90–90 versus parallel plating of distal humeral
advertisement

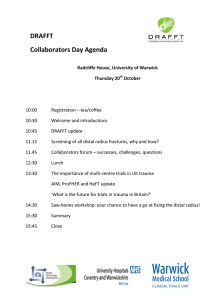
expert zone Clinical topic 28 What is the evidence? Thierry G Guitton, Jesse B Jupiter 90–90 versus parallel plating of distal humeral fractures While relatively uncommon injuries, intraarticular fractures of the distal humerus continue to provide operative challenges to the surgeon in order that such complications as nonunion, malunion, decreased motion, and instability, are minimized. One way to accomplish this is to enhance the stability of the plate and screw fixation construct. The long established technique of orientation of two plates relatively perpendicular to each other (90–90) has recently been challenged on both biomechanical and clinical perspectives by the concept of parallel plate application. This fixation strategy focuses on maximizing stability between the distal fragments and the shaft of the humerus at the metaphyseal level. According to O’Driscoll this can be achieved by following a set of eight technical objectives: 1. Every screw should pass through a plate. 2. Each screw should engage a fragment on the opposite side that is also fixed to a plate. 3. As many screws as possible should be placed in the distal fragments. 4. Each screw should be as long as possible. 5. Each screw should engage as many articular fragments as possible. 6. The screws should lock together by interdigitation within the distal fragment, thereby creating a fixed-angle architecture that provides stability to the entire distal humerus. 2 | 09 7. Plates should be applied such that compression is achieved at the supracondylar level for both columns. 8. Plates used must be strong enough and stiff enough to resist breaking or bending before union occurs at the supracondylar level (Fig 1a–h). This review will investigate the evidence for both plating techniques for the treatment for complex distal articular humeral fractures. Materials and methods The studies considered for possible inclusion in the current review were identified in a search (MeSH), in MEDLINE (National Library of Medicine, Bethesda, MD), EMBASE (Elsevier, Amsterdam, the Netherlands) and the Cochrane review for randomized controlled trials (Wiley InterScience, Hoboken, NJ) for the word distal humerus fractures and the key words plating, perpendicular or parallel. The bibliographic citations for each of the articles ultimately selected were also examined to identify any other acceptable studies that were not captured by the database searches. Furthermore, a grey literature search was conducted in an effort to identify all available literature that may not have been identified by the database searches. Selection of core articles was restricted to original research in the English language with human subject that examined the different plating orientations of distal humeral fractures. Randomized controlled and retrospective studies were included while animal studies, review articles, commentary, editorial, or letters were excluded. expert zone 29 Fig 1a–h The technique an important facts developed by the Mayo Clicinc “school” (O’Ddriscoll). (a) Every screw in the distal fragment should pass through a plate. (b) Every screw in the distal fragment should be anchored in a fragment on the opposite side that is fixed by a plate. (c) As many screws as possible should be placed in the distal fragment. (d) Every screw in the distal fragment should be as long as possible. (e) Every screw in the distal fragment should engage as many articular fragment as possible. (f) The screws in the distal fragments should lock together by interdigitation, creating a fixed angle structure, thereby completing the arch or closing the loop. (g) The plate should be applied with compression at the supracondylar level. (h) The plate should be strong and stiff enough to resist bending or breakage. 1a 1b 1c 1d 1e 1g 1f 1h Results Clinical evidence: While there are numerous reports on internal fixation of distal humeral fractures, they are for the most part retrospective studies using a single plating technique. Unfortunately no prospective studies specifically comparing both methods, exist up to the present time. While the placement of plates nearly perpendicular to each other was promoted early on by the AO group the biomechanical study of Helfet and Hotchkiss added credibility to this technique (Fig 2a–e and 3). A number of subsequent clinical studies revealed nearly 75–85% good to excellent results with 90–90 plating. A long term follow-up study at a mean of 19 years after injury by Doornberg concluded that the long term results of open reduction and internal fixation of 19 Type C fractures of the distal part of the humerus treated with perpendicular orientation are similar to those reported in the short term. They suggested that the results are durable over time. The clinical experience with parallel plating has not been as extensive or with longer follow up, however current reports reveal no evidence of failure of the fixation and comparable clinical results as with 90-90 plating. Biomechanical evidence: Which technique is more stable? Several biomechanical studies compared parallel plating with perpendicular 90–90 orientation, concluding that parallel plating with additional use of bolts was favorable to perpendicular plating. Their observations were supported by Arnander who concluded that, parallel plating was superior to the perpendicu2 | 09 expert zone Clinical topic 30 2a 2b lar orientation although they expressed concern that placing a plate lateral can be technically difficult. Jacobson concluded that perpendicular plate orientation was strongest in the sagittal plane while Korner stated that perpendicular plating had increased stiffness to torsional and anteroposterior bending forces. Schwartz found similar stabilization among both plate orientations. How do the results of stability testing relate to physiologic loading? Wong tested both fixation methods and concluded that both methods may be above the threshold necessary for early motion and predictable fracture healing, rendering the marginal strength of parallel plating clinically unimportant. Kimball found that the risk of delayed union or nonunion increased by the extensive subperiosteal elevation with parallel plating orientation. Schutzer tested the perpendicular plate orientation with different plate types and concluded that implant choice was not critical in good bone quality. Korner showed that locking plates have a substantial advantage in poor bone quality or if significant metaphysical comminution is present. Otherwise they concluded that there was no difference in plate type and that plate position is critical. Discussion 2c 2d Although some biomechanical evidence may favor parallel orientation, the real take home message may be that both orientations are strong enough to be able to mobilize the elbow after fracture fixation. Additionally it should be noted that biomechanical evidence raises as many questions as solutions. Some biomechanical studies fail to actually resemble the true clinical setting, and often have low samples sizes and a lack of statistical power. From a clinical perspective, there are not sufficient data to make valid comparisons. Several different outcome measures are used; fractures types vary and non-homogenous patient selections have been reported. Long term follow-up for parallel plating and clinical trials are needed to compare different plate orientation. Until then both fractures orientations seem adequate enough to treat complex distal articular humeral fractures and the choice should be made by fracture specifications and surgeon’s preference. 2e 3 Figure 2a–e The AO technique: Reconstructing a multifragmentary distal humeral fracture. Figure 3 Fixation with two anatomically precontoured perpendicular plates. 2 | 09 expert zone 31 Suggested reading Ackerman G, Jupiter JB (1988) Non-union of fractures of the distal end of the humerus. J Bone Joint Surg Am; 70(1):75–83. Caja VL, Moroni A, Vendemia V, et al (1994) Surgical treatment of bicondylar fractures of the distal humerus. Injury; 25(7):433–438. Thierry G Guitton Harvard Medical School, Orthopedic Hand and Upper Extremity Service Boston, United States tguitton@partners.org Henley MB, Bone LB, Parker B (1987) Operative management of intraarticular fractures of the distal humerus. J Orthop Trauma; (1):24–35. Jupiter JB, Neff U, Holzach P, et al (1985) Intercondylar fractures of the humerus. An operative approach. J Bone Joint Surg Am; 67(2):226–239. Ring D, Jupiter JB (2000) Fractures of the distal humerus. Orthop Clin North Am; 31(1):103–113. Helfet DL, Hotchkiss RN (1990) Internal fixation of the distal humerus: a biomechanical comparison of methods. J Orthop Trauma; 4(3):260–264. Jesse B Jupiter Harvard Medical School, Orthopedic Hand and Upper Extremity Service Boston, United States jjupiter1@partners.org Self J, Viegas SF, Buford WL Jr, et al (1995) A comparison of doubleplate fixation methods for complex distal humerus fractures. J Shoulder Elbow Surg; 4(1 Pt 1):10–16. O’Driscoll SW (2005) Optimizing stability in distal humeral fracture fixation. J Shoulder Elbow Surg; 4(1 Suppl S):186S–194S. Sanchez-Sotelo J, Torchia ME, O’Driscoll SW (2007) Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique. J Bone Joint Surg Am; 89(5):961–969. Sanchez-Sotelo J, Torchia ME, O’Driscoll SW (2008) Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique. Surgical technique. J Bone Joint Surg Am; 90 Suppl 2 Pt 1:31–46. Doornberg JN, van Duijn PJ, Linzel D, et al (2007) Surgical treatment of intra-articular fractures of the distal part of the humerus. Functional outcome after twelve to thirty years. (2007) J Bone Joint Surg Am; 89(7):1524–1532. McKee MD, Wilson TL, Winston L, et al (2000) Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach. J Bone Joint Surg Am; 82-A(12):1701–1707. Wong AS, Baratz ME (2009) Elbow fractures: distal humerus. J Hand Surg [Am]; 34(1):176–190. Arnander MW, Reeves A, MacLeod IA, et al (2008) A biomechanical comparison of plate configuration in distal humerus fractures. J Orthop Trauma; 22(5):332–336. Jacobson SR, Glisson RR, Urbaniak JR (1997) Comparison of distal humerus fracture fixation: a biomechanical study. J South Orthop Assoc; 6(4):241–249. Korner J, Diederichs G, Arzdorf M, et al (2004) A biomechanical evaluation of methods of distal humerus fracture fixation using locking compression plates versus conventional reconstruction plates. J Orthop Trauma; 18(5):286–293. Schwartz A, Oka R, Odell T, et al (2006) Biomechanical comparison of two different periarticular plating systems for stabilization of complex distal humerus fractures. Clin Biomech (Bristol, Avon); 21(9):950–955. Kimball JP, Glowczewskie F, Wright TW (2007) Intraosseous blood supply to the distal humerus. J Hand Surg [Am]; 32(5):642–646. Schuster I, Korner J, Arzdorf M, et al (2008) Mechanical comparison in cadaver specimens of three different 90-degree double-plate osteosyntheses for simulated C2-type distal humerus fractures with varying bone densities. J Orthop Trauma; 22(2):113–120. Korner J, Lill H, Muller LP, et al (2003) The LCP-concept in the operative treatment of distal humerus fractures—biological, biomechanical and surgical aspects. Injury; 34 Suppl 2:B20–30. 2 | 09