community care
advertisement

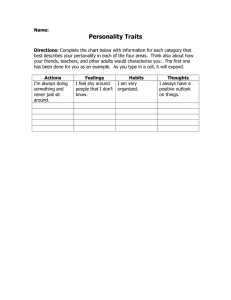
Personality Disorder Integrated Care Pathway (PD–ICP) 10: Community Care July 2015 Acknowledgements This document was produced by a partnership of NHS Highland staff, volunteers, service users and staff from other public and third sector organisations. The NHS Highland Personality Disorder Service will coordinate future reviews and updates of this document. NHS Highland would like to thank everyone involved in the creation of this document. July 2015 Contents 10 Community Care 10.1 Introduction .................................................................................................................... 10.2 Primary Care ................................................................................................................. 10.2.1 When to refer to mental health services ............................................................ 10.2.2 General Principles .............................................................................................. 10.3 Community Mental Health Teams .................................................................................. 10.3.1 Role of the CMHT in the treatment of Personality Disorder ............................... 10.3.1.1 Assessment, Diagnosis and Formulation ........................................... §1 Phase of treatment .......................................................... §2 Symptoms ........................................................................ §3 Personality Traits ............................................................ §4 Needs Assessment ......................................................... §5 Risk Assessment ............................................................. §6 Environmental Context .................................................... 10.3.1.2 Treatment and Management .............................................................. §1 What constitutes treatment of personality disorder within a CMHT? .............................................................. §2 Care planning .................................................................. §3 Co-occurring disorders .................................................... §4 Crisis planning ................................................................ §5 Phase of treatment .......................................................... §6 Care Programme Approach ............................................. 10.3.1.3 Risk management ............................................................................... 10.3.1.4 Supervision ........................................................................................ 10.3.1.5 Social Network Involvement ................................................................ References .............................................................................................................................. 10. Community Care 10.1 Introduction Personality disorder is a common disorder affecting upwards of one in ten of the general population. Of these people, around a quarter will be treatment-seeking, while about three quarters while be treatment-resisting (will not seek treatment or will actively avoid treatment). Most treatment of people with personality disorder occurs in the community. As with most conditions, large numbers of people with milder forms of the disorder will be managed within primary care, smaller numbers with more severe difficulties will be managed in secondary care and a yet smaller number with the most severe difficulties will receive input from specialist tertiary services. Even at the most severe end of the spectrum of difficulties, community treatment is generally preferred to hospital treatment for the reasons outlined in the In-patient Section. General issues relating to care and treatment of personality disorder within Primary Care and Community Mental Health Teams (CMHTs) are discussed in this section. Specific psychosocial and pharmacological interventions are discussed in their respective sections. 10.2 Primary Care People with personality disorder are heavy users of primary care services. Typically, around a quarter of people in a general practice clinic fulfil the diagnostic criteria for personality disorder. Although personality disorder may not be the given reason for attendance, the condition appears to be associated with increased rates of other mental health and physical health problems, substance use conditions, medically unexplained symptoms and frequent attendance in primary care settings. 10.2.1 When to refer to mental health services For patients already involved with mental health services, any existing care plan should be followed except in exceptional circumstances. Care plans should be made easily available in the casenotes or other patient information systems. Patients who have no current involvement with mental health services and who are assessed as needing the input of these services should be directed to the appropriate service according to whether they represent an emergency or not. Emergency referrals (those patients who require to be seen the same day for reasons of significant risk) should generally be directed to the Mental Health Assessment Team (MHAT) at New Craigs Hospital. MHAT can assess which treatment, including inpatient treatment is most appropriate. GPs in the Inverness sector may also consider referring to Braeside Crisis and Intensive Treatment Service. Braeside aims to provide an alternative to in-patient care for patients with mental disorder who present a current significant risk to themselves or others. Non-emergency referrals should be made to the sector Community Mental Health Team (CMHT) via the single point of referral. Sometimes it can be difficult to establish if a presentation is related to a mental state condition or a personality disorder (or both). In these circumstances, referral to the CMHT for clarification of diagnosis is reasonable. Other situations when referral to the CMHT might be considered include when the patient is unable to be managed solely in primary care because of issues of severity, complexity, co-morbidity or risk; or when the person’s personality appears to be acting as a vulnerability factor to mental illness. Just as it would be inappropriate for all people with depression to be referred to secondary care mental health services, so it would also be inappropriate for all people with personality disorder to be referred; matched care should be the aim. Regular communication and discussion between primary care and community mental health services is likely to be of benefit in maintaining the referral threshold at the most appropriate level. Useful referral information includes: • whether the general criteria for personality disorder are met, with some description of severity • an outline of the difficulties experienced by the patient in the four main domains: cognitive-perceptual affective interpersonal o relationship with self including sense of self o interpersonal relationships o relationship with society behavioural/impulse control (including self-harm and suicidal behaviour) • concurrent physical and mental health conditions • appropriate risk assessment, perhaps using a structured tool such as STORM 10.2.2 General Principles Whether a person has mental health services involvment or not, they are likely to continue to require the input of primary care to some degree. Every contact should be informed by the concepts and principles outlined in the General Principles Section: • Collaboration This applies equally to collaboration with the patient and collaboration with the wider team. Ensure that everyone is clear about their roles and responsibilities, and the treatment frame. The importance of personal responsibility and self-management should be emphasised. The Care Program Approach (CPA) can be very valuable in helping clarify roles and promote consistency. CPA meetings provide a valuable opportunity for professionals and the patient to assess needs and risk and develop an appropriate care plan collaboratively. While it is recommended that patients at the more severe end of the personality disorder spectrum who have multi-disciplinary or multi-agency involvement should be managed under the CPA, any clear written care plan shared between all relevant professionals and the patient is likely to improve care delivery. • Consistency Limiting the number of General Practitioners a patient sees to one or two in order to allow a good working relationship to develop can be of value in promoting collaboration and consistency. If a Care Program Approach (CPA) care plan or other written care plan is in existence, then it is important that clinicians (including out of hours staff) are aware and able to easily access the information. Inconsistency, for whatever reason, can lead to significant anxiety and dysregulation. A shared plan can make it less difficult to appropriately maintain limits in the face of pressure. Consider placing any care plan in “special notes” or similar. Often GPs, working within tight clinic schedules or in out-of-hours settings, come under significant pressure from patients in distress to “do something”. This can sometimes result in unhelpful reactive prescribing. It is important to remember that standing by a decision not to prescribe, while validating the patient’s desire for the situation to change and explaining the rationale of the care plan, is in fact often “doing something” therapeutic. If medication is felt to be appropriate, it is recommended that a written prescribing agreement is used. See Medication Section for further details. • Motivation Some suggested strategies for increasing motivation to change can be found in General Principles Section. • Validation Validation involves active listening and observation, accurate reflection of the patient’s emotions, thoughts and behaviours, and direct validation (the explicit acknowledgement of a thought, emotion or behaviour as valid and legitimate for that person, both understandable in the current context and in the context of previous experiences). It is important to recognise that validation does not necessarily imply approval. • Promotion of self-management Supporting self-management across health conditions is a key part of the role of primary care. Further information on how the concept relates to personality disorder can be found in the Self-management Section. Promoting self-knowledge and self-reflection are a component of self-management which is particularly important in personality disorder. This process may involve provision of general information about the condition but should also comprise more individual-specific knowledge gained by a process of self-reflection. Wherever possible, consider highlighting the importance of attempting to understand the mental state of oneself and others and how thoughts and emotions influence behaviour. For the clinician, a “not knowing” or gently curious style which encourages the patient to reflect on the thoughts, emotions and behaviours of themselves and others is usually more useful than simply providing patients with “the answers”. 10.3 Community Mental Health Teams People with personality disorder make up a significant component of the clinical load of CMHTs. This will include people with a primary problem of personality disorder and people with other mental disorders whose treatment may be made more challenging by coexisting personality disorder or whose personality functions as a contributing factor to other mental disorders. Most people with personality disorder in mental health services receive their treatment from generalist rather than specialist services and this is likely always to be the case. The value of a multidisciplinary team approach in treating personality disorder cannot be over-estimated and increasing evidence is emerging which suggests that generalist multi-disciplinary care based upon a shared psychologically-informed care plan can be as effective as specific psychological treatments for personality disorder. In some instances it may be clinically indicated to limit the number of professionals involved with a patient at any one time. In all cases, it is of real importance that someone in the team functions as a caseholder, keyworker or point of contact, and maintains an overview of the persons care and treatment, ideally for the duration of their involvement with the team. Over the past decade or so, documents such as the report “Personality Disorder in Scotland: Demanding Patients or Deserving People” (Scottish Executive Mental Health Division and Centre for Change and Innovation, 2004) have emphasised that no one should be excluded from services solely on the basis of a diagnosis of personality disorder. While such exclusion did unfortunately happen in the past, this practice is now regarded as absolutely unacceptable, not least because of the ever-increasing evidence base of effective treatments for personality disorder. 10.3.1 Role of the CMHT in the treatment of Personality Disorder At a minimum, CMHTs should be able to provide assessment, diagnosis and formulation, offer a variety of treatment strategies based upon the formulation, and signpost to other services as appropriate. 10.3.1.1 Assessment, Diagnosis and Formulation CMHTs should be able to provide an assessment, diagnosis and formulation function as outlined in the Assessment, Diagnosis and Formulation Section of this ICP. While most clinicians are well placed to describe and discuss personality traits and symptoms, a formal diagnosis of personality disorder should usually only be made by a senior psychiatrist. During the diagnosis process, is important that the patient receives balanced, honest feedback in a form which they can understand. Personal strengths should be emphasised while acknowledging difficulties and the importance of personal responsibility in the recovery process. Explanation of treatment options and the relatively positive prognosis should be given. For example, patients are often heartened to hear that studies suggest that around three quarters of those meeting the diagnostic criteria for borderline personality disorder no longer do so after a period of six years. While many patients describe a sense of relief on receiving a diagnosis or formulation that makes sense of their difficulties, many others find receiving a diagnosis of personality disorder an upsetting experience. This is at least in part due to myths and misinformation perpetuated by the media, and the associated stigma. Psychiatrists should consider giving verbal and written information on personality disorder when discussing the diagnosis with the patient and asking them to return with any questions once they have reflected on the information. It is also reasonable to advise patients about the large amount of misleading information regarding personality disorder on the internet, and recommend that they exercise caution in what they read. Some useful information leaflets are available in the Appendix. Occasionally, patients can have difficulty with the term “personality disorder”. If this is the case, it may be helpful to explain that the term simply serves as short hand to describe sets of symptoms and traits which typically occur together, and has the principle purpose of ensuring delivery of the treatment that is best matched to the patient’s problems. Some patients with borderline personality disorder find the reframing of their difficulties as “emotional intensity disorder” (which is the terminology used in the STEPPS program) to be more acceptable. In any case, the terminology is much less important than the clinician and patient agreeing on the presenting features. Assessment should aim to establish diagnosis and produce a formulation upon which an individual’s treatment plan should be based. Particularly important components of the assessment in guiding treatment planning include: • phase of treatment • symptoms • personality traits • needs assessment • risk assessment • environmental context §1 Phase of treatment Most commonly, patients will be referred to a CMHT needing input at phase 1 or 2. See the General Principles Section for a more detailed description of phases of treatment. §2 Symptoms Symptoms occur as a result of maladaptation of the personality to the environment. It can be helpful to think in terms of four broad headings: • cognitive-perceptual (for example, excessive suspiciousness) • affective (for example, emotional dysregulation and harmful anger) • interpersonal ◦ relationship with self including sense of self ◦ interpersonal relationships ◦ relationship with society • behavioural/impulse control (including self-harm and suicidal behaviour) §3 Personality Traits A personality trait or variable is a complex structure which represents a basic building block of personality. In any given individual, genetic factors and environmental factors transact with each other to form a complex biopsychological system which produces observable trait-based behaviour. This biopsychological system can be described in terms of both biological processes and psychological processes. Essentially, a personality trait represents a disposition to behave in a particular way. The term “trait” is also sometimes used to refer to individual features of specific personality disorders, especially when the full diagnostic criteria are not met. For example, someone meeting four of the five criteria needed for a diagnosis of borderline personality disorder may be referred to as having “borderline traits”. Some traits which are of particular importance in personality disorder are listed below with brief descriptions of associated behaviours. Traits can be usefully organised into four main higher order trait domains: dyregulated, detached, dissocial, and compulsive. There may be some overlap between some traits and it is worth noting that some of the names used for particular traits may have different meanings when used in other contexts. The traits below are drawn from the Personality Assessment Schedule (Tyrer, 2000), and other sources may label particular traits differently. It is important to remember that no personality trait is inherently negative. Many traits can be described by more than one term, some with negative connotations and some with positive connotations. For example: impulsive versus spontaneous; stubborn versus determined; aloof versus self-contained and so on. Problems arise when a person’s personality traits are maladapted to their environment. With more extreme expressions of particular traits, maladaption is likely in a greater number of environments leading to greater severity of personality disturbance. Dysregulated (Internalising) Domain Pessimism — holds a pessimistic outlook on life. Worthlessness — feelings of inferiority Lability — mood instability Anxiousness — anxiety-proneness Shyness — shyness and lack of self-confidence Sensitivity — personal sensitivity and tendency to self-reference Vulnerability — experiences excessive emotional distress when faced with adversity Childishness — excessive self-centeredness Resourcelessness — tendency to give up when faced with adversity Dependence — excessive reliance on others for advice and reassurance Submissiveness — limited ability to express own views or stand up for oneself Hypochondriasis — over-concern about illness and health Detached (Schizoid/inhibited) Domain Suspiciousness — excessive mistrust of others Introspection — prone to rumination and fantasy Aloofness — detachment and lack of interest in other people Eccentricity — oddness in behaviour and attitudes; unwilling or unable to conform Dissocial (Externalising) Domain Optimism — unrealistically optimistic, over-confident, excessively self-important Irritability — excessively irritable Impulsiveness — excessive impulsiveness Aggression — excessive levels of aggression Callousness — indifferent to the feelings of others Irresponsibility — indifferent to the consequences of one’s behaviour Compulsive (Anankastic) Domain Conscientiousness — overly fussy, perfectionistic Rigidity — inflexibility and difficulty adjusting to new situations §4 Needs Assessment While it will certainly not be necessary to provide the CPA for every patient referred to the CMHT, the Care Program Approach Needs Assessment Checklist provides a comprehensive systematic guide to needs assessment. Common areas of need for people with personality disorder, from which specific treatment goals can be identified, include: • medication including: polypharmacy compliance issues • concurrent mental health conditions including: mood and anxiety disorders substance misuse disorders • physical health including: not accessing appropriate care for medical conditions reduced self-care including suboptimal management of chronic medical conditions • emotional support including: crisis resolution containment strategies • accommodation including: difficulty maintaining a tenancy • social/interpersonal situation including: lack of interpersonal contacts lack of leisure time activities • employment, education or other meaningful, structured use of time • financial including debt problems benefits issues financial management difficulties • dependent children/ other dependents including difficulties managing childcare tasks §5 Risk Assessment Each individual risk should be specified in the care plan with indicators of an increase in risk identified. Current level of risk of each specific situation occurring should be estimated as far as possible. A clear risk management plan should be in place for each identified risk, with roles and responsibilities made explicit. Consideration should be given to the use of a recognised tool such as STORM in assessing the particular risk of suicide. The overall aim is to minimise the risk of harm to the patient and those around them, while always promoting the personal responsibility so vital for recovery. The CPA documentation provides a useful structure for risk assessment and risk management. §6 Environmental Context This includes the interpersonal and social context which should become apparent during assessment. 10.3.1.2 Treatment and Management Evidence is emerging that structured multidisciplinary treatment based upon a sound formulation can be of equal benefit to specific psychotherapies in the treatment of personality disorder. CMHTs are well placed to enable the continuity of care which is so important in maintaining consistency in the treatment of personality disorder, and to oversee the treatment plan over the longer term. As well as this more general approach, all CMHTs should be regularly delivering STEPPS groups for patients with borderline personality disorder and similar difficulties (see Psychosocial Section). CMHTs can usefully deliver focused preparatory work for STEPPS groups in the period between referral to the team and the start of the next STEPPS group, for example anxiety management strategies for people who experience anxiety in group settings. Aside from treatment directed towards personality disorder itself, community teams play a vital role in wider treatment and management including treatment of comorbidity, management and monitoring of medication and environmental management. Any treatment offered by the team should be focused and time-limited (although perhaps of long duration). At any given time, both the clinician and the patient should be absolutely clear about the nature and purpose of the work they are undertaking. Open-ended, unstructured contact should be avoided as this may encourage unhelpful dependence. If a patient is unwilling to engage in their treatment plan, motivation work may be indicated. However, sometimes, despite motivational strategies, a patient may still decide that they do not wish to engage in treatment at that time. In these cases, it may be less harmful to discharge a patient rather than engage in unfocused, unstructured, dependence-inducing contact. §1 What constitutes treatment of personality disorder within a CMHT? For an intervention to be considered a treatment for personality disorder, the primary goal must be to improve the difficulties associated with the patient’s personality disorder. A distinction can be drawn between treatments aimed at a patient “overcoming” their personality difficulties by seeking to initiate change in the patient, and treatment or interventions which “take account” of the personality difficulties in order to minimise the impact of the personality disorder on the patient and those around them. Examples of the former include psychological treatments like DBT and STEPPS and any skills reinforcement or skills generalisation carried out by the CMHT. Examples of the latter include environmental management (interventions aiming to improve adaptive fit between the person and their environment), interventions aimed at changing the social or interpersonal environment (family interventions etc) and adaptations to standard interventions for another condition (changing the treatment approach for major depressive disorder in someone with a concurrent personality disorder). §2 Care planning The following points are important to consider in collaboratively developing a care plan: • The jointly developed care plan should be based on the individual formulation and cover personality disorder and any co-occurring disorders. • The patient should be supported to develop a crisis self-management plan as early as possible in the treatment episode. • A crisis care plan identifying how a team aims to respond to a crisis should be made explicit • The phase of treatment should be clearly identified. • Risk management plans should be explicit. • Care Program Approach may by useful in helping to manage complexity or severity. See http://intranet.nhsh.scot.nhs.uk/org/dhs/mhandlearningdisabilities/cpa/Page/ Default.aspx. • Quality assurance including appropriate supervision. • Social network involvement where appropriate §3 Co-occurring disorders Personality disorder not only causes difficulties in its own right, but often functions as a vulnerability factor for other mental health problems which can frequently be more challenging to treat in the presence of personality disorder. Consequently, due attention should be paid to any personality difficulties when there are co-occurring mental health problems. It is rarely adequate to simply treat mental state disorders using standard approaches in such situations. §4 Crisis planning Crisis planning is of particular importance in personality disorder and should be a task considered very early in any treatment process. When people with personality disorder experience intense emotions, the ability to think clearly is reduced even more than it would be for other people. Hence a crisis self-management plan, with options and contacts for dealing with a crisis situation clearly listed, can be invaluable. Although a crisis may be produced in collaboration with a clinician, it necessarily remains the patient’s document. However, clearly it is likely to be beneficial for the patient to share copies with relevant people. Examples of template crisis self-management plans can be found in the Appendix. §5 Phase of treatment Identification of the phase of treatment is a primary task. This section should be read in conjunction with the General Principles Section. 1 Stabilisation (or MAKING STABLE). The focus here is on the present: a Safety and b Containment: The main aims of the first two parts of the stabilisation phase are management of symptoms and crises. Interventions should be kept simple and focused with the goal of returning the patient to the previous level of functioning as soon as possible. It is important to avoid attempting to achieve too much during the safety and containment phases of treatment. See Crisis Management Section. c Regulation and control: Once acute behavioural dysregulation has stabilised (even temporarily), work can begin on the third part of the stabilisation phase. The main aims are to promote self-management of impulsivity, self-harming behaviour and emotions. Useful strategies include behavioural analysis which can help the person to identify the antecedents and reinforcing consequences of unhelpful behaviours. Distancing, mindfulness, emotion regulation, distress tolerance and interpersonal effective skills and strategies are likely to be of value in identifying solutions. These generic approaches do not “belong” to any particular psychosocial intervention. However, while it is entirely reasonable for these skills to be taught on an individual basis outwith specific psychosocial approaches like STEPPS or DBT, it is important that the clinician and patient are clear that what is being delivered in such a situation does not constitute a DBT or STEPPS intervention. A crisis self-management plan can prove very valuable in maintaining stabilisation and preventing dysregulation by providing a clear set of helpful options when a patient’s capacity to think clearly is reduced. STEPPS and DBT are essentially stabilisation treatments which can be considered as adjunctive to standard community psychiatric care (see Psychosocial Intervention Section). If a patient in DBT or STEPPS treatment has contact with a CMHT clinician, reinforcement and generalisation of skills represents a useful focus for therapeutic work. The responsibility should rest with the patient to collaborate with the CMHT clinician in such a way that reinforcement and generalisation occurs. This may include keeping the CMHT clinician up to date on which skills are currently being taught and examples of how they are applying them in their daily lives. While the concept of a reinforcer is built into STEPPS, this concept is not a core concept of DBT. However, if a CMHT clinician has concerns that a patient in DBT is not using their CMHT time to effectively reinforce and generalise skills, then it would be reasonable to alert the DBT therapist, with the patient’s knowledge. Solutions could then be found within DBT individual therapy. DBT can be considered for patients with severe borderline personality disorder and recent, potentially lethal parasuicidal behaviour or emergency hospitalisation who are also on the Care Programme Approach. STEPPS skills training groups run within each of the CMHTs and this intervention should be considered for moderate borderline personality disorder or borderline traits (the terminology used within the STEPPS program is “emotional intensity disorder”). Ideally, every participant should have a reinforcement team. This is ideally composed of members of the social network and a health professional (CPN, GP, support worker etc). The reinforcers need not have in-depth knowledge of STEPPS but serve to help consolidation and generalisation of skills. The health professional reinforcer can support the participant to complete the weekly homework. Other ways of delivering reinforcement including by telephone or in small groups have also proven effective. Borderline problems form a continuum of severity and while benefit is likely to be greater if a patient has a full reinforcement team, service-based evidence suggests that a health professional reinforcer is not an absolute requirement, although it is certainly preferable. 2 Exploration and change (or MAKING SENSE). The focus here is on the past: This phase can involve dealing with the effects of trauma and dissociation; treating self and interpersonal problems; and treating maladaptive traits. Post-traumatic stress disorder can be treated via specific psychosocial interventions such as EMDR or trauma-focused CBT, (see Psychosocial Interventions Section). However, for less severe presentations, psychoeducation and self-directed exposure may be of value. Dissociation is likely to benefit from general improvement in emotion regulation but the patient may also benefit from learning grounding strategies. Intrapersonal (self) and interpersonal problems often relate to maladaptive schemas. These can be addressed through formal psychological interventions or by within general clinical contact by supporting self-reflection, identification of long-standing patterns of thinking and behaviour, and introduction of more adaptive patterns. For example, it might be gently brought to a patient’s attention that they have a pattern of negatively interpreting neutral comments, becoming angry and breaking off relationships. Clearly, this kind of work can very naturally take place within general clinical contact and does not need to be limited to specific psychotherapy settings. Behavioural strategies which may be useful include challenging behavioural avoidance, environmental management strategies (guided by needs assessment), behavioural rehearsal and role play. No personality trait is intrinsically maladaptive. Maladaptation occurs when the behaviours through which the trait is expressed interact with the environment to prove unhelpful. Some traits can be relatively plastic and amenable to some change but others are less so. In case of less malleable traits, the task is to modulate the trait as far as possible but also to help modify the social and environmental context so that adaptive fit is improved. In many situations, it can be helpful to view traits as relatively stable characteristics which the patient needs to learn to use constructively. • Increase acceptance and tolerance of the trait Many (but certainly not all) people with personality disorder can be intolerant of their own basic traits in contrast to most non-personality disordered individuals who are usually reasonably comfortable with their traits, even those which they would like to change. Related negative self-judgements and self-invalidation can have markedly detrimental effects in terms of self-view, emotional responses and unhelpful behaviours used to change intolerable emotional states. Mindfulness-based approaches can be helpful in increasing acceptance of traits. Psycho-education may help reduce internal conflict and increase self-acceptance. Explanation that traits are to a significant extent biologically determined can help people assume ownership of their traits, whereas emphasising the role of environmental influence on traits can help the patient understand that it is possible, within limits, to change the way traits are expressed. Another useful strategy is to encourage patients to identify ways in which their traits might be beneficial if the fit with the environment was more adaptive. A good example is the trait of conscientiousness. . Clearly, moderate levels of conscientiousness, attention to detail and orderliness would be regarded as desirable by most people. The realisation that traits are only maladaptive when they are expressed in unhelpful or inflexible ways can facilitate change by helping the person see that they do not need to change a fundamental part of themselves but rather more specific aspects of behaviour related to the trait. • Reduce trait expression For people at the extreme end of a trait distribution, the threshold for interpreting situations as relevant to the trait is low. Cognitive and behavioural strategies can be of value here in helping to restructure the way situations are perceived so that the tendency to see situations as relevant to a given trait is reduced. For example, the core beliefs and assumptions that are typical for people with high levels of anxiousness can be identified and challenged cognitively and via behavioural experiment. This may modify a tendency to over-estimate the risk associated with particular situations. Increasing behavioural alternatives can also be a useful strategy. For example, someone with high levels of submissiveness can modify trait expression by learning assertiveness skills and putting new, more assertive behaviours into practice. Similarly, teaching effective relaxation skills can provide incompatible behavioural alternatives to becoming anxious for people with high anxiousness levels. People with high levels of anxiousness and emotional lability traits could usefully attempt to substitute the unhelpful, trait-amplifying behaviours of rumination and catastrophisation with healthier, trait-reducing behaviours of problem solving, distraction and self-soothing. • Promote more adaptive trait-based behaviour The goal here is not to reduce trait expression but to replace the maladaptive behaviours associated with the trait with more adaptive behaviours. For example someone with high levels of stimulus-seeking may engage in risky sexual behaviour, become involved in fights and misuse substances. More adaptive replacement behaviours could include, for example, high-risk sports. • Promote the selection and creation of environments compatible with the adaptive expression of problematic traits This strategy is about improving the goodness of fit between the person and the environment by modifying the environment rather than the traits. For example, someone with high levels of social avoidance may function poorly in a busy sales job, but may do very well in a relatively solitary occupation such as a long distance lorry driver. Similarly, a person with high levels of compulsivity may do very well in an administrative job which requires methodical attention to detail but do less well in a less ordered work environment. Similar considerations apply to accommodation, leisure time activities and the interpersonal environment. 3 Integration and synthesis (or MAKING CONNECTIONS). The focus here is on the future: The key difference with this phase, with a primary focus on the future, is not so much about changing existing psychological and interpersonal structures and processes as putting new ones in place. The aim is to promote a more integrated sense of self and a healthier interpersonal environment — this may include development of new leisure activities, occupational or educational activities, together with new roles and relationships. A wide range of activities can help with this process of developing more stable and healthy representations of the self and others by promoting new roles, relationships and responsibilities. The role of the CMHT more likely to be in supporting this process rather than in providing the activities. §6 Care Programme Approach Where there are issues of particular complexity or severity, consideration should be given to using the Care Programme Approach or similar approach or process which supports the aims listed below: • Clarity about roles and responsibilities • Improved communication and reduced “splitting” • Regular needs assessment and planning • Regular risk assessment and planning • Allowing for the care team, rather than one individual clinician to support the patient to take positive, clinically-indicated risks. This helps avoid scenarios where one clinician is overly risk-averse to the detriment of the patient by ensuring that clinical decisions are taken in a well-reasoned way by a multidisciplinary team. • Enabling managed transition from one phase of treatment to another and ensuring that all involved are aware of the current treatment phase • Influencing the interpersonal environment (including the CMHT) to minimise the impact of personality disorder. For example, mental health services can sometimes represent most or all of a patient’s interpersonal contacts. In these cases, the balance between providing support without fostering dependency becomes very important. • Influencing nature and frequency of contact between patients and other services and agencies with a view to gains in some of the areas described in the needs assessment. This might include involving agencies such as housing in an attempt to help stabilise the environment. • Highlighting which interventions are helpful at which times and, conversely, which are not. 10.3.1.3 Risk management Many patients with personality disorder carry significant risk issues and a degree of anxiety can be experienced by patients, relatives and professionals as a result. However, elimination of risk is impossible and working in a way which tries to eliminate all risk is often harmful. Clinically indicated positive risk taking with the aim of increasing personal responsibility and development of skills is a key part of the treatment of personality disorder. Unless there is a compelling reason to do otherwise (for example, co-occurring severe mental state disorder), it is important at all times to treat a patient with personality disorder as a competent adult, with capacity to make their own choices and responsible for their own behaviour. Although the clinician is responsible for carrying out clinical practice at a reasonable standard of care, the patient is ultimately responsible for their own behaviour. This understanding is necessary to enable the collaboration between the team and the patient which is necessary for recovery. At times, patients may pose a risk to other people. Staff should remain aware of what constitutes unacceptable behaviour, taking appropriate action as per NHS Highland policy if such behaviour occurs. If the unacceptable behaviour constitutes criminal behaviour such as displays of aggression or the obstruction of health care workers in the legimate course of their duties, consideration should be given to involving the police rather than treating law-breaking as a health issue in the first instance. The importance of maintaining a safe treatment frame is paramount. Clinical experience suggests that if external behavioural modifiers such as the ability to access police and criminal justice services are inappropriately removed, then clinical, behavioural and functional deterioration is likely. An individual is unlikely to be harmed by appropriately maintaining a limit whereas they are unlikely to be helped by inappropriately ignoring a limit. Multidisciplinary care planning means that the team jointly accepts any risk associated with a patient, rather than a single clinician. The Care Program Approach can help formalise risk assessment and management plans and identify roles and responsibilities clearly. At times it may be helpful to document if a person has a chronically raised risk of completed suicide (for example in situations where a history of parasuicidal behaviour is present), which treatments have been offered and what has been helpful, unhelpful or harmful. It is important to distinguish between chronic and acute risk of suicide. Acute risk increase often occurs in the presence of increased impulsivity or intent. Important factors to consider in reviewing an adverse event are: • Was there a foreseeable risk? Appropriate assessment and documentation of risk is crucial. • Was there a reasonable response? Any decision should be well reasoned, come from a caring, therapeutic position and have a documented cost-benefit analysis. This allows for clinically indicated (but sometimes superficially counterintuitive) responses. For example, not admitting someone with potentially lethal self-harming behaviour to hospital. • Was there a reasonable standard of practice? Quality of practice should be assured with regular supervision and communication with the rest of the team. Relevant guidance should be followed and reasons documented if it is not. Documentation should be of a reasonable standard. 10.3.1.4 Supervision Appropriate supervision is important for clinicians providing treatment for individuals with personality disorder. Peer supervision, discussion within multidisciplinary team meetings, time within usual clinical supervision and specific supervision may all be valuable according to the nature, severity and complexity of the situation. The Personality Disorder Service is available for consultation as appropriate. 10.3.1.5 Social Network Involvement The issue of carer involvement in the treatment of personality disorder is a contentious one. There is even some controversy over the term carer itself inasmuch as it is deemed by some to be an invalidating term which moves the focus from self-management. Bearing that in mind, the term “social network” is used here. It is recommended that consideration of individual circumstances is given in relation to social network involvement. Some patients will be very keen to avoid such involvement for a variety of reasons and this should always be respected. However, involvement of social supports can sometimes be helpful in modifying the interpersonal environment. If the decision is made to involve social supports, education about personality disorder and how it can present can be helpful to all concerned. References Appleby, L., et al. (2000). An educational intervention for front-line health professionals in the assessment and management of suicidal patients (The STORM Project). Psychological Medicine, 30(4), 805–812. 2, 14 Bateman, A., & Krawitz, R. (2013). Borderline Personality Disorder—An evidence-based guide for mental health professionals. Oxford. Blum, N., et al. (2008). Systems training for emotional predictability and problem solving (STEPPS) for outpatients with borderline personality disorder: A randomized controlled trial and 1-year follow-up. American Journal of Psychiatry, 165, 468–478. Davidson, K. (2008). Cognitive Therapy for Personality Disorders. Routledge. Division, S. E. M. H., for Change, C., & Innovation. (2004). Personality Disorder in Scotland: Demanding Patients or Deserving People? Linehan, M. (1993). Cognitive-Behavioural Treatment of Borderline Personality Disorder. Guilford. Livesley, J. (2003). Practical Management of Personality Disorder. Guilford. Murphy, M., & McVey, D. (Eds.). (2010). Treating Personality Disorder. Routledge. National Institute for Mental Health in England. (2003). Personality Disorder: No longer a diagnosis of exclusion. NICE. (2009). Borderline Personality Disorder Treatment and Management. NICE Clinical Guideline 78. Samson, M., McCubbin, R., & Tyrer, P. (2006). Personality disorder and community mental health teams. Wiley. Tyrer, P. ed. (2000). Personality Assessment Schedule. In Personality Disorders: Diagnosis, Management and Course (pp. 133–159). Butterworth Heinemann.