Review article
Genomic Medicine
W. Gregory Feero, M.D., Ph.D., and Alan E. Guttmacher, M.D., Editors
Genomics and the Eye
Val C. Sheffield, M.D., Ph.D., and Edwin M. Stone, M.D., Ph.D.
From the Departments of Pediatrics (V.C.S.)
and Ophthalmology and Visual Sciences
(V.C.S., E.M.S.), Howard Hughes Medical
Institute, University of Iowa Carver College
of Medicine, Iowa City. Address reprint requests to Dr. Stone at the University of Iowa
Institute for Vision Research, 375 Newton
Rd., Iowa City, IA 52242, or at edwin-stone@
uiowa.edu.
This article (10.1056/NEJMra1012354) was
updated on May 19, 2011, at NEJM.org.
N Engl J Med 2011;364:1932-42.
Copyright © 2011 Massachusetts Medical Society.
T
he eye has had a pivotal role in the evolution of human genomics. At least 90% of the genes in the human genome are expressed in one or
more of the eye’s many tissues and cell types at some point during a person’s
life. Consistent with this impressive genomic footprint is the observation that about
a third of entries in the Online Mendelian Inheritance in Man database for which a
clinical synopsis is provided include a term that refers to the structure or function of
the eye.1 Moreover, the phenotypic effects of even small genetic variations are made
readily apparent by the many layers of amplification in the human visual system. For
example, a single-nucleotide change in PAX6 can cause an anatomic abnormality of
the macula less than a millimeter in diameter that results in noticeably reduced visual acuity and nystagmus.2
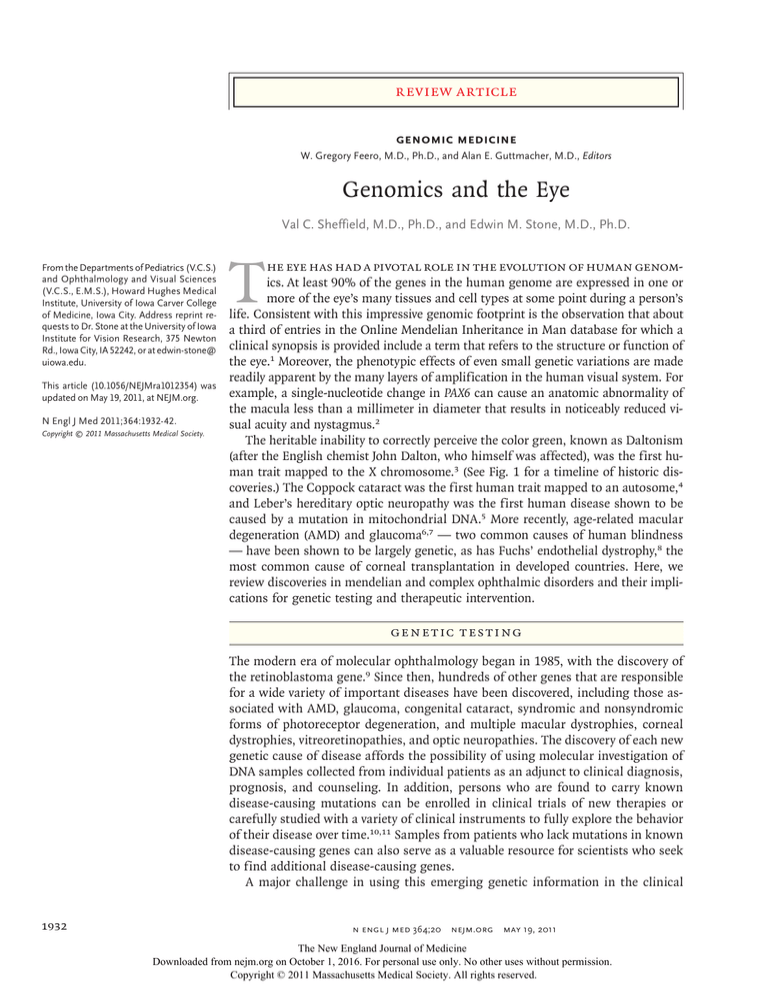
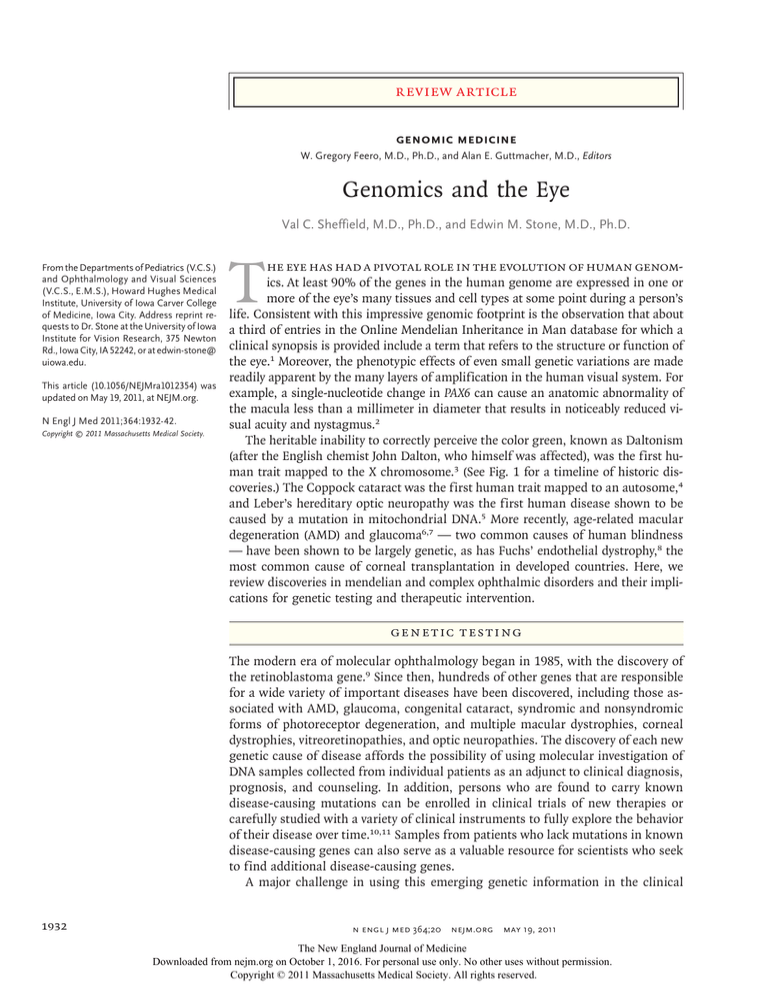
The heritable inability to correctly perceive the color green, known as Daltonism
(after the English chemist John Dalton, who himself was affected), was the first human trait mapped to the X chromosome.3 (See Fig. 1 for a timeline of historic discoveries.) The Coppock cataract was the first human trait mapped to an autosome,4
and Leber’s hereditary optic neuropathy was the first human disease shown to be
caused by a mutation in mitochondrial DNA.5 More recently, age-related macular
degeneration (AMD) and glaucoma6,7 — two common causes of human blindness
— have been shown to be largely genetic, as has Fuchs’ endothelial dystrophy,8 the
most common cause of corneal transplantation in developed countries. Here, we
review discoveries in mendelian and complex ophthalmic disorders and their implications for genetic testing and therapeutic intervention.
Gene t ic Te s t ing
The modern era of molecular ophthalmology began in 1985, with the discovery of
the retinoblastoma gene.9 Since then, hundreds of other genes that are responsible
for a wide variety of important diseases have been discovered, including those associated with AMD, glaucoma, congenital cataract, syndromic and nonsyndromic
forms of photoreceptor degeneration, and multiple macular dystrophies, corneal
dystrophies, vitreoretinopathies, and optic neuropathies. The discovery of each new
genetic cause of disease affords the possibility of using molecular investigation of
DNA samples collected from individual patients as an adjunct to clinical diagnosis,
prognosis, and counseling. In addition, persons who are found to carry known
disease-causing mutations can be enrolled in clinical trials of new therapies or
carefully studied with a variety of clinical instruments to fully explore the behavior
of their disease over time.10,11 Samples from patients who lack mutations in known
disease-causing genes can also serve as a valuable resource for scientists who seek
to find additional disease-causing genes.
A major challenge in using this emerging genetic information in the clinical
1932
n engl j med 364;20 nejm.org may 19, 2011
The New England Journal of Medicine
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
genomic medicine
domain is the gap that exists between the amount
of information that is needed to convincingly
demonstrate a pathogenic role of a given gene
in a group of research subjects and the amount
of information that is needed to reliably assert
that a given genetic variation is responsible for
a disease in an individual patient. Some of the
factors that are responsible for this gap include
the large number of non–phenotype-altering variations scattered throughout many genes, the wide
variety of types of true disease-causing mutations
460–322 B.C.E.
Hippocrates and Aristotle study
familial transmission of ocular traits
1865
Mendel
experiments
with plant
hybridization
1869
Leber describes
congenital
amaurosis
1800s
1900s
(e.g., missense, nonsense, splice-site, promoterinactivation, and copy-number variation) (see Glossary), the genetic differences among different
ethnic groups, the genetic heterogeneity of many
phenotypes (e.g., retinitis pigmentosa can be
caused by a mutation in any one of more than 40
genes), and the clinical variation among patients
with similar genotypes.
Because all genetic variations are not equally
likely to cause disease, some investigators have
suggested methods for taking this uncertainty
2011
Ranibizumab and bevacizumab are shown to be essentially equivalent in neovascular AMD
1911
Thomas Morgan identifies the chromosome
as the physical repository of genetic material
1953
Structure of DNA is deduced
Color blindness is the first human trait
mapped to the X chromosome
1997
First human
glaucoma gene, MYOC,
is identified
1963
Coppock cataract
is the first human trait
mapped to an autosome
1917
Ophthalmology is the first
medical specialty to create its
own assessment board
1910s
1920s
1930s
1847
Charles Babbage
invents the
ophthalmoscope
Stargardt’s disease
gene, ABCA4, is identified
1971
Folkman recognizes
therapeutic implications of
tumor angiogenesis factor
1940s
1950s
1960s
1970s
1980s
1990s
2000s
2010s
1983
Polymerase chain reaction is introduced
1985
First human cancer gene, retinoblastoma, is cloned
1987
Rhodopsin is the first gene associated with a retinal degenerative disease
1989
Leber’s hereditary optic neuropathy is the first human disease
shown to be caused by a mutation of mitochondrial DNA
2000
Gene therapy for canine blindness caused by Leber’s congenital amaurosis is successful
2004
Bevacizumab is approved for use in colon cancer
2005
AMD is the first eye disease to yield a positive genomewide association
2006
Off-label bevacizumab is shown to be effective in neovascular AMD
Ranibizumab is approved for use in neovascular AMD
2007
First gene-replacement therapy for a human eye disease, Leber’s congenital amaurosis, is successful
Figure 1. Timeline of Landmarks in Ophthalmic Genetics.
AMD denotes age-related macular degeneration.
COLOR FIGURE
Draft 5
Author
Fig #
5/02/11
Stone
1
Title
n engl j med 364;20
nejm.org
may 19, 2011
1933
ME
DE
Artist
Phimister
Knoper
The New England Journal of Medicine
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission. AUTHOR PLEASE NOTE:
Figure has been redrawn and type has been reset
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
Please check carefully
Issue date
5/19/11
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Glossary
Allele: One of two or more versions of a genetic sequence at a particular location in the genome.
Autosome: All the chromosomes except for the sex chromosomes and the mitochondrial chromosome.
Chaperone complex: An oligomeric protein that assists in the folding, unfolding, assembly, or disassembly of other
macromolecular structures without being permanently incorporated into the assisted structures.
Codon: A three-nucleotide sequence of DNA or RNA that specifies a single amino acid.
Copy-number variation: Variation from one person to the next in the number of copies of a particular gene or DNA sequence. The full extent to which copy-number variation contributes to human disease is not yet known.
De novo mutation: Any DNA sequence change that occurs during replication, such as a heritable gene alteration occurring in a family for the first time as a result of a DNA sequence change in a germ cell or fertilized egg.
Genomewide association study: An approach used in genetics research to look for associations between typically hundreds of thousands of specific genetic variations (most commonly single-nucleotide polymorphisms) and particular diseases.
Linkage analysis: An approach to the discovery of the genetic basis of a disease that correlates the pattern of disease
inheritance within families with specific alleles of genetic markers of known location.
Locus: The specific chromosomal location of a gene or other DNA sequence of interest.
Loss-of-function mutation: A mutation that decreases the production or function of a protein (or does both).
Missense mutation: The alteration of a single DNA nucleotide so that the resulting codon specifies a different amino acid.
Nonsense mutation: The alteration of a single DNA nucleotide so that the resulting codon signals a termination of
translation, thus leading to truncation of the encoded protein.
Penetrance: The likelihood that a person carrying a particular genetic variant will have a detectably altered phenotype.
Population attributable risk: The difference in the rate of disease between a population that is exposed to a given factor
and one that is not. The population attributable risks of individual factors that contribute to a single clinical entity,
such as age-related macular degeneration, often total more than 100% because the disease in a specific patient
may be caused by a combination of factors that are counted more than once when individual population attributable risks are summed.
Promoter-inactivation mutation: A genetic variation in the promoter of an otherwise normal gene that results in a dramatic reduction in gene expression.
Single-nucleotide polymorphism: A single-nucleotide variation in a genetic sequence, a common form of variation in
the human genome.
Splice-site mutation: A sequence variation at or near an intron–exon boundary that perturbs normal splicing of the adjacent intron.
into account in a standardized fashion when interpreting the results of genetic testing.12 The
advent of whole-exome sequencing as a diagnostic tool accentuates the need for this type of
probabilistic interpretation, because every person
carries several recessive disease-causing mutations
that would be incidental and medically irrelevant
to any disease that they might have in their lifetimes. For example, approximately 1 in 30 Europeans is heterozygous for the deletion of codon
508 in the gene that is associated with cystic fibrosis.13 The ability to distinguish between newly
encountered benign variants and those that might
confer risk is central to the task of interpreting
genetic data, especially those generated by large
data sets, such as the whole genome of an individual. As in all of medicine, a genetic test result
is more likely to be meaningful when it is accom1934
panied by a robust pretest hypothesis. Thus, the
growth of molecular ophthalmology has increased
the need for experienced clinicians who can place
the observed genetic variations in the correct clinical context.
Mendel i a n Disor der s
According to the World Health Organization, the
most common causes of blindness across the globe
are cataracts, glaucoma, AMD, corneal opacity,
diabetic retinopathy, infections, and parasitic diseases.14 Genetic factors play a role in many of
these conditions, sometimes in the form of relatively rare, high-penetrance monogenic diseases
and sometimes in the form of more common
conditions caused by the complex interplay of
multiple genes and the environment. From the
n engl j med 364;20 nejm.org may 19, 2011
The New England Journal of Medicine
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
genomic medicine
many known monogenic eye disorders, we have
selected three to illustrate the wide variety of
pathophysiological mechanisms involved in human blindness.
Mutation in ABCA4 — identified by Allikmets
in 1997 as a cause of Stargardt’s disease15 — is
one of the most important causes of monogenic
retinal disease in humans. ABCA4 is an enzyme
that flips a retinoid intermediate of the visual
cycle known as N-retinylidene-phosphatidylethanolamine (N-retPE) from the inner leaflet to the
outer leaflet of the photoreceptor outer segment
disk membrane16 (Fig. 2, and interactive graphic,
available with the full text of this article at NEJM
.org). Mutations in ABCA4 result in an intradiscal
accumulation of N-retPE, which in turn leads to
the formation of a toxic, insoluble bisretinoid
known as A2E. Variations in ABCA4 are responsible
for more than 95% of cases of Stargardt’s disease,
30% of cases of cone–rod dystrophy, and 8% of
cases of autosomal recessive retinitis pigmentosa.17 This range of phenotypes results from the
interplay of at least three factors: the degree of
residual enzymatic function associated with a
given genotype, the fact that cones are more readily harmed than rods by the accumulation of A2E,
and the fact that injury to the retinal pigment
epithelium results in secondary injury to both
rods and cones.10 ABCA4 mutations with a relatively mild effect result in the accumulation of
A2E within and beneath the retinal pigment epithelium, those with an intermediate effect result
in a direct injury to photoreceptors that is somewhat cone-selective, and those with the most severe effect result in injury to both cone and rod
photoreceptors.17
A second example, mutation in MYOC in autosomal dominant juvenile-onset primary open-angle
glaucoma, involves mistrafficking of a normally
secreted trabecular meshwork protein to the peroxisome. Linkage analysis of several large families mapped the causal mutations to the long arm
of chromosome 1,18 and further genetic dissection of this locus revealed mutations in MYOC as
the cause of the disease.19 Certain missense mutations are associated with very high intraocular
pressures and early onset of vision loss, whereas
a nonsense mutation at codon 368 is associated
with milder disease and a later onset,20 an unexpected finding because nonsense mutations typically have a more severe effect on protein integrity
than do missense mutations. It was later discov-
ered that the missense mutations in MYOC cause
the myocilin protein to misfold, with consequent
unmasking of an otherwise cryptic signal that
targets myocilin to the peroxisome.21 The resulting intracellular retention of myocilin causes injury to the cells that make up the trabecular
meshwork, which in turn reduces the outflow of
aqueous humor. The elevated intraocular pressure
resulting from this reduced outflow causes injury to the optic nerve. MYOC mutations have been
shown to be involved in approximately 4% of all
cases of primary open-angle glaucoma, including
adult-onset disease.19
A third example illustrates the phenomenon
of genetic heterogeneity: mutations in at least 14
genes cause a clinical syndrome known as the
Bardet–Biedl syndrome (BBS). BBS is a pleiotropic
autosomal recessive disorder that is characterized
by the combination of retinitis pigmentosa, obesity, polydactyly, congenital heart defects, renal
abnormalities, hypogenitalism, cognitive impairment, and an increased incidence of hypertension
and diabetes mellitus.22 Patients with BBS present with progressive photoreceptor degeneration
and are usually blind by the third decade of life.
Studies of animal models have shown that proteins that are affected by mutations causing BBS
are components of cilia or serve in intraflagellar
or intracellular transport.23 The fact that the mutation of multiple different genes can be associated with a single pleiotropic phenotype has now
been largely explained by the discovery of two
BBS protein complexes: the BBSome (consisting of
seven BBS proteins), which plays a role in intra­
flagellar transport; and a chaperone complex (con­
sisting of three BBS proteins), which is required
for BBSome assembly (Fig. 3).
An interactive
graphic regarding
ABCA4 mutations
is available at
NEJM.org
C ompl e x Disor der s
Disorders with complex inheritance result from
the interaction of multiple genetic loci and environmental factors such that a mendelian inheritance pattern is not observed. As a result, an allele
contributing to a complex disease has a much
lower penetrance than an allele involved in a single-gene disorder. This fact affects both the manner in which investigators identify such alleles and
the way in which the presence or absence of such
alleles has an effect on the care and counseling
of patients and their families. As a general rule,
linkage analysis of affected families has been
n engl j med 364;20 nejm.org may 19, 2011
The New England Journal of Medicine
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
1935
The
n e w e ng l a n d j o u r na l
more successful in identifying disease-causing alleles in single-gene disorders (e.g., those described
in the previous section), whereas genomewide or
candidate association studies have been more successful in identifying factors involved in complex
diseases, such as AMD, glaucoma, and Fuchs’ endothelial dystrophy. In a counseling context, alleles of single-gene disorders can often be reasonably said to cause disease, whereas alleles that are
involved in complex diseases are more commonly
said to increase the risk of disease.
Three of the most common causes of blindness
— AMD, glaucoma, and Fuchs’ endothelial corneal dystrophy — have both genetic heterogeneity
and genetic complexity, and genomewide association studies have recently revealed clues to the
pathogenicity of all three disorders.
AMD is the leading cause of blindness in developed countries. As the name implies, the
disorder usually affects persons over the age of
60 years and results in loss of macular (central)
vision (Fig. 4). The prevalence of AMD increases
with age, and more than 30% of persons over
the age of 75 years will have some manifestation
of the disease.6 Initial attempts to identify AMD
loci involved screening genes that were known
to cause monogenic macular disease in patients
with AMD and in ethnically matched control subjects.24 Later, the development of cost-effective
high-throughput genotyping made genomewide
association studies possible. Of all diseases studied in this manner, AMD has been one of the
most successful in that it has yielded loci that
contribute a high relative risk. For example, persons who carry a certain variant of the gene encoding complement factor H (CFH)25-28 have a relative risk of AMD that is more than 2.7 times that
of persons without this variant.25,26 A variant at
chromosome 10q26, in the vicinity of three genes
(ARMS2, HTRA1, and PLEKHA1), is also strongly
associated with AMD.29-31 In all, more than a
dozen genes have been linked to AMD.6 Although
these studies are important to the further understanding of the pathophysiological mechanisms
of AMD and may aid in the development of new
therapies, clinical testing for AMD-associated polymorphisms is of little value in the clinical management of AMD at this time. AMD will develop
in only about a third of persons with the highestrisk CFH genotype by the age of 70 years. Thus,
unless and until a safe and effective treatment
specific for CFH-associated AMD is developed,
1936
of
m e dic i n e
Figure 2 (facing page). Retinal Disease Associated with
ABCA4 Mutations.
Panel A shows a series of photographs of the retinas
of patients with progressively decreasing amounts of
ABCA4 function (from left to right), ranging from a normal retina to those of patients with Stargardt’s disease,
cone–rod dystrophy, and retinitis pigmentosa. Panel B
shows the effects of reduced ABCA4 function on fullfield electroretinograms. The relatively mild reduction in
ABCA4 activity in patients with Stargardt’s disease has
little effect on global photoreceptor function. Moderate
loss of ABCA4 function in patients with cone–rod dystrophy has a greater effect on cone photoreceptors than it
does on rods. Complete loss of ABCA4 function in some
patients with retinitis pigmentosa is associated with extensive loss of both cones and rods and a nonrecordable
electroretinogram. Panel C shows the effects of reduced
ABCA4 function on the accumulation of bisretinoid (yellow
symbols) on the inner leaflet of the photoreceptor outer
segment disk membranes. Mild reduction in ABCA4 activity in Stargardt’s disease is associated with some bisretinoid formation; moderate loss of function in cone–rod
dystrophy is associated with intermediate amounts of accumulation; and complete loss of function in retinitis
pigmentosa results in maximal accumulation. Panel D
shows the histopathological effects of reduced ABCA4
activity. In patients with Stargardt’s disease, the rate of
bisretinoid formation in the outer segments is relatively
slow and the photoreceptors are not directly injured. Bisretinoids are delivered to the secondary lysosomes of the
retinal pigment epithelium (RPE) during the normal
phagocytosis of photoreceptor outer segments. Some of
this material accumulates beneath the RPE as accumulations known as pisciform flecks that are visible on ophthalmoscopy. In patients with cone–rod dystrophy, moderate loss of ABCA4 function results in sufficient
accumulation of ­bisretinoids in photoreceptor outer segments to cause some apoptosis of photoreceptors (in
cones more than rods). In patients with retinitis pigmentosa, complete loss of ABCA4 function causes extensive
accumulation of bisretinoids in photoreceptor outer segments, apoptosis of both rod and cone photoreceptors,
and associated RPE thinning.
there will be little clinical benefit in a genetic test
that is less sensitive and specific for the detection
of AMD than a routine eye exam.
Glaucoma is the second leading cause of blindness in the United States and the leading cause of
blindness among blacks. As many as 60 million
people worldwide currently have glaucoma.32 The
most common form of glaucoma in the United
States is primary open-angle glaucoma, which
is characterized by optic-nerve damage and loss
of peripheral visual field. Studies of mendelian
(monogenic) forms of the disorder have implicated two genes (MYOC and OPTN) and mapped the
chromosomal location of an additional 13 genes.33
n engl j med 364;20 nejm.org may 19, 2011
The New England Journal of Medicine
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
genomic medicine
Normal
A
Stargardt’s Disease
Cone–Rod Dystrophy
Retinitis Pigmentosa
B
Rods
Cones
C
ABCA4
Outer
segment
disk
Partially
functional ABCA4
ABCA4 absent
Bisretinoid
Plasma membrane
D
Rods
Cones
RPE
Bisretinoid
Pisciform fleck
However, less than 5% of cases of primary open- proportion of the remaining cases are caused by
Draft 13
angle glaucoma have been attributed to mutations the combined actions of multiple variant genes
Author Stone
in these single genes, which suggests that a large and environmental influences. Each variant
gene
2
Fig #
COLOR FIGURE
5/02/11
Title
n engl j med 364;20 nejm.org may 19, 2011
ME
DE
Artist
Phimister
Knoper
1937
The New England Journal of Medicine
AUTHOR PLEASE NOTE:
Figure has been redrawn and type has been reset
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission.
Please check carefully
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
Issue date 5/19/11
The
n e w e ng l a n d j o u r na l
A
Microtubule
Ciliary
membrane
IFT particle
Kinesin 2
Dynein
Transitional
fiber
Basal body
BBS3
B
BBSome
BBS6/10/12
and CCT
complex
BBS4
BBS8
BBS2
BBS7
BBS9
m e dic i n e
Figure 3. The Bardet–Biedl Syndrome.
Panel A shows the role of seven Bardet–Biedl syndrome
(BBS) proteins (BBS1, 2, 4, 5, 7, 8, and 9) that along
with BBIP10 form a protein complex known as the
BBSome. The BBSome plays a role in cargo transport to
and out of the cilia and potentially to other membrane
compartments. BBS3, which is not part of the BBSome,
is required for BBSome transport to cilia. Panel B shows
the known physical interactions of the components of
the BBSome protein complex, as determined by coimmunoprecipitation experiments. The formation of
the BBSome requires a second complex, which includes
proteins BBS6, 10, and 12. CCT denotes chaperonincontaining T-complex polypeptide, and IFT intraflagellar
transport.
Cilium
Cargo
of
BBS1
BBS5
probably contributes a relatively small risk of primary open-angle glaucoma on its own but in unfavorable combinations may tip the balance toward
the development of disease. Recently, the first such
risk factor was mapped in a genomewide association study to a region of chromosome 7q31
that spans the genes encoding caveolin 1 and
caveolin 2. The causal mutation in this region,
which has not yet been discovered, confers a population attributable risk of at most 12%.34 This
relatively small effect size suggests that the genetic basis of primary open-angle glaucoma involves the contribution of more genes with smaller population attributable risks than have been
found in studies of AMD.
Fuchs’ corneal dystrophy is an age-related corneal disease that affects about 5% of the population over the age of 40 years and is the leading
cause of corneal transplantation. This disorder is
characterized by a gradual loss of cells from the
endothelial surface of the cornea, the development
of small excrescences known as guttae in the underlying basement membrane, and eventual thickening and clouding of the corneal stroma. Recently, a genomewide association study showed
that alleles of the transcription factor 4 gene
(TCF4), which encodes a member of the E-protein
family (E2-2), are strongly associated with typical
age-related Fuchs’ corneal dystrophy.6 The likelihood of the disease among persons who are homozygous for the risk allele is 30 times the likelihood among persons who do not have the risk
allele. However, unlike the role of CFH in AMD, in
which the most strongly associated single-nucleotide polymorphism (SNP) actually alters the CFH
protein in a functionally meaningful way, there is
COLOR FIGURE
5/02/11
Draft 4
1938
Author
Fig #
Stone
3n
engl j med 364;20
nejm.org
may 19, 2011
Title
The New England Journal of Medicine
Downloaded from nejm.orgME
on October 1, 2016. For personal use only. No other uses without permission.
DE
Phimister
CopyrightArtist
© 2011
Massachusetts Medical Society. All rights reserved.
Knoper
AUTHOR PLEASE NOTE:
genomic medicine
currently little corroborating biologic evidence to
support the involvement of TCF4 in Fuchs’ corneal
dystrophy. For example, the linked SNP lies within
an intron of TCF4 and is unlikely to alter TCF4
expression. Also, persons with de novo loss-offunction mutations in TCF4 have a severe neurologic disease that does not have corneal endothelial
dysfunction as a feature.8,35 Thus, as with many
findings obtained through a genomewide association study, more work is needed to unravel the
mechanism through which the statistically associated locus is linked to the corneal phenotype.
Ther a pie s for Gene t ic
E y e Dise a se
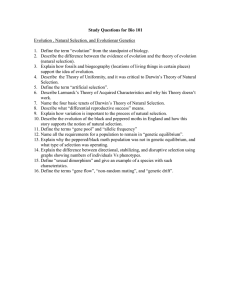
A
B
Physicians have sought to treat inherited eye diseases at every level of the disease process —
ranging from a very specific inhibition of a single
mutant allele with a small inhibitory RNA molecule36 to a broad alteration of the metabolic milieu with the use of a cocktail of vitamins with an
uncertain mechanism of action.37 Gene discov200 µm
ery experiments have aided in this effort by providing an improved understanding of specific
C
biologic pathways that when perturbed lead to
disease or susceptibility to disease. Such pathways can become important targets for therapeutic agents, and scientists have been very creative
in devising treatments aimed at those targets.
For example, the discovery that ABCA4 is involved in transporting vitamin A derivatives out
of outer segment disks16 led to the discovery that
200 µm
vitamin A inhibitors such as fenretinide inhibit
the accumulation of lipofuscin in animal models
Figure 4. Treatment of Age-Related Macular Degeneration (AMD)
of Stargardt’s disease.38 The identification of the
with Bevacizumab.
role of vascular endothelial growth factor in choA retinal photograph of a 67-year-old patient with a subretinal neovascular
membrane (Panel A) shows yellow deposits (drusen) beneath the retinal
roidal neovascularization led to the development
pigment epithelium (arrows), which are the clinical hallmarks of AMD.
of therapeutic antibodies (e.g., ranibizumab and
Cloudy subretinal fluid and small hemorrhages in the center of the macula
bevacizumab) to combat the major blinding comare suggestive of subretinal neovascularization. The horizontal black line
plication of AMD (Fig. 4). (An article describing
indicates the center of the macula. The visual acuity in this eye is 20/80.
a test of noninferiority of these drugs in the
A spectral-domain optical coherence tomogram (SDOCT) taken through
the center of the macula reveals subretinal neovascular tissue and fluidtreatment of AMD appears in this issue of the
filled spaces within the retina (Panel B). A repeat SDOCT taken after three
Journal.39) Growth factors40 and neuroprotective
intravitreal injections of bevacizumab during a 3-month period reveals a
41
agents have also been used to reduce the rate
dramatic reduction of neovascular tissue and intraretinal fluid (Panel C).
of an apoptotic response to inherited cellular
The visual acuity has improved to 20/50.
abnormalities. In recent years, gene-replacement
therapy, therapeutic stem cells, and retinal prostheses have also moved to the threshold of clini- es is that a complete knowledge of the specific
cal use for the treatment of genetic eye disease. molecular cause of a patient’s disease may not be
A potential advantage of the latter two approach- necessary for the treatment to be successful.
n engl j med 364;20
nejm.org
may 19, 2011
The New England Journal of Medicine
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
1939
The
n e w e ng l a n d j o u r na l
Gene Ther a py
Most human photoreceptor diseases are inherited
in an autosomal recessive manner, and in these
cases the mechanism of disease usually involves a
profound loss of function of the gene product.
More than a dozen recessive retinal diseases have
been successfully treated with viral- or nanoparticle-based gene transfer in animal models.42 For
example, one molecular form of Leber’s congenital
amaurosis is caused by the lack of the retinoid
isomerase encoded by RPE65. A decade ago, Acland
and colleagues43 successfully restored vision in a
naturally occurring canine model of this disease
using an adeno-associated viral vector to transfer a
normal version of RPE65 to the retinal pigment
epithelium. More recently, three different groups
have extended this work to humans.44-46 For example, 3 years ago, Maguire and colleagues44 reported results in 12 patients who were treated
with gene-replacement therapy. They observed visual improvement in all 12 patients, with the greatest gains among younger patients.
T r a nspl a n tat ion of S tem Cel l s
Several important cell types in the eye have little
if any capacity for endogenous regeneration, and
as a result the only viable treatment option for patients with hereditary disorders that involve the
loss of such cells is some type of cell-replacement
therapy. Although the replacement of highly differentiated cells, such as photoreceptors, poses
challenges, a number of recent experiments suggest that the use of stem cells to achieve such a
goal is now feasible.
In 2004, Klassen and colleagues47 found that
transplanted retinal progenitor cells could develop into functional photoreceptors and give rise
to enhanced visual function in mice with retinal
degeneration. Since these original reports, an assortment of different cell types, ranging from
the fate-restricted photoreceptor precursor to the
pluripotent embryonic stem cell,48-51 have been
used to replace photoreceptors in animals with
inherited retinal disease. Embryonic stem cells
have been of particular interest because of their
ability to undergo unlimited self-renewal and
tissue-specific cell production. For instance,
Eiraku and colleagues52 recently found that by
using a three-dimensional cell-culture system, they
could recapitulate development and reliably gen1940
of
m e dic i n e
erate functional photoreceptor cells in vitro. These
properties permit the generation of cells in sufficient numbers to perform clinical transplantation
from a single isolation rather than the multiple
donations that are required when more developmentally restricted cell types are used.
Regardless of the theoretical utility of these cell
types in humans, the isolation of cells from human
embryos is rife with ethical concerns and immunologic limitations. As a result, freshly isolated embryonic stem cells seem unlikely to be widely used
in the treatment of degenerative eye disease. A cell
type that overcomes the majority of these limitations is the induced pluripotent stem cell (iPSC).
Initially produced by Takahashi and Yamanaka
5 years ago,53 iPSCs can be generated by genetic
re­programming of dermal fibroblasts to pluripotency through retroviral transduction of only four
transcription factors.53 Several groups of investigators have been able to show that iPSCs have the
capacity to generate a variety of retinal-cell types,
including photoreceptors,54,55 and that after transplantation these photoreceptors will integrate
with­in the dystrophic retinal architecture,56,57
which results in partial recovery of the electroretinographic response.57 Although methodologic
barriers, such as the use of retroviruses, preclude
the immediate clinical translation of this technology, and recent studies suggest that the process of somatic-cell reprogramming may result in
the introduction of pathway-specific genetic defects,58-60 this field is evolving rapidly, and it is
possible that these cells will eventually make their
way into clinical use.
R e t ina l Pros the se s
In normal vision, decreased glutamate at the
photoreceptor axon terminals stimulates bipolar
and amacrine cells, which in turn release glutamate to stimulate the ganglion cells that communicate with the brain. In an attempt to bypass
photoreceptors and other neuronal elements that
have been damaged by degenerative retinal disease, investigators have explored the possibility
of stimulating the ganglion cells directly with
the use of electrical impulses delivered from a
planar array of microelectrodes. Several different
designs for retinal prostheses have had promising results in both animals and humans,61 and
one of these designs has recently been approved
for clinical use in Europe.
n engl j med 364;20 nejm.org may 19, 2011
The New England Journal of Medicine
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
genomic medicine
C onclusion
The eye has figured prominently in the development of genetic and genomic approaches to human
disease. Vision is critically important to most activities of daily living, and cures for blindness will
remain an important goal for medicine for many
years to come. Physicians and scientists will be
aided in the pursuit of this goal by the optical and
anatomic accessibility of the organ, as well as by
the large amount of visual cortex devoted to the
interpretation of the neural information originating
in the retina. That is, a patient with a disease that
injures only a few thousand neurons in the fovea
can describe this injury to his physician in great
detail, and the physician can in turn view these
neurons in the living patient at microscopic resolution by taking advantage of the near perfect optics
of the anterior portion of the eye. These natural
optics also contribute to a surgical accessibility that
is unmatched by any other part of the central nervous system. This latter attribute will be a tremendous advantage for clinician scientists seeking to
translate all the recent progress in gene-transfer and
stem-cell biology into effective therapies for their
patients with genetic eye diseases.
Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
References
1. Senju S, Haruta M, Matsunaga Y, et al.
Characterization of dendritic cells and
macrophages generated by directed differentiation from mouse induced pluripotent stem cells. Stem Cells 2009;27:102131.
2. Azuma N, Nishina S, Yanagisawa H,
Okuyama T, Yamada M. PAX6 missense
mutation in isolated foveal hypoplasia.
Nat Genet 1996;13:141-2.
3. Wilson EB. The sex chromosomes.
Arch Mikrosk Anat Enwicklungsmech
1911;77:249-71.
4. Renwick JH, Lawler SD. Probable
linkage between a congenital cataract locus and the Duffy blood group locus. Ann
Hum Genet 1963;27:67-84.
5. Newman NJ, Lott MT, Wallace DC.
The clinical characteristics of pedigrees
of Leber’s hereditary optic neuropathy
with the 11778 mutation. Am J Ophthalmol 1991;111:750-62.
6. Swaroop A, Chew EY, Rickman CB,
Abecasis GR. Unraveling a multifactorial
late-onset disease: from genetic susceptibility to disease mechanisms for age-related
macular degeneration. Annu Rev Genomics Hum Genet 2009;10:19-43.
7. Kwon YH, Fingert JH, Kuehn MH, Alward WL. Primary open-angle glaucoma.
N Engl J Med 2009;360:1113-24.
8. Baratz KH, Tosakulwong N, Ryu E, et
al. E2-2 protein and Fuchs’s corneal dystrophy. N Engl J Med 2010;363:1016-24.
9. Cavenee WK, Hansen MF, Nordenskjold M, et al. Genetic origin of mutations
predisposing to retinoblastoma. Science
1985;228:501-3.
10. Schindler EI, Nylen EL, Ko AC, et al.
Deducing the pathogenic contribution of
recessive ABCA4 alleles in an outbred
population. Hum Mol Genet 2010;19:3693701.
11. Cideciyan AV, Swider M, Aleman TS,
et al. ABCA4 disease progression and a
proposed strategy for gene therapy. Hum
Mol Genet 2009;18:931-41.
12. Stone EM. Finding and interpreting
genetic variations that are important to
ophthalmologists. Trans Am Ophthalmol
Soc 2003;101:437-84.
13. Hamosh A, FitzSimmons SC, Macek
M Jr, Knowles MR, Rosenstein BJ, Cutting
GR. Comparison of the clinical manifestations of cystic fibrosis in black and
white patients. J Pediatr 1998;132:255-9.
14. Resnikoff S, Pascolini D, Etya’ale D, et
al. Global data on visual impairment in
the year 2002. Bull World Health Organ
2004;82:844-51.
15. Allikmets R. A photoreceptor cellspecific ATP-binding transporter gene
(ABCR) is mutated in recessive Stargardt
macular dystrophy. Nat Genet 1997;17:
122.
16. Weng J, Mata NL, Azarian SM, Tzekov
RT, Birch DG, Travis GH. Insights into
the function of Rim protein in photoreceptors and etiology of Stargardt’s disease from the phenotype in abcr knockout
mice. Cell 1999;98:13-23.
17. Maugeri A, Klevering BJ, Rohrschneider K, et al. Mutations in the ABCA4
(ABCR) gene are the major cause of autosomal recessive cone-rod dystrophy. Am J
Hum Genet 2000;67:960-6.
18. Sunden SL, Alward WL, Nichols BE, et
al. Fine mapping of the autosomal dominant juvenile open angle glaucoma (GLC1A)
region and evaluation of candidate genes.
Genome Res 1996;6:862-9.
19. Stone EM, Fingert JH, Alward WLM,
et al. Identification of a gene that causes
primary open angle glaucoma. Science
1997;275:668-70.
20. Alward WL, Fingert JH, Coote MA, et
al. Clinical features associated with mutations in the chromosome 1 open-angle
glaucoma gene (GLC1A). N Engl J Med
1998;338:1022-7.
21. Shepard AR, Jacobson N, Millar JC, et
al. Glaucoma-causing myocilin mutants
require the peroxisomal targeting signal-1 receptor (PTS1R) to elevate intraoc-
ular pressure. Hum Mol Genet 2007;16:
609-17.
22. Sheffield VC. The blind leading the
obese: the molecular pathophysiology of a
human obesity syndrome. Trans Am Clin
Climatol Assoc 2010;121:172-81.
23. Shah AS, Farmen SL, Moninger TO, et
al. Loss of Bardet-Biedl syndrome proteins alters the morphology and function
of motile cilia in airway epithelia. Proc
Natl Acad Sci U S A 2008;105:3380-5.
24. Stone EM, Webster AR, Vandenburgh
K, et al. Allelic variation in ABCR associated with Stargardt disease but not agerelated macular degeneration. Nat Genet
1998;20:328-9.
25. Haines JL, Hauser MA, Schmidt S, et
al. Complement factor H variant increases
the risk of age-related macular degeneration. Science 2005;308:419-21.
26. Edwards AO, Ritter R III, Abel KJ,
Manning A, Panhuysen C, Farrer LA.
Complement factor H polymorphism and
age-related macular degeneration. Science 2005;308:421-4.
27. Hageman GS, Anderson DH, Johnson
LV, et al. A common haplotype in the
complement regulatory gene factor H
(HF1/CFH) predisposes individuals to
age-related macular degeneration. Proc
Natl Acad Sci U S A 2005;102:7227-32.
28. Klein RJ, Zeiss C, Chew EY, et al.
Complement factor H polymorphism in
age-related macular degeneration. Science 2005;308:385-9.
29. Jakobsdottir J, Conley YP, Weeks DE,
Mah TS, Ferrell RE, Gorin MB. Susceptibility genes for age-related maculopathy
on chromosome 10q26. Am J Hum Genet
2005;77:389-407.
30. Rivera A, Fisher SA, Fritsche LG, et al.
Hypothetical LOC387715 is a second major susceptibility gene for age-related
macular degeneration, contributing independently of complement factor H to disease risk. Hum Mol Genet 2005;14:322736.
n engl j med 364;20 nejm.org may 19, 2011
The New England Journal of Medicine
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
1941
genomic medicine
31. Dewan A, Liu M, Hartman S, et al.
HTRA1 promoter polymorphism in wet
age-related macular degeneration. Science 2006;314:989-92.
32. Quigley HA, Broman AT. The number
of people with glaucoma worldwide in
2010 and 2020. Br J Ophthalmol 2006;90:
262-7.
33. Fan BJ, Wiggs JL. Glaucoma: genes,
phenotypes, and new directions for therapy.
J Clin Invest 2010;120:3064-72.
34. Thorleifsson G, Walters GB, Hewitt
AW, et al. Common variants near CAV1
and CAV2 are associated with primary
open-angle glaucoma. Nat Genet 2010;42:
906-9.
35. Zweier C, Peippo MM, Hoyer J, et al.
Haploinsufficiency of TCF4 causes syndromal mental retardation with intermittent hyperventilation (Pitt-Hopkins syndrome). Am J Hum Genet 2007;80:9941001.
36. Gorbatyuk M, Justilien V, Liu J, Hauswirth WW, Lewin AS. Preservation of
photoreceptor morphology and function
in P23H rats using an allele independent
ribozyme. Exp Eye Res 2007;84:44-52.
37. Age-Related Eye Disease Study Research
Group. A randomized, placebo-controlled,
clinical trial of high-dose supplementation with vitamins C and E and beta carotene for age-related macular degeneration
and vision loss: AREDS report no. 9. Arch
Ophthalmol 2001;119:1439-52.
38. Radu RA, Han Y, Bui TV, et al. Reductions in serum vitamin A arrest accumulation of toxic retinal fluorophores: a
potential therapy for treatment of lipo­
fuscin-based retinal diseases. Invest Ophthalmol Vis Sci 2005;46:4393-401. [Erratum,
Invest Ophthalmol Vis Sci 2006;47:3735.]
39. The CATT Research Group. Ranibizumab and bevacizumab for neovascular
age-related macular degeneration. N Engl
J Med 2011;364:1897-908.
40. Sieving PA, Caruso RC, Tao W, et al.
Ciliary neurotrophic factor (CNTF) for
human retinal degeneration: phase I trial
of CNTF delivered by encapsulated cell
intraocular implants. Proc Natl Acad Sci
U S A 2006;103:3896-901.
1942
41. Boatright JH, Moring AG, McElroy C,
et al. Tool from ancient pharmacopoeia
prevents vision loss. Mol Vis 2006;12:
1706-14.
42. den Hollander AI, Black A, Bennett J,
Cremers FP. Lighting a candle in the dark:
advances in genetics and gene therapy of
recessive retinal dystrophies. J Clin Invest
2010;120:3042-53. [Erratum, J Clin Invest
2011;121:456-7.]
43. Acland GM, Aguirre GD, Ray J, et al.
Gene therapy restores vision in a canine
model of childhood blindness. Nat Genet
2001;28:92-5.
44. Maguire AM, Simonelli F, Pierce EA,
et al. Safety and efficacy of gene transfer
for Leber’s congenital amaurosis. N Engl
J Med 2008;358:2240-8.
45. Bainbridge JW, Smith AJ, Barker SS, et
al. Effect of gene therapy on visual function in Leber’s congenital amaurosis.
N Engl J Med 2008;358:2231-9.
46. Hauswirth WW, Aleman TS, Kaushal
S, et al. Treatment of Leber congenital
amaurosis due to RPE65 mutations by
ocular subretinal injection of adeno-associated virus gene vector: short-term results of a phase I trial. Hum Gene Ther
2008;19:979-90.
47. Klassen HJ, Ng TF, Kurimoto Y, et al.
Multipotent retinal progenitors express
developmental markers, differentiate into
retinal neurons, and preserve light-mediated behavior. Invest Ophthalmol Vis Sci
2004;45:4167-73.
48. Osakada F, Ikeda H, Mandai M, et al.
Toward the generation of rod and cone
photoreceptors from mouse, monkey and
human embryonic stem cells. Nat Biotechnol 2008;26:215-24.
49. MacLaren RE, Pearson RA, MacNeil
A, et al. Retinal repair by transplantation
of photoreceptor precursors. Nature
2006;444:203-7.
50. Lamba DA, Karl MO, Ware CB, Reh
TA. Efficient generation of retinal progenitor cells from human embryonic
stem cells. Proc Natl Acad Sci U S A 2006;
103:12769-74.
51. Ikeda H, Osakada F, Watanabe K, et
al. Generation of Rx+/Pax6+ neural reti-
nal precursors from embryonic stem
cells. Proc Natl Acad Sci U S A 2005;102:
11331-6.
52. Eiraku M, Takata N, Ishibashi H, et al.
Self-organizing optic-cup morphogenesis
in three-dimensional culture. Nature 2011;
472:51-6.
53. Takahashi K, Yamanaka S. Induction
of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by
defined factors. Cell 2006;126:663-76.
54. Meyer JS, Shearer RL, Capowski EE, et
al. Modeling early retinal development
with human embryonic and induced pluri­
potent stem cells. Proc Natl Acad Sci U S A
2009;106:16698-703.
55. Osakada F, Jin ZB, Hirami Y, et al. In
vitro differentiation of retinal cells from
human pluripotent stem cells by smallmolecule induction. J Cell Sci 2009;122:
3169-79.
56. Lamba DA, McUsic A, Hirata RK,
Wang PR, Russell D, Reh TA. Generation,
purification and transplantation of photoreceptors derived from human induced
pluripotent stem cells. PLoS One 2010;5(1):
e8763.
57. Tucker B, Park I-H, Qi SD, et al. Transplantation of adult mouse iPS cell-derived
photoreceptor precursors restores retinal
structure and function in retinal degenerative mice. PLoS One (in press).
58. Gore A, Li Z, Fung HL, et al. Somatic
coding mutations in human induced pluripotent stem cells. Nature 2011;471:63-7.
59. Hussein SM, Batada NN, Vuoristo S,
et al. Copy number variation and selection
during reprogramming to pluripotency.
Nature 2011;471:58-62.
60. Lister R, Pelizzola M, Kida YS, et al.
Hotspots of aberrant epigenomic reprogramming in human induced pluripotent
stem cells. Nature 2011;471:68-73.
61. Dowling J. Current and future prospects for optoelectronic retinal prostheses. Eye (Lond) 2009;23:1999-2005.
Copyright © 2011 Massachusetts Medical Society.
n engl j med 364;20 nejm.org may 19, 2011
The New England Journal of Medicine
Downloaded from nejm.org on October 1, 2016. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.