HPI
advertisement
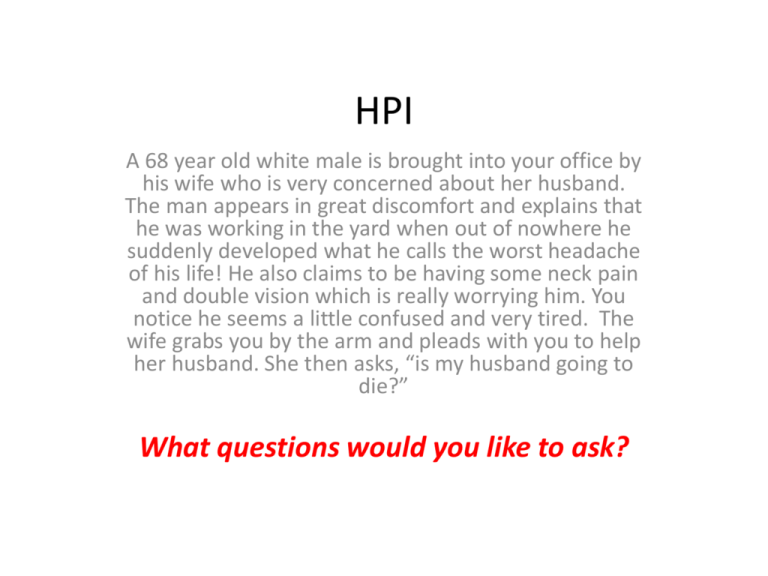
HPI A 68 year old white male is brought into your office by his wife who is very concerned about her husband. The man appears in great discomfort and explains that he was working in the yard when out of nowhere he suddenly developed what he calls the worst headache of his life! He also claims to be having some neck pain and double vision which is really worrying him. You notice he seems a little confused and very tired. The wife grabs you by the arm and pleads with you to help her husband. She then asks, “is my husband going to die?” What questions would you like to ask? HPI cont. • What makes it better? Nothing • What makes it worse? Nothing • PMHx: Hypertension, DM2, Hyperlipidemia. Not a person who usually experiences headaches, no history of heart attack, stroke or vascular symptoms • Has annual physicals with PCP. Wife says all of his problems are well controlled with medication, which her husband takes religiously. But neither can remember what medications he is taking • All: None • SxHx: None • FMHx: Father had HTN, HLD, died of MI at 73. Mother has history of migraine headaches, HTN and suffers from dementia. Currently lives in a assisted living facility on the outskirts of town. • Social Hx: Happily married with 4 children, retired blimp pilot. Drinks 2-3 PBR’s a days and has really cut back on smoking lately, only smokes 1 pk/day of marlboro reds. Has been smoking for 40yrs. Claims he does not using any illegal drugs What is included in your differential diagnosis? Differential Diagnosis • Headache – Migraine – Cluster – Tension • Trauma – Did he really fall and hit his head? – Did something fall on him and hit his head? • Infection – Stiff neck, vision issues. • Heat exhaustion/stroke/dehydration – What season is it? Is it hot out? How long was he outside? • Stroke • Tumor What is your next step to assess this patient? Physical Exam • Vitals: – BP 157/94 – T 37.2 – RR 24 • • • • • Gen: patient appears uncomfortable, holding head with both hands with eyes closed. CV: RRR, normal S1/S2, no murmurs, rubs or gallops appreciated. Resp: CTA Abd: Soft non tender, non distended belly with bowel sounds appreciated. Neuro: – – – – – Alert and oriented x3. Neck is tender to palpation with limited ROM Strength UE/LE bilaterally 5/5 All reflexes in tact Finger to nose, heel to shin slow but documented as normal. Rapid alternating hand movements very slow – Gait is normal, can walk on heels and toes without issue. – Anything else? Cranial Nerves • I: rarely tested, we will say normal • II: visual fields/acuity/fundoscopic exam all difficult to assess because patient claims his double vision is making it tough to see anything • III/IV/VI: EOM intact, PERRL, normal eye lid opening • V: facial sensation seems to be somewhat decreased on the left • VII: eye brow raise reduced on left, labored smile, but seems to easily frown. • VIII: WNL • IX/X: WNL • XI: difficult to assess as patient claims it hurts to touch his head and neck • XII: WNL Patient is getting more and more frustrated, what would you like to do next? Labs? • CBC: wnl • WBC: wnl • VDRL/RPR: negative Now what? Head CT Will recognize 90% of ruptured aneurysms Angiography performed to identify where exactly the aneurysm is located and plan treatment Subarachnoid Hemorrhage • Many describe as the “worst headache of my life” • Many have no previous symptoms • Risk factors include: HTN, atherosclerosis, renal disease, vasculitis, drug use (esp. cocaine) • the most frequent cause of clinically significant subarachnoid hemorrhage is rupture of berry (saccular) aneurysms • Other causes: traumatic hematoma, rupture of hypertensive intracerebral hemorrhage, vascular malformations, tumors, and Quick Review • Aneurysm- an abnormal widening or ballooning of a portion of an artery due to weakness in the wall of the blood vessel • Cause is not exactly clear. Some are present at birth, some thought to be due to vessel wall defects. • Major locations include: heart (aorta), brain, leg (popliteal artery), intestine (mesenteric artery), spleen (splenic artery) Berry/Saccular Aneurysm - Most common type of intracranial aneurysm. - Most often found in the anterior circulation near major arterial branch points within the COW - Found in 2% general population Pathogenesis • Again etiology is unknown; mostly sporadic • Despite this, genetic factors are thought to be involved as there is an increased incidence of aneurysms in first degree relatives of those affected. • Also an increased risk on those with certain disorders such as AD Polycystic Kidney Disorder, Ehlers-Danlos syndrome type IV, NF1, and Marfans Fibrin within wall Top left: Diagram of most vulnerable spots within the COW, where aneurysms often form. Top Right: The effect of weakening of the wall of a small intracerebral blood vessel, with the formation of a small aneurysm. This section has been stained for fibrin, which appears red. Note seepage of fibrin into the wall. Bottom: gross view of berry aneurysm Normal artery wall with slightly thickened intima, internal elastic lamina (arrows) and well organized smooth muscle in the media with a thin adventitia. Clinical Features • Rupture – Most common in fifth decade – More common in females – Can occur at any time, but often associated with increased ICP such as with sexual intercourse, straining, or lifting heavy objects • Blood forced into the subarachnoid space leading to excruciating HA, loss of consciousness, diplopia, sensory loss etc. • Blood covers the surface of the brain • 25-50% die with first rupture • Complications: Further Hemorrhage, Hydrocephalus ( blockage of arachnoid granulations), Permanent neurological defects. Treatment • Unruptured – Depends on following factors: Size and Location, patient age, overall state of health – Options include: observation with serial imaging along with tight BP control (CCB or BB’s), or neurosurgery consult to consider surgical clipping or coiling. • Ruptured – Re-bleed 20% of the time – Therefore need surgical clipping/coiling Board Questions • Most common site for Berry Aneurysm? Junction with ACA • What does the CSF show? Xanthochromia (yellowish tint due to broken down bilirubin) • Common complaint? Worst headache of my life • Most common complication? Vasospasm • What if suspect SAH, but CT inconclusive? Get LP to look for xanthochromia • http://pittsburghneurosciences.com/conditions/b rain_aneurysm/treatments.html • http://www.medicinenet.com/brain_aneurysm/p age2.htm • Goljan, Edward. Rapid Review Pathology, Elsevier 2009 Edition • http://www.nlm.nih.gov/medlineplus/ency/articl e/001414.htm • http://radiopaedia.org/articles/ruptured-berryaneurysm-1