Journal of Biomechanics 43 (2010) 2657–2664
Contents lists available at ScienceDirect
Journal of Biomechanics
journal homepage: www.elsevier.com/locate/jbiomech
www.JBiomech.com
Alterations to movement mechanics can greatly reduce anterior cruciate
ligament loading without reducing performance
Casey A. Myers a,c, David Hawkins a,b,c,n
a
Exercise Science Graduate Group, University of California, Davis, CA 95616, United States
Department of Neurobiology, Physiology and Behavior, University of California, Davis, CA 95616, United States
c
Human Performance Laboratory, University of California, Davis, CA 95616, United States
b
a r t i c l e in fo
abstract
Article history:
Accepted 25 June 2010
Anterior cruciate ligament (ACL) injuries are one of the most common and potentially debilitating sports
injuries. Approximately 70% of ACL injuries occur without contact and are believed to be preventable.
Jump stop movements are associated with many non-contact ACL injuries. It was hypothesized that an
athlete performing a jump stop movement can reduce their peak tibial shear force (PTSF), a measure of
ACL loading, without compromising performance, by modifying their knee flexion angle, shank angle,
and foot contact location during landing. PTSF was calculated for fourteen female basketball players
performing jump stops using their normal mechanics and mechanics modified to increase their knee
flexion angle, decrease their shank angle relative to vertical and land more on their toes during landing.
Every subject tested experienced drastic reductions in their PTSF (average reduction¼ 56.4%) using
modified movement mechanics. The athletes maintained or improved their jump height with the
modified movement mechanics (an average increase in jump height of 2.5 cm). The hypothesis was
supported: modifications to jump stop movement mechanics greatly reduced PTSF and therefore ACL
loading without compromising performance. The results from this study identify crucial biomechanical
quantities that athletes can easily modify to reduce ACL loading and therefore should be targeted in any
physical activity training programs designed to reduce non-contact ACL injuries.
& 2010 Elsevier Ltd. All rights reserved.
Keywords:
ACL
Training programs
Mechanics
1. Introduction
Anterior cruciate ligament (ACL) injuries are one of the most
common and potentially debilitating sports related injuries. It has
been estimated that between 80,000 (McLean et al., 2003) and
175,000 (Gottlob et al., 1999; Gottlob and Baker, 2000) ACL injuries
occur annually within the United States. The annual cost to treat
ACL injuries has been estimated between one and two billion
dollars. Additionally, this injury has a traumatic impact on quality
of life. ACL injury presents an eight to ten fold increase in the longterm incidence of osteoarthritis (Gillquist and Messner, 1999;
Lohmander et al., 2007). 70% of all ACL injuries occur without
contact and injured individuals frequently report that the injury
occurred while performing a movement they had performed
numerous times before without incidence (Conn et al., 2003).
It has been well documented that female athletes exhibit a
four to eight fold higher incidence of ACL injury compared to male
athletes participating in the same sports. This fact has led many
researchers to investigate the influence of anthropometric and
n
Corresponding author at: One Shields Avenue, College of Biological Sciences,
Department of Neurobiology, Physiology, and Behavior, Room 196, Briggs Hall,
University of California, Davis, CA 95616, USA. Tel.: + 1 530 752 2748;
fax: + 1 530 752 6681.
E-mail address: dahawkins@ucdavis.edu (D. Hawkins).
0021-9290/$ - see front matter & 2010 Elsevier Ltd. All rights reserved.
doi:10.1016/j.jbiomech.2010.06.003
hormonal factors on ACL loading. Characteristics such as higher
blood estrogen concentrations, decreased femoral notch width,
and increased Q-angle (a measure of leg alignment), have been
associated with greater risk for sustaining an ACL injury
(Shelburne et al., 1998; Hewett et al., 2006). While these factors
may play an important role in an individual’s risk for sustaining
an ACL injury, they are not under the functional control of an
athlete and therefore not easily modified to reduce injury risk. The
focus of this investigation was on factors associated with ACL
injury that an athlete can easily modify.
The purpose of this study was to determine if an athlete
performing a jump stop movement can reduce their peak tibial
shear force (PTSF), a measure of ACL loading, without compromising
performance, by modifying their knee flexion angle, shank angle,
and the part of the foot contacting the ground during landing.
2. Methods
Fourteen high school and collegiate women basketball players were recruited.
Subjects were required to have 2 years of playing experience and have no history
of knee pathology. All procedures were approved by the University of California,
Davis Medical Center Human Subjects Institutional Review Board. The subjects’
height, weight, foot length, and Achilles tendon moment arm were measured
using standard anthropometric measurement tools. Dempster’s (1955) regression
equations were used to estimate mass, center of mass, and moment of inertia for
each segment of the lower limb.
2658
C.A. Myers, D. Hawkins / Journal of Biomechanics 43 (2010) 2657–2664
Subjects were prepared for surface electromyogram (EMG) data collection.
Surface electrodes were applied to the skin over the right vastus medialis, vastus
lateralis, biceps femoris, semimembranosus, tibalis anterior, and the medial head
of the gastrocnemius muscles. Electrodes were connected to a Noraxon
telemetered EMG system (Noraxon USA, Inc., Scottsdale, Arizona).
Isometric maximum voluntary contraction (MVC) knee flexion/extension and
ankle plantar flexion torque were recorded along with EMG data. Subjects were
strapped into a Biodex (Biodex Medical Systems, Inc., Shirley, New York) and
performed three isometric MVC knee extension trials followed by three isometric
MVC knee flexion trials. Subjects then completed three isometric MVC ankle
plantar flexion trials while positioned in a customized chair equipped with a force
transducer. In all trials, the knee angle was fixed at 301 to represent the average
knee angle during a jump stop landing. Torque and EMG data were collected
during each MVC effort.
Reflective markers were attached to the subject’s body to facilitate kinematic
analysis. One inch diameter retro-reflective spheres were taped to the right side of
the subject’s body on the skin covering the calcaneus, 5th metatarsal, lateral and
medial malleoli, lateral and medial femoral epicondyles, the lateral and medial
anterior superior iliac spines (ASIS), and shoulder. A marker triad was placed in the
middle, lateral aspect of the shank and thigh. A two marker rod was also placed at
the midpoint of the two posterior iliac spines (PSIS) and used to generate a virtual
marker of the hip expressed in the thigh coordinate system according to the BellPSIS rod method (Bell et al., 1990). Virtual markers of the ankle and knee joint
centers, expressed in the shank coordinate system, were generated by calculating
the midpoint between medial and lateral markers located at these joints (Fig. 1).
Subjects performed jump stop movements similar to those performed in
basketball practice drills. They ran 6.1 m towards a force platform (roughly the
distance from the NCAA three point line to the basket) and performed a jump stop
in the field of view of four digital cameras. Subjects were instructed to go ‘full
speed’, using an approach speed that mimicked that used during competition. The
subjects landed from the initial jump with both feet striking the ground at the
same time, flexed their knees, and attempted to jump as high as possible towards a
simulated basket. The initial landings were analyzed for trials in which the subject
landed on both feet simultaneously with the right foot contacting the force plate. A
total of 10–15 ‘‘baseline’’ jump stop trials were collected in which no instruction
was given to the subjects regarding their landing mechanics.
Subjects were then instructed to perform the jump stop task using a modified
movement strategy. The intervention targeted: increasing the amplitude of the
jump prior to landing, increasing the amount of knee flexion at landing, and
striking the ground with the toes first. All subjects received the same verbal
instructions and a physical demonstration of the desired changes to their landing
mechanics. Subjects were asked to practice the jump stop using the altered
technique until they felt comfortable performing the movement at full speed. Data
were then collected as the subjects performed 10–15 intervention jump stop trials.
Performance measures that included the vertical jump height, approach velocity,
and time on the force plate were calculated to assess changes in the subjects’ jump
stop performance.
Video, EMG, and force platform data were collected during each jump stop
movement. A motion analysis system (Motion Analysis Corporation, Santa Rosa,
CA) recorded video data at 240 Hz. Custom software developed using LabView 7.0
was used to collect Kistler force platform (Kistler Corporation, Winterthur,
Switzerland) data and EMG data at 960 Hz.
Force platform, video, and anthropometric data were combined to estimate
intersegmental forces and moments using standard inverse dynamics analysis
techniques (Fig. 2, left, Eqs. 1–6) (Winter, 1990). The resultant intersegmental
forces at the knee were then transformed into a shank reference frame (Fig. 2,
middle, Eqs. 7 and 8).
A distribution analysis technique, similar to ones used by Escamilla et al.
(1998), Zheng et al. (1998), and Escamilla et al. (2009), was used to estimate tibial
shear force (TSF). TSF represents the component of the intersegmental force minus
muscle forces acting in a direction parallel to the tibial plateau (Fig. 2, right) (Eqs. 9
and 10). The passive structures of the knee that can contribute to this force include
the cruciate ligaments, the collateral ligaments, the menisci, and bone on bone
contact forces. It is difficult to quantify individual structure contributions to TSF;
however, studies have shown that the ACL provides approximately 90% of the total
resisting force to anterior displacement (Butler et al., 1980). Though it is difficult to
accurately determine absolute ACL force or TSF values, for purposes of this study, it
was reasonable to compare relative peak tibial shear force (PTSF) values between
baseline and intervention conditions within subjects to test the hypothesis and
determine if the intervention altered peak ACL loading.
Muscle forces acting at the knee (gastrocnemius, hamstrings, and quadriceps)
were estimated using an EMG and velocity-based muscle force model. A linear
relationship between the magnitude of a filtered and normalized EMG signal and
the isometric MVC muscle force was created using the torque data collected from
the MVC trials. Muscle force was adjusted for muscle velocity. To calculate muscle
velocity, angular velocity data of the included hip, knee, and ankle angles,
calculated from the marker position data taken during the jump stop trials, were
combined with the muscle moment arm data estimated using SIMM (Software for
Interactive Musculoskeletal Modeling, Motion Analysis Corporation, Santa Rosa,
CA) and the default leg model. A Hill force–velocity relationship (Hill, 1970) (Fig. 2,
Eqs. 11 and 12) was used to scale the muscle forces. A 40 ms electromechanical
delay was used to account for the time between EMG onset and force onset (Lloyd
and Besier, 2003). Muscle forces (Fig. 2, Eq. 13) were subtracted from the resultant
intersegmental knee force. TSF was calculated as the component of this force
difference acting parallel to the tibial plateau (Fig. 2, Eq. 10). Average PTSF was
determined for the baseline and intervention condition. These values were
compared for all 14 subjects using a paired T-test.
3. Results
On average, the intervention significantly changed two of the
three target quantities. Subjects increased their knee flexion angle
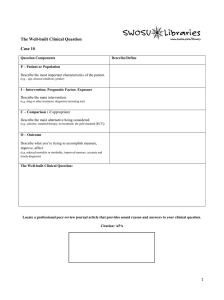
Fig. 1. Illustration of the full set (left) and subset of reflective markers (right) used to quantify movement kinematics during jump stop testing. Video of the full marker data
set was obtained while the subject stood stationary on the force plate. These data were used to quantify the location of virtual markers that could be determined from a
subset of markers. The subset of markers was left in place during the jump stop testing, but the other markers were removed. Left: 1, 5th metatarsal; 2, Calcaneus; 3, lateral
malleous; 4, medial malleous; 5, shank trial; 6, lateral epicondyle; 7, medial epicondyle; 8, thigh triad; 9, left ASIS; 10, right ASIS; 11, shoulder; 12, rod #1; 13, rod #2.
Right: 1, 5th metatarsal; 2, Calcaneus; 3, shank triad; 4, thigh triad.
C.A. Myers, D. Hawkins / Journal of Biomechanics 43 (2010) 2657–2664
2659
Fig. 2. Free body diagrams (FBD) of the foot and shank during the jump stop (left), the intersegmental forces at the knee transformed from the global reference frame into a
local shank reference frame (middle) and the distribution of the intersegmental forces at the knee among various structures (right). Equations used in the inverse dynamics,
distribution problem, and muscle force estimation analyses are shown below the FBD. Abbreviations and symbols: Rx, ground reaction force in the X-direction; Ry, ground
reaction force in the Y-direction; g, gravity (9.81 m/s/s); mF, mass of foot; aFx, acceleration of the foot in the X-direction; aFy, acceleration of the foot in Y-direction; aF,
angular acceleration of the foot; MA, moment at the ankle; FAx, force at the ankle in the X-direction; FAy, force at the ankle in the Y-direction; mS, mass of the shank; aSx,
acceleration of the shank in the X-direction; aSy, acceleration of the shank in the Y-direction; aS, angular acceleration of the shank; FKx, force at knee in the X-direction; FKy,
s
S
force at the knee in the Y-direction; FKx
, force on knee in the X-direction in the shank coordinate system; FKx
, force on knee in the Y-direction in the shank coordinate
system; yS, the angle of the shank with respect to the vertical YG; MK, moment at the knee; FQuads, quadriceps muscle force; FHams, hamstrings muscle force; FGastroc,
gastrocnemius muscle force; FL, knee ligament force, either ACL or PCL depending on resultant knee force direction; FAT, achilles tendon force; Fc, menisci cartilage force; FB,
bone contact force; TSF, tibial shear force. If bone and cartilage forces act primarily perpendicular to the tibial plateau, then TSF is a reasonable estimate of ACL force when
it is directed posteriorly, in the direction of the line of action of the ACL; XAB, horizontal distance from foot center of pressure (A)–foot center of mass (B); XCB, horizontal
distance from ankle joint center (C)–foot center of mass (B); XDC, horizontal distance from Shank center of mass (D)–ankle joint center (C); XED, horizontal distance from
knee joint center (E)–shank center of mass (D); YB, 0–vertical height of foot center of mass (B); YCB, vertical distance from Ankle joint center (C)–foot center of mass (B); YDC,
vertical distance from shank center of mass (D)–ankle joint center (C); YED, vertical distance from knee joint center (E)–shank center of mass (D).
2660
C.A. Myers, D. Hawkins / Journal of Biomechanics 43 (2010) 2657–2664
Fig. 2. (Continued)
an average of 5.31 and moved the center of pressure at contact an
average of 6.6 cm closer to their toes. There was no change in
shank angle relative to the vertical during landing (Table 1). The
subjects basically performed the intervention jump stops with
greater bend at the knees and landed more on their toes.
All subjects experienced a reduction in PTSF between the
baseline and intervention conditions (Fig. 3). The average
intervention PTSF was significantly less than the average
baseline PTSF for all subjects (0.38 70.28 body weight (BW) vs.
0.8170.42 BW; Po0.001). The average change in PTSF from the
baseline condition to the intervention condition was
0.43 BW 70.27, a 56.4% reduction. Additionally, PTSF occurred
significantly earlier following ground contact in the intervention
trials versus the baseline trials (4.3 76.8 ms vs. 19.7 77.1;
Po0.001).
Several quantities that affect PTSF (see Eq. 10d, Fig. 2) were
affected by the intervention. On average, there was 7.8% decrease
in their average peak resultant ground reaction force (PRGRF) for
the intervention condition compared to the baseline condition
(3.6871.06 BW vs. 3.9971.40 BW). There was a significant 25.7%
decrease in the resultant shank center of mass acceleration at
contact (39.3712.0 m/s/s vs. 52.9713.1 m/s/s; Po0.05) (Table 2).
The magnitude of the changes to various quantities resulting
from the intervention varied between subjects (Fig. 4). 11 of the
C.A. Myers, D. Hawkins / Journal of Biomechanics 43 (2010) 2657–2664
2661
Table 1
Mean intervention target variable values from the baseline and the intervention conditions. The knee angle at contact was significantly larger for the intervention vs.
baseline condition. Center of pressure (COP) of the ground reaction force relative to the foot center of mass (COM) was significantly larger for the intervention vs. baseline
condition, illustrating that jump stops were performed with the toes striking the ground first during the intervention condition versus the majority of jump stops
performed with the heels striking the ground first in the baseline condition. Shank angle with respect to the vertical was used as an assessment of changes to approach
jump amplitude and demonstrated no difference between baseline and intervention conditions.
Intervention target variable
Baseline
SD
Intervention
SD
19.6
0.018
18.9
5.9
0.099
5.2
24.9
0.048
19
8.4
0.022
4.5
*
Knee angle at contact (deg.)
COP relative to foot COM (m)*
Shank angle with respect to the vertical (deg.)
*
Significant difference Po 0.05.
2.5
Baseline PTSF
Intervention PTSF
Mean PTSF (BW)
2.0
1.5
1.0
0.5
0.0
1
2
3
4
5
6
7 8 9 10 11 12 13 14
Subject #
Fig. 3. A comparison of mean magnitude of baseline condition peak tibial shear
force (PTSF) when directed posterior with mean magnitude of intervention
condition PTSF when directed posterior 7 1 standard deviation for all subjects. All
14 subjects demonstrated a reduction in PTSF following the intervention. Data
normalized to body weight (BW).
Table 2
Mean peak ground reaction force (GRF) values for the baseline condition and the
intervention condition. Peak resultant ground reaction force (PRGRF), peak vertical
ground reaction force (PVGRF), and peak shear ground reaction force (PSGRF) all
demonstrated slight, but not significant, decreases for the intervention condition
vs. baseline condition. There was a significant decrease in the resultant shank
center of mass acceleration (RScom Acc) at contact, but no change at the point of
peak tibial shear force (PTSF). There were reductions in shank angular acceleration
(as) that did not prove to be significant.
*
GRF and shank acceleration
Baseline
SD
Intervention
SD
PRGRF (BW)
PVGRF (BW)
PSGRF (BW)
RScom Acc at contact (m/s/s)*
RScom Acc at PTSF (m/s/s)
as at contact (rad/s/s)
as at PTSF (rad/s/s)
3.99
3.63
1.66
52.9
40.0
121.0
187.9
1.40
1.27
0.57
13.1
12.2
81.4
59.8
3.68
3.34
1.54
39.3
39.6
194.7
156.5
1.06
1.02
0.36
12.0
10.4
59.7
92.4
Significant difference Po 0.05.
14 subjects demonstrated a significant increase in knee flexion at
foot contact during the intervention compared to the baseline
condition (24.978.41 vs. 19.675.91, Po0.01) (Fig. 4A). Subjects
2, 5, and 14 did not significantly increase their knee flexion angle
at contact and yet had an average reduction in PTSF of 44.8%.
These subjects successfully performed toe strikes during the
intervention conditions, moving the center of pressure of the
ground reaction force at contact, an average of 12.5 cm75.2 from
the rear portion of the foot to the front portion of the foot
(Fig. 4B). While toe strikes that were accompanied by an increase
in knee flexion angle at contact produced the largest decreases in
PTSF, some subjects were able to reduce PTSF without increasing
their knee angle (Fig. 5).
On average for all subjects, jump stops performed during the
intervention tended to result in the PRGRF being directed behind
the knee joint center (Kjc) (a negative moment arm), while half of
those performed in the baseline condition resulted in PRGRF
directed in front of the Kjc (a positive moment arm) (3.0 73.5 cm
vs. 5.274.4; p o0.01) (Fig. 4C). Jump stop trials in which the
PRGRF was directed in front of the Kjc resulted in PTSF values 3
times greater than jump stop trials in which the PRGRF was
directed along the axis of the shank or behind the Kjc
(1.3170.52 BW vs. 0.4370.35 BW; Po0.001). The largest PTSF
values in the posterior direction, in the direction of the line of
action of the ACL, occurred when the PRGRF was directed in front
of the Kjc. When the PRGRF was directed behind the Kjc, PTSF was
much lower and/or directed in the anterior direction, in the
direction of the line of action of the PCL (Fig. 6).
The intervention did not result in any compromise in
performance. There was a significant 2.5 cm increase in vertical
jump height from the baseline condition to the intervention
condition (23.477.0 vs. 25.9 76.2; Po0.05) and no change to
either approach velocity or time on the plate (Table 3).
4. Discussion
Female basketball players were able to significantly reduce
their PTSF during a jump stop maneuver (22.0–87.9%) by making
adjustments to their movement mechanics, increasing knee
flexion and/or contacting the ground with the toes first. The
movement mechanics adjustments did not reduce the subjects’
jump stop performance, but rather increased their vertical jump
height, by an average of 2.5 cm. All subjects performed at least 10
baseline jump stops prior to performing the intervention trials;
therefore, an analysis was performed to determine if reductions in
PTSF could have resulted from the practice. There was no
correlation between PTSF and baseline condition trial number.
Therefore, we are confident that the reductions in PTSF from the
baseline to intervention condition were not a result of practice.
These results are certainly noteworthy and support the hypothesis that simple modifications in joint mechanics can greatly
reduce ACL loading without sacrificing performance.
Previous studies demonstrated that when the knee angle is
greater than 301 of flexion, the ACL experiences very little strain
(Cabaud, 1983). Therefore, it was thought that landings that
occurred with the knee angle greater than 301 of flexion would
place lower loads on the ACL compared to landings involving
more extended knee angles. While the subjects did not on average
have knee angles greater than 301 during the intervention, an
increase from an average knee angle at foot contact of 19.6 75.91
in the baseline condition to 24.9 78.41 in the intervention
condition was sufficient to produce significant reductions in PTSF
2662
C.A. Myers, D. Hawkins / Journal of Biomechanics 43 (2010) 2657–2664
Fig. 4. A: Each subject’s mean knee angle at contact 71 standard deviation for baseline condition jump stops compared to intervention condition jump stops. Only three
subjects failed to demonstrate an increase in the average knee angle at contact from baseline to intervention. B: Each subject’s center of pressure (COP) relative to the foot
center of mass (COM) at contact 7 1 standard deviation for baseline condition jump stops compared to intervention condition jump stops. C: Each subject’s moment arm of
the peak resultant ground reaction force (PRGRF) relative to the knee joint center (Kjc) 7 1 standard deviation for baseline condition jump stops compared to intervention
condition jump stops. D: Each subject’s peak resultant ground reaction force 7 1 standard deviation for baseline condition jump stops compared to intervention condition
jump stops.
while maintaining performance. These finding are consistent with
those from Chappell et al. (2002) and Malinzak et al. (2001) who
showed that females performing a landing task with low angles of
knee flexion are at risk for injury. Yu et al. (2005) showed that
soccer players started decreasing their knee flexion angle during a
jump stop task after 13 years of age. An increase of 51 in knee
flexion angle at contact can make significant reductions in ACL
loads and lower the risk of injury for these females.
Jump stops performed with larger ground reaction forces
(GRFs) did not always lead to higher PTSF values, as has been
suggested in the literature. Larger GRFs have been linked to ACL
injury by the large knee flexion moments that result from
landings with greater GRFs (Yu and Garrett, 2007). However,
without considering factors such as the direction of the ground
reaction force, the knee angle and a breakdown of the components of the GRF, it is difficult to assess whether the GRF profile
contributes to ACL loading or not. This is evident by examination
of Eq. 10. The ground reaction force can contribute to a posterior
or anterior tibial shear force depending on the direction of the
force relative to the angle of the shank. Directing the GRF behind
the knee rather than in front of the knee can greatly reduce ACL
loading, despite the fact that this causes a knee extension moment
that must be overcome by the quadriceps. This can occur if the
GRF causes a resultant intersegment knee force with an anterior
tibial shear component that exceeds the anterior tibial shear force
created by the quadriceps force. This can easily occur because the
quadriceps force acts more to compress the knee and rotate the
shank relative to the femur than it does to create an anterior shear
force at the knee (Herzog and Read, 1993).
This study was limited to a two dimensional analysis of the
behavior of the knee joint in the sagittal plane. There is evidence
to suggest that twisting and valgus moments that act outside of
this plane can be associated with the ACL injury mechanism
(Hewett et al., 2005; Sigward and Powers, 2007; Quatman and
Hewett, 2009). They were not assessed in this study because
studies that have analyzed combined loading states that produce
high ACL forces in-vitro have concluded that a twisting or valgus
moment does not produce significant strain in the ACL in the
absence of anterior displacement of the tibia relative to the femur
(Berns et al., 1992; Markolf et al., 1995; Fleming et al., 2001).
Therefore, it was thought that altering the forces and moments
acting in the sagittal plane would provide the most direct means
to decrease the loads on the ACL. Future studies could assess how
the intervention changes frontal plane kinematics and what affect
that has on ACL loading.
Current ACL injury prevention programs emphasize plyometrics, flexibility, and muscle strengthening training. These
programs claim to decrease impact forces, increase quadriceps
and hamstrings strength and activation and decrease injury risk
(Hewett et al., 1996, 1999; Lephart et al., 2005; Gilchrist et al.,
2008). Our results indicate that while lowering impact forces can
be beneficial to lowering knee loading, it may not be as important
C.A. Myers, D. Hawkins / Journal of Biomechanics 43 (2010) 2657–2664
2663
Fig. 5. A surface plot illustrating the interaction between knee angle at contact, the center of pressure (COP) relative to the foot center of mass (COM) at contact and peak
tibial shear force (PTSF). Illustrated are specific data from two different subjects. Subject 3 moved the center of pressure at contact 11.4 cm anterior on the foot between the
baseline condition and the intervention condition (1.47 7.6 cm vs. 12.8 7 4.6) and demonstrated a 20.71 increase in knee flexion angle at contact (10.17 4.01 vs. 30.87 3.3)
and a 71.2% reduction in the magnitude of the posterior-directed (negative) PTSF from baseline to intervention (1.129 7 0.403 BW vs. 0.325 7 0.194). Subject 2 saw no
change in knee angle at contact but moved the center of pressure at contact 14.9 cm anterior on the foot ( 7.3 7 4.6 cm vs. 7.6 72.1), and had a 54.4% reduction in PTSF
(0.727 70.287 BW vs. 0.332 70.159).
Fig. 6. A surface plot illustrating the interaction between the moment arm of the peak resultant ground reaction force (PRGRF), the magnitude of the PRGRF, and peak tibial
shear force (PTSF). Illustrated is a specific example from two different subjects. Not only did subject 14 demonstrate a large change in the direction of the PRGRF between
the baseline and intervention condition (5.7 7 2.9 cm vs. 6.57 4.1), but she also lowered the magnitude of the PRGRF by 28.7% from the baseline to the intervention
condition (6.684 BW7 1.062 vs. 4.766 70.891). Without any change in her knee angle between conditions, the change in the direction and magnitude of the PRGRF
resulted in a lower average posterior-directed (negative) PTSF by 36.0% from baseline to the intervention condition (1.687 BW7 0.594 vs. 1.0797 0.128). Subject 4
demonstrated a similar shift in the moment arm of the PRGRF (3.1 cm 7 5.4 vs. 3.07 7.1); however, the magnitude of the PRGRF increased for this subject from the
baseline condition to the intervention condition. Despite the increase in the magnitude of the PRGRF, PTSF still decreased for this subject by 22% (0.772 7 0.282 BW vs.
0.602 70.147).
as where those forces are directed relative to the knee joint
center. Additionally, any benefits from alterations in quadriceps
and hamstrings muscle strength and activation are highly
dependent on factors of jumping technique, such as knee angle
and foot strike position. While the current ACL injury prevention
programs include some landing mechanics instruction, there is
2664
C.A. Myers, D. Hawkins / Journal of Biomechanics 43 (2010) 2657–2664
Table 3
Mean jump stop performance values from the baseline condition and the
intervention conditions. There was a significant increase in vertical jump height.
Performance variable
Baseline
SD
Intervention
SD
Vertical jump height (cm)*
Approach velocity (m/s)
Time on plate (s)
23.4
3.42
0.299
7.0
0.46
0.090
25.9
3.33
0.331
6.2
0.47
0.112
*
Significant difference (Po 0.05) between the baseline and intervention condition,
while approach velocity and time on the plate were unaffected by the
intervention.
evidence to suggest that a greater emphasis on landing
mechanics, coupled with the benefits of increased muscle
strength and activation that have been demonstrated, can provide
these programs with a better chance of lowering ACL injury risk.
Conflict of interest statement
None of the authors have any financial or personal relationships
with other people or organizations that could inappropriately
influence the quality of the work presented in this manuscript.
Acknowledgments
The authors thank the athletes from the UC Davis, Davis High
School, Woodland High School, and Del Oro High School women’s
basketball teams who participated in this study.
References
Bell, A.L., Pedersen, D.R., Brand, R.A., 1990. A comparison of the accuracy of several
hip center location prediction methods. Journal of Biomechanics 23, 617–621.
Berns, G.S., Hull, M.L., Patterson, H.A., 1992. Strain in the anteromedial bundle of
the anterior cruciate ligament under combination loading. Journal of
Orthopaedic Research 10, 167–176.
Butler, D.L., Noyes, F.R., Grood, E.S., 1980. Ligamentous restraints to anteriorposterior drawer in the human knee. A biomechanical study. Journal of Bone
and Joint Surgery 62, 259–270.
Cabaud, H.E., 1983. Biomechanics of the anterior cruciate ligament. Clinical
Orthopaedics and Related Research 172, 26–31.
Chappell, J.D., Yu, B., Kirkendall, D.T., Garrett, W.E., 2002. A comparison of knee
kinematics between male and female recreational athletes in stop-jump tasks.
American Journal of Sports Medicine 30, 261–267.
Conn, J.M., Annest, J.L., Gilchrist, J., 2003. Sports and recreation related injury
episodes in the US population, 1997–99. Injury Prevention 9, 117–123.
Dempster, W.T., 1955. Space requirements of the seated operator, Aerospace
Medical Research Laboratory WADC Technical Report 55 159.
Escamilla, R.F., Fleisig, G.S., Zheng, N., Barrentine, S.W., Wilk, K.E., Andrews, J.R.,
1998. Biomechanics of the knee during closed kinetic chain and open kinetic
chain exercises. Medicine and Science in Sports and Exercise 30, 556–569.
Escamilla, R.F., Zheng, N., Imamura, R., Macleod, T.D., Edwards, W.B., Hreljac, A.,
Fleisig, G.S., Wilk, K.E., Moorman 3rd, C.T., Andrews, J.R., 2009. Cruciate
Ligament force during the wall squat and the one-leg squat. Medicine and
Science in Sports and Exercise 41, 408–417.
Fleming, B.C., Renstrom, P.A., Beynnon, B.D., Engstrom, B., Peura, G.D., Badger, G.J.,
Johnson, R.J., 2001. The effect of weightbearing and external loading on
anterior cruciate ligament strain. Journal of Biomechanics 34, 163–170.
Gilchrist, J., Mandelbaum, B.R., Melancon, H., Ryan, G.W., Silvers, H.J., Griffin, L.Y.,
Watanabe, D.S., Dick, R.W., Dvorak, J., 2008. A randomized controlled trial to
prevent noncontact anterior cruciate ligament injury in female collegiate
soccer players. American Journal of Sports Medicine 36, 1476–1483.
Gillquist, J., Messner, K., 1999. Anterior cruciate ligament reconstruction and the
long-term incidence of gonarthrosis. Sports Medicine 27, 143–156.
Gottlob, C.A., Baker Jr., C.L., Pellissier, J.M., Colvin, L., 1999. Cost effectiveness of
anterior cruciate ligament reconstruction in young adults. Clinical Orthopaedics and Related Research, 272–282.
Gottlob, C.A., Baker Jr., C.L., 2000. Anterior cruciate ligament reconstruction:
Socioeconomic issues and cost effectiveness. American Journal of Orthopaedics
29, 472–476.
Herzog, W., Read, L.J., 1993. Lines of action and moment arms of the major forcecarrying structures crossing the human knee joint. Journal of Anatomy 182,
213–230.
Hewett, T.E., Stroupe, A.L., Nance, T.A., Noyes, F.R., 1996. Plyometric training in
female athletes. Decreased impact forces and increased hamstring torques.
American Journal of Sports Medicine 24, 765–773.
Hewett, T.E., Lindenfeld, T.N., Riccobene, J.V., Noyes, F.R., 1999. The effect of
neuromuscular training on the incidence of knee injury in female athletes. A
prospective study. American Journal of Sports Medicine 27, 699–706.
Hewett, T.E., Myer, G.D., Ford, K.R., 2005. Reducing knee and anterior cruciate
ligament injuries among female athletes: a systematic review of neuromuscular training interventions. Journal of Knee Surgery 18, 82–88.
Hewett, T.E., Myer, G.D., Ford, K.R., 2006. Anterior cruciate ligament injuries in
female athletes: Part 1, mechanisms and risk factors. American Journal of
Sports Medicine 34, 299–311.
Hill, A.V., 1970. First and last experiments in muscle mechanics.. Cambridge
University Press, London.
Lephart, S.M., Abt, J.P., Ferris, C.M., Sell, T.C., Nagai, T., Myers, J.B., Irrgang, J.J., 2005.
Neuromuscular and biomechanical characteristic changes in high school
athletes: a plyometric versus basic resistance program. British Journal of
Sports Medicine 39, 932–938.
Lloyd, D.G., Besier, T.F., 2003. An EMG-driven musculoskeletal model to estimate
muscle forces and knee joint moments in vivo. Journal of Biomechanics 36,
765–776.
Lohmander, L.S., Englund, P.M., Dahl, L.L., Roos, E.M., 2007. The long-term
consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. American Journal of Sports Medicine 35, 1756–1769.
Malinzak, R.A., Colby, S.M., Kirkendall, D.T., Yu, B., Garrett, W.E., 2001. A
comparison of knee joint motion patterns between men and women in
selected athletic tasks. Clinical Biomechanics 16, 438–445.
Markolf, K.L., Burchfield, D.M., Shapiro, M.M., Shepard, M.F., Fineman, G.A.,
Slauterbeck, J.L., 1995. Combined knee loading states that generate
high anterior cruciate ligament forces. Journal of Orthopedic Research 13,
930–935.
McLean, S.G., Su, A., van den Bogert, A.J., 2003. Development and validation of a 3D model to predict knee joint loading during dynamic movement. Journal of
Biomechanical Engineering 125, 864–874.
Quatman, C.E., Hewett, T.E., 2009. The anterior cruciate ligament injury
controversy: is ’’valgus collapse’’ a sex-specific mechanism? British Journal
of Sports Medicine 43 328–335.
Shelburne, K.D., Davis, T.J., Klootwyk, T.E., 1998. The relationship between
intercondylar notch width of the femur and the incidence of anterior cruciate
ligament tears. A prospective study. American Journal of Sports Medicine 26,
402–408.
Sigward, S.M., Powers, C.M., 2007. Loading characteristics of females exhibiting
excessive valgus moments during cutting. Journal of Clinical Biomechanics 22,
827–833.
Winter, D., 1990. Biomechanics and motor control of human movement. John
Wiley and Sons, New York.
Yu, B., McClure, S.B., Onate, J.A., Gustiewicz, K.M., Kirkendall, D.T., Garrett, W.E.,
2005. Age and gender effects on lower extremity kinematics of youth soccer
players in a stop-jump task. American Journal of Sports Medicine 33, 1356–
1364.
Yu, B., Garrett, W.E., 2007. Mechanisms of non-contact acl injuries. British Journal
of Sports Medicine 41 (Suppl. 1), i47–51.
Zheng, N., Fleisig, G.S., Escamilla, R.F., Barrentine, S.W., 1998. An analytical model
of the knee for estimation of internal forces during exercise. Journal of
Biomechanics 31, 963–967.