REVIEW
doi:10.1111/j.1360-0443.2011.03621.x
Alcohol consumption and the intention to engage in
unprotected sex: systematic review and meta-analysis
of experimental studies
add_3621
51..59
Jürgen Rehm1,2,3, Kevin D. Shield1,2, Narges Joharchi1,4 & Paul A. Shuper1,5,6
Centre for Addiction and Mental Health (CAMH),Toronto, Canada,1 Institute of Medical Science (IMS), University of Toronto,Toronto, Canada,2 Dalla Lana School
of Public Health (DLSPH), University of Toronto,Toronto, Canada,3 Department of Statistics, University of Toronto,Toronto, Canada,4 Department of Psychology,
University of Toronto, Toronto, Canada5 and Center for Health, Intervention and Prevention, University of Connecticut, Storrs, CT, USA6
ABSTRACT
Aims To review and analyse in experimentally controlled studies the impact of alcohol consumption on intentions to
engage in unprotected sex. To draw conclusions with respect to the question of whether alcohol has an independent
effect on the incidence of human immunodeficiency virus (HIV) and other sexually transmitted infections (STIs).
Methods A systematic review and meta-analysis of randomized controlled studies examined the association between
blood alcohol content (BAC) and self-perceived likelihood of using a condom during intercourse. The systematic review
and meta-analysis were conducted according to internationally standardized protocols (Preferred Reporting Items for
Systematic Reviews and Meta-Analyses: PRISMA). The meta-analysis included an estimate of the dose–response effect,
tests for publication bias and sensitivity analyses. Results Of the 12 studies included in the quantitative synthesis, our
pooled analysis indicated that an increase in BAC of 0.1 mg/ml resulted in an increase of 5.0% (95% CI: 2.8–7.1%)
in the indicated likelihood (indicated by a Likert scale) of engaging in unprotected sex. After adjusting for potential
publication bias, this estimate dropped to 2.9% (95% CI: 2.0–3.9%). Thus, the larger the alcohol intake and the
subsequent level of BAC, the higher the intentions to engage in unsafe sex. The main results were homogeneous,
persisted in sensitivity analyses and after correction for publication bias. Conclusions Alcohol use is an independent
risk factor for intentions to engage in unprotected sex, and as risky sex intentions have been shown to be linked to actual
risk behavior, the role of alcohol consumption in the transmission of HIV and other STIs may be of public health
importance.
Keywords Alcohol consumption, HIV, meta-analysis, randomized controlled trial, sexual behavior, sexually
transmitted infections, unprotected sex.
Correspondence to: Kevin D. Shield, CAMH, 33 Russell Street, Toronto, Ontario, Canada M5S 2S1. E-mail: Kevin.shield@utoronto.ca
Submitted 24 January 2011; initial review completed 29 April 2011; final version accepted 15 August 2011
INTRODUCTION
Alcohol use is associated with the acquisition of human
immunodeficiency virus/acquired immune deficiency
syndrome (HIV/AIDS) and other sexually transmitted
infections (STIs) [1–4], with one major potential pathway
between alcohol and the acquisition of HIV and STIs
being unprotected sex [5,6]. It has been purported that
the consumption of alcohol can result in disinhibition [5]
and a constraint in cognitive capacity that leads to a focus
on risk-impelling rather than risk-inhibiting cues [7]
which, in turn, can increase the likelihood of having sex
© 2011 The Authors, Addiction © 2011 Society for the Study of Addiction
without a condom. However, this direct causal pathway
linking alcohol use to unsafe sex and subsequent transmission of HIV and other STIs has been difficult to establish conclusively, as there may be confounding due to
personality factors such as sensation seeking, risk taking
or compulsivity (e.g. people who consume alcohol and
then engage in unsafe sex may be doing so because they
have different, riskier personality traits) [8]. The role of
such third variables may, in part, be responsible for the
somewhat inconsistent evidence supporting a behaviorally based alcohol use—unprotected sex association [8].
For example, meta-analyses and reviews based on studies
Addiction, 107, 51–59
52
Jürgen Rehm et al.
assessing the relationship between generalized measures
of alcohol use and/or abuse and the occurrence of
unprotected sex over time (so-called global-level studies)
have provided supportive evidence [1,4,9,10], but these
investigations are typically unable to control for potentially confounding and ‘in-the-moment’ variables [8].
In contrast, meta-analyses and systematic reviews based
on event-level studies, which are able to control for third
variables such as personality traits, have yielded mixed
results, with two meta-analyses finding significant eventlevel associations [1,11] and others finding no significant
associations [10,12,13]. Thus, based on these data alone,
causality cannot be asserted with confidence.
One way to establish causality in such a situation is to
vary exposure experimentally; in this case, exposure to
alcohol. Manipulating alcohol exposure experimentally
for longer time-periods to examine potential disease consequences is both unethical and unfeasible; however,
experimental variation of alcohol exposure is possible for
shorter periods [14,15]. If such experimental variation
can be combined with the measurement of an outcome
which is a valid precursor to unsafe sex, causality could
be established, following the tradition of nutritional epidemiology to establish causality of nutrients for cancer
[16] or in the cardiovascular disease area (see: http://
www.who.int/nutrition/topics/5_population_nutrient/
en/index.html). For example, to show that certain
nutrients can causally impact coronary heart disease,
nutrients have been varied for short periods of time in
randomized controlled clinical trials, and then their effect
on blood lipids as a precursor to heart disease has been
measured. Similarly, alcohol use can be varied experimentally to measure the effect on intentions to engage in
unsafe sex, an established link in the pathway to unsafe
sex behaviors and, thus, to acquisition of HIV and other
STIs [17–19]. Experimental studies investigating the
behaviorally based association between alcohol consumption and unsafe sex do so by randomizing alcohol
consumption and assessing the impact on the selfperceived intent to engage in unprotected sex. Despite
focusing on intentions to use condoms rather than actual
condom use behavior, conclusions can be drawn regarding a potential association between alcohol use and HIV
and other STIs, as the literature clearly shows a significant link between condom use intentions and actual use
of condoms under a variety of conditions and circumstances [17]. Furthermore, intentions have been shown
to be one of the strongest predictors of subsequent
condom use behavior [17].
To exclude the potential effect of personality variables
and to establish an independent effect of alcohol consumption on subsequent sexual behavior, we performed
a systematic review and a meta-analysis of randomized
controlled studies to establish a quantitative estimate of
© 2011 The Authors, Addiction © 2011 Society for the Study of Addiction
the effect of alcohol consumption as measured by blood
alcohol content (BAC) on self-perceived intentions to
engage in unsafe sex, including establishing a dose–
response relationship to assess if alcohol can have a
behaviorally based effect on the intent to engage in unsafe
sex independent of personality factors.
METHODS
The systematic review was conducted and reported
according to the standards set out in PRISMA (Preferred
Reporting Items for Systematic Reviews and MetaAnalyses) (http://www.prisma-statement.org/)[20].
Search strategy and study selection
PsycInfo and PubMed (including MEDLINE and Life
Science Journals) databases were queried for articles
that tested the association between experimental
manipulations of alcohol consumption and intentions to
engage in unprotected sex. Search terms for alcohol were
‘alcohol’, ‘ethanol’ and ‘drink*’. For risky sex, the search
terms were ‘HIV’, ‘sex*’, ‘condom*’ and ‘unprotect*’.
Finally, the search terms for intentions were ‘intention*’,
‘intend’, ‘decision making’, ‘willingness’ and ‘motivation’. Searches of the databases were concluded on 2
May 2011. Articles were restricted to those published in
English on or before the search date. Titles and abstracts
for all references were reviewed, with relevant articles
retained for full paper reviews.
Articles were retained if they met the following
inclusion criteria: (i) consisted of original, quantitative
research published in a peer-reviewed journal; (ii)
involved an experimental manipulation of BAC during
the course of the study; (iii) assessed intentions to engage
in unprotected sexual acts; (iv) tested the association
between BAC and intentions to engage in unprotected
sexual behavior; and (v) involved individual (rather than
group) assessments with participants. To be included
in our quantitative synthesis, articles also needed to
provide a measure of uncertainty for the abovementioned association.
Quality criteria
The minimum quality criteria for inclusion were as
follows: (i) the allocation of placebo and alcohol had to be
randomized; (ii) the participant had to be blinded; and (iii)
the participants had to have not been able to distinguish
between the placebo and alcohol.
Data collection
Measures of association were: (i) linear regression beta
coefficients and their 95% confidence interval (CI);
Addiction, 107, 51–59
Alcohol and intention for unprotected sex
53
P-value; and/or standard error (SE) or (ii) group means
with their standard deviation (SD) for the effect of BAC on
the likelihood of engaging in unprotected sex.
or differed by the sample source (community versus a
campus sample) using a meta-regression analysis.
Measurement of alcohol consumption
RESULTS
The average BAC (if not available, the target BAC) was
used from each study to adjust for individual differences
in body weight. The mean target BAC ranged from
0.03 mg/ml to 0.10 mg/ml. To ensure comparability
between studies, the magnitude of the difference between
means was adjusted for the mean BAC of the intervention
group for each study.
Study selection and study characteristics
Standardization of outcome measures and
measurement of risk relations
As the SD of the self-perceived likelihood of using a
condom during sexual intercourse as indicated on a
Likert scale was not provided for the control groups in
each study, it was not possible to formulate a standard
measure that could be used in the meta-analysis. Instead,
all outcome estimates were corrected for the size of the
scale by dividing each of the estimates by the range of the
corresponding scale.
Differences between mean scores and the SE estimates
for those studies that did not provide a linear regression
beta coefficient were calculated from provided group
means and the SD of these means [21]. In addition, we
standardized risk relations by adjusting all estimates to an
effect for 0.10 mg/ml assuming a linear dose–response
effect. The assumption of a linear relationship was
checked using a meta-regression analysis.
Statistical analysis
Our meta-analysis examined univariate linear regression
beta coefficients by means of DerSimonian & Laird’s
random effects [22]. For studies which provided a P-value
less than an a threshold, a conservative estimate of this
threshold minus 0.001 was taken as the P-value.
The overall point estimate and 95% CI were based on a
weighted pooled measure. Heterogeneity between studies
was assessed using the Cochrane Q-test and the I2 statistic. Publication bias was tested by visually inspecting a
funnel plot for skewed distribution, by using a ranked
correlation test proposed by Begg & Mazumdar, and by
employing a weighted regression test proposed by Egger
et al. [23]. To adjust the pooled estimate for publication
bias we used the trim and fill method [24]. All analyses
were performed using STATA version 11.0 [25].
Sensitivity analysis
We investigated if the association of alcohol and the
intention to engage in unprotected sex differed by gender
© 2011 The Authors, Addiction © 2011 Society for the Study of Addiction
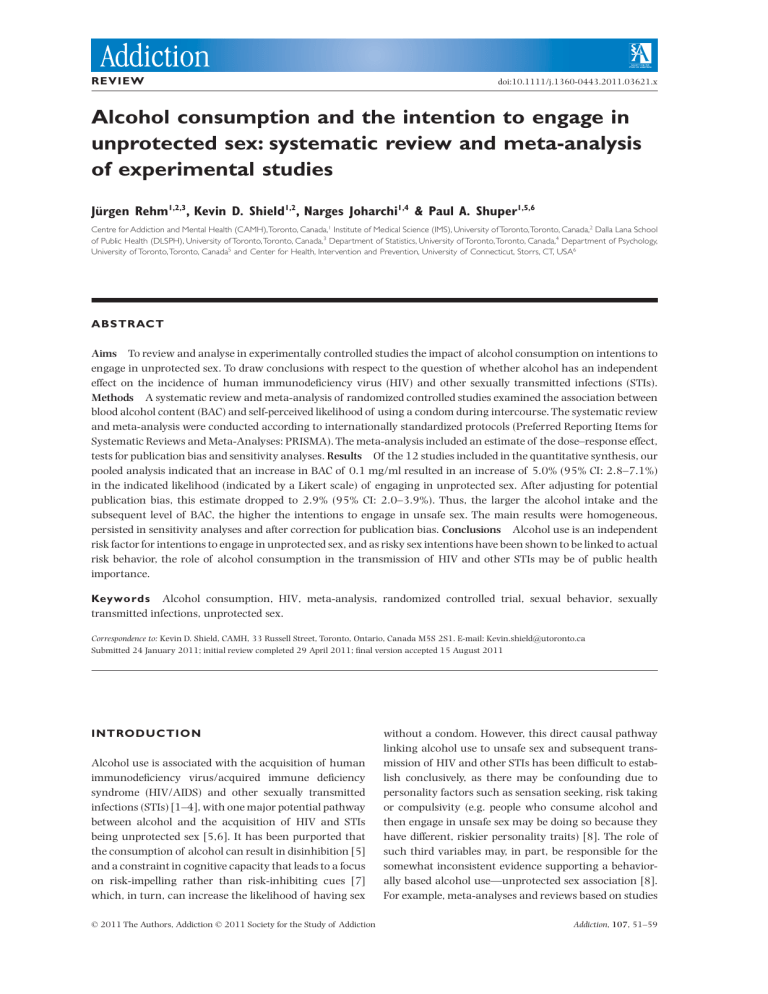
Figure 1 outlines the search strategy. Search results
yielded 631 articles from PubMed and 307 articles from
PsycInfo. Titles and abstracts for all references were
reviewed, and 50 articles were retained for full paper
reviews.
In total, nine publications satisfied the above eligibility
criteria of containing quantitative data relating to the
effects of alcohol consumption on the intent to engage
in unprotected sex where participants were questioned
individually (two papers were excluded for questioning
individuals in groups). Two additional publications that
met the inclusion criteria were found by examining the
reference sections of the 50 relevant publications.
The 11 papers retained for analysis contained a total
of 14 relevant studies. Of the 14 relevant studies, two
involved an analysis of the same participants. Of these
two papers, we retained the paper that examined the
effect of BAC on condom use intentions (the other paper
examined the effect of alcohol dose on condom use intention), resulting in 13 studies. One of the 13 remaining
studies provided a linear regression beta coefficient but
did not provide any indication of uncertainty (e.g. a
P-value, CI or SE) and, thus, was excluded from our
analysis [26]. Of the remaining 12 studies that formed
the basis of our meta-analysis, eight provided differences
between means using linear regression analysis, and two
studies provided the difference between the means as well
as the estimated standard deviation (SD) of each mean.
The remaining 12 studies met all quality criteria and
were retained for analysis. The key study characteristics
and outcomes for the relevant studies can be found in
Table 1.
Definition of intent to have unprotected sex
Measurement of the intent to have unprotected sex was
highly variable across all studies (see Table 1). The constructs and questions also varied in terms of the number
of questions asked, the SD of the measure in the control
groups and the range of the scale.
Meta-analysis
Random effects analysis indicated a significant positive
association between BAC and the intention to engage
in intercourse without a condom, demonstrating that
the higher the BAC, the more pronounced the intention to engage in unsafe sex. Tests demonstrated that
Addiction, 107, 51–59
Jürgen Rehm et al.
Search Result
PsycInfo = 307 PubMed = 631
Articles found by examining the reference
section of relevant articles. n= 2
938 Titles/Abstracts screened
Excluded (including
duplicates) n = 888
50 full- text articles screened
for eligibility
39 articles excluded
n= 38 for not meeting eligibility criteria
n= 1 for analysis of the same participants
11 articles (containing 13
studies) included in qualitative
synthesis
1 study that reported a non-significant effect
was excluded for not reporting a S.E., CI or
P-value
Included
Eligibility
Screening
Identification
54
12 studies included in
quantitative synthesis
(meta-analysis)
Figure 1 Search strategy for randomized controlled trials that assessed likelihood of condom use during intercourse after alcohol
consumption; CI: confidence interval; CI: confidence interval
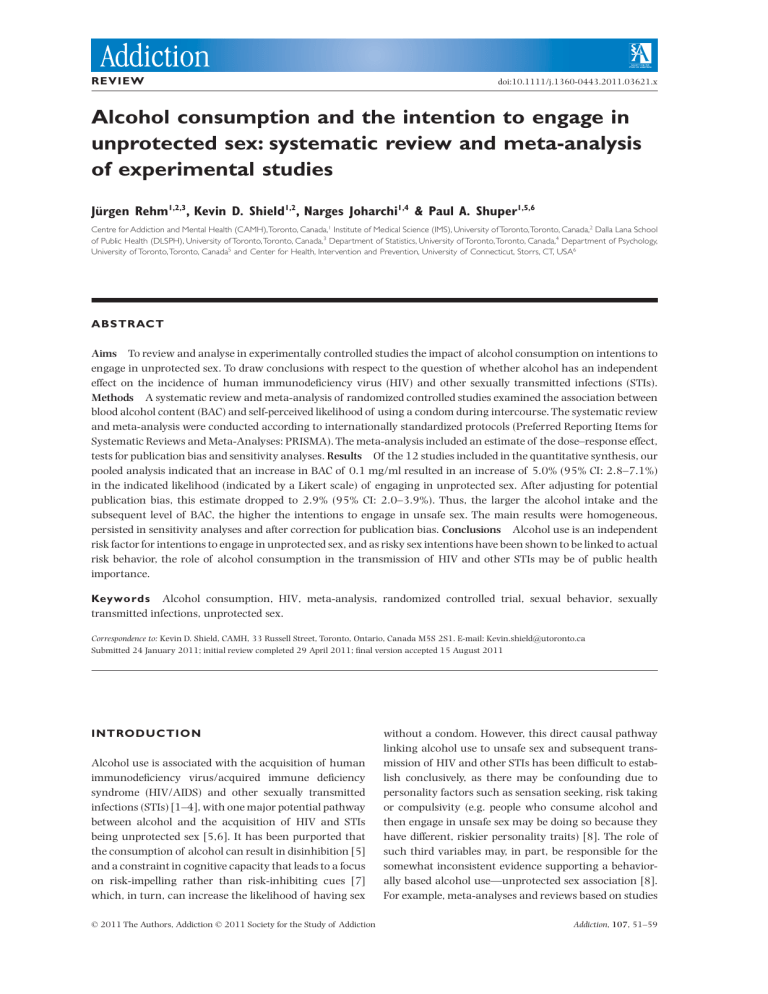
heterogeneity in the estimates was present [Q(11) = 28.52,
P = 0.003; I2 = 61%, P = 0.000]. As demonstrated in
Fig. 2 (forest plot), while all studies showed effects of
alcohol consumption in the hypothesized directions, four
studies had non-significant results whereas the other
eight studies showed a significant association between
alcohol consumption and the intent to engage in unprotected sex. Additionally, all studies had a similar effect size
except for the Ebel-Lam and colleagues’ study [27], which
exhibited the largest effect size. Our pooled analysis indicated that an increase in BAC of 0.1 mg/ml from a BAC
of 0.00 mg/ml resulted in an increase of 5.0% (95% CI:
2.8–7.1%) in the indicated likelihood (indicated by a
Likert scale) of engaging in unprotected sex. Additional
analyses showed that the association between BAC
and intention to engage in unprotected sex was indeed
linear, and the alternative hypothesis of a curvilinear
relationship could be rejected for BAC between 0 and
0.10 mg/ml. Neither gender nor the sample (community,
community and campus, campus) significantly modified
the relationship between alcohol consumption and the
intent to engage in unprotected sex.
Publication bias appeared to be present, as observed in
our funnel plot (see Fig. 3). The funnel plot indicates that
© 2011 The Authors, Addiction © 2011 Society for the Study of Addiction
when plotting the point estimates by the SE of the point
estimate from the studies used in our meta-analysis,
the plot does not take the shape of a triangle which is
expected under the central limit theorem [23,28]. Additionally, the Egger weighted regression also indicated the
presence of publication bias (P = 0.001), while a Begg
rank correlation test did not indicate publication bias
(P = 0.059). These tests indicate that overall publication
bias is probably present and, thus, it is likely that findings
of some studies were not published in peer-reviewed
journals that would have been captured in a search of
the PubMed and PsycInfo databases. Adjustment of the
pooled estimate for publication bias resulted in an
overall pooled estimate of 2.9% (95% CI: 2.0–3.9%) for
an increase of 0.10 mg/ml in BAC from a BAC of
0.00 mg/ml.
DISCUSSION
In experimental studies there is a consistent significant
effect of the level of alcohol consumption on intention to
use condoms, indicating that the higher the BAC, the
higher the intention to engage in unsafe sex. In this study,
we observed that if an individuals BAC increases from 0
Addiction, 107, 51–59
© 2011 The Authors, Addiction © 2011 Society for the Study of Addiction
25.0 (3.8)
24.3 (3.8)
22.7 (2.7)
22.8 (2.2)
23.8
25.0 (3.9)
n = 173 female; USA (campus)
n = 80 male; USA (community)
n = 60 male; USA (community)
n = 48 male; USA (campus)
n = 173 female; USA
(community and campus)
n = 115 (58 female, 57 male);
USA (campus)
n = 79 male; Canada (campus)
Maisto et al. 2004 [49]
Norris et al. 2009 [51]
3
1
2
George et al. 2009 [46]
Kruse et al. 2005 [47]
Kruse et al. 2005 [47]
aMean
blood alcohol content (BAC) levels. bTarget BAC levels. SD: standard deviation.
Schacht et al. 2010 [53]
Ebel-Lam et al. 2009 [27]
Stoner et al. 2007 [52]
2
George et al. 2009 [46]
n = 64; USA (community)
22.4 (2.9)
n = 200 (99 female, 101 male);
USA (community)
n = 61 (30 female, 31 male);
USA (community and
campus)
n = 165 male USA (campus)
Cho et al. 2010 [44]
27.0 (4.0)
20.9 (1.8)
24.9 (3.6)
24.3 (7.2)
24.2 (3.3)
n = 120 (60 female, 60 male);
USA (campus)
Abbey et al. 2006 [26]
Davis et al. 2007[45]
24.0 (3.0)
Sample
n = 180 (90 female, 90 male);
USA (campus)
Substudy
Abbey et al. 2005 [43]
Author
Mean age
(years) (SD)
0.08b
0.079 (0.013)
a
0.034 (0.008)/
0.064 (0.009)a
0.04/0.08b
0.059 (0.011)a
0.05 (0.01)a
0.06 (0.01)a
0.06/0.08/0.10
(mean = 0.08)b
0.06/0.08/0.10
(mean = 0.06)b
0.10
b
0.08b
0.072 (0.010)a
0.069 (0.018)a
Blood alcohol content
(BAC) (mg/ml)
(standard deviation)
Multi-dimensional condom
attitudes scale (MCAS) [50].
Scale 1–7
Condom desire/request; mean of
2 questions [52]. Scale 1–5
Condom desire/request; mean of
2 questions. Scale 1–5
Likelihood of having
unprotected sex (1 Likert
scale question). Scale 1–9
Condom desire/request; mean of
2 questions. Scale 1–10
Intention to use a condom [48].
Scale 0 to 100
Intention to use a condom [48].
Scale 0–100
Likelihood of unprotected sex.
Mean of 4 Likert scale
questions. Scale 1–5
Likelihood of having
unprotected sex (1 Likert
scale question). Scale 1–7
Likelihood of having
unprotected sex (1 Likert
scale question). Scale 1–7
Intention not to use a condom
(3 questions). Scale 0–100
Intention to have unprotected
sex (1 Likert scale question).
Scale 1–5
Likelihood of unprotected sex.
Mean of 4 Likert scale
questions. Scale 1–5
Sexual risk indicator
5.0 (2.2–7.8)
28.8 (17.2–40.5)
4.2 (0.8–7.7)
3.7 (-9.0 to 16.4)
4.1 (0.6–7.6)
10.3 (-0.7 to 21.4)
16.7 (-6.7 to 40.2)
Mean BAC calculated assuming an
equal number of participants were
randomized to each group
Mean BAC calculated assuming an
equal number of participants were
randomized to each group
Confidence intervals calculated based
on P-value. Mean BAC calculated
assuming an equal number of
participants were randomized to
each group
Confidence intervals calculated based
on P-value. Mean BAC calculated
assuming an equal number of
participants were randomized to
each group
Mean difference calculated from means
of alcohol and placebo groups
assuming equal variance of means
Mean difference calculated from means
of alcohol and placebo groups
assuming equal variance of means
Linear regression compares alcohol
condition versus placebo and control
2.2 (0.6–3.8)
9.7 (-10.2 to 29.6)
Confidence intervals calculated based
on P-value
Excluded from meta-analysis due to
insufficient statistical information
Comments
2.1 (0.0–4.2)
5.7 (0.2–11.1)
Not significant
but unstated
7.7 (0.0–15.4)
Mean increase (as a % of
the scale) per 0.1 mg/ml
increase in BAC
Table 1 Summary of alcohol risk intentions studies that analyzed the relationship between BAC and likelihood of not using a condom through a randomized controlled trial.
Alcohol and intention for unprotected sex
55
Addiction, 107, 51–59
56
Jürgen Rehm et al.
%
Study
Linear
ID
Regression Beta (95% CI) Weight
Abbey et al. (2005)
0.08 (0.00, 0.15)
5.67
Davis et al. (2007)
0.06 (0.00, 0.11)
8.66
George et al. (2009)
0.02 (-0.00, 0.04)
16.49
George et al. (2009)
0.02 (0.01, 0.04)
17.88
Kruse et al. (2005)
0.10 (-0.10, 0.30)
1.10
Kruse et al. (2005)
0.17 (-0.07, 0.40)
0.81
Maisto et al. (2004)
0.10 (-0.01, 0.21)
3.23
Norris et al. (2009)
0.04 (0.01, 0.08)
12.92
Stoner et al. (2007)
0.04 (-0.09, 0.16)
2.50
Ebel-Lam et al. (2009)
0.29 (0.17, 0.41)
2.90
Schacht et al. (2010)
0.05 (0.02, 0.08)
14.93
Cho et al. (2010)
0.04 (0.01, 0.08)
12.92
Overall (I-squared = 61.4%, P = 0.003)
0.05 (0.03, 0.07)
100.00
NOTE: Weights are from random effects analysis
-0.405
0
0.405
0.15
Standard error
0.1
0.05
0
Figure 2 Forest plot of the 12 studies used in the meta-analysis and the weighted point estimates. The size of the box around the point
estimate is representative of the weight of the estimate in calculating the aggregated point estimate; CI: confidence interval
-0.2
-0.1
0
0.1
Point estimate
to 0.10 mg/ml this results in an increased perceived
likelihood of engaging in unprotected sex by 0.29% compared to what they perceived it as being when they were
at a BAC of 0 mg/ml. Before we discuss the implications of
these findings, the potential weaknesses associated with
this analysis should be mentioned.
© 2011 The Authors, Addiction © 2011 Society for the Study of Addiction
0.2
0.3
Figure 3 Funnel plot of the 12 studies
used in the meta-analysis with pseudo
95% confidence intervals. An Egger
weighted regression line was plotted and
indicates a right skew in the data
Most importantly, this investigation does not focus on
actual condom use, but instead examines the intentions
to use condoms. By focusing on intentions, rather than
behavior, it leaves open the possibility that in real-life situations the effect of alcohol on the incidence of new HIV
infections could be diminished by planned precautions
Addiction, 107, 51–59
Alcohol and intention for unprotected sex
(e.g. asking a friend to watch out for oneself). The combination of planned precautions with social influence and
structured behavioral interventions may be an effective
multi-level intervention strategy for preventing new HIV
infections, as the magnitude of the relationship between
alcohol consumption and the intention to have unprotected sex may be dependent on other factors [29].
However, given the high experimental realism of most
studies [30], as well as the reports on actual behaviors in
situations which could lead to unsafe sex [31], this possibility may be true in some instances but probably does not
pertain to the typical cases. It is likely that the underlying
cognitive processes that are undertaken are similar in
experimental settings as in real-world alcohol-related settings, suggesting that even in these ‘artificial’ conditions
under which intentions are being measured, alcohol may
impact cognitive capacity [7], in turn altering the ‘in-themoment’ risky behavioral intentions that may result. This
line of reasoning is supported further through investigations on generalized executive functioning and HIV risk
behavior, which have demonstrated significant associations between diminished planning and problem-solving
capabilities and risky behaviors, such as sharing injection
equipment for illicit drugs [e.g. 32,33]. Risk intentions
may thus serve as a valid surrogate of condom-related
behaviors that occur in real-world sexual encounters
[17–19].
Secondly, the reasoning that alcohol use is an independent risk factor for HIV incidence further assumes
that unsafe sex is indeed linked to HIV. The overwhelming research evidence supports this assumption (see [34]
for an overview). Additionally, as unsafe sex is also
linked to various other STIs [2], alcohol consumption
probably plays a role in the acquisition of these infections as well.
Because alcohol consistently had an effect on intentions in experimentally controlled settings, the argument
that personality factors explain fully the association
between alcohol consumption and unsafe sex, or the
association between alcohol consumption and HIV incidence, can be ruled out (e.g. [35]). This does not preclude,
however, that such factors may codetermine the magnitude of these relationships or the effects of the factors
associated with the context of alcohol consumption. For
instance, being in a bar-like atmosphere where there may
be novel sex partners may increase the probability of
engaging in unsafe sex.
The BAC in this study was never greater than
0.10 mg/ml and, thus, the results are limited to BAC
levels between 0.00 and 0.10 mg/ml. Capacity and functioning have been observed to decrease further where
BAC is above 0.10 mg/ml [7,36], and the effect of BAC
above 0.10 mg/ml on intentions and behavior may not
be linear.
© 2011 The Authors, Addiction © 2011 Society for the Study of Addiction
57
The studies included in the analysis are all from North
America, with all samples comprised of young men and
women, either from a university setting or a community
setting. Thus, the magnitude of the association may be
different in other age groups or populations.
Additionally, our study was limited by the exclusion of
studies that did not provide sufficient statistical information on the association between alcohol consumption and
the intent to engage in unprotected sex. Typically, studies
with non-significant results do not give a P-value, variance and/or SE for the association of interest which
typically causes them to be excluded from meta-analyses.
Given that these estimates are not published, the process
of adjusting our overall point estimate for publication
bias takes the exclusion of these studies into account.
Overall, in addition to the literature on the association
of alcohol use and HIV/STI [1,3,4] [2], we found evidence
on potential pathways explaining this association. Thus,
alcohol impacted on intentions about unsafe sex with a
clear dose–response relationship. This may, in large part,
be explained by its effect on cognitive functioning.
As alcohol affects detrimentally both the innate and
acquired immune system [37,38], many indications
point towards an important role of alcohol in the incidence of HIV and other STIs. Given the high prevalence of
alcohol consumption around the world [39,40], these
findings have potential public health implications. In this
context, both for scientific and public health reasons,
studies varying alcohol consumption experimentally
using proven effective interventions in at risk groups with
later measurement of incidence of HIV and STI would be
advisable [41,42].
Declaration of interests
Financial support for this study was provided to the
first author listed above by the National Institute for
Alcohol Abuse and Alcoholism (NIAAA) with contract
no. HHSN267200700041C to conduct the study entitled
‘Alcohol- and Drug-attributable Burden of Disease and
Injury in the US’. In addition, the first and last author
received a salary and infrastructure support from the
Ontario Ministry of Health and Long-Term Care. The
authors have declared that no competing interests exist.
References
1. Baliunas D., Rehm J., Irving H., Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus
infection: a meta-analysis. Int J Public Health 2010; 55:
159–66.
2. Cook R. L., Clark D. B. Is there an association between
alcohol consumption and sexually transmitted diseases?
A systematic review. Sex Transm Dis 2005; 32: 156–64.
3. Fisher J. C., Bang H., Kapiga S. H. The association between
HIV infection and alcohol use: a systematic review and
Addiction, 107, 51–59
58
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
Jürgen Rehm et al.
meta-analysis of African studies. Sex Transm Dis 2007; 34:
856–63.
Kalichman S. C., Simbayi L. C., Kaufman M., Cain D., Jooste
S. Alcohol use and sexual risks for HIV/AIDS in subSaharan Africa: systematic review of empirical findings.
Prev Sci 2007; 8: 141–51.
Dingle G. A., Oei T. P. Is alcohol a cofactor of HIV and AIDS?
Evidence from immunological and behavioral studies.
Psychol Bull 1997; 122: 56–71.
O’Leary A., Hatzenbuehler M. Encyclopedia of drugs,
alcohol and addictive behavior. In: Carson-Dewitt R., editor.
Alcohol and AIDS. New York: Macmillan; 2009, p. 104–11.
Steele C., Josephs R. Alcohol myopia: its prized and dangerous effects. Am Psychol 1990; 45: 921–33.
Shuper P. A., Neuman M., Kanteres F., Baliunas D., Joharchi
N., Rehm J. Causal considerations on alcohol and HIV/
AIDS—a systematic review. Alcohol Alcohol 2010; 45: 159–
66.
Halpern-Felsher B. L., Millstein S. G., Ellen J. M. Relationship
of alcohol use and risky sexual behavior: a review and
analysis of findings. J Adolesc Health 1996; 19: 331–6.
Leigh B. C., Stall R. Substance use and risky sexual behavior
for exposure to HIV. Issues in methodology, interpretation,
and prevention. Am Psychol 1993; 48: 1035–45.
Shuper P. A., Joharchi N., Irving H., Rehm J. Alcohol as a
correlate of unprotected sexual behavior among people
living with HIV/AIDS: review and meta-analysis. AIDS
Behav 2009; 13: 1021–36.
Weinhardt L., Carey M. Does alcohol lead to sexual risk
behavior? Findings from event-level research. Annu Rev Sex
Res 2000; 11: 125–57.
Woolf S. E., Maisto S. A. Alcohol use and risk of HIV infection among men who have sex with men. AIDS Behav 2009;
13: 757–82.
Hendershot C. S., George W. H. Alcohol and sexuality
research in the AIDS era: trends in publication activity,
target populations and research design. AIDS Behav 2007;
11: 217–26.
National Institute on Alcohol Abuse and Alcoholism.
2005. National Advisory Council on Alcohol Abuse and
Alcoholism—Recommended Council Guidelines on Ethyl
Alcohol Administration in Human Experimentation.
Bethesda, MD: National Institute on Alcohol Abuse
and Alcoholism. Available at: http://www.niaaa.nih.gov/
Resources/ResearchResources/job22.htm (accessed 1
August 2010; archived by Webcite at http://www.
webcitation.org/61tJyRA6F).
World Cancer Research Fund/American Institute for
Cancer Research (AICR). Food, Nutrition, Physical Activity,
and the Prevention of Cancer: A Global Perspective. Washington, DC: AICR; 2007.
Sheeran P., Abraham C., Orbell S. Psychosocial correlates of
heterosexual condom use: a meta-analysis. Psychol Bull
1999; 125: 90–132.
Sheeran P., Orbell S. Do intentions predict condom use?
Meta-analysis and examination of six moderator variables.
Br J Soc Psychol 1998; 37: 231–50.
Albarracín D., Johnson B. T., Fishbein M., Muellerleile P. A.
Theories of reasoned action and planned behavior as
models of condom use: a meta-analysis. Psychol Bull 2001;
127: 142–61.
Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gotzsche P.
C., Ioannidis J. P. et al. The PRISMA statement for reporting
systematic reviews and meta-analyses of studies that
© 2011 The Authors, Addiction © 2011 Society for the Study of Addiction
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6: 7.
Pagano M., Gauvreau K. Principles of Biostatistics. Pacific
Grove, USA: Brooks/Cole; 2000.
DerSimonian R., Laird N. Meta-analysis in clinical trials.
Control Clin Trials 1986; 7: 177–88.
Begg C. B., Mazumdar M. Operating characteristics of a
rank correlation test for publication bias. Biometrics 1994;
50: 1088–101.
Duval S. J., Tweedie R. L. Trim and fill: a simple funnel plotbased method of testing and adjusting for publication bias
in meta-analysis. Biometrics 2000; 56: 276–84.
StataCorp. 2009. Statistical Software: Release 11.0. College
Station, TX: Stata Corporation.
Abbey A., Saenz C., Buck P. O., Parkhill M. R., Hayman L. W.
J. The effects of acute alcohol consumption, cognitive
reserve, partner risk, and gender on sexual decision making.
J Stud Alcohol 2006; 67: 113–21.
Ebel-Lam A. P., MacDonald T. K., Zanna M. P., Fong G. T.
An experimental investigation of the interactive effects of
alcohol and sexual arousal on intentions to have unprotected sex. Basic Appl Soc Psych 2009; 31: 226–33.
Egger M., Smith G. D., Schneider M., Minder C. Bias in metaanalysis detected by a simple, graphical test. BMJ 1997;
315: 629–34.
Kalichman S. Social and structural HIV prevention in
alcohol serving establishments review of international
interventions across populations. Alcohol HIV/AIDS 2010;
33: 184–94.
Aronson E., Ellsworth P., Carlsmith J. M., Gonzales M.
Methods of Research in Social Psychology, 2nd edn. New York:
McGraw-Hill; 1990.
MacDonald T. K., Zanna M. P., Fong G. T. Why common
sense goes out the window: effects of alcohol on intentions to use condoms. Pers Soc Psychol Bull 1996; 22: 763–
75.
Severtson S. G., Mitchell M. M., Mancha B. E., Latimer W. W.
The association between planning abilities and sharing
injection drug use equipment among injection drug users in
Baltimore, MD. J Subst Use 2009; 14: 325–33.
Mitchell M. M., Severtson S. G., Latimer W. W. Interaction of
cognitive performance and knowing someone who has died
from AIDS on HIV risk behaviors. AIDS Educ Prev 2007; 19:
289–97.
Slaymaker E., Walker N., Zaba B., Collumbien M. Unsafe sex.
In: Ezzati M., Lopez A. D., Rodgers A., Murray C. J. L., editors.
Comparative Quantification of Health Risks. Global and
Regional Burden of Disease Attributable to Selected Major
Risk Factors. Geneva: World Health Organization; 2004,
p. 1177–254.
Pearl J. Causality: Models, Reasoning and Inference.
Cambridge, UK: Cambridge University Press; 2009.
Giancola P. R. Executive functioning: a conceptual framework for alcohol-related aggression. Exp Clin Psychopharmacol 2000; 8: 576–97.
Friedman H., Newton C., Klein T. W. Microbial infections,
immunomodulation, and drugs of abuse. Clin Microbiol Rev
2003; 16: 209–19.
Friedman H., Pros S., Klein T. W. Addictive drugs and their
relationships with infectious diseases. FEMS 2006; 47:
330–42.
World Health Organization. Global status report on alcohol
and health. Geneva, Switzerland: World Health Organization; 2011.
Addiction, 107, 51–59
Alcohol and intention for unprotected sex
40. Shield K., Rehm M., Patra J., Rehm J. Global and country
specific adult per capita consumption of alcohol, 2008.
Sucht 2011; 57: 99–117.
41. Kalichman S. C., Simbayi L. C., Vermaak R., Cain D., Jooste
S., Peltzer K. HIV/AIDS risk reduction counseling for
alcohol using sexually transmitted infections clinic patients
in Cape Town South Africa. J Acquir Immune Defic Syndr
2007; 44: 594–600.
42. Kalichman S. C., Simbayi L. C., Vermaak R., Cain D., Smith
G., Mthebu J. et al. Randomized trial of a community-based
alcohol-related HIV risk-reduction intervention for men and
women in Cape Town South Africa. Ann Behav Med 2008;
36: 270–9.
43. Abbey A., Saenz C., Buck P. O. The cumulative effects
of acute alcohol consumption, individual differences and
situational perceptions on sexual decision making. J Stud
Alcohol 2005; 66: 82–90.
44. Cho Y. H., Span S. A. The effect of alcohol on sexual risktaking among young men and women. Addict Behav 2010;
35: 779–85.
45. Davis K. C., Hendershot C. S., George W. H., Norris J.,
Heiman J. R. Alcohol’s effects on sexual decision making: an
integration of alcohol myopia and individual differences.
J Stud Alcohol Drugs 2007; 68: 843–51.
46. George W. H., Davis K. C., Norris J., Heiman J. R., Stoner
S. A., Schacht R. L. et al. Indirect effects of acute alcohol
intoxication on sexual risk-taking: the roles of subjective
and physiological sexual arousal. Arch Sex Behav 2009; 38:
498–513.
© 2011 The Authors, Addiction © 2011 Society for the Study of Addiction
59
47. Kruse M. I., Fromme K. Influence of physical attractiveness and alcohol on men’s perceptions of potential sexual
partners and sexual behavior intentions. Exp Clin Psychopharmacol 2005; 13: 146–56.
48. Agocha V. B., Cooper M. L. Risk perceptions and safer-sex
intentions: does a partner’s physical attractiveness undermine the use of risk-relevant information? Pers Soc Psychol
Bull 1999; 25: 746–59.
49. Maisto S. A., Carey M. P., Carey M. P., Carey K. B., Gordon C.
M., Schum J. L. et al. The relationship between alcohol and
individual differences variables on attitudes and behavioral
skills relevant to sexual health among heterosexual young
adult men. Arch Sex Behav 2004; 33: 571–84.
50. Helweg-Larsen M., Collins B. E. The UCLA Multidimensional
Condom Attitudes Scale: documenting the complex determinants of condom use in college students. Health Psychol
1994; 13: 224–37.
51. Norris J., Stoner S. A., Hessler D. M., Zawacki T. M., George
W. H., Morrison D. M. et al. Cognitive mediation of alcohol’s
effects on women’s in-the-moment sexual decision making.
Health Psychol 2009; 28: 20–8.
52. Stoner S. A., George W. H., Peters L. M., Norris J. Liquid
courage: alcohol fosters risky sexual decision-making in
individuals with sexual fears. AIDS Behav 2007; 11: 227–
37.
53. Schacht R. L., George W. H., Davis K. C., Heiman J. R., Norris
J., Stoner S. A. et al. Sexual abuse history, alcohol intoxication, and women’s sexual risk behavior. Arch Sex Behav
2010; 39: 898–906.
Addiction, 107, 51–59