An 11-year-old Girl with Burning Sensation in Her Hands
advertisement
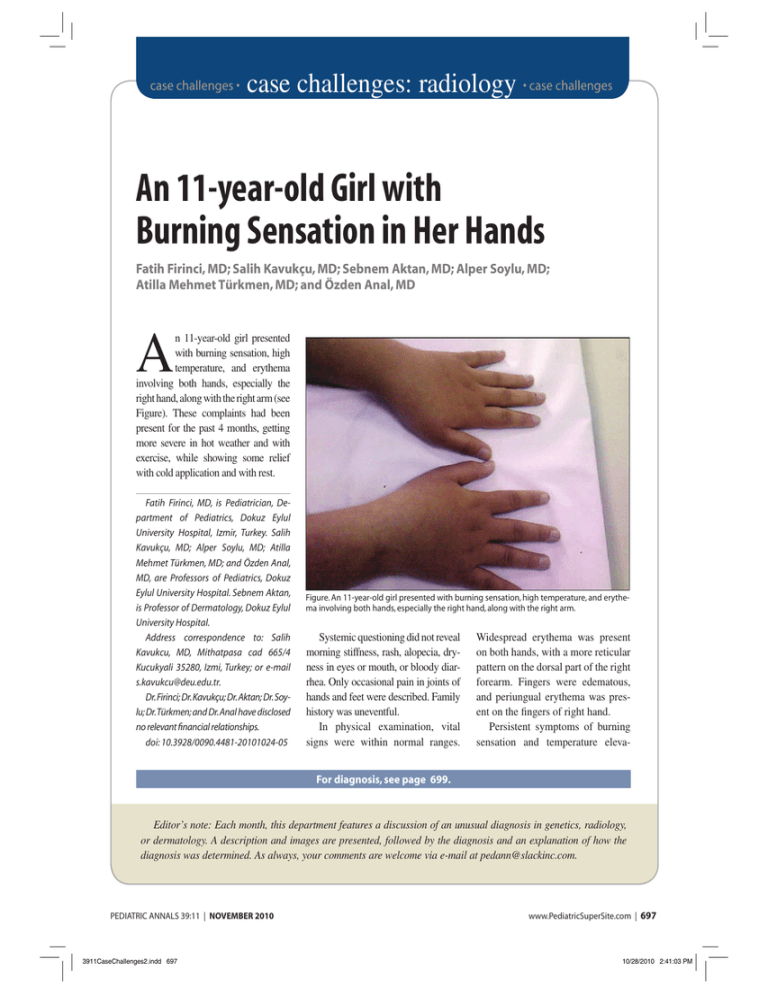
case challenges • case challenges: radiology • case challenges An 11-year-old Girl with Burning Sensation in Her Hands Fatih Firinci, MD; Salih Kavukçu, MD; Sebnem Aktan, MD; Alper Soylu, MD; Atilla Mehmet Türkmen, MD; and Özden Anal, MD A n 11-year-old girl presented with burning sensation, high temperature, and erythema involving both hands, especially the right hand, along with the right arm (see Figure). These complaints had been present for the past 4 months, getting more severe in hot weather and with exercise, while showing some relief with cold application and with rest. Fatih Firinci, MD, is Pediatrician, Department of Pediatrics, Dokuz Eylul University Hospital, Izmir, Turkey. Salih Kavukçu, MD; Alper Soylu, MD; Atilla Mehmet Türkmen, MD; and Özden Anal, MD, are Professors of Pediatrics, Dokuz Eylul University Hospital. Sebnem Aktan, is Professor of Dermatology, Dokuz Eylul University Hospital. Address correspondence to: Salih Kavukcu, MD, Mithatpasa cad 665/4 Kucukyali 35280, Izmi, Turkey; or e-mail s.kavukcu@deu.edu.tr. Dr. Firinci; Dr. Kavukçu; Dr. Aktan; Dr. Soylu; Dr. Türkmen; and Dr. Anal have disclosed no relevant financial relationships. doi: 10.3928/0090.4481-20101024-05 Figure. An 11-year-old girl presented with burning sensation, high temperature, and erythema involving both hands, especially the right hand, along with the right arm. Systemic questioning did not reveal morning stiffness, rash, alopecia, dryness in eyes or mouth, or bloody diarrhea. Only occasional pain in joints of hands and feet were described. Family history was uneventful. In physical examination, vital signs were within normal ranges. Widespread erythema was present on both hands, with a more reticular pattern on the dorsal part of the right forearm. Fingers were edematous, and periungual erythema was present on the fingers of right hand. Persistent symptoms of burning sensation and temperature eleva- For diagnosis, see page 699. Editor’s note: Each month, this department features a discussion of an unusual diagnosis in genetics, radiology, or dermatology. A description and images are presented, followed by the diagnosis and an explanation of how the diagnosis was determined. As always, your comments are welcome via e-mail at pedann@slackinc.com. PEDIATRIC ANNALS 39:11 | NOVEMBER 2010 3911CaseChallenges2.indd 697 www.PediatricSuperSite.com | 697 10/28/2010 2:41:03 PM case challenges tion, along with local vasodilation and hyperemia, which are activated by environmental heat and exercise and are relieved by cold application and rest, suggested erythromelalgia. Treatment with misoprostol was begun, considering the low rate of adverse effect of the drug and to avoid masking any probable underlying collagen disorder. Laboratory evaluation for differential diagnosis and classification of erythromelalgia yielded the following results: • Hb 13.3 g/dL; • leukocyte 5000/µL; • platelet 134,000/µL; • urine specific gravity 1010; • pH 6.0; • protein (1+); • blood (-); • 2-3 WBC/hpf; • glucose 82 mg/dL; • BUN 21 mg/dL; 698 | www.PediatricSuperSite.com 3911CaseChallenges2.indd 698 • • • creatinine 0.55 mg/dL; albumin 4.6 g/dL; LDL 160 mg/dL; On the seventh day of prednisolone treatment, erythema, pain, and edema in the right forearm decreased significantly, while ESR regressed to normal values. HDL 77 mg/dL; triglycerides 68 mg/dL. Electromyography and upper extremity and renal Doppler ultrasonography were normal. Serologic tests revealed hypocomple• • mentemia as C3 74 mg/dL (82-173 mg/dL), C4 9.6 mg/dL (13-46 mg/ dL), and positivity in ANA (1/160); anti-dsDNA (1/20), pANCA and anticardiolipin IgM (40 MPL/mL), and IgG (24 GPL/mL) antibodies. Other laboratory results were erythrocyte sedimentation rate (ESR): 42 mm/h, CRP: 1.2 mg/dL (0.1-8.2 mg/dL), rheumatoid factor: negative, extractable nuclear antigen panel: negative. Steroid treatment with 2 mg/kg/ day prednisolone was started, and misoprostol was stopped. On the seventh day of prednisolone treatment, erythema, pain, and edema in the right forearm decreased significantly, while ESR regressed to normal values. Prednisolone was decreased to alternate day doses at the end of 4-week treatment course, and acetyl salicylic acid (100 mg/d) was added. PEDIATRIC ANNALS 39:11 | NOVEMBER 2010 10/28/2010 2:41:04 PM case challenges D I A G N O S I S Secondary Erythromelalgia due to Systemic Lupus Erytematosus (SLE) DISCUSSION A patient with complaints of burning sensation, erythema, and an increase in temperature of the extremities, relieved by cold application and rest, should raise the suspicion of erythromelalgia. A careful evaluation in such a case is needed for differential diagnosis of some clinical conditions, such as Raynaud’s syndrome, burning feet syndrome, reflex sympathetic dystrophy, angiodyskinesis, acrocyanosis, lipodermatosclerosis, and erysipelas.1,2 Five criteria suggested by Thompson et al. are used in the diagnosis of erythromelalgia:3 burning pain in the extremities; increase in pain in exposure to high environmental temperature; decrease in pain by cold application; erythema in the affected body area; and increase in temperature in the affected skin region. All of these were observed in this child, and she was diagnosed with erythromelalgia. Erythromelalgia can be primary but also may appear secondary to another disease. Therefore, other underlying clinical conditions that might be the cause of erythromelalgia should be properly excluded, such as drugs (verapamile, nicardipine, bromocriptine, pergolide, mercury); vasculitis syndromes; cardiovascular diseases (hypertension, venous insufficiency); hematologic disorders (pernicious ane- PEDIATRIC ANNALS 39:11 | NOVEMBER 2010 3911CaseChallenges2.indd 699 mia, thrombocytemia, thrombotic thrombocytopenic purpura, polycytemia, hereditary spherocytosis, leukemias); neuropathies (polyneuropathy, hereditary sensory neuropathy, central nervous system lesions); infections (syphilis, AIDS); autoimmune diseases; musculoskeletal disorders; cholesterol crystal embolism syndrome; diabetes mellitus; hypercholesterolemia; gout and familial nephritis; conversion disorder, and malignancies.1-6 In this patient with erythromelalgia, history of arthralgia, hypocomplementemia, high ESR, along with low CRP, ANA and anti dsDNA Erythromelalgia can be primary but also may appear secondary to another disease. positivity, and complaints that affect the life quality, there were suggestions of erythromelalgia secondary to SLE, although the lupus criteria were not completely fulfilled. However, the diagnosis of SLE is a dynamic process. Thus, a patient may fulfill the SLE criteria in time. The dramatic improvement of the patient in response to steroid treatment provided further support for SLE. It is probable that, when the dose of steroid is decreased or stopped completely, the patient will develop other SLE manifestations. Thus, the patient should be in close follow-up for other clinical findings and complications of SLE. Primary erythromelalgia can be quite resistant to treatment, although the symptoms in the secondary type usually decrease with the treatment of the underlying condition.2 In primary erythromelalgia, various treatment modalities have been tried, such as: • non-steroidal anti-inflammatory drugs (NSAIDs; aspirin, indomethacin); • beta-blockers; • antihistamines; physical methods; • vasodilators (nitroprusside); • anticonvulsants (gabapentin, carbamazepine); • antidepressants (amytriptylline); • antimitotics (carmustine); • alpha-blockers (prazoscine, doxazoscine); • immunosuppressants; • migraine medications; • dapsone; • prostaglandin E1 analogues; • topical nitroglycerine; • pentoxyphylline; • dipyridamole; • mexiletine HCl; • quinine; • muscle relaxants; • surgical treatments, such as sympathectomy. The effectiveness of these medications is variable.1,4,7,8 However, improvement in secondary erythromelalgia is usually observed with the treatment of the underlying cause.2 In this patient, prostaglandin E1 analogue, misoprostol, was administered initially. However, because secondary erythromelalgia in SLE has been reported to be a cutaneous vasculitis responding to oral prednisolone,9 the treatment was changed to prednisolone when SLE was considered www.PediatricSuperSite.com | 699 10/28/2010 2:41:04 PM case challenges as the primary clinical condition. Although steroids also have been mentioned to be effective in idiopathic erythromelalgia, the rapid response of the patient to steroid treatment favored the diagnosis of SLE associated erythromelalgia. CONCLUSION The presentation of this case demonstrates that when erythromelalgia is considered in a pediatric patient, underlying clinical conditions should be carefully sought before it is diagnosed as idiopathic, and proper treatment should be instituted accordingly. 700 | www.PediatricSuperSite.com 3911CaseChallenges2.indd 700 REFERENCES 1. Davis MD, O’Fallon WM, Rogers RS, Rooke TW. Natural history of erythromelalgia: presentation and outcome in 168 patients. Arch Dermatol. 2000;136(3):330-336. 2. Mork C, Kvernebo K. Erythromelalgia — a mysterious condition? Arch Dermatol. 2000;136(3):406-409. 3. Thompson GH, Hahn G, Rang M. Erythromelalgia. Clin Orthop Relat Res. 1979;144:249-254 4. Cohen JS. Erythromelalgia: new theories and new therapies. J Am Acad Dermatol. 2000;43:841-847. 5. Herskovitz S, Loh F, Berger AR, Kucherov M. Erythromelalgia: association with hereditary sensory neuropathy and response to amitriptyline. Neurology. 1993;43(5 Pt 1):621-622. 6. Odom RB, James WD, Berger TG: An- drew’s diseases of the skin. In: Clinical Dermatology. 9th ed. Philadelphia: W.B. Saunders; 2000:1012-1103. 7. Mork C, Salerud EG, Asker CL, Kvernebo K. The prostaglandin E1 analog misoprostol reduces symptoms and microvascular arteriovenous shunting in erythromelalgia-a double-blind, crossover, placebo-compared study. J Invest Dermatol. 2004;122(3):587-593. 8. Suh DH, Kim SD, Ahn JS, et al. A case of erythromelalgia successfully controlled by systemic steroids and pentazocine--is it related to a unique subtype of neutrophilic dermatosis? J Dermatol. 2000;27(3):204-210. 9. Drenth JP, Michiels JJ, van Joost T, Vuzevski VD. Secondary erythermalgia in systemic lupus erythematosus: comment. J Rheumatol. 1993;20(1):144-146. PEDIATRIC ANNALS 39:11 | NOVEMBER 2010 10/28/2010 2:41:04 PM