Perioperative Management of Patients with Cardiac Rhythm
advertisement
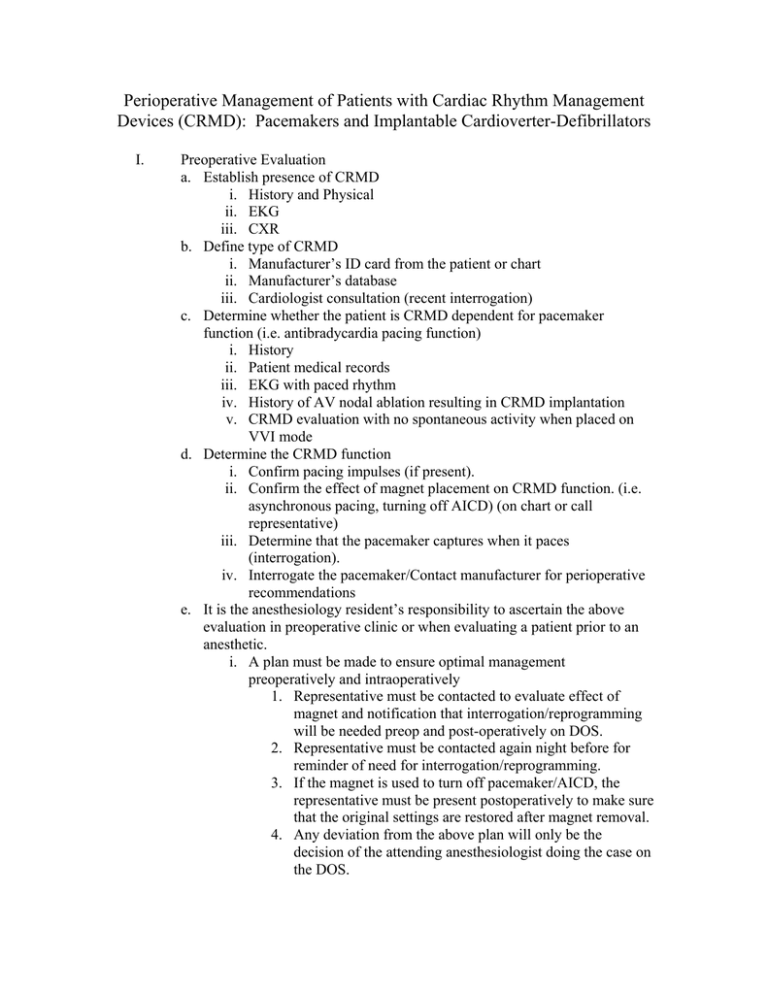
Perioperative Management of Patients with Cardiac Rhythm Management Devices (CRMD): Pacemakers and Implantable Cardioverter-Defibrillators I. Preoperative Evaluation a. Establish presence of CRMD i. History and Physical ii. EKG iii. CXR b. Define type of CRMD i. Manufacturer’s ID card from the patient or chart ii. Manufacturer’s database iii. Cardiologist consultation (recent interrogation) c. Determine whether the patient is CRMD dependent for pacemaker function (i.e. antibradycardia pacing function) i. History ii. Patient medical records iii. EKG with paced rhythm iv. History of AV nodal ablation resulting in CRMD implantation v. CRMD evaluation with no spontaneous activity when placed on VVI mode d. Determine the CRMD function i. Confirm pacing impulses (if present). ii. Confirm the effect of magnet placement on CRMD function. (i.e. asynchronous pacing, turning off AICD) (on chart or call representative) iii. Determine that the pacemaker captures when it paces (interrogation). iv. Interrogate the pacemaker/Contact manufacturer for perioperative recommendations e. It is the anesthesiology resident’s responsibility to ascertain the above evaluation in preoperative clinic or when evaluating a patient prior to an anesthetic. i. A plan must be made to ensure optimal management preoperatively and intraoperatively 1. Representative must be contacted to evaluate effect of magnet and notification that interrogation/reprogramming will be needed preop and post-operatively on DOS. 2. Representative must be contacted again night before for reminder of need for interrogation/reprogramming. 3. If the magnet is used to turn off pacemaker/AICD, the representative must be present postoperatively to make sure that the original settings are restored after magnet removal. 4. Any deviation from the above plan will only be the decision of the attending anesthesiologist doing the case on the DOS. ii. You must discuss this plan with an attending anesthesiologist assigned to preop iii. The primary service (resident, chief resident, or attending) must be aware of the plan the night before as to placing a magnet or the need the representative to reprogram the CRMD. Documentation of this conversation must be made on the preoperative paperwork. f. Company Representatives and Contact information i. Guidant Kevin Fosdick, RN, RCIS Cell: 760 908-3487 1-800-CARDIAC ii. Medtronic Shawn Murdock Cell: 310-600-4466 iii. St. Jude Medical Steve Rons Sales Rep Cell: 619 887-0351 II. Preoperative Management a. Determine if electromagnetic interference (EMI) is anticipated during the case i. Electrocautery ii. Radiofrequency ablation (RFA) iii. Magnetic Resonance Imaging (MRI) iv. Radiation Therapy v. Extracorporeal Shock Wave Lithotripsy (ESWL) b. Determine if reprogramming the CRMD to asynchronous pacing mode is needed. i. Representative should be available on the operative day as discussed during the preoperative visit. ii. Magnet when applicable iii. Representative can reprogram 1. Determine optimal rate given the patient’s medical comorbidities. (i.e. HR 65-70 bpm in cardiac patient instead of default HR of 100bpm) c. Suspending any antitachyarrhythmia/cardioverter-defibrillation functions present i. Turn off the AICD portion d. Advising the operative surgeon to consider using bipolar electrocautery or harmonic scalpel to minimize potential adverse events e. Assure the availability of temporary pacing and defibrillation equipment i. Place trancutaneous pacing/defibrillator pads when necessary/indicated. f. Evaluate the possible effects of anesthetic techniques and of the procedure on CRMD function and interactions. i. Anesthetic induced physiologic changes may induce unexpected CRMD responses or adversely affect the CRMD-patient interactions. III. Intraoperative Management a. Intraoperative EKG b. Monitoring peripheral pulse (i.e. pulse oximetry) i. Any unexpected interactions should postpone/discontinue case until source of interaction is elucidated c. Manage potential sources of EMI i. Assure that the electrocautery receiving pad is positioned so that the pathway does not pass through or near the CRMD system. (i.e. superior posterior aspect of the shoulder contralateral to the generator position for a Head and Neck case) ii. Advise the operative surgeon: 1. avoid proximity of the cautery’s electrical field to the pulse generator and leads 2. use short, intermittent, and irregular bursts at the lowest feasible energy levels 3. consider use of bipolar electrocautery or harmonic (ultrasound) scalpel in place of monopolar electrocautery iii. Radiofrequency Ablation (RFA) 1. Should keep the RF current path as far away from the pulse generator and lead system as possible. 2. Avoid direct contact between ablation catheter and the CRMD and leads iv. Lithotripsy (ESWL) 1. Avoid focusing the lithotripsy beam near the pulse generator 2. If beam triggers on R wave of EKG, consider preoperative disabling of atrial pacing v. MRI 1. Generally contraindicated 2. If must be performed, consult with cardiologist, ordering physician, radiologist, and CRMD manufacturer vi. Radiation Therapy 1. Can be safely performed in patients with CRMDs unless in the field of radiation vii. Electroconvulsive Therapy (ECT) 1. May have associated transient or long-term myocardial and nervous system effects 2. If ECT must be performed, consult with the ordering physician and cardiologist to plan for the first and subsequent ECTs. 3. All CRMDs should undergo a comprehensive interrogation before the procedure. 4. ICD functions should be disabled for the shock therapy during ECT 5. CRMD-dependent patients may require temporary transcutatneous pacemaker to preserve rate and rhythm during shock therapy 6. CRMD may require programming to asynchronous activity to avoid myopotential inhibition of the device in pacemaker-dependent patients. d. Emergency Defibrillation i. If emergency defibrillation is needed: 1. Reenable antitachycardia therapies by a. Removing magnet to turn on antitachycardia function b. Reprogram to turn on AICD c. Place defibrillator/cardioverter pads in an anteroposterior placement as far away from the pulse generator IV. Postoperative Management a. Continuously monitor cardiac rate and rhythm. b. Have backup pacing and defibrillation equipment immediately available in the postoperative period. c. Representative should be available, as discussed in the preoperative visit to interrogate and restore CRMD function in the immediate postoperative period. d. Restore all antitachyarrhythmic therapies in the ICDs. Practice advisory for the perioperative management of patients with cardiac rhythm management devices: pacemakers and implantable cardioverter-defibrillators: a report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Rhythm Management Devices. American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Rhythm Management Devices. Anesthesiology 2005;103(1):186-98.