Comparison of Specific Femoral Short Stems and Conventional
advertisement

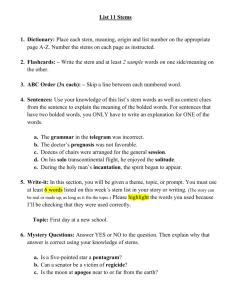
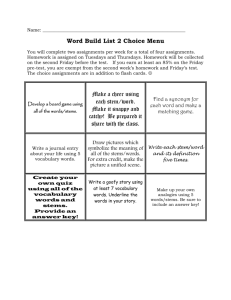
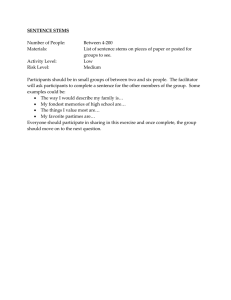
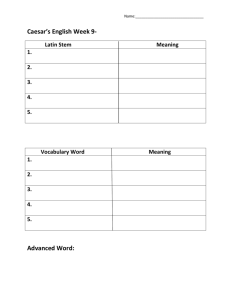
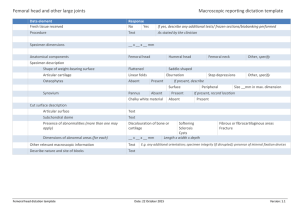
n Feature Article Comparison of Specific Femoral Short Stems and Conventional-Length Stems in Primary Cementless Total Hip Arthroplasty Young-Soo Shin, MD; Dong-Hun Suh, MD; Jong-Hoon Park, MD; Jeong-Lae Kim, MD; Seung-Beom Han, MD abstract There are several reported disadvantages with conventional-length femoral stems in cementless total hip arthroplasty (THA). Therefore, various efforts have been made to develop a specific femoral short stem to improve physiologic bone remodeling at the femoral aspect of a cementless THA. However, there are potential disadvantages with specific femoral short stems, such as malalignment, inadvertent subsidence, and potential proximal femoral fracture. Therefore, the authors quantitatively compared radiographic and clinical outcomes as well as component-specific complications between 2 groups of patients following primary cementless THA. A matched comparison was made between specific femoral short stems (n=50) and conventional-length femoral stems (n=50) in cementless THA procedures performed between January 2008 and January 2012. Patients were matched for age, sex, body mass index, height, surgical approach, and surgeon. No significant differences were found between the 2 groups in mean postoperative radiographic outcomes, functional outcomes, or complications. Both groups showed satisfactory performance at 5-year follow-up. Specific femoral short stems resulted in a higher incidence of malalignment and subsidence and a lower incidence of thigh pain and proximal bone resorption compared with conventional-length femoral stems. Although longer follow-up is required, specific femoral short stems may have clinical and radiographic advantages with equivalent perioperative complications relative to conventional-length femoral stems. However, this technique requires proper patient selection in combination with careful preoperative planning and meticulous surgical technique. [Orthopedics. 2016; 39(2):e311-e317.] O ver the past several decades, conventional femoral fixation with tapered stems has been used in cementless total hip arthroplasty (THA) MARCH/APRIL 2016 | Volume 39 • Number 2 in an effort to provide reliable long-term fixation in patients with functional improvement. Recent studies showed overall survivorship of greater than 94% for sev- eral conventional-length tapered femoral components at 20-year follow-up.1-3 However, conventional-length femoral stems in cementless THA have several reported disadvantages, including challenges with proximal-distal femoral mismatch, preservation of the osseous femoral neck, and optimal proximal load transfer.4,5 There has been a recent surge of interest in the use of shorter stems for younger, more active patients undergoing cementless THA. Pain relief, improved function, and the radiographic stability of short stems of various designs were shown with followup of 2 to 8 years.6,7 Various efforts have been made to develop a femoral neck-preserving short stem to improve physiologic bone remodeling at the femoral aspect of a cementless THA. In addition, femoral neck-preserving short stems have several proposed advantages, including their inThe authors are from the Veterans Health Service Medical Center (Y-SS), Korea University Ansan Hospital (D-HS), and Korea University Anam Hospital (J-HP, J-LK, S-BH), Seoul, South Korea. The authors have no relevant financial relationships to disclose. Correspondence should be addressed to: Seung-Beom Han, MD, Korea University Anam Hospital, Anamdong 5 ga, Seoul, South Korea (oshan@korea.ac.kr). Received: April 6, 2015; Accepted: September 1, 2015. doi: 10.3928/01477447-20160222-04 e311 n Feature Article clinical outcomes as well as componentspecific complications in 2 groups of patients after primary cementless THA. It was hypothesized that the results with the specific femoral short stems would be at least equivalent to those with the currently available conventional-length femoral stems. Materials and Methods Figure 1: Photograph of the specific femoral short stem prosthesis (METHA, Aesculap, Tuttlingen, Germany) analyzed in the current study. herent bone-preserving nature wherein a more oval-shaped stem is fixed to the proximal femur. This allows more rotational stability and prevents distal migration, and the absence of the distal portion of the stem helps to avoid stress shielding and thigh pain.8-12 However, femoral neck-preserving short stems also have potential disadvantages. First, they tend to have a higher incidence of malalignment; therefore, they have been associated with poor functional outcomes and survivorship.12 Second, incorrect stem sizing may cause inadvertent subsidence; therefore, precise stem sizing of short stems is difficult compared with conventional stems.13 Third, there are concerns about potential proximal femoral fracture.12 To the best of the authors’ knowledge, no studies have simultaneously compared specific femoral short stems with conventionallength femoral stems in patients undergoing primary cementless THA. This study quantitatively compared radiographic and e312 Patient Selection and Study Design Starting in January 2008, THA with BiCONTACT (Aesculap, Tuttlingen, Germany) was performed predominantly at the study institution, along with METHA (Aesculap). During the study period, the stem type was selected by the surgeon in a nonsystematic manner, with the typical process of trial and implementation. The 2 stems were compared in patients who had 5 years of follow-up. The authors were aware that the BiCONTACT stem had good longterm results compared with other contemporary femoral stems.14 A total of 237 THA procedures were performed at the study institution between January 2008 and January 2012. The current study included patients with indications for primary THA. The use of specific femoral short stems was begun at the institution in June 2008. Exclusion criteria for METHA treatment were radiographically noticeable osteoporosis with T-score of less than 2.5 and dysplastic hips with abnormal deviation of the femoral neck or metaphyseal deformity secondary to fracture that would exclude insertion of the specific model of short stem that was used. Simple radiographs, dual-energy x-ray absorptiometry, and intraoperative bone stock findings were used to assess bone quality because inadequate bone structure may lead to poor fixation, even in patients with good bone quality. The authors evaluated 54 consecutive THA procedures performed with specific femoral short stems between June 2008 and January 2012. Four patients declined to participate in follow-up for reasons unrelated to the THA. After these patients were excluded, 50 patients who had specific femo- ral short stems were included in the current study, with a minimum 5-year follow-up. These patients underwent THA with specific femoral short stems (METHA) with a modular acetabular component consisting of a hemispherical titanium cup (PLASMACUP SC; Aesculap) with an outer coating of plasma-sprayed pure titanium (Plasmapore; Aesculap) and a 36mm delta ceramic femoral head and liner. This stem was composed of monoblock with 120°, 130°, and 135° head-neck-shaft angles and had a proximal rough titanium, plasma-sprayed, microporous coating with a thin 20-μm layer of pure calcium phosphate (Figure 1). Digital templating is considered an essential step before METHA implantation and is commonly used to determine the head-neck-shaft angle preoperatively and to ensure the femoral resection level and the anatomy of the femoral neck intraoperatively. Patients receiving the short stem THA were classified as group A and were reviewed in a case-matched analysis with 133 consecutive THA procedures performed with conventional-length femoral stems (BiCONTACT; Aesculap). In these patients, THA was performed with conventional-length femoral stems (BiCONTACT) with a modular acetabular component consisting of a hemispheric titanium cup (PLASMACUP SC) with an outer coating of plasma-sprayed pure titanium (Plasmapore) and a 36-mm delta ceramic femoral head and liner. This is a straight, collarless stem made of titanium alloy with plasma spray (pore size, 50-200 μm). Patients who underwent THA with the conventional-length stem were classified as group B. For every patient who was treated with a specific femoral short stem, a matched patient who was treated with a conventional-length stem was identified from the database by age (±5 years), sex, body mass index (±2 kg/m2), height (±5 cm), surgical approach, and surgeon in a 1:1 ratio. Matching in a 1:2 ratio was not possible because of the limited sample size. All procedures were performed by a single surgeon (S.-B.H.) using a postero- Copyright © SLACK Incorporated n Feature Article lateral surgical approach. All patients were administered prophylactic antibiotics perioperatively to prevent postoperative infection. This study was approved by the ethics committee at the study institution, and informed consent was obtained from all patients. Clinical Evaluation A simple questionnaire was completed, and clinical outcomes were determined using the Harris Hip Score (HHS) and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score at each visit. Data were recorded preoperatively and at 6 weeks, 6 months, 1 year, and annually thereafter. Preoperative demographic and clinical data for the 2 groups were evaluated (Table 1). Preoperative HHS and WOMAC score were not significantly different between the 2 groups. Radiographic Evaluation Each patient had regular evaluation preoperatively and at 6 weeks, 6 months, 1 year, and annually thereafter by analyzing radiographic outcomes for implant alignment and stability as assessed by 2 independent radiographic reviewers. The patients were placed in the supine position, with the affected leg in 20° internal rotation. The foot was fixed by an assistant to inhibit measurement errors. Stem position was defined as angulation along the stem relative to the femoral shaft. Varus or valgus positioning (>5° from neutral) was measured. Subsidence was analyzed by measuring the change in distance from the superior tip of the greater trochanter to the distal tip of the implant and was defined as greater than 2 mm.15,16 Radiographic findings in the femur were evaluated in the conventional 7 zones for bony ingrowth or resorption, including proximal bone resorption, defined as loss of trabecular bone density or loss of definition between the cortical and cancellous bone, blending into a uniform density; endosteal spot welds, defined as local deposition of new MARCH/APRIL 2016 | Volume 39 • Number 2 Table 1 Preoperative Demographic and Functional Data Variable Group A (n=50) Sex, M/F, No. Group B (n=50) P 35/15 32/18 .211 48.45 (30-68) 49.91 (40-67) .472 Body mass index, mean (range), kg/m2 23.4 (19.5-34.2) 23.8 (18.4-38.1) .337 Height, mean (range), m 1.73 (1.53-1.82) 1.71 (1.50-1.79) .281 56.5 (36-77) 59.5 (36-83) .255 Neck 0.785 (0.542-0.935) 0.711 (0.527-0.910) .207 Trochanter 0.732 (0.530-0.851) 0.776 (0.541-0.816) .809 Intertrochanter 1.210 (0.883-1.336) 1.058 (0.776-1.280) .439 Ward’s triangle 0.635 (0.437-0.912) 0.666 (0.432-0.953) .664 Total 0.999 (0.607-1.108) 0.974 (0.684-1.211) Age, mean (range), y Follow-up, mean (range), mo Bone mineral density, mean (range), g/cm2 Diagnosis, No. (%) .373 >.999 Osteoarthritis 5 (10) 8 (16) Avascular necrosis 39 (77) 36 (71) 6 (13) 6 (13) Harris Hip Score, mean±SD (range) Septic hip sequelae 55.0±10.4 (29-76) 53.0±8.4 (25-75) .316 Western Ontario and McMaster Universities Arthritis Index, mean±SD (range) 53.0±14.6 (40-64) 49.5±12.3 (32-78) .359 Abbreviations: F, female; M, male. bony trabeculae bridging the cortex and the implant surface; and cortical hypertrophy, defined as new bone of cortical density that resulted in an increase in cortical thickness.17 Additionally, heterotopic ossification was observed and classified according to the Brooker grading system.18 Component-specific complications, such as subsidence, fracture, and malalignment, were evaluated. Statistical Analysis Statistical analysis was performed with SPSS statistical software, version 20 (IBM Corp, Armonk, New York). P<.05 was considered statistically significant. The HHS, WOMAC score, and radiographic data in the 2 groups at final follow-up were compared with an independent samples t test for continuous vari- ables. Chi-square (Fisher’s exact) test was used for categorical variables to determine whether the incidence of complications and sex were different in the 2 groups. Results Clinical Outcomes In group A, mean preoperative HHS and WOMAC score of 55.0 and 53.0, respectively, improved to mean postoperative values of 98.6 and 3.3, respectively, at an average follow-up of 37.2 months. Therefore, HHS and WOMAC score improved by 43.6 and 49.7 points, respectively, in group A. In group B, mean preoperative HHS and WOMAC score of 53.0 and 49.5, respectively, improved to mean postoperative values of 97.8 and 4.4, respectively, at an average follow-up of 35.3 months. Therefore, in group B, HHS e313 n Feature Article Table 2 Valgus Position of Implants (Group A) Mean±SD (Range) Variable Patients in Valgus Position (n=2) Patients in Neutral Position (n=48) Pa Preoperative Harris Hip Score Preoperative Western Ontario and McMaster Universities Arthritis Index 41.5±13.4 (32-51) 55.9±9.7 (29-74) .056 51.9±1.4 (50-52) 52.7±15.1 (24-79) .875 Postoperative Harris Hip Score 98.5±2.1 (97-100) 98.6±2.0 (93-100) .935 5.0±4.2 (2-8) 3.2±2.8 (0-8) .404 Postoperative Western Ontario and McMaster Universities Arthritis Index a Independent samples t test. Table 3 Incidence of Complications No. (%) Group A (n=50) Group B (n=50) Pa Subsidence 1 (2) 0 (0) .313 Periprosthetic fracture 1 (2) 1 (2) 1.000 Malalignment 2 (4) 1 (2) .554 Leg length discrepancy 1 (2) 0 (0) .313 Thigh pain 0 (0) 2 (4) .151 Heterotopic ossification 1 (2) 2 (4) .554 Infection 0 (0) 1 (2) .313 Dislocation 1 (2) 1 (2) 1.000 Complication a Fisher’s exact test. and WOMAC score improved by 44.8 and 45.1 points, respectively. In addition, no significant differences in mean postoperative HHS (P=.168) or WOMAC score (P=.158) were observed in the 2 groups, according to an independent samples t test. Table 2 shows 2 stems (4%) located in valgus position (>5° from neutral). Mean preoperative and postoperative HHS and WOMAC score were similar to those for stems located neutrally in group A. Radiographic Findings All stems in group A showed bone bridging and endosteal spot welds distributed in Gruen zones 2 and 6 as evidence of bony ingrowth with no radiolucencies e314 (Figure 2). Two patients in group B had a slight decrease in bone density, mostly in Gruen zones 1 and 7. No radiographic evidence of osteolytic lesions, cortical hypertrophy, or acetabular fractures was detected in either group, and no patient required revision surgery for aseptic loosening. Complications Chi-square (Fisher’s exact) test showed no significant difference in patient complications in the 2 groups (Table 3). One patient in group A with a head-neck-shaft angle of 135° had subsidence (>2 mm, P=.313) that showed bony ingrowth, with no further progression of subsidence at fi- Figure 2: Radiograph showing well-fixed acetabular and femoral components in an ideal position in the right hip without osteolysis. Bone trabeculae are seen streaming toward the METHA stem (Aesculap, Tuttlingen, Germany) (spot welds) in Gruen zones 2 and 6. nal follow-up. Two patients (1 in group A and 1 in group B) had intraoperative minor femur neck fracture (P=1.00). These patients were treated with cerclage wires without further incident. Three patients (2 in group A, valgus and head-neck-shaft angle of 135°; 1 in group B, varus) had malalignment (P=.554) that was not associated with loosening. One patient in group A with a head-neck-shaft angle of 135° had leg length discrepancy of greater than 1 cm (shortening, P=.313). Two patients in group B had thigh pain (P=.151) that disappeared after a few months. Three patients (1 in group A and 2 in group B) had heterotopic ossifications (P=.554) that were categorized as Brooker class I in 2 patients and class II in 1 patient and did not limit their activities. One patient in group B had a superficial wound infection that was treated with local debridement and antibiotics. Early dislocation occurred Copyright © SLACK Incorporated n Feature Article in 2 patients (1 in group A and 1 in group B). Two patients reported postoperative falls at the bedside, and both were treated with closed reduction without further procedures. No hips had deep venous thrombosis or pulmonary embolism. Discussion The most important finding of the current study was that no significant differences in clinical or radiographic outcomes or component-specific complications were observed between the 2 groups. Additionally, valgus alignment after insertion of METHA stems did not negatively affect clinical outcomes at short- to midterm follow-up. Although no significant differences were observed in thigh pain or proximal bone resorption in the 2 groups, patients in group B had a higher incidence of thigh pain (4%) and proximal bone resorption (4%) than patients in group A. Additionally, although no significant difference in malalignment or subsidence was found between the 2 groups, patients in group A who had a head-neck-shaft angle of 135° had a higher incidence of malalignment (4%) and subsidence (2%) than those in group B. One of the most common complications of conventional-length stems in cementless THA is the potential risk of proximal stress shielding.19 Therefore, many studies investigated patients who underwent treatment with a femoral neck-preserving short stem to allow more proximal load transfer and reduction of the stress shielding effect. However, there have been no direct in vivo simultaneous comparisons of specific femoral short stems (METHA) and conventional-length femoral stems (BiCONTACT) after primary cementless THA. Only 1 biomechanical study of strain patterns with 2 synthetic femora showed that both stems apparently decreased strain in the greater trochanter region; furthermore, the BiCONTACT stem dramatically decreased strain around the calcar with a combination of metaphyseal and diaphyseal load transfer.10 These earlier MARCH/APRIL 2016 | Volume 39 • Number 2 results indicated that both stems similarly decreased fundamental strain and the risk of stress shielding in the proximal femur; however, the anchorage location of the femur may be different. In contrast, a study of clinical and radiographic outcomes in 177 patients who underwent THA with a BiCONTACT stem reported that proximal bone resorption was 6% at long-term follow-up.20 This discrepancy was likely due to the use of synthetic bone, which may have affected the measurement of proximal bone resorption as a result of altered stress in the proximal femur. In the current study, patients in group B had a higher incidence (4%) of proximal bone resorption than those in group A, even with a short follow-up period. This proximal bone resorption may have occurred because there was no primary goal to achieve press-fit and maximal canal filling, including less reproducible insertion with a surgical technique because of an initial learning curve. In addition, all patients who had proximal bone resorption had thigh pain. In general, thigh pain is related to a stem design that occupies the diaphysis, although BiCONTACT stems are designed to achieve proximal load transfer.5,21 This may explain the current finding that the METHA stem minimized stress shielding as a result of proximal bone resorption and thigh pain and provided more successful bone remodeling, according to Wolff’s law.22 With the METHA stem, it is necessary to avoid any valgus position that could lead to subsidence without proximallateral support, whereas other short stems may be prone to the varus position when encountering osteoporotic bone with a widened intramedullary canal.23,24 One study showed that the level of neck resection with a short metaphyseal stem affects the stem position, the head-neck-shaft angle, femoral offset, and leg length, indicating that a lower neck resection causes a more vertical stem position, which decreases offset and leg length and increases the head-neck-shaft angle.25 This was similar to previous findings that showed that the final position of the METHA stem and the head-neck-shaft angle were significantly higher with lower neck resection and that the offset was in a lower position compared with more proximal resections.26 The current study showed that 1 of 2 patients in group A who had a valgus stem position with a head-neck-shaft angle of 135° simultaneously had subsidence and leg length discrepancy. This finding suggested that an unintentionally lower neck resection could change stem position and offset, leading to subsidence. Interestingly, the current findings showed no difference in HHS and WOMAC score in the valgus position of implants compared with the neutral position of implants in group A. Discrepancies between clinical and radiographic outcomes may be the result of the lack of standardized scoring systems based on a relatively arbitrary patient report. Other differences may be the result of unexpectedly complicated biomechanics of the hip between various tissues and bony structures. Together, clinically, these studies suggest that preservation of a 5- to 10-mm cortical ring around the femoral neck and osteotomy at an angle of 50° to the femoral shaft axis may have advantages during METHA stem implantation, including more accurate neck resection and better control of the stem position (Figure 3). Many studies have investigated the factors that predispose patients to periprosthetic fractures of the femur and found that they may include stem design and individual parameters, such as body mass index and bone mineral density.27,28 However, the current study showed no significant differences in periprosthetic fractures between the 2 groups in body mass index, bone mineral density, age, sex, preoperative diagnosis, or stem design, although the very specific tapered nature of the stemless implant caused significant hoop stress, increasing the likelihood of femoral neck fracture. It is possible that most of the periprosthetic fractures were seen e315 n Feature Article Figure 3: Radiographic templates showing a 5- to 10-mm–thick ring of cortex around the femoral neck that provides considerable anchorage. Osteotomy of the femoral neck is performed at an angle of 50° to the femoral shaft axis, measuring the distance from the lesser trochanter. in the initial learning period. This could be the result of an inaccurate implantation technique, most likely involving intentionally high neck resection and the use of a bigger rasp than planned to avoid undersizing. This study had several limitations. First, although the data were collected prospectively, the study design was retrospective and not randomized. Second, all THA procedures were performed by a single surgeon. Although the authors attempted to standardize the surgical techniques, it may be difficult to distinguish clearly between the 2 procedures and to avoid the potential drawback of selecting patients who are satisfactory candidates. However, the surgeon who performed these procedures was highly experienced with these techniques, especially with respect to femoral neck resection. Additionally, the authors attempted to minimize selection bias resulting from the inclusion of a single surgeon through case-matched analysis. Third, the study did not compare reliability between 2 implants with completely different stems in analyzing clinical and radiographic out- e316 comes because the specific femoral short stem was not just a shorter design of the conventional-length stem. Furthermore, the design of this particular stemless implant allows subsidence in the short term, and unlike most cementless stems, subsidence of greater than 2 mm is consistent with ingrowth because of the tapered stem design.29,30 However, no consensus has been reached on specific criteria for comparison of 2 implants. Finally, the median followup of 5 years was relatively short to allow a conclusion regarding implant safety. However, the current study provides baseline comparison data, especially in terms of functional scores and complication rates. Despite these limitations, to the authors’ knowledge, this in vivo study is the first to simultaneously compare specific femoral short stems with conventional-length femoral stems in patients undergoing primary cementless THA. Conclusion No significant differences in clinical and radiographic outcomes or componentspecific complications were observed between the 2 groups, showing satisfactory performance at 5-year follow-up. Group A had a higher incidence of malalignment and subsidence and a lower incidence of thigh pain and proximal bone resorption than group B. Although longer follow-up is required, specific femoral short stems may have clinical and radiographic advantages and equivalent perioperative complications compared with conventionallength femoral stems. In addition, specific femoral short stems provide a step toward a specific design that more closely resembles the physiologic joint, and they appear to be a viable treatment option for active patients. However, their effective use requires proper patient selection in combination with careful preoperative planning and meticulous surgical technique. References 1. Bourne RB, Rorabeck CH. A critical look at cementless stems: taper designs and when to use alternatives. Clin Orthop Relat Res. 1998; 355:212-223. 2.Berend KR, Lombardi AV, Mallory TH, Dodds KL, Adams JB. Cementless doubletapered total hip arthroplasty in patients 75 years of age and older. J Arthroplasty. 2004; 19(3):288-295. 3. Kiyama T, Naito M, Shinoda T, Maeyama A. Hip abductor strengths after total hip arthroplasty via the lateral and posterolateral approaches. J Arthroplasty. 2010; 25(1):76-80. 4. Engh CA, Bobyn JD, Glassman AH. Porouscoated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987; 69(1):45-55. 5. Glassman AH, Bobyn JD, Tanzer M. New femoral designs: do they influence stress shielding? Clin Orthop Relat Res. 2006; 453:64-74. 6. Santori FS, Santori N. Mid-term results of a custom-made short proximal loading femoral component. J Bone Joint Surg Br. 2010; 92(9):1231-1237. 7. Stulberg SD, Dolan M. The short stem: a thinking man’s alternative to surface replacement. Orthopedics. 2008; 31(9):885-886. 8. Chen HH, Morrey BF, An KN, Luo ZP. Bone remodeling characteristics of a shortstemmed total hip replacement. J Arthroplasty. 2009; 24(6):945-950. 9. Whiteside LA, White SE, McCarthy DS. Effect of neck resection on torsional stability of cementless total hip replacement. Am J Orthop (Belle Mead NJ). 1995; 24(10):766770. 10. Gronewold J, Berner S, Olender G, et al. Changes in strain patterns after implantation of a short stem with metaphyseal anchorage compared to a standard stem: an experimental study in synthetic bone. Orthop Rev (Pavia). 2014; 6(1):5211. 11. Patel RM, Stulberg SD. The rationale for short uncemented stems in total hip arthroplasty. Orthop Clin North Am. 2014; 45(1):19-31. 12. Pozowski A, Ścigała K, Kierzek A, Paprocka-Borowicz M, Kuciel-Lewandowska J. Analysis of the influence of a Metha-type metaphysical stem on biomechanical parameters. Acta Bioeng Biomech. 2013; 15(2):1321. 13. Gill IR, Gill K, Jayasekera N, Miller J. Medium term results of the collum femoris preserving hydroxyapatite coated total hip replacement. Hip Int. 2008; 18(2):75-80. 14. Poolman RW, Verhaar JA, Schreurs BW, et al. Finding the right hip implant for patient and surgeon: the Dutch strategy. Empowering patients. Hip Int. 2015; 25(2):131-137. 15.Engh CA Jr, McAuley JP, Sychterz CJ, Sacco ME, Engh CA Sr. The accuracy and reproducibility of radiographic assessment Copyright © SLACK Incorporated n Feature Article of stress-shielding: a postmortem analysis. J Bone Joint Surg Am. 2000; 82(10):14141420. 16.Mulliken BD, Bourne RB, Rorabeck CH, Nayak N. A tapered titanium femoral stem inserted without cement in a total hip arthroplasty: radiographic evaluation and stability. J Bone Joint Surg Am. 1996; 78(8):12141225. 17.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; 141:17-27. 18. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973; 55(8):1629-1632. 19. Bieger R, Ignatius A, Decking R, Claes L, Reichel H, Dürselen L. Primary stability and strain distribution of cementless hip stems as a function of implant design. Clin Biomech (Bristol, Avon). 2012; 27(2):158-164. 20. Swamy G, Pace A, Quah C, Howard P. The Bicontact cementless primary total hip ar- MARCH/APRIL 2016 | Volume 39 • Number 2 throplasty: long-term results. Int Orthop. 2012; 36(5):915-920. 21. Brown TE, Larson B, Shen F, Moskal JT. Thigh pain after cementless total hip arthroplasty: evaluation and management. J Am Acad Ortho Surg. 2002; 10(6):385-392. 22.Østbyhaug P, Klaksvik J, Romundstad P, Aamodt A. An in vitro study of the strain distribution in human femora with anatomical and customised femoral stems. J Bone Joint Surg Br. 2009; 91(5): 676-682. 23.Jerosch J, Grasselli C, Kothny PC, Litz kow D, Hennecke T. Reproduction of the anatomy (offset, CCD, leg length) with a modern short stem hip design: a radiological study [in German]. Z Orthop Unfall. 2012; 150(1):20-26. 24. Kamada S, Naito M, Nakamura Y, Kiyama T. Hip abductor muscle strength after total hip arthroplasty with short stems. Arch Orthop Trauma Surg. 2011; 131(12):1723-1729. 25.Floerkemeier T, Gronewold J, Berner S. The influence of resection height on proximal femoral strain patterns after Metha short stem hip arthroplasty: an experimental study on composite femora. Int Orthop. 2013; 37(3):369-377. 26. Mihalko WM, Saleh KJ, Heller MO, Mollard B, König C, Kammerzell S. Femoral neck cut level affects positioning of modular shortstem implant. Orthopedics. 2009; 32(10):1821. 27. Beals RK, Tower SS. Periprosthetic fractures of the femur: an analysis of 93 fractures. Clin Orthop Relat Res. 1996; 327:238-246. 28. Berry DJ. Periprosthetic fractures associated with osteolysis: a problem on the rise. J Arthroplasty. 2003; 18(3 suppl 1):107-111. 29. Krismer M, Biedermann R, Stöckl B, Fischer M, Bauer R, Haid C. The prediction of failure of the stem in THR by measurement of early migration using EBRA-FCA: Einzel-BildRoentgen-Analyse-femoral component analysis. J Bone Joint Surg Br. 1999; 81(2):273280. 30. Fottner A, Schmid M, Birkenmaier C, Mazoochian F, Plitz W, Volkmar J. Biomechanical evaluation of two types of short-stemmed hip prostheses compared to the trust plate prosthesis by three-dimensional measurement of micromotions. Clin Biomech (Bristol, Avon). 2009; 24(5):429-434. e317