Health Hazard Evaluation: A Useful Tool for Risk Escalation
advertisement

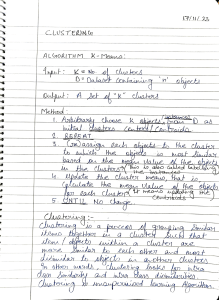
QUALITY & COMPLIANCE Health Hazard Evaluation: A Useful Tool for Risk Escalation By Thomas Morrissey, MD Early in my career as a medical director in the medical device industry, a young engineer approached me with a corrective and preventive action (CAPA) file and asked me to perform a health hazard evaluation (HHE) regarding a product issue. In reviewing the file, I noticed that a decision on whether an HHE was required was part of the CAPA process and one of the many boxes on the checklist required for closing this CAPA. This decision was his to make, I thanked him for getting me involved. Realizing that the CAPA was already three months old, I had a few questions: • Why are we now evaluating patient risk on an issue this old? • Why do we expect an engineer to make a clinical determination on patient risk? • Do we have a process that helps us to identify and escalate the right issues to the right people? • Shouldn’t patient risk drive decisions such as CAPA and not the other way around? Role of Health Hazard Evaluations When I began to examine how to better incorporate patient safety into our decision-making process in 2004, there was not much direction or consistency regarding HHEs in the emerging field of risk management in the medical device industry. The US Food and Drug Administration (FDA) has utilized the HHE for years to categorize the risk of an issue and classify recalls. Many device companies utilize the HHE only when a recall is being considered. I sought the opinion of several industry colleagues about HHE utilization; it seemed that standard practice was utilizing HHEs on an ad hoc, somewhat random basis. It was also the “perfect storm” time to examine how healthcare companies evaluate and escalate postmarket risk. Merck was questioned about its response to Vioxx data, Guidant had problems with its defibrillators, and several major medical device companies received Warning Letters, many of which cited inadequate postmarket surveillance and medical input into their decision-making process. Companies with otherwise excellent reputations were under fire for what some considered unethical decisions. Guidant responded to the criticism by 34 May 2010 establishing the Guidant Safety Advisory Panel1 of physicians, engineers, statisticians and ethicists. The panel offered guidance to medical device companies on how to evaluate safety issues and potentially avoid common mistakes. Among its findings and recommendations: • Designate or hire an in-house physician whose primary responsibility is patient safety and who will participate in product performance analysis, health hazard analysis, internal communications and external communication policies and procedures. • Enforce the primacy of patient safety by better integrating patient safety concerns into the factual and statistical analysis of product performance and failures and safety event trends. • Develop processes to identify and act on even a single event when it is associated with risk of death or serious injury, has a suspected or defined basis for malfunction or failure and is likely to be systemic and to occur in other patients. • Strengthen oversight by corporate management and develop specific processes to quickly identify and act on potentially life-threatening product performance problems. Develop a Process One of the speakers at a May 2005 risk management meeting sponsored by the Advanced Medical Technology Association (AdvaMed) was Dr. Dan Schultz, then director of FDA’s Center for Devices and Radiological Health (CDRH). The meeting was informative but only provided a high-level look at risk management. Specific recommendations on techniques to improve corporate risk management and postmarket surveillance processes were not provided. When questioned about ways companies could perform solid postmarket surveillance, Schultz replied with three specifics: • a robust electronic system to capture and analyze events, with data mining capabilities a big plus • the right mix of people looking at the data • a well-thought-out plan on what to do with the data and an escalation decision Figure 1. HHE as Cornerstone of Postmarket Surveillance Ongoing monitoring of nonconformances, complaints, vigilance, MDR’s Product nonconformance process No Issue affects product in the field? Yes No CAPA Yes Product risk assessment (HHE) Escalation required? CAPA required? Yes No Field action? Document action Yes Quality board Yes tree, encompassing actions all the way from continue to trend to recall Schultz reinforced the Guidant panel’s recommendation that companies should have a process for identifying, evaluating and escalating potential field safety issues. The industry norm is to identify product related issues through field complaints or manufacturing nonconformances. Companies also trend complaints and monitor adverse events. However, once potential safety issues are identified, what is the next step? How do companies get from event to recall? Edwards Lifesciences has instituted a threestep postmarket surveillance process that uses the HHE as the centerpiece (Figure 1): 1. Identify issues that impact distributed product such as complaints, nonconformances that escape containment in the manufacturing facility when an nonconformance report (NCR) is discovered, and manufacturing nonconformances confirmed by the product return lab on devices associated with complaints returned by users for evaluation. 36 May 2010 2. 3. Operational decision required? QB required? Perform a product risk assessment (PRA) consisting of an HHE and a compliance evaluation by a quality affairs (QA) director Decide whether the issue needs to be escalated. If not, decide whether to open a CAPA decision. If the decision is no, the rationale must be documented. Tying it all Together Another benefit of a well-defined, risk-based approach to issues in the field is overall strengthening of your complaint files. When an external auditor arrives at a company, these files are typically the first documents to be reviewed. In addition to gauging the quality of the complaint investigations and medical device reporting (MDR) rationales, auditors like to see that companies evaluate and act on complaints. Linking the complaint file to your HHE/risk assessment, which also links to a CAPA decision, allows your company to tell a story and the auditor to follow your thought process. Although the auditor may not ultimately agree with all of your actions, the linking of documents demonstrating your riskbased decisions will help communicate that your company makes patient safety a top priority. Requirements for Success A Clear, Concise Story The issue description in the HHE is extremely important. It should be simple, but clearly inform the reader about the issue under review. It should be easily understood by someone unfamiliar with the issue who reviews it one or two years after the event. If it is complaint driven, a table summarizing complaint and lot numbers, dates, MDRs/injuries, product evaluation results, etc., is helpful. Pictures are extremely valuable. Timeliness The goal of any successful postmarket surveillance program is to expeditiously escalate the right issues to the right people. Dates of issue identification and decisions must be clearly documented. Metrics and reasonable targets must be established and monitored. Consistency Across Documents Any HHE requires an evaluation of the severity of a particular failure. Obviously, this severity needs to be consistent with the corresponding failure mode and effects analysis (FMEA). If the FMEA has not been updated for some time and the existing document was created without clinical input, it should be updated with the correct designation. information we collect. The days of robotically filling out forms, checking boxes, filing MDRs and stamping “continue to trend” in the files are numbered. Regulatory bodies, customers and patients expect more from us. Companies need to develop processes to react to events in the field with the sole intent of improving their products and protecting patient safety. An HHE is the most important document for determining patients’ risk and should be an integral part of a company’s postmarket surveillance program. References 1. Myerburg RJ, Apostolakis GE, Beller GA, et al. “Report of the Independent Panel of Guidant Corporation.” http:// www.guidant.com/panel/. Published 20 March 2006. Accessed 8 May 2006. 2.. Morrissey T. Health Hazard Evaluations. Talk presented at AdvaMed/MLTI Meeting. Washington, DC. April 2006. Author Thomas B. Morrissey, MD, is vice president of product safety at Edwards Lifesciences. He is responsible for the risk management process in both product development and postmarket surveillance, as well as for providing medical oversight for worldwide complaint investigations and MDR reporting. He previously was responsible for risk management activities at Abbott Laboratories and Cordis (Johnson & Johnson) Corporation. He holds an MD from Oregon Health Sciences University, completed a General Surgery residency at Louisiana State University and a fellowship in Cardiothoracic Surgery at University of Rochester. Morrissey can be reached at Thomas_ Morrissey@Edwards.com. Revisions as Needed When developing a postmarket surveillance process, do not expect perfection from the beginning. Identify bottlenecks and impediments and revise your forms and process as needed. Buy-in From Management It is well known that any risk management system will fail without support from the executive team. It is imperative to seek their input when developing the process and after its implementation. A Culture of Patient Safety If you are successful in developing a dedicated postmarket surveillance risk management process based on patient risk, this is the most gratifying result. It is important to educate engineers, complaint handlers and management about when to identify issues and initiate the process. Summary When I was training to be a surgeon, my professor taught me a valuable lesson. He instructed me to never order a test on a patient without first having a plan for the results. This lesson is analogous to what we in the medical device industry typically do. We set up processes to monitor complaints and nonconformances, but often do not have a plan for handling the Regulatory Focus 37