Extraction of maxillary first permanent molars in patients with Class II
advertisement

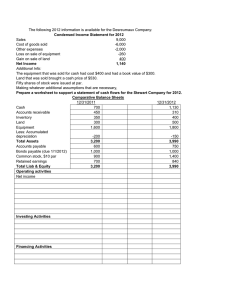
ORIGINAL ARTICLE Extraction of maxillary first permanent molars in patients with Class II Division 1 malocclusion Mattijs J. P. Stalpers,a Johan W. Booij,b Ewald M. Bronkhorst,c Anne Marie Kuijpers-Jagtman,d and Christos Katsarose Nijmegen and Gorinchem, the Netherlands Introduction: Our objectives were to assess treatment outcomes in Class II Division 1 patients who were treated orthodontically with extraction of the maxillary first permanent molars and to describe the changes in their facial profiles. Methods: This was a prospective, longitudinal, 1-group outcome analysis in a private practice, with outcome evaluation by independent observers at an academic clinic. One hundred consecutively treated patients were enrolled prospectively and treated by 1 orthodontist. The inclusion criteria were white, Class II Division 1, sagittal overjet of ⱖ4 mm, extraction of maxillary first permanent molars, no missing teeth or agenesis, maxillary third molars present, and 1-stage full fixed appliance treatment. Standardized lateral cephalometric radiographs were made before and after active treatment. Occlusal outcome was scored on dental casts by comparing pretreatment and posttreatment casts with the peer assessment rating (PAR) index. Backward regression analysis was used to explain the soft-tissue changes on the basis of dental changes and the soft-tissue characteristics. Results: The mean reduction in weighted PAR score was 89.9% (SD, 0.9). During treatment, the lower lip retruded 1.6 mm (SD, 1.7) relative to the esthetic line. The nasolabial angle became 2.1° (SD, 7.0) more obtuse during treatment. Overjet reduction and initial upper lip thickness could explain 15% of the variation in upper lip position. The changes in the position of the mandibular incisor relative to the Point A-pogonion line and initial lower lip thickness could explain 23% of the variation of lower lip position. Conclusions: Orthodontic treatment involving extraction of the maxillary first permanent molars has a good treatment outcome. Extraction of the maxillary first permanent molars has only a small effect on the soft-tissue profile. (Am J Orthod Dentofacial Orthop 2007;132:316-23) T he Class II relationship is the most prevalent subclassification of malocclusion. Recognizing the limitations of this description, epidemiologists have formulated indexes and scales for use in public health studies. The results of these surveys suggest that 15% to 22% of American teenagers have an overjet of 5 mm or greater.1 For those seeking orthodontic treatment to have the overjet corrected, there are generally 3 treatment options. Clinical and anamnestic findings are key factors in narrowing the choices. Growth modification, with either headgear or activator, might be suggested for a prepubertal patient a Orthodontist, Department of Orthodontics and Oral Biology, Radboud University Nijmegen Medical Center, Nijmegen, the Netherlands. Private practice, Gorinchem, the Netherlands. c Biostatistician, Department of Preventive and Curative Dentistry, Radboud University Nijmegen Medical Center, Nijmegen, the Netherlands. d Professor and chair, Department of Orthodontics and Oral Biology, Radboud University Nijmegen Medical Center, Nijmegen, the Netherlands. e Professor, Department of Orthodontics and Oral Biology, Radboud University Nijmegen Medical Center, Nijmegen, the Netherlands. Reprint requests to: Christos Katsaros, Radboud University Nijmegen Medical Center, Department of Orthodontics and Oral Biology, 117 Tandheelkunde, PO Box 9101, 6500 HB Nijmegen, the Netherlands; e-mail, c.katsaros@dent.umcn.nl. Submitted, June 2005; revised and accepted, January 2006. 0889-5406/$32.00 Copyright © 2007 by the American Association of Orthodontists. doi:10.1016/j.ajodo.2006.01.034 b 316 with a favorable growth pattern. For a postpubertal patient seeking treatment, surgical correction of the jaw abnormality can be an option. The third option is orthodontic treatment combined with extraction of teeth. In case of crowding in both arches, extraction of 4 teeth is often indicated. In case of overjet and a good or potentially good mandibular arch, extractions can be limited to the maxillary arch only. Space analysis of the mandibular arch involves factors such as crowding or spacing, the curve of Spee, and the position of the mandibular incisors.2 Within reason, these incisors can be left slightly proclined. This compensated position is presumably stable, provides extra arch space, and reduces the amount of retraction needed for the maxillary incisors. This in turn can provide an improved facial profile in many Class II patients.3 When the clinician decides to extract teeth, the next question is which teeth are to be extracted. The most obvious choice might be to extract the first or second premolars. In certain cases, extraction of the first permanent molars can be preferred. In addition to extracting the first permanent molars in a systematic othodontic treatment approach, there are certain objective indications for first molar extractions. These might be extensive caries lesions, large fillings, endodontic or periodontal problems, American Journal of Orthodontics and Dentofacial Orthopedics Volume 132, Number 3 or hypoplastic enamel. A dogma in orthodontics is that extraction in the posterior part of the dental arch has a bite-closing effect that would be beneficial for high-angle patients and, on the other hand, detrimental in low-angle patients.4 Another extensively debated belief is that extraction in the molar area would have less influence on the facial profile than premolar extractions. In a study of cephalometric changes in a group of borderline extraction patients treated with or without premolar extractions, it was observed that the facial profiles of the extraction group were, on average, 2 mm flatter than the profiles of the nonextraction patients.5 Katsaros et al6 found, in a study on extraction vs nonextraction treatment, high variability in soft-tissue changes, which were unpredictable for an individual patient.6 In the orthodontic literature, there are few data concerning the extraction of first molars as part of orthodontic treatment. Patients and methods have been described, but prospectively collected data are absent.7,8 The purposes of our study were to assess treatment outcomes in Class II Division 1 patients treated with extraction of the maxillary first permanent molars and to describe the changes in their facial profiles. MATERIAL AND METHODS The sample consisted of 100 consecutively treated patients (45 girls, 55 boys) who were enrolled prospectively. The intake of patients started in 1998 and finished in 2004. All patients were treated by 1 orthodontist (J.W.B.). The following inclusion criteria were used: white, Class II Division 1 malocclusion, sagittal overjet of ⱖ4 mm, treatment plan included extraction of maxillary first permanent molars, no missing teeth or agenesis, maxillary third molars present, and 1-stage full fixed appliance treatment. The mean age at the start of treatment was 13.2 years (range, 10.5-17.2; SD, 1.4). The maxillary second molars and the mandibular molars were banded before the extractions. The molar bands had 6-mm single 0.018-in round buccal tubes and palatal sheaths. The maxillary first molars were separated to facilitate the extractions, and, after 3 weeks, both arches were bonded with light wire Begg brackets. The maxillary premolars were not bonded in the first phase of the treatment to reduce friction. The maxillary second molars were connected by a removable palatal bar to increase anchorage and to correct possible rotations and transverse malpositions. Canine retraction was performed with elastics (light 5/16 in) from the maxillary canine to the maxillary second molar, and the patient was instructed to replace them only once a week. If the maxillary second molars moved mesially too fast, the intra-arch elastics were replaced by Class II elastics. In most patients, Class I canine and premolar Stalpers et al 317 interdigitation was reached in 6 months. At this point, the maxillary premolars were bonded. In the end phase of treatment, adjustments were made in the archwires for detailed finishing. In most cases, retention was with fixed retainers. To prevent overeruption of the mandibular second molars, local retention wires were bonded between the first and second molars; the wires were removed when the maxillary third molars were in occlusal contact with the mandibular second molars. Standardized lateral cephalometric radiographs were made before (T1) and after (T2) active treatment. The radiographs were scanned on an 8-bit scanner (Linotype-Hell, Eschborn, Germany). Tracing of the films was done in Viewbox (dHal Orthodontic Software, Athens, Greece), a software program for cephalometric analysis. All tracings were corrected to life size. Skeletal, dental, and soft-tissue cephalometric landmarks were used. The cephalometric landmarks and reference lines are illustrated in Figure 1. To evaluate the influence of treatment on different vertical facial types, the sample was divided into 3 groups: horizontal (ANS-Me/N-Me ⱕ56%; n ⫽ 18), normal (56% ⬍ANS-Me/N-Me ⬍58%; n ⫽ 21), and divergent (ANS-Me/N-Me ⱖ58%; n ⫽ 61).9 Mean tracings of the 100 patients were constructed and superimposed. To calculate a mean tracing, the tracings were superimposed on the anterior nasal spine (ANS)-posterior nasal spine (PNS) line at ANS. After all tracings had been superimposed on each other, Viewbox calculated the mean coordinates for each cephalometric point. These mean coordinates were used to construct a new tracing, the mean tracing. This was done for T1 and T2. These mean tracings were, in their turn, superimposed on ANS-PNS at ANS to illustrate treatment effect and growth. The occlusal outcome of treatment was scored on the dental casts, by comparing the casts at T1 and T2 with the peer assessment rating (PAR index).10 The PAR index is applied to a patient’s pretreatment and posttreatment dental casts. Scores are assigned to the various occlusal traits that make up the malocclusion. The components of the PAR index are alignment of maxillary anterior segments, alignment of mandibular anterior segments, left buccal occlusion, right buccal occlusion, overjet, overbite, and center line. British weightings were used; this means that the individual scores for overjet were multiplied by 6, overbite by 2, and center line by 4. A score of zero indicates good alignment and occlusion, and higher scores indicate increased levels of irregularity or malocclusion. The difference between the pretreatment and posttreatment PAR scores indicates improvement as a result of orthodontic intervention. Furthermore, the percentage 318 Stalpers et al American Journal of Orthodontics and Dentofacial Orthopedics September 2007 ⱖ30% reduction), and greatly improved (generally a reduction of 22 weighted PAR points or more).11 To assess the method error, the cephalograms of 20 patients and the dental casts of 50 patients were measured by a second orthodontist. For the assessment of interobserver error, the duplicate measurement error was calculated with Dahlberg’s formula.12 Paired t tests were used to assess systematic differences between the 2 observers for the cephalometric variables. Statistical analysis Fig 1. Cephalometric points and reference lines used in study. of improvement was calculated. This percentage also reflects the change relative to the pretreatment score but gives a more sensitive assessment. To illustrate the degree of improvement, the nomogram was used, in which the degree of change is separated into 3 sections: worse or no different (patients with less than 30% reduction), improved (patients with Differences between the cephalometric variables and the PAR score before and after treatment were analyzed by using paired t tests. To evaluate the influence of treatment on the various vertical facial types, ANOVA was applied, followed post hoc by the Bonferroni correction for multiple testing. T tests were used to assess the difference in the treatment effect between boys and girls. For only 2 of the 22 variables tested (21 cephalometric variables and the PAR score), a statistically significant difference between the sexes was found: overbite and length of the nose (N-No). Therefore, the results are presented for the complete patient group, regardless of sex. Multiple linear regression was used to attempt to explain the soft-tissue changes on the basis of dental changes. The change in the sagittal position of the upper lip relative to the esthetic line (Ls to E-line) was used as the dependent variable. Several independent variables were used: change in the sagittal position of the maxillary incisor relative to Point A-pogonion (U1 to A-Pog), change in the maxillary incisor inclination (U1L/ANS-PNS), change in overjet, and sex. The pretreatment thickness (Ls-U1) of the upper lip was added as a controlling variable. To reduce the initial model, stepwise backward regression was applied with a threshold for the P value of .1 for removing a variable from the model. A similar approach was used for the lower lip: change in the sagittal position of the lower lip relative to the esthetic line (Li to E-line) was used as a dependent variable, and change in the sagittal position of the mandibular incisor relative to A-Pog (L1 to A-Pog), change in mandibular incisor inclination (L1L/ ML), change in overjet, and sex were the independent variables. Again, the pretreatment thickness of the lip (Li-L1) was added as a controlling variable. To analyze the relationship between age at start of treatment and treatment effect on cephalometric variables, scatter plots were made to check for nonlinear relationships. Without indications for a nonlinear relationship, Pearson correlations were calculated to quantify the relationship between age and the cephalometric variables. For the relationshipbetween the reduction in American Journal of Orthodontics and Dentofacial Orthopedics Volume 132, Number 3 Table I. Results of method error analysis (first 2 columns relate to paired t test) Variable Dental cast analysis PAR Cephalometric analysis SNA angle (°) SNB angle (°) ANB angle (°) SN/ANS-PNS (°) SN/ML (°) ANS-PNS/ML (°) ANS-ME/N-ME (ratio) U1L/ANS-PNS (°) U1 to A-Pog (mm) L1L/ML (°) L1 to A-Pog (mm) Overbite (mm) Overjet (mm) Nasolabial angle (°) Ls to Sn-Pog’ (mm) Li to Sn-Pog’ (mm) Ls to E-line (mm) Li to E-line (mm) N-No (mm) Ls-U1 (mm) Li-L1 (mm) Mean difference Duplicate between measurement observers P value error ⫺1.595 ⬍.0001 3.297 ⫺0.044 ⫺0.047 0.015 0.065 ⫺0.044 ⫺0.106 0.094 ⫺0.032 0.121 0.124 0.121 ⫺0.018 0.003 0.759 ⫺0.041 ⫺0.076 ⫺0.029 ⫺0.059 ⫺0.144 0.047 ⫺0.206 .357 .147 .682 .017 .176 .006 .443 .583 .002 .043 .005 .338 .861 .358 .657 .387 .658 .442 .185 .702 .024 0.194 0.133 0.145 0.114 0.133 0.165 0.495 0.238 0.167 0.254 0.184 0.068 0.075 3.351 0.375 0.358 0.268 0.310 0.444 0.497 0.383 the PAR score (both absolute and relative reductions), the same procedure was followed. RESULTS The average duration of active orthodontic treatment was 2.5 years (SD, 0.6). All 100 patients who were enrolled in the study finished treatment. The mean age at T2 was 15.7 years (SD, 1.6; range, 12.4-19.8). In Table I, for all variables, the results of the paired t test comparing the 2 observers and the duplicate measurement error are given. For 6 cephalometric variables (SN/ANS-PNS, ANS-PNS/ML, U1 to A-Pog, L1L/ML, L1 to A-Pog, and Li-L1) and the PAR score, a statistically significant difference between the 2 observers was found. For angles, a maximum duplicate measurement error of 0.25° and, for distances, a maximum duplicate measurement error of 0.38 mm were found. However, for all variables, the duplicate measurement error was small compared with the standard deviations of the measurement (Table II). The descriptive statistics for the PAR score are summarized in Table II. The average PAR score at T1 was 29.2 (SD, 7.3). Eighty-four of the 100 patients had an initial score of ⱖ22 points; 15 was the lowest initial score. The mean percentage reduction in weighted PAR Stalpers et al 319 score was 89.9% (SD, 0.9). The mean absolute reduction was 26.3 points (SD, 7.3) to 2.9 points (SD, 2.4) at T2. Thirteen patients had a PAR score of zero at T2; 10 was the highest PAR score at T2. There were no patients in the “worse or no different” group, 27 were in the “improved” group, and 73 were in the “greatly improved” group. The nomogram is shown in Figure 2. For both the absolute and the relative reduction of the PAR score, no statistically significant correlation with age was found. Just 1 cephalometric variable showed a statistically significant correlation with age. The difference of N-No (T2 – T1) had a negative correlation with age (r ⫽ – 0.344, P ⫽ .0%). All other cephalometric variables had P values above 5% for the statistical significance of the correlation with age. Therefore, the results are presented without considering the patients’ ages. As shown in Table II, at T1, the patient group had typical Class II Division 1 characteristics: enlarged ANB angle (mean, 5.5°), overjet (mean, 7.3 mm), and overbite (mean, 2.9 mm). Furthermore, the maxillary incisors were protruded in relation to the A-Pog line. At T2, the ANB angle showed a significant reduction of 1.8° (SD, 1.5), mainly due to a reduction in the SNA angle. Superimposition of the mean tracings at T1 and T2 visually represents the overall treatment effect (Fig 3). During treatment, the maxillary incisors were retracted 2.7 mm (SD, 1.9) in relation to A-Pog. The inclination of the maxillary and mandibular incisors changed significantly. The maxillary incisors retroclined 2.3° (SD, 6.6) on ANS-PNS, and the mandibular incisors proclined 5.3° (SD, 5.0) to 103.2°(SD, 6.7) on mandibular line. The retraction and the retroclination of the maxillary incisors and the proclination of the mandibular incisors together with growth must have contributed to the overjet reduction of 4.8 mm (SD, 1.8) from 7.3 mm (SD, 1.8) at T1 to 2.5 mm (SD, 0.9) at T2. Overbite was reduced from 2.9 mm (SD, 2.7) at T1 to 1.3 mm (SD, 0.8) at T2. These changes were all significant. The position of the upper lip relative to the E-line (Ls to E-line) was 0.77 mm (SD, 2.5) at T1. At T2, its position was 3.3 mm (SD, 2.1) behind the E-line, a change of –2.6 mm (SD, 1.7). The position of the lower lip relative to the E-line (Li to E-line) was ⫹0.1 mm (SD, 2.3) at T1. At T2, its position was 1.6 mm (SD, 2.3) behind the E-line, a change of –1.6 mm (SD, 1.7). The nasolabial angle became 2.1° (SD, 7.0) more obtuse during treatment. In Table III, the results of the regression analysis aiming at prediction of the soft-tissue changes by dental variables are given. For the upper lip after applying 320 Stalpers et al Table II. American Journal of Orthodontics and Dentofacial Orthopedics September 2007 Descriptive statistics for cephalometric and dental cast measurements (P values calculated with paired t tests) T1 Variable Dental cast analysis PAR* PAR† Cephalometric analysis Skeletal sagittal SNA angle (°) SNB angle (°) ANB angle (°) Skeletal vertical SN/ANS-PNS (°) SN/ML (°) ANS-PNS/ML (°) ANS-ME/N-ME (ratio) Dentoalveolar U1L/ANS-PNS (°) U1 to A-Pog (mm) L1L/ML (°) L1 to A-Pog (mm) Dental Overbite (mm) Overjet (mm) Soft tissue Nasolabial angle (°) Ls to Sn-Pog’ (mm) Li to Sn-Pog’ (mm) Ls to E-line (mm) Li to E-line (mm) N-No (mm) Ls-U1 (mm) Li-L1 (mm) T2 Mean SD Mean 29.16 29.16 7.34 7.34 79.82 74.34 5.48 T2–T1 SD Mean SD P value 2.88 2.88 2.43 2.43 ⫺26.28 89.9% 7.32 0.9 ⬍.0001 ⬍.0001 3.74 3.67 1.92 77.70 73.98 3.72 3.94 3.72 2.23 ⫺2.12 ⫺0.35 ⫺1.76 1.92 1.24 1.54 ⬍.0001 .0051 ⬍.0001 7.23 35.02 27.80 58.21 3.31 5.74 5.12 2.34 7.30 35.35 28.06 58.54 3.38 6.31 5.54 2.35 0.07 0.33 0.26 0.32 1.50 1.66 1.78 1.29 .6361 .0485 .1515 .0147 110.38 9.03 97.92 1.66 5.56 2.41 6.33 1.99 108.05 6.30 103.18 3.82 5.39 1.86 6.57 1.86 ⫺2.33 ⫺2.72 5.26 2.15 6.62 1.88 4.94 1.63 .0006 ⬍.0001 ⬍.0001 ⬍.0001 2.87 7.28 2.65 1.84 1.34 2.48 0.84 0.85 ⫺1.53 ⫺4.81 2.42 1.80 ⬍.0001 ⬍.0001 114.85 4.66 3.44 ⫺0.77 0.10 48.62 11.01 14.56 9.27 1.81 1.98 2.46 2.33 3.77 2.32 1.56 116.98 3.26 2.63 ⫺3.32 ⫺1.55 51.54 13.47 13.10 10.35 1.58 1.91 2.14 2.31 4.07 2.04 1.43 2.12 ⫺1.39 ⫺0.80 ⫺2.56 ⫺1.64 2.92 2.47 ⫺1.46 7.02 1.42 1.46 1.71 1.67 2.15 1.59 1.52 .0032 ⬍.0001 ⬍.0001 ⬍.0001 ⬍.0001 ⬍.0001 ⬍.0001 ⬍.0001 *Absolute difference. Percentage improvement. † backward regression, only initial lip thickness and change in overjet remained in the model. For every millimeter of overjet reduction, a reduction of 0.396 mm of Ls to E-line is to be expected. For every millimeter of upper lip thickness at T1, a 0.168-mm reduction in Ls to E-line is expected. For the lower lip, all variables except initial thickness and change in L1 to A-Pog were excluded from the model. For every millimeter of increase in L1 to A-Pog, an increase of 0.216 mm in Li to E-line is expected. For every millimeter of lower lip thickness (Li-L1) at T1, a reduction of 0.512 mm in Li to E-line is expected. When we divided our pretreatment sample into 3 groups— horizontal (ANS-Me/N-Me ⱕ56%), normal (56%⬍ ANS-Me/N-Me ⬍58%), and divergent (ANSMe/N-Me ⱖ58%)—we found no significant differences in the change of the measurements SN/ML (P ⫽ .429). The values for variable ANS-PNS/ML show that the bite closed 0.1° in the divergent group and opened 0.8° and 0.9° in the horizontal and normal groups, respectively. The difference between the vertical and the other 2 groups was statistically significant (P ⫽ .018). DISCUSSION This study is the first to evaluate the quality of the treatment results of Class II Division 1 patients treated with extraction of the maxillary first molars. To do this, we looked at the occlusion, and we described the cephalometric and profile changes. The PAR index was developed to quantify the extent to which a dentition deviates from an ideally formed dental arch and occlusion. It does not assess other results, such as quality of life, reduced susceptibility to oral diseases, and dysfunctions.13 The PAR score gives a general impression of the dental arches and the occlusion but does not take all dental variables into account. For instance, in our study, the mandibular incisors were slightly proclined at T2. This does not have a negative effect on the PAR score. This is a Stalpers et al 321 American Journal of Orthodontics and Dentofacial Orthopedics Volume 132, Number 3 Table III. Prediction of soft-tissues changes, results of backward regression analysis Beta Fig 2. Nomogram with PAR score at T1 compared with PAR score at T2 and improvement categories; 73% of patients were in “greatly improved” section; no patients were in “worse or no different” section. Fig 3. Mean tracings: black, T1; red, T2. Note relatively small changes in sagittal position of upper and lower lips compared with greater changes in incisor position when superimposed on palatal plane at ANS. reason that we included cephalometric analysis in our study.14 For all cephalometric variables and the PAR score, a method error analysis was conducted, based on duplicated measurements by a second orthodontist. In most published studies, the intraobserver error is given. This error is usually smaller than the interobserver Dependent variable Ls to E-line (T2⫺T1) Independent variables Included Constant Overjet (T2⫺T1) Ls-U1 at T1 Excluded U1 to A-Pog (T2⫺T1) U1L/ANS-PNS (T2⫺T1) Sex at T1 Model fit Dependent variable Li to E-line (T2⫺T1) Independent variables Included Constant L1 to A-Pog (T2⫺T1) Li-L1 at T1 Excluded L1L/ML (T2⫺T1) Overjet (T2⫺T1) Sex at T1 Model fit P value 95% CI for beta 1.192 0.396 ⫺0.168 .245 .000 .021 Adj R2: .153 5.349 0.216 ⫺0.512 .000 .019 .000 Adj R2: .234 ⫺0.831 3.216 0.214 0.578 ⫺0.309 ⫺0.206 2.601 8.097 0.036 0.396 ⫺0.701 ⫺0.323 error. We chose to use the interobserver error because the intraobserver error cannot detect systematic errors in the identification of cephalometric points. For 6 of the cephalometric variables and the PAR score, a systematic difference between the observers was found. This was a matter of concern. However, for all 6 cephalometric variables, the systematic difference between the observers was small, always smaller than the duplicate measurement error. The duplicate measurement error in turn was much smaller than the standard deviation of the variable concerned (a factor 4 for Li-L1 and more than a factor 10 for the other cephalometric variables). In comparison with the variability of the PAR scores in the patient group, the duplicate measurement error for the PAR score was not as small (about half of the standard deviation for the PAR score). But when compared with the size of the treatment effect, the duplicate measurement error was small (a difference of a factor 10). Therefore, the uncertainty added by the measurement error was too small to consider exclusion of variables from the analysis. In this study, the average PAR score at T1 was high. Eighty-four of the 100 patients had an initial score of ⱖ22 points, and 15 was the lowest initial score. Thirteen patients had a PAR score of zero at T2; 10 was the highest PAR score at T2. Ten or fewer PAR points are considered a slight deviation from normal occlu- 322 Stalpers et al sion; 5 or fewer reflect nearly ideal occlusion.10,15 Previous studies showed that a 70% reduction of the PAR score can be considered a great improvement in occlusal factors.11,16 In our study, the sample showed an 89.9% average reduction in PAR score. Other studies ranged from a 68% reduction in PAR score in orthodontically treated British patients to 78% in a sample treated by Norwegian orthodontists to 88% in a study of American Board of Orthodontics cases.17-19 In our study, no patients were in the “worse or no different” category at T2, whereas 73% of our patients could be categorized as “greatly improved.” However, all our patients had a Class II malocclusion with an enlarged overjet. Because overjet has a weighting of 6 in the British weighting system, this adds considerably to a high pretreatment PAR score. It is less difficult to achieve striking, recordable changes when the initial PAR score is high.20 Nevertheless, our study suggests that the standard of the treatment was high. For the soft-tissue profile changes during orthodontic treatment, normal growth changes should be kept in mind. It was shown that the upper and lower lips become significantly more retruded to the E-line with age.21,22 Ricketts23 found the lower lip in women to be 2.0 mm posterior to the E-line; it was slightly more retruded in men. Bishara et al21 found the relative position of the lower lip to be, on average, 1.7 mm posterior to the E-line for adolescent boys and girls 15 years of age. In the sample of Paquette et al,5 the lower lips retruded 3.1 mm in the 4-premolar extraction group and 0.5 mm in the nonextraction group. In our study, the lower lip at T1 was 0.1 mm anterior of the E-line. At T2, the lower lip was 1.6 mm posterior of the E-line, a retrusion of 1.8 mm. An explanation for this observation might be that, since all our patients had an enlarged overjet, the lower lip rested on the protruded maxillary incisors at T1. Overjet was, in our patients, corrected by retraction of the maxillary incisors, proclination of the mandibular incisors (since we did not extract in the mandibular arch), and growth. When the maxillary incisors are retracted, the lower lip follows this movement. We were able to retract the maxillary incisors with a relatively controlled retroclination of 2.3°, but we could not avoid proclination of the mandibular incisors. The mandibular incisors proclined on average 5.3° from 98.0° at T1 to 103.2° at T2. This provided extra arch space and reduced the amount of retraction needed for the maxillary incisors. This in turn provided for an improved profile in many patients.4 The standard deviations for the changes in upper and lower lip thickness were high (6.62 and 4.94, respectively). This indicates high individual variability. American Journal of Orthodontics and Dentofacial Orthopedics September 2007 The variable upper lip position relative to the E-line (Ls to E-line) was suggested by Ricketts23 as a way to evaluate the position of the upper lip relative to the chin and nose. He found that ideally the upper lip should be 4.0 mm posterior to this line in women and slightly more retruded in men. These values were similar to the adult values of Bishara et al.21 They found, for 15-yearolds, that the upper lip was on average 2.9 mm posterior of the E-line. We found, in our sample, the upper lip to be on average 0.8 mm posterior of the E-line at T1 and 3.3 mm posterior of the E-line at T2. We retracted the maxillary incisors on average 2.7 mm relative to the A-Pog line and maintained good inclination. We observed retrusion of the upper lip relative to the subnasale-soft-tissue-Pog line of 1.4 mm. This means that, in our sample, the upper lip followed the movement of the maxillary incisors for about 50% after extraction of the first permanent maxillary molars. Also, Katsaros24 found only small soft-tissue profile changes compared with the dental changes in identical twins, with 1 boy treated with extraction of 4 premolars and the other without extractions. The relatively small changes in the sagittal position of the lips with A-Pog as a reference line, compared with the larger changes measured with the E-line as the reference, show that the influence of the growth of the chin or the nose on the facial profile might be more important than the orthodontic treatment. In a stereophotogrammetric study on the growth of the nose, early growth was found in girls and late growth in boys, suggesting an adolescent growth spurt in the nose.25 Developmentally, the greatest change occurred in the anteroposterior prominence of the nasal tip. An important factor in our analysis was the prediction of changes in lip position for the individual patient. When we applied a backward regression model for the upper lip, sex, change in maxillary incisor position, and inclination did not seem to significantly influence the change of the position of the upper lip in relation to the E-line (Ls to E-line). However, change in overjet and initial upper lip thickness could explain 15% of the variation. For the prediction of the change of lower lip position, sex, overjet, and inclination of the mandibularr incisors did not seem to have significant influence. However, mandibular incisor position (L1 to A-Pog) and initial lower lip thickness (Li-L1) could explain 23% of the variation. It was suggested that supraerupted maxillary first molars are a consistent finding in patients with skeletal open bite.5 Therefore, extraction of these molars might aid in mandibular autorotation and thereby reduce anterior facial height. In a sample of 8 patients with anterior open bite treated orthodontically with the extraction of 4 first molars, closing of the bite of 1.5° American Journal of Orthodontics and Dentofacial Orthopedics Volume 132, Number 3 (SN/GoGn angle) was found.26 These patients, however, had open bite extending to the posterior teeth. Our findings are not consistent with this treatment philosophy. The only statistically significant difference between T1 and T2 with regard to the skeletal vertical measurements for the horizontal, normal, and divergent groups was found for the measurement ANS-PNS/ML. The bite closed 0.1° in the divergent group and opened 0.8° and 0.9° in the horizontal and normal groups, respectively. This difference was statistically significant, but the clinical relevance of this finding is limited. In other words, we did not find a bite-closing effect of our treatment. That means that divergent patients do not seem to benefit more from this treatment modality than do deepbite patients. CONCLUSIONS Our results suggest that extraction of the maxillary first permanent molars in Class II Division 1 patients leads to good treatment outcomes. Extraction of the maxillary first permanent molars has only a minor effect on the soft-tissue profile. The bite-closing effect of extracting the maxillary first permanent molars is statistically significant, but the clinical relevance is questionable. REFERENCES 1. Proffit WR, Fields HW, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthod Orthognath Surg 1998;13:97-106. 2. Steiner CC. Cephalometrics for you and me. Am J Orthod 1953;39:729-55. 3. Bennett JC, McLaughlin RP. Orthodontic management of the dentition with the preadjusted appliance. Oxford: Isis Medical Media; 1997. p. 231-50. 4. Subtelny JD, Sakuda M. Open bite diagnosis and treatment. Am J Orthod 1964;50:337-58. 5. Paquette DE, Beattie JR, Johnston LE. A long-term comparison of nonextraction and premolar extraction edgewise therapy in “borderline” Class II cases. Am J Orthod Dentofacial Orthop 1992;102:1-14. 6. Katsaros C, Ripplinger B, Hoegel A, Berg R. The influence of extraction versus non-extraction orthodontic treatment on the soft tissue profile. J Orofac Orthop 1996;57:354-65. 7. Sandler PJ, Atkinson R, Murray AM. For four sixes. Am J Orthod Dentofacial Orthop 2000;117:418-34. 8. Williams R. Single arch extraction— upper first molars or what to do when nonextraction treatment fails. Am J Orthod 1979;76: 376-93. Stalpers et al 323 9. Riolo ML, Moyers RE, McNamara JA Jr, Hunter WS. An atlas of craniofacial growth: cephalometric standards from the University School growth study. Craniofacial Growth Series. Ann Arbor: Center for Human Growth and Development; University of Michigan; 1974. 10. Richmond S, Shaw WC, O’Brien KD, Buchanan IB, Jones R, Stephens CD, et al. The development of the PAR index (peer assessment rating: reliability and validity). Eur J Orthod 1992; 14:125-39. 11. Richmond S, Shaw WC, Roberts CT, Andrews M. The PAR index (peer assessment rating): methods to determine the outcome of orthodontic treatment in terms of improvement and standards. Eur J Orthod 1992;14:180-7. 12. Dahlberg G. Statistical methods for medical and biological students. New York: Interscience Publications; 1940. 13. Shaw WC, Richmond S, O’Brien KD. The use of occlusal indices: a European perspective. Am J Orthod Dentofacial Orthop 1995;107:1-10. 14. Birkeland K, Furevik J, Boe OE, Wist PJ. Evaluation of treatment and posttreatment changes by the PAR index. Eur J Orthod 1997;19:279-88. 15. Richmond S, Shaw WC, Stephens CD, Webb WG, Roberts CT, Andrews M. Orthodontics in the general dental service of England and Wales: a critical assessment of standards. Br Dent J 1993;174:315-29. 16. DeGuzman L, Bahiraei D, Vig KW, Vig PS, Weyant MS, O’Brien KD. The validation of the peer assessment rating index for malocclusion severity and treatment difficulty. Am J Orthod Dentofacial Orthop 1995;107:172-6. 17. O’Brien KD, Shaw WC, Roberts CT. The use of occlusal indices in assessing the provision of orthodontic treatment by the hospital orthodontic service of England and Wales. Br J Orthod 1993;20:25-35. 18. Richmond S, Andrews M. Orthodontic treatment standards in Norway. Eur J Orthod 1993:15;7-15. 19. Dyken RA, Sadowsky PL, Hurst D. Orthodontic outcomes assessment using the peer assessment rating index. Angle Orthod 2001;71:164-9. 20. Buchanan IB, Russell JI, Clark JD. An illustrative comparison of the outcome of treatment using 2 fixed appliances techniques. Br J Orthod 1996;23:351-7. 21. Bishara SE, Jakobsen JR, Hession TJ, Treder JE. Soft tissue profile changes from 5 to 45 years of age. Am J Orthod Dentofacial Orthop 1998;114:698-706. 22. Nanda RS, Meng H, Kapila S, Goorhuis J. Growth changes in the soft tissue profile. Angle Orthod 1990;60:177-90. 23. Ricketts RM. Esthetics, environment, and the laws of lip relation. Am J Orthod 1968;54:272-89. 24. Katsaros C. Profile changes following extraction vs. nonextraction orthodontic treatment in a pair of identical twins. J Orofac Orthop 1996;57:56-9. 25. Burke PH, Hughes-Lawson CA. Stereophotogrammetric study of growth and development of the nose. Am J Orthod Dentofacial Orthop 1989;96:144-51. 26. Aras A. Vertical changes following orthodontic extraction treatment in skeletal open bite subjects. Eur J Orthod 2002;24:407-16.