Ch. 10 – Muscle Tissue and Muscle Physiology Skeletal muscles
advertisement
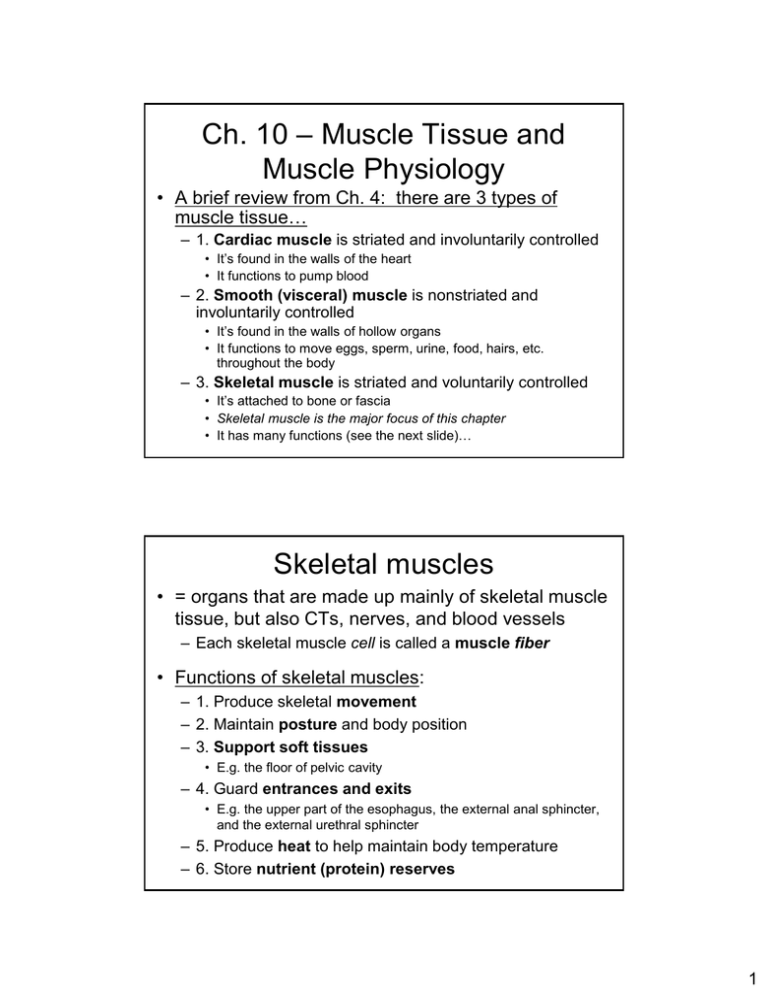
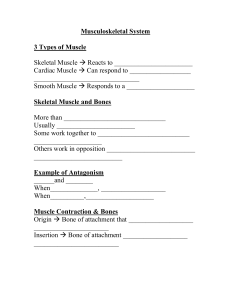
Ch. 10 – Muscle Tissue and Muscle Physiology • A brief review from Ch. 4: there are 3 types of muscle tissue… – 1. Cardiac muscle is striated and involuntarily controlled • It’s found in the walls of the heart • It functions to pump blood – 2. Smooth (visceral) muscle is nonstriated and involuntarily controlled • It’s found in the walls of hollow organs • It functions to move eggs, sperm, urine, food, hairs, etc. throughout the body – 3. Skeletal muscle is striated and voluntarily controlled • It’s attached to bone or fascia • Skeletal muscle is the major focus of this chapter • It has many functions (see the next slide)… Skeletal muscles • = organs that are made up mainly of skeletal muscle tissue, but also CTs, nerves, and blood vessels – Each skeletal muscle cell is called a muscle fiber • Functions of skeletal muscles: – 1. Produce skeletal movement – 2. Maintain posture and body position – 3. Support soft tissues • E.g. the floor of pelvic cavity – 4. Guard entrances and exits • E.g. the upper part of the esophagus, the external anal sphincter, and the external urethral sphincter – 5. Produce heat to help maintain body temperature – 6. Store nutrient (protein) reserves 1 Organization of CTs in skeletal muscles Part 1 • Skeletal muscles (as a whole): – Are surrounded by epimysium, which is… • Dense irregular CT • Connected to deep fascia – Are subdivided into many compartments called fascicles Fig. 10-1, p. 281 • Fascicles: – Are surrounded by perimysium, which… Organization of CTs in skeletal muscles Part 2 • Is dense irregular CT • Also contains blood vessels and nerves – Contain many individual muscle fibers Fig. 10-1, p. 281 2 • Muscle fibers: – Are surrounded by endomysium, which… • Is areolar CT • Contains capillaries, nerve fibers (axons), and… – Myosatellite cells = stem cells that function in muscle development, repair, and perhaps growth (via hyperplasia) Organization of CTs in skeletal muscles Part 3 – Contain long, contractile protein-filled cylindrical structures called myofibrils Fig. 10-1, p. 281 A summary of the CTs in skeletal muscles • All 3 “–mysiums” fuse together at the end of the muscle to form a tendon, which… – Connects muscle to bone – Is continuous with the periosteum of bone – Is called an aponeurosis if it’s a broad, flat tendon Fig. 10-1, p. 281 3 More about skeletal muscle fibers • They are… – – – – A.k.a. muscle cells or myofibers Formed by the fusion of embryonic myoblast cells Extremely large – up to a foot long and 10X the diameter of a typical cell! Multinucleate and striated Fig. 10-2, p. 282 Skeletal muscle fiber structure • Sarcolemma = the cell membrane of a muscle fiber – “Sarco” = “flesh”; “lemma” = “husk” – Transverse (T) tubules = deep invaginations of the sarcolemma, which… • Are continuous with the sarcolemma • Carry action potentials (electrical impulses) deep into the muscle fiber • Sarcoplasm = the cytoplasm of a muscle fiber Fig. 10-3, p. 283 4 Skeletal muscle fiber structure • Sarcoplasmic reticulum (SR) = a membranous network of tubules that surrounds each myofibril – The SR is modified smooth ER – Function: store and release Ca2+ ions Fig. 10-3, p. 283 Calcium ions and muscle fibers • Ca2+ is continuously pumped (via active transport) into the SR from the sarcoplasm – The SR is not very permeable (leaky) to Ca2+ in a resting muscle fiber • SR contains a Ca2+-binding (the binding is reversible) protein called calsequestrin • As a result of the pumping of Ca2+ into the SR: – The free (unbound) [Ca2+] in the SR is ~ 1,000X higher than in the sarcoplasm – The total [Ca2+] = free Ca2+ + Ca2+ bound to calsequestrin – About 40X more Ca2+ is bound to calsequestrin than is in the form of free Ca2+ – So, the total [Ca2+] in SR can be up to 40,000X higher than in the sarcoplasm! • During the contraction process, the SR membrane becomes extremely permeable (leaky) to Ca2+, and Ca2+ rapidly diffuses into the sarcoplasm – Remember that flux = P x ΔC 5 Skeletal muscle fiber structure • Myofibrils = long, parallel, cylindrical structures that are surrounded and separated by SR – They contain contractile protein filaments called myofilaments: • Thin filaments are mostly made of the protein actin • Thick filaments are mostly made of the protein myosin • Sarcomeres = regular, repeating, functional sections/units of myofilaments within myofibrils (see the next slide) Fig. 10-3, p. 283 • Sarcomeres are the smallest functional units of muscle contraction Sarcomeres – They are repeating units along the entire length of the myofibril and thus the muscle fiber • Their regular arrangement causes skeletal muscle tissue to have a striated (banded) appearance microscopically Fig. 10-2, p. 282 Fig. 10-4, p. 285 6 • Sarcomere structure A band = dark colored – = the center of a sarcomere – It does not shrink when muscle contracts – It contains: • 1. The M line = proteins that centrally stabilize the thick filaments • 2. The H band (H zone) – where there are thick filaments only – The H band does shrink when muscle contracts • 3. Two zones of overlap – where both thin and thick filaments are present • I band = light in color – It shrinks when muscle contracts – It contains thin filaments, titin (an elastic protein), and the… • Z line = the boundary between adjacent sarcomeres – It’s made of actinin proteins that anchor the thin filaments of adjacent sarcomeres (see the next slide) – Titin attaches here, too Fig. 10-4, p. 285 Cross-sections of different parts of a sarcomere Fig. 10-5, p. 286 7 A closer look at the myofilaments Fig. 10-7, p. 288 Thin filaments • Contain 4 proteins: – 1. F-actin (filamentous actin) = a twisted strand composed of 2 rows of globular G-actin subunits; has active sites (= myosin-binding sites) – 2. Nebulin – helps hold the G-actin subunits together in the F-actin strand – 3. Tropomyosin – covers the active sites on G-actin in resting muscle – 4. Troponin – binds to G-actin and tropomyosin; it has a Ca2+-binding site Note: troponin and tropomyosin combine to form the troponintropomyosin complex Fig. 10-7ab, p. 288 8 Thick filaments • • • • = bundles of myosin molecules around a titin core The myosin molecules have an elongated tail, a globular head, and a hinge region The myosin heads have an ATP-binding site The myosin heads form crossbridges (connections/ interactions) with actin during contraction Fig. 10-7cd, p. 288 The sliding filament theory of skeletal muscle contraction • The sarcomere shortens as the thin and thick filaments slide past one another – The I bands and H band shrink; the A band does not • The zones of overlap increase in length! • Sarcomeres shorten → myofibrils shorten → muscle fibers shorten → the whole muscle shortens! Fig. 10-8, p. 288 9 the most macroscopic level the most microscopic level A summary of the levels of organization in a skeletal muscle Fig. 10-6, p. 287 An overview of skeletal muscle contraction Fig. 10-9, p. 289 10 The steps involved in muscle contraction • 1. An electrical signal or impulse (= an action potential, or AP) travels along the axon of a motor neuron to the neuromuscular junction (NMJ) – NMJ = the synaptic terminal of a motor neuron and the motor end plate of a muscle fiber, plus the synaptic cleft in between Note: my numbered steps differ slightly from Martini’s, so I’ve blanked out the step numbers on the figures in these notes Fig. 10-11, p. 292 The steps involved in muscle contraction • 2. In response to the incoming action potential, neurotransmitter (acetylcholine, or ACh) is released via exocytosis into the synaptic cleft Fig. 10-11, pp. 292-293 11 The steps involved in muscle contraction • 3. ACh diffuses across the synaptic cleft and binds to ACh receptors on the surface of the sarcolemma at the motor end plate • 4. The ACh receptors change shape and allow Na+ to move down its concentration gradient into the sarcoplasm Fig. 10-11, p. 293 The steps involved in muscle contraction • 5. Excitation (of the muscle fiber) = another AP is generated, and it spreads along the sarcolemma and deep into the T tubules – Meanwhile, the enzyme acetylcholinesterase (AChE) breaks down the ACh, returning the NMJ to its resting state Fig. 10-11, pp. 292-293 12 Conditions in a resting muscle fiber • The [Ca2+] in the sarcoplasm is relatively low • The free [Ca2+] in the sarcoplasmic reticulum (SR) is relatively high (~ 1,000X higher than in the sarcoplasm) • The myosin heads are already “cocked” and storing potential energy due to their prior breakdown of ATP (see the next slide) • The active (myosin-binding) sites on actin are blocked by the troponin-tropomyosin complex Fig. 10-10a, p. 291 The steps involved in muscle contraction • • 6. In response to the muscle fiber’s AP, the SR releases Ca 2+ into the sarcoplasm (this is excitation-contraction coupling!) 7. The Ca2+ binds to the troponin, which then changes position, pulling the tropomyosin to the side and uncovering the active (myosin-binding) sites on actin Fig. 10-10b, p. 291 Fig. 10-12, p. 294 13 The steps involved in muscle contraction • 8. The “cocked” (energized) myosin heads of the thick filaments bind to the actin of the thin filament, forming crossbridges Fig. 10-12, p. 295 Fig. 10-10c, p. 291 The steps involved in muscle contraction • 9. The myosin heads release their stored energy as they pivot (“uncock”), pulling the thin filament toward the center (M line) of the sarcomere – This is the “power stroke” of muscle contraction Fig. 10-12, p. 295 14 The steps involved in muscle contraction • 10. The myosin heads bind to new ATP, breaking the crossbridges Fig. 10-12, p. 295 The steps involved in muscle contraction • 11. The myosin heads break down the newly bound ATP, and “recock” to get ready for the next power stroke – Steps 8-11 are repeated (as long as the [Ca2+] and [ATP] are high enough), shortening the sarcomeres and thus the entire muscle, creating tension (which is a pulling force) – Cross-bridges are formed at different times by different individual myosin heads, causing an overall smooth sliding of the filaments Fig. 10-12, p. 295 15 Ending contraction (= relaxation) • The motor neuron quits firing (sending APs), so no additional ACh is released at the NMJ • AChE in the synaptic cleft continually breaks down previously released ACh • As a result: – No new APs are generated along the sarcolemma of the muscle fiber – The [Ca2+] in the sarcoplasm drops, because… • No new Ca2+ is released from the SR • Ca2+ is continuously pumped back into the SR – The troponin-tropomyosin complex returns to its resting/original position, covering up the active (myosin-binding) sites on the thin filaments – There is no interaction/cross-bridge formation between actin and myosin • The muscle returns (stretches) to its resting length passively (due to other external forces, such as elasticity, gravity, or the contraction of antagonist muscles) A review of skeletal muscle contraction Table 10-1, p. 297 16 → due to a combination of elastic forces, opposing (antagonistic) muscle contractions, and gravity A review of skeletal muscle relaxation Table 10-1, p. 297 Tension (force/strength) production • By individual muscle fibers vs. by whole muscles • By individual muscle fibers: • By whole muscles: • The all-or-none principle = all sarcomeres in an individual muscle fiber will contract together maximally when the fiber is stimulated; i.e., a muscle fiber is either “on” (producing tension) or “off” (relaxed) • Main factors: • Ultimately, the amount of tension produced by an individual muscle fiber depends on the number of pivoting cross-bridges formed • Main factors: – 1. Resting fiber length – affects the degree to which thin and thick filaments overlap – 2. Frequency of stimulation – affects the duration of high [Ca2+] – 3. The size (diameter) of the individual muscle fiber – affects the amount of actin and myosin available to interact with each other – 1. The amount of tension produced by individual muscle fibers (see the box to the left) – 2. Recruitment – affects the # of motor units (and thus fibers) that are stimulated – 3. The size of the whole muscle – which depends on the # of muscle fibers present (and the diameter of those fibers, as discussed in the box to the left) 17 • • The resting length of a muscle fiber affects the amount of overlap between the thin and thick filaments There is an optimal resting length for a fiber at which force generation is maximal Tension production by individual muscle fibers: resting fiber length Fig. 10-14, p. 298 Tension production by individual muscle fibers: frequency of stimulation • 1. Single stimulus: – Twitch • 2. Multiple stimuli: – Treppe – Wave summation (a.k.a. summation of twitches) – Incomplete tetanus – Complete tetanus 18 Single stimulus: twitch • A twitch = a single stimuluscontraction-relaxation sequence in a muscle fiber – Note: a single twitch is too brief to be part of any useful muscular activity by itself Fig. 10-15, p. 299 • A twitch has 3 parts: – 1. The latent period • The AP is followed by Ca2+ release from the SR – 2. The contraction phase • Tension increases to a peak – 3. The relaxation phase • Tension decreases • There’s no more stimulation, so Ca2+ is pumped back into the SR Multiple stimuli: treppe • Treppe = the gradual increase in tension (i.e., strength of contraction) that is generated by a muscle fiber when it is repeatedly stimulated immediately after each relaxation phase ends • A relatively low maximum tension is reached • The main explanation for treppe: – There is increasing [Ca2+] in the sarcoplasm • There’s not enough time in between stimuli to pump it all back into the SR Fig. 10-16a, p. 301 19 • Wave summation (a.k.a. summation of twitches) = the gradual increase in tension that is generated by a muscle fiber when it is repeatedly stimulated before each relaxation phase has been completed Multiple stimuli: wave summation – One twitch is added to another, so the contraction gets stronger and stronger • The stronger contractions are probably due to: – The prolonged presence of high [Ca2+] in the sarcoplasm – Action potential duration vs. twitch duration • An AP is short: 1-2 msec • A muscle twitch is longer: up to 100 msec • So another AP can stimulate a muscle fiber before the relaxation phase of the previous twitch has ended Fig. 10-1b6, p. 301 Multiple stimuli: wave summation leading to tetanus • • Incomplete tetanus = the muscle fiber never relaxes completely between twitches Complete tetanus = the stimulation rate is higher, so the relaxation phase is eliminated entirely – Almost all normal whole muscle contractions involve tetanic contractions by individual muscle fibers Fig. 10-16bc, p. 301 20 Tension production by whole muscles: recruitment • Motor unit = one motor neuron and all of the muscle fibers that it innervates – The size of a motor unit is inversely related to the precision of its control (e.g. eye muscles vs. leg muscles) • Recruitment = the stimulation of additional motor units – The more motor units stimulated → the more actively contracting muscle fibers → a stronger total contraction by the whole muscle Asynchronous motor unit summation Fig. 10-17, p. 302 Tension production by whole muscles: muscle tone • Muscle tone = the low level of resting tension that is present in skeletal muscle at all times (it is NOT enough tension to produce movement, however) – Some motor units are active at any given point in time – Which motor units are active varies constantly • Functions of muscle tone: – Stabilize bones and joints – Maintain body position (posture) – Allow more rapid activation of a whole muscle (i.e., accelerate recruitment) – ↑ Energy usage when muscles are at rest (i.e., ↑ resting metabolic rate) – Lookin’ good! 21 Types of contractions: isotonic • Isotonic contraction (isotonic = “same tension”) – The muscle length changes, so movement occurs (it’s a “dynamic contraction”) – There are 2 types of isotonic contractions: • 1. Concentric contraction (shown here) = the muscle shortens if the tension produced exceeds (even if just barely) the load • 2. Eccentric contraction = the muscle lengthens in a controlled manner (exerting tension in opposition to an external force such as gravity), if the tension produced is slightly less than the load Fig. 10-18a, p. 303 Types of contractions: isometric • Isometric contraction (isometric = “same length”) • No movement occurs (it’s a “static contraction”) – Tension is produced, but it isn’t strong enough to overcome the load and cause shortening/movement, so the length of the muscle remains the same – E.g. maintaining posture against gravity Fig. 10-18c, p. 303 22 Load and speed of contraction • Contraction speed (= distance ÷ time) is inversely related to load – I.e., ↑ load (lifting a heavy weight) → ↓ contraction speed (slower) • This should be intuitive and hopefully fairly obvious from everyday life experiences! Fig. 10-19, p. 304 Energy use and muscular activity • Muscle contraction requires lots of ATP energy: – There are 15 billion thick filaments per muscle fiber – When a muscle fiber is actively contracting, each thick filament breaks down 2,500 ATP molecules per second – 15 billion X 2,500 = 37.5 X 1012 = 37,500,000,000,000 ATPs are needed per muscle fiber per second! • There’s only enough ATP present in muscle fibers for about 2 seconds of maximal (tetanic) contraction • There are 3 main processes used to generate additional ATP in skeletal muscle for contraction: – 1. ATP and CP reserves – 2. Glycolysis – 3. Aerobic metabolism • Which process muscles use depends upon both the INTENSITY and DURATION of their activity 23 ATP and CP reserves • This process is only found in muscle cells • It involves creatine phosphate (CP) and ATP • It is a fast, SHORT-TERM method of ATP generation – It involves only 1 enzyme (creatine kinase); i.e., it’s not a long, time-consuming pathway • CP “recharges” spent ADP into fresh ATP – The reversible equation: CP + ADP ↔ creatine + ATP • The total amount of CP stored in a muscle is enough for a burst of MAXIMUM-intensity contraction for ABOUT 15 SECONDS – This allows time for other processes such as glycolysis to “kick in” Glycolysis • Glucose (either absorbed from your last meal or released from stored glycogen reserves) is broken down to form 2 pyruvate (pyruvic acid) molecules (see Ch. 25 for much more detail) • It does not require oxygen (i.e., it’s anaerobic) • It occurs in the cytoplasm of cells • It is relatively inefficient: a net of only 2 ATPs are generated from each glucose molecule • In anaerobic conditions, glycolysis is used after ATP/CP reserves are depleted during a burst of maximum-intensity contraction – The problem: in anaerobic conditions, glycolysis ends up with the pyruvate converted to lactate (lactic acid), leading to H+ buildup… • Muscle fiber intracellular pH ↓ • Enzyme function is negatively affected • So muscle fibers can only provide a burst of NEAR-MAXIMUM-intensity contraction for ABOUT 2 MINUTES before fatigue kicks in • Glycolysis also supplies 2 pyruvate molecules as organic substrates for the initial step of aerobic metabolism (see the next slide) 24 Aerobic metabolism • Pyruvate (from glycolysis) or other organic substrates are broken down in a multi-enzyme pathway (see Ch. 25 for much more detail) • It requires oxygen (i.e., it’s aerobic) – So it depends on the ability of the respiratory and cardiovascular systems to deliver enough oxygen to meet the demand for it • It occurs in the mitochondria of cells • It is very efficient: 17 ATPs are generated from each pyruvate (so 34 ATPs are generated from each glucose) • Resting skeletal muscle: – Uses small quantities of mostly free fatty acids (from the bloodstream) as substrates • Moderately active skeletal muscle: – Uses larger quantities of mostly pyruvate (from glycolysis) and free fatty acids (from the bloodstream) as substrates • It provides energy for LONG-TERM exercise (A FEW MINUTES TO A FEW HOURS) of SUBMAXIMAL-intensity muscular contractions – E.g. a marathon run is almost all aerobic • Resting = LOW intensity – There’s low ATP demand – There’s lots of O2 available • At rest, muscles use small quantities of mostly free fatty acids (from the bloodstream) as substrates for aerobic metabolism in mitochondria • This restocks supplies for maximum intensity activity that may be needed later: ATP generation in resting skeletal muscle – Surplus ATP → CP – Surplus glucose → glycogen Fig. 10-20a, p. 307 25 • Moderate = SUBMAXIMAL intensity – There’s increased demand for ATP – There’s increased demand for O2, but O2 delivery is still matching demand ATP generation in moderately active skeletal muscle • So aerobic metabolism is still dominant • Pyruvate (from glycogen/glucose) is the main substrate – But if you have low glycogen reserves, you can use fatty acids (or even amino acids) as substrates Fig. 10-20b, p. 307 • Peak = MAXIMUM or NEAR-MAXIMUM – O2 delivery cannot meet O2 demand • So aerobic/ mitochondrial ATP production can provide only about 1/3 of the ATP needed ATP generation in skeletal muscle that is in peak activity • Most ATP is produced from CP (for the first 10-15 seconds) and via anaerobic glycolysis (for a few minutes) – The downside: lactate (lactic acid) production and ↓ intracellular pH limits exercise duration Fig. 10-20c, p. 307 26 Fatigue • Muscle fatigue = skeletal muscle can no longer perform at the desired level of activity • Some factors that lead to muscle fatigue: – ↓ Energy reserves, so there’s ↓ substrate availability – ↓ pH effects: • a) Changes in enzyme activity (usually for the worse) • b) H+ displaces Ca2+ from troponin • c) H+ interferes with hemoglobin reoxygenation – Sarcolemma and SR damage, leading to slower Ca2+ uptake and release • Consider also “central (mental/motivational) fatigue”: – ↓ pH has harmful effects on neurons – Pain affects the brain (↑ weariness, ↓ desire) Recovery from skeletal muscle activity • Recovery = the return of conditions (pH, oxygen consumption, temperature, etc.) in muscle fibers and the entire body to normal, resting levels after exercise • Recovery mechanisms include: – Lactate removal and recycling • Within a recovering muscle fiber, local lactate is converted back to pyruvate, which can then be burned aerobically and/or used to synthesize glucose and replenish glycogen reserves • The Cori cycle – excess lactate that diffuses into the bloodstream is transported to the liver, where it’s converted back to pyruvate, which can then be burned aerobically and/or used to synthesize glucose, which is then transported back to muscle fibers to replenish their glycogen reserves – Oxygen debt • A.k.a. excess postexercise oxygen consumption (EPOC) • = the amount of O2 required to restore normal resting conditions – Heat loss • E.g. via dermal vasodilation and/or sweating 27 Muscle performance • Consider the tradeoffs of generating maximal force/strength vs. having longer endurance • Muscle performance is mainly dependent upon: – 1. Muscle fiber type • Slow fibers (“dark meat”) • Intermediate fibers • Fast fibers (“white meat”) – 2. Physical conditioning/training Fast vs. slow fibers Fig. 10-21, p. 310 28 A comparison of skeletal muscle fiber types Table 10-3, p. 309 Physical conditioning • Anaerobic endurance – maximum or nearmaximum effort, shorter duration (up to 2 minutes) – Improvements are due mainly to hypertrophy – It’s limited by: • ATP/CP availability • Glycogen/glucose availability • Tolerance for acidosis (due to lactate production) • Aerobic endurance – sustained sub-maximal effort, longer duration (from a few minutes to a few hours) – Improvements are due mainly to muscle fiber type alterations, ↑ cardiovascular and respiratory function, and ↑ capillary density – It’s limited by: • Oxygen delivery to mitochondria • The number of mitochondria • Aerobic substrate (glycogen/glucose, fatty acids, and/or amino acids) availability 29 FYI Cardiac muscle tissue • We will cover this topic with the rest of Ch. 20 Fig. 10-22, p. 313 Smooth muscle tissue • Is not striated (because there are no sarcomeres/myofibrils) • Has no T tubules, but it does have SR • Myosin – Is scattered within the sarcoplasm – Has more heads than in skeletal muscle • Actin – Is attached to dense bodies • Some are anchored to the sarcolemma • Some are held in place by intermediate filaments • Some anchor one cell to another • Dense bodies are analogous to the Z lines in skeletal muscle • Intermediate filaments – Are made of a protein called desmin – Form the “scaffolding” between dense bodies Fig. 10-23, p. 315 30 Smooth muscle contraction • Smooth muscle contraction is slower and longerlasting than skeletal muscle contraction • Stimulation of smooth muscle causes Ca2+ release from the SR and Ca2+ entry from the ECF – Ca2+ ions bind to the protein calmodulin – The calmodulin-Ca2+ complex activates the enzyme myosin light chain kinase – Myosin light chain kinase activates myosin, allowing cross-bridges to form – Myosin pulls on actin, and the cell shortens (“bunches up”) • Length-tension relationship – If you stretch smooth muscle, it adapts to its new length, and it can then contract again – The range of lengths over which smooth muscle contraction can occur is 4X that of skeletal muscle (this property is called plasticity) Control of smooth muscle contraction • Remember, smooth muscle is involuntarily (subconsciously/autonomically/automatically) controlled • There are 2 types of smooth muscle cells: – 1. Multiunit smooth muscle cells • Respond to stimuli from nerves that are arranged into motor units • Are precisely controlled • E.g. the iris, the walls of large arteries, and arrector pili – 2. Visceral (single unit) smooth muscle cells • May include pacesetter cells (similar to those in cardiac muscle) • Respond to local stimuli (chemicals/hormones, stretching, etc.); nervous stimulation is not required • Have gap junctions, so the tissue contracts in a rhythmic wave • E.g. the walls of the digestive tract and urinary bladder 31