AACR Poster
advertisement

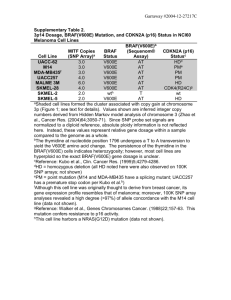
Kinase activity profiles distinguish papillary thyroid cancers with AACR 2015# 4322 and without BRAF V600E mutations 1 Hilhorst , 1 Berg , 2 Wezel , 3 Kievits , Riet Adriënne van den Tom van Tim Rik de Rob , Hans 1PamGene International BV, 's-Hertogenbosch, Netherlands; 2Leiden University Medical Center , Leiden, Netherlands, 3Vitromics Holding BV, 's-Hertogenbosch, Netherlands Background 1 Wijn , 1 , Ruijtenbeek Wim 2 Corver 2 Morreau . Results Serine/threonine kinase activity in malignant thyroid tumors, notably ATC’s and PTC’s, is in many instances higher than in benign tumors (Fig. 2). The V600E mutation results in many cases in increased activity. To predict whether a sample is benign or malignant, a model was built with Partial Least Squares Discriminant Analysis (PLS-DA) with validation by Leave One Out Cross Validation (Fig. 3). We investigated whether inhibition profiles with the inhibitors dabrafenib, regorafenib or sorafenib could discriminate BRAF WT and V600E PTC thyroid tumors (Fig. 4). 11 0 V600E WT malignant VE PTC Basal kinase activity profiles of PTC’s were not able to distinguish BRAF V600E and BRAF WT samples due to biological heterogeneity. Tumor subgroup benign Tumor properties Muation status BRAF V600E 0 Not determined 10 Tumor subgroup ATC BRAF WT BRAF V600E FTC BRAF WT PTC BRAF WT BRAF V600E * one sample: ATC from PTC Malignant 35 WT FTC WT 7 2 10 7* 9* 4x Mean Mean of row 0.25x Mean PamChip® Cell-Based Kinase Assay Kinase activity profiles without inhibitor. B C Tumor lysates D Kinase activity Profiles C1 C2 C Inhibition profile low 1 0.5 Inhibition profiles with sorafenib BRAF V600E PKA signaling BRAF WT Cytoskeleton reorganisation 1 0.5 Ratio inhibited/non inhibited 2 Peptides 1 Ratio inhibited/non inhibited Ratio inhibited/non inhibited C2 signal intensity Inhibition by drug 2 log Dynamic incubation drug Drug added ex vivo BRAF WT 2 C1 high 20-50 µl D Serine/threonine kinase activity profiling appears to be able to differentiate benign and malignant thyroid tumors. Ex vivo spiking in of kinase inhibitors shows the ability to differentiate BRAF V600E mutants only for dabrafenib. P array 96 PamChip® arrays Inhibition profiles with regorafenib BRAF V600E Peptides Lysate, no drug Phosphosite in peptide E signal intensity 18 BRAF WT Ratio inhibited/non inhibited BRAF V600E Kinase inhibition profiles of PTC’s with dabrafenib, an inhibitor directed against BRAF V600E, overcame the interpatient heterogeneity. 34/144 peptides were significantly different (p<0.05) between the BRAF V600E and BRAF WT groups. The RAF inhibitors sorafenib and regorafenib showed very similar inhibition profiles that did not discriminate BRAF V600E from BRAF WT samples. Conclusions cAMP signaling Inhibition profiles with dabrafenib Peptides BRAF WT Peptides BRAF V600E B 2 log A 0.0 A Fig. 3. Prediction scores for benign/malignant for 57 thyroid tumors. Prediction scores are coloured by clinical assessment and by tumor subgroup. Green stars indicate a BRAF mutation. Fig. 2. Normalised kinase activity profiles of 57 lysates of thyroid tumors. Signals are expressed with respect to the mean per peptide (row). ND: BRAF mutation status not determined. VE: BRAF V600E. Tissue cryosections from fresh frozen thyroid tumors were lysed. Tumor specimens were analyzed for BRAF mutations. Serine/threonine kinase (STK) activity profiles of the lysates were generated on PamChip® peptide microarrays, comprising peptide sequences from known human phosphorylation sites. The ex vivo effect of BRAF inhibitors sorafenib, regorafenib and dabrafenib on kinase activity profiles of 14 PTC’s was determined as well. Data were analysed with Bionavigator software. A classifier built on the STK kinase activity profiles of 57 thyroid cancer samples was able to classify malignant and benign tumors with a limited error rate. Leave One Out Cross Validation classified 17/22 of benign and 26/35 of malignant samples correctly (PPV = 0.65, NPV = 0.84). Misclassification was not associated with tumor subgroup or BRAF mutation status. BRAFV600E malignant Benign 22 ND ATC WT Clinical assessment Prediction score Table 1. Subgroup and mutation status of 57 samples. Malignant benign Benign Peptides Most differentiated non medullary thyroid cancers (DTC) are curatively treated by surgery and radio-active iodine ablation therapy. A subset of patients shows recurrence due to a loss of iodine transport. Two main subgroups of recurrent DTC are seen: papillary thyroid cancers (PTC) with somatic BRAF mutations (V600E ) and oncocytic follicular cancer. Recurrent DTC are clinically treated by multi-kinase inhibitors such as sorafenib, with a low affinity for BRAF V600E. Vemurafenib and dabrafenib were specifically designed against this mutant. The aim of this study was twofold: - Can benign and malignant DTC be classified based on kinase activity profiles? - Can dabrafenib (or sorafenib or regorafenib) inhibition profiles differentiate BRAF WT and mutant PTC tumors? Discussion 2 Potentially, an industrial prediction platform can be envisioned for testing of novel drugs in tumor tissue. Whether individual patient responses against registered kinase inhibitors can be predicted must be investigated. 1 0.5 0.1 Fig. 1. Kinase activity profiling of lysates of tumor tissue on serine/threonine PamChip® peptide microarrays (A) without and with inhibitor (B, C). Signal intensities for samples were converted to activity profiles (D) and to inhibition profiles (E) by calculation of the ratio of signals in the presence and absence of inhibitor. 1 implies no change in activity, 0.1 implies 10 % remaining activity. Fig. 4. Kinase activity profiles of lysates of 14 PTC thyroid tumors without inhibitor (A) and inhibition profiles obtained by addition of 10 µM dabrafenib (B), 50 µM regorafenib (C) or 10 µM sorafenib (D) in the assay. The inhibition profiles show ratios compared to the incubations without inhibitor. Peptides are presented in the same order in heatmaps A-D. Fig. 5. cAMP and PKA signalling are differentially affected by dabrafenib in BRAF V600E and BRAF WT samples. Info: rhilhorst@pamgene.com