SUBPUL OBSTR IN CONGENITALLY CORRECTED TGA/Krongrad et al.
Fallot: Analysis by His bundle recordings. Circulation 49: 214, 1974
14. James FW, Kaplan S: Unexpected cardiac arrest in patients after surgical
correction of tetralogy of Fallot. Circulation 52: 691, 1975
15. Kaplan S, McKinivan CE, Helmsworth JA, Benzing G III, Schwartz
DC, Schreiber JT: Complications following homograft replacement of
the right ventricular outflow tract. Ann Thorac Surg 18: 250, 1974
16. James FW, Kaplan S: Systolic hypertension during submaximal exercise
after correction of coarctation of the aorta. Circulation 50 (suppl II): II27, 1974
17. Goldberg SJ, Weiss R, Adams FH: Comparison of the maximal endurance of normal children and patients with congenital cardiac disease.
J Pediatr 69: 46, 1966
18. Goldberg SJ, Weiss R, Kaplan E, Adams FH: Comparison of work required by normal children and those with congenital heart disease to participate in childhood activities. J Pediatr 69: 56, 1966
679
19. Bengtsson E: The working capacity in normal children, evaluated by submaximal exercise on the bicycle ergometer and compared with adults.
Acta Med Scand 154: 91, 1956
20. Snedecor GW, Cochran WG: Statistical Methods, ed 3. Ames, Iowa
State College Press, 1967, p 59
21. !bid, p 172
22. Strieder DJ, Aziz K, Zaver AG, Fellows KE: Exercise tolera.nce after
repair of tetralogy of Fallot. Ann Thorac Surg 19: 397, 1975
23. Brodeur MTH, Lees MH, Bristow JD, Kloster FE, Griswold HE: Right
ventricular volumes in pulmonic valve disease. Am J Cardiol 19: 671,
1967
24. Gey GO, Levy RH, Pettet G, Fisher L: Quinidine plasma concentration
and exertional arrhythmia. Am Heart J 90: 19, 1975
25. Jelinek MV, Lohrbauer L, Lown B: Anti-arrhythmia drug therapy for
sporadic ventricular ectopic arrhythmias. Circulation 49: 659, 1974
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Subpulmonary Obstruction
in Congenitally Corrected Transposition of the Great Arteries
due to Ventricular Membranous Septal Aneurysms
EHUD KRONGRAD, M.D., KENT ELLIS, M.D., CARL N. STEEG, M.D.,
FREDERICK 0. BOWMAN, JR., M.D., JAMES R. MALM, M.D.,
AND WELTON M. GERSONY, M.D.
SUMMARY The clinical, hemodynamic, and angiographic observations, as well as the surgical approach used for repair in three
patients with congenitally corrected transposition of the great
arteries and ventricular membranous septal aneurysms, are
presented. In two of the three patients the membranous septal
aneurysm caused subpulmonary obstruction, with 94 and 125 mm Hg
systolic gradients. In each patient the aneurysm was demonstrated by
angiocardiography, which also showed differences in size and shape
with cardiac systole and diastole.
Review of the previously described reports indicates that patients
with congenitally c~rected transposition often display various forms
of pulmonary outflow obstruction and when a ventricular membranous septal aneurysm exists, a significant subpulmonary obstruction is present in most patients. The unique anatomic relationship
between the pulmonary artery and a ventricular membranous septal
aneurysm in patients with transposition of the great arteries with and
without atrioventricular discordance explains why subpulmonary
obstruction sometimes develops.
VENTRICULAR MEMBRANOUS SEPTAL ANEURYSMS are commonly found in small, uncomplicated ventricular septal defects. Over the last decade, numerous
reports have described the clinical, anatomic, hemodynamic, and angiographic findings associated with these
lesions and their possible complications.15
In patients with normal ventricular development, atrioventricular (A-V) concordance and normally related great
arteries, the aneurysms are often described as incidental
findings following angiocardiographic studies and only
rarely cause right ventricular outflow obstruction. Ventricular membranous septal aneurysms in patients with transposition of the great arteries (TGA) with and without A-V
concordance and ventricular septal defects have been
reported rarely.2 6-11 When present, however, these
aneurysms usually caused significant subpulmonary obstruction.
The purpose of this report is to present the clinical, hemodynamic, and angiographic findings of three patients with
congenitally corrected transposition of the great arteries and
ventricular membranous septal aneurysms recently operated
upon at the Columbia-Presbyterian Medical Center. In two
of the three patients the ventricular membranous septal
aneurysm caused significant subpulmonary obstruction. The
unique relationship between the ventricular septal defect and
the pulmonary valve in these cases makes it likely that ventricular membranous septal aneurysms will result in significant subpulmonary obstruction. We believe that these
findings are of special significance at this time when an increasing number of children with various forms of transposition of the great arteries are being referred for surgical
correction.
For the purpose of this presentation the authors define
congenitally corrected transposition as the congenital cardiac anomaly resulting from atrioventricular discordance
and transposition of the great arteries such that both great
arteries arise from the inappropriate ventricle.12
From the Departments of Pediatrics, Radiology and Surgery, College of
Physicians and Surgeons, Columbia University and the Presbyterian
Hospital, New York, New York 10032.
Supported in part by research grant HE-12738-07, from the National
Heart and Lung Institute, U.S. Public Health Service.
Address for reprints: Ehud Krongrad, M.D., Department of Pediatrics,
Babies Hospital, Division of Pediatric Cardiology, 3975 Broadway, New
York, New York 10032.
Received March 4, 1976; revision accepted May 17, 1976.
680
CI RCULATION
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Clinical Observations
Table 1 summarizes the clinical, electrocardiographic,
and roentgenographic findings in the three patients with congenitally corrected transposition seen in our institution. All
three patients had situs solitus. Two patients were asymptomatic and one patient had severe left-sided A-V valve insufficiency and congestive heart failure. Two patients had
tiny ventricular septal defects and in one patient the ventricular membranous septal aneurysm was completely intact.
The hemodynamic data are presented in table 2. The
femoral arterial oxygen saturation ranged between 95-97%
and in none of the cases was there evidence of an intracardiac left-to-right shunt by oxygen saturation analysis. In two
patients the anatomical left ventricular pressure (subpulmonic right-sided ventricle) exceeded systemic ventricular pressure, with a subvalvar peak systolic gradient of 94
and 125 mm Hg. There was no pressure gradient recorded at
the subvalvar region in the other child.
In each of the patients the diagnosis of ventricular membranous septal aneurysm was made by angiocardiography.
Figure I shows anteroposterior and lateral views of a selective ventricular (anatomic left ventricle) angiocardiogram in
diastole and in systole in the patient with a subpulmonary
systolic gradient of 94 mm Hg. A filling defect is clearly seen
at the subpulmonary region, indicating the presence of the
ventricular membranous septal aneurysm.
Serial biplane films and cineangiocardiograms revealed a
distinct change in the systolic and diastolic location and
appearance of the filling defect. With ventricular systole the
aneurysm decreased in size, became flattened, and moved
upward toward the pulmonary orifice (fig. IA, IC).
Figure 2A shows an anatomical left ventricular injection
in the 14-year-old patient with congenitally corrected transposition and dextrocardia. The filling defect in the subpulmonary region (fig. 2A) is due to the ventricular membranous septal aneurysm. In figure 2B the aneurysm is
clearly seen filled with contrast material.
TABLE 1. Patient Data
Patient
SM
Age (yr)
Sex
Symptoms
Segmental Descrip.'3
Cardiac Position
Murmurs
Systolic
5
Diastolic
S2
S3
ECG
P-R (sec)
FAQRS
qVY
R/S V, (mm)
R/S V6 (mm)
Chest X-ray
C/T Ratio
PVM
Aortic Arch
TB
MC
8
Male
None
(S,L,L)
(S,L,L)
Levocardia Dextrocardia
14
Female
CHF
5/6 LSB
2/6 Ap.
None
Single
4/6 LSB
4/6 Ap.
Absent
None
Single
Absent
2/6 Ap.
Single
Present
0.16
0.14
+900
+900
Present
20/0
20/12
Absent
14/17
3/0
0.22
+600
Absent
12/6
4/4
Increased
Normal
Left
Normal
Normal
Left
Increased
Increased
Left
Male
None
(SL,L)
Dextrocardia
Abbreviations: LSB = left sternal border; Ap = apical; C/T = cardiothoracic; CHF = congestive heart failure; S2 and Ss = second and third
heart sounds; PVM = pulmonary vascular markings; FAQRS = direction of QRS vector in the frontal plane.
VOL 54, No 4, OCTOBER 1976
Following cardiac catheterization, all three patients underwent open heart surgery for repair of their defects.
Surgical correction was carried out by excision of the
aneurysm and ventricular septal defect closure in two
patients and plication of the aneurysm in one patient.
Because of an additional subpulmonary stenosis in one of
the former patients, a dacron conduit incorporating a porcine valve (Hancock prosthesis) was used to bypass the
obstruction. Sutures were placed in the fibrotic rather than
muscular portions of the septum in order to avoid injury to
the bundle of His, which crosses in these cases anterior and
superior to the ventricular septal defect.'4 15
Discussion
Although ventricular membranous septal aneurysms have
been described in association with a number of congenital
cardiac anomalies, the association with transposition of the
great arteries with or without A-V discordance is rather
rare.', 6-1 We are aware of several previously published
reports of congenitally corrected transposition who had ventricular membranous septal aneurysms.2' 6-8,11 Most of the
previously reported cases deal with the pathological description of this congenital malformation. Including the present
series, available hemodynamic data revealed that the
anatomical left ventricular pressure was similar to or exceeded systemic pressure in six of eight cases. These findings
indicate that ventricular membranous septal aneurysms in
association with congenitally corrected transposition are
likely to cause subpulmonary obstruction.
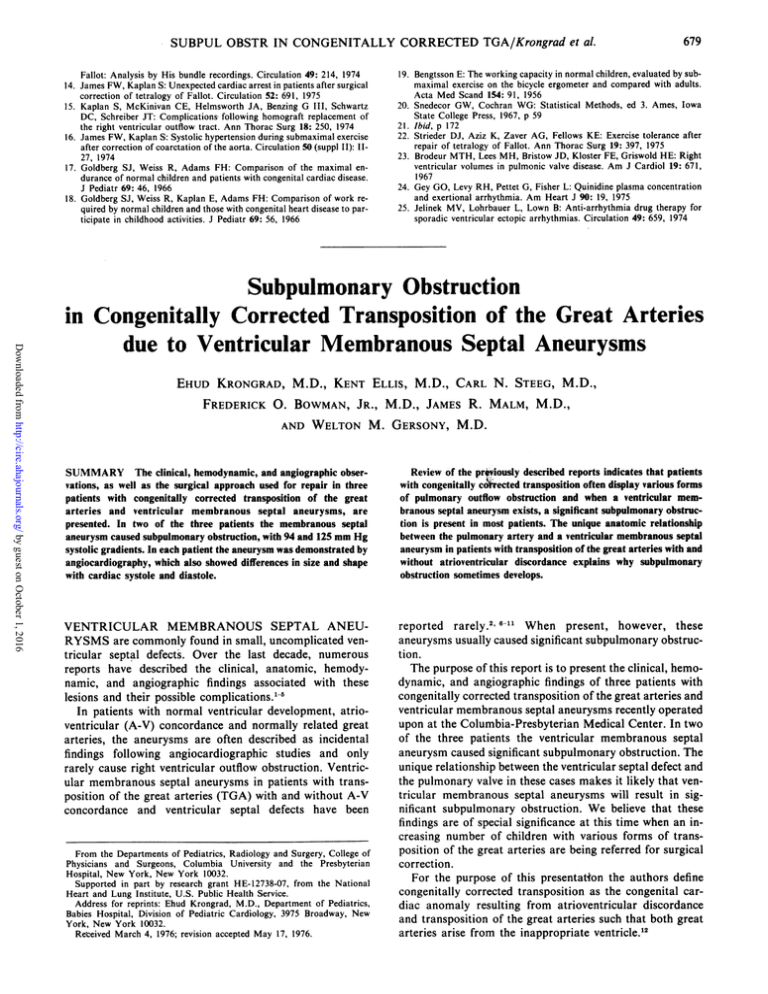
This phenomenon is related in part to the intraventricular
anatomy in these patients. With normal ventricular anatomy
and viscero-atrial concordance, the pulmonary artery is
separated from the tricuspid valve by the conus arteriosus,
(fig. 3). The membranous ventricular septal defect lying inferior to the conus arteriosus is separated from the pulmonary valve by the crista supraventricularis and is below
the infundibulum. In this situation it is unlikely that a ventricular membranous septal aneurysm will cause severe
obstruction to the subpulmonary region. In contrast, in
patients with congenitally corrected transposition, the
pulmonary valve is usually in continuity with the right-sided
A-V valve. The ventricular septal defect is adjacent and immediately inferior to the pulmonary valve, and there is no interposed crista supraventricularis (fig. 3). When a ventricular membranous septal aneurysm occurs in this situation it
lies virtually within the pulmonary valve orifice and is likely
to cause a significant subpulmonary obstruction.
It has been previously suggested that the direction toward
which the aneurysm develops (e.g., within the right or left
TABLE 2. Hemodynamic Findings in Three Patients with
Congenitally Corrected Transposition and Ventricular Membranous Septal Aneurysm
Pt.
No.
Pressures (mm Hg)
02 Saturation (%)
Tricuspid
LV
MPA Systemic MVB MPA FA Qp/Qs Insufficiency
1 114/5 20/6 95/5* 77
2 145/15 20/10 120/80t 68
3 55/10 55/30
59
77
68
59
95
97
1:1
1:1
96
1:1
0
+1
+3
*Anatomical right ventricular pressure.
tFemoral artery pressure.
Abbreviations: LV = anatomical left ventricle; MPA = main pulmonary artery; MVB = mixed venous blood; Qp/Qs = pulmonary to systemic flow ratio.
SUBPUL OBSTR IN CONGENITALLY CORRECTED TGA/Krongrad et al.
681
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
FIGURE 1. Simultaneous anteroposterior and lateral views of an
anatomical left ventricular angiocardiogram in a patient with congenitally corrected transposition, ventricular septal defect, and a
membranous septal aneurysm in diastole (A and B) and in systole
(C and D). Note the filling defect (A, arrows) below the pulmonary
artery. Also note the differences in size, shape and location of the
aneurysm between diastole (arrows, A) and systole (arrow, C).
ventricle) relates to the differences in pressure between the
two cardiac chambers.2' In two of our patients the ventricular membranous septal aneurysm bulged toward the left
ventricle and into the subpulmonary region, although the
anatomical left ventricular pressure exceeded systemic
pressure. It appears likely that the ventricular membranous
septal aneurysm originally developed within the anatomical
left ventricle, when the pressure was low. As the aneurysms
682
VOL 54, No 4, OCTOBER 1976
CIRCULATION
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
FIGURE 2. A) An anatomical left ventricular injection in the
anteroposterior view in a patient with dextrocardia, congenitally
corrected transposition, ventricular septal defect and a ventricular
membranous septal aneurysm. The filling defect due to the membranous septal aneurysm is marked by arrows. B) An anatomical
right ventricular injection in the same patient. The ventricular membranous septal aneurysm (arrows) is clearly seen protruding into the
anatomical left ventricle.
gradually enlarged, increased systolic gradients developed
across the subpulmonary regions. It is reasonable to assume
that when the anatomical left ventricular pressure reached
or exceeded systemic pressure, the aneurysms were established by virtue of size and their final positions were no
longer dependent on ventricular pressure relationships.
S
ar R
FIGURE 3. Schematic drawing of hearts with
normal ventricular anatomy [S,ED Sj(on the right)
and congenitally corrected transposition [S,L,LI
(on the left) to demonstrate ventricular septal
defect to pulmonary artery relationship. Note that
in patients with normal cardiac anatomy the septal defect is separated from the pulmonary artery
by the conus arteriosus and in most cases by the
crista
supraventricularis.
In contrast, in patients
with congenitally corrected transposition the ventricular septal defect is adjacent to the pulmonary
valve.
SUBPUL OBSTR IN CONGENITALLY CORRECTED TGA/Krongrad et al.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
The ventricular membranous septal aneurysms in our
patients changed shape and relationship to the pulmonary
valve during systole and diastole. In diastole, the filling
defects due to the aneurysms are larger and somewhat lower
in the anatomical left ventricular chamber. In our two
patients in whom the pressure in the anatomical left ventricle exceeded the pressure in the anatomical right ventricle,
the obstructing ventricular membranous septal aneurysms
became smaller during systole and shifted toward the pulmonary valve. This phenomenon could be seen particularly
well with cineangiographic studies.
Patients with congenitally corrected transposition often
have various forms of pulmonary outflow obstruction."'
Among nine children with congenitally corrected transposition recently operated upon at our institution, seven had
some type of pulmonary obstruction; two patients had pulmonary valve stenosis, one had isolated infundibular
stenosis, one had pulmonary infundibular and valvar
stenosis, one had pulmonary atresia and two had obstructive ventricular membranous septal aneurysms. Four of the
nine patients required insertion of a Hancock prosthesis
from the anatomical left ventricle to the pulmonary artery in
order to bypass the pulmonary obstruction.
In each of the nine patients, the intraventricular conduction system was identified electrophysiologically and was
found to be superior and anterior to the septal defects, as
previously described.14 15 All nine remained in normal sinus
rhythm following completion of surgery. In one patient who
required repeat surgery for a residual ventricular septal
defect, the precise location of the conduction system was not
identified at the second operation and complete heart block
ensued.
Improvement in surgical techniques during the past few
years and the ability to localize the cardiac conduction
system during open heart surgery has allowed an increasing
number of patients with congenitally corrected transposition to undergo open heart correction. In such patients it is
of utmost importance that a precise anatomic diagnosis is
made. It may be expected that with the increase in the
683
number of children with congenitally corrected transposition referred for surgical correction, subpulmonary obstruction secondary to ventricular membranous septal aneurysm
will be more frequently encountered.
References
1. Freedom RM, White RD, Pieroni DR, Varghese PJ, Krovetz LI, Rowe
RD: The natural history of the so-called aneurysm of the membranous
ventricular septum in childhood. Circulation 49: 375, 1974
2. Baron MG, Wolf BS, Grishman A, Van Mierop LHS: Aneurysm of the
membranous septum. Am J Roentgenol 91: 1303, 1964
3. Varghese PJ, Izukawa T, Celermajer J, Simon A, Rowe RD: Aneurysm
of the membranous ventricular septum: A method of spontaneous closure
of small ventricular septal defects. Am J Cardiol 24: 531, 1969
4. Pombo E, Pilapil VR, Lehan PH: Aneurysm of the membranous ventricular septum. Am Heart J 79: 188, 1970
5. Yarum R, Griffel B: Aneurysm of interventricular septum with subaortic
stenosis. J Pathol Bacteriol 88: 93, 1964
6. Summerall CP, Clowes GHA, Boone JA: Aneurysm of ventricular septum with outflow obstruction of the venous ventricle in corrected transposition of great vessels. Am Heart J 72: 525, 1966
7. Greene RA, Mesel E, Sissman NJ: The windsock syndrome: Obstructing
aneurysm of the interventricular septum associated with corrected transposition of the great vessels. (abstr) Circulation 36 (suppl II): II-125,
1967
8. Falsetti HL, Anderson MN: Aneurysm of the membranous ventricular
septum producing right ventricular outflow tract obstruction and left ventricular failure. Chest 59: 578, 1971
9. Vidne BA, Subramanian S, Wagner HR: Aneurysm of the membranous
ventricular septum in transposition of the great arteries. Circulation 53:
157, 1976
10. Shaher RM, Puddu GC, Khoury G, Moes CAF, Mustard WT: Complete
transposition of the great vessels with anatomic obstruction of the outflow tract of the left ventricle. Am J Cardiol 19: 658, 1967
11. Anderson RH, Becker AE, Gerlis LM: The pulmonary outflow tract in
classically corrected transposition. J Thorac Cardiovasc Surg 69: 747,
1975
12. Van-Praagh R: What is congenitally corrected transposition? N Engl J
Med 282: 1097, 1970
13. Van-Praagh R, Durnin RE, Jockin H, Wagner H, Korms M, Garabedian
H, Ando M, Calder AL: Anatomically corrected malposition of the great
arteries [S,D,L]. Circulation 51: 20, 1975
14. Kupersmith J, Krongrad E, Gersony WM, Bowman FO Jr.: Electrophysiological identification of the specialized conduction system in corrected transposition of the great arteries. Circulation 50: 795, 1974
15. Waldo AL, Pacifico AD, Bargeron LM, James TN, Kirklin JW: Electrophysiological delineation of the specialized A-V conduction system in
patients with corrected transposition of the great vessels and ventricular
septal defect. Circulation 52: 435, 1975
Subpulmonary obstruction in congenitally corrected transposition of the great arteries
due to ventricular membranous septal aneurysms.
E Krongrad, K Ellis, C N Steeg, F O Bowman, Jr, J R Malm and W M Gersony
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Circulation. 1976;54:679-683
doi: 10.1161/01.CIR.54.4.679
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1976 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/54/4/679
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/