Repeated intermittent stress exacerbates myocardial ischemia
advertisement

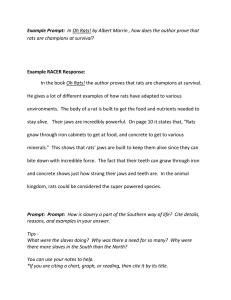
Repeated intermittent stress exacerbates myocardial ischemia-reperfusion injury DEBORAH A. SCHEUER AND STEVEN W. MIFFLIN Department of Pharmacology, The University of Texas Health Science Center, San Antonio, Texas 78284-7764 myocardial infarction; restraint stress; chronic stress; corticosterone; arrhythmia STRESS HAS BEEN IMPLICATED as a risk factor for increased morbidity and mortality due either to myocardial ischemia or to malignant arrhythmia in the absence of ischemia (8, 11, 12, 14, 15, 20). Correlative studies in humans have implicated acute episodes of stress associated with emotional upset or catastrophic events as triggers for myocardial ischemia (11) and cardiac arrhythmia (14). In experimental animals, it has been shown that acute stress decreases the fibrillation threshold of the myocardium (14) and increases the risk for cardiac arrhythmias associated with myocardial ischemia (21, 23). Controlled laboratory studies in humans have demonstrated that a single episode of mental stress can trigger myocardial ischemia, particularly in patients with existing coronary artery disease (11, 15). Also, patients exhibiting larger increases in arterial pressure and/or heart rate and more frequent episodes of myocardial ischemia in response to experimentally induced acute mental stress are reported to have more frequent episodes of myocardial ischemia in daily life (2, 12). This suggests that susceptibility to ischemia in response to acute mental stress is indicative of susceptibility to daily life ischemic episodes, which can lead to myocardial infarction or sudden R470 cardiac death. The evidence that chronic stress increases the risk of ischemic heart disease, including myocardial infarction, is not as substantial. Most of the evidence is from epidemiological studies that have linked chronic stressors such as social isolation, depression, and self-reported stress to increased morbidity and mortality from ischemic heart disease (8, 11, 20). Controlled studies to assess the impact of chronic stress on myocardial ischemia and infarction are lacking. Therefore, the following experiments were conducted to test the hypothesis that repeated exposure to stress increases the severity of infarction resulting from myocardial ischemia-reperfusion injury in rats. Many experimental protocols have been utilized to produce chronic stress in rats. In the present experiments, we chose to use repeated restraint stress. This is a stressor that is primarily psychological, evoking an escape reaction, although there is a component of physical stress resulting from the escape effort. In these experiments, the rats were exposed to a moderate stress of repeated intermittent restraint for 1–2 h daily for 8–14 days using two slightly different protocols, one with a moderate and one with a high degree of predictability. The two different protocols were utilized because it has been reported that the magnitude of stress produced by a stressor varies inversely with the degree of predictability of the stressor (16). Chronic stress has been shown to decrease thymus and increase adrenal weight (3). Therefore, to provide an index of the efficacy of the restraint protocol as a chronic stressor, thymus and adrenal weights were measured at the conclusion of the experiments. On the day after the final day of restraint stress, the animals were anesthetized and a myocardial ischemiareperfusion protocol was performed. Infarct size is a primary predictor of morbidity and mortality from myocardial infarction in humans (18). Therefore, in these experiments, infarct size, quantitated as a percentage of the area at risk, was used as the measure of severity of infarction. The incidence of life-threatening arrhythmic episodes during ischemia and/or reperfusion was also measured. METHODS General Methods Successful experiments were performed on 19 male Sprague-Dawley rats purchased from Charles River Laboratories (Wilmington, MA). Seven additional rats were excluded from the study. Four were excluded because at the end of the experiment, the area at risk was found to be insufficiently large (,18% of the left ventricle), and three were excluded because the surgical preparation was flawed. The rats were housed in quiet rooms with a 12:12-h light-dark cycle (7 AM to 0363-6119/98 $5.00 Copyright r 1998 the American Physiological Society Downloaded from http://ajpregu.physiology.org/ by 10.220.33.5 on September 30, 2016 Scheuer, Deborah A., and Steven W. Mifflin. Repeated intermittent stress exacerbates myocardial ischemia-reperfusion injury. Am. J. Physiol. 274 (Regulatory Integrative Comp. Physiol. 43): R470–R475, 1998.—Chronic stress in humans has been correlated with increased risk for ischemic heart disease. Thus experiments were conducted to determine if repeated intermittent restraint stress increased infarct size in a rat model of myocardial ischemia-reperfusion injury. Male Sprague-Dawley rats were subjected to no stress (control) or to daily restraint stress for 1–1.5 h for 8–14 days (stress protocol A) or for 2 h daily for 11 or 12 days (stress protocol B). Myocardial ischemia-reperfusion (30-min ischemia, 3-h reperfusion) was performed in anesthetized rats. Average baseline arterial pressures were 111 6 4, 120 6 10, and 125 6 7 mmHg in the control, stress protocol A, and stress protocol B groups, respectively. Infarct size (%area at risk) was significantly larger in both groups of stressed rats compared with control rats (58 6 5, 78 6 2, and 79 6 3% in the control, stress protocol A, and stress protocol B groups, respectively). During ischemia or early reperfusion, zero of eight control, two of six protocol A stress, and two of five protocol B stress rats had at least one period of severe arrhythmia. Therefore, these results provide experimental evidence corroborating correlative studies in humans that link chronic stress with increased morbidity and mortality from ischemic heart disease. REPEATED INTERMITTENT STRESS INCREASES INFARCT SIZE 7 PM) in a fully accredited (American Association for Accreditation of Laboratory Animal Care and United States Department of Agriculture) laboratory animal care facility at the University of Texas Health Science Center in San Antonio. Normal-sodium rat chow and water were available ad libitum. The experimental protocol was approved by the Institutional Animal Care and Use Committee. Repeated Restraint Stress Surgical Preparation On the day of the experiment, rats were anesthetized with the long-acting rodent anesthetic thiobarbital sodium (Inactin, Research Biomedicals) at an initial intraperitoneal dose of 110 mg/kg. Supplemental anesthetic was given in intraperitoneal doses of 10 mg/kg as required to maintain a plane of anesthesia in which there was an absence of withdrawal to pinch of the hindpaw and no evidence of fluctuations in blood pressure in response to surgical manipulation. Body temperature was maintained at 36–38°C with a ventral heating pad and, when required, a dorsal infrared lamp. The animal was intubated through a tracheotomy and ventilated with room air that was supplemented with 100% O2. Catheters constructed of PE-50 or microbore Tygon tubing (0.03 in. OD) were placed in a femoral artery and vein for withdrawal of blood samples and administration of drugs. The muscle relaxant pancuronium bromide (0.5 mg · kg21 · h21 ) was infused through the venous catheter throughout the experimental protocol. An additional catheter was introduced into the right carotid artery and advanced (,3.5–4.0 cm) to the root of the aorta for measurement of arterial pressure. The animals were prepared for the myocardial ischemia-reperfusion protocol as previously described (17). A left thoracotomy was made at the third or fourth intercostal space. The lungs were retracted, and the pericardium was teased open to expose the heart. To position a loose ligature around a branch of the left main coronary artery, a stitch was placed in the left ventricular myocardium, between the origin of the left atrial appendage and the sulcus marking the ventricular septum. Ties were placed around either side of the suture that passed through the myocardium. The ties were subsequently used to loosen the suture to allow for easy reperfusion of the myocardium. Experimental Protocol The experimental protocol was initiated 30 min after completion of the surgical procedures to allow for stabilization of hormonal and cardiovascular variables. The protocol was a total of 4 h long, consisting of a 30-min baseline period, a 30-min period of myocardial ischemia, and a 3-h period of reperfusion. To produce ischemia, the ligature around the coronary artery was tied tightly, and the ends of the suture were placed through a piece of tubing which was used to keep the ligature closed and to provide an additional means of occluding the vessel. At the end of the experiment, the coronary artery was reoccluded and the heart was perfused with Unisperse Blue dye (Ciba-Geigy, Newport, DE) through the left ventricular catheter. This procedure delineated the area at risk, which is defined as the portion of the myocardium perfused by the occluded vessel. The animal was then killed with an overdose of pentobarbital sodium (100 mg/kg iv), and the heart was quickly removed. Chronic stress can decrease thymus weight and increase adrenal weight (3). Therefore, the adrenal and thymus glands were also removed, and their weights were used as indexes of the physiological efficacy of the repeated restraint stress protocol. The adrenals were not weighed in one control and one stress protocol A rat, and the thymus was not weighed in two control rats and one stress protocol A rat. Experimental groups. Experiments were performed in three groups of rats. Group 1 consisted of unstressed, control rats (n 5 8). Group 2 consisted of the rats subjected to the shorter but less predictable restraint protocol (stress protocol A, n 5 6), whereas group 3 consisted of rats subjected to the invariant 2-h stress protocol (stress protocol B, n 5 5). Rats in group 1 were housed separately from those in groups 2 and 3 to minimize disturbance of the control rats. The control rats were not handled every day but were subject to the normal handling associated with usual animal care. Normal care includes, but is not limited to, a complete cage change at least twice a week and a change of water bottles three times a week. The daily handling of the stressed rats required to place them in and remove them from the restraint devices was therefore considered to be part of the repeated-stress protocol. Cardiovascular data. Arterial pressure was measured from the carotid arterial catheter using a pressure transducer (Cobe Cardiovascular, Arvada, CO) and a transducer coupler (Coulbourn Instruments, Allentown, PA). Mean arterial pressure (MAP) and heart rate were determined from pulsatile pressure using a Coulbourn blood pressure processor. Cardiovascular data were collected using MacLab (ADInstruments, Castle Hill, Australia) or Cambridge Electronic Design (Cambridge, UK) analog-to-digital converters connected to Macintosh or IBM clone computers. Heart rate values were unavailable for one control rat. Measurement of infarct and risk areas. After the heart was excised from the animal, the left ventricle was sliced into four to five transverse slices 2- to 3-mm thick and stained with 1% triphenyl tetrazolium chloride (TTC). TTC stains viable tissue red, and the necrotic portions of the myocardium become white (22). Both sides of each slice were imaged (Optimus, BioScan, Edmonds, WA) to determine the total area, area at risk, and area of infarct for each slice. Each slice was then weighed. The total area, area at risk, and area of infarct were calculated for the entire left ventricle based on the areas and weight determined for each slice. The total area at risk was quantitated as a percentage of the left ventricle, and the area of infarct was quantitated as a percentage of the area at risk. On the basis of previous experience, we set 18% as the minimum acceptable area at risk, because with an area at risk smaller than this, there is frequently little or no infarct in control rats (17). Plasma corticosterone concentration. In some experiments, arterial blood samples (<100 µl) for the measurement of plasma corticosterone concentration were obtained during the baseline period, at the end of the ischemia period, and 1 and 3 h after the initiation of reperfusion. All blood samples were placed in EDTA-coated microcentrifuge tubes and centrifuged at 4°C. The plasma was removed and kept frozen until analysis. The plasma corticosterone concentration in each Downloaded from http://ajpregu.physiology.org/ by 10.220.33.5 on September 30, 2016 To produce chronic intermittent stress, rats were restrained in rodent restraining devices (Fisher Scientific, Fair Lawn, NJ). The restraint period was usually started within 2 h of lights on, when plasma corticosterone is at the nadir of its diurnal rhythm and the corticosterone response to stress is most robust (3). Occasionally the restraint was initiated later, but always before 11 AM. Two protocols were used. In stress protocol A, rats were subjected to restraint stress for a randomly varying duration of 1–1.5 h for 8–14 consecutive days (averaging 12 6 1 days). In stress protocol B, rats were always restrained for exactly 2 h for 11 or 12 consecutive days. Rats were not subjected to restraint stress on the morning of the experiment. R471 R472 REPEATED INTERMITTENT STRESS INCREASES INFARCT SIZE sample was determined in duplicate or triplicate by radioimmunoassay using a commercially available kit (ImmuChem double antibody B 125I radioimmunoassay kit; ICN Pharmaceuticals, Costa Mesa, CA). Interassay and intra-assay coefficients of variation are ,11% for all sample pools. Crossreactivity of the antiserum at 50% displacement of corticosterone is #0.05% for aldosterone, progesterone, and cortisol. Data Analysis RESULTS Experiments were performed 9–15 days after initiation of the daily restraint stress and in control rats. On the day of the ischemia-reperfusion experiment, rats that had been subjected to stress protocol B weighed less (369 6 6 g, P , 0.05) than rats subjected to stress protocol A (426 6 11 g) or control rats (420 6 15 g). Chronic stress has been shown to decrease thymus weight and increase adrenal weight (3). In the present studies, thymus weight, measured as grams of thymus weight per kilogram of body weight, was significantly reduced in both groups of stressed rats compared with control rats, indicating that the protocols used were effective in producing chronic stress (Fig. 1). However, adrenal weights were not different among the groups (Fig. 1). Figure 2 shows the average MAP for each experimental time period (baseline, ischemia, and reperfusion) for all three groups of rats. Although there was a tendency for stress to increase baseline MAP, the differences among the groups were not significant. Average baseline arterial pressures were 111 6 4, 120 6 10, and Fig. 1. Average thymus (A) and adrenal (B) weights in control rats and rats subjected to stress protocols A and B. Weights are expressed as mg tissue/kg body wt. Thymus weights were significantly decreased by both stress protocols. * P , 0.05 relative to control group. Downloaded from http://ajpregu.physiology.org/ by 10.220.33.5 on September 30, 2016 Data were analyzed using MacLab (ADInstruments), Spike2 (Cambridge Electronic Design), and SuperANOVA (Abacus Concepts, Berkeley, CA) software. Continuous measurements of arterial pressure and heart rate were averaged over each experimental time period (30 min of control, 30 min of ischemia, and 3 h of reperfusion) and were analyzed using analysis of variance (ANOVA). Additional analyses were performed on these data averaged into 2-min bins. Area at risk as a percentage of the left ventricle and area of infarct as a percentage of area at risk were analyzed by ANOVA after arcsin transformation. Body weight, adrenal and thymus weights (mg/kg body wt), and plasma corticosterone concentrations were also analyzed by ANOVA. Average values are reported as means 6 SE. Post hoc analyses were performed using Fisher’s protected least-significant differences test. Results were considered significant at P # 0.05. 125 6 7 mmHg in the control, stress protocol A, and stress protocol B groups, respectively. In control rats, there was no significant change in arterial pressure during ischemia or reperfusion. In contrast, arterial pressure fell significantly during reperfusion in the both the stress protocol A and B groups. As with MAP, baseline heart rate was not different among the experimental groups (Fig. 3A). Analyzed by two-way ANOVA, heart rate increased significantly during ischemia, with no significant difference between groups. To better illustrate the effect of ischemia on heart rate, the time course of the increase in heart rate in response to ischemia in the individual experimental groups is illustrated in Fig. 3B. Analyzed by one-way repeatedmeasures ANOVA, heart rate was significantly elevated above baseline throughout the first 10 min of ischemia (t 5 2 through t 5 10 min) in the stress protocol B group, and at t 5 4, 6, and 10 min in the control group. By this method of analysis, there were no significant increases in heart rate in the stress protocol A group. All the increases in heart rate in response to ischemia were transient, and heart rate returned to baseline by the end of the 30-min period of ischemia. Plasma corticosterone was measured in four control and five stress protocol B rats. Baseline plasma corticosterone concentration was not significantly different in these two groups of rats, averaging 52 6 6 and 44 6 2 µg/dl in control (n 5 4) and stress protocol B rats (n 5 5), respectively. In response to ischemia and reperfusion, plasma corticosterone concentration tended to increase in the stressed rats and decrease in the control rats (Fig. 4). Although the changes in corticosterone from baseline were not significant for either group of animals, plasma corticosterone increased significantly during ischemia-reperfusion in the stressed rats relative to the control rats. Area at risk was defined as the %left ventricle perfused by the occluded artery. Area at risk, which was dependent on the exact placement of the ligature and the anatomy of the coronary arteries in each rat, was not different among the groups (Fig. 5A). In all experiments, the area at risk was largely or completely in the anterior portion of the left ventricular myocardium. Area of infarct was defined as the percentage of the area at risk that was no longer viable, as indicated by the TTC staining of the myocardium at the conclusion of the experiment. Rats from both chronic intermittent REPEATED INTERMITTENT STRESS INCREASES INFARCT SIZE weights were used to indicate the efficacy of the stress protocol (3). Thymus weight was significantly reduced in both groups of stressed rats, indicating that both stress protocols successfully actualized chronic stress. Chronic stress did not increase adrenal weight in these experiments, suggesting that the magnitude of stress produced by these protocols was not severe. In some studies, chronic stress has also been reported to increase baseline MAP (7) and increase the glucocorticoid response to a novel stressor (3). In the present experiments there was a tendency for baseline arterial pressure to be increased in the chronically stressed rats, although the increase was not statistically significant. This is in agreement with other studies reporting that mild or moderate chronic stress is not sufficient to produce hypertension in normal laboratory animals (6). In the present experiments, the corticosterone response to ischemia-reperfusion was measured in some of the rats. Although the changes in corticosterone from baseline were not significant for either group of animals, plasma corticosterone increased significantly during stress protocols had significantly larger areas of infarct than did the control rats (Fig. 5B). Average areas of infarction were 58 6 5, 78 6 2, and 79 6 3% in the control, stress protocol A, and stress protocol B groups, respectively. During ischemia or early reperfusion, two of six rats in the protocol A stress group and two of five rats in the protocol B stress group had at least one period of severe arrhythmia accompanied by severe hypotension (MAP #40 mmHg). Normal sinus rhythm and arterial pressure were reestablished by gently tapping or stroking the heart with a cotton swab. No similar episodes of severe arrhythmia requiring intervention were observed in the control rats. One rat in the protocol A stress group was killed 25 min early due to an additional episode of arrhythmia that produced intractable hypotension. DISCUSSION There are many clinical reports that suggest that exposure to excessive stress correlates with increased morbidity and mortality from cardiovascular diseases, including myocardial ischemia (8, 11, 12, 14, 15, 20). The primary finding of this study is that daily exposure of rats to 8–14 days of 1–2 h of restraint stress increased the size of infarction resulting from ischemiareperfusion injury. Because the animals were not restrained on the day of the experiment, the increased infarct size was not due to an acute episode of stress experienced just before ischemia-reperfusion. Patients with myocardial ischemia can suffer fatal arrhythmias, a cause of mortality termed ‘‘sudden cardiac death’’ (11). In the present study, it was observed that rats subjected to the repeated stress had a higher incidence of potentially fatal arrythmias. Therefore, the results from this study suggest that repeated exposure to stress influences the outcome of an episode of myocardial ischemia both by increasing infarct size and by increasing the incidence of fatal arrhythmia. Repeated restraint was used to produce chronic stress in the present studies, and adrenal and thymus Fig. 3. A: average heart rate [beats/min (bpm)] during the baseline (solid bars), ischemia (crosshatched bars), and reperfusion (hatched bars) experimental periods. Data are shown for rats in control, stress protocol A, and stress protocol B groups. * P , 0.05 relative to baseline period analyzed by 2-factor analysis of variance. B: detailed illustration of average heart rate during 30-min period of ischemia and first 30 min of reperfusion. Data are shown for control (solid line), stress protocol A (dotted line), and stress protocol B (dashed line). * P , 0.05 relative to baseline value for that group. Heart rate increased significantly at time 5 2, 4, 6, 8, and 10 min of ischemia in the stress protocol B group and at 4, 6, and 10 min in the control group. Increase in heart rate during ischemia in stress protocol A group was not statistically significant. However, there was no statistical difference in values for heart rate among the 3 experimental groups. Downloaded from http://ajpregu.physiology.org/ by 10.220.33.5 on September 30, 2016 Fig. 2. Average mean arterial pressure during the baseline (solid bars), ischemia (crosshatched bars), and reperfusion (hatched bars) experimental periods. Data are shown for rats in control, stress protocol A, and stress protocol B groups. * P , 0.05 relative to baseline period; ** P , 0.05 relative to baseline and ischemia periods. Thus in the stress protocol A group, pressure decreased significantly from baseline during reperfusion. In the stress protocol B group, pressure during reperfusion was decreased significantly relative to both baseline and ischemia periods. R473 R474 REPEATED INTERMITTENT STRESS INCREASES INFARCT SIZE ischemia-reperfusion in the stressed rats relative to the control rats. The corticosterone response in the stressed rats could have been due directly to the chronic stress or due to the greater myocardial damage in the stressed rats. All the results, taken together, indicate that the repeated intermittent stress protocols used in this study produced only a moderate degree of chronic stress. It has been reported that the magnitude of stress produced by a stressor varies inversely with the degree Fig. 5. Average area at risk [as %left ventricle (LV); A] and average infarct (as %area at risk; B). Data are shown for rats in control, stress protocol A, and stress protocol B groups. * P , 0.05 relative to control group. Infarct size was significantly increased in both groups of stressed rats. Downloaded from http://ajpregu.physiology.org/ by 10.220.33.5 on September 30, 2016 Fig. 4. Average change in plasma corticosterone (Cort) from baseline period at end of 30 min of ischemia and after 1 and 3 h of reperfusion in 4 control rats (j) and 5 stress protocol B rats (r). * Corticosterone responses to ischemia and reperfusion were significantly different between the 2 groups of rats (P , 0.05). of predictability of the stressor (16). Two slightly different stress protocols were used. Stress protocol A was of shorter but less predictable duration (varying randomly between 1 and 1.5 h), whereas stress protocol B was longer in duration but highly predictable (always 2 h). The first group of rats was stressed for a somewhat unpredictable length of time to minimize desensitization due to the predictability of the stress. The second group of rats was stressed for exactly 2 h so that the protocol was completely reproducible from day to day and rat to rat. We thought it possible that without the element of unpredictability the restraint stress might not be sufficient to increase infarct size, and we wanted to investigate this possibility. Subtle differences between these two groups of rats were observed in the cardiovascular responses to myocardial ischemia. During ischemia, the stress protocol B group responded with a significant increase in heart rate (Fig. 3B), whereas the stress protocol A group did not. During reperfusion, the MAP fell significantly relative to baseline in the stress protocol A group. In the stress protocol B group, the reduction in MAP during reperfusion was significant relative to both the baseline and the ischemia periods. On the day of the ischemia experiment, body weight was significantly reduced in the protocol B stressed rats relative to the control and protocol A stressed rats. However, body weight changes over the course of the repeated stress and control protocols were not determined. Although the rats were purchased to be within the same weight range, the differences in body weight on the day of the experiment should not be used as conclusive evidence regarding the severity of the stress. On the basis of the cardiovascular data, infarct size, and incidence of arrhythmia, there were no obvious differences in the two stress paradigms. Numerous mechanisms could contribute to the effect of repeated intermittent stress to increase infarct size. These mechanisms can be divided into two categories. First, chronic restraint stress could produce anatomical or physiological changes which predispose the myocardium to increased damage during episodes of ischemiareperfusion. For example, stress alone has been shown to produce small areas of myocardial necrosis (14). The elevations in corticosterone that accompany chronic stress could also contribute to the increased myocardial necrosis observed in the stressed rats (17). Second, the repeated restraint stress could alter the physiological response to the novel acute stress of myocardial ischemia. Stress evokes a number of responses that could impact the development of ischemia-reperfusion injury. Some of these responses are protective, such as stimulation of antioxidant mechanisms and increasing the number of adenosine receptors (14). Detrimental responses include activation of the sympathetic nervous system (5, 10), increases in angiotensin (5, 19), and increases in platelet aggregation and blood viscosity (11). For example, abundant evidence implicates increases in sympathetic nerve activity in the pathogenesis of myocardial ischemia and cardiac arrhythmia (5, 13). Elevations in sympathetic nerve activity can increase myocardial oxygen demand and decrease oxygen supply and can decrease the electrical threshold for REPEATED INTERMITTENT STRESS INCREASES INFARCT SIZE 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Perspectives The results presented here reinforce the concept that moderate increases in daily life stress, even when predictable, can increase the risk of morbidity and mortality from ischemic heart disease. Although clinical studies have demonstrated that stress-reduction programs are a valuable addition to postinfarction therapy in humans (15), stress reduction is not routinely incorporated into patient therapy. Studies like the present one could bolster the case for inclusion of such stress-reduction programs. Additionally, future elucidation of the mechanisms involved in stressinduced exacerbation of myocardial injury could indicate effective avenues for preventative pharmaceutical therapies. The authors thank Melissa Vitela, Myrna Herrera-Rosales, and Andrew Suhrbier for excellent technical assistance. This work was supported by the Texas Affiliate of the American Heart Association and National Heart, Lung, and Blood Institute Grant HL-41894. Address for reprint requests: D. A. Scheuer, Dept. of Pharmacology, The University of Texas Health Science Center, 7703 Floyd Curl Drive, San Antonio, TX 78284-7764. 13. 14. 15. 16. 17. 18. 19. 20. 21. Received 25 June 1997; accepted in final form 6 November 1997. REFERENCES 1. Armario, A., A. Lopez-Calderon, T. Jolin, and J. Balasch. Response of anterior pituitary hormones to chronic stress. The specificity of adaptation. Neurosci. Behav. Physiol. 10: 245–250, 1986. 2. Blumenthal, J. A., W. Jiang, R. A. Waugh, D. J. Frid, J. J. Morris, E. Coleman, M. Hanson, M. Babyak, E. T. Thyrum, 22. 23. D. S. Krantz, and C. O’Conner. Mental stress-induced ischemia in the laboratory and ambulatory ischemia during daily life. Association and hemodynamic features. Circulation 92: 2102– 2108, 1995. Dallman, M. F., S. F. Akana, K. A. Scribner, M. J. Bradbury, C.-D. Walker, and A. M. Strack. Stress, feedback and facilitation in the hypothalamo-pituitary-adrenal axis. J. Neuroendocrinol. 4: 517–526, 1992. Drolet, G., and J. A. Mansi. Chronic stress induces sensitization in the sympathoadrenal responses to stress in borderline hypertensive rats. Am. J. Physiol. 272 (Regulatory Integrative Comp. Physiol. 41): R813–R820, 1997. Goldstein, D. S. Stress, Catecholamines, and Cardiovascular Diseases. New York: Oxford Univ. Press, 1995, p. 287–392. Harrap, S. B., W. J. Louis, and A. E. Doyle. Failure of psychosocial stress to induce chronic hypertension in the rat. J. Hypertens. 2: 653–662, 1984. Henry, J. P., Y.-Y. Liu, W. E. Nadra, C.-G. Qian, P. Mormede, V. Lemaire, D. Ely, and E. D. Hendley. Psychosocial stress can induce chronic hypertension in normotensive strains of rats. Hypertension 21: 714–723, 1993. Ketterer, M. W. Secondary prevention of ischemic heart disease. The case for aggresive behavior monitoring and intervention. Psychosomatics 34: 478–484, 1993. Kiss, A., and G. Aguilera. Regulation of the hypothalamic pituitary adrenal axis during chronic stress: responses to repeated intraperitoneal hypertonic saline injection. Brain Res. 630: 262–270, 1993. Konarska, M., R. E. Stewart, and R. McCarty. Habituation of sympathetic-adrenal medullary responses following exposure to chronic intermittent stress. Physiol. Behav. 45: 255–261, 1989. Krantz, D. S., W. J. Kop, H. T. Santiago, and J. S. Gottdiener. Mental stress as a trigger of myocardial ischemia and infarction. Cardiol. Clin. 14: 271–287, 1996. Krittayaphong, R., K. C. Light, P. L. Biles, M. N. Ballenger, and D. S. Sheps. Increased heart rate response to laboratoryinduced mental stress predicts frequency and duration of daily life ambulatory myocardial ischemia in patients with coronary artery disease. Am. J. Cardiol. 76: 657–660, 1995. Malliani, A., P. J. Schwartz, and A. Zanchetti. Neural mechanisms in life-threatening arrythmias. Am. Heart J. 100: 705–715, 1980. Meerson, F. Z. Stress-induced arrhythmic disease of the heart— Part 1. Clin. Cardiol. 17: 362–371, 1994. Merz, C. N. B., D. S. Krantz, and A. Rozanski. Mental stress and myocardial ischemia. Tex. Heart Inst. J. 20: 152–157, 1993. Quirce, C. M., M. Odio, and J. M. Solano. The effects of predictable and unpredictable schedules of physical restraint upon rats. Life Sci. 28: 1897–1902, 1981. Scheuer, D. A., and S. W. Mifflin. Chronic corticosterone treatment increases myocardial infarct size in rats with ischemiareperfusion injury. Am. J. Physiol. 272 (Regulatory Integrative Comp. Physiol. 41): R2017–R2024, 1997. Sobel, B. E., G. F. Bresnahan, W. E. Shell, and R. D. Yoder. Estimation of infarct size in man and its relation to prognosis. Circulation 46: 640–648, 1972. Tan, L. B., J. E. Jalil, R. Pick, J. S. Janicki, and K. T. Weber. Cardiac myocyte necrosis induced by angiotensin II. Circ. Res. 69: 1185–1195, 1991. Tennant, C. C., K. J. Palmer, P. M. Langeluddecke, M. P. Jones, and G. Nelson. Life event stress and myocardial reinfarction: a prospective study. Eur. Heart J. 15: 472–478, 1994. Verrier, R. L., and J. A. Kovach. Autonomic nervous system: primary role of beta-adrenergic receptors in arrhythmogenesis during sympathetic nervous system activation. In: Cardiac Arrythmia. Mechanisms, Diagnosis and Management, edited by P. J. Podrid and P. R. Kowey. Baltimore, MD: Williams and Wilkins, 1995, p. 151–168. Vivaldi, M. T., R. A. Kloner, and F. J. Schoen. Triphenyltetrazolium staining of irreversible ischemic injury following coronary artery occlusion in rats. Am. J. Pathol. 121: 522–530, 1985. Wolf, S. Forebrain involvement in fatal cardiac arrhythmia. Integr. Physiol. Behav. Sci. 30: 215–225, 1995. Downloaded from http://ajpregu.physiology.org/ by 10.220.33.5 on September 30, 2016 arrhythmias (11, 14). Adaptation to repeated stress has been demonstrated for some responses to acute stress, such as the stimulation of the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis (1, 10). However, this adaptation is stressor specific, and chronic stress has been reported to facilitate some responses to acute stress, particularly if the stressor is novel (3, 4, 9). Therefore, chronic stress could potentiate the increases in sympathetic nervous system activity, angiotensin, or other detrimental factors that are activated during myocardial ischemia-reperfusion. Clearly, a number of experiments will be required to sort out the mechanism of the stress-induced exacerbation of myocardial ischemia-reperfusion injury. In summary, the results from this study demonstrate that 1–2 h of daily restraint stress for 8–14 days increased the size of the infarction resulting from ischemia-reperfusion injury. The repeated exposure to stress before ischemia-reperfusion also increased the incidence of severe arrhythmia. The degree of stress produced by the intermittent restraint stress protocol can be classified as moderate, because thymus weight was decreased but adrenal weights and baseline arterial pressure were not increased by the stress protocols. Even when the stressor was highly predictable, infarct size and arrhythmia incidence were increased. Therefore, these results provide experimental evidence corroborating correlative studies in humans that link chronic stress with increased morbidity and mortality from ischemic heart disease. R475