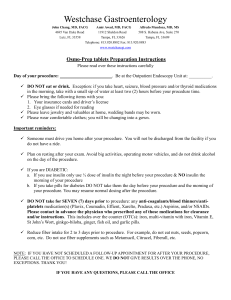
opioid equianalgesic conversion chart
advertisement

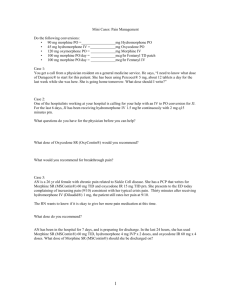
30-60 mg PO q 3-4 hours Initial transdermal dose depends upon daily opioid requirement. 100 mg 10 mg N/A N/A N/A N/A N/A 120 mg 100 mcg 300 mg 20 mg 20 mg 20 mg Vague 300-400 mg 30 mg 30 mg 200 mg Fentanyl patch Oxycodone Hydromorphine Morphine (IR. CR) Opioid (PO doses) 24 hr analgesic requirement (oral doses) 25 ug/hr 50 ug/hr 30-90 mg 90-150 mg 11-33 mg 33-56 mg 45-134 mg 135-224 mg Watch for ibuprofen content: Maximum recommended dose is 3200 mg per 24 hours Watch APAP content: Maximum recommended amount is 4000 mg per 24 hours 5-10 mg PO q 3-4 hours NOT Recommended - Accumulation of toxic metabolite with repetitive dosing in patients with renal dysfunction. Inappropriate in the elderly. Do not exceed 6 tablets (600 mg) in any 24 hour period. 10-20 mg PO q 12 h (Not for PRN dosing) 5-10 mg PO q 3-4 hours PO conversion dose may be less. The ratio can vary considerably and may be as little as 30 mg Morphine = 5 mg Methadone with repetitive dosing. Not recommended 2-4 mg PO q 3-4 hours 1.5 mg 7.5 mg 15-30 PO q 12h (Not for PRN dosing) 5-10 mg PO q 3-4h N/A 10 mg USUAL ORAL STARTING DOSE FOR MODERATE TO ADULTS (ELDERLY MAY REQUIRE lower doses) SEVERE PAIN IN 30 mg 30 mg APPROXIMATE EQUIANALGESIC DOSAGE Oral Parenteral This list is not inclusive of all oral agents but limited to what is available at Aspirus Wausau Hospital Pharmacy. Quick conversion: Percocet 2 tabs q4h = 2 – Hydrocodone/APAP 7.5/500 tablets q4h = 15 mg Morphine IR tablets q4h = 45 mg MS Contin q12 = 1.25 mg/hr IV Morphine infusion = Fentanyl 25 mcg/hr transdermal patch q72hrs. Meperidine is NOT an option for oral dosing. Meperidine is not recommended for multiple dosing or chronic use. Meperidine should be avoided in patients with renal dysfunction, history of seizures, or the elderly. Need to provide PRN medication while starting and adjusting transdermal dosing. After patch is removed the serum levels drop 50% in 17 hours. Fentanyl (Sublimaze®) Duragesic® Transdermal patch 25, 50, 75, 100 mcg/hr Codeine 15, 30, and 60 mg tabs 15 mg/5 ml oral soln. Codeine/APAP (Tylenol # 2, 3, or 4) Hydrocodone/ibuprofen (Vicoprofen®) 7.5 mg/200 mg Hydrocodone/APAP (various- Vicodin, Lortab, Lorcet, Norco) 5 mg/500 mg 7.5 mg/500 mg 10 mg/325 mg 2.5 mg/167 mg per 5 ml liquid Propoxyphene/APAP (Darvocet-N 100®) 100 mg/650 mg Oxycodone controlled release tablets (Oxycontin®) 10 , 20, 40, and 80 mg tablets Oxycodone/ASA 5 mg/325 mg tablet (Percodan®) Oxycodone/APAP 5 mg/325 mg (Percocet®) 5 mg/325 mg per 5 ml liquid (Roxicet® liquid) Oxycodone IR Roxycodone, Percolone®, OxyIR® 5 mg immediate release tablets Methadone (Dolophine®) 10 mg tablets Meperidine (Demerol®) Hydromorphone tablets (Dilaudid®) 2 & 4 & 8 mg tablets Morphine sulfate controlled release (MS Contin®) 15, 30, 60,100 mg tablets Morphine sulfate oral solution 2 & 4 mg/ml 10 mg immediate release tabs (IR) 20 mg/ml concentrated soln DRUG Medication listed are oral dosages forms available at Aspirus Wausau Hospital Opioid Equianalgesic Conversion chart Aspirus Wausau Hospital 11/2003 OPIOID EQUIANALGESIC CONVERSION CHART Aspirus Wausau Hospital DECEMBER 2004 PHARM-033 mmk 12/04 INSTRUCTION FOR USE OF EQUIANALGESIC CONVERSION CHART* DON’T PANIC - YOU CAN DO THIS!! 1. Calculate the total amount of narcotic used by the patient in the last 24 hours. 2. Set up ratio using values from the table for new medication or change in route of administration. Note: all boxes are equal on chart (vertically and horizontally). X = total mg of desired medication/24 hours = mg of new medication from equivalency chart Total mg of present medication in 24 hours mg of present medication from equivalency chart 3. Solve for X**. 4. Calculate new medication dosage into appropriate frequency for a 24-hour period. Example: divide by 6 for q 4 hours, divide by 4 for q 6 hours and so on. 5. Figure breakthrough dose by 5 to 15% of the total daily dose. 6. Remember stimulant laxative (e.g. Senokot, Senna). Example 1 • Mrs. D, 45 years old. Breast cancer, metastatic to bone. Comfortable on MSO4 at 6 mg/hr IV. • Convert to PO medication before discharge. 1. Figure out total 24 hour daily dose of IV morphine. 6 mg/hr IV x 24 hours = 144 mg morphine IV 2. Set up ratio of IV to PO morphine from table = 30 mg PO MSO4 X mg/day PO MSO4 144 mg/day IV MSO4 10 mg IV MSO4 3. Solve for X (144 x 30/10 = 442) X = 442 mg/day PO morphine 4. Divide by 2 for BID formulation of extended release morphine or divide by 6 for immediate release morphine administered every 4 hours. Sig: 200 mg extended release morphine PO BID or 70 mg immediate release morphine PO q 4 hours. 5. Also prescribe breakthrough doses of 5% to 15% of total daily dose. Sig: 20–60 mg immediate release morphine PO q 1 hour PRN. 6. Remember stimulant laxative. Example 2 • Mr. B, 67 years old. Severe left hip osteoarthritis. POD #3, S/P total hip arthroplasty. • Comfortable on PCA MSO4 1mg q 6 minutes with 30 mg q 4 hours lockout.. • Over past 24 hours, patient required 18 mg IV MSO4. • Convert to PO hydrocodone. 1. Figure out total 24 hour dose of IV morphine. From PCA records patient received = 18 mg IV MSO4 24 hrs 2. Set up ratio of IV MSO4 to PO Hydrocodone using equianalgesic table. 18 mg IV MSO4 x 30 mg PO Hydrocodone 10 mg IV MSO4 = 54 mg PO Hydrocodone per 24 hours 3. Divide by 6 for q 4 hour dosing. 54 mg PO hydrocodone divide by 6 = 9 mg hydrocodone q 4 hours 4. Consider hydrocodone/APAP options: 10 mg/325 mg PO q 4 hours = 60 mg/24 hours or 7.5 mg/500 PO q 4 hours = 45 mg/24 hours 5. Remember stimulant laxative. *When converting to methadone, these instructions generally do not apply. Recommend consulting a pharmacist or physician experienced in converting to methadone. **When changing to a different opiate (not route) in patients requiring a narcotic analgesic chronically may need to reduce the calculated dose by 25 to 50% (or more) due to the lack of cross tolerance between different opiates.