The Spine Journal 14 (2014) 1712–1721
Clinical Study
Microwave diathermy for treating nonspecific chronic neck pain: a
randomized controlled trial
on Cer
on Fernandez, PTb,
Juan Alfonso Andrade Ortega, MD, PhDa,*, Encarnaci
Rosario Garcıa Llorent, PTb, Marisa Ribeiro Gonzalez, PTb,
Alberto Damian Delgado Martınez, MD, PhDc,d
a
Department of Physical Medicine and Rehabilitation, Complejo Hospitalario de Jaen, Avenida del Ejercito Espa~nol, s/n, 23005 Jaen, Spain
b
Physiotherapy Unit, Complejo Hospitalario de Jaen, Avenida del Ejercito Espa~nol, s/n, 23005 Jaen, Spain
c
Department of Orthopedic Surgery, Hospital ‘‘San Agustın’’, Avenida de San Cristobal, s/n, Linares, 23700 Jaen, Spain
d
University of Jaen, Campus de las Lagunillas, s/n, 23071 Jaen, Spain
Received 27 May 2012; revised 12 September 2013; accepted 17 October 2013
Abstract
BACKGROUND CONTEXT: Although the use of deep heat therapy is widespread, there is scant
literature available on its effectiveness in treating back or neck pain.
PURPOSE: The purpose of this study was to determine the efficacy of microwave diathermy to
treat nonspecific chronic neck pain.
DESIGN: The study was designed as a double-blind, randomized controlled trial.
PATIENT SAMPLE: The patient sample consisted of 149 patients with nonspecific chronic neck
pain in a hospital of the Andalusian Public Health Care System, Spain
OUTCOME MEASURES: The study outcome measures are as follows: at baseline, pain intensity
(using a visual analogue scale), disability (Neck Disability Index), and health-related quality of life
(36-item short form health survey [SF-36]); at 3 weeks, baseline measures and patients’ perceived
overall outcome and satisfaction with the treatment; and at 6 months, 3–week measures, therapeutic
co-interventions, and adherence to exercises.
METHODS: Patients were allocated randomly to three groups. The first group received continuous
microwave diathermy, the second group was administered pulsed microwaves, and the third group
(the control group) received unplugged microwaves. All three groups received the same general
treatment: range of motion, isometric exercises, and transcutaneous electrical nerve stimulation.
RESULTS: The three groups had reduced pain and disability, and improvement was seen in some
dimensions of the SF-36. However, there were no differences found in any of the parameters measured among the three therapeutic groups.
CONCLUSIONS: Microwave diathermy does not provide additional benefit to a treatment regimen of chronic neck pain that already involves other treatment approaches. Ó 2014 Elsevier
Inc. All rights reserved.
Keywords:
Neck pain; Microwaves; Diathermy; Physical therapy modalities; Exercise; Transcutaneous electrical stimulation
Introduction
Neck pain is a common and expensive condition [1]. Its
age-adjusted prevalence ranges from 67% to 86% [2,3].
FDA device/drug status: Approved (microwave diathermy and TENS
[transcutaneous electrical nerve stimulation]).
Author disclosures: JAAO: Support for travel to meetings for the
study or other purposes: Instituto de Salud ‘‘Carlos III’’ (B); Provision
of writing assistance, medicines, equipment, or administrative support:
Instituto de Salud ‘‘Carlos III’’ (B). ECF: Nothing to disclose. RGL:
Nothing to disclose. MRG: Nothing to disclose. ADDM: Nothing to disclose.
1529-9430/$ - see front matter Ó 2014 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.spinee.2013.10.025
Neck pain increases with age and is more frequent in women than men, although such bias is not accepted unanimously by all experts [3]. About 50% to 80% of neck
The disclosure key can be found on the Table of Contents and at
www.TheSpineJournalOnline.com.
This study was supported by a research project from the Instituto de
Salud Carlos III (PI11/087). There is no topic-specific conflict of interest
related to the authors of this study.
* Corresponding author. C/Dr Federico del Castillo, 8, 1 E, 23005Jaen, Spain. Tel.: 34679650663.
E-mail address: juanalfonsoandrade@gmail.com (J.A. Andrade Ortega)
J.A. Andrade Ortega et al. / The Spine Journal 14 (2014) 1712–1721
pain cases are not fully resolved, and thus become chronic
and cause significant direct and indirect costs [4–6]. Most
direct costs are generated by physical treatments, including
patient education and counseling, exercises, manual therapies, and electrothermal therapies [6,7]. However, only
physical exercise—alone or combined with manual therapies—is supported by solid scientific evidence [8].
Although the use of electrophysical agents is widespread,
little evidence is available on its effectiveness in neck pain
[5,9]. Kroeling et al. [5] concluded there is no scientific evidence—either limited or contradictory—on the effectiveness of galvanic currents, iontophoresis, transcutaneous
electrical nerve stimulation (TENS), pulsed electromagnetic fields, electrical muscle stimulation, and permanent
magnets.
Considering the number of patients seeking treatment
for neck pain, surprisingly few studies have addressed the
physical interventions used in such cases, especially for
heat therapy, for which there is a great variability in use
[10]. A lack of uniformity in heat use for this patient population is illustrated by several studies. From the report by
Jette and Jette [11] in 1996 to the report by Boissonnault
and Badke [10] in 2008, ‘‘usual treatment’’ for patients
with neck pain provided by physiotherapists includes the
use of heat modalities in a range that goes from 91% of
the first to less than 17% of the latter. From a recent survey
in North Carolina, Goode et al. [12] found that heat was
used by 57% of people with neck pain. These authors note
that, based on current evidence for best practice, their findings indicate overuse of modalities and underuse of effective treatments such as therapeutic exercise.
A cross-sectional study [13] of the Spanish National
Health Service in the Canary Islands, where the public
health service covers a total population of two million
people, showed that as much as 60% of the resources spent
on physical treatments for nonspecific chronic neck pain,
back pain, and shoulder pain between 2004 and 2007 were
allocated to treatments that were found to be either ineffective or for which there was no evidence of effectiveness. Heat therapy was a major part of these physical
treatments.
Microwave diathermy once had a place in therapy, but
since the 1980s, interest in its use has declined in many
countries, more than shortwave diathermy or ultrasound
[14–16]. The Food and Drug Administration [14] differentiates between diathermy devices according to their thermal
or nonthermal mechanism of action. Specifically, it separates diathermy devices into ‘‘diathermy for use in applying
therapeutic deep heat for selected medical conditions’’ and
‘‘diathermy intended to treat medical conditions by means
other than the generation of deep heat.’’ Today, most commercial devices allow both types of application. Microwave
diathermy is a form of electromagnetic energy that uses its
conversion to thermal energy, which is produced by increased kinetic energy of molecules within the microwave
field; radiation is absorbed selectively by water, and muscle
1713
Context
Microwave diathermy is a treatment used at some centers for neck and back pain. The authors present the results of their RCT for patients with chronic nonspecific
neck pain.
Contribution
They found that the microwave treatment made no impact compared to a sham procedure. These data suggest
that observed patient improvements were due to other
matched co-interventions, natural history, or a generalized placebo effect.
Implications
The findings indicate that patients in this specific group
do not benefit from the study treatment. Unless other
studies conflict with these findings, risks and costs of
this procedure can be avoided. An open mind to other
biologically feasible applications (eg, different patient
groups) is reasonable.
—The Editors
should be heated preferentially. Fourteenth Federal Communications Commission-approved frequencies for therapeutic microwave are 915 MHz and 2,450 MHz. The
lower frequency has the advantage of increased depth of
penetration but also the disadvantages of greater beam dispersion and the requirement of larger applicators [14].
Microwaves do not penetrate tissue as deeply as shortwave diathermy and ultrasound. Shortwave therapy is generally preferred over microwave because it has a more
predictable heat distribution pattern [14,15]. Recently, particularly in Europe, microwaves are being used at 434 MHz
and, therefore, are realizing increased penetration [17–20].
Because of this, microwave diathermy seems to have
become popular again, as evidenced by trials looking at
its effectiveness in knee osteoarthritis [17] and other musculoskeletal conditions [18–20].
Indications and contraindications of microwave and shortwave therapy are practically the same [15,16]. In a trial conducted with patients with nonspecific neck pain (most of
them chronic), the use of pulsed shortwave diathermy in
combination with physical exercise and patient counseling
did not improve patients’ health status [21]. Consequently,
the efficacy of pulsed shortwave diathermy has been questioned by some authors [22]. Studies on the efficacy and
cost-effectiveness of the therapies used to treat neck pain
are required [23]. Because of the significant lack of supporting studies about diathermy and the considerable economic
burden for many health systems [13], it is important to clarify
the role to be played by these physical modalities. No trials
have been conducted on the effectiveness of microwaves in
patients with neck pain. This study is intended to determine
1714
J.A. Andrade Ortega et al. / The Spine Journal 14 (2014) 1712–1721
the effectiveness of microwave diathermy in treating nonspecific chronic neck pain.
Methods
A double-blind, randomized controlled trial was conducted with 149 patients with nonspecific chronic neck pain
in a hospital of the Andalusian Public Health Care System
in Jaen, Spain. The patients were referred from a primary
care setting to the Department of Rehabilitation between
September 2008 and December 2010, because of failure
of the treatment prescribed by the general practitioner. Subjects were recruited consecutively when they met the
requirements described later. Most people in Jaen, a rural
area in southern Spain, are covered by the public health
care system. Patients’ epidemiological data are shown in
Table 1. The trial was approved by the ethics committee
of the hospital. The eligibility criteria were patients
between 18 years and 65 years with a diagnosis of nonspecific chronic neck pain, ie, 3-month or longer duration, and
the absence of red flags (clinical features that indicate an
increased risk of specific conditions) such as weight loss,
fever, progressive neurologic signs, cancer history, infectious or inflammatory disease history, osteoporosis, or
major structural abnormalities or neurologic conditions
affecting the neck. Exclusion criteria included women
who were pregnant, individuals on sick leave or involved
in a lawsuit or claim process in which neck pain was the
cause, and subjects with a pacemaker, metal implants, or
any other device that contraindicated the use of microwaves
[15,16]. This study was registered under the unique identifier NCT01487122 (www.clinicaltrials.gov).
Table 1
Baseline values
Variable
Total
N
149
Age, y (SD)
Males, n (%)
Females, n (%)
BMI, kg/m2 (SD)
LA, n (%)
HA, n (%)
VAS, pt (SD)
NDI, pt (SD)
SF-36, pt (SD)
PF, pt (SD)
RP, pt (SD)
RE, pt (SD)
BP, pt (SD)
SF, pt (SD)
VT, pt (SD)
GH, pt (SD)
MH, pt (SD)
44.2
36
113
24.9
93
56
53.5
34.4
56.5
72.7
36.9
53.3
42.1
71.5
51.6
47.5
58.5
C
P
50
(10.1)
(24.1)
(75.9)
(3)
(62.4)
(37.6)
(15.8)
(12.1)
(14.9)
(22.9)
(42.9)
(46.7)
(20.8)
(22.3)
(12.8)
(12.6)
(8.4)
43.6
13
37
24.6
33
17.0
52.9
34.4
55.4
69.8
31.0
52.7
39.0
72.0
52.0
49.3
60.8
U
48
(11.2)
(26)
(74)
(3.2)
(66)
(34)
(16.7)
(11.9)
(14.5)
(26.3)
(42.1)
(44.7)
(22.5)
(20.8)
(12.4)
(10.2)
(6.3)
45.5
10
38
25.2
29
19.0
54.7
33.6
60.1
79.1
46.9
59.8
43.8
76.3
51
47.5
57.1
51
(7.9)
(20.8)
(79.2)
(3.2)
(60.4)
(39.6)
(13.9)
(12.5)
(15.6)
(19.8)
(42.1)
(48.1)
(19.5)
(21)
(15.7)
(14.3)
(10)
43.6
13
38
24.9
31
20.0
53
35.2
54.1
69.6
33.3
47.7
43.6
66.4
51.8
45.7
57.5
(10.9)
(25.5)
(74.5)
(2.5)
(60.8)
(39.2)
(16.9)
(12.1)
(14.3)
(21.2)
(43.5)
(47.3)
(20.4)
(24.3)
(10.2)
(13)
(8.1)
BP, bodily pain; BMI, body mass index; C, continuous microwave;
GH, general health perceptions; HA, heavy activity; LA, light activity;
MH, mental health; NDI, Neck Disability Index; P, pulsed microwave;
PF, physical functioning; RE, role emotional; RP, role physical; SD, standard deviation; SF, social functioning; SF-36, 36-item short form health survey; U, unplugged microwave; VAS, visual analogue scale; VT, vitality.
After informed consent was obtained, patients were
randomized to three treatment arms (Group C, continuous
microwave; Group P, pulsed microwave; or Group U, unplugged microwave) using a series of random, repeating
three possible figures generated by free software. This
series was only known by the chief of physiotherapists,
who allocated to each figure a treatment group before
starting the trial. In the rehabilitation department, the same
two physiotherapists delivered 15 physical treatment
sessions (five per week for 3 weeks) according to each
group schedule. The rationale for the use of 15 sessions
in 3 weeks has been reported elsewhere [24]. The comprehensive treatment included, in this order, range of motion
and isometric exercises (initially in treatment room and,
after 3 weeks, at home), TENS, and diathermy. The latter
was provided differently according to the treatment arm.
Group C received continuous microwaves, Group P
received pulsed microwaves, and Group U received unplugged microwaves. One of the physiotherapists conducted the exercises, and the other administered TENS
and microwaves.
Exercise included monitored free movements and resisting elastic band isometric exercises of the cervical spine
(flexion, extension, left and right rotations, and left and
right lateral bending), and raising and forward and rearward
rotation of the shoulders. Each exercise was performed 10
times with patients sitting in front of a mirror, their back
against the backrest of a chair, and their feet touching the
ground. The position was maintained for 5 seconds after
each exercise. All patients were instructed to perform the
learned exercises at home, a minimum of three times per
week indefinitely.
Transcutaneous electrical nerve stimulation was performed using the Enraf-Nonius Tensmed 911 model (Rotterdam, Netherlands) through four 55-cm square
electrodes. One pair was placed between C5 and C7 (on
both sides) and the other pair was placed on the upper fibers
of the trapezius. We used the continuous mode at a frequency of 80 Hz, with a pulse duration of 150 microseconds. Intensity was adjusted to produce a tingling
sensation, and TENS was delivered for 30 minutes. Similar
parameters have been used by others [24].
Microwaves were delivered using the Enraf-Nonius Radarmed 12S259 generator (Rotterdam, Netherlands).
Group C received continuous microwaves at 80 W for
20 minutes through a large circular electrode placed 15
cm from the neck. Individuals in Group P received pulsed
microwaves (mean power, 5 W) using the same conditions
as group C. Similar doses have been used elsewhere [25].
Group U was provided with the same therapy, but the device was unplugged and a light-emitting diode induced patients to think that the device was operating. At all times
the patients did not know to which treatment arm they
were assigned.
During the medical consultation before the treatment,
patients were informed of the importance of performing
J.A. Andrade Ortega et al. / The Spine Journal 14 (2014) 1712–1721
1715
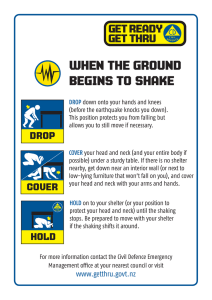
Figure. Flow of participants through each stage of the trial.
their exercises at home. They were allowed to take any pain
relief medication as necessary, and were asked to record
their analgesic medication intake. Similarly, patients were
asked to record any therapeutic co-interventions received
during the follow-up, especially if they attended physiotherapy sessions outside the public health system. At all
times, except for the therapist who administered
electrothermal therapy and the chief of physiotherapists
(who did not participate directly in the treatment), all professionals were blinded to treatment allocation.
Before the treatment started, the following variables
were recorded: age, sex, body mass index, and intensity
of work activity (‘‘light’’ for nonphysically demanding
jobs, and ‘‘heavy’’ for physically demanding jobs).
1716
J.A. Andrade Ortega et al. / The Spine Journal 14 (2014) 1712–1721
Table 2
Pain at baseline, after treatment, and at 6 months
Pain intensity
Total
C
P
U
General linear model
N
141
45
47
49
Within subjects (time)
Between subjects
(timegroup)
VAS at baseline pt (SD)
VAS after treatment, pt (SD)
VAS at 6 mo, pt (SD)
52.9 (15.8)
37.2 (21.5)
37.3 (21.1)
52.8 (17.4)
36.0 (19.8)
36.1 (18.6)
53.7 (13.6)
39.4 (21.3)
37.7 (19.6)
52.1 (16.5)
36.2 (23.4)
38.1 (24.7)
p!.001
p5.420
C, continuous microwave; P, pulsed microwave; U, unplugged microwave; VAS, visual analogue scale.
Note: Measures are average values (standard deviation).
Housework, which as highly represented in our sample, was
included in the ‘‘heavy’’ category.
The primary outcome was pain intensity. Secondary outcomes were disability for cervical pain, health-related quality of life, patients’ perceived overall outcome, satisfaction
with the treatment, therapeutic co-interventions, and adherence to exercise. Outcome measures were obtained at session 1, session 15, and at 6 months by a physiotherapist
blinded with respect to the treatment groups. At three time
points (session 1, session 15, and at 6 months), pain intensity was measured using a visual analogue scale (a tool for
measuring pain intensity, the use of which is widespread
[26]), disability in terms of cervical pain was measured
according to the Neck Disability Index (NDI; the Spanish
version of the NDI has been validated [27,28]), and
health-related quality of life, which was measured according to the 36-item short form health survey (SF-36). Respect of this, overall value and each of the eight
dimensions values were assessed, including physical functioning, role physical, role emotional, bodily pain, social
functioning, vitality, general health perceptions, and mental
health. The Spanish version of the SF-36 was validated by
Alonso et al. [29]. At session 15, additional parameters assessed were as follows: patients’ perceived overall outcome
according to a 6-point scale for the measures excellent,
very good, good, fair, poor, and very bad (a similar scale
has been used elsewhere for measuring perceived outcome
in neck pain [30]), and satisfaction with the treatment according to a 5-point scale for the measures very satisfied,
satisfied, neither satisfied or dissatisfied, dissatisfied, and
very dissatisfied. The latter scale is one of the items of an
NDI-based satisfaction questionnaire that has been used
elsewhere [31]. At 6 months, in addition to the parameters
measured at the other two time points, therapeutic cointerventions (narrative description) and adherence to
exercises (often, sometimes, or never) were further evaluated. The measurements taken at the beginning and on
completion of treatment were collected at the hospital,
whereas those taken at 6 months were collected by telephone and by mail.
A pilot clinical trial with 64 patients was performed previously. In this study, Groups C, P, and U achieved a mean visual analogue scale pain score relief of 17.76 points, 10.21
points, and 15.95 points after treatment, with an overall
standard deviation of 11.73 points. With these data, using
the sample size calculator Ene 2.0 (Department of Biometry,
Glaxo-Smith-Kline, Barcelona, Spain), it was established
that 133 patients were required, with p5.05 and a 0.80 power.
Because we predicted a dropout rate of 10%, 148 patients
were recruited. Statistical analysis was performed by the first
author, who was also blinded to treatment allocation. All
quantitative variables were transformed to normal distribution (Kolmogorov-Smirnov test). Analysis was done on an
intent-to-treat basis. A repeated-measures general linear
model was used to analyze numerical data such as pain,
disability, and health-related quality of life; time was
within-subject factor and therapeutic groups were the
between-subjects factor. The chi-square test was used for categorical data. Statistical significance was set at the 5% level
(two tailed). Analysis of the outcomes was performed using
SPSS version 15.0 (SPSS Inc., Chicago, IL, USA).
Results
The Figure shows the flow of participants through each
stage of the trial. Table 1 shows the distribution of baseline
values. Two patients from Group C and another two from
Group U dropped out of treatment, so a total of 145 patients
completed the treatment. The reasons given were job
Table 3
Disability at baseline, after treatment, and at 6 months
Disability
Total
C
P
U
General linear model
N
141
45
47
49
Within subjects (time)
Between subjects
(timegroup)
NDI at baseline, pt (SD)
NDI after treatment, pt (SD)
NDI at 6 mo, pt (SD)
33.9 (12.1)
25.8 (14.5)
23.3 (14.2)
34.1 (11.6)
25.2 (14.4)
23.1 (14.6)
32.8 (12.6)
25.3 (14.0)
22.2 (12.9)
34.9 (12.3)
26.8 (15.3)
24.7 (15.3)
p!.001
p5.923
C, continuous microwave; NDI, Neck Disability Index; P, pulsed microwave; U, unplugged microwave.
Note: Measures are average values (standard deviation).
J.A. Andrade Ortega et al. / The Spine Journal 14 (2014) 1712–1721
1717
Table 4
Perceived outcome and satisfaction, and adherence to treatment
Perceived outcome, satisfaction,
and adherence to exercise
Initial, N
After treatment, N
Perceived outcome after treatment, n (%)
Excellent
Very good
Good
Fair
Poor
Very bad
Satisfaction after treatment, n (%)
Very satisfied
Satisfied
Neither satisfied or dissatisfied
Dissatisfied
Very dissatisfied
After follow-up, N
Perceived outcome at 6 mo, n (%)
Excellent
Very good
Good
Fair
Poor
Very bad
Satisfaction at 6 mo, n (%)
Very satisfied
Satisfied
Neither satisfied or dissatisfied
Dissatisfied
Very dissatisfied
Adherence to physical exercise, n (%)
Often
Sometimes
Never
Total
C
P
U
149
145
50
48
48
48
51
49
p (Chi-square)
3
28
62
52
0
0
(2)
(19.3)
(42.8)
(35.9)
(0)
(0)
1
9
21
17
0
0
(2)
(18.8)
(43.8)
(35.4)
(0)
(0)
0
9
20
19
0
0
(0)
(18.8)
(41.7)
(39.6)
(0)
(0)
2
9
22
16
0
0
(4.1)
(18.4)
(44.9)
(32.7)
(0)
(0)
49 (33.8)
72 (49.7)
24 (16.6)
0 (0)
0 (0)
141
17
24
7
0
0
45
(35.4)
(50)
(14.6)
(0)
(0)
17
21
10
0
0
47
(35.4)
(43.8)
(20.8)
(0)
(0)
15
27
7
0
0
49
(30.6)
(55.1)
(14.3)
(0)
(0)
1
28
60
43
9
0
(0.6)
(19.9)
(42.6)
(30.5)
(6.4)
(0)
0
9
19
16
1
0
(0)
(20)
(42.2)
(35.6)
(2.2)
(0)
0
10
30
15
2
0
(0)
(21.3)
(63.8)
(31.9)
(4.3)
(0)
1
8
22
12
6
0
(2)
(16.3)
(44.9)
(24.5)
(12.2)
(0)
40
77
24
0
0
(28.4)
(54.6)
(17)
(0)
(0)
15
25
5
0
0
(33.3)
(55.6)
(11.1)
(0)
(0)
12
24
10
0
0
(25.5)
(51.1)
(21.3)
(0)
(0)
12
28
9
0
0
(24.5)
(57.1)
(18.4)
(0)
(0)
p5.77
p5.62
p5.91
p5.36
p5.52
30 (21.2)
60 (42.4)
51 (36.2)
9 (20)
22 (48.9)
14 (31.1)
8 (17)
22 (46.8)
17 (36.2)
13 (26.5)
16 (32.7)
20 (40.8)
C, continuous microwave; P, pulsed microwave; U, unplugged microwave.
incompatibility (one patient from Group C and two patients
from Group U) or housework incompatibility (one patient
from Group C). Another four patients dropped out at 6
months, three of whom could not be contacted (two from
Group C and one from Group P), and one patient refused to
continue participating in the study (Group C). Consequently,
a total of 141 patients completed the study. One patient from
Group C and another from Group U experienced dizziness on
one occasion after the therapy session. These symptoms were
relieved after a few minutes without any intervention. No other adverse reactions or side effects were reported.
Tables 2 and 3 show the improvements in pain and disability on treatment completion and after 6 months. Treatment arms did not influence the results. Pain relief was
maintained at the 6-month follow-up assessment, and the
reduction of disability was even greater after 6 months than
on treatment completion.
Table 4 shows the results in terms of patient satisfaction
on treatment completion and at 6 months after treatment;
therapeutic arms did not influence them. In the same way,
this table also shows that treatment arms did not influence
patients’ adherence to exercises at 6 months.
Table 5 shows that health-related quality of life improved by more than 11% in all groups. Again, therapeutic
arms did not influence the results. Improvements in role
physical, role emotional, bodily pain, and general health
perceptions after treatment and at 6 months were remarkable in all treatment arms.
Therapeutic co-interventions during the follow-up are
shown in Table 6. Treatment groups did not affect the final
outcome. None of the therapeutic co-interventions included
the use of any type of diathermy.
Discussion
The results suggest that continuous microwaves (thermal
effect), pulsed microwaves (athermal effect), and unplugged microwaves (placebo) have the same influence in
terms of pain or disability reduction. The same can be applied to the patients’ perceived outcome and satisfaction
with the treatment.
The minimal detectable and minimal clinically important changes have been explored for neck pain severity
[32]. Improvements less than or equal to 1.5 points in pain
1718
J.A. Andrade Ortega et al. / The Spine Journal 14 (2014) 1712–1721
Table 5
Health-related quality of life at baseline, after treatment, and at 6 months
Health-related quality of life
Total
C
P
U
General linear model
After treatment, N
141
45
47
49
Within subjects (time)
Between subjects
(timegroup)
SF-36 at baseline, pt (SD)
SF-36 after treatment, pt (SD)
SF-36 at 6 mo, pt (SD)
PF at baseline, pt (SD)
PF after treatment, pt (SD)
PF at 6 mo, pt (SD)
RP at baseline, pt (SD)
RP after treatment, pt (SD)
RP at 6 mo, pt (SD)
RE at baseline, pt (SD)
RE after treatment, pt (SD)
RE at 6 mo, pt (SD)
BP at baseline, pt (SD)
BP after treatment, pt (SD)
BP after treatment, pt (SD)
SF at baseline, pt (SD)
SF after treatment, pt (SD)
SF at 6 mo, pt (SD)
VT at baseline, pt (SD)
VT after treatment, pt (SD)
VT at 6 mo, pt (SD)
GH at baseline, pt (SD)
GH after treatment, pt (SD)
GH at 6 mo, pt (SD)
MH at baseline, pt (SD)
MH after treatment, pt (SD)
MH at 6 mo, pt (SD)
57.1
63.3
63.3
73.1
75.7
75.5
38.5
47.1
47.2
55.3
68.8
68.4
42.8
53.8
51.9
72.4
77.8
77.7
51.6
51.7
52.4
47.8
60.5
60.4
58.6
59.7
60.8
p!.001
p5.387
p5.011
p5.767
p5.006
p5.070
p!.001
p5.226
p!.001
p5.633
p!.001
p5.303
p5.520
p5.978
p!.001
p5.130
p5.048
p5.188
(15.0)
(15.2)
(15.1)
(23.0)
(23.5)
(23.3)
(43.4)
(42.7)
(42.8)
(46.4)
(41.4)
(41.2)
(20.9)
(23.6)
(24.9)
(22.2)
(21.0)
(21.0)
(12.9)
(11.3)
(9.9)
(12.7)
(16.7)
(17.0)
(8.4)
(5.9)
(8.0)
55.5
61.9
61.6
69.2
73.7
73.4
31.7
38.3
38.4
53.3
67.4
66.7
38.6
53.6
50.8
72.5
78.3
78.1
51.9
52.8
53.1
49.6
61.0
59.6
61.2
61.2
63.9
(14.3)
(13.5)
(13.3)
(26.6)
(23.7)
(23.6)
(42.4)
(38.7)
(38.9)
(44.6)
(40.5)
(40.0)
(22.1)
(21.1)
(21.9)
(20.2)
(18.6)
(18.5)
(12.1)
(10.6)
(9.60)
(10.6)
(14.8)
(16.3)
(6.3)
(6.5)
(11.1)
61.2
65.9
65.8
79.8
81.3
81.1
48.9
50.0
50.1
63.2
73.1
72.7
46.0
53.5
52.4
77.9
80.9
80.8
51.4
51.1
52.1
48.2
61.6
62.9
57.3
58.5
58.6
(15.7)
(16.2)
(16.1)
(19.9)
(21.4)
(21.1)
(42.7)
(43.9)
(44.0)
(47.3)
(40.9)
(40.7)
(19.6)
(25.6)
(28.3)
(20.6)
(22.1)
(20.8)
(15.9)
(11.9)
(10.7)
(13.9)
(18.6)
(18.3)
(9.8)
(5.6)
(5.4)
54.7
62.3
62.4
70.3
72.1
72.0
34.7
52.6
52.6
49.7
66.0
66.0
43.6
54.3
52.3
67.1
74.3
74.2
51.6
51.2
51.9
45.7
59.0
58.8
57.6
59.6
59.9
(14.3)
(15.7)
(15.7)
(21.2)
(24.6)
(24.6)
(43.8)
(43.0)
(44.8)
(47.2)
(41.4)
(43.3)
(20.8)
(24.0)
(24.3)
(24.4)
(22.2)
(20.8)
(10.3)
(11.4)
(9.5)
(13.1)
(16.6)
(16.5)
(8.2)
(5.2)
(5.6)
BP, bodily pain; C, continuous microwave; GH, general health perceptions; MH, mental health; P, pulsed microwave; PF, physical functioning; RP, role
physical; RE, role emotional; SF, social functioning; SF-36, 36-item short form health survey; U, unplugged microwave; VT, vitality.
Note: Measures are average values (standard deviation).
intensity could be seen as irrelevant, so our results suggest
that patients experienced significant improvement in pain
relief. The minimal detectable and minimal clinically important changes have also been explored for disability
[33]. For NDI, these values were 10.2 and 7.5, respectively.
Our results partially meet these requirements after treatment and fully meet them after the 6-month follow-up.
The Spanish version of the SF-36 was validated by
Alonso et al. [29]. The mean age in their study was 45.52
years, with a slight prevalence of women. The reference
values were as follows: physical functioning, 84.7 points;
role physical, 83.2 points; role emotional, 86.6 points; bodily pain, 79 points; social functioning, 90.1 points; vitality,
66.9 points; general health perceptions, 58.3 points; and
mental health, 73.3 points. Because our study included
patients with chronic pain, it is not surprising that the baseline scores obtained were low. As far as we know, minimal
clinically important changes have not been explored for
health-related quality of life in patients with neck pain. A
comparable study could be that of Escobar et al. [34],
who determined responsiveness and clinically important
differences for the SF-36 after total knee replacement (minimal clinically important differences were at least 10
points). On the basis of this study, our results suggest that
health-related quality of life did not improve after treatment
or after follow-up, although we could accept that some dimensions, such as role emotional, bodily pain, and general
health perceptions, did. Furthermore, allocation to a treatment arm did not influence the variations.
With regard to therapeutic co-interventions, allocation to
a specific treatment arm did not influence the outcome obtained. Similarly, no differences were found among the
three groups in terms of adherence to exercise.
The approach to nonspecific chronic neck pain tends to
be empirical, and many of the physical therapies provided
are of questionable efficacy. Physical treatments for patients with chronic neck pain include exercises, manual
therapies, and electrothermal therapies [6,7]. Only physical
exercise—alone or combined with manual therapies—is
supported by solid scientific evidence [8]. Although the
use of electrophysical agents is widespread, little evidence
is available on its effectiveness in neck pain [5,8,9]. Transcutaneous electrical nerve stimulation was effective for
patients with chronic neck pain in terms of disability, isometric neck muscle strength, and pain [35]. There is some
evidence supporting the use of low-level laser therapy for
pain reduction and functional improvement in the intermediate term for acute/subacute and chronic mechanical
J.A. Andrade Ortega et al. / The Spine Journal 14 (2014) 1712–1721
Table 6
Therapeutic co-interventions during the 6-month follow-up
Co-interventions
Total
C
P
U
At 6 mo, N
None, n
Paracetamol or metamizol, n
NSAIDs (with or without
paracetamol or
metamizol), n
Tramadol alone or combined
with paracetamol, n
Physiotherapy without
manual therapy*, n
Manual therapy*, n
141
41
40
29
45
16
13
8
47
13
14
11
49
12
13
10
15
4
4
7
4
1
1
2
12
4
3
5
p Value
p5.93 (chi-square)
C, continuous microwave; NSAIDs, nonsteroidal anti-inflammatory
drugs; P, pulsed microwave; U, unplugged microwave.
* In all cases, except for two, it was combined with paracetamol and/or
metamizol and/or NSAIDs and/or tramadol.
neck disorders [8]. There is no scientific evidence for using
ultrasound and other modalities. Pulsed shortwave diathermy did not provide any additional clinical benefit over
a short course of active physical treatment incorporating
advice and exercise [21]. Modalities are used mostly in
combination with exercise. Of these modalities, shortwave
and microwave diathermy are used in different ratios that
vary over time from country to country. From several surveys administered to specialists in physical medicine and
rehabilitation, rheumatologists, and physiotherapists, the
use of microwaves or shortwaves to treat neck or low back
pain was advocated by 22% to 47% of respondents [36–38].
In a report published in 1999 [39], the Danish Center for
Evaluation and Health Technology Assessment advised
against the use of ultrasound and shortwave diathermy in
the treatment of low back pain; however, in 2003, of the
12,387 treatments provided by 254 Danish physiotherapists, 22% included ultrasound and shortwave diathermy.
The European guide on low back pain [40] concluded that
there is no scientific evidence on the effectiveness of thermal therapy compared with placebo or other therapeutic
modalities in the treatment of chronic low back pain.
Scarce literature is available on electrothermal therapy
in the treatment of cervical pain. Dziedzic et al. [21] conducted a multicenter trial that included 350 patients (mean
age, 51 years) with nonspecific chronic neck pain who were
randomized to three groups: manual therapy and exercises/
patient counseling (N5114), shortwaves combined with exercises/counseling (N5121), and exercises/counseling
(N5115). No differences were found between the latter
two groups after 6 months. In other words, the combination
of shortwave diathermy with exercise/counseling did not
improve outcome. As far as we know, no study about the
use of microwaves in neck pain has been published.
Ideally, the design of this study should have only included
a comparison between microwave diathermy and placebo.
However, this posed ethical problems. Physical exercise therapy is usually studied in combination with other physical
treatments [21,41–44], so we provided a standardized
1719
treatment, including therapies based on solid scientific evidence (physical exercise) [35,45–47], therapies of questionable effectiveness (TENS) [35,46], and the therapy under
study—namely, microwave diathermy. However, because
of this design, it is possible that exercise and TENS could
have masked any positive effects of microwave diathermy.
This could be clarified by additional research in a trial in
which microwave diathermy is studied as the only treatment.
With regard to adherence to exercises, although some
studies have reported information about this item [48–50],
a recent systematic review [51] noted that few high-quality
trials have been conducted on this topic. Furthermore, there
is no standardized method for measuring adherence to treatment in the long term. In the study by Kolt and McEvoy
[50], conducted in patients with low back pain, the possibility of receiving some compensation was a relevant factor in
terms of adherence. Because one of the eligibility criteria in
our study was not being on sick leave or involved in a lawsuit, this possible bias is scarcely represented.
A frequent limitation of trials conducted with patients
with musculoskeletal pain is the fact that professionals
and patients are not blinded, and they do not use standardized outcome measures to assess pain, disability, and quality of life. Such limitations are common among research
studies within the fields of physiotherapy and physical
medicine and rehabilitation, and have received criticism
by a number of authors [52]. In his systematic review of
the use of electrotherapy in the treatment of neck pain, Kroeling et al. [5] made some recommendations for future
studies: larger sample sizes, more accurate standardizations, and a thorough description of the treatment are
required. In addition, Kay et al. [45] indicated that conducting a comparative study on the relative benefits of physical
exercise compared with those of other physical therapies—
frequently provided in combination with physical
exercise—is still difficult. The reason is that patients and
evaluators should be blinded, and adherence to treatment
and recourse to therapeutic co-interventions should be controlled. Accordingly, future research—both on neck pain
and other musculoskeletal disorders—based on more accurate methodologies is required [53]. Considering the design
and features of the current study, we believe our study
sheds light on certain aspects that have not yet been evidenced, and that it solves some of the methodological limitations found in previous studies.
Considering that treatment arms did not influence the results after the intervention and at 6 months, we did not
assess outcomes at time points longer than 6 months.
Nevertheless, this could be a limitation in the study design
because of the chronic nature of this painful condition.
Conclusions
Our study suggests that microwave diathermy provides
no additional benefit to a treatment regimen of chronic neck
1720
J.A. Andrade Ortega et al. / The Spine Journal 14 (2014) 1712–1721
pain that already involves other treatment approaches (eg,
exercise, TENS), in terms of pain, disability, patient satisfaction, perceived outcome, quality of life, adherence to exercise, and use of therapeutic co-interventions. Additional
research is needed to determine the relative efficacy of diathermy when used as an independent modality.
References
[1] Hogg-Johnson S, van der Velde G, Carroll LJ, et al. The burden and
determinants of neck pain in the general population: results of the
bone and joint decade 2000–2010 task force on neck pain and its
associated disorders. Spine 2008;33(4 Suppl):S39–51.
[2] C^
ote P, Cassidy D, Corroll L. The Saskatchewan Health and Back Pain
Survey: the prevalence of neck pain and related disability in Saskatchewan adults. Spine 1998;23:1689–98.
[3] Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of
neck pain. Best Pract Res Clin Rheumatol 2010;24:783–92.
[4] Korthals-de Bos IB, Hoving JL, van Tulder MW, et al. Cost effectiveness of physiotherapy, manual therapy, and general practitioner
care for neck pain: economic evaluation alongside a randomised
controlled trial. BMJ 2003;326:911.
[5] Kroeling P, Gross A, Goldsmith CH, Houghton PE, Cervical Overview Group. Electrotherapy for neck pain. Cochrane Database Syst
Rev 2009;CD004251.
[6] Borghouts JA, Koes BW, Vondeling H, Bouter LM. Cost-of-illness
of neck pain in the Netherlands in 1996. Pain 1999;80:629–36.
[7] David J, Modi S, Aluko AA, et al. Chronic neck pain: a comparison
of acupuncture treatment and physiotherapy. Br J Rheumatol
1998;37:1118–22.
[8] Gross AR, Goldsmith C, Hoving JL, et al, Cervical Overview
Group. Conservative management of mechanical neck disorders: a
systematic review. J Rheumatol 2007;34:1083–102.
[9] Watson T. The role of electrotherapy in contemporary physiotherapy
practice. Man Ther 2000;5:132–41.
[10] Boissonnault WG, Badke MB. Influence of acuity on physical therapy outcomes for patients with cervical disorders. Arch Phys Med
Rehabil 2008;89:81–6.
[11] Jette DU, Jette AM. Physical therapy and health outcomes in patients with spinal impairments. Phys Ther 1996;76:930–41.
[12] Goode AP, Freburger J, Carey T. Prevalence, practice patterns and evidence for chronic neck pain. Arthritis Care Res 2010;62:1594–601.
[13] Serrano-Aguilar P, Kovacs F, Cabrera-Hernandez JM, et al. Avoidable
costs of physical treatments for chronic back, neck and shoulder pain
within the Spanish National Health Service: a cross-sectional study.
BMC Musculoskelet Disord 2011;12:287.
[14] Cameron MH. Physical agents in rehabilitation: from research to
practice. 3rd ed. St. Louis, MO: Saunders Elsevier, 2008.
[15] Basford JR. Therapeutic physical agents. In: Delisa JA, Gans BM,
Walsh NE, et al, eds. Medicine & rehabilitation: principles and practice. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2005:
250–70.
[16] Weber DC, Hoppe KM. Physical agent modalities. In: Braddom RL,
ed. Physical medicine & rehabilitation. 3rd ed. Philadelphia, PA: Saunders, 2006:459–77.
[17] Giombini A, Di Cesare A, Di Cesare M, et al. Localized hyperthermia induced by microwave diathermy in osteoarthritis of the knee: a
randomized placebo-controlled double-blind clinical trial. Knee
Surg Sports Traumatol Arthrosc 2011;19:980–7.
[18] Di Cesare A, Giombini A, Dragoni S, et al. Calcific tendinopathy of
the rotator cuff: conservative management with 434 MHz local microwave diathermy (hyperthermia): a case study. Disabil Rehabil
2008;30:1578–83.
[19] Giombini A, Giovannini V, Di Cesare A, et al. Hyperthermia induced by microwave diathermy in the management of muscle and
tendon injuries. Br Med Bull 2007;83:379–96.
[20] Frasca G, Maggi L, Padua L, et al. Short-term effects of local microwave hyperthermia on pain and function in patients with mild to
moderate carpal tunnel syndrome: a double blind randomized
sham-controlled trial. Clin Rehabil 2011;25:1109–18.
[21] Dziedzic K, Hill J, Lewis M, et al. The effectiveness of manual
therapy or pulsed shortwave diathermy in addition to advice
and exercise for neck disorders: a pragmatic randomised controlled trial in physiotherapy clinics. Arthritis Rheum 2005;53:
214–22.
[22] Lewis M, James M, Stokes E, et al. An economic evaluation of three
physiotherapy treatments for non-specific neck disorders alongside
a randomized trial. Rheumatology 2007;46:1701–8.
[23] Carroll LJ, Hurwitz EL, C^ote P, et al. Research priorities and methodological implications: the bone and joint decade 2000–2010 task
force on neck pain and its associated disorders. J Manipulative
Physiol Ther 2009;32:S244–51.
[24] Dusunceli Y, Ozturk C, Atamaz F, et al. Efficacy of neck stabilization exercises for neck pain: a randomized controlled study. J Rehabil Med 2009;41:626–31.
[25] Al Mandeel M, Watson T. The thermal and nonthermal effects of
high and low doses of pulsed short wave therapy (PSWT). Physiother Res Int 2010;15:199–211.
[26] Huskisson EC. Measurement of pain. Lancet 1974;2:1127–31.
[27] Andrade Ortega JA, Delgado Martınez AD, Almecija Ruiz R. Validation of a Spanish version of the Neck Disability Index. Med Clin
(Barc) 2008;130:85–9.
[28] Andrade Ortega JA, Delgado Martınez AD, Almecija Ruiz R. Validation of the Spanish version of the Neck Disability Index. Spine
2010;35:E114–8.
[29] Alonso J, Prieto L, Anto JM. The Spanish version of the SF-36
health survey (the SF-36 health questionnaire): an instrument
for measuring clinical results. Med Clin (Barc) 1995;104:
771–6.
[30] Garvey TA, Transfeldt EE, Malcolm JR, Kos P. Outcome of anterior
cervical discectomy and fusion as perceived by patients treated for
dominant axial–mechanical cervical spine pain. Spine 2002;27:
1887–94.
[31] Hessler C, Boysen K, Regelsberger J, et al. Patient satisfaction after
anterior cervical discectomy and fusion is primarily driven by relieving pain. Clin J Pain 2012;28:398–403.
[32] Kovacs FM, Abraira V, Royuela A, et al. Minimum detectable and
minimal clinically important changes for pain in patients with nonspecific neck pain. BMC Musculoskelet Disord 2008;10:43.
[33] Young BA, Walker MJ, Strunce JB, et al. Responsiveness of the
Neck Disability Index in patients with mechanical neck disorders.
Spine J 2009;9:802–8.
[34] Escobar A, Quintana JM, Bilbao A, et al. Responsiveness and clinically important differences for the WOMAC and SF-36 after total
knee replacement. Osteoarthritis Cartilage 2007;15:273–80.
[35] Chiu TT, Hui-Chan CW, Chein G. A randomized clinical trial of
TENS and exercise for patients with chronic neck pain. Clin Rehabil
2005;19:850–60.
[36] Rush PJ, Shore A. Physician perceptions of the value of physical
modalities in the treatment of musculoskeletal disease. Br J Rheumatol 1994;33:566–8.
[37] Foster N, Thompson KA, Baxter GD, Allen JM. Management of
nonspecific low back pain by physiotherapists in Britain and Ireland: a descriptive questionnaire of current clinical practice. Spine
1999;24:1332.
[38] Li LC, Bombardier C. Physical therapy management of low back
pain: an exploratory survey of therapist approaches. Phys Ther
2001;81:1018–28.
[39] Hamm L, Mikkelsen B, Kuhr J, et al. Danish physiotherapists’ management of low back pain. Adv Physiother 2003;5:109–13.
J.A. Andrade Ortega et al. / The Spine Journal 14 (2014) 1712–1721
[40] Airaksinen O, Brox JI, Cedraschi C, et al. European guidelines for
the management of chronic nonspecific low back pain: COST B13
Working Group on Guidelines for Chronic Low Back Pain. Eur
Spine J 2006;15:S192–300.
[41] Koes BW, Bouter LM, van Mameren H, et al. Randomised clinical
trial of manipulative therapy and physiotherapy for persistent back
and neck complaints: results of one year follow up. BMJ 1992;304:
601–5.
[42] Koes BW, Bouter LM, van Mameren H, et al. The effectiveness of
manual therapy, physiotherapy, and treatment by the general practitioner for nonspecific back and neck complaints: a randomized clinical trial. Spine 1992;17:28–35.
[43] Hurwitz EL, Morgenstern H, Harber P, et al. The effectiveness of
physical modalities among patients with low back pain randomized
to chiropractic care: findings from the UCLA Low Back Pain Study.
J Manipulative Physiol Ther 2002;25:10–20.
[44] Borman P, Keskin D, Ekici B, Bodur H. The efficacy of intermittent
cervical traction in patients with chronic neck pain. Clin Rheumatol
2008;27:1249–53.
[45] Kay TM, Gross A, Goldsmith C, et al, Cervical Overview Group.
Exercises for mechanical neck disorders. Cochrane Database Syst
Rev 2005;CD004250.
[46] Chiu TT, Lam TH, Hedley AJ. A randomized controlled trial on the
efficacy of exercise for patients with chronic neck pain. Spine
2005;30:E1–7.
1721
[47] Hurwitz EL, Carragee EJ, van der Velde G, et al. Bone and joint
decade 2000–2010 task force on neck pain and its associated disorders treatment of neck pain: noninvasive interventions: results of the
bone and joint decade 2000–2010 task force on neck pain and its
associated disorders. Spine 2008;33(4 Suppl):S123–52.
[48] Bergman P, Grjibovski AM, Hagstr€omer M, et al. Adherence to
physical activity recommendations and the influence of sociodemographic correlates: a population-based cross-sectional study.
BMC Public Health 2008;8:367.
[49] Jack K, McLean SM, Moffett JK, Gariner E. Barriers to treatment
adherence in physiotherapy outpatient clinics: a systematic review.
Man Ther 2010;15:220–8.
[50] Kolt GS, McEvoy JF. Adherence to rehabilitation in patients with
low back pain. Man Ther 2003;8:110–6.
[51] Jordan JL, Holden MA, Mason EE, Foster NE. Interventions
to improve adherence to exercise for chronic musculoskeletal
pain in adults. Cochrane Database Syst Rev 2010;20:
CD005956.
[52] Fregni F, Imamura M, Chien HF, et al. Challenges and recommendations for placebo controls in randomized trials in physical and rehabilitation medicine: a report of the International Placebo
Symposium Working Group. Am J Phys Med Rehabil 2010;89:
160–72; discussion 1045–6; reply 1046–7.
[53] Roques CF. Analgesic physical therapy: present clinical data. Ann
Readapt Med Phys 2003;46:565–77.