TECHNICAL CORNER: DETERMINING RISE TIME AND OTHER
advertisement

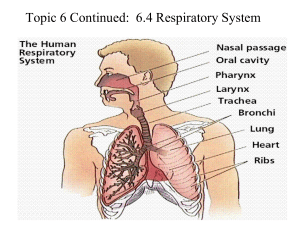
30 TECHNICAL CORNER: DETERMINING RISE TIME AND OTHER PAP DEVICE SETTINGS IN RELATION TO THE PATIENT'S RESPIRATORY CYCLE AND PATHOPHYSIOLOGY By Will Eckhardt, BS, RST, RPSGT, CRT T he act of ventilation moves gas into and out of the alveoli facilitating exchange of gases at the alveolar capillary membrane and respiratory bronchioles. Without this gas exchange, respiration (process of gas molecules moving at the cellular level) would essentially not be possible. The respiratory cycle moves a volume of air in and out of the airways and lungs; this volume is one’s tidal volume. Achieving ventilation has a cost: the energy required to ventilate the alveoli or work of breathing (WOB). Two components of this workload are elastic work or compliance, and resistive work due to the air molecules flowing through the airways. This article will discuss what these components are and how these forces along with disease process (pathophysiology) of the patient determines how we might set respiratory cycle parameters of the positive airway pressure (PAP) device used for the patient. Air flows from a region of high pressure to one of a lesser pressure. Ventilation stops when alveolar gas pressure is equal to the atmospheric pressure (e.g., at end expiration). During inhalation the muscles of ventilation cause the chest cavity to enlarge, creating a greater degree of negative or subatmospheric intrathoracic pressure. Normally the lung (other than during exhalation) is somewhat subatmospheric due to the forces of elastic recoil. The lowering of intrathoracic pressure invites the expansion of the alveoli making the exchange of gases possible, presuming the capillaries are filled with blood from a viable pulmonary circulation. Upon end inspiration, normally the muscles of inspiration relax and the elastic tissues of the lungs and thorax recoil causing a positive pressure within. This pressure becomes greater than atmospheric, expelling a quantity of the total lung volume termed the tidal volume (VT). In some lung diseases active contraction of expiratory muscles must be used, but in normal physiology exhalation is passive. The term compliance is used to describe the forces produced by the elastic properties of the lung and thorax. Compliance can be decreased in the patient with lung disease. Decreasing compliance causes an increase in the work of breathing (increasing muscular work for adequate ventilation). Patients with reduced compliance usually increase their respiratory rate to compensate for a decrease in tidal volume. Airway resistance is related to friction, whether it is between the gas molecules as the gas flows through the airways and lungs or as the molecules collide with the airway walls. When the airways are unrestricted, the flow is usually laminar. Laminar flow is related to the viscosity of the gas, the distance within the airways and lungs, and inversely related to the radius of the lumen (size of the tube). Turbulent flow, however, is proportional to the square of the volume flow and the density of the gas and not related to viscosity. A smooth, straight tube will have turbulence only at high flow rates. Acute and chronic conditions may exacerbate turbulence within the airway; tumors, mucus, bronchoconstriction, airway collapse and increased respiratory rate. When there is increased airway resistance during expiration, the full tidal volume may not have time to be completely exhaled; this will lead to an increas- ing volume in the lungs at end expiration, thereby hampering gas exchange. Giving more time for expiration will allow the return to a normal expiratory volume. If not given this time, the patient may exhibit a more active exhalation, increasing the work of breathing. Increasing work of breathing will cost the patient in increased oxygen consumption and possible ventilatory failure. The act of ventilation (movement of gases during inspiration and expiration) is a dynamic process aiding alveolar ventilation (volume of oxygenated air entering the alveoli). If we breathe in a volume only equal to that of the conducting airways, there would be no alveolar ventilation. The air in the conducting airways is termed “dead space” (dead space also includes unperfused alveoli). In the normal adult, dead space is about 150 ml. This 150 ml is the first air to reach the alveoli upon inspiration. If the tidal volume in a breath is 500ml and the dead space is 150 ml, the alveolar ventilation equals 350 ml. During expiration the first air leaving the body is the dead space, followed by air that was actively used in respiration. Large tidal volumes cause a larger volume to enter the alveoli, whereas shallow breathing causes a smaller portion of the tidal volume to enter the alveoli. This pulmonary ventilation must supply adequate oxygen for the cells to use and remove the carbon dioxide produced by metabolic activity of the body. Some parameters used in ventilation by some PAP devices are: Respiratory Rate (RR), Tidal volume (VT), Rise Time, Inspiratory Time (Ti), Expiratory Time, I:E Ratio, and Pressure Support. See Figure 1. Respiratory rate settings are generally set a couple of breaths lower than the patient’s normal respiratory rate. This enables the machine to cycle when the time between breaths lengthens beyond what the algorithm calculates is needed to maintain the prescribed respiratory rate. Rise time is the time it takes the pressure on a PAP device to move from the expiratory PAP (EPAP) pressure to the inspiratory PAP (IPAP) pressure; there would be no rise time on a CPAP device as the pressure is constant. More on rise time to follow. Inspiratory Time is the time over which the device is in the inspiratory phase. Expiratory time is the time in which the device is in the expiratory phase of a breath cycle. I:E Ratio is inspiratory time plus the inspiratory pause time:expiration. In a normal adult this is usually set to 1:2. • I:E ratio = (inspiratory time + inspiratory pause time) :expiration usually set to 1:2 to mimic usual pattern of breathing • In general longer inspiratory times: improve oxygenation by: • increasing the mean airway pressure (longer period of high pressure increases mean airway pressure over the entire respiratory cycle) • allowing re-distribution of gas from more compliant alveoli to less compliant alveoli present potential problems such as: • increased risk of gas trapping, intrinsic PEEP and barotrauma due to reducing expiratory time A2 Zzz 21.2 | July 2012 31 • ventilation is less well tolerated by the patient, necessitating a deeper level of sedation • Pressure Support is determined by the difference between the settings for IPAP and EPAP FIGURE 1. POSITIVE AIRWAY PRESSURE (PAP) AND THE RESPIRATORY CYCLE. In patients with purely obstructive lung disease (e.g. COPD), resistive work increases without a change in elastic work. In purely restrictive lung disease (e.g. Kyphoscoliosis), elastic work increases with no change in resistive work. When setting PAP parameters, we need to evaluate the patient’s respiratory cycle (see Figure 1) and pathophysiology to the device settings available; one such setting is rise time. Rise time is the time it takes a device to change from EPAP to IPAP. With a faster rise time, flow is greater at the beginning of inspiration. A fast rise time can decrease dyspnea in patients with a high respiratory drive, whereas increasing the rise time can increase the work of breathing and decrease patient comfort. A rise time that is too fast can cause turbulent air flow and cause discomfort to the patient, hampering efforts toward compliance with the therapy. Adjustments to rise time are generally made for patient comfort. Rise time can be set to a minimum, creating a fast rise time; or by increasing the rise time setting, we can increase the time it takes for the pressure to go from EPAP to IPAP. In cases where the patient has a high demand, the rise time can be set to the minimum, giving the patient the fastest rise time. The rise time is affected by the patient’s compliance, resistance and the difference between the EPAP and the IPAP. The patient needs adequate flows to prevent air hunger (the feeling of not getting adequate ventilation as flow rates are too low); but this needs to be tempered with decreasing the rise time and creating air turbulence causing discomfort. An example of this setting would be settings in a range of 1-6, with each increment corresponding to a tenth of a second; such a setting of 3 would be 0.3 second rise time. Gas trapping may occur with a rapid change to expiration as the alveoli do not have time to empty before the start of the next breath. Gas trapping may occur in COPD and asthma, and when the setting for inspiratory time is long and therefore expiratory time is shortened. An example of an inspiratory time setting would be 0.5 to 3 seconds with increments of 0.1 seconds. PAP devices trigger according to proprietary algorithms. Inspiratory positive airway pressure (IPAP) is delivered in response to a trigger initiated by a spontaneous inspiratory effort. At end inspiration, the equipment will cycle to expiratory positive airway pressure (EPAP) according to the device’s algorithm. Patients with obstructive lung disease such as COPD can decrease the chance of barotraumas by using an expiratory time that is somewhat protracted. In these patients, settings that decrease minute ventilation and inspiratory time change the I:E ratio, shortening the inspiratory time and thereby lengthening the expiratory time (e.g., I:E ratio’s of 1:3 or 1:4). However, the effects of this change will increase peak pressures and hypercapnia; these side effects are usually well tolerated. VTs of 5-7 ml/kg and a faster inspiratory flow (e.g., 80-100 L/min.) will tend to extend expiratory time and avoid breath staking or air trapping. A faster TiMax setting allows a maximum inspiratory time that gives adequate time for patients to exhale fully through their diseased airways. For patients with restrictive disease (e.g., Amyotrophic Lateral Sclerosis [ALS]), neuromuscular disorders, or deformity disorders (e.g., Kyphoscoliosis), getting air in is more of the issue. With these patients we can extend the inspiratory time, allowing the lungs to more completely fill, minimizing the air hunger associated with an abridged inhalation. Airflow obstruction occurs in pathologies such as asthma and COPD. To a lesser extent this is also seen in bronchiectasis, cystic fibrosis, and bronchiolitis in which the small and large airways often have obstructive processes. The narrowing of the airways can diametrically increase airway resistance. The overload to the respiratory pump muscles may cause ventilatory pump failure with minute volumes unable to provide adequate spontaneous minute ventilation, resulting in an inability to provide proper gas exchange at the alveolar level. Another problem these patients may face is air trapping caused by airway narrowing with some alveolar regions within the patients’ lungs unable to properly empty. The area unable to empty may overinflate upon subsequent breaths. The best method of dealing with the hyperinflation is to keep VT and pressures low. It is also recommended to lengthen the expiratory time to deal with air trapping. Getting it right for the patient is essential for compliance and may take a number of adjustments. Patients requiring PAP therapies for ventilation issues are often not seen in a sleep laboratory setting, giving the clinician less time to evaluate setting changes. An understanding of how the parameters affect patients and how differing pathophysiologies affect ventilation will make the clinician more comfortable with setting up PAP for ventilation. PAP devices serve a more complex array of patients from ALS and COPD to complex sleep apnea and obesity hypoventilation. Patients often are affected by their medications (e.g., opioids), making it difficult to adjust equipment to address patient comfort. The individual who sets up patients in the home or long-term care environment needs to focus on the patients and interact with them to accommodate their needs in relation to the equipment parameters. ADDITIONAL READING Comroe JH. The lung: clinical physiology and pulmonary function tests. Chicago: Year Book Medical Publishers; 1962. Hlastala MP, Berger AJ. Physiology of respiration. New York: Oxford University Press; 2001. MacIntyre NR, Branson RD. Mechanical ventilation. St. Louis: Saunders Elsevier; 2009. Will Eckhardt, BS, RST, RPSGT, CRT, has been in the sleep field for more than 20 years and is a clinical liaison for Genter Healthcare in New Hampshire. A2 Zzz 21.2 | July 2012