Nipple discharge in male patients: Imaging findings.
advertisement

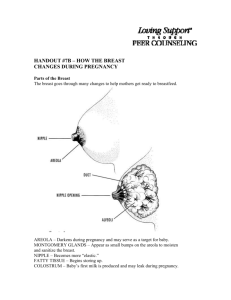
Nipple discharge in male patients: Imaging findings. Poster No.: C-0082 Congress: ECR 2012 Type: Scientific Exhibit Authors: R. Muñoz Carrasco, M. Alvarez Benito; CORDOBA/ES Keywords: Ultrasound, Mammography, Breast, Comparative studies, Neoplasia DOI: 10.1594/ecr2012/C-0082 Any information contained in this pdf file is automatically generated from digital material submitted to EPOS by third parties in the form of scientific presentations. References to any names, marks, products, or services of third parties or hypertext links to thirdparty sites or information are provided solely as a convenience to you and do not in any way constitute or imply ECR's endorsement, sponsorship or recommendation of the third party, information, product or service. ECR is not responsible for the content of these pages and does not make any representations regarding the content or accuracy of material in this file. As per copyright regulations, any unauthorised use of the material or parts thereof as well as commercial reproduction or multiple distribution by any traditional or electronically based reproduction/publication method ist strictly prohibited. You agree to defend, indemnify, and hold ECR harmless from and against any and all claims, damages, costs, and expenses, including attorneys' fees, arising from or related to your use of these pages. Please note: Links to movies, ppt slideshows and any other multimedia files are not available in the pdf version of presentations. www.myESR.org Page 1 of 14 Purpose Breast carcinoma in men is an uncommon disease. Male breast carcinoma represents less than 1% of all reported breast cancers and less than 1% of all cancers in men. The vast majority of male breast cancers are invasive ductal carcinoma (82%). Ductal carcinoma in situ represents 4.8% of all male breast cancers. Nipple discharge in male patients is rare. Nevertheless, male patients with nipple discharge have a higher incidence of carcinoma than female patients. Although most male breast carcinomas are clinically apparent and typically presents as a palpable mass, the first and unique clinical sign in a patient with ductal carcinoma in situ may be bloody nipple discharge. Nipple discharge in men can be related to benign breast conditions such as gynaecomastia, duct ectasia and papilloma. Physical breast examination is very sensitive for the detection of male breast cancer but lacks specificity. A hard painless mass in the subareolar region, eccentric to the nipple or a mass fixed to the skin, nipple or chest is a very sensitive indicator for male breast carcinoma. Accompanying signs include nipple discharge and axillary lymphadenopathy. Nipple discharge cytology is very specific for detection of malignant breast lesions but its sensitivity is low. Both mammography and breast ultrasound have showed a high diagnostic performance in male patients with breast symptoms. Due to its strong association with underlying malignancy, an increased awareness of the significance of nipple discharge in men may allow for earlier detection of breast carcinoma improving the prognosis. In the same way, unnecessary procedures must be avoided in benignant diseases. To our knowledge, there has been very little published experience with mammography and/or breast ultrasound of male patients with nipple discharge. The purpose of our study is to analyse the contribution of mammography and breast ultrasound in the evaluation of male patients with nipple discharge. Methods and Materials A retrospective study was undertaken in which male patients at our hospital with nipple discharge were examined with mammography and/or breast ultrasound between Page 2 of 14 September 1993 and December 2010. The hospital's breast mammography and breast ultrasound database was searched for male patients with a clinical history of nipple discharge. We included in this study the patients with an adequate clinical-radiological follow-up (minimum of 1 year) or with histopathological results. A standard database for further analysis was designed and included the following patient data: physical examination findings, mammographic and/or ultrasonography findings, cytohistological results, data from the clinical-radiological follow-up, stage and treatment in cases of carcinoma, and final diagnosis. On physical examination two categories were determined: positive or suspected malignancy (hard and eccentric to nipple mass or mass fixed to skin, nipple or chest wall) and negative or no suspected malignancy (soft, retroareolar and centred with respect to the nipple mass, diffuse breast enlargement without palpable mass and normal breast examination). Mammograms were performed on three units specialised in mammography: Mammo Diagnost UC (Philips Medical System, Best, The Netherlands), Senographe DMR (General Electric Medical System,Milwaukee,Wisconsin,USA) and Lorad Selenia (Hologic,Danbury,USA). Standard examinations were both mediolateral-oblique and craniocaudal views of each breast. All mammograms were read by two radiologists and discordant interpretations were solved with discussion. The mammographic findings were placed in one of the predetermined categories according to theAmericanCollegeof Radiology BI-RADS lexicon. Gynaecomastia and pseudogynaecomastia were placed in BI-RADS category 2. The mammographic criteria used to diagnose gynaecomastia, pseudogynaecomastia and normal male breast were those described by So et al. and Appelbaum et al. Gynaecomastia was diagnosed when mammography showed a subareolar density concentrically distributed around the nipple with three possible patterns (nodular, dendritic and diffuse). Pseudogynaecomastia appears as an enlarged breast with preponderance of radiolucent fat and the absence of dense retroareolar tissue. Normal male breast appears in mammography as radiolucent fat with a few strands like subareolar densities extending from the nipple. Intramammary lymph nodes can be found in normal male breast. Ultrasound was performed by using a 7.5 mHz transducer (Sonolayer SSA-250ª, Toshiba) and 7.5-10 mHz transducer (MyLab70, Esaote Biomedica). The ultrasound findings were classified into categories according to theAmericanCollegeof Radiology BI-RADS lexicon. Gynaecomastia and pseudogynaecomastia were placed in BIRADS category 2. The ultrasound criteria used to diagnose gynaecomastia, pseudogynaecomastia and normal male breast were those described by Stewart et al. and Sarteschi et al. There are two characteristic ultrasound patterns of gynaecomastia: discrete subareolar, triangular or nodular, hypoechoic area, centric to the nipple and overall increase in the volume and echogenicity of the breast parenchymal tissue. In pseudogynaecomastia, ultrasound shows hypoechoic adipose tissue accumulation Page 3 of 14 separated by echogenic septa. The normal mammary disk appears as a triangular, hypoechoic area which is centred with respect to the nipple and measures less than 8mm. Discharge was classified as bloody based on color only. We reviewed cytological findings from the smears from the nipple discharge. Findings were classified as positive, negative, inconclusive and inadequate. Histological confirmation was made by core needle biopsy or surgical biopsy. The clinical follow-up of the patients consisted of a chart review, telephone interview, or both. Radiological follow-up was performed with mammography and/or ultrasound. The final diagnosis was made based on histopathological results or, if no diagnostic tissue was obtained, a clinical follow-up was required for at least 1 year to confirm the benign radiological diagnosis. Using standard formulae, the sensitivity, specificity, positive predictive value and negative predictive value of physical breast examination, mammography and ultrasound for the detection of malignant disease were calculated. We considered as positive the mammograms or ultrasounds classified as BI-RADS categories 3, 4 and 5, and as negative those classified as BI-RADS categories 1 and 2. Results Between September 1993 and December 2010, a total of 1143 male patients underwent mammography and/or breast ultrasound in our Department of Radiology. Twenty four (2.1%) among these patients presented with a complaint of nipple discharge and they are the basis of this study. Twenty mammograms and 17 breast ultrasounds were performed in these patients. Male patients aged between 13 and 83 years (mean age: 49 years; SD:±22.03). The final diagnoses were: 4 (16.7%) infiltrating carcinomas, 1 (4.2%) ductal carcinoma in situ, 10 (41.7%) gynaecomastias, 2 (8.3%) pseudogynaecomastias and 7 (29.2%) normal. Nipple discharge in men was associated to carcinoma in 20.8%. All 20 mammograms and 17 ultrasound examinations were reviewed. Mammograms and ultrasound examinations performed on all the patients with infiltrating carcinoma showed a mass classified as BI-RADS categories 4 and 5 (Fig.1). All these patients also noted a breast mass. In all these patients the physical breast examination was positive or suspected malignancy. Ultrasound was more sensitive than mammography for identifying axillary lymphadenopathy in these patients (0/4 vs 1/4). Page 4 of 14 Mammography showed calcifications (classified as BI-RADS category 4) in the patient with carcinoma in situ. These calcifications were not visible on ultrasound and the only conspicuous clinical sign in this patient was bloody nipple discharge. In this patient the physical breast examination did not suspect malignancy. Radiological findings of all the patients without malignancy were classified as BI-RADS categories 1 and 2 (Figs 2 and 3). In three of these patients the physical breast examination was suspected malignancy. The diagnostic performance of physical breast examination, mammography and ultrasound for detection of malignant breast lesions is show in Table 1. Cytologic evaluation of the nipple discharge was performed in five patients: two cases were considered inadequate, one case inconclusive and two cases negative for malignancy (true negative results). The nipple discharge cytology of one of our patients with a bloody discharge without a breast mass with suspected malignancy was inconclusive. A ductal carcinoma in situ was histopathologically diagnosed. One core-needle biopsy guided by ultrasound was performed. The result of the coreneedle biopsy was positive for malignancy (true positive result). The results of the different diagnostic methods of the male patients included in our study are show in Table 2. Six of the 24 patients underwent excisional biopsy after mammography or breast ultrasound. The histopathological results were: 1 gynaecomastia (16.7%) and 5 carcinomas (83.3%). Eighteen of the 24 patients were followed up clinically. At the time this article was written, the patients had been followed up for 14-193 months after mammography and/or breast ultrasound (mean, 55.3 months). Two patients underwent radiological follow-up (with mammography in one patient and with ultrasound in the other one). In all the patients the clinical and/or radiological follow-up did not demonstrate changes. The stage at presentation in cases of carcinoma was as follows: stage 0: 1 patient; stage IA: 1 patient; stage IIB: 1 patient; stage IIIA: 1 patient. One patient was not staged at the moment of the presentation. In all patients with carcinoma surgery was performed (modified radical mastectomy in three, simple mastectomy in one and local excision in the other one). Table 1. Diagnostic accuracy of physical breast examination, mammography and ultrasound for detection of malignant breast lesions in male patients with nipple discharge. Page 5 of 14 Sensitivity Specificity PPV NPV Physical breast 80% examination 62.5% 57.1% 83.3% Mammography 100% 100% 100% 100% Ultrasound 80% 100% 100% 92.3% Table 2. Results of the different diagnostic methods in male patients with nipple discharge Patient Age Physical Mammography UltrasoundCytology Corebreast of nipple needle examination discharge biopsy Diagnosis 1 67 Negative Category Category Inconclusive 4 2 Ductal carcinoma in situ 2 80 Positive Category Category 4 4 - Infiltrating carcinoma 3 78 Positive Category Category 4 4 - Infiltrating carcinoma 4 59 Positive Category Category 4 4 - Infiltrating carcinoma 5 44 Positive Category 2 - - Gynaecomastia 6 13 Negative Category Category 2 2 - Gynaecomastia 7 15 Negative - - Gynaecomastia 8 46 - 9 54 Category Category 2 2 Pseudogynaecomastia 10 69 Category Category 2 2 Pseudogynaecomastia 11 62 Category Category 2 2 Gynaecomastia 12 83 Category Category Negative 1 1 Normal Positive Category 1 Category 2 - Normal Page 6 of 14 13 47 14 41 Positive 15 28 Negative . Category 2 Gynaecomastia 16 38 Negative Category Category 2 2 Gynaecomastia 17 47 Category Category 1 1 Normal 18 25 . Category 1 Normal 19 19 . Category 1 Normal 20 38 Category . 1 21 78 22 16 23 69 Negative Category . 2 24 61 Category . 2 Positive Category . 1 Inadecuate Normal Category . 2 Inadecuate Gynaecomastia Normal Category Category 5 5 Positive Category Category 2 2 Infiltrating carcinoma Gynaecomastia Gynaecomastia Negative Gynaecomastia Images for this section: Page 7 of 14 Fig. 1: Mediolateral oblique (A) and craniocaudal (B) mammograms of the right breast show a irregular mass, eccentrically located relative to the nipple. The nipple is retracted and the overlying skin is thickened. The lesion was classified as BI-RADS category 5. An infiltrating ductal carcinoma was probed. Page 8 of 14 Fig. 2: Nodular gynaecomastia. Mediolateral oblique (A) and craniocaudal (B) mammograms of the right breast show a subareolar density concentrically distributed around the nipple (nodular pattern). Transverse ultrasound images (C) show a discrete subareolar, nodular hypoechoic area, centric to the nipple. Page 9 of 14 Page 10 of 14 Fig. 3: Bilateral gynaecomastia (dendritic pattern). Mammograms of a male breast show a glandular opacity radiating from behind the nipple into the fatty tissue. Page 11 of 14 Conclusion Breast carcinoma must always be excluded in male patient with nipple discharge. An increased awareness of this clinical sign may allow for earlier detection of breast cancer. Mammography and breast ultrasound are useful in the evaluation of male patients with nipple discharge diagnosing carcinoma in initial stages and avoiding unnecessary biopsies given its high negative predictive values. References • Al-Saleh N. Bilateral ductal carcinoma in situ (DCIS) in a male breast. Gulf J Oncolog. 2011;1:68-72. • American College of Radiology. Breast imaging reporting and data system th atlas (BIRADS Atlas). 4 ed. Reston, VA: American College of Radiology, 2003. • Appelbaum AH, Evans GFF, Levy KR, Amirkhan RH, Schumpert TD. Mammographic appearances of male breast disease. Radiographics. 1999;19:559-68. • Braunstein GD. Clinical practice: gynecomastia. N Engl J Med. 2007;357:1229-37. • Chen L, Chantra PK, Larsen LH, Barton P, Rohitopakarn M, Zhu EQ, et al. Imaging characteristics of malignant lesions of the male breast. Radiographics. 2006;26:993-1006. • Crichlow RW, Galt SW. Male breast cancer. Surg Clin N Am. 1990;70:1165-77. • Cutuli B, Dilhuydy JM, De Lafontan B, Berlie J, Lacroze M, Lesaunier F, et al. Ductal carcinoma in situ of the male breast. Analysis of 31 cases. Eur J Cancer. 1997;33:35-8. • Desai DC, Brennan EJ, Carp NZ. Paget's disease of the male breast. Am Surg. 1996;62:1068-72. • Detraux P, Benmussa M, Tristant H, Garel L. Breast disease in the male: galactographic evaluation. Radiology. 1985;154:605-6. • Donegan WL, Redlich PN. Breast cancer in men. Surg Clin North Am. 1996;76:343-63. • Doyle S, Steel J, Porter G. Imaging male breast cancer. Clin Radiol. 2011;66:1079-85. • Fentiman IS, Fourquet A, Hortobagyi GN. Male breast cancer. Lancet. 2006;367:595-604. [Erratum in: Lancet. 2006;367:1818]. Page 12 of 14 • Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN. Breast carcinoma in men. Cancer. 2004;101:51-7. • Goss PE, Reid C, Pintilie M, Lim R, Miller N. Male breast carcinoma. A review of 229 patients who presented to the Princess Margaret Hospital during 40 years: 1955-1996. Cancer. 1999;85:629-39. • Iuanow E, Kettler M, Slanetz PJ. Spectrum of disease in the male breast. AJR. 2011;196:W247-59. • Kapila K, Verma K. Cytology of nipple discharge in florid gynecomastia. Acta Cytol. 2003;47:36-40. • López-Ríos F, Vargas-Castrillón J, González-Palacios F, de Agustín PP. Breast carcinoma in situ in a male. Report of a case diagnosed by nipple discharge cytology. Acta Cytol. 1998;42:742-4. • Morrogh M, King TA. The significance of nipple discharge of the male breast. Breast J. 2009;15:632-8. • Muñoz Carrasco R, Álvarez Benito M, Muñoz Gomariz E, Raya Povedano JL, Martínez Paredes M. Mammography and ultrasound in the evaluation of male breast disease. Eur Radiol. 2010;20:2797-805. • Planas J, Rabanal E, Rosell R, Salvia J, García R. Patología mamaria en el varón. Radiología. 1992;34:159-75. • Ribeiro G. Male breast cancer. A review of 301 cases from the Christie Hospital and Holt Radium Institute, Manchester. Br J Cancer. 1985;51:115-9. • Sandler B, Carman C, Perry RR. Cancer of the male breast. Am Surg. 1994;60:816-20. • Sarteschi M, Turchi P, Paoli R, Sabo C, Massei A, Massei P, Menchini Fabris GF. Echography aspects of gynecomastia. Arch Ital Urol Androl. 1993;65:331-5. • Simmons RM. Male ductal carcinoma in situ presenting as bloody nipple discharge: a case report and literature review. Breast J. 2002;8:112-4. • So GJ, Chantra PK, Wollman JS, Bassett LW. The male breast. In: Bassett LW, Jackson VP, Jahan R, Fu YS, Gold RH, editors. Diagnosis of diseases of the breast. Philadelphia: WSaunders Company; 1997. p. 501-18. • Stewart RAL, Howlett DC, Hearn FJ. Pictorial Review: the imaging features of male breast disease. Clin Radiol. 1997;52:739-44. • Stierer M, Rosen H, Weitensfelder W, Hausmaninger H. Teleky B, Jakesz R, et al. Male breast cancer: Austrian experience. World J Surg. 1995;19:687-93. Page 13 of 14 • Treves N, Robbins CF, Amorosos WL. Serous and serosanguinous discharge from the male nipple. Arch Surg. 1956;73:319-29. • Weshler Z, Sulkes A. Contrast mammography and the diagnosis of male breast cysts. Clin Radiol. 1980;31:341-3. • Yamamoto H, Okada Y, Taniguchi H, Handa R, Naoi Y, Oshima S, et al. Intracystic papilloma in the breast of a male given long-term phenothiazine therapy: a case report. Breast Cancer. 2006;13:84-8. Personal Information Page 14 of 14