional Disturbance) Continuing day treatment Mental Retardation and Developmental Disabilities Long-term therapies Day treatment Housing services Comprehensive Medicaid case management Services received under the Home and Community Based Service Waiver Medical Model (Care-at-Home) Waiver Services Chemical Dependency Services Methadone treatment Out-patient substance abuse treatment Outpatient alcohol rehab Other Medicaid Services Pre-school and school services programs (early intervention) Early start programs Case management Long term home health care Hospice services SERVICES NOT COVERED These Services are not available from TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or Medicaid. If the Member receives any of these services they may have to pay the bill: Cosmetic surgery if not medically needed Routine foot care (for those 21 years and older) Personal and comfort items Infertility treatments Revised January 2015 Section 7 Page 4 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Services of a provider that is not part of the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Network (unless approved by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN ) Those services not given an approval in advance by the Member’s PCP The Member may have to pay for any service that their PCP does not approve. This includes: Non-covered services (listed above) Unauthorized services Services provided by providers not part of the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN NETWORK You must advise the enrollee prior to providing the service that it is not covered and you must advise member of the cost of the service. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN CHILD HEALTH PLUS (CHIP) Covers Preventive Health Services Physical exams Immunizations Well child visits Nutrition education Counseling Tuberculin testing (Mantoux) Development screening Lead screening Medical Service Prescription and Non-Prescription Drugs No copayment for drugs prescribed by a physician Vision Care Emergency, preventative and routine vision care Standard prescription lenses and frames once in a 12-month period Contact lenses covered only when medically necessary Dental Care Emergency, preventative and routine dental care Dental exams, visits, and consultations covered once within a 6 month consecutive period Speech and Hearing Speech therapy services for a condition correctable to significant clinical improvement within a two month period Hearing exams, one per calendar year Hearing aids, including batteries and repairs Revised January 2015 Section 7 Page 5 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Durable Medical Equipment Medically necessary devices and equipment ordered by a participating provider of the treatment of a specific medical condition Inpatient/Outpatient Treatment for Alcoholism, Substance Abuse and Mental Health There are no coverage limitations for inpatient or outpatient services Inpatient Hospital Care As a registered bed patient for the proper treatment of an illness, injury or condition that can not be treated on an outpatient basis Diagnosis and Treatment of Illness or Injury Services on an in office or ambulatory basis by a covered provider Laboratory test X-rays Other diagnostic procedures medically necessary for diagnosis and treatment of sickness, injury or other conditions Outpatient Therapies Up to 10 Physical Therapy Visits Up to 10 Occupational Therapy Visits Speech and Hearing Services Therapeutic Services Ambulatory radiation therapy Chemotherapy Renal dialysis Injections and medications given in a physician’s office Pre-Surgical Testing Performed at the hospital where the surgery is scheduled Includes tests (laboratory, x-ray, etc.) necessary prior to inpatient or outpatient surgery Outpatient Surgery Procedures performed within the provider’s office will be covered Ambulatory Surgery Centers Anesthesia Home Health Care Services Home health care services provided by a certified home health care agency that is a participating provider only to avoid hospitalization in the absence of home care Diabetic Education and Home Visits Provided upon the diagnosis of diabetes, a significant change in condition, the onset of a condition that make changes in self management necessary Revised January 2015 Section 7 Page 6 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Home Visits are covered if medically necessary Maternity Care Inpatient hospital care for at least 48 hours after childbirth and at least 96 hours following a C-section Necessary maternal and newborn clinical assessments and training in breast or bottle feeding The mother will have the option to be discharged earlier than 48/96 hours If early discharge is chosen, one home care visit is covered when requested from TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN within a 48 hours of delivery Prenatal, labor and delivery care is covered (subsidized children requiring maternity care services will be referred to Medicaid) Transportation Pre-hospital emergency (non-airborne) ambulance services SERVICES THAT ARE NOT COVERED UNDER CHIP Experimental medical or surgical procedures Experimental drugs Cosmetic, plastic or reconstructive surgery (except as defined) Services in a nursing home or rehabilitation facility (except as defined) Over–the-counter drugs (except as defined) Personal or comfort items In Vitro Fertilization, artificial insemination or other means of assisted conception Private duty nursing Hospice services Autologous blood donation Physical manipulation services Routine foot care Orthodontic services Services covered by another payment source Services which are not medically necessary Members Could Be Responsible for Payment 1. 2. 3. 4. Non emergent Emergency Room visits Services from a specialist without a PCP referral Care not provided, authorized or arranged by the PCP Out of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Network services without an authorization from the PCP 5. Non covered services provided by a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Network provider Revised January 2015 Section 7 Page 7 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL FAMILY HEALTH PLUS (FHP) COVERS Beginning with services of September 1, 2005, co-payment are applied to the Family Health Plus Benefit Plan. These co-payment amounts are applicable to the FHP Benefit Plan only. Medicaid Managed Care and Child Health Plus programs are not affected. Please see the bottom of this listing for the FHP co-payment information. Regular Medical Care Office visits with the PCP Referrals to specialists Eye/hearing exams Preventive Care Regular check-ups Tests and procedures ordered by the PCP or specialist Maternity Care Pregnancy care Doctors/midwife and hospital services Post-partum care Note: Women who become pregnant while enrolled in FHPlus should be encouraged to call the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member Service Department to have their benefit package re-evaluated. Their financial requirements are different and the family size has changed. The patient may qualify for Medicaid. Medicaid covers more services then FHPlus that the patient may or may not need, depending on their medical needs. Home Health Care Hospital stay less than 48 hours after giving birth Hospital stay less than 96 hours after a Cesarean birth Other visits as needed and ordered by the PCP/specialist Vision Care Emergency vision care Eye exam provided once in any twenty-four month period One pair of prescription eyeglass lenses and frame or prescription contact lenses where medically necessary. Eyeglasses or medically necessary lenses are limited to one pair in any twenty-four month period One pair of medically necessary occupational eyeglasses in a twenty-four month period Note: Replacement of lost, damaged or destroyed eyeglasses is not a benefit under the FHP Benefit Plan. Hospital Care Inpatient care Revised January 2015 Section 7 Page 8 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Outpatient care Lab, x-ray, other tests Emergency Care - An emergency is: a medical or behavioral condition, the onset of which is sudden, that manifests itself by symptoms of sufficient severity, including severe pain, that a prudent lay person possessing an average knowledge of medicine and health, could reasonably expect the absence of immediate medical attention to result: • • • • In placing the health of the person afflicted with such condition in serious jeopardy, or in the case of a behavioral condition, placing the health of the person or others in jeopardy: or Serious impairment to such person’s bodily functions; or Serious dysfunction of any bodily organ or part of such person; or Serious disfigurement of such person Mental Health/Alcohol/Substance Abuse Services Outpatient mental health/alcohol/substance abuse services (up to 60 days per year) Inpatient mental health/alcohol/substance abuse services (up to 30 days per year) Inpatient detoxification services are covered by the plan as an inpatient hospital benefit, and don’t count toward the limits mentioned above) Specialty Care Medical and nursing staff Occupational, physical and speech therapists needed on a short-term basis Midwives Audiologist Other Covered Services Emergency ambulance Durable Medical Equipment (DME) Hearing Aids/Supplies Prosthetics/Orthotics Pharmacy (prescription drugs, smoking cessation products, hearing aid products and diabetic supplies (from TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s participating pharmacy) Dental Court ordered services, if covered by the plan TB diagnosis and treatment. The patient may choose to go either to their PCP or to the county public health agency for diagnosis and/or treatment. The patient does not require a referral to go to the county public health agency. Revised January 2015 Section 7 Page 9 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Services NOT Covered These services are not available from TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN . If the patient receives any of these services, they may have to pay the bill. Cosmetic surgery if not medically needed Routine foot care (for those 21 years and older) Personal and comfort items Infertility treatments Services of a provider that is not part of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Network (unless TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or the PCP refers the patient to an out of network provider) Those services not approved in advance by the PCP Personal care services Private duty nursing services Over the counter medical supplies and non-prescription drugs Nursing home stays that are permanent Non-emergency transportation Replacement of lost, damaged or destroyed eyeglasses in a twenty-four month period Family Health Plus Co-payments For services beginning September 1, 2005 most FHPlus Members will be responsible for making co-payments for the following: • Brand Name Prescription Drugs $6 for each prescription and refill • Generic Prescription Drugs $3 for each prescription and refill • Clinic visits $5 per visit • Physician visits $5 per visit • Dental Service Visits $5 per visit up to a total of $25 per year • Lab tests $0.50 per test • Radiology Services $1 per radiology service • Inpatient hospital stays $25 per stay • Non-urgent emergency room visit $3 per visit • Covered over-the-counter medications $0.50 per medication • Covered medical supplies $1 per supply (Hearing aid batteries, enteral formula, and Diabetes test strips, lancets and syringes) Co-payments will not apply to the following services: • Emergency services • Family planning services and supplies • Mental health clinics • Chemical dependence clinics Revised January 2015 Section 7 Page 10 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL • • • Mental illness drugs Tuberculosis drugs Prescription drugs for a resident of an Adult Care Facility FHP Members who do not have to pay the co-payments: • Under age 21 • Pregnant (Even if the service is unrelated to pregnancy) • A permanent resident of a nursing home • A resident of a community based residential facility licensed by the Office of Mental Health or the Office of Mental Retardation and Developmental Disability As is the rule for regular Medicaid, Family Health Plus members who cannot afford the co-payment may not be denied a service based on their inability to pay. Providers cannot refuse to give care or services because the FHP Member is unable to pay. The Member will still owe the unpaid co-pay amounts to the provider and the provider may bill for payment later or send a bill. Revised January 2015 Section 7 Page 11 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 8 MEMBERS RIGHTS/RESPONSIBILITIES MEMBER RIGHTS AND RESPONSIBILITIES MEMBER RIGHTS As a Member of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, the member has the following rights: o Be cared for with respect without regard for health status, sex, race, color, religion, national origin, age, marital status or sexual orientation o Be told where, when and how to get the services needed from TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN o Be told by their PCP what is wrong, what can be done for them, and what will likely be the result in language they understand o Get a second opinion about their care o Give their approval to any treatment or plan for their care after that plan has been fully explained to them o Refuse care and be told what they may risk if they do o Get a copy of their medical record, and talk about it with their PCP, and to ask, if needed, that your medical record be amended or corrected o Be sure that their medical record is private and will not be shared with anyone except as required by law, contract, or their approval o Use TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN complaint system to settle any complaints, or they can complain to the NY State Department of Health or the local Department of Social Services any time they feel they were not fairly treated o File for External Appeal o Use the New York State’s Fair Hearing system o Appoint someone (relative, friend, lawyer, etc.) to speak for them if they are unable to speak for themselves about their care and treatment o Receive considerate and respectful care in a clean and safe environment free of unnecessary restraints Revised July 2014 Section 8 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL MEMBER RESPONSIBILITIES As a member of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, they agree to: o Work with their PCP to guard and improve their health o Find out how their health care system works o Listen to their PCP’s advice and ask questions when they are in doubt o Call or go back to their PCP if they do not get better, or ask for a second opinion o Treat health care staff with the respect they expect themselves o Call Member Service if they have problems with any health care staff o Keep their appointments; if they must cancel, call as soon as possible o Use the emergency room only for real emergencies o Call their PCP when they need medical care, even if it is after-hours Revised January 2015 Section 8 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 9 ACTION/GRIEVANCES/APPEALS SYSTEMS Definitions This section addresses two important subjects: • • Actions/Action Appeals Grievances/Grievance Appeals To comprehend these systems, providers need clear definitions for the following terms: Actions Actions are defined as activities of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN that result in: The denial or limited authorization of a Service Authorization Request, including the type or level of service; The reduction, suspension, or termination of a previously authorized service; The denial, in whole or in part, of payment for a service; Failure to provide services in a timely manner as defined by the State; Failure of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to act within the timeframes for resolution and notification of determinations regarding Grievances (Complaints), Action Appeals and Grievance (Complaints) Appeals provided in this manual section. Grievances A Grievance is defined as an expression of dissatisfaction about any matter other than an action (a Complaint). The term is also used to refer to the overall system that includes grievances and appeals handled at the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN level and access to the State’s Fair Hearing Process. (Possible subjects for grievance include, but are not limited to, the quality of care or services provided, and aspects of interpersonal relationships such as rudeness of a provider or employee, or failure to respect the enrollee’s rights.) Service Authorization Requests There are some treatments and services that need to be approved before the enrollee receives them or to be able to continue receiving them. This is a prior authorization. These services require prior approval: Primary Care Providers (PCP’s) or specialists with a valid referral from the PCP must call the Quality Assurance/Utilization Management Department at (315) 634-5555 extension 1112 or toll free at (877) 8724716 in advance to preauthorize the following services: • Elective inpatient admission • Emergency admit (within one business day) • Inpatient Mental Health and/or Chemical Services • Maternity admission (within one business day) • Surgery not performed in the doctor’s office • MRI scans (Only when performed by a non participating provider) • Services to newborns in NICU • Home Care, includes infusion and physical therapy • Private duty nursing • Referrals to NON-PAR providers Revised July 2014 Section 9 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL A TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN preauthorization review must be done before a Family Health Plus or Child Health Plus member receives any specialty dental service such as: dental extractions under general anesthesia or sedation, endodontal services such as root canals, and periodontal services from any specialty dentist or non-participating dentist. Concurrent Review A review that is performed when preauthorized services are to continue past the initial authorized period. Service Authorization Determination TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s approval or denial of a Service Authorization Request. Adverse Determination A denial of a Service Authorization Request by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN on the basis that the requested service is not Medically Necessary or an approval of a Service Authorization Request is in an amount, duration, or scope that is less than requested. Adverse determinations will be made by a clinical peer reviewer. Fair Hearings In some cases the enrollee/enrollee designee may ask for a fair hearing from New York State. • Enrollee/enrollee designee is not happy with a decision that the local Department of Social Services or the State Department of Health made about an enrollee staying or leaving TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. • The enrollee/enrollee designee is not happy with a decision that TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has made about medical care. The enrollee/enrollee designee feels that the decision limits managed care benefits or that TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN did not make the decision in a reasonable amount of time. • The enrollee/enrollee designee is not happy about a decision made by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN that denied medical care wanted. Enrollee/enrollee designee feels that the decision limits managed care benefits. • The enrollee/enrollee designee is not happy with a decision that the practitioner would not order services that the enrollee wanted. The enrollee/enrollee designee feels that the practitioner’s decision stops or limits managed care benefits. The enrollee/enrollee designee must file a complaint with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN agrees with your practitioner, the enrollee/enrollee designee may ask for a state fair hearing. • The decision received from the fair hearing officer will be final. If the services that the enrollee is now getting are scheduled to end, the enrollee/enrollee designee can choose to ask to continue the services that the practitioner ordered until the case can be decided. However, if the enrollee chooses to ask for services to be continued, and the fair hearing is decided against the enrollee, the enrollee may have to pay the cost for the services they received while waiting for a decision. The enrollee/enrollee designee can use one of the following ways to request a Fair Hearing: 1. By phone, call toll-free 1-800-342-3334 2. By fax, 518-473-6735 Revised January 2015 Section 9 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 3. By internet, www.otda.state.ny.us/oah/forms.asp 4. By mail, NYS Office of Temporary Disability Assistance, Office of Administrative Hearings, Managed Care Hearing Unit, P.O. Box 22023, Albany, New York 12201-2023 Enrollee/enrollee designee can complain anytime to the New York State Department of Health by calling 1800-206-8125. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will make assistance available to members when filing complaints, appeals and action appeals. Aid Continuing TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is required to continue the provision of the Benefit Package services that are the subject of a Fair Hearing to an Enrollee, if so ordered by the New York State Office of Administrative Hearings (OAH) under the following circumstances: 1. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has or is seeking to reduce, suspend or terminate a treatment or Benefit Package service currently being provided: 2. Enrollee/Enrollee designee has filed a timely request for a Fair Hearing with OAH; and 3. There is a valid order for the treatment or service from a Participating Provider. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide aid continuing until the matter has been resolved to the Enrollee’s satisfaction or until the administrative process is completed and there is a determination from OAH that the Enrollee is not entitled to receive the service; the Enrollee withdraws the request for aid continuing and/or the Fair Hearing in writing: or the treatment or service originally ordered by the provider has been completed, whichever occurs first. If the services and/or benefits in dispute have been terminated, suspended or reduced and the Enrollee/Enrollee designee timely requests a Fair Hearing, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will; at the direction of either the State Department of Health (SDOH) or the Local Department of Social Services (LDSS), restore the disputed services and/or benefits. Fast Track is a term used to describe an act of expediting a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN obligation. The obligation may be to either expedite a Service Authorization Review Request, a Concurrent Review Request or any portion of the Appeal Process. Standard Action is a term used to describe a more measured timeframe than Fast Track or Fast Track act of obligation. The obligation may be in regards to a Service Authorization Review Request, a Concurrent Review Request or any portion of the Appeal Process. Retrospective Services A determination involving health care services that have been delivered. A review of these services will be made within thirty days of receipt of the necessary information to make such a determination. Upon Receipt of A Service Authorization Request TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s policies and procedures for Service Authorization Determinations and utilization review determinations include the following: o Fast Track review of a Service Authorization Request must be conducted when TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN determines or the provider indicates that a delay would seriously jeopardize the Enrollee’s life or health or ability to attain, maintain, or regain maximum function. The Enrollee/Enrollee designee may request Fast Track review of a Prior Authorization Request or Concurrent Review Request. If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN denies the Enrollee’s request for Fast Track review, TOTAL CARE, A TODAY’S Revised January 2015 Section 9 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL OPTIONS OF NEW YORK HEALTH PLAN must handle the request under standard review timeframes as outlined in this manual section. o TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is required to provide notice by phone and in writing to the Enrollee/Enrollee designee and to the provider of Service Authorization Determinations, whether adverse or not, within the same timeframes found in section “Prior Authorization Determinations”. Notice to the provider must contain the same information as the Notice of Action for the Enrollee. o When an adverse determination is rendered without provider input, the provider has the right to reconsideration. The reconsideration will occur within one (1) business day of the receipt of the request and will be conducted by the enrollee’s health care provider and the clinical peer reviewer making the initial determination. o If the enrollee or enrollee designee and TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN have jointly agreed to waive the internal appeal process offered by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, the information required in the Adverse Determinations Section of this Policy must be provided to the enrollee or enrollee designee simultaneously with the letter agreeing to such waiver. The letter agreeing to such waiver and the information required in the Adverse Determinations section of this Policy must be provided to the enrollee or enrollee designee within 24 hours of the agreement to waive the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN internal appeal process. Prior Authorization Determinations For Prior Authorization requests, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must make a Service Authorization Determination and notify the Enrollee/Enrollee designee and provider of the determination by phone and in writing as fast as the Enrollee’s condition requires and no more than: o o In the case of a Fast Track Review, three (3) business days after receipt of the Service authorization Request; or For Standard Review, within three (3) business days of receipt of necessary information, but no more than fourteen (14) days after receipt of the Service Authorization request. Revised January 2015 Section 9 Page 4 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Concurrent Review Determinations For Concurrent Review Requests, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must make a Service Authorization Determination and notify the Enrollee/Enrollee designee and provider of the determination by phone and in writing as fast as the Enrollee’s condition requires and no more than: o In the case of a Fast Track Review, (1) business day upon receipt of the necessary information, but no later than (3) business days after receipt of the request. o In the case of a Standard Review, within (1) business day upon receipt of the necessary information, but no later than (14) business days after receipt of the request. Revised January 2015 Section 9 Page 5 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Extension of Service Authorization Timeframes: the determination timeframe may be extended up to 14 days if: The Enrollee/Enrollee’s designee or the Enrollee’s provider requests an extension orally or in writing: or TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN can demonstrate or substantiate that there is a need for additional information and how the extension is in the enrollee’s interest. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must send notice of the extension to the Enrollee/Enrollee designee. If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN extends its review, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must make a Service Authorization Determination and notify the Enrollee/Enrollee designee and provider by phone and in writing as fast as the enrollee’s condition requires and within the applicable timeframes after the information comes in – but in no event later than the date the extension expires. Retrospective Review Retrospective Reviews are determinations involving health care services that have been pre-authorized. Enrollee, enrollee designee or provider may file a UR appeal for a retrospective denial. Pre-authorized services can be reviewed retrospectively when: a) Relevant medical information is presented to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN that is materially different from the information that was presented during the pre-authorization review; and b) The information existed at the time of the pre-authorization review but was withheld or not made available: and c) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN was not aware of the existence of the information at the time of the pre-authorization review: and d) Had TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN been aware of the information, the treatment, service or procedure being requested would not have been authorized. Retrospective determinations will be made within thirty days (30) of receipt of the necessary information. Revised January 2015 Section 9 Page 6 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Notice of Actions (Adverse Determinations) When TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN intends to reduce, suspend, or terminate a previously authorized service within an authorization period, it must provide the Enrollee/Enrollee designee with a written notice at least ten (10) days prior to the intended Action, except 1. When the period of advance notice is shortened to five (5) days in cases of confirmed Enrollee fraud; or 2. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN may mail notice not later than date of the Action for the following: a) The death of the Enrollee; b) A signed written statement from the Enrollee/Enrollee designee requesting service termination or giving information requiring termination or reduction of services (where the Enrollee understands that this must be the result of supply the information. c) The Enrollee’s admission to an institution where the Enrollee is ineligible for further services; d) The Enrollee’s address is unknown and mail directed to the Enrollee is returned stating that there is no forwarding address; e) The Enrollee has been accepted for Medicaid services by another jurisdiction; or f) The Enrollee’s physician prescribes a change in the level of medical care. 3. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must mail written notice to the Enrollee/Enrollee designee and provider on the date of the Action when the Action is denial of payment, in whole or in part, except as outlined below under “Obligation to Notify” 4. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN does not reach a determination within the service Authorization Determination timeframes described above, it is considered an Adverse Determination and is subject to appeal. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must send notice of Action to the Enrollee/Enrollee designee and provider on the date the timeframes expire. 5. When an adverse determination is rendered without provider input, the provider has the right to a reconsideration. The reconsideration will occur within one (1) business day of receipt of the request and will be conducted by the enrollee’s health care provider and the Utilization Reviewer who made the initial determination Formats and Content of Notices TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will ensure that all notices are in writing, in easily understood language and are accessible to non-English speaking and visually impaired Enrollee/Enrollee designee. Notices will include that oral interpretation and alternate formats of written material for Enrollee/Enrollee designee with special needs are available and how to access the alternate formats. 1. Notice to the Enrollee/Enrollee designee and the provider that the Enrollee’s request for an Fast Track review has been denied will include that the request will be reviewed under standard timeframes, including a description of the timeframes. Revised January 2015 Section 9 Page 7 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 2. Notice to the Enrollee regarding TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s-initiated extension will include: The reason for the extension; An explanation of how the delay is in the best interest of the Enrollee: Any additional information TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN requires from any source to make its determination; The right of the Enrollee to file a Grievance (as defined in this Section) regarding the extension; The process for filing a Grievance with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and the timeframes within which a Grievance determination must be made; The right of an Enrollee to designate a representative to file a Grievance on behalf of the Enrollee; and The right of the Enrollee to contact the New York State Department of Health regarding his or her Grievance, including the SDOH’S toll-free number for Grievances. 3. Notice to the Enrollee of an Action will include: a) The description of the Action TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has taken or intends to take; b) The reasons for the Action, including the clinical rationale, if any; c) The Enrollee’s right to file an Action Appeal as defined in this Section, including: The fact that TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will not retaliate or take any discriminatory action against the Enrollee because he/she filed an Action Appeal. The right of the Enrollee to designate a representative to file Action Appeals on his/her behalf; d) The process and timeframe for filing an Action Appeal with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, including an explanation that an Fast Track review of the Action Appeal can be requested if a delay would significantly increase the risk to an Enrollee’s health, a toll-free number for filing an oral Action Appeal; e) A description of what additional information, if any, must be obtained by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN from any source in order the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to make an Appeal determination; f) The timeframes with which the Action Appeal determination must be made; g) The right of the Enrollee to contact the New York State Department of Health with his or her Grievance, including the SDOH’s toll-free number for Grievances; and h) The notice entitled “Managed Care Action Taken” for denial of benefits or for termination or reduction in benefits, as applicable, containing the Enrollees Fair Hearing and aid continuing rights. i) For actions based on issues of Medical Necessity or an experimental or investigational treatment, the notice of Action will also include: 1. A clear statement that the notice constitutes the initial adverse determination and specific use of the terms “medical necessity” or “experimental/investigational”; 2. A statement that the specific clinical review criteria relied upon in making the determination is available upon request; and Revised January 2015 Section 9 Page 8 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 3. The Enrollee/Enrollee Designee have the right to an external appeal. A statement that the Enrollee may be eligible for an External Appeal and instructions to request an External Appeal. The denial has been upheld as a final adverse determination or both TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and the enrollee/enrollee designee have jointly agreed to waive any internal appeal. Written notification of this agreement will be sent to the Enrollee/Enrollee Designee within 24 hours. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Obligation to Notify TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must provide written Notice of Action to Enrollees/Enrollee designee and providers in accordance with the requirements of this Section, including, but not limited to, the following circumstances: 1) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN makes a coverage determination or denies a request for a referral, regardless of whether the Enrollee has received the benefit; 2) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN determines that a service does not have appropriate authorization; 3) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN denies a claim for services provided by a Non-Participating Provider for any reason; 4) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN denies a claim or service due to medical necessity; 5) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN rejects a claim or denies payment due to a late claim submission; 6) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN denies a claim because it has determined that the Enrollee was not eligible for MMC or FHPlus coverage on the date of service; 7) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN denies a claim for service rendered by a Participating Provider due to lack of a referral; 8) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN denies a claim because it has determined it is not the appropriate payer; or 9) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN denies a claim due to a Participating Provider billing for Benefit Package services not included in the Provider Agreement between the Contract and the Participating Provider. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is not required to provide written Notice of Action to Enrollees in the following circumstances: o When there is a prepaid capitation arrangement with a Participating Provider and the Participating Provider submits a fee-for-service claim to TOTAL CARE, A TODAY’S Revised January 2015 Section 9 Page 9 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL OPTIONS OF NEW YORK HEALTH PLAN for a service that falls within the capitation payment; o If a Participating Provider of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN itemizes or “unbundled” a claim for services encompassed by a previously negotiated global free arrangement: o If a duplicate claim is submitted by the Enrollee or a Participating Provider, no notice is required, provided an initial notice has been issued; o If the claim is for a service that is carved-out of the MMC Benefit Package and is provided to a MMC Enrollee through Medicaid fee-for-service, however, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN should notify the provider to submit the claim to Medicaid; o If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN makes a coding adjustment to a claim (up-coding or down-coding) and its Provider Agreement with the Participating Provider includes a provision allowing TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to make such adjustments; o If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has paid the negotiated amount reflected in the Provider Agreement with a Participating Provider for the services provided to the Enrollee and denies the Participating Provider’s request for additional payment; or o If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has not yet adjudicated the claim. If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has pended the claim while requesting additional information, a notice is not required until the coverage determination has been made. Retrospective Review TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN may reverse a preauthorized treatment, service or procedure on retrospective review pursuant to section 4905(5) of the Public Health Law when: a. b. c. d. Relevant medical information presented to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN upon retrospective review is materially different from the information that was presented during the pre-authorization review; and The information existed at the time of the pre-authorization review but was withheld or not made available; and TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN was not aware of the existence of the information at the time of the pre-authorization review; and Had TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN been aware of the information, the treatment, service or procedure being requested would not have been authorized. Action Appeals Process TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member Services may be contacted regarding Appeals at TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, PO Box 11507, Syracuse, NY 13218-1507 or toll free at (877) 872-4715. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Action Appeals process indicates the following regarding resolution of Appeals of an Action: Revised January 2015 Section 9 Page 10 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 1. The Enrollee/Enrollee designee, will have no less than sixty (60) business days from the date of the notice of Action to file an Action Appeal and no more than 90 days. An Enrollee filing an Action Appeal within 10 days of the notice of Action or by the intended date of an Action, whichever is later, that involves the reduction, suspension, or termination of previously approved services may request “aid continuing”. See “Aid Continuing” above under Definitions. 2. The Enrollee/Enrollee designee may file a written Action Appeal or an oral Action Appeal. Oral Action Appeals must be followed by a written, signed, Action Appeal. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN may provide a written summary of an oral Action Appeal to the Enrollee/Enrollee designee (with the acknowledgement or separately) for the Enrollee/Enrollee designee to review, modify if needed, sign and return to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. If the Enrollee/Enrollee or provider requests Fast Track resolution of the Action Appeal, the oral Action Appeal does not need to be confirmed in writing. The date of the oral filing of the Action Appeal will be the date of the Action Appeal for the purposes of the timeframes for resolution of Action Appeals. Action Appeals resulting from a Concurrent Review must be handled as a Fast Track Action Appeal. 3. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must send a written acknowledgement of the Action Appeal or reason for additional information, if additional information is needed, within fifteen (15) days of receipt. If a determination is reached before the written acknowledgement is sent, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN may include the written acknowledgement with the notice of Action Appeal determination (one notice). 4. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must provide the Enrollee/Enrollee designee reasonable opportunity to present evidence, and allegations of fact or law, in person as well as in writing. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must inform the Enrollee/Enrollee designee of the limited time to present such evidence in the case of an Fast Track Action Appeal. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must allow the Enrollee/Enrollee designee, both before and during the Action Appeals process, to examine the Enrollee’s case file, including medical records and any other documents and records considered during the Action Appeals process. In the event that only a portion of such necessary information is received, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will request the missing information, in writing, within five (5) business days of receipt of the partial information. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will consider the Enrollee/Enrollee designee or legal estate representative of a deceased Enrollee a party to the Action Appeal. 5. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must have a process for handling Fast Track Action Appeals (Expedited Appeals). An expedited appeal is used for adverse determinations involving continued or extended health care services, procedures or treatments or additional services for a member undergoing a course of continued treatment prescribed by a health care provider or an adverse determination in which TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or the health care provider believes an immediate appeal is warranted except for any retrospective determination. Fast Track resolution of the Action Appeal must be conducted when TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN determines or the provider indicates that a delay would seriously jeopardize the Enrollee’s life or health or ability to attain, maintain, or regain maximum function. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK Revised January 2015 Section 9 Page 11 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL HEALTH PLAN will immediately notify the Enrollee/Enrollee designee and the enrollee’s health care provider by telephone or facsimile to identify and request the necessary information, followed by written notification. A clinical peer reviewer will be available within one business day. The Enrollee/Enrollee designee may request an Fast Track review of an Action Appeal. If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN denies the Enrollee’s request for an Fast Track review, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must handle the request under standard Action Appeal resolution timeframes, make reasonable efforts to provide prompt oral notice of the denial to the Enrollee/Enrollee designee and send written notice of the denial within two (2) days of the denial determination. 6. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will ensure that punitive action is not taken against a provider who either requests a Fast Track resolution or supports an Enrollee’s Appeal. 7. Action Appeals of clinical matters must be decided by personnel qualified to review the Action Appeal by a clinical reviewer who did not make the initial determination. Qualified personnel at a higher level than the personnel who make the original determination will determine action Appeals of non-clinical matters. Timeframes for Resolution of Action Appeals TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Action Appeals process will indicate the following specific timeframes regarding Action Appeal resolution: o In the event that additional information is required to complete a Standard Appeal, will make their determination within 60 days after the receipt of necessary information. o TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will resolve Action Appeals as fast as the Enrollee’s condition requires, and no later than thirty (30) days from the date of the receipt of the Action Appeal. o TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will resolve Fast Track Action Appeals (Expedited Appeal) as fast as the Enrollee’s condition requires, within two (2) business days of receipt of necessary information and no later than three (3) business days of the date of the receipt of the Action Appeal. Written notice of final adverse determination concerning an expedited UR appeal will be transmitted to the Enrollee/Enrollee designee and provider within 24 hours of rendering the determination. Fast Track (Expedited) appeals not resolved to the satisfaction of the appealing party may be re-appealed through the standard appeal or external appeal process. o Timeframes for Action Appeal resolution may be extended for up to fourteen (14) days if: The Enrollee/Enrollee designee, or the provider requests an extension orally or in writing; or TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN can demonstrate or substantiate that there is a need for additional information and the extension is in the Enrollee’s interest. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must send notice of the extension to the Enrollee/Enrollee designee. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must maintain sufficient documentation of extension determinations to demonstrate, upon SDOH’S request, that the extension was justified. Revised January 2015 Section 9 Page 12 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL o TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN makes a reasonable effort to provide oral notice to the Enrollee/Enrollee designee, and the provider where appropriate, for Fast Track Action Appeals at the time the Action Appeal determination is made. o TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must send written notice to the Enrollee/Enrollee designee, and the provider where appropriate, within two (2) business days of the Action Appeal determination. o Providers notice that failure by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to make a determination within the applicable time periods in this section will be deemed to be a reversal of the utilization review reviewer’s adverse determination. Appeal Requests Appeal requests may be mailed to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, PO Box 11507, Syracuse, NY 13218-1507, ATTN: Appeals Department. Appeals may be requested by telephone toll free at (877) 872-4715. This toll free number is the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member Service line. Member Services will direct your call to the appropriate person within TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. Action Appeal Notices TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will ensure that all notices are in writing and in easily understood language and are accessible to non-English speaking and visually impaired Enrollee/Enrollee designee. Notices will include that oral interpretation and alternate formats of written material for Enrollee/Enrollee designee with special needs are available and how to access the alternate formats. 1. Notice to the Enrollee/Enrollee designee that the Enrollee’s request for a Fast Track Action (Expedited) Appeal has been denied, will include that the request will be reviewed under standard Action Appeal timeframes, including a description of the timeframes. This notice may be combined with the acknowledgement. 2. Notice to the Enrollee/Enrollee designee and provider regarding a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN initiated extension will include: a. The reason for the extension; b. An explanation of how the delay is in the best interest of the Enrollee; c. Any additional information TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN requires from any source to make its determination; d. The right of the Enrollee to file a Grievance regarding the extension; e. The process for filing a Grievance with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and the timeframes within which a Grievance determination must be made; f. The right of an Enrollee to designate a representative to file a Grievance on behalf of the Enrollee; and g. The right of the Enrollee to contact the New York State Department of Health regarding their Grievance, including the SDOH’S toll-free number for Grievances. Revised January 2015 Section 9 Page 13 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 3. Notice to the Enrollee/Enrollee Designee of Action Appeal Determination will include: a. Date the Action Appeal was filed and a summary of the Action Appeal; b. Date the Action Appeal process was completed; c. The results and the reasons for the determination, including the clinical rationale, if any; d. If the determination was not in favor of the Enrollee, a description of Enrollee’s Fair Hearing rights, if applicable; e. The right of the Enrollee/Enrollee designee to contact the New York State Department of Health regarding his or her Grievance, including the SDOH’s toll-free number for Grievances (New York State Department of Health Toll free at 1 800 206-8125); and f. For Action Appeals involving Medical Necessity or an experimental or investigational treatment, the notice must also include: 1 A clear statement that the notice constitutes the final adverse determination and specifically use the terms “medical necessity” or “experimental/ investigational,” 2 The Enrollee’s coverage type; 3 The procedure in question, and if available and applicable the name of the provider and developer/manufacturer of the health care service; 4 Statement that the Enrollee is eligible to file an External Appeal and the timeframe for filing; 5 If the enrollee or enrollee designee and TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN have jointly agreed to waive the internal appeal process offered by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, the information required in the Adverse Determinations Section of this Policy must be provided to the enrollee or enrollee designee simultaneously with the letter agreeing to such waiver. The letter agreeing to such waiver and the information required in the Adverse Determinations section of this Policy must be provided to the enrollee or enrollee designee within 24 hours of the agreement to waive the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN internal appeal process. 6 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s contact person and telephone number; The contact person, telephone number, company name and full address of the utilization review agent. External Appeals An external appeal may be filed: The enrollee has had coverage of a health care service, which would otherwise be a covered benefit under a subscriber contract or governmental health benefit program, denied on appeal, in whole or in part, pursuant to title one of PHL article 4910.0(a) on the grounds that such health care service is not medically necessary and a) When the enrollee has had coverage of a health care service denied on the basis that such service is experimental or investigational, and b) The denial has been upheld on appeal or both TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and the enrollee/enrollee designee have jointly agreed to waive any internal appeal c) And the enrollee’s attending physician has certified that the enrollee has a lifethreatening or disabling condition of disease 1) for which standard health Revised January 2015 Section 9 Page 14 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL services or procedures have been ineffective or would be medically inappropriate or 2) for which there does not exist a more beneficial standard health service or procedure covered by the health care PLANor for which there exist a clinical trial d) And the enrollee’s attending physician, who must be a licensed, board-certified physician qualified to practice in the area of practice appropriate to treat the enrollee’s life-threatening or disabling condition or disease, must have recommended either 1) a health service or procedure (including a pharmaceutical product within the meaning of Public Health Law 4900(5) (b) (B) , that based on two documents from the available medical and scientific evidence, is likely to be more beneficial to the enrollee than any covered standard health service or procedure; or 2) a clinical trial for which the enrollee is eligible. Any physician certification provided under this section will include a statement of the evidence relied upon by the physician in certifying his or her recommendation, e) And the specific health service or procedure recommended by the attending physician would otherwise be covered under the policy except for TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s determination that the health service or procedure is experimental or investigational. Request made to the state by health care consumers or health care providers for an independent review of denial of services by the health care plan on the grounds that the health care service is not medically necessary or is experimental or investigational. External appeals can be made only for services or procedures that are covered benefits of the plan. If services are denied as experimental or investigational the member must have a life threatening or disabling condition or disease to be eligible for an external appeal. 11. Response to External Appeal Requests TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will facilitate the prompt completion of external appeal requests, including but not limited to, the following: A. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide the enrollee with a copy of the standard description of the external appeal process as developed jointly by the commissioner and superintendent, including a form and instructions for requesting an external appeal: • Simultaneous with a notice of a final adverse determination that a health care service is not medically necessary, including on the grounds that the health care service is experimental or investigational; or • Simultaneous with the written confirmation of agreement between the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and the enrollee to waive the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s internal appeal process; and • Within three business days of a request by an enrollee or an enrollee’s designee B. Upon receiving notification regarding the identity and address of the certified external appeal agent, the assigned staff member will transmit the insured’s medical and treatment records and in the case of medical necessity appeals, the clinical standards used to determine medical necessity for health care services to the agent. This transmission will occur within three business days for standard appeals and within 24 hours for an expedited appeal. C. Requests for additional information by the assigned certified external appeal agent will be responded to as soon as possible, but no longer than two business days for standard appeals. Requests for information relative to expedited appeals will be provided to the assigned external appeal agent within 24 hours of the request. Revised January 2015 Section 9 Page 15 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 12. Provider Request For External Appeal: If a health care provider requests a copy of a form for an external appeal in connection with a retrospective adverse utilization review determination, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s QA/UR Director will send to the provider a form and instructions within three business days of the provider’s request. The Enrollee/Enrollee Designee also has the right to an external appeal of a final adverse determination. Please see page 8, number 3 of section 9. 13. Results Of External Appeal A. In the event an adverse determination is overturned on external appeal, or if reverses a denial B. C. which is the subject of external appeal, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide, arrange to provide or to make payment for the health care service(s) which is the basis of the external appeal, to the enrollee to the extent that such health care service(s) is provided while the enrollee has coverage with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is not required to provide any health care services to an individual who is no longer a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN enrollee at the time of an external appeal agent’s reversal of TOTAL CARE’s utilization review denial. If the external appeal was expedited, the enrollee or enrollee’s designee and TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will be notified immediately by telephone or fax of the external appeal agent’s decision. Written notification will follow. If the external appeal was not expedited, the enrollee or enrollee’s designee and TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will be notified in writing within two business days of the external appeal agent’s decision. Grievances Grievances may be mailed to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, PO Box 11507, Syracuse, NY 13218-1507, ATTN: Member Services. Grievances may be requested by telephone toll free at (877) 872-4715. This toll free number is the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member Service line. Member Services will direct your call to the appropriate person within TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. Grievances Process TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Grievance Process includes the following regarding the handling of the Enrollee Grievance: 1 The Enrollee/Enrollee designee may file a Grievance regarding any dispute with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN orally or in writing. The Contractor may have requirements for accepting written Grievances either by letter or TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN supplied form. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN cannot require an Enrollee/Enrollee designee to file a Grievance in writing. 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN must provide written acknowledgment of any Grievance not immediately resolved, including the name, address and telephone number of the individual or department handling the Grievance, within fifteen (15) business days of receipt of the Grievance. The acknowledgment must identify any additional information required by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN from any source to make a determination. If a Grievance determination is made before the written Revised January 2015 Section 9 Page 16 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL acknowledgement is sent, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN may include the acknowledgement with the notice of the determination (one notice). 3 Grievances pertaining to clinical matters will be reviewed by one or more licensed, certified or registered health care professionals in addition to whichever non-clinical personnel TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN designates. Timeframes for Grievance Resolution by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN‘s Grievance Process will indicate the following specific timeframes regarding Grievance resolution: 1 If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN immediately resolves an oral Grievance to the Enrollee’s satisfaction, that Grievance may be consider resolved without any additional written notification to the Enrollee. Such Grievances must be logged by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and included in TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s quarterly Health Provider Network (HPN) Grievance Report submitted to SDOH. 2 Whenever a delay would significantly increase the risk to an Enrollee’s health, the Grievances will be resolved within forty-eight (48) hours after receipt of all necessary information and no more than seven (7) days from the receipt of the Grievance. 3 All other Grievances will be resolved within forty-five (45) days after the receipt of all necessary information and no more than sixty (60) days from receipt of the Grievance. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will maintain reports of Grievances unresolved after forty-five (45) days. On a quarterly basis TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN provides a Grievance Summary Form via the HPN that have been unresolved. Grievance Determination Notices TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s procedures regarding the resolution of Enrollee Grievances will include the following: 1 Grievance Determinations by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will be made in writing to the Enrollee/Enrollee designee and include: a b c Revised January 2015 The detailed reasons for the determination; In cases where the determination has a clinical basis, the clinical rationale for the determination; The procedures for the filing of an appeal of the determination, including a form, used by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN for the filing of such a Grievance Appeal; and notice of the right of the Enrollee/Enrollee designee to contact the State Department of Health regarding his or her Grievance, including SDOH’S toll-free number for Grievances. Section 9 Page 17 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL 2 If TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN was unable to make a Grievance determination because insufficient information was presented or available to reach a determination, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will send a written statement that a determination could not be made to the Enrollee/Enrollee designee on the date the allowable time to resolve the Grievance has expired. 3 In cases where delay would significantly increase the risk to an Enrollee’s health, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide notice of a determination by telephone directly to the Enrollee/ Enrollee designee, or when no phone is available, some other method of communication, with written notice to follow within three (3) business days. Grievance Appeals TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s procedures regarding Enrollee Grievance Appeals will include the following: 1 The Enrollee/Enrollee designee has no less than sixty (60) business days after receipt of the notice of the Grievance determination to file a written Grievance Appeal. Grievance Appeals may be submitted by letter or by a form provided by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. 2 Within fifteen (15) business days of receipt of the Grievance Appeal, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide written acknowledgement of the Grievance Appeal, including the name, address and telephone number of the individual designated to respond to the Appeal. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will indicate what additional information, if any, must be provided for TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to render a determination. 3 Grievance Appeals of clinical matters must be decided by personnel qualified to review the Appeal, including licensed, certified or registered health care professionals who did not make the initial determination, at least one of whom must be a clinical peer reviewer. 4 Qualified personnel at a higher level than the personnel who made the original Grievance determination will determine grievance Appeals of non-clinical matters. 5 Grievance Appeals will be decided and notification provided to the Enrollee/Enrollee designee no more than: Two (2) business days after the receipt of all necessary information when a delay would significantly increase the risk to an Enrollee’s health; or Thirty (30) business days after the receipt of all necessary information in all other instances. 6 The notice of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s Grievance Appeal determination will include: The detailed reasons for the determination; The clinical rational for the determination in cases where the determination has a clinical basis; The notice will also inform the Enrollee of his/her option to also contact the State Department of Health with his/her Grievance, including the SDOH’s toll-free number for Grievances (New York State Department of Health Toll free at 1 800 206-8125); Revised January 2015 Section 9 Page 18 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Instructions for any further Appeal, if applicable. Important Telephone Numbers and Addresses Enrollees/Enrollee designees and providers may contact the following agencies at any time with a Grievance: TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member Service Department Toll free at 1 877 872-4715 or write to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PO Box 11507 Syracuse, New York 13218-1507 Cortland County Department of Social Services (607) 753-5248 Onondaga County Department of Social Services (315) 435-3525 Oswego County Department of Social Services (315) 963-5481 Tompkins County Department of Social Services (607) 274-5667 New York State Department of Health Toll free at 1 800 206-8125 Or write to: New York State Department of Health Bureau of Certification and Surveillance Corning Tower Albany, New York 12237 Revised January 2015 Section 9 Page 19 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 10 EXTERNAL APPEALS External Appeals Request made to the state by health care consumers or health care providers for an independent review of denial of services by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN that the health care service is: a) Not medically necessary or is experimental or investigational. b) The denial has been upheld as a final adverse determination or both TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and the enrollee/enrollee designee have jointly agreed to waive any internal appeal. Written notification of this agreement will be sent to the Enrollee/Enrollee Designee within 24 hours. c) And the enrollee’s attending physician has certified that the enrollee has a lifethreatening or disabling condition of disease 1) for which standard health services or procedures have been ineffective or would be medically inappropriate or 2) for which there does not exist a more beneficial standard health service or procedure covered by the health care plan or #0 for which there exist a clinical trial d) And the enrollee’s attending physician, who must be a licensed, boardcertified physician qualified to practice in the area of practice appropriate to treat the enrollee’s life-threatening or disabling condition or disease, must have recommended either 1) a health service or procedure (including a pharmaceutical product within the meaning of Public Health Law 4900(5) (b) (B) , that based on two documents from the available medical and scientific evidence, is likely to be more beneficial to the enrollee than any covered standard health service or procedure; or 2) a clinical trial for which the enrollee is eligible. Any physician certification provided under this section will include a statement of the evidence relied upon by the physician in certifying his or her recommendation, e) And the specific health service or procedure recommended by the attending physician would otherwise be covered under the policy except for TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s determination that the health service or procedure is experimental or investigational. External appeal requests must be submitted within 45 days upon receipt of the final adverse determination of the first level appeal. An enrollee, enrollee designee and, in connection with retrospective determinations, an enrollee’s health care provider has the right to request an external appeal. Response to External Appeal Requests TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will facilitate the prompt completion of external appeal requests, including but not limited to, the following: Revised September 2014 Section 10 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL A TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide the enrollee with a copy of the standard description of the external appeal process as developed jointly by the commissioner and superintendent, including a form and instructions for requesting an external appeal: • • • • Simultaneous with a notice of a final adverse determination that a health care service is not medically necessary, including on the grounds that the health care service is experimental or investigational; or Simultaneous with the written confirmation of agreement between the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and the enrollee to waive the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s internal appeal process; and Within three business days of a request by an enrollee or an enrollee’s designee Within three business days of a request by an enrollee or an enrollee’s designee B Upon receiving notification regarding the identity and address of the certified external appeal agent, the assigned staff Enrollee/Enrollee designee will transmit the insured’s medical and treatment records and in the case of medical necessity appeals, the clinical standards used to determine medical necessity for health care services to the agent. This transmission will occur within three business days for standard appeals and within 24 hours for an expedited appeal. C Requests for additional information by the assigned certified external appeal agent will be responded to as soon as possible, but no longer than two business days for standard appeals. Requests for information relative to expedited appeals will be provided to the assigned external appeal agent within 24 hours of the request. Provider Request For External Appeal If a health care provider requests a copy of a form for an external appeal in connection with a retrospective adverse utilization review determination, TOTAL CARE’s QA/UR Director will send to the provider a form and instructions within three business days of the provider’s request. Results Of External Appeal a In the event an adverse determination is overturned on external appeal, or if TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN reverses a denial which is the subject of external appeal, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide, arrange to provide or to make payment for the health care service(s) which is the basis of the external appeal, to the enrollee to the extent that such health care service(s) is provided while the enrollee has coverage with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Revised January 2015 Section 10 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL is not required to provide any health care services to an individual who is no longer a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN enrollee at the time of an external appeal agent’s reversal of TOTAL CARE, A TODAY’s OPTIONS OF NEW YORK HEALTH PLAN’s utilization review denial. b If the external appeal was expedited, the enrollee or enrollee’s designee and TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will be notified immediately by telephone or fax of the external appeal agent’s decision. Written notification will follow. c If the external appeal was not expedited, the enrollee or enrollee’s designee and TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will be notified in writing within two business days of the external appeal agent’s decision. Revised January 2015 Section 10 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDE MANUAL Section 11 PHARMACY TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN views the managing of outpatient prescription drugs as an integral part of the health care delivery system. Outpatient prescription drugs are a covered benefit for Medicaid Managed Care, Family Health Plus and Child Health Plus members. Pharmacy charges billed to Express Scripts. Express Scripts is the Pharmacy Benefit Manager for TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN; they can be reached at 1-877891-5279. Here is a brief overview of how the program works: • • • • • Providers must adhere to the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Formulary. The formulary can be found at www.totalcareny.com under Pharmacy Services Request for non-Formulary medication must be approved by the Medical Director In cases of an emergency, non-Formulary medication can be prescribed for a oneweek supply. Refills require an approval by the Medical Director Patients must obtain their prescriptions from an approved network pharmacy Request for additions to the Formulary may be directed to the Medical Director by submission of the Request Form for a Formulary addition Revised January 2015 Section 11 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDE MANUAL Section 12 TERMINATION OF CONTRACT PROCEDURES FOR TERMINATION OF CONTRACT BETWEEN TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN AND HEALTH CARE PROFESSIONALS To afford a health care professional the opportunity for review or hearing, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will provide a written explanation of reasons for a proposed termination with the health care professional. However, written notification will not be required in cases involving imminent harm to patient care, a determination of fraud, or a final disciplinary action by a state licensing board or other governmental agency that impairs the health care professional’s ability to practice, nor are they eligible for hearing or review. The notification of the proposed termination by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN to the health care professional will include: A. The reasons for the proposed action; B. Notice that the provider has the right to request a hearing or review before a panel appointed by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN; C. A time limit of not less than thirty days within which a health care professional may request a hearing, and D. A time limit for a hearing date that will be held within thirty days after the date of receipt of a request for a hearing. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will not terminate a contract or employment, or refuse to renew a contract, solely because a health care provider has: A. Advocated on behalf of an enrollee; B. Filed a complaint against TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN; C. Appealed a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN decision; D. Provided information or filed a report pursuant to PHL §4406-c regarding prohibitions by plans, or E. Requested a hearing or review pursuant to PHL §4406-d and the following sections. Revised January 2015 Section 12 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDE MANUAL Except as provided above, no contract or agreement between TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and a health care professional will contain any provision, which will supersede or impair a provider’s right to notice of reasons for termination and the opportunity for a hearing or review concerning such termination. HEARING A health care professional that has been notified of his or her proposed termination will be allowed a hearing. The health care professional must request a hearing within 30 days of notification by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. A hearing will be held within 30 days after the date of receipt of a request for a hearing. The procedures for this hearing must meet the following standards: A. The hearing panel will be comprised of three persons appointed by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN. At least one person on such panel will be a clinical peer in the same discipline and the same or similar specialty as the health care professional under review. The hearing panel may consist of more than three persons, provided however that the number of clinical peers on such panel will constitute one-third or more of the total membership of the panel. B. The hearing panel will render a decision on the proposed action in a timely manner. Such decision will include reinstatement of the health care professional by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, provisional reinstatement subject to conditions set forth by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN or termination of the health care professional. Such decision will be provided in writing to the health care professional. C. A decision by the hearing panel to terminate a health care professional will be effective not less than thirty days after the receipt by the health care professional of the hearing panel’s decision. Notwithstanding the termination of a health care professional for cause or pursuant to a hearing, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will permit an enrollee to continue an on-going course of treatment for a transition period of up to ninety (90) days, and post-partum care, subject to provider agreement, pursuant to §4406(6)(e). D. In no event will termination be effective earlier than sixty days from the receipt of the notice of termination. Revised January 2015 Section 12 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDE MANUAL NON-RENEWAL Either party to a contract may exercise a right of non-renewal at the expiration of the contract period set forth therein or, for a contract without a specific expiration date, on each January first occurring after the contract has been in effect for at least one year, upon sixty days notice to the other party; provided, however, that any non-renewal will not constitute a termination for purposes of this section. PHL §4403(6)(e), concerning continuation of course of treatment and post-partum care, also applied to disaffiliations based upon non-renewal. Notification of non-renewal will contain explanation of the right of non-renewal, time frames and language that non-renewal does not constitute termination. Revised January 2015 Section 12 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL Section 13 Fraud and Abuse Health Care fraud and abuse increases costs for everyone. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is required by The New York State Department of Health to safeguard the entrusted Health Care Programs that we administer. To meet our obligation, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN has contracted with Ingenix to perform proprietary review of claims and medical records. Effective July 1, 2006, you will be receiving medical records requests from Ingenix on behalf of TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN for any claim(s) under review. We encourage your prompt response to these requests. We at TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN thank you and appreciate your cooperation in this matter. Ingenix is considered a HIPAA “Business Associate”, who has access to Provider and/or Member’s Protected Health Information (a.k.a. PHI). Attached is a copy of the Ingenix Request for Medical Records Form for your review. For information regarding fraud and abuse providers will find the following website educational: http://www.health.state.ny.us/health_care/medicaid/fraud/index.htm The important issues addressed on this website include: Impact of Medicaid Fraud Who commits fraud Examples of fraud How to report fraud Contact TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN If you wish to speak with someone from TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN regarding these issues, please contact Provider Relations at (315) 234-5907, (315) 234-5908 or toll free (877) 872-4716. Revised January 2015 Section 13 Page 1 0 Section 14 Page TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL Section 14 HIV Guidelines HIV Confidentiality All providers must comply with the HIV confidentiality provisions of Section 2782 of the New York Public Health Law to assure the confidentiality of HIV related information. Compliance requires: Initial and annual in-service education of staff and contractors Identification of staff allowed access to HIV related information and the limits of access Procedure to limit access to trained staff, including contractors Protocol for secure storage, including electronic storage Procedures for handling requests for HIV related information; and Protocols to protect from discrimination persons with or suspected of having HIV infection. For complete details, please see the following websites: http://www.health.ny.gov/diseases/aids/providers/regulations/ http://public.leginfo.state.ny.us/LAWSSEAF.cgi?QUERYTYPE=LAWS+&QUERYD ATA=$$PBH2782$$@TXPBH02782+&LIST=LAW+&BROWSER=EXPLORER+& TOKEN=42601282+&TARGET=VIEW Role of the Primary Care Provider (PCP): The PCPs’ roles are critical in the early identification of members at risk for HIV infection or disease. A person of any age, sex, race, ethnic group, religion, economic background, or sexual orientation can get HIV. At Risk Members: The following partial factors heighten the possibility that a member may be at risk for HIV: Injection drug users (IDU) – Injected drugs or steroids with others, piercing, tattooing, or used shared equipment (e.g. syringes, needles, works) currently or any time in the past; Been diagnosed with or been treated for hepatitis, tuberculosis (TB), or a sexually transmitted disease such as gonorrhea, Chlamydia or syphilis; Unprotected anal, vaginal and oral sex – Had unprotected vaginal, anal, or oral sex with multiple partners, anonymous partners , or men who have sex with men; Revised January 2015 Section 14 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL Sexual partner with known HIV infection; Had sex with a partner they located on the Internet; Infants born to HIV infected mothers - Babies can potentially become infected during their mother's pregnancy, during delivery, or after birth in the immediate postpartum period. They can also become infected through breastfeeding. Health care and maintenance workers who may be exposed to blood and/or body fluids at work sometimes get infected through on-the-job exposures like needlestick injuries. Individuals who received a transfusion of blood or blood products before screening of the blood supply for HIV antibody was initiated in 1985. See specific guidelines at: https://www.health.ny.gov/diseases/aids/consumers/hiv_basics/100_questions/basicinfo rmation.htm) Symptoms: The PCP should consider the possibility of HIV infection when minimally the following signs or symptoms are noted: Persistent fevers Night sweats Weight loss Lymphadenopathy Chronic diarrhea Counseling, Screening: Members may seek HIV counseling and testing services outside of the plan network providers. Members also should be advised that such services are obtainable anonymously through the New York State Anonymous Counseling and Testing Programs. This is available at various clinics in each NYS county in addition to free testing for sexually transmitted diseases. Hours and locations can be accessed at https://www.health.ny.gov/diseases/communicable/std/clinics/ and the AIDS Hotline: 1-800-541-AIDS. The Provider must counsel, screen, manage and/or refer patients consistent with the guidelines established by the AIDS Institute of the New York State Department of Health. Every individual between the ages of 13 and 64 years (or younger or older if there is evidence or indication of risk activity) who receives health services as an inpatient or in Section 14 Page 2 Revised January 2015 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL the emergency department of a general hospital defined in Subdivision 10 of Section 2801 of the Public Health Law or who receives primary care services in an outpatient department of such hospital or in a diagnostic and treatment center licensed under Article 28 of the Public Health Law or from a physician, physician assistant, nurse practitioner, or midwife providing primary care in any office, clinic, facility or other setting shall be offered an HIV-related test unless the health care practitioner providing such services reasonably believes that: the individual is being treated for a life threatening emergency; or the individual has previously been offered or has been the subject of an HIVrelated test (except that a test shall be offered if otherwise indicated); or the individual lacks capacity to consent to an HIV-related test. Consent for Testing: If HIV testing is done, informed verbal consent must be obtained and documented in the medical record. Consent can remain in effect for a period of time stipulated by the patient or until revoked by the patient orally or in writing. The member still must be informed each time an HIV test is to be performed and must be given the opportunity to decline. Multi-lingually translated consent templates can be found at https://www.health.ny.gov/diseases/aids/providers/forms/informedconsent.htm. Prior to being asked to consent to HIV testing, patients must be provided information about HIV required by the Public Health Law. Prior to asking for consent to perform the HIV test, the following key points must be provided. The key points may be delivered orally, in writing or via electronic means. These key points are listed below and can be found at http://www.health.ny.gov/publications/9678/index.htm HIV is the virus that causes AIDS. It can be spread through unprotected sex (vaginal, anal, or oral sex) with someone who has HIV; contact with HIV-infected blood by sharing needles (piercing, tattooing, drug equipment, including needles); by HIV-infected pregnant women to their infants during pregnancy or delivery, or by breast feeding. There are treatments for HIV/AIDS that can help a person stay healthy. People with HIV/AIDS can use safe practices to protect others from becoming infected. Safe practices also protect people with HIV/AIDS from being infected with different strains of HIV. Testing is voluntary and can be done at a public testing center without giving your name (anonymous testing). By law, HIV test results and other related information are kept confidential (private). Discrimination based on a person’s HIV status is illegal. People who are discriminated against can get help. Revised January 2015 Section 14 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL Consent for HIV-related testing remains in effect until it is withdrawn verbally or in writing. If the consent was given for a specific period of time, the consent applies to that time period only. Persons may withdraw their consent at any time. Health care and other HIV test providers authorizing HIV testing must arrange, with the consent of the patient, an appointment for medical care for those confirmed as positive. Anonymous HIV testing of source patients in occupational exposure situations who are unable to provide consent is allowed in certain circumstances, though results cannot be shared with the source patients or included in their medical record. The capacity to consent to an HIV test (either confidential or anonymous) is determined without regard to age. Providers offering HIV testing must make a determination as to the patient’s capacity to consent. If a practitioner determines a person under 18 years old does not have the capacity to consent, the offer of testing for the young person should be made to a parent or other person authorized to provide consent. If a member is tested, pre- and post-test counseling must be completed and documented in the medical record. Member Educational materials related to HIV are available through the New York State Department of Health Institute (Attachment A– New York State Department of Health AIDS Institute, HIV/AIDS – consumer Educational Materials Order Form). Reporting: The PCP is responsible to report all members testing HIV positive to the New York State Department of Health consistent with the communicable disease reporting requirements. This would apply to new HIV disease as well as any change in HIV status. Positive Results: All determinations or diagnoses of Human Immunodeficiency Virus (HIV) infection, HIV-related illness and Acquired Immune Deficiency Syndrome (AIDS) shall be reported to the commissioner by physicians and other persons authorized to order diagnostic tests or make medical diagnoses or their agents as soon as possible after post-test counseling but no later than 14 days after the provider's receipt of a positive laboratory result or after diagnosis, whichever is sooner. (Source: Effective Date: 02/22/2012, Title: Section 63.3 - HIV-related testing (http://w3.health.state.ny.us/dbspace/NYCRR10.nsf/11fb5c7998a73bcc852565a1004e9 f87/8525652c00680c3e8525652c004f3d82?OpenDocument) Revised January 2015 Section 14 Page 4 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL The testing provider must provide test results (directly or through a representative) to a person who tests HIV positive. The testing provider also must, with the consent of the patient, help arrange an appointment for medical care for those members confirmed as positive as soon as possible. coping emotionally with the test results; discrimination issues relating to employment, housing, public accommodations, health care and social services; authorizing the release and revoking the release of confidential HIVrelated information; preventing high risk sexual or needle-sharing behavior; the availability of medical treatment; HIV reporting requirements for the purposes of monitoring of the HIV/AIDS epidemic; the advisability of contacts being notified to prevent transmission, and to allow early access of exposed persons to HIV testing, health care, and prevention services, and a description of notification options and assistance available to the protected individual; the risk of domestic violence in conformance with a domestic violence screening protocol developed by the commissioner pursuant to law; the fact that known contacts, including a known spouse, will be reported and that protected persons will also be requested to cooperate in contact notification efforts of known contacts and may name additional contacts they wish to have notified with the assistance of the provider or authorized public health officials; protection of names and other information about HIV-infected persons during the contact notification process; the right to have an appointment made for HIV follow-up medical care, the use of HIV chemotherapeutics for prophylaxis and treatment, and the availability of peer group support. the risk of perinatal transmission Negative Results: A person who tests HIV negative must be provided with the result and information concerning risks of participation in sexual and needle-sharing activities that can result in infection. This information may be in the form of written materials such as that available on the Department’s website. The negative test result and required information do not need to be provided in person. Other mechanisms such as email, mail, and phone may be used as long as you have taken steps to ensure the patient’s confidentiality. Patients who are consented orally and given a rapid test should be provided their results during the same clinic visit or the same day. Also, it is not appropriate to only tell patients that if they are not contacted, they may assume their tests were negative. However, it is acceptable to provide patients with the required information and a phone number or other means of confirming their negative result if they choose to. Revised January 2015 Section 14 Page 5 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL Pregnant Women: 1. Identifying Acute HIV Infection (AHI) During Pregnancy: Immediate testing is recommended for any pregnant woman who presents with a clinical syndrome compatible with Acute HIV Infection (AHI) without a known cause, even if she tested HIVnegative earlier in pregnancy. General information on AHI may be found at http://www.hivguidelines.org. In suspected cases of AHI during pregnancy: • Immediate testing using an HIV antibody test and an HIV RNA test should be performed. If either is positive or there is strong clinical suspicion: • Immediate consultation with an HIV specialist regarding diagnosis and treatment; • Confirmatory antibody testing 3-6 weeks later if the HIV RNA test is positive and the initial antibody test is negative or indeterminate. Testing for AHI in pregnancy may be accessed by contacting: • In New York City: New York City Department of Health & Mental Hygiene, HIV Surveillance and Epidemiology Program, Provider Line (212) 442-3388; • Outside New York City: New York State Department of Health, Wadsworth Center, Diagnostic HIV Laboratory (518) 474-2163. 2. HIV Testing in the Third Trimester: In concert with the Centers for Disease Control and Prevention (CDC), the New York Department of Health recommends that prenatal providers routinely recommend repeat HIV testing, preferably at 34-36 weeks, for all women who test negative early in prenatal care. The second test ideally should be at least three months after the initial test. Repeat testing will identify women who become infected with HIV during pregnancy, a group which accounts for an increasing proportion of MTCT. Revised January 2015 Section 14 Page 6 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL 3. Point-of-Care Rapid HIV Testing in Delivery Settings: Implementing point-of-care (rapid) testing facilitates timely administration of prophylaxis to HIV-positive women and their exposed newborns. For women diagnosed with HIV during labor, HIV antiretroviral (ARV) regimens to prevent mother-to-child HIV transmission (MTCT) are most effective if initiated during labor, HIV antiretroviral (ARV) regimens to prevent MTCT are most effective if initiated during labor or, if intrapartum ARV is not possible, to the newborn within 12 hours of birth. The New York Department of Health recommends: All birth facilities adopt point-of-care rapid HIV testing in labor and delivery settings. Expedited HIV test results should be available within an hour to facilitate effective administration of ARV prophylaxis. For information on rapid testing, see: http://www.nyhealth.gov/diseases/aids/testing/rapid/index.htm 4. Assuring Access to Care and Supportive Services: To facilitate linkages to care and to provide the support many women need, we consider it a standard of care to link HIV-positive pregnant and postpartum women, including those who deliver without prenatal care, to HIV-specific case management and supportive services. 5. Resources: Consultation and technical assistance for prenatal care providers and hospital obstetrical departments is available from: • HIV Clinical Education Initiative (CEI): call (518) 473-8815 or visit www.hivguidelines.org. • HIVAIDS Regional Training Centers: These centers offer training on reducing MTCT and expedited and rapid testing in obstetrical settings. See http://nyhealth.gov/diseases/aids/training/index.htm. Resources specific to case management of HIV patients are available at www.cobracm.org. HIV Practice Guidelines: Total Care, A Today’s Options of New York Health Plan has adopted the clinical practice guidelines of the New York State Department of Health AIDS Institute. Clinical Guidelines pertain to HIV prevention and medical management of adults, children, and adolescents with HIV infection. Clinical guidelines can be accessed at www.hivguidelines.org. Revised January 2015 Section 14 Page 7 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN MANUAL HIV Provider Access: HIV qualified providers are listed in the Provider Directory as HIV Specialty Care Centers and HIV/AIDS specialists. If services are not available in network or geographically convenient for the member, the member can request services outside the TC/TONY provider network. If the member prefers to have the HIV provider act as their PCP, the member can request such. HIV Member Educational Materials: Providers can order additional New York State Resources using this form: http://www.health.ny.gov/forms/order_forms/hiv_educational_materials.pdf Revised January 2015 Section 14 Page 8 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 15 Transportation Policy TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is required to provide emergency transportation (ambulance) services for Family Health Plus and Child Health Plus members in Oswego, Onondaga, Cortland and Tompkins Counties. Medicaid Managed Care members emergency transportation in Onondaga County is billed to fee for service Medicaid. Non emergency transportation for Onondaga County Medicaid Managed Care members is arranged for through the Medical Answering Service (MAS) at 1-855-852-3287 or www.medanswering.com. Family Health Plus and Child Health Plus Benefit Plans have no non emergency benefits. Non emergency transportation for Owego, Cortland and Tompkins Counties are billed to fee for service Medicaid. Providers in these counties may contact their local Department of Social Services for assistance in obtaining non-emergent medical transportation services. Revised January 2015 Section 15 page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 16 Section 16 DEFINITIONS For the purposes of this manual, the following terms shall have the meanings set forth below: 1 Allied Provider: Non-physician professionals, such as psychologists, social workers, nurse-midwives, and physical, occupational, speech and respiratory therapists, who provide direct health care services to patients. 2 Ancillary Provider: Non-physician and non-hospital providers such as diagnostic laboratories, physiological laboratories, home health agencies, skilled nursing facilities, hospices, urgent care centers, outpatient surgical centers, durable medical equipment suppliers, home infusion suppliers, pharmacies, and other suppliers and vendors. 3 Authorization: A determination that a service is medically necessary based upon the circumstances described at the time that the authorization was given and the duration specified at the time that the authorization was given. An approval given by the PCP for covered services or in certain instances as defined in the precertification section and approval given by the Plan. 4 Covered: A term to describe those health care services included in a health insurance plan. 5 Disenrollment: Leaving the Plan. Voluntary disenrollment: TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN member chooses to leave the plan. Involuntary disenrollment: Loss of Medicaid or CHIP eligibility based on the policies and procedure of the Department of Social Services and/or the Plan. 6 Emergency Care: An emergency is a medical or behavioral condition, the onset of which is sudden, that manifests itself by symptoms of sufficient severity, including severe pain, that a prudent layperson possessing an average knowledge of medicine and health, could reasonably expect the absence of immediate medical attention to result: 1) in placing the health of the person afflicted with such condition in serious jeopardy, or in the case of a behavioral condition, placing the health of the person or others in jeopardy or 2) serious impairment to such person’s bodily functions or 3) serious dysfunction of any bodily organ or part of such person, or serious disfigurement of such person. 7 Encounter: A visit to a Network Provider to receive medical services. 8 Enrollment: Becoming a member of the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Revised January 2015 Section 16 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 16 9 Explanation of Payment ("EOP"): A printed statement addressed to a TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN member or provider-itemizing services performed and benefit information related to those services. 10 Fee-For-Service: Reimbursement of services based on the cost per procedure. 11 Guaranteed Eligibility: The period beginning on the Enrollee’s Effective Date of Enrollment with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN and ending six (6) months thereafter, during which the Enrollee may be entitled to continued enrollment in TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s plan despite the loss of Medicaid eligibility. 12 Medically Necessary: Means health care and services that are necessary to prevent, diagnose, manage or treat conditions in the person that cause acute suffering, endanger life, result in illness or infirmity, interfere with such person’s capacity for normal activity, or threaten some significant handicap. 13 Plan: A program of health care benefits offered or administered to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN members for groups and individuals. 14 Primary Care Provider (PCP): A board certified physician or licensed nurse practitioner in general practice, internal medicine or pediatrics that has entered into an agreement with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN INC. The TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN member selects the PCP. All aspects of medical care for the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN member become the responsibility of the selected PCP. These responsibilities include providing personal medical care by the PCP or referring the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN member to an appropriate source of medical care. The appropriate source of medical care may be a specialist physician, allied or ancillary provider or inpatient facility. 15 Referral care: Medical care or testing arranged for by the PCP provided by a specialist and/or facility outside the PCP office. 16 Explanation of Payment Statement: A detailed summary of all claims and encounters processed for an individual provider that may be accompanied by a check payable to that provider. 17 Specialist Physician: Typically a board-certified physician, such as a dermatologist, neurologist, cardiologist or OB\GYN, who provides specialty Revised January 2015 Section 16 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 16 medical care to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN member. 18 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Member: A person eligible for health care benefits under TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Revised January 2015 Section 16 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL SECTION 17 PROVIDER CREDENTIALING PROCEDURE Scope of Providers to be credentialed TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will credential all licensed and certified Providers who are seeking to join the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Participating Providers Network. Participating Providers are those who have contracted with TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN, give services to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN members, are listed as Participating in the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Provider Directory, and are listed by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN as Participating on all reports to NYSDOH (i.e. HPN submissions). Participating Providers to be credentialed will include, but not be limited to: MD DO DDS DMD DPM NP CDN RPAC OD PhD OT SLP PT Audiologist MC, MA Counselors CASAC Counselors CM CNM CSW TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN requires Primary Source Verification of the following criteria for credentialing: Evidence of a valid current license (license must be in effect at the time of the credentialing decision) Evidence of valid DEA as applicable (Certificate must be in effect at the time of credentialing decision) Education and training of Provider Board certification, when applicable Work history Malpractice History-history of professional liability claims that resulted in settlements of judgments paid by or on behalf of the practitioner. Additional Credentialing Criteria will include: Revised January 2015 Section 17 Page 1 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Application and Attestation including: Reasons for any inability to perform the essential functions of the position, with or without accommodation; Lack of present illegal drug use; History of loss of license and felony convictions; History of loss or limitation of privileges or disciplinary activity; Current malpractice insurance coverage; and Correctness and completeness of the application. The application must be signed and dated within 180 calendar days of the credentialing decision. Query National Practitioner Data Bank (NPDB) for any sanctions imposed by Medicare/Medicaid and includes it in the credentialing files. (Within 180 days of credentialing decision) License sanctions or limitations Previous sanction activity by Medicare and Medicaid Review of provider’s physical site of practice (per Policy #035) including review of medical record documentation. Query the List of Excluded Individuals and Entities (LEIE), the Social Security Administration Death Master File, and the National Plan Provider Enumeration System (NPPES) TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN recredentials providers at least once every three years. During such recredentialing, plan will reexamine the items covered during the initial credentialing, as well as: Complaints lodged against the provider by plan members; Results of chart audits and other quality improvement activities. In the event that TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN denies credentialing or terminates a provider’s contract (including in response to the recredentialing process) for program integrity related reasons, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will report such adverse action to the New York State Department of Health and the Office of the Medicaid Inspector General as described in TC.PR.001. Revised January 2015 Section 17 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Credentialing Validation Organization Vendor TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN contracts with a credentialing validation organization (Optum) contracted to provide primary source verification and other credentialing duties. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will retain responsibility to ensure that every participating provider in the network meets the credentialing criteria set forth by the Plan. The agreement with Optum specifically authorizes such duties and TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is indemnified by Optum for services rendered Optum. Optum provides a written document to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN that each participating provider meets the established credentialing criteria, or clearly indicates where, if applicable, any criterion is omitted. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will review and approve the Vendor credentialing and recredentialing policies and procedures to ensure compliance with the NYSDOH guidelines. If applicable, this evaluation will include a review of the files for the presence of: Plan Approved criteria collection; Availability of required data elements and primary source verification per Plan Policy; Evaluation of provider credentialing files for completeness including all supporting documentation per Plan Policy and Procedure. If applicable, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN shall provide technical assistance and consultation to the Vendor as appropriate. Optum must obtain approval from TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN before making any changes to the credentialing policy. Optum provides TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN with an accurate detailed provider file and if applicable, any reports of the Vendor Credentialing Activities. The Medical Director shall ensure that an annual audit of the vendor credentialing procedures and files is done to assess the vendor’s activity through evaluation of the adequacy and completion of the provider credentialing files per Plan Credentialing Policy and Procedure (see Validation Process). Revised January 2015 Section 17 Page 3 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Once provider information is received from Optum, the file is reviewed for completeness by QA/UR staff (Attachment 1). Once all information is reviewed, the provider is added to the listing for acceptance by the Credentialing Committee. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will review and approve the credentialing and recredentialing of each provider by obtaining approval and acceptance of each provider by the Credentialing Committee. For providers new to the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN network, notification is sent to the provider confirming their acceptance into the network (Attachment 2). This notification must occur within 90 days of when TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN received the completed application. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will notify the provider as to whether the provider is credentialed; or whether additional time is necessary to make a determination despite: TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s best efforts or because a third party failed to provide necessary documentation. Non-Routine or unusual circumstances require additional time for review. In such instances where additional time is necessary because of a lack of necessary documentation, TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN will make every effort to obtain such information as soon as possible. 1.1 Annual Validation Process: Because TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN contracts with a Credentialing Validation Organization, a representative sampling of provider credentialing files will be audited by TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN annually. The criteria for selection of files are: Credentialing Validation Organization-At a minimum, 5% or 50 Provider files (whichever is less) from the various specialty types should be reviewed. The selection should include both initial credentialing and recredentialing files. The credentialing files reviewed must demonstrate that the Vendor is effective in: Applying collection criteria uniformly; Processing new applications and reapplications within the time frames established by policy, bylaws, and Contract. Credentialing files/data are kept in accordance with Plan Credentialing Policy and Procedure. Validation Checklist will be used to document audit results. (Attachment 3) Revised January 2015 Section 17 Page 4 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Medical Director will bring results of the Annual Validation Audit to TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Credentialing Committee and Quality Assurance Committee. As issues arise with the Vendor, they should be resolved by the Medical Director. A summary of issues with the Vendor and resolutions should be included in the Medical Director’s annual report to the board of directors on the annual validation. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s audit report will be presented by the Medical Director to the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Board of Directors for approval and/or recommendations for corrective action annually. In instances where findings of the validation audit show significant disagreement between the Vendor policies and its functional credentialing, the Plan Medical Director may choose to provide technical assistance or may rescind the vendor agreement. TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Credentialing Process Quality Assurance Nurse Role- Quality Assurance Nurse receives all credentialing files weekly and reviews against criteria. Nurse will note whether provider meets criteria under each criteria point. Nurse will indicate if all criteria is met or whether it requires additional review. Nurse forwards files for Medical Director Review. Medical Director reviews the initial credentialing and re-credentialing files and signs off on “clean” files. Clean files are defined as those in which no additional review is required. Medical Director role- The Medical Director is responsible to present the credential findings to the Credentialing Committee. The Credentialing Committee has the delegated authority to approve, or approve with conditions and/or deny/terminate participation in TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN’s network. The Medical Director will at a minimum refer for full Credentials Committee review the following: Primary Care Provider with more than 3 malpractice awards/settlements within the past 10 years. Primary Care Provider with more than $1,000,000 in aggregate malpractice awards/settlements within the past 10 years. Specialists with more than 5 malpractice awards/settlements >$20,000 within the past 10 Revised January 2015 Section 17 Page 5 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL years. Specialists with more than $2 million in malpractice awards /settlements within the past 10 years. For the purposes of this calculation any one malpractice award/settlement is capped at $1,000,000. Any disciplinary action by NYSDOH, Medicare of Medicaid. Any criminal conviction or pending prosecution within the past 15 years. 1.1.1 Board of Directors’ role- Delegate approval process to the Medical Director and the Credentialing Committee. The Medical Director is responsible to provide quarterly reports to the Board of Directors on the results of the credentialing process. Related Documentation Attachment 1- Credentialing File Checklist Attachment 2- Provider Acceptance Letter Attachment 3- Annual Validation Checklist Revised January 2015 Section 17 Page 6 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 1- Credentialing File Checklist PHYSICIAN: The above captioned physician was credentialed: Re-credentialing: CHECKLIST . . / Current valid license / Valid DEA / Board Certification / Malpractice coverage ($1/3 million current coverage) / History of professional liability claims / Medicare/Medicaid sanctions (Excluded Individuals and Entities (LEIE)) / Office of Professional Medical Conduct / NPDB (Covers Medicare/Medicaid Sanctions, OPMC Actions) / Social Security Administration Death Master File / National Plan Provider Enumeration System (NPPES) / Attestation to correctness/completeness of application / Chart Review (Recred Only) Reappointment application includes statements re: physical and mental competency to perform the privileges requested, history of loss of license and/or felony convictions, or limitation of privileges or disciplinary activity, pending and settled malpractice cases. Date Revised January 2015 Section 17 Page 7 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 2- Provider Acceptance Letter Date Dear Provider: We would like to take this opportunity to welcome you as a new Provider to the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Network. Our credentialing process has been completed and you have been accepted by the Plan’s Board of Directors to participate in our Network. Your TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN provider number is . Your name will be added to the TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Provider Directory as soon as possible. Please visit our website at www.totalcareny.com Here are some helpful phone numbers: Member Services Provider Dedicated Line (800) 223-7242 (315) 234-5901 or (877) 872-4716 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN is committed to assuring access to high quality, comprehensive, cost-effective health care services to Child Health Plus, Family Health Plus, and Medicaid Eligible populations throughout the State of New York, respectful of the dignity of those we serve, and responsive to the needs of our members. Thank you for sharing in our mission! If you have any questions regarding our credentialing process, please feel free to contact Maureen Fitzpatrick at (315) 634-5555 or toll free at (877) 872-4716. Sincerely, Dr. Mustafa Awayda MD TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN Assistant Medical Director Revised January 2015 Section 17 Page 8 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Attachment 3- Annual Validation Checklist VALIDATION CHECKLIST PHYSICIAN: The above captioned physician was credentialed: Re-credentialed: PRIMARY SOURCE VERIFICATION Current Valid License Valid DEA Education and Training of Provider Board Certification Work History Malpractice History. History of professional liability claims that resulted in settlements of judgments paid by or on behalf of the practitioner APPLICATION AND ATTESTATION INCLUDES: Reasons for any inability to perform the essential functions of the position, with or without accommodation Lack of present illegal drug use History of loss of license and felony convictions History of loss or limitation of privileges or disciplinary activity Malpractice Coverage ($1/3 million current coverage) The correctness and completeness of the application. The application must be signed and dated within 180 calendar days of the credentialing decision SANCTIONS National Practitioner Data Bank Query License sanctions or limitations Previous sanction activity by Medicare and Medicaid (List of Excluded Individuals and Entities (LEIE)) Social Security Administration Death Master File National Plan Provider Enumeration System (NPPES) Review of provider’s physical site of practice including review of medical record documentation ADDITIONAL RECREDENTIALING ITEMS Complaints lodged against the provider by plan members Results of chart audits and other quality improvement activities Plan Surveyors Signature Revised January 2015 Date Section 17 Page 9 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 18 SECTION 18 Tuberculosis Tuberculosis screening, diagnosis and treatment is a covered benefit for members of Total Care, A Today’s Options of New York Health Plan (TC/TONY). Screening Providers are responsible to appropriately screen TC/TONY members in accordance with the following: • Children: American Academy of Pediatrics, Recommendations for Preventive Pediatric Health Care • Adults: Adult Preventive Care Guidelines as defined by the US Preventive Services Health Task Force (http://www.uspreventiveservicestaskforce.org/) • Symptomatic considerations: skin test or chest x-ray for the following • Productive and/or prolonged cough; Chest pain; Hemoptysis; Fever, chills, night sweats, fatigue; or Weight loss. High Risk Populations: skin test or chest x-ray should be considered for the following: Positive HIV status; Foreign born persons where tuberculosis is common; Exposed to persons with tuberculosis; Unreliable histories; Suspected or known elicit injectable drug use; Residence of long term facilities; Socio-economic - homeless or low income; Persons with certain medical conditions in addition to +HIV status; or Children four years of age and under. Diagnosis and Testing • The Mantoux skin testing is the preferable skin testing method consisting of .1 ML of 5 TU PPD intradermally. The provider is responsible to ensure that the interpretation and documentation of the results are conducted by trained staff (i.e., licensed nurse, P.A., N.P., or physician). • A skin test is considered positive as below: Revised January 2015 Section 18 Page 1 Section 18 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Treatment o Equal or greater than 15MM induration (no known risk factors) o Equal or greater than 10MM induration (symptomatic or at risk groups). o Equal or greater than 5MM induration for patients that are immunocompromised, IV drug users, or having had contact with known infectious cases, people that have chest radiograph, suggestive of previous tuberculosis o Patients with a positive skin test should have a chest x-ray obtained to rule out pulmonary tuberculosis • TC/TONY has agreements with the County Health Department for consultation and referral for members with diagnosed or suspected tuberculosis. TC/TONY Network Providers must notify TC/TONY Case Management with the names of diagnosed patients for referral and coordination and any necessary authorizations. • Treatment guidelines can be found at: http://www.cdc.gov/tb/publications/guidelines/default.htm TC/TONY Participating providers must engage infection control procedures to isolate suspected and known patients with tuberculosis in order to minimize the transmission of disease. The suspected patient should not wait in general waiting areas. The provider will need to assure appropriate room ventilation for the performance of procedures. The provider must demonstrate that support staff is educated on the appropriate infection control procedures including the use of personal respiratory masks. • • The primary care provider is responsible to promptly report all suspected and positive TB cases to the County Health Department. The County Health Department will assist providers on infection control procedures. Directly Observed Therapy for Tuberculosis Disease (TB/DOT) • TB/DOT is the direct observation of oral ingestion of TB medications to assure patient compliance with the prescribed medication regimen • TB/DOT is the standard of care for all patients with active TB • TC/TONY Case Management is responsible for the coordination, communication and cooperation of the Clinical Management of the TB/DOT Provider but where applicable, services may be billed directly to eMedNY by an SDOH approved Medicaid Fee-for-Service TB/DOT provider • The service may be provided in the community at the local health department (LDH), in the patient’s home) or on an inpatient basis. • Outpatient TB/DOT involves the observation of dispensing of medication, assessing any adverse reactions to the medications and case follow up. Revised January 2015 Section 18 Page 2 TOTAL CARE, A TODAY’S OPTIONS OF NEW YORK HEALTH PLAN PROVIDER MANUAL Section 18 • Inpatient long term treatment may be indicated where the LHD has determined the patient has a poor treatment response, has medical complications, remains infectious with no other appropriate residential placement available, or other intensive residential placement is not possible. • Total Care, a Today’s Options of New York Health Plan, is contracted with four local Department of Health agencies that provide this service. The contracted agencies are listed below: 1. Onondaga County Department of Health 421 Montgomery Street Syracuse, New York 13202 315-435-3252 2. Tompkins County Department of Health 401 Harris B. Dates Drive Ithaca, NY 14850 607-274-6674 3. Cortland County Department of Health 60 Central Avenue Cortland, NY 13045 607-753-5209 4. Oswego County Department of Health 70 Bunner Street Oswego, NY 13126 315-349-3545 • Clinical protocols followed by the LDH agencies above are established by the Centers for Disease Control and can be found at: http://www.cdc.gov/tb/publications/guidelines/default.htm Revised January 2015 Section 18 Page 3