®
Results may vary. Not all patients receive the same results.
This device should be used only by physicians trained in percutaneous, intravascular techniques and procedures at
medical facilities with the appropriate fluoroscopy equipment. The Pipeline® Embolization Device should be used by
physicians who have received the appropriate training for this device.
Indications for Use:
The Pipeline® Embolization Device is indicated for the endovascular treatment of adults (22 years of age and older)
with large or giant wide-necked intracranial aneurysms in the internal carotid artery from the petrous to the superior
hypophyseal segments. CAUTION: Federal (USA) law restricts this device to sale, distribution and use by or on the
order of a physician. CONTRAINDICATIONS: The use of the Pipeline® Embolization Device is contraindicated for
patients with any of the following conditions: 1) Patients with an active bacterial infection; 2) Patients in whom dual
antiplatelet therapy (aspirin and clopidogrel) is contraindicated; 3) Patients who have not received dual antiplatelet
agents prior to the procedure; or 4) Patients in whom a pre-existing stent is in place in the parent artery at the target
aneurysm location. WARNINGS: 1) While advancing the Pipeline® Embolization Device inside the microcatheter,
do not pull back or torque the wire. This may make device release more difficult or impossible; 2) Do not rotate the
delivery wire for more than 10 full turns. Over-rotation may cause delivery wire breakage. If the Pipeline® Embolization
Device does not open after 10 turns, remove the entire system (microcatheter and Pipeline® Embolization Device
delivery system) simultaneously; 3) If the capture coil tip of the delivery system becomes stuck in the mesh of a
delivered Pipeline® Embolization Device, rotate the wire clockwise while advancing the wire to try to release it, then
slowly pull back on the delivery wire; 4) Persons with known allergy to platinum or cobalt/chromium alloy (including
the major elements Platinum, Cobalt, Chromium, Nickel or Molybdenum) may suffer an allergic reaction to the
Pipeline® Embolization Device.
Plavix is a trademark of Sanofi.
Introducing a New Treatment
Method for Brain Aneurysms
NEUROVASCULAR | PERIPHERAL VASCULAR
Access · Balloons · Embolic Coils · Embolic Protection · Flow Diversion · Flow Restoration · Liquid Embolics ·
Plaque Excision · Procedural Support · Remodeling Devices · Retrieval Devices · Stents
ev3 Corporate
World Headquarters
Peripheral Vascular
3033 Campus Drive
Plymouth, MN 55441
USA
PH +1 763 398 7000
FX +1 763 398 7001
Cust Srvc +1 800 716 6700
ev3 Neurovascular
9775 Toledo Way
3033 Campus Drive
Irvine, CA 92618
USA
PH +1 949 837 3700
FX +1 949 837 2044
ev3 Europe
International Headquarters
106-108 rue La Boétie
75008 Paris
France
PH +33 156 88 59 10
FX +33 156 88 59 11
Pipeline® Embolization Device
www.ev3.net
©2011 ev3. All rights reserved.
76077-001 (A) MAY/11
www.ev3.net
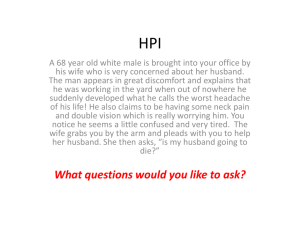
Understanding Aneurysms
Understanding Aneurysms
SA CCU L A R
What is a
brain aneurysm?
—
An aneurysm is an outpouching in an artery
caused by weakness in the vessel wall.
—
As the aneurysm grows, it may cause neurologic
symptoms such as headaches, vision loss, etc.
—
Untreated cerebral aneurysms may rupture,
resulting in hemorrhagic stroke.
—
What are the
different types
of aneurysms?
—
F U SI F OR M
Aneurysms can be classified by size:
•
•
•
Small aneurysms are less than 10 mm in diameter
Large aneurysms are 10-25 mm in diameter
Giant aneurysms are greater than 25 mm in diameter
< 10 mm
10 - 25 mm
Hemorrhagic stroke has potentially devastating
consequences including:
•
•
•
W I DE -NE CKE D
> 25 mm
Severe functional disability
Cognitive loss
Death
CEREBRAL
ANEURYSM
—
Aneurysms can also be classified by shape:
Fus i f orm
BLOOD
VESSELS
(ARTERIES)
S a cc ul a r
W i de- Nec k ed
What are traditional
treatment methods
for aneurysms?
The Pipeline® Embolization
Device is a new treatment
option for large or giant
aneurysms with wide necks.
T R A D I T I O N A L T R E AT M E N T M E T H O D S I N C L U D E :
—
Treatment Options
Surgical Clipping:
•
•
—
Permanently removing or destroying
the artery from which the aneurysm originates.
S u rg i ca l
Clipping
Surgical procedure requiring
an opening of the skull.
The Pipeline Device received FDA
approval in April of 2011 after completing
a clinical trial called PUFs (Pipeline for
Uncoilable or Failed Aneurysms)
Immediately post
treatment with the
Pipeline Device,
blood flow into the
aneurysms slows.
—
The Pipeline Device has been used to
treat patients in Europe since 2009
—
During the procedure, the Pipeline
Device (a braided cylindrical mesh
device) is implanted across the
aneurysm neck and allows for
healing of the diseased vessel
—
The Pipeline Device can be used by
itself to treat aneurysms
Placement of a clip on the neck of the
aneurysm to prevent blood flow into aneurysm.
Over time, blood
no longer enters
the aneurysm as the
body’s natural healing
process works with the
Pipeline Device. The
aneurysm shrinks.
Endovascular Embolization:
•
—
Minimally invasive approach through
a small incision in the leg.
•
Placement of embolic coils or
liquids into aneurysm to prevent
blood flow into aneurysm.
E m b o l i za ti o n wi th
Embolic Liquid
benefits*
- The Pipeline Device has been shown to be effective at treating large, giant
and wide-necked aneurysms in the internal carotid artery.
*As outlined in PUFs trial results.
E m b o l i z a t io n w it h
E m b o lic Co ils
—
Large, giant and wide-necked aneurysms can
be challenging to treat with traditional methods
•
Long-term care of these
aneurysms can be difficult.
risks**
**Discuss all risks with your doctor.
- The Pipeline Device is a relatively new technology compared to traditional
treatment methods.
- Medications like aspirin and Plavix are required before and after treatment
as instructed by your doctor.
TM
- Persons with known allergy to platinum or cobalt/chromium alloy (including
the major elements Platinum, Cobalt, Chromium, Nickel or Molybdenum)
may suffer an allergic reaction to the Pipeline® Embolization Device.
Treatment Options
—
Pipeline® Embolization Device is the first and
only flow diversion device approved by the FDA
Before treatment,
blood flows into
the aneurysm.
Parent Artery Deconstruction:
•
—
What can I expect
before, during and
after my procedure?
DURING THE PROCEDURE:
—
The procedure may be done under local or general anesthesia.
Because patients must remain still for long periods of time, general
anesthesia is usually preferred. Your doctor will determine the
best and safest method for treating your aneurysm.
—
The Pipeline procedure time includes accessing
the aneurysm location and placing the Pipeline
Device in the vessel. The entire procedure may
only take an hour, but 2-3 hours is not uncommon.
PRE-PROCEDURE EXAMS:
—
You will undergo a series of exams and diagnostic procedures
to fully assess the size, shape and location of your aneurysm.
Exams and procedures generally include the following:
•
•
•
Medical history review
Physical examination
Blood tests
•
•
•
Neurological examination
Imaging (CT, MRI)
Angiography
P R E - P R O C E D U R E M E D I C AT I O N S :
—
Your doctor may require you to prepare
for the procedure for a few days in advance.
Preparation may include taking aspirin and other
medications several days before the procedure.
Additional medications may be prescribed by your
doctor depending on your general health and other
medications you are taking.
—
After the procedure is complete, you will be moved to a recovery room.
—
You will likely experience some pain and tenderness in the groin area
where the micro catheter was inserted into your blood vessel.
—
You will be required to take medications (such as aspirin and Plavix )
after the procedure. Your doctor will provide you with specific instructions.
TM
•
It is very important for your safety to carefully follow
the directions and medications prescribed by your doctor.
—
You will be provided with an MRI
card that explains how the Pipeline
Device will behave under different
medical scans.
•
—
Please keep this card
with you at all times.
Please contact your doctor
for more information.
About the Procedure
About the Procedure
•
AFTER THE PROCEDURE: