B05679 Rev.0/03-14
Bard® LifeStent® XL Stent and Delivery System
Vascular Application
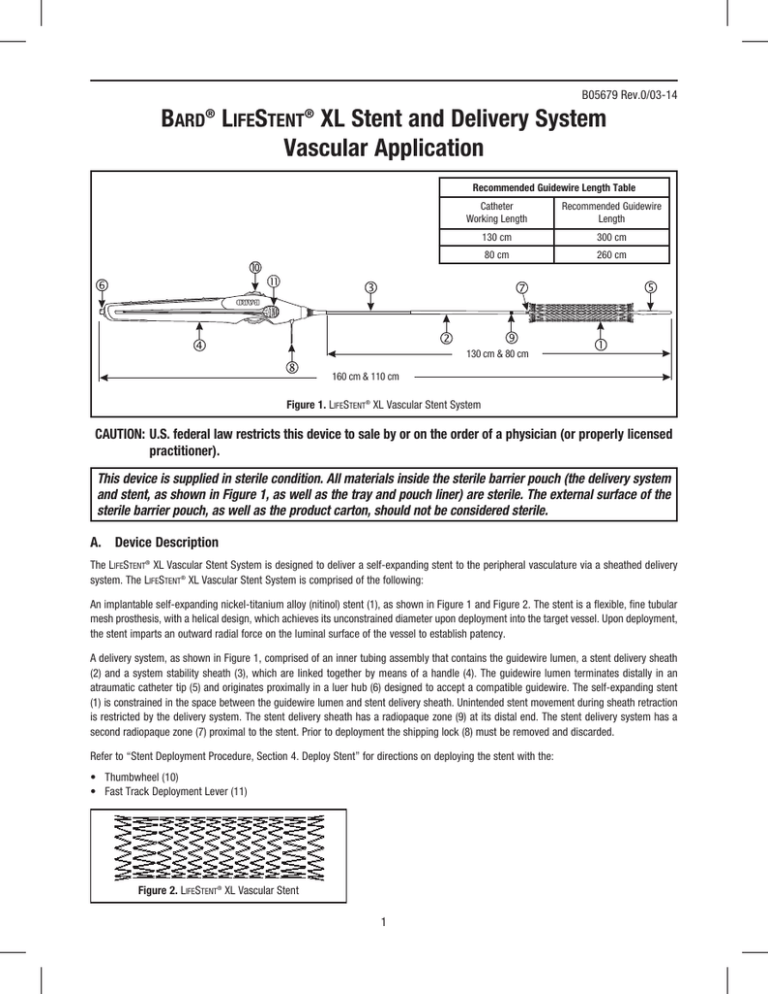
Recommended Guidewire Length Table
Catheter
Working Length
Recommended Guidewire
Length
130 cm
300 cm
80 cm
260 cm
130 cm & 80 cm
160 cm & 110 cm
Figure 1. LifeStent® XL Vascular Stent System
CAUTION:U.S. federal law restricts this device to sale by or on the order of a physician (or properly licensed
practitioner).
This device is supplied in sterile condition. All materials inside the sterile barrier pouch (the delivery system
and stent, as shown in Figure 1, as well as the tray and pouch liner) are sterile. The external surface of the
sterile barrier pouch, as well as the product carton, should not be considered sterile.
A. Device Description
The LifeStent® XL Vascular Stent System is designed to deliver a self-expanding stent to the peripheral vasculature via a sheathed delivery
system. The LifeStent® XL Vascular Stent System is comprised of the following:
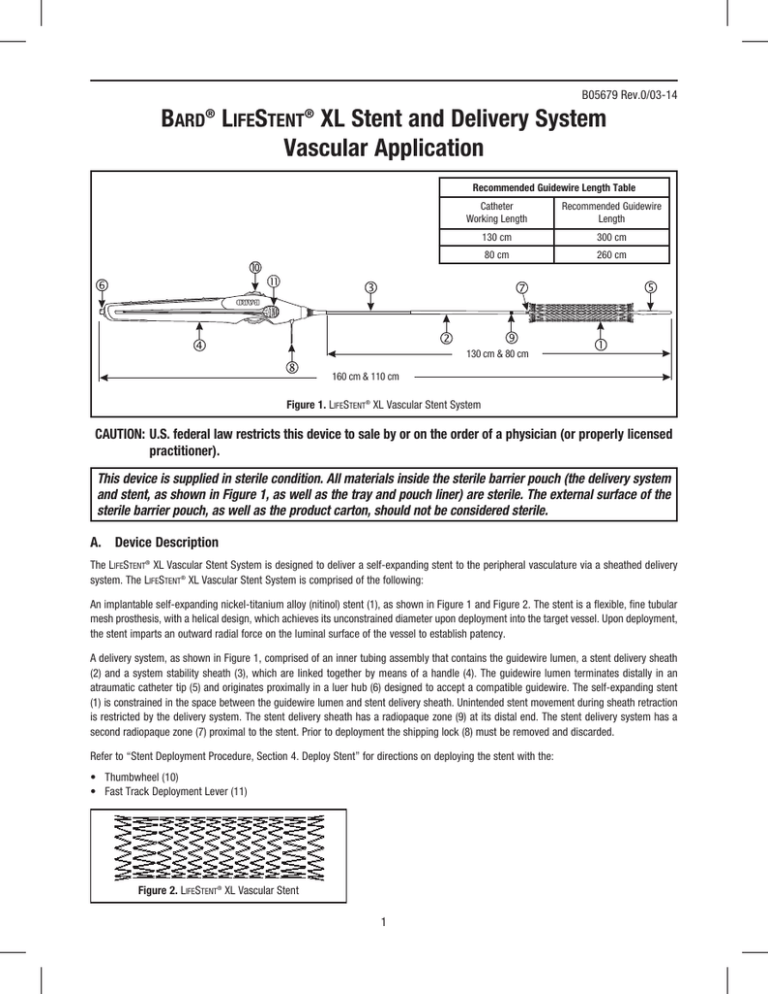
An implantable self-expanding nickel-titanium alloy (nitinol) stent (1), as shown in Figure 1 and Figure 2. The stent is a flexible, fine tubular
mesh prosthesis, with a helical design, which achieves its unconstrained diameter upon deployment into the target vessel. Upon deployment,
the stent imparts an outward radial force on the luminal surface of the vessel to establish patency.
A delivery system, as shown in Figure 1, comprised of an inner tubing assembly that contains the guidewire lumen, a stent delivery sheath
(2) and a system stability sheath (3), which are linked together by means of a handle (4). The guidewire lumen terminates distally in an
atraumatic catheter tip (5) and originates proximally in a luer hub (6) designed to accept a compatible guidewire. The self-expanding stent
(1) is constrained in the space between the guidewire lumen and stent delivery sheath. Unintended stent movement during sheath retraction
is restricted by the delivery system. The stent delivery sheath has a radiopaque zone (9) at its distal end. The stent delivery system has a
second radiopaque zone (7) proximal to the stent. Prior to deployment the shipping lock (8) must be removed and discarded.
Refer to “Stent Deployment Procedure, Section 4. Deploy Stent” for directions on deploying the stent with the:
• Thumbwheel (10)
• Fast Track Deployment Lever (11)
Figure 2. LifeStent® XL Vascular Stent
1
B. Indication for Use
The LifeStent® XL Vascular Stent System is intended to improve luminal diameter in the treatment of symptomatic de-novo or restenotic
lesions up to 240 mm in length in the native superficial femoral artery (SFA) and proximal popliteal artery with reference vessel diameters
ranging from 4.0-6.5 mm.
C. Contraindications
The LifeStent® XL Vascular Stent System is contraindicated for use in:
• Patients with a known hypersensitivity to nitinol (nickel, titanium), and tantalum.
• Patients who cannot receive recommended anti-platelet and/or anti-coagulation therapy.
• Patients who are judged to have a lesion that prevents complete inflation of an angioplasty balloon or proper placement of the stent or
stent delivery system.
D. Warnings
• DO NOT use if the temperature exposure indicator (i.e., square label found on the pouch) is black as the unconstrained stent diameter
may have been compromised. The temperature exposure indicator label should be grey and must be clearly visible on the pouch.
• The LifeStent® XL Vascular Stent System is supplied sterile and is intended for single use only. DO NOT resterilize and/or reuse the device.
• DO NOT use if pouch is opened or damaged.
• DO NOT use the stent after the end of the month indicated by the “Use By” date specified on the package.
• Persons with allergic reactions to nickel titanium (nitinol) alloy may suffer an allergic response to this implant.
• DO NOT use with Ethiodol™ or Lipiodol contrast media.
• DO NOT expose the delivery system to organic solvents (e.g., alcohol).
• The stent is not designed for repositioning or recapturing.
• Stenting across a major branch could cause difficulties during future diagnostic or therapeutic procedures.
• If multiple stents are placed in an overlapping fashion, they should be of similar composition (i.e., nitinol). • The long-term outcomes following repeat dilatation of endothelialized stents are unknown.
E. Precautions
•
•
•
•
•
•
•
•
•
The device is intended for use by physicians who have received appropriate training.
The delivery system is not designed for use with power injection systems.
Recrossing a partially or fully deployed stent with adjunct devices must be performed with caution.
Prior to stent deployment, remove slack from the delivery system catheter outside the patient.
If excessive force is felt during stent deployment, do not force the delivery system. Remove the delivery system and replace with a new
unit.
Store in a cool, dark, dry place.
Do not attempt to break, damage, or disrupt the stent after placement.
Cases of fracture have been reported in clinical use of the LifeStent® Vascular Stent. Cases of stent fracture occurred in lesions that were
moderate to severely calcified, proximal or distal to an area of stent overlap and in cases where stents experienced >10% elongation at
deployment. Therefore, care should be taken when deploying the stent as manipulation of the delivery system may, in rare instances, lead
to stent elongation and subsequent stent fracture. The long-term clinical implications of these stent fractures have not yet been
established (see section J).
The safety and effectiveness of this device for use in treatment of instent restenosis has not been established.
F. Magnetic Resonance Imaging (MRI) Compatibility
Conditions for All Stents
Non-clinical testing has demonstrated that the LifeStent® Vascular Stent is MR Conditional for vascular placement in lesions up to a length
of 240 mm. It can be scanned safely under the following conditions:
• Static magnetic field of 1.5-Tesla or 3-Tesla.
• Spatial gradient field of 2500 Gauss/cm or less.
• Maximum whole-body-averaged specific absorption rate (SAR) of 1 W/kg for 15 minutes of scanning. For landmarks superior of the
umbilicus, a whole body SAR up to 2 W/kg may be applied.
• In a configuration where the patients legs are not in contact with each other.
3.0 Tesla Temperature Rise
In an analysis based on non-clinical testing and computer modeling of a patient, the 60 mm length LifeStent® Stent was determined to
produce a potential worst-case temperature rise of 5.5 °C for a whole body averaged specific absorption rate (SAR) of 1 W/kg for 15 minutes
of MR scanning in a 3.0 Tesla, whole body MR system for a landmark in the legs. Temperature rises can be twice as high at a whole
body averaged SAR of 2 W/kg for landmarks below the umbilicus. Temperature rises were reduced for landmarks above the umbilicus.
2
Temperature rises of stents were measured according to ASTM F2182-11a in a nonclinical configuration using a GE Signa HDX Whole Body
active shield MR scanner using software version 14/LX/MR and a phantom designed to simulate human tissue. The phantom average SAR
calculated using calorimetry was 2.7 W/kg. When the stent was placed in a worst-case location within the phantom, the maximal temperature
rise was 2.4 °C when the local SAR was scaled to 2 W/kg.
1.5 Tesla Temperature Rise
In an analysis based on non-clinical testing and computer modeling of a patient, the 100 mm length LifeStent® Stent was determined to
produce a potential worst-case temperature rise of 6.0 °C for a whole body averaged specific absorption rate (SAR) of 1 W/kg for 15 minutes
of MR scanning in a 1.5 Tesla, whole body MR system for a landmark in the legs. Temperature rises can be twice as high at a whole
body averaged SAR of 2 W/kg for landmarks below the umbilicus. Temperature rises were reduced for landmarks above the umbilicus.
Temperature rises of stents were measured according to ASTM F2182-11a in a nonclinical configuration using a GE Signa whole body coil
and a phantom designed to simulate human tissue. The phantom average SAR calculated using calorimetry was 2.3 W/kg. When the stent
was placed in a worst-case location within the phantom, the maximal temperature rise was 3.2 °C when the local SAR was scaled to 2 W/kg.
Image Artifact
MR image quality may be compromised if the area of interest is in the exact same area or relatively close to the position of the stent. Artifact
tests were performed according to ASTM F2182-11a. Maximum artifact extended 3 mm beyond the stent for the spin echo sequence and
10 mm for the gradient echo sequence. The lumen was obscured.
Additional Information
The LifeStent® Vascular Stent has not been evaluated in MRI systems other than 1.5 or 3.0 Tesla. The heating effect in the MRI environment
for fractured stents is not known. The presence of other implants or the health state of the patient may require reduction of the MRI limits
listed above.
G. Overview of Clinical Studies
Three independent clinical studies and a retrospective analysis support the safety and effectiveness of the LifeStent® Vascular Stent Systems.
The RESILIENT pivotal trial was a prospective, randomized, multi-center study designed to compare the safety and effectiveness of the
LifeStent® Vascular Stent System to PTA in the treatment of symptomatic vascular disease of the superficial femoral artery (SFA) and proximal
popliteal artery. 206 subjects were randomized in a 2:1 fashion between the test and control arm at 22 U.S. and 2 European centers. In total,
134 subjects were randomized to the test arm (treatment with the LifeStent® Vascular Stent System) and 72 subjects were randomized to the
control arm (treatment with stand alone balloon angioplasty). The primary safety endpoint was 30-day mortality and the primary effectiveness
endpoint was the 6-month re-intervention rate. 30-day data is available for 96.1% (198/206) of the randomized subjects and 6-month
effectiveness data is available for 89.8% (184/205) of the randomized subjects. All subjects were followed for a total of three years following
the index procedure.
The E-TAGIUSS supporting trial was a prospective, non-randomized, multi-center study designed to assess the acute deliverability of the
LifeStent® and LifeStent® XL Vascular Stent Systems. 37 subjects were treated in 7 European centers. The primary safety endpoint was 30day mortality and the primary effectiveness endpoint was the assessment of stent length following deployment. 30-day mortality data is
available for 91.9% (34/37) of the treated subjects and deployed stent length data is available for 46 deployed stents. All subjects were
followed for 30 days following the index procedure.
A retrospective analysis of the performance of the LifeStent® Vascular Stent Systems for long segment lesions was also undertaken.
285 subjects were included in the analysis in which 46 lesions had lengths ≥ 160 mm. The primary endpoints of this analysis were
acute safety (freedom from death, amputation or TVR) at 30-days, long-term safety (freedom from death or amputation) at 12 months
in patients with total lesion lengths ≥ 160 mm and effectiveness (freedom from TVR) at 12 months in lesions of length 50 mm, 100 mm, 160 mm,
200 mm and 240 mm.
Furthermore, the REALITY study, a single-arm, non-randomized, prospective, single-center study was conducted to demonstrate the safety
and effectiveness of the Bard® LifeStent® Vascular Stent Systems with a 5 mm diameter size offering. The primary objective of this study
was to assess the acute effectiveness of the Bard® LifeStent® Vascular Stent Systems. Primary effectiveness was defined as successful
deployment and placement accuracy based upon a rating scale completed by the investigators at time of index procedure. Primary safety
was defined as freedom from occurrence of death, amputation and TVR/TLR at 30 days post-index procedure.
H. Adverse Events
a. Observed Adverse Events
The following adverse events were documented during the course of the RESILIENT trial (N=226).
3
RESILIENT Trial Adverse Event Summary
RESILIENT Randomized
Event
LifeStent® (N=134)
% (N pts) [N events]
PTA (N=72)
% (N pts) [N events]
RESILIENT Feasibility
LifeStent® (N=20)
% (N pts) [N events]
In-Hospital Events
Major Adverse Events
Death
Myocardial Infarction
Target Limb Loss / Amputation
TVR
TLR
Non-TLR
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
5.0 (1/20) [1]
0 (0/134) [0]
41.7 (30/72) [31]
0 (0/134) [0]
41.7 (30/72) [30]
0 (0/20) [0]
0 (0/134) [0]
1.4 (1/72) [1]
5.0 (1/20) [1]
Stroke/CVA
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Distal Embolization
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
5.0 (1/20) [1]
Access Site Bleeding / Hematoma
0.7 (1/134) [1]
0 (0/72) [0]
Blood Loss requiring Transfusion
1.5 (2/134) [2]
1.4 (1/72) [1]
0 (0/20) [0]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Vessel Perforation
Vessel Aneurysm
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Vessel Pseudo-Aneurysm
0 (0/134) [0]
1.4 (1/72) [1]
5.0 (1/20) [1]
4.5 (6/134) [6]
20.8 (15/72) [16]
5.0 (1/20) [1]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Vessel Dissection
Thrombosis
Events at 30-Days
Major Adverse Events
Death
Myocardial Infarction
Target Limb Loss / Amputation
TVR
TLR
Non-TLR
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
5.0 (1/20) [1]
0.7 (1/134) [2]
41.7 (30/72) [31]
0.7 (1/134) [1]
41.7 (30/72) [30]
0 (0/20) [0]
0.7 (1/134) [1]
1.4 (1/72) [1]
5.0 (1/20) [1]
Stroke/CVA
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Distal Embolization
0 (0/134) [0]
1.4 (1/72) [1]
0 (0/20) [0]
5.0 (1/20) [1]
Access Site Bleeding / Hematoma
0.7 (1/134) [1]
1.4 (1/72) [1]
Blood Loss requiring Transfusion
1.5 (2/134) [2]
2.8 (2/72) [2]
0 (0/20) [0]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Vessel Perforation
Vessel Aneurysm
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Vessel Pseudo-Aneurysm
0 (0/134) [0]
1.4 (1/72) [1]
5.0 (1/20) [1]
4.5 (6/134) [6]
20.8 (15/72) [16]
5.0 (1/20) [1]
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
8.2 (11/134) [13]
6.9 (5/72) [6]
5.0 (1/20) [1]
3.7 (5/134) [5]
2.8 (2/72) [2]
0 (0/20) [0]
4.5 (6/134) [8]
1.4 (1/72) [1]
5.0 (1/20) [1]
Vessel Dissection
Thrombosis (24 Hrs - 30 Days Only)
Events at 12-Months
Major Adverse Events
Death
Myocardial Infarction
Target Limb Loss / Amputation
TVR
TLR
0 (0/134) [0]
4.2 (3/72) [3]
0 (0/20) [0]
16.4 (22/134) [28]
54.2 (39/72) [54]
15.0 (3/20) [3]
11.9 (16/134) [16]
54.2 (39/72) [46]
10.0 (2/20) [2]
Non-TLR
8.2 (11/134) [12]
8.3 (6/72) [8]
5.0 (1/20) [1]
Stroke/CVA
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Vessel Aneurysm
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Vessel Pseudo-Aneurysm
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
Late Thrombosis (>30 Days Only)
0 (0/134) [0]
0 (0/72) [0]
0 (0/20) [0]
4
RESILIENT Trial Adverse Event Summary
Event
RESILIENT Randomized
LifeStent® (N=134)
PTA (N=72)
% (N pts)
% (N pts)
[N events]
[N events]
RESILIENT Feasibility
LifeStent® (N=20)
% (N pts)
[N events]
Events at 24-Months Major Adverse Events
Death
Myocardial Infarction
Target Limb Loss / Amputation
TVR
TLR
Non-TLR
Stroke/CVA
Vessel Aneurysm
Vessel Pseudo-Aneurysm
Late Thrombosis (>30 Days Only)
13.4 (18/134) [23]
7.5 (10/134) [10]
6.0 (8/134) [11]
1.5 (2/134) [2]
25.4 (34/134) [48]
20.1 (27/134) [30]
12.7 (17/134) [18]
0.7 (1/134) [1]
0 (0/134) [0]
0 (0/134) [0]
0 (0/134) [0]
11.1 (8/72) [11]
5.6 (4/72) [4]
5.6 (4/72) [4]
4.2 (3/72) [3]
58.3 (42/72) [69]
56.9 (41/72) [53]
15.3 (11/72) [16]
0 (0/72) [0]
0 (0/72) [0]
0 (0/72) [0]
0 (0/72) [0]
5.0 (1/20) [1]
0 (0/20) [0]
5.0 (1/20) [1]
0 (0/20) [0]
15.0 (3/20) [4]
10.0 (2/20) [3]
5.0 (1/20) [1]
0 (0/20) [0]
0 (0/20) [0]
0 (0/20) [0]
0 (0/20) [0]
Latest Data Available
Major Adverse Events
Death
Myocardial Infarction
Target Limb Loss / Amputation
TVR
TLR
Non-TLR
Stroke/CVA
Vessel Aneurysm
Vessel Pseudo-Aneurysm
Late Thrombosis (>30 Days Only)
36-Months
15.7 (21/134) [27]
9.0 (12/134) [12]
7.5 (10/134) [13]
1.5 (2/134) [2]
28.4 (38/134) [57]
21.6 (29/134) [35]
15.7 (21/134) [22]
1.5 (2/134) [2]
0 (0/134) [0]
0 (0/134) [0]
0 (0/134) [0]
36-Months
11.1 (8/72) [12]
6.9 (5/72) [5]
5.6 (4/72) [4]
4.2 (3/72) [3]
58.3 (42/72) [71]
56.9 (41/72) [54]
16.7 (12/72) [17]
0 (0/72) [0]
0 (0/72) [0]
0 (0/72) [0]
0 (0/72) [0]
36-Months
10.0 (2/20) [2]
0 (0/20) [0]
10.0 (2/20) [2]
0 (0/20) [0]
15.0 (3/20) [4]
10.0 (2/20) [3]
5.0 (1/20) [1]
0 (0/20) [0]
0 (0/20) [0]
0 (0/20) [0]
0 (0/20) [0]
The following adverse events were documented during the course of the E-TAGIUSS trial (N=37).
E-TAGIUSS Trial Adverse Event Summary
Event
Major Adverse Event
Death
Myocardial Infarction
Target Limb Loss
Target Lesion Revascularization (TLR)
Stent Thrombosis
Distal Embolization
Access Site Bleeding
Non-Access Site Bleeding
Vessel Perforation
Vessel Aneurysm
Vessel Pseudo-Aneurysm
Vessel Dissection
In-Hospital
0% (0/37)
0% (0/37)
0% (0/37)
2.7% (1/37)
0% (0/37)
0% (0/37)
2.7% (1/37)
2.7% (1/37)
0% (0/37)
0% (0/37)
0% (0/37)
0% (0/37)
0% (0/37)
b. Potential Adverse Events
Potential adverse events that may occur include, but are not limited to, the following:
•
•
•
•
•
Allergic/anaphylactoid reaction
Amputation
Aneurysm
Angina/coronary ischemia
Arterial occlusion/thrombus, near the puncture site
5
30 Day
0% (0//37)
0% (0//37)
0% (0//37)
2.7% (1//37)
0% (0//37)
0% (0//37)
2.7% (1/37)
2.7% (1/37)
0% (0//37)
0% (0//37)
0% (0//37)
0% (0//37)
0% (0//37)
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Arterial occlusion/thrombus, remote from puncture site
Arterial occlusion/restenosis of the treated vessel
Arteriovenous fistula
Arrhythmia
By-pass Surgery
Death related to procedure
Death unrelated to procedure
Embolization, arterial
Embolization, stent
Fever
Hemorrhage/bleeding requiring a blood transfusion
Hematoma bleed, remote site
Hematoma bleed at needle, device path: nonvascular procedure
Hematoma bleed, puncture site: vascular procedure
Hypotension/hypertension
Incorrect positioning of the stent requiring further stenting or surgery
Intimal injury/dissection
Ischemia/infarction of tissue/organ
Liver failure
Local infection
Malposition (failure to deliver the stent to the intended site)
Open surgical repair
Pain
Pancreatitis
Pulmonary embolism/edema
Pneumothorax
Pseudoaneurysm
Renal failure
Respiratory arrest
Restenosis
Septicemia/bacteremia
Stent Fracture
Stent Migration
Stroke
Vasospasm
Venous occlusion/thrombosis, remote from puncture site
Venous occlusion/thrombosis, near the puncture site
I. Clinical Studies
a. RESILIENT FEASIBILITY STUDY
The RESILIENT study included a feasibility study to assess the safety of the LifeStent® Vascular Stent System. This feasibility study enrolled
20 subjects at six US investigative sites. Results from this study provided justification for initiation of a pivotal study to assess the safety and
effectiveness of the LifeStent® Vascular Stent System.
b. RESILIENT RANDOMIZED STUDY
Design
The RESILIENT trial was a prospective, multi-center, randomized clinical investigation to evaluate the superiority of the LifeStent® Vascular
Stent System compared to PTA in the treatment of symptomatic vascular disease of the SFA and/or proximal popliteal artery. A total of 206
subjects were treated at 22 US and 2 European investigative sites. Each site not participating in the feasibility study was required to perform
one roll-in case. A total of 20 roll-in cases were performed and 206 randomized cases were performed. Seventy-two (72) subjects were
randomized to the PTA arm and 134 subjects were randomized to treatment with the LifeStent® Vascular Stent System.
Subjects eligible to be enrolled in this study had stenotic or occluded lesions of the SFA and/or proximal popliteal artery and suffered from lifestyle
limiting claudication (Rutherford Category 1 – 3). Lesions could be either de novo or restenotic. Subjects with previously stented lesions or target
limb vascular by-pass were excluded. Reference vessel diameter (RVD) of the treated subjects was to be 4.0 – 6.5 mm in diameter and the
collective length of the treated segment was to be less than 150 mm. Subjects underwent angiographic analysis of the lesion prior to and
immediately following treatment. Subjects were followed at 30 days, 6 months and annually thereafter with follow-up planned out to 36-months.
Office visits were coupled with duplex ultrasound assessments of the treated segments. X-ray evaluation of the stented lesions was also performed.
The RESILIENT trial utilized a Frequentist approach with its statistical plan. The primary objectives were to show the following:
6
• that the probability of the occurrence of Target Lesion Revascularization (TLR) or Target Vessel Revascularization (TVR) at 6-months postprocedure for the subjects treated with LifeStent® NT (test arm) was significantly lower than (and therefore superior to) that for the subjects
treated with PTA-alone (control arm); and,
• that the death rates at 30-days post-procedure were not significantly different between the test arm and the control arm.
Continuous variables were compared using an independent samples t-test. Dichotomous variables were compared using Fisher‘s exact test.
Ordinal variables were compared using a Chi-square test. Time to event was compared using a log-rank test. Interval censored data were
analyzed using the Kaplan-Meier method as the primary analysis. A sensitivity analysis for interval censored data was performed using the
Weibull distribution. Effectiveness endpoints were analyzed as one-sided tests. Safety endpoints were analyzed as two-sided tests.
The results were evaluated using an Intent-to-Treat (ITT) analysis. In particular, control subjects requiring stent placement to salvage a failed
angioplasty remained in the cohort to which they were randomized.
Demographics
Characteristics of the subjects enrolled in the study including age, gender, medical history as well as lesion characteristics are provided in
the tables below.
RESILIENT Trial Subject Demographics
Variable
Age at Procedure (Yrs)
Gender, % (n/N)
Race, % (n/N)
Category
Test
Control
N, Mean ± SD
134, 68.4 ± 9.9
72, 66.1 ± 9.2
Female
29.1 (39/134)
33.3 (24/72)
Male
70.9 (95/134)
66.7 (48/72)
African American
9.0 (12/134)
9.7 (7/72)
Caucasian
89.6 (120/134)
84.7 (61/72)
1.5 (2/134)
5.6 (4/72)
Hypertension, % (n/N)
Other
83.6 (112/134)
94.4 (68/72)
Hypercholesterolemia, % (n/N)
79.9 (107/134)
76.4 (55/72)
Diabetes, % (n/N)
38.1 (51/134)
38.9 (28/72)
Smoking, % (n/N)
72.4 (97/134)
83.3 (60/72)
Coronary Artery Disease, % (n/N)
56.0 (75/134)
54.2 (39/72)
20.1 (27/134)
26.4 (19/72)
Myocardial Infarction, % (n/N)
Target Limb Rutherford Category, % (n/N)
Class 1
3.0 (4/134)
6.9 (5/72)
Class 2
35.8 (48/134)
41.7 (30/72)
Class 3
61.2 (82/134)
50.0 (36/72)
Class 5
1.4 (1/72)
Target Limb ABI (mm Hg)
N, Mean ± SD
124, 0.71 ± 0.19
67, 0.72 ± 0.19
Contralateral Limb ABI (mm Hg)
N, Mean ± SD
120, 0.88 ± 0.21
64, 0.84 ± 0.21
RESILIENT Trial Lesion Characteristics
Variable
Number of Lesions, % (n/N)
Target Side, % (n/N)
Lesion Location, % (n/N)
Lesion Classification, % (n/N)
Category
Test
Control
1 Lesion(s)
85.8 (115/134)
87.5 (63/72)
2 Lesion(s)
14.2 (19/134)
12.5 (9/72)
Left
47.7 (73/153)
54.3 (44/81)
Right
52.3 (80/153)
45.7 (37/81)
Proximal 1/3 of SFA
13.1 (20/153)
14.8 (12/81)
Middle 1/3 of SFA
32.0 (49/153)
38.3 (31/81)
Distal 1/3 of SFA
50.3 (77/153)
45.7 (37/81)
Proximal Popliteal
4.6 (7/153)
1.2 (1/81)
De Novo/Stenosed
80.4 (123/153)
79.0 (64/81)
18.5 (15/81)
Occlusion
17.0 (26/153)
Restenosed
2.6 (4/153)
2.5 (2/81)
Target Vessel RVD (mm)
N, Mean ± SD
153, 5.2 ± 0.8
81, 5.2 ± 0.9
Lesion % Diameter Stenosis
N, Mean ± SD
153, 86.3 ± 12.5
80, 87.9 ± 11.6
Lesion Length (mm)
N, Mean ± SD
153, 61.3 ± 42.4
81, 57.0 ± 37.0
7
Methods
Subjects underwent either PTA or PTA plus LifeStent® Vascular Stent System placement in the target lesion(s). In cases where the PTA only
result was sub-optimal, stent placement was performed. This occurred in 40% (29/72) of the subjects that were randomized to the PTA-only
treatment arm. Post procedure medication was suggested as aspirin for 6 months and clopidogrel for 12 weeks.
All data were collected on case report forms at investigative sites. Adverse events were adjudicated by the clinical events committee and the
data safety monitoring board routinely reviewed the study outcomes to ensure that the benefits of continuing the study outweighed any
potential risks. Independent core laboratories were utilized to analyze angiographic, x-ray and duplex imaging.
Results
As shown in the principal Safety and Effectiveness table (Section J) the LifeStent® Vascular Stent System demonstrated a significantly higher
freedom from intervention rate (freedom from TVR/TLR) at 6 months (LifeStent® 94.6%; control 52.6%), 12 months (LifeStent® 82.7%; control
45.2% ), 24 months (LifeStent® 70.5%; control 40.1%), and 36 months (LifeStent® 68.1%; control 40.1%) than the PTA control group (p < 0.0001).
Additionally, as expected, there was no difference in the 30-day mortality rate between the two study arms.
c. E-TAGIUSS CONFIRMATORY STUDY
Design
The E-TAGIUSS trial was a prospective, multi-center, confirmatory clinical investigation to evaluate the LifeStent® and LifeStent® XL Vascular
Stent Systems in the treatment of symptomatic vascular disease of the SFA and proximal popliteal artery. A total of 37 subjects were treated
at 7 European investigative sites. Subjects eligible to be enrolled in this study had to demonstrate Trans-Atlantic Inter-Society Consensus (TASC) A, B or C lesions. Reference
vessel diameter (RVD) of the treated subjects was to be 4.0 – 6.5 mm in diameter and the collective length of the treated segment was to
be less than 200 mm. Subjects underwent angiographic analysis of the lesion prior to and immediately following treatment. Subjects were
followed at 30 days with an office visit.
Demographics
Characteristics of the subjects enrolled in the study including age, gender, medical history as well as lesion characteristics are provided in
the tables below.
E-TAGIUSS Trial Subject Demographics
Variable
Age at Procedure (Yrs)
Gender, % (n/N)
Race, % (n/N)
Category
Total
Mean ± SD (N)
37, 71.1 ± 7.8
Female
29.7 (11/37)
Male
70.3 (26/37)
Caucasian
97.3 (36/37)
Other
2.7 (1/37)
Hypertension, % (n/N)
83.8 (31/37)
Hypercholesterolemia, % (n/N)
56.8 (21/37)
Smoking, % (n/N)
48.6 (18/37)
Coronary Artery Disease, % (n/N)
32.4 (12/37)
Diabetes, % (n/N)
24.3 (9/37)
Myocardial Infarction, % (n/N)
13.5 (5/37)
Target Limb Rutherford Category, % (n/N)
Class 1
5.4 (2/37)
Class 2
35.1 (13/37)
Class 3
45.9 (17/37)
Class 4
5.4 (2/37)
Class 5
8.1 (3/37)
Target Limb ABI (mm Hg)
Mean ± SD (N)
35, 0.6 ± 0.2
Contralateral Limb ABI (mm Hg)
Mean ± SD (N)
31, 0.9 ± 0.2
8
E-TAGIUSS Trial Lesion Characteristics
Variable
Category
Total
1
86.5 (32/37)
Number of Lesions, % (n/N)
Target Side, % (n/N)
2
13.5 (5/37)
Left
47.6 (20/42)
Right
52.4 (22/42)
Popliteal
2.4 (1/42)
SFA
95.2 (40/42)
Lesion Location, % (n/N)
Lesion Classification, % (n/N)
Lesion Severity/TASC Grade, % (n/N)
SFA & Popliteal
2.4 (1/42)
Occlusion
42.9 (18/42)
Reoccluded
7.1 (3/42)
Restenosed
2.4 (1/42)
Stenosed
47.6 (20/42)
TASC A
45.9 (17/37)
TASC B
24.3 (9/37)
TASC C
29.7 (11/37)
Target Vessel RVD (mm)
N, Mean ± SD
42, 5.3 ± 0.6
Lesion % Diameter Stenosis
N, Mean ± SD
42, 89.3 ± 15.1
Lesion Length (mm)
N, Mean ± SD
42, 89.2 ± 69.8
Methods
Subjects underwent PTA plus LifeStent® and/or LifeStent® XL Vascular Stent placement in the target lesion(s). Post procedure medication was
suggested as aspirin and clopidogrel for a minimum of 30 days.
All data were collected on case report forms at investigative sites. Adverse events were adjudicated by the clinical events committee and the
data safety monitoring board reviewed the study outcomes. Independent core laboratories were utilized to analyze angiographic data.
Results
As shown in the principal Safety and Effectiveness table (Section J) the LifeStent® and LifeStent® XL Vascular Stent Systems were able to
accurately deploy the stent and demonstrated minimal length change (deployment success 100.0%). Additionally, the acute safety and
effectiveness measures demonstrated positive results.
d. Retrospective Analysis of LifeStent® Vascular Stent Systems in the Treatment of Long Segment Lesions
Design
This study consisted of a post-hoc analysis of four sources of data: (1) a pivotal IDE clinical trial (RESILIENT: IDE G040023; “RESILIENT”), (2)
a multi-center, non-randomized, observational study conducted in Europe (“ELODIE I”), (3) the routine clinical practice of a United States (U.S.)
physician (“US Series”), and (4) the routine clinical practice of a European Union (EU) physician (“EU Series”). In total, two-hundred-eightyfive (285) patients with one or more implanted LifeStent® devices were identified and included in the analysis. There were a total of 46 lesion
segments in this analysis with lesion lengths beyond 160 mm.
Demographics
Characteristics of the subjects and lesions analyzed are provided in the tables below.
9
Demographics: Retrospective Analysis of LifeStent® Vascular Stent Systems in the Treatment of Long-Segment Lesions
Characteristic
RESILIENT
ELODIE I
US Series
EU Series
TOTAL
Age at Procedure (years)
N reported
Mean
198
11
66
10
285
68.4
71.8
72.6
73.9
69.7
St Dev
10.2
8.63
10.9
5.53
10.3
Range
20.7 - 88.2
53.9 - 85.6
36.3 - 96.8
63.9 - 83.1
20.7 - 96.8
Gender (% male)
69.2
45.5
60.6
44.4
65.5
N reported*
198
11
66
9
284
Race (% Caucasian)
88.9
100
77.3
100
86.6
N reported
198
3
66
10
277
Hypertension (%)
85.4
72.7
84.9
100
85.3
N reported
198
11
66
10
285
Hypercholesterolemia (%)
80.3
54.6
75.8
80.0
78.3
N reported
198
11
66
10
285
Smoking (%)
25.8
36.4
60.6
0.0
33.3
N reported
198
11
66
10
285
CAD (%)
56.6
27.3
57.6
30.0
54.7
N reported
198
11
66
10
285
DM (%)
38.9
0.00
50.0
30.0
39.7
N reported
198
11
66
10
285
N reported
198
11
NR
10
219
Class 1 (%)
3.5
0
0
3.2
Class 2 (%)
40.4
45.5
10.0
39.3
Class 3 (%)
56.1
36.4
60.0
55.3
Class 4 (%)
0.0
0
0
0
Class 5 (%)
0.0
18.2
30.0
2.3
Rutherford Category of Target Limb
Indication of Target Limb
N reported
Claudication (%)
Critical Limb Ischemia (%)
198
11
71
10
290
100
90.9
49.3
70.0
86.6
0
9.1
50.7
30.0
13.4
183
NR
ABI of Target Limb
N reported
Mean
0.72
51
10
244
0.61
0.41
0.69
St Dev
0.20
0.22
0.18
0.22
Range
0.24 - 1.45
0 - 1.34
0.1 - 0.67
0 - 1.45
* One patient did not report gender
NR- Not Reported
10
Lesion and Stent Characteristics
Characteristic
RESILIENT
ELODIE I
US Series
EU Series
N Patients
198
11
66
10
285
N Treated Limbs
198
11
72
10
291
212
16
72
10
310
N Treated Lesions
Individual Lesion Length
N reported
TOTAL
212
16
72
10
310
Mean (mm)
66.0
108.8
152.6
214.0
93.1
St Dev Length
35.7
44.7
104.5
109.6
75.1
1.1
1.5
1.1
1.0
1.1
Mean N per Limb
Percent Stenosis (max per limb):
N reported
Mean
198
11
87.8
92.7
0
10
219
96.0
88.5
St Dev
11.3
9.05
6.99
11.2
Range
50 - 100
80 - 100
80 - 100
50 - 100
N Total Lesion Lengths:
< 50 mm
62
1
9
0
72
50 – <100 mm
93
0
19
0
112
100 – <160 mm
37
6
15
3
61
160 – <200 mm
5
1
3
4
13
200 – 240 mm
1
2
8
0
11
0
1
18
3
22
≥ 240 mm
Total Lesion Lengths:
N
Mean
198
11
72
10
291
70.6
158.2
152.6
214
99.15
St Dev
37.7
57.8
104.5
109.6
77.3
Range
10 - 202
30 - 240
16 - 360
140 - 500
10 - 500
N Total Stented Lengths:
< 60 mm
40
0
NR
0
40
60 – < 110 mm
71
0
NR
0
71
110 – < 170 mm
73
1
NR
1
75
170 – < 210 mm
7
7
NR
5
19
210 – < 250 mm
5
0
NR
1
6
2
3
NR
3
8
198
11
NR
104.5
204.5
≥ 250 mm
Total Stent Lengths:
N
Mean
10
219
244.4
115.9
St Dev
55.4
53.2
125.1
69.4
Range
30 - 340
160 - 290
160 - 574
30 - 574
TASC Classification
N Grade A (%)
N Grade B (%)
N Grade C (%)
N Grade D (%)
Total
NR
1 (9.1%)
23 (39.0%)
3 (27.3%)
11(18.6 %)
24 (34.3%)
NR
14 (20.0%)
7 (63.6%)
6 (10.2%)
0 (0%)
19 (32.2%)
13 (18.6%)
19 (27.1%)
11
59
70
* For lesion characteristics, core lab data were used when available; the site reported data were used otherwise. Five (5) patients did not have
lesion characteristics reported by the core lab
NR- Not Reported
11
Methods
Subjects received at least one commercially available LifeStent® stent - in the case of those subjects enrolled in the RESILIENT study (IDE G040023), they received the device as described in G040023, which were identical to the current commercially available LifeStent® device.
Specifically, the following analyses were undertaken:
• Estimating the patency (defined in this analysis as freedom from TVR) at 12-months post-procedure of lesions of length: 50 mm, 100 mm,
160 mm, and 240 mm (long-term effectiveness)
• Comparing the acute safety performance of the LifeStent® device at 30-days post-procedure to the ViVa OPC, and,
• Estimating the freedom from death and amputation at 12-months post-procedure in patients with long lesions treated with the LifeStent®
device by calculating the observed rates in this study (long-term safety).
Data for this retrospective analysis were compiled ‘as received‘ from their respective sources.
Results
The rate of freedom from death, amputation, and TVR, at 30 days post-procedure was 99.6% for the combined performance of the LifeStent® and
LifeStent® XL Vascular Stent Systems, and 88% for the VIVA OPC. Furthermore, long-term safety was shown to have a clinically acceptable freedom
from death and amputation rate through 12-months (84.5%). Moreover, effectiveness was evaluated through estimation of patency at 12 months
post-procedure for lesion lengths of 50 mm, 100 mm, 160 mm, 200 mm and 240 mm via the lesion-length model. The patency at 12 months for
lesions greater than 160 mm in length is 67%.
e. REALITY study
Design
The REALITY Study was a single-arm, non-randomized, prospective, single center study to assess the deliverability, clinical utility, and
effectiveness of the 5 mm diameter size offering of the LifeStent® Vascular Stent System in subjects with lifestyle-limiting claudication
or minor tissue loss (Rutherford Category 2 - 5) who were candidates for PTA and stenting with lesion(s) in the infra-inguinal segment
(SFA and/or popliteal artery). A total of 30 subjects were treated at 1 European investigative site.
Subjects eligible to be enrolled in this study had to be Rutherford Category 2 - 4. The target vessel reference diameter was (by visual estimate)
appropriate for treatment with available stent diameter of 5.0 mm. The reference vessel diameter (RVD) of the treated subjects was to
4.0 - 4.5 mm in diameter. Subjects were followed at 30 days.
Demographics
Characteristics of the subjects enrolled in the study including age, gender, medical history as well as lesion characteristics are provided in
the tables below.
Subject Demographics
Variable
Age at Procedure (yrs)
Gender, % (n/N)
Race, % (n/N)
Category
Total
Mean
69
Standard Deviation
10.5
Female
60.0 (18/30)
Male
40.0 (12/30)
Caucasion
96.7 (29/30)
Asian
3.3 (1/30)
Hyperlipidemia
~57%
Hypercholesteremia
~87%
Diabetes
~37%
12
Lesion Characteristics
Variable
Number of Lesions
Category
1
2
Left
Right
Mean, Standard deviation
Mean, Standard Deviation
Stenosed
Occluded
Re-Occluded
TASC A
TASC B
TASC C
TASC D
No Calcification
Mild Calcification
Moderate Calcification
Severe Calcification
Target Side
Lesion Length (mm)
Target Vessel (RVD)
Lesion Classification
Lesion Severity/TASC Grade
Lesion Calcification
Total
30/32
2/32
62.5%
37.5%
64.8, 50.0
4.5, 0.2
68.8%
28.1%
3.1%
43.8%
34.4%
15.6%
6.3%
34.4%
21.9%
18.8%
25.0%
Methods
Subjects underwent PTA plus LifeStent® Vascular Stent placement in the target lesion(s). All data were collected on case report forms at the
investigative site.
Results
The LifeStent® Vascular Stent System is effective, as technical success was shown, i.e. deployment accuracy was good or excellent and
placement accuracy was successful at target site. Additionally, freedom from TLR and/or TVR was achieved. The LifeStent® Vascular Stent is
safe in the acute period (index procedure through the 30-day follow-up period) as demonstrated through freedom from occurrence of death,
amputation, and TLR and/or TVR. No ADEs were reported during this period.
J. Principal Safety and Effectiveness Tables
a. RESILIENT RANDOMIZED STUDY
RESILIENT Principal Safety and Effectiveness Table
Variable
MACE at 30 Days, % (n/N)
Freedom from MACE at 6 Months, %
Freedom from MACE at 12 Months, %
Freedom from MACE at 24 Months, %
Freedom from MACE at 36 Months, %
Lesion Success, % (n/N)
Hemodynamic Success, % (n/N)
Procedure Success, % (n/N)
Clinical Success at 6 Months, % (n/N)
Primary Patency at 6 Months, %
Secondary Patency at 6 Months, %
Freedom From TVR/TLR at 6 Months, %
Clinical Success at 12Months, % (n/N)
Primary Patency at 12 Months, %
Secondary Patency at 12 Months, %
Freedom From TVR/TLR at 12 Months, %
Clinical Success at 24 months, % (n/N)
Freedom From TVR/TLR at 24 months, %
Clinical Success at 36 months, % (n/N)
Freedom From TVR/TLR at 36 months, %
Test
0.0 (0/134)
93.9
86.6
80.5
75.2
95.8 (114/119)
71.2 (79/111)
95.8 (114/119)
82.2 (97/118)
94.2
100.0
94.6
72.3 (81/112)
81.5
100.0
82.7
68.6 (70/102)
70.5
63.2 (60/95)
68.1
ns* - not significant
Definitions (secondary endpoints denoted with an asterisk (*)):
13
Control
1.4 (1/72)
92.8
85.1
79.7
75.2
83.9 (52/62)
59.6 (31/52)
83.9 (52/62)
30.9 (21/68)
47.4
98.3
52.6
31.8 (21/66)
36.7
98.3
45.2
25.4 (16/63)
40.1
17.9 (10/56)
40.1
p-value
ns*
ns*
ns*
ns*
ns*
0.009
ns*
0.009
<0.0001
<0.0001
ns*
<0.0001
<0.0001
<0.0001
ns*
<0.0001
<0.0001
<0.0001
<0.0001
0.0002
Major adverse clinical events* (MACE): Any event of death (through 30-days), stroke, myocardial infarction, significant distal embolization,
emergent surgical revascularization of target limb, thrombosis, and/or worsening Rutherford category post procedure at the indicated time
point.
Lesion Success*: Attainment of < 30% residual stenosis of the target lesion using any percutaneous method and/or non-investigational
device.
Hemodynamic Success*: Angiographic evidence of improved flow across the treated area immediately post-procedure. ABI improved from
baseline by > 0.10 and not deteriorated by > 0.15.
Procedure Success*: Attainment of < 30% residual stenosis of the target lesion and no in-hospital serious adverse events defined as: death,
stroke, myocardial infarction, emergent surgical revascularization, significant distal embolization in the target limb, and thrombosis of the
target vessel.
Clinical Success*: Relief or improvement of baseline symptoms by Rutherford categories/grades for acute or chronic limb ischemia and the
“definition of improvement”. Improvement must be sustained by one clinical category above the pre-treatment clinical value.
Primary Patency*: The continued flow through the target lesion as evidenced by DUS or angiogram without further/repeat intervention over
time.
Secondary Patency*: The patency history for the target lesion that is sustained or restored (with repeated intervention) over time.
Target Vessel Revascularization (TVR) / Target Lesion Revascularization (TLR): Any “clinically-driven” repeat percutaneous intervention of the
target lesion or bypass surgery of the target vessel. If a control subject requires a stent peri-procedurally due to a bailout procedure, it will
be considered a TLR/TVR for the control group.
Survival Analysis – Freedom from MACE (at 36 months)
Time Until MACE
14
MACE
Event Free
Event Rate
Test (LifeStent®)
75.2%
24.8%
Control (balloon angioplasty)
75.2%
24.8%
P-Value*
0.98
*p-value is from Log-rank test on all available data.
Survival Analysis – Freedom from Loss of Primary Patency (at 12 months)
Time Until Loss of Primary Patency
Loss of Primary Patency
Event Free
Event Rate
Test (LifeStent®)
81.5%
18.5%
Control (balloon angioplasty)
36.7%
63.3%
P-Value*
<0.0001
*p-value is from Log-rank test on all available data.
Stent Fracture Analysis
Independent Analysis
As pre-specified in the RESILIENT protocol, A-P and lateral x-rays were taken at 6-, 12-, and 18-months post-procedure and analyzed by an
independent core lab. X-rays on 291 stents were available for analysis from all phases of the RESILIENT trial. Fractures were classified as
follows:
15
Classification Type
1
Single-strut fracture only
2
Multiple single-stent fractures occuring at different sites
3
Multiple stent fractures resulting in complete transverse linear fracture but without stent displacement
4
Complete transverse linear fracture with stent displacement
Based on Allie, et. al. Endovascular Today 2004; July/August: 22-34.*
* Please note that the fracture analysis in the RESILIENT Study was conducted by an independent core laboratory using the classification
system described by Allie et al., 2004 in accordance with the protocol approved in the IDE prior to study initiation (G040023, 3/19/2004).
This system classifies fractures into four distinct types. Since study initiation, other stent classification systems have been proposed
(Scheinert et al, 2005; Roca-Singh et al., 2007; Popma et al., 2009). The classification system published by Rocha-Singh et al., is currently
used by many core labs in the U.S., and splits the Type 4 fractures as defined by Allie et al. into “stent fracture(s) with mal-alignment of
components”(Type 4) and “stent fracture(s) in a trans-axial spiral configuration” (Type 5). The Type 4 fractures in the RESILIENT Study were
not sub-categorized according to the system proposed by Rocha-Singh and colleagues.
One (1) fracture was noted at the time of the six-month analysis, eight (8) additional fractures were noted at the twelve-month analysis (i.e.,
between 6 and 12 months), and three (3) more fractures were noted at the final eighteen-month analysis (i.e., between 12 and 18 months).
67% (8/12) of the fractures were identified within 7 months of implantation. At the eighteen month analysis, six fractures were noted as Type
I (single-strut fracture) and six fractures were classified as Type IV (complete transverse fracture). Since the overall number of stent fractures
was low throughout the course of the RESILIENT trial, statistical analysis as to cause was not possible.
It was observed however, that of the six Type IV fractures, all six were elongated at deployment, four of six occurred in lesions that were
moderate to severely calcified, and four of six occurred proximal or distal to an area of stent overlap. 38% of patients with >10% elongation
went on to develop Type 4 fractures in less than 1 year and 36% of the fractures occurred in patients where multiple (≥ 2) stents were
deployed in an overlapping fashion. No patients with stent fractures developed restenosis as evaluated at the 12-month follow-up, and no
fractures were associated with MACE. Overall, fractures in RESILIENT had no apparent effect on device safety or effectiveness. The following
table summarizes the fractures categorized according to Allie, et. al.
RESILIENT Fracture Analysis (18 Months)
Type
Type 1
Type 4
Type 1 & 4
Total
Count (stents/subjects)
6/6
5/4
1/1
12/11
Review of Medical Device Reporting
Since February 13, 2009, in the global commercial experience, Bard Peripheral Vascular received complaints of suspected LifeStent® fractures
in 38 patients. Of these reports, nine (9) patients with 10 fractures were confirmed from evaluation of baseline or follow-up angiograms. A
review of the confirmed fractures showed that seven (7) of the stents had single strut fractures and three (3) of the stents had multiple strut
fractures. These were associated with one case of stent twisting, one case of stent elongation, and three cases of stent compression that
may have contributed to the occurrence of fracture. Classification of fracture type was not completed due to the limitations of the data
received from the user and a systematic review of all stents by an angiographic core lab was not performed. Because of the difficulty in
identifying stent fracture and the lack of comprehensive angiographic follow-up, it is not possible to determine the true fracture rate of the
LifeStent® in commercial use.
Conclusion
Stent fractures were noted to be an uncommon event in the RESILIENT trial and appeared to not impact the safety and performance of the
LifeStent® implant. Stent fractures may occur with the use of overlapping stents; however there was no correlation between stent fractures
and the number of stents implanted in the RESILIENT trial. Fractures may occur in SFA or popliteal segments that undergo significant motion,
particularly in areas with severe angulation and tortuosity. The RESILIENT trial was not designed to show a correlation between stent fractures
and the location, although six (6) fractured stents were observed in areas with severe calcification, and one (1) stent placed across the point
of flexion in the mid-popliteal region resulted in a fracture.
16
Patency vs. Lesion Length
In order to assess the impact of lesion length on patency outcomes, a Cox regression analysis, with the total lesion length as a risk factor
was performed which demonstrated that for the LifeStent® group, lesion length is not a significant predictor of primary patency outcomes
(p-value = 0.46). Additionally, the calculated hazard ratio of 1.003 indicates that there is only a remote relationship between lesion length
and patency outcomes in the LifeStent® group. It should be noted that based on the analysis, the lesion length is a significant predictor of
patency outcomes for the control group (p-value = 0.0025).
b. E-TAGIUSS CONFIRMATORY STUDY
E-TAGIUSS Principal Safety and Effectiveness Table
Variable
Test % (n/N)
Death at 30 Days
0% (0/37)
MACE at 30 Days
2.7% (1/37)
Deployment Success
100.0 (46/46)
Lesion Success
90.9 (30/33)
Procedure Success
90.9 (30/33)
Definitions (secondary endpoints denoted with an asterisk (*)):
Major adverse clinical events* (MACE): Any event of death, stroke, myocardial infarction, emergent surgical revascularization, significant distal
embolization in the target limb, amputation of the target limb and thrombosis of the target vessel at the indicated time point.
Deployment Success: Ability to deliver the stent to the intended site with the post deployment stent length being within 10% of the predeployment length.
Lesion Success*: Attainment of ≤ 30% residual stenosis of the target lesion using any percutaneous method and/or non-investigational device.
Procedure Success*: Attainment of ≤ 30% residual stenosis of the target lesion and no in-hospital serious adverse events defined as: death,
stroke, myocardial infarction, emergent surgical revascularization, significant distal embolization in the target limb, and thrombosis of the
target vessel.
c. Retrospective Analysis of LifeStent® Vascular Stent Systems in the Treatment of Long-Segment Lesions
The results for the primary effectiveness endpoint as defined by freedom from TVR/TLR are shown in table below.
Freedom from TLR/TVR* by Time and Lesion Length
12 months Weibull* / Kaplan-Meier
(n/N**at 12 months)
24 months Weibull* / Kaplan-Meier
(n/N**at 24 months)
82.4% / 79.2% (54/291)
63.3% / 62.5% (29/170)
85.4% / 83.4 (11/72)
69.0% / 68.1% (7/48)
(n=112) 50 - < 100 mm lesions (Weibull: 100 mm)
81.9% / 87.9% (12/112)
62.5% / 74.3% (9/73)
(n=61)
100 - < 160 mm lesions (Weibull: 160 mm)
76.7% / 76.5% (13/61)
53.6% / 55.2% (9/35)
(n=13)
160 - < 200 mm lesions (Weibull: 200 mm)
72.6% / 38.9% (7/13)
47.0% / 38.9% (0/2)
(n=11)
200 - < 240 mm lesions (Weibull: 240 mm)
67.9% / 67.5% (3/11)
40.2% / NA (1/5)
(n=22)
NA / 55.9% (8/22)
NA / 23.9% (3/7)
Variable
Average of all (total) lesion lengths (= 101.1 mm)
(n=72)
< 50 mm lesions (Weibull: 50 mm)
> 240 mm lesions
* From the Weibull covariate-adjusted analysis
** Number starting the year
The primary acute safety endpoint of the LifeStent® and LifeStent® XL Vascular Stent Systems at 30 days post-procedure showed the freedom
from rates were higher than the ViVa OPC (88%). The 30-day freedom-from-death, amputation and TVR rate was 99.6% with a standard
error of 0.34% (95% CI: 97.59% - 99.95%).
The primary long-term safety endpoint was freedom from death/amputation. The Kaplan-Meier analysis showed that the freedom-fromdeath/amputation rate at 12 months was 100% (lesions < 50 mm), 94.5% (lesions 50 - 100mm), 91.4% (lesions 100 - 160 mm), 63.6%
(lesions 160 - 200 mm), 90.9% (lesions 200 - 240 mm) and 94.1% (lesions >240 mm).
17
Freedom from Death/Amputation*
12 months (n/N**)
All Lesions
93.8 (17/291)
Lesions < 50 mm
100% (0/72)
Lesions 50 - 100 mm
94.5% (6/112)
Lesions 100 - 160 mm
91.4% (5/61)
Lesions 160 - 200 mm
63.6% (4/13)
Lesions 200 - 240 mm
90.9% (1/11)
Lesions > 240 mm
94.1% (1/22)
* From the Kaplan-Meier analysis
** Number starting the year
d. REALITY study
The safety and effectiveness results are shown below.
Technical Success: All 36 stents deployed in the study were successfully deployed.
Placement Accuracy: The deployment accuracy was evaluated and found to be acceptable in all cases.
Freedom from Death through 30 days post index procedure: All subjects showed freedom from occurrence of death.
Freedom from Amputation through 30 days post index procedure: All subjects showed freedom from occurrence of amputation.
Freedom from TLR/TVR through 30 days post index procedure: All subjects showed freedom from TLR and/or TVR.
Primary Effectiveness Endpoint: Technical success, defined as successful deployment and placement accuracy based upon a rating scale
completed by the Investigators at the time of the index procedure. Bookend sizes were evaluated for clinical utility of size range.
All stents had good or excellent deployment accuracy with successful placement at the target site. In none of the patients, TLR and/or TVR
was conducted until day 30 from the index procedure.
Primary Safety Endpoint: Freedom from occurrence of death, amputation, and TVR and/or TLR at 30 days post index procedure.
All 30 subjects showed freedom from occurrence of death, amputation, and TLR and/or TVR at day 30 post index procedure. Overall, this
study demonstrated the safety of the LifeStent® Vascular Stent Systems deploying stents of 5 mm in diameter.
K. Patient Selection and Treatment
Patient selections should be based on the populations treated in the RESILIENT and E-TAGIUSS investigations. Demographics for the two
investigations are provided in Section I – Clinical Investigations of this “Instructions for Use” document. Additionally, treatment of the patients
should follow the treatment practices used by the RESILIENT and E-TAGIUSS investigators. These methods have been reiterated below in
Section L – Patient Counseling Information and Section N – Instructions for Use.
L. Patient Counseling Information
Physicians should consider the following in counseling the patient about this product:
• Discuss the risks associated with stent placement.
• Discuss the risks associated with a LifeStent® implant.
• Discuss the risks/benefits issues for this particular patient.
• Discuss alterations to current lifestyle immediately following the procedure and over the long term.
• Discuss the risks of early discontinuation antiplatelet therapy.
The following information is provided in the packaging for the physician to provide their patients:
• A Patient Guide which includes information on the LifeStent® XL Vascular Stent System, peripheral artery occlusive disease, the
implantation procedure and patient care following the implant.
• A Patient Implant Card that is used to record and disseminate information about the patient and the stent.
18
M. How Supplied
STERILE: FOR SINGLE USE ONLY. The LifeStent® XL Vascular Stent System is supplied sterile (by ethylene oxide gas) and is nonpyrogenic.
Do not resterilize and/or reuse the device. Do not use if the temperature exposure indicator (i.e., square label found on the pouch) is black as
the unconstrained stent diameter may have been compromised. The temperature exposure indicator label should be grey and must be clearly
visible on the pouch. Do not use if pouch is opened or damaged. Do not use the stent after the end of the month indicated by the “Use By”
date specified on the package. For returned product or product issues, please contact Bard Peripheral Vascular at the address below:
Bard Peripheral Vascular, Inc.
1625 West 3rd Street
Tempe, AZ 85281 USA
CONTENTS for one (1) LifeStent® XL Vascular Stent System:
• One (1) LifeStent® XL Vascular Stent System
• One (1) Patient Implant Card
• One (1) Instructions for Use
• One (1) Patient Guide
STORAGE: Store in a cool, dark, dry place. Storage temperature should not exceed 60°C. Use by the end of the month indicated by the “Use
By” date specified on the package.
DISPOSAL INSTRUCTIONS: After use, dispose of product and packaging in accordance with hospital, administrative and/or local government
policy.
N. Instructions for Use
Pre-Deployment Procedure
1. Inject Contrast Media
Perform an angiogram using standard technique.
2. Evaluate and Mark Target Site
Fluoroscopically evaluate and mark the target site, observing the most distal diseased or obstructed segment.
3. Select Stent Size
Measure the length of the target lesion to identify the appropriate length of stent(s) required. Ensure that the stent is long enough to permit
the area proximal and distal of the lesion to be covered by the stent.
Identify the diameter of the reference vessel (proximal and distal to the lesion). To ensure secure placement, refer to the stent size
selection table for proper sizing scheme.
Stent Size Selection Table: LifeStent® XL Vascular Stent System
Reference Vessel Diameter
Unconstrained Stent Inner Diameter
4.0 – 4.5 mm
5.0 mm
4.0 – 5.5 mm
6.0 mm
5.6 – 6.5 mm
7.0 mm
Refer to product labeling for stent length
4. Materials Required
In addition to the LifeStent® XL Vascular Stent System, the following standard materials may also be required to facilitate delivery and
deployment of the LifeStent® XL Vascular Stent System: heparinized normal saline, 6F (2.0 mm) or larger introducer sheath, 0.035”
diameter guidewire, standard balloon angioplasty (PTA) catheter, contrast medium diluted 1:1 with heparinized normal saline, inflation
device and appropriate anticoagulation and antiplatelet drugs.
19
5. Prepare Stent System
a) Open the box and remove the pouch containing the stent system.
b) Check the temperature exposure indicator label on the pouch to confirm that the grey background is clearly visible. See “Warnings” section.
c)Carefully inspect the pouch for damage to the sterile barrier. Do not use after the expiration date. Peel open the pouch and remove the
tray containing the stent system. Extract the stent system from the tray and check the following:
i) Verify that the shipping lock is still secure in the stent system handle.
ii) Examine the stent system for any damage. If it is suspected that the sterility or performance of the device has been compromised,
the stent system should not be used.
d)Visually inspect the distal end of the stent system to ensure that the stent is contained within the sheath. Do not use if the stent is partially
deployed.
e) Flush the inner lumen of the stent system with heparinized normal saline prior to use.
f) Wipe the usable length portion of the stent system with a gauze soaked with heparinized normal saline.
Stent Deployment Procedure
1. Insert Introducer Sheath and Guidewire
a) Gain femoral access at the appropriate site using a 6F (2.0 mm) or larger introducer sheath.
b) Insert a 0.035“ diameter guidewire of appropriate length (see table) across the lesion to be stented via the introducer sheath.
Recommended Guidewire Length Table
Catheter Working Length
Recommended Guidewire Length
130 cm
300 cm
80 cm
260 cm
2. Dilate Lesion
Predilation of the lesion should be performed using standard techniques. While maintaining site access with a guidewire, remove the
balloon catheter from the patient.
Caution: During dilation, do not expand the balloon such that dissection complication or perforation could occur.
3. Introduce stent system
a)Advance the stent system over the 0.035“ diameter guidewire through the sheath introducer. Always use for contralateral access the stent
system in conjunction with a long introducer sheath which covers the aortic bifurcation.
Note:
If resistance is met during stent system introduction, the stent system should be removed and another stent system should
be used.
Caution:Always use an introducer sheath for the implant procedure to protect the vasculature and the puncture site. A 6F (2.0 mm)
or larger introducer sheath is recommended.
b) Position the tip of the stent system past the target site.
c)Pull back the stent system until the distal and proximal ends of the stent are in position so that they are distal and proximal to the target
site.
d) Remove slack from the stent system held outside the patient.
Caution:
Any slack in the stent system (outside the patient) could result in deploying the stent beyond the target site.
20
4. Deploy stent
a) Verify that the distal and proximal stent ends are distal and proximal to the target lesion.
b) Confirm that the introducer sheath is secure and will not move during deployment.
c) Remove the shipping lock.
d) To ensure the most accurate placement, firmly hold the black system stability sheath throughout deployment.
Note: Do NOT hold the silver stent delivery sheath at any time during deployment. DO NOT constrict the stent delivery sheath during
stent deployment.
e) Initiate stent deployment by rotating the thumbwheel in the direction of the arrows while holding the handle in a fixed position.
Note:
If excessive force is felt during stent deployment, do not force the stent system. Remove the stent system as possible, and
replace with a new unit.
f)While using fluoroscopy, maintain position of the distal and proximal stent ends relative to the targeted site. Watch for the distal stent end
to begin expanding; separation of the distal stent end signals that the stent is deploying. Continue turning the thumbwheel until the distal
end of the stent obtains complete wall apposition.
While maintaining a fixed handle
position, rotate thumbwheel
to obtain initial stent wall
apposition of 1 cm
minimum.
Figure 3. Initial Thumbwheel Deployment
Note:The thumbwheel is designed to initially deploy the stent distal end a minimum of 1 cm. Final stent deployment is achieved
by using the deployment lever.
g) With distal end of the stent apposing the vessel wall, deployment continues with the following method (Fig. 4).
While maintaining a fixed handle position,
place your finger in front of the
deployment slide and slide it from the
distal to proximal end.
Figure 4. Fast Track Deployment Lever
Note:To ensure correctly deployed stent length, fluoroscopically monitor the distal stent end initially until wall apposition then
monitor the delivery system proximal radiopaque marker relative to the proximal edge of the target site.
h)Deployment of the stent is complete when the proximal stent end apposes the vessel wall and the sheath radiopaque zone is proximal to
the proximal end of the stent.
i) DO NOT attempt to re-sheath stent system prior to removal.
5. Post stent placement
a) Remove the stent system from the body.
Note:
If resistance is met while retracting the delivery system over a guidewire, remove the delivery system and guidewire
together.
b) P ost stent expansion with a PTA catheter is recommended. If performed, select a balloon catheter that matches the size of the reference
vessel, but that is not larger than the stent diameter itself.
21
c) Remove the guidewire and introducer sheath from the body.
d) Close entry wound as appropriate.
e) Discard the stent system, guidewire, and introducer sheath.
Note:
Physician experience and discretion will determine the appropriate drug regimen for each patient.
22
23
Symbols used on labeling
Keep away from sunlight
The Green Dot
Keep dry
Recyclable
MR Conditional
LifeStent® XL Vascular Stent Systems
Bard and LifeStent are trademarks and/or registered trademarks of C. R. Bard, Inc.
All other trademarks are the property of their respective owners.
Caution: Federal (USA) law restricts this device to sale by or on the order of a physician.
Copyright © 2014 C. R. Bard, Inc.
All Rights Reserved
Distributed in the USA by:
Bard Peripheral Vascular, Inc.
1625 West 3rd Street
Tempe, AZ 85281
USA
TEL:
1-480-894-9515
1-800-321-4254
FAX:1-480-966-7062
1-800-440-5376
www.bardpv.com
B05679 Rev.0/03-14
24