Nutrition in Surgical Patients Ronald Merrell, MD Chairman of Surgery

Nutrition in Surgical Patients
Ronald Merrell, MD
Chairman of Surgery
Virginia Commonwealth University
•
Carbohydrate
•
Lipid
•
Protein
•
Trace elements
•
Vitamins
What?
Who?
•
Malnourished (>10% lean body mass)
•
Incapable of eating (>10 days)
Why?
•
Risks of malnutrition including infection, poor healing and higher mortality
•
Malnutrition is exacerbated by physiological stress
When?
•
Preoperative?
•
Early?
•
Late?
•
---after initial resuscitation following injury or surgery
•
Parenteral
•
Enteral
•
Total
•
Partial
How?
Issues
•
Metabolic response to injury
•
Cytokines, inflammation, hormones
•
Biology of substrates
•
Enteral vs. Parenteral
“Ashen faces, a thready pulse and cold clammy extremities…”
The Ebb Phase
Cuthbertson, Quart. J.
Med.25:233,1932
The Ebb Phase
• Hypometabolic
•
Hypothermic
• Hypoinsulinemic
•
Hypoperfusion
• Hypercortisolism
•
Hyperglucagonemia
• Hyperglycemia
•
Hypercatecholemia
“The patient warms up,cardiac output increases and the surgical team relaxes…”
The Flow Phase
Cuthbertson. Lancet 1:233, 1942
The Flow Phase
• Hypermetabolic
•
Hyperthermic
• Catabolic
• Hyperinsulinism
•
Hypercortisolism
• Hyperglucagonemia
•
High cardiac output
Nutritional Assessment
•
Body weight
•
Body mass index
• creatinine height index
•
Serum proteins:albumin, prealbumin, transferrin
•
Immune competence: lymphocytes, DH
•
Nitrogen balance
Caloric Requirement
•
Formula
•
Indirect calorimetry
•
PRN for nitrogen balance
•
Approximation
Nutritional Requirements
•
25 cal/kg/day
• carbohydrate ~70%
•
Lipid 15-30%
•
Protein 1.5-2.0g/kg/day. Not for calories
•
Additional 50% to 100% for stress as in
ICU patients
Nutritional Goals
•
Nitrogen balance
•
Preserve or restore visceral protein
•
Reduce morbidity
•
Reduce mortality
•
Reduce hospital stay
Early Enteral Feeding: a metaanalysis
•
Eight prospective randomized trials with trauma and high risk surgical patients(118 enteral, 112 parenteral)
•
Septic complications:enteral 18%, parenteral 35%
•
Moore. Ann. Surg. 216:172,1992
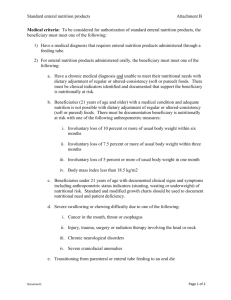
Parenteral requirements
•
Dilution in right heart return because of hyperosmolarity…….Central Venous Line
•
Delivery of simple carbohydrate
(20%glucose)
•
Lipid emulsion
•
Amino acids
Enteral Requirements
•
Delivery into the GI tract by tube with minimum risk of aspiration or patient effort
•
Delivery of nutrients with minimal need for digestion
•
Control of rate to prevent osmotic diarrhea
Advantages of enteral nutrition
•
Easier
•
GI bacterial translocation
•
Cheaper
•
Fewer specific complications
Nutrients with specific putative contributions
•
Branch chain amino acids
•
Glutamine
•
Arginine
•
Nucleotides
•
Omega-3 fatty acids
Immune Enhancing Diet
•
Arginine, nucleotide, fish oil
•
Shorter stay, fewer infections
•
Bower Critical Care Medicine. 23:436,
1995
Parenteral Nutrition
Immunosuppressive
IF...
•
Poorly administered
•
Hyperglycemia
•
No nucleotides
•
No arginine
•
No taurine
•
Excessive fats
Overfeeding with parenteral diets
•
Carbohydrate: hyperglycemia, hypercarbia, fatty liver
•
Lipids: hypertriglyceridemia, hypoxia, infection
•
Protein: azotemia
Conclusions
•
Nutrition is a powerful determinate of patient outcome
•
The proper provision of nutrition is a component of basic patient care
•
Nutrition is a precise and potentially very hazardous form of intervention