senior design projects 2015
advertisement

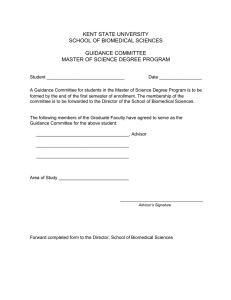
SENIOR DESIGN PROJECTS 2015 OPUS COLLEGE OF ENGINEERING DEPARTMENT OF BIOMEDICAL ENGINEERING industry sponsors 2014–2015 2008–2009 GE Healthcare, Waukesha, WI Medtronic USA Inc., Minneapolis, MN Rowheels, Fitchburg, WI DePuy Orthopedics, Inc., Warsaw, IN Siemens Medical Solutions, Hoffman Estates, IL GE Healthcare, Waukesha, WI ACTRA Rehabilitation Associates, Brookfield, WI Gauthier Biomedical Inc., Grafton, WI Stevenson Industries, Simi Valley, CA 2013–2014 Cytophil, Inc., East Troy, WI DesignWise Medical, Loretto, MN GE Healthcare, Waukesha, WI Siemens Healthcare, Hoffman Estates, IL Medtronic USA Inc., Minneapolis, MN 2012–2103 NeoCoil, LLC, Pewaukee, WI Gauthier Biomedical, Grafton, WI 3M, Minneapolis, MN 2011–2012 GE Healthcare, Waukesha, WI Medtronic USA Inc., Minneapolis, MN Innovator of Disability Equipment and Adaptations, LLC, Pewaukee, WI 2010–2011 Cardiac Science Corporation, Deerfield, WI DePuy Orthopedics, Inc. Warsaw, IN GE Healthcare, Waukesha, WI Medtronic USA Inc., Minneapolis, MN 2009–2010 DePuy Orthopedics, Inc. Warsaw, IN GE Healthcare, Waukesha, WI 3M, St. Paul, MN 2007–2008 3M, Saint Paul, MN Siemens Medical Solutions, Hoffman Estates, IL Baxter Healthcare, Deerfield, IL 2006–2007 Medtronic USA Inc., Minneapolis, MN DePuy Orthopedics, Inc., Warsaw, IN Siemens Medical Solutions, Hoffman Estates, IL GE Healthcare, Waukesha, WI 2005–2006 Medtronic USA Inc., Minneapolis, MN Guidant Corporation, St. Paul, MN AKSYS, Ltd., Lincolnshire, IL U.S. Navy Institute for Dental and Biomedical Research, Great Lakes, IL 2004–2005 Medtronic USA Inc., Minneapolis, MN DePuy Orthopedics, Inc., Warsaw, IN Rehabilitation Engineering Research Center, Milwaukee, WI Discovery World Museum, Milwaukee, WI Animark, Inc., Aurora, CO ON THE COVER: Team members create and assemble parts in the Discovery Learning Laboratory for a portable mount to allow spinal cord injury patients to exercise with a hand ergometer while recovering in bed. See page 10 for details. Marquette University Opus College of Engineering • Department of Biomedical Engineering to our industry partners W e are pleased to present the Biomedical Engineering Senior Design Projects completed during the 2014–2015 academic year at Marquette University. The Department of Biomedical Engineering at Marquette University is dedicated to preparing students for their professional and personal lives after graduation. Undergraduate students can specialize in biomechanical, bioelectrical, or biocomputer engineering. In addition to courses in engineering, mathematics, and the life sciences, students are required to complete several design challenges in the freshman year and a year-long projectbased capstone design course in the senior year. Students develop their teamwork skills, learn about the product development process used in industry, and are made aware of the unique requirements and constraints of medical device design. They consider legal and regulatory issues, use standards where applicable, conduct economic analyses, and learn about packaging, sterilization, and testing of medical devices. Several project deliverables, similar to those used in industry, are required. This capstone design experience provides students with the knowledge base and skill sets needed to be effective, contributing members of a medical device company, clinical engineering department, or academic research laboratory. This year we continued our 10-year collaboration with the Milwaukee Institute of Art and Design (MIAD). Five of our project teams collaborated with industrial design students from MIAD during the spring semester. This was the fourth year of external funding for service learning, assistive technology, and other projects. We appreciate this support made possible by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. At Marquette University, students may enhance their design experience and preparation for careers in the engineering profession through work experience. At the Les Aspin Center for Government Studies, students can work as interns for the US Food and Drug Administration and learn first-hand how the FDA functions and what is required to market a regulated medical device. Students participating in our highly popular and nationally recognized Cooperative Education Program gain work experience at medical device companies prior to graduation. As you read through this report and learn of the benefits of industry sponsorship of senior design projects, please consider becoming a sponsor. We recognize the value to our students and program of strong ties to industry, and we are interested in working with additional companies to help us prepare our students for careers in biomedical engineering. Respectfully, Jay R. Goldberg, Ph.D., P.E. Clinical Professor of Biomedical Engineering, Senior Design Course Instructor Senior Design • Lars Olson, Ph.D. Associate Professor and Interim Chair, Department of Biomedical Engineering 3 • 2014–2015 industry sponsorship Senior Design Course Sequence: Benefits of Sponsorship: At Marquette University, all senior biomedical engineering students are required to successfully complete a set of project-based capstone design courses (BIEN 4920, Principles of Design, and BIEN 4998, Senior Design). The objectives of this two-course sequence are to: Benefits to companies sponsoring design projects include: • develop students’ knowledge of the engineering design process, project management, and the product development process; • provide students with the opportunity to apply and develop their design, analytical, project management, interpersonal, and communication (oral and written) skills via a team based project experience; and • prepare students for careers in biomedical engineering. Senior Design Project: The major component of the course is a design project that is managed by a multidisciplinary team of three to five students for an entire academic year. During the year, project teams identify customer needs, develop potential designs, construct and test prototypes, and deliver a design and/or working prototype to their industry sponsors. Project teams develop project schedules, maintain project notebooks, conduct economic and risk analyses of their design solutions, and develop and present written and oral project proposals and final reports. • Additional resources at little or no cost to company. Three to five senior engineering students will be dedicated to each project for two semesters. The sponsoring company can specify the composition of the project team (biomedical, electrical, computer, and mechanical engineering students). This can be very beneficial to companies with limited engineering resources and can allow companies to focus efforts on higher-priority projects. • Involvement and participation in the training of new engineers and potential employees. • On-campus advertisement of the sponsoring company. Involvement in the senior design project will provide the company access to and a higher profile among graduating engineers. Many of the projects are industry sponsored and provide students with an opportunity to learn about the needs of the medical device market and the operations of a company. Experience gained from industry sponsored projects helps prepare students for careers in the medical device industry. Teams are advised by a biomedical engineering faculty member and a representative from the sponsoring company. Marquette University Opus College of Engineering • 4 • Department of Biomedical Engineering Benefits to students of industry-sponsored projects: • Opportunity to work on real-world problems important to industry. • Exposure to the medical device industry and market. • Experience with project management and product development. • Familiarity with requirements and constraints of medical device design. Requirements for Industry Sponsorship: Personnel: Sponsoring companies must identify at least one company representative to act as an industry advisor to the project team. The industry advisor would be the company contact for the project team, advise students on issues involving customer needs, provide technical expertise and advice, and approve design concepts and prototypes. Faculty advisors will be responsible for administrative issues (grading, meeting deadlines, monitoring progress of teams, dealing with team personnel issues, etc.) and providing guidance to the team. Time: At a minimum, industry advisors must be available to discuss project requirements, customer needs, and potential designs. Communications can be in-person or by phone, e-mail or video conference. The advisor determines the frequency of communications. Other: Students have access to Marquette University’s computer network, libraries, Discovery Learning Laboratory (machine shop, collaboration space, prototyping resources), faculty expertise, and engineering laboratories. Sponsors may want to provide additional resources (prototyping facilities and/or personnel, laboratories, etc.) to their project teams if desired. Types of Projects Appropriate for a Senior Design Project: • Lower priority projects for which the company lacks resources • Projects that can be completed in nine months or less • New products (hardware or software) • Product improvements (new features, packaging, materials, etc.) • Process improvements • Development of test procedures and/or test equipment Protection of Proprietary Information: Sponsors can request that members of their project teams sign non-disclosure agreements to protect confidential and trade secret information. To Sponsor a Biomedical Engineering Senior Design Project: Travel:The sponsoring company determines the need for travel. If you have any questions about our senior design program or if you are interested in sponsoring a senior design project please contact Dr. Jay Goldberg at (414) 288-6059 or jay.goldberg@mu.edu. Funding: Depending upon the needs and expectations of the sponsor, a fund of $1000 may be necessary to pay for prototypes and testing. We look forward to working with you. Senior Design • 5 • 2014–2015 projects • 2014–2015 projects Improved Design of a Head Holder for GE Revolution CT Scanner Project Team: Isaac Gerke Nicole Gibson Honnalee Fern Go Antonella Mantovano Alexander Matzuk Kevin Vanneman MIAD Partners: Evan Hoffman Emilie Troedson Faculty Advisor: Dr. Taly Gilat-Schmidt Sponsor: Michael Vaz, GE Healthcare C omputed tomography (CT) provides a fast, accurate, and reliable way to noninvasively see inside of a patient. When scanning, it is important to realize that, like other scanning procedures, some level of radiation exposure does come with a CT scan. For the head, the typical absorbed dose of radiation is 56 milligray, higher than most other body parts. This is a sensitive part of the body for radiation, so it is important to take proper precautions when preparing for a scan.. With proper head positioning, the eyes can avoid a large amount of radiation by not being on the same plane as the part of the brain being observed through the scans. The new Revolution CT machine from GE Healthcare allows for a patient friendly experience while providing doctors with the most advanced images possible. The implementation of a proper head holding device can increase patient comfort and safety while further assisting doctors in properly positioning any patient’s head. Currently, GE has only one option to assist with proper head alignment during CT scanning. This involves two foam wedges to position the head at two different angles. Due to the limited positions for head arrangement, a device needs to be created to allow a technician to easily adjust the head in more than two positions when using the new Revolution CT scanner. The device should be easily applied, removed, and adjusted by the technician performing the CT scan. Through adjustment, the head should be easily and comfortably maneuvered along the x- and z-axis for different angles, which must allow proper imaging, as well as comfort for the patient. Additionally, the material used must be easily cleaned and sterilized. Since the purpose of the design is to make imaging clearer, the material must also not disrupt imaging. The end goal of this new design is to make not only the technician’s job easier, but to improve the patient’s experience. The final head holder prototype fits all the functional needs specified by GE and the hospital technicians. Measurements taken from the original CT head holder ensured that the new design would easily slide into the CT bed as well as fit inside the bore of the machine. As expected, the device easily slides into the slot of the CT bed, and its weight allows for easy positioning of the device. A head mold provided by GE was used to ensure a human head could fit into the device and that the head holder could withstand the weight of a human head. The nylon used in the final prototype has similar radiolucent properties as carbon fiber, so minimal artifacts would be expected. Angle adjustment between 0 to 25 degrees can easily be performed after the head holder is placed in the CT bed. Marquette University Opus College of Engineering • 6 • Department of Biomedical Engineering Project Team: Carlos Peña Andrew Summers Andrew Tran Colton Rujevcan Abdulla Al Falasi William Thompson Faculty Advisor: Dr. Said Audi Sponsor: Val Eisele, Medtronic USA Inc. V irtual Interactive Patient III is a cardiac waveform simulator that is used to internally test implantable devices developed by Medtronic. Implantable devices are common in many people, especially the elderly, and in order to verify that these devices meet safety requirements, as well as the appropriate response to a stimulus, it is of extreme importance to have a reliable testing method. Previous versions of the Virtual Interactive Patient (I and II) are not versatile enough to keep up with the technological advancement of implantable devices. Therefore, a modular, reliable, and versatile version of the simulator is needed. The generated ECG waveforms met the specifications of a sinus rhythm at 60 beats per minute and 20 mV peakto-peak amplitude, and the waveform morphology of an atrial fibrillation. The hardware specifications were also successfully met. Future developments will include extending the software specifications to allow for the simulation of other types of cardiac arrhythmias, as well as the ability to detect and display the response of an implantable device to a given stimulus. The purpose of the project was to develop the software and hardware needed for the new simulator to generate and display an analog sinus rhythm and atrial fibrillation electrocardiogram (ECG) waveforms. This was accomplished using a Xilinx Zedboard Field Programmable Gate Array (FPGA), a digital-to-analog convertor (DAC) integrated circuit DAC0808, a 741 operational amplifier which drives the current of the DAC output, as well as a low-pass filter to remove unwanted noise that can distort the signal. The generated analog ECG waveforms were externally detected and displayed using an oscilloscope. The output programmability was achieved through Xilinx SDK, which is an Objective C compiler. Senior Design • 7 • 2014–2015 projects • 2014–2015 Virtual Interactive Patient III projects • 2014–2015 Dynamometer for Testing of a Novel Wheelchair Wheel Project Team: Ian Novotny Mark Dimas Paul Koster Kevin Cortes Colin Liedeka Faculty Advisor: Dr. Robert Scheidt Sponsor: Salim Nasser, Rowheels S pinal Cord injury patients not only deal with the burden of limited mobility, but also find themselves at risk of repetitive strain injury due to extended use of wheelchairs. Studies have shown that people who use wheelchairs are subject to high amounts of shoulder stress that could lead to severe disability of upper extremity function. Unfortunately, the high cost of electronic wheelchairs sway people to use manual propulsion methods with the associated long-term health consequences. Rowheels seeks to address this dilemma and has designed a wheelchair that utilizes rowing-like motions to generate forward propulsion in an attempt to mitigate these health risks. The purpose of this project was to create a device that will measure the force applied by the user to the hand rim of the wheelchair, and through custom computer coding, wirelessly transmit the amount of applied torque to an off-board computer. A major design constraint was that the device should not interfere with normal use and motion of the wheelchair. This constraint allows for a more accurate representation of applied torques. To measure the applied force, strain gauges Marquette University Opus College of Engineering • were used and calibrated to set known voltages coinciding with known applied forces. Using the known radius of the hand rim, the software then transformed the measured force values into torque values. All necessary hardware machining and embedded systems programming was performed by the team. Testing to verify the design involved comparing theoretical torque calculations to the actual values found during testing. When comparing these values, the average error was around 1.4%. Use testing found that the device did not interfere with user motion and comfort. 8 • Department of Biomedical Engineering This project was supported by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. projects • 2014–2015 Biofeedback System to Improve Body Alignment Project Team: Jasmine Balangue Christopher Bauer Rebecca Heinen Krista McClure David Mysliwy Timothy Vernon MIAD Partners: Charles Martin Maddy Straka Faculty Advisor: Dr. Jack Winters Clinical Advisor: Christine Cayo T he purpose of this project was to design a biofeedback system to improve the body alignment of our client, an eleven year old girl born with Trisomy 14. She suffers from constant flexion in her lateral trunk on her right hand side, as well as torticollis causing flexion in her neck on the same side. By developing a biofeedback system to alert our client of her recurring body misalignment, she would be able to regain independence in understanding and correcting her posture without continuously relying on therapy sessions and orthotic braces. It was also important to develop a design that was discrete and non-disruptive so as not to draw unnecessary attention to her nor distract her from activities of daily living. With the implementation of the 1-sided suspender beltclip design as well as the head-clip design, both of our client’s issues with trunk misalignment and torticollis are adequately addressed. Through the use of an analog linear position transducer concealed within a sleek housing attached to our client’s hip and the free end of the linear position transducer attached to an elastic band around our client’s chest, the 1-sided suspender device produces a gentle vibration at the hip alerting her when her trunk Senior Design • translates to an angular displacement of approximately 10° to her right from vertical. The head-clip design similarly produces a gentle vibration near the client’s ear when her head displaces approximately 10° to her right from vertical, using a tilt sensor cleverly concealed within a hair clip. With the unique housings of both designs, the team was able to not only address the issue of our client’s recurring body misalignment in her trunk and head but also was able to do so in a way that was gentle enough not to disturb her and subtle enough not to alert the surrounding public. 9 • 2014–2015 projects • 2014–2015 This project was supported by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. Hand Cycle Mount to Provide Exercise for SCI Patients in Hospital Beds Project Team: Rebecca Avena Eric Holakiewicz Kevin Lang Stanko Pilipovic Devin Roach Matthew Roegner MIAD Partners: Natalie Quinnies Luis Hernandez Faculty Advisor: Dr. Brian Schmit Clinical Advisor: Linda Schweisberger, Zablocki VA Medical Center S pinal cord injury (SCI) is an injury which involves significant trauma to the spinal column and can result in partial or total paralysis. Such injuries require extensive amounts of rehabilitation and exercise, as well as periods of bed rest. During long periods of bed rest, patients may develop pressure sores, which would make moving a patient to a separate room for rehabilitation painful and even dangerous. Such occurrences usually result in longer periods of bed rest. While on bed rest, spinal cord injury patients at the Clement J. Zablocki VA Medical Center have limited access to exercise equipment. Without an opportunity to exercise, patients on bed-rest will face longer recovery times and negative health effects. Marquette University Opus College of Engineering • By stimulating the cardiovascular system and the upper body muscles, patients will reap positive benefits that aid in recovery and can reduce the length of a hospital stay. To solve this problem, the team’s clinical advisor requested a mounting device for a Monark© hand ergometer. This mounting device would allow use of the ergometer by patients on temporary or permanent bed rest, aiding in a swift recovery. The final design consists of a large bridging device capable of fitting over a hospital bed with angle adjustment capabilities. The device was constructed primarily of aluminum in order to minimize weight while providing enough stiffness for use with the ergometer. Extensive testing verified that the mounting structure is both safe and stable, and could therefore be used in a hospital environment. Furthermore, the device allows for a change in angle from 0 to 30 degrees. The swivel-locking casters and handles added to the device, ensure that the structure is simple and easy to move from patient to patient. The device can drastically increase patient access to exercise equipment, and therefore greatly reduce the length of hospital stays. 10 • Department of Biomedical Engineering This project was supported by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. Project Team: Joel Haberkorn Ryan Haberkorn Kelly Molinaro Heidi Reichert Mara Thompson Rachel Wilk MIAD Partners: Jean-Marc Bastien Shannon Ingles Faculty Advisor: Dr. Jay Goldberg Clinical Advisor: Dr. Maya Evans, Medical College of Wisconsin M otor conditions, such as cerebral palsy and arthrogryposis multiplex congenita (AMC), limit the range of motion of joints and affect muscle control. Both of these conditions can severely impact a child’s gait to the point where he or she needs a walker to ambulate. Current pediatric walkers provide support for gait only on smooth surfaces, limiting children to paved areas when outside. Commercially available walkers are not able to maneuver on alternate terrains such as grass and woodchips, which are typically found in playgrounds. position lock swivel wheels. The treaded wheels allow the walkers to traverse rough terrains. The walkers can fold flat so that they can easily fit into the trunk of a compact car to be transported. The position lock swivel casters provide maneuverability for a child with more independence and when locked, provide stability for a child who needs more support. Verification testing indicated that the walkers 1) could travel more easily on rough terrains than existing walkers, 2) were able to be folded quickly into a small enough size to be easily transported, and 3) were easily maneuvered. The purpose of this project was to design and build two pediatric all-terrain walkers for two specific clients. The walkers were required to successfully travel on rough terrains such as grass, woodchips, and rubber mulch, and be easily portable and maneuverable. The walkers have treaded robotic wheels, an easy-to-use folding mechanism, and Senior Design • 11 • 2014–2015 projects • 2014–2015 All-Terrain Walker for Improved Playground Access projects • 2014–2015 This project was supported by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. Human-Powered Nebulizer Project Team: Ghadeer Alsultan Sims Chacko Morgan Loeb Kurt Mess Zach Nelson Faculty Advisor: Dr. Lars Olson R espiratory diseases are major causes of death in many developing countries in South and Central America. The spread of these diseases are caused by air pollution and low socioeconomic status. The use of appropriate medical treatment is limited due to their expense and inadequate access to electricity. The idea of designing a human powered nebulizer started in 2004. When the project advisor traveled to Guatemala with a group of Marquette University students he found that many children with respiratory diseases were unable to afford the nebulizer due to its cost and lack of electricity. Two attachment options were designed in the process of developing the human-powered nebulizer (HPN) project: the leg-powered and hand-powered HPN. The leg powered HPN used common bicycle components. However, due to cultural constraints in El Salvador, the design did not pass the trial phase. The hand- powered HPN, which was driven manually by operating a crankshaft, can be very exhausting. independence, compatibility with the current HPN device, and fit with the cultural requirements of the potential users. A treadle design provided a solution to almost all the problems that were encountered in the previous two designs. The device was tested to ensure that the treadle design met the customer needs and target specifications. The device provides a constant flow of the inhaled drug passively using only the foot of the operator to power it. The purpose of this project was to provide an alternative option for powering the HPN. The new attachment needed to satisfy specific criteria, including low cost, ease of use, electricity Marquette University Opus College of Engineering • 12 • Department of Biomedical Engineering This project was supported by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. Project Team: Jacob Vildibill William Boswell Jack Lawinger Adam Hurrle Ryan Kammerer MIAD Partners: Peter Morris Adam Carter Faculty Advisor: Dr. Lars Olson A mong the common deficiencies in developing world medical care is the lack of reliable access to concentrated oxygen. This absence is significant as oxygen is used to treat malaria and neonatal medical problems, two major causes of death in these regions. While oxygen concentration technologies exist, they rely on the electrical grid for power which in these regions is unreliable and can lead to long periods without access to oxygen. This project involved the development of an oxygen concentration system that does not rely on electrical power. This way, medical oxygen supply to rural hospitals in poorer regions could be reliable and consistent. Correspondence with providers in these medical facilities confirmed the need for the creation of such a device. The multi-year scope of this project encompasses the creation of a system that can provide medical- grade oxygen to several patients at once. Since this project is in its very beginning stages, much of the work done Senior Design • was to prove the concept that oxygen could, in fact, be concentrated without using electricity and that the proper specifications in order to do so could be met. In both respects, this project was successful. Oxygen was successfully concentrated seven times greater than that achieved previously. The amount of pressure required to concentrate oxygen was achieved using a bike-powered compression system. This indicates great potential for future success in the creation of a non-electric solution to this global problem. After months of experimentation it was discovered that crushed, dehydrated Zeolite, with maximum surface area, could concentrate oxygen at 60 psi. Preliminary testing concentrated oxygen to over 34%. An apparatus was also constructed that connected a flywheel to a road bike. The flywheel was connected to pistons that were capable of compressing air. The compression system was capable of producing more than the required 60 psi. 13 • 2014–2015 projects • 2014–2015 NEOX: Non-Electric Oxygen Concentrator projects • 2014–2015 This project was supported by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. EMG-Controlled Hand Prosthesis Project Team: Brock Brilowski Erin Davis Nicholas Grassel Nicholas Jelacic Valay Shah Faculty Advisor: Dr. Scott Beardsley T he goal of this project was to develop a signal processing and control method that will allow realistic hand motion and individual control of the prosthetic hand digits using residual EMG signals from the forearm. Control of the human hand by the brain requires the ability to continuously manipulate multiple degrees of freedom via sensory and peripheral information. Nerves forward this information to muscles in the forearm to control the hand. A wide range of prostheses and control options are available to amputees, ranging from completely passive systems, primarily providing cosmesis, to active systems which are used for everyday activities. Active systems can either be body powered or externally powered. Body powered systems use body motion to control the prostheses while externally powered systems use EMG, or electromyography, signals and external battery power to control the prosthesis. Myoelectric prosthetic devices are some of the most promising and advanced devices on the market because of their functionality and usability. However, the devices are relatively expensive, ranging from $25,000 to $40,000, and they are hindered by the use of discrete, classification based, control methods. A control method that allows for continuous motion in the prosthetic hand digits would allow amputees to perform many tasks that they would otherwise be unable to complete using current methods. Marquette University Opus College of Engineering • The final device focused on independent control of the fingers, providing realistic hand motion using an intuitive EMG-driven control interface. The device utilizes an array of six surface electrodes, each of which is connected to an EMG shield that provides filtering and envelope functions. An Arduino Due was used to implement a nonlinear autoregressive model that used EMG signal inputs to provide real-time prediction and control of finger angle in a mechatronic hand (Roemotion, Inc.). Five servo motors were used to move each of the five fingers on the hand, and the entire system was powered by two 11.1 V lithium ion batteries. The final design was portable and provided power for 6 hours of continuous use. The controller provided a low lag time of about 30 milliseconds between receiving an EMG input and producing an output, and finger flexion speeds of up to 472.42 mm/second. The final design offers a promising solution for consumers in the field of prosthetics. The combination of an electrode array, together with an autoregressive model to predict future digit location, enables continuous and independent control of the fingers and provides an avenue for development of lowcost yet highly functional terminal devices. 14 • Department of Biomedical Engineering This project was supported by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. Project Team: Tanner Basten Casey French Maxwell Lindell William Lundin Michael Potocnik Brendan Ryan Faculty Advisor: Dr. Dean Jeutter Clinical Advisor: Dr. Christine Schindler, Marquette University College of Nursing tress induced hyperglycemia has recently become a target of interest in Intensive Care Units (ICU) across the country because of studies showing its association with increased mortality rates, especially in critically ill patients. Insulin therapy is currently used to combat hyperglycemia and induce normoglycemia which reduces the mortality rate and optimizes patient stability. As a result, all ICU patients in the United States have their blood glucose levels monitored. The blood glucose reading is taken every hour. This is done with the traditional method of pricking the patient’s finger and placing the blood sample on a test strip. The test strip is placed into a glucometer and the blood glucose level is then displayed. Next, the nurse scans the patient’s identification band, followed by her identification card, before docking the glucometer. Finally, the patient’s blood glucose level is uploaded to the patient’s electronic records. This total process typically takes an ICU nurse approximately two to three minutes. S The purpose of this project was to develop a device that streamlines the blood glucose monitoring processes currently used in the ICU. The Glusync system needed to 1) increase the testing speed without comprising the accuracy of the blood glucose readings, 2) minimize the patient anxiety that results from seeing the lance prick the Senior Design • finger, and 3) be user-friendly. The Glusync system is a two component design including a single-use disposable piece and a main body to house the hardware and blood glucose sensor. The single-use disposable piece is a 3D-printed component with an internal lancing mechanism and test strip that combined three steps in current practice: sanitizing the patient’s finger; pricking the patient’s finger; and placing the blood sample on the test strip. The disposable piece has an open cavity to insert the finger, and a mechanical pushbutton within this cavity that triggers the lance and pricks the finger. The main body is 3D-printed and is the instrument the nurse holds to administer a blood glucose test. It has a cavity for the single-use disposable piece to be inserted before each blood glucose test. The main body also houses the digital components necessary for outputting a blood glucose reading to the instrument’s LCD screen. The main body also contains the system that sends the glucose reading to the Glusync’s iPhone application in a manner that mimics a healthcare records system. projects • 2014–2015 Automated Blood Glucose Monitoring Device Verification testing of the Glusync prototype design indicated that the device does output blood glucose readings that are accurate within + 5 mg/dL of commercially available products. Additionally, the prototype reduces the time required to obtain a blood glucose reading from 2–3 minutes to an average of 27 seconds. To bring this product to market, clinical trials need to be performed in an ICU setting to verify the functionality and practicality of the Glusync system. 15 • 2014–2015 projects • 2014–2015 This project was supported by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. Enabling Use of Real Diagnostic Devices to Measure Vital Signs of Mannequins Project Team:Jerome Kolf Tomas Fandel Daniel Tournoux William Ebel Jr. Matthew Mesko Zachary McKeown Faculty Advisor: Dr. John LaDisa Clinical Advisor: Mary Paquette, Marquette University College of Nursing T he College of Nursing at Marquette University has a simulation facility where nursing students learn practical skills. The simulations need to be as realistic as possible in order to train the students properly before they work with real patients. The students use real medical equipment to evaluate high tech mannequins or hired actors. There are a few vital signs that the mannequins and actors are still unable to simulate. The most critical of these is temperature. In current simulations, temperature is simulated by placing a note on the thermometer or by announcing temperature changes verbally. Another vital sign that is critical for simulations is blood pressure. In current simulations, the blood pressure of patients (typically actors) is not able to be simulated to any desired value. The simulation is only able to use the actual blood pressure of the patient (actor). pressure from the lab simulation control room while nursing students were participating in clinical simulations. The devices also had to wirelessly communicate with the control room, and have the same look and function as the normal devices used in a real clinical setting. Trial simulations were performed with the completed devices and the clinical simulation staff to verify they functioned as needed. The devices will be used and further evaluated over the next year to enhance the learning environment for all Marquette Nursing students. The purpose of this project was to provide a new thermometer and blood pressure cuff to further enhance the Marquette College of Nursing lab simulations. The devices were required to receive an input of a temperature or blood Marquette University Opus College of Engineering • 16 • Department of Biomedical Engineering This project was supported by R25 EB013070 from the National Institute of Biomedical Imaging and Bioengineering. Project Team: Daphne Gutierrez Criselda Harsono Richard Schroeder Miguel Sotelo Kelly Vonderhaar Faculty Advisor: Dr. Scott Beardsley harcot-Marie-Toothe (CMT) disease is a genetically acquired peripheral neuropathy that destroys the myelin sheath around the peripheral nerve cells. As a result, muscles at the extremities do not receive the electro-chemical signals from the central nervous system and eventually atrophy. This has consequences on the gait cycle. Drop foot is a gait abnormality that results from weak or non-existent dorsi-flexor muscles and is a common symptom of CMT disease. Drop foot can result in the person tripping, or eliciting their knee and hip flexors to compensate for lost range of motion, which increases energy expenditure. Current solutions for individuals with muscle atrophy include passive ankle-foot orthoses (AFOs). These solutions dorsi-flex the ankle at all times. However, by applying all of the dorsi-flexor moment, the user cannot exercise their muscles and therefore their muscles continue to atrophy. Active AFOs have been developed for research, however, the systems are often large and heavy. C The purpose of this project was to develop an active AFO that provided dorsiflexion only during the swing phase of the gait cycle. The device was developed to provide stability during the stance phase and mimic the range of motion during the swing phase. The use of low torque motors to provide compensatory movement about the ankle resulted in a lightweight AFO that provided compensatory lifting of the foot while also Senior Design • engaging the remaining force generation capability of the users’ muscles. The solution was developed to prolong the onset of atrophy. The active AFO consists of custom-made pulleys which couple the torque created by servomotors (one on each medial-lateral side of the ankle) to the tension propagators (high-tension strings). The custom-fit AFO shell is made of polypropylene with an inner foam lining for added comfort. Two forcesensing resistors detect the phase of the gait cycle, and a flex sensor detects the ankle angle. An Arduino was used to control the servomotors and continuously adjust the ankle based on location in the gait cycle as measured by the external sensors. projects • 2014–2015 Active Ankle Foot Orthosis Testing confirmed that the device dorsiflexes the ankle at the correct times of the gait cycle at a speed that is consistent with the user’s gait cycle. Although the AFO was wider about the leg compared to commercial passive AFOs, it was less bulky than current active AFOs. Further testing across a range of ambulation speeds is needed to validate the robustness of the system. 17 • 2014–2015 department of biomedical en B iomedical Engineering is a discipline that advances knowledge in engineering, biology and medicine to improve human health. Students in biomedical engineering participate in cross-disciplinary activities that integrate the engineering sciences with the biomedical sciences and clinical practice. Biomedical engineers develop strategies to effectively solve challenging problems in medicine and biology. Most graduates secure employment working in the medical device/biotechnology industry. Some graduates use our “renaissance” training as a stepping stone for careers in fields such as medicine, law, healthcare management, and academics. Distinctive Features of Biomedical Engineering at Marquette University Marquette’s Department of Biomedical Engineering is the largest at a Catholic university, larger than all others combined at both the Marquette University Opus College of Engineering • undergraduate and graduate levels, and one of two such accredited programs. The program has strong linkages with the Medical College of Wisconsin (MCW), Zablocki Veteran’s Administration Medical Center, and the Rehabilitation Institute of Chicago, and manages a number of Centers including the Orthopaedic Rehabilitation and Engineering Center (OREC), the Falk Neurorehabilitation Engineering Research Center and the Rehabilitation Engineering Research Center on Accessible Medical Instrumentation. The department has unique laboratory capabilities including CT and SPECT microfocal imaging, biotelemetry, implantable devices, telerehabilitation, and neurorehabilitation robots, in areas including neurorehabilitation, imaging systems, and cardiovascular technologies. Marquette’s Biomedical Engineering department offers degrees at the bachelors, masters and doctorate levels. 18 • Department of Biomedical Engineering ngineering Co-op and Internship Program Marquette University has developed one of the leading co-op/internship programs among Biomedical Engineering Departments in the nation. Seventy percent of the undergraduate biomedical engineers gain co-op or internship experience before graduation. The Biomedical Engineering department has forged partnerships with many major medical device companies in the Midwest who rely on the excellent reputation established by our students as co-ops, interns and permanent employees. The Co-op and Internship Program offers students the opportunity to gain meaningful practical and professional experiences in the health care industry, in addition to their on-campus educational experiences. completed at the Food and Drug Administration, Office of Science and Technology in Rockville, MD. Marquette University began its Engineering Co-op Program in 1919. Students usually enter the Co-op program at the end of their sophomore year and complete three to four terms of offcampus employment. The employment experience is alternated with semesters of on-campus study, extending graduation by only one year. Internships, in comparison, are summer only engineering experiences. Undergraduate Offerings Les Aspin Center for Government (FDA Internships) The Les Aspin Center for Government at Marquette University and the Department of Biomedical Engineering offer internships on biomedical research and regulatory issues. The Les Aspin/Biomedical Engineering Internships began in 1997 with Biomedical Engineering undergraduates participating in this innovative program in Washington, D.C. To date, more than 100 biomedical engineers have completed Les Aspin Biomedical Internships. The internships are All undergraduate tracks in Biomedical Engineering are compatible with other programs offered by the Opus College of Engineering. Each track contains the requisite humanities courses, and requires 132 credit hours for graduation. Students automatically earn a minor in biology, and can earn an optional minor in areas such as mathematics, electrical, mechanical, or computer engineering. In addition, all tracks retain most of the core courses of the initial year, which allows the student flexibility to transfer to other curricula if so desired. Choose from Three Specializations The Biomedical Engineering Program at Marquette offers a strong undergraduate education. There are three tracks in the Biomedical Engineering curriculum: • Bioelectronics • Biomechanics • Biocomputing Senior Design • 19 • 2013–2014 The Biomedical Engineering curriculum is interdisciplinary in nature, incorporating courses in biology, chemistry, physics, mathematics, computer science and engineering. We provide a solid foundation in the mathematical, physical, and life sciences necessary for the engineer to function effectively in a medically or biologically oriented problem solving environment. Social science and humanities courses prepare students to deal with contemporary ethical, cultural, and social issues. In addition, we prepare biomedical engineers to communicate with life scientists, physicians and other health care providers to describe and model complex biological systems, collect and analyze experimental or clinical data, understand the capabilities and limitations of sophisticated instrumentation, and understand the principles of design. Undergraduate Design Curriculum Biomedical engineering students at Marquette University learn about design throughout the four year curriculum. Freshman Year: Students first gain experience with the design process in the freshman year during BIEN 1100 and 1110 (Introduction to Biomedical Engineering Methods I and II). In these courses, they participate in several team design challenges such as • Physiological monitoring: Design of an algorithm for analysis of ECG, blood pressure, and other waveforms • Medical imaging: Design and testing of an imaging phantom • Biomaterials/Biomechanics: Design of a wound care material • Entrepreneurship: Design of a medical device, includes elevator speech, business plan, and oral presentation to potential student investors/fellow classmates These experiences help develop teamwork skills, and teach students about the engineering design process, including technical, legal/ethical, regulatory, and economic design constraints. Students learn to identify customer needs, develop a list of performance requirements and specifications, convert requirements into design concepts, and build and test prototypes. At the end of BIEN 1110 students learn about basic business concepts and entrepreneurship followed by a team-based design project in which teams try to sell their new product ideas to potential student investors (The Business of Biomedical Engineering). Marquette University Opus College of Engineering • 20 • Department of Biomedical Engineering Sophomore and Junior Years: During the sophomore and junior years of the biomedical engineering curriculum, students take courses that include individual and team-based design projects which allow them to apply what they are learning in the course to the solution of a related problem. This helps them relate theory with practice. In the junior year, students can take BIEN 3400 Clinical Issues in Biomedical Engineering Design, an elective in which students observe procedures in the clinical environment and learn to identify unmet clinical needs and opportunities for new product development. Their final project proposals can serve as the basis of their senior capstone design projects. Senior Year: During the senior year, students are required to take BIEN 4920 Principles of Design and BIEN 4998 Senior Design. These courses require students to apply what they have learned during their previous years of the undergraduate curriculum in a multidisciplinary team-based project experience. They further develop their design, analytical, project management, communication, time management, and teamwork skills. They learn about the product development process, the medical device industry, testing for safety and efficacy, design validation, standards and regulations, risk management, project scheduling, patent issues, and a variety of design issues. Students complete a design project from problem definition to design validation (per ISO 9001 and 13485) and gain experience in generating the same project deliverables as required in industry. Five Year B.S./M.S. Program This program allows qualified students to receive a Bachelor of Science Degree and a Master of Science Degree in Biomedical Engineering in just five years. Students with qualifying grade point averages apply to the program during their Junior year. They begin their thesis research the summer between their Junior and Senior years, and continue their research during the summer between their Senior and fifth years and throughout their fifth year, culminating in the preparation of a written thesis and defense. Research in Biomedical Engineering BIEN faculty and students at Marquette are engaged in a wide range of research activities, with many opportunities available for students at both the graduate and undergraduate levels. Research-oriented Faculty More than 60 faculty who are active in research have primary (12), secondary (10), or adjunct (43) appointments in our department, and are available for supervision or co-supervision of students. Senior Design • 21 • 2014–2015 Research Laboratories and Centers The number of research laboratories and centers within our department has been growing dramatically, with the BIEN department now housing ten research laboratories and three centers. Most recently, the NIDRR awarded our department a Rehabilitation Engineering Research Center on Technologies for Children with Orthopedic Disabilities (TECH4POD). Faculty, students, clinicians, and researchers from six area institutions are developing a national center with a focus on advancing engineering research and development based on innovative technologies addressing children with orthopedic disabilities. Externally Funded Research More than $3 million/year in externally funded research, the largest of any department on campus, flows through the Department of Biomedical Engineering (BIEN). Research and training grants are managed by BIEN core faculty and support research projects for 45 graduate students. Additionally, other graduate students are funded through projects led by BIEN adjunct faculty whose primary appointment is at The Medical College of Wisconsin (MCW) or the Zablocki Veterans Affairs Medical Center. Strong Partners We are a member of the Clinical and Translational Science Institute of Southeast Wisconsin. Supported by a $20M grant from NIH, this consortium of eight Milwaukee institutions is dedicated to transforming biomedical research in southeast Wisconsin, accelerating the translation of research Marquette University Opus College of Engineering • discoveries, and advancing patient care and education. The eight member organizations include the Medical College of Wisconsin, Marquette University, Milwaukee School of Engineering, University of Wisconsin-Milwaukee, BloodCenter of Wisconsin, Children’s Hospital and Health System, Froedtert Hospital, and the Clement Zablocki VA Medical Center. Targeted Areas of National Leadership While our students and faculty are engaged in many areas of research, three areas of excellence stand out: Functional Imaging, Rehabilitative Bioengineering, Systems Physiology, and Biocomputing. Department of Biomedical Engineering Mission Statement The Department of Biomedical Engineering is a dedicated team committed to the Jesuit tradition of the pursuit of truth. We develop leaders and problem solvers skilled at applying engineering, science and design principles to improve health in the service of humanity by: • Discovering and disseminating new knowledge • Providing excellent undergraduate and graduate education • Promoting critical thinking and lifelong learning • Guiding students to meaningful and ethical professional and personal lives • Fostering interdisciplinary and collaborative research and education through academic and industrial alliances • Continuing innovative leadership in education, research and industrial relationships • Inspiring faculty and students to serve others • Valuing diversity and uniqueness of the individual 22 • Department of Biomedical Engineering faculty Olson, Lars E., Ph.D. Associate Professor and Interim Chair. Optical instrumentation, tissue engineering, biological transport and circulation physiology, mathematical modeling of physiological systems, biosensors Audi, Said H., Ph.D. Pulmonary mass transfer, tracer kinetics, pulmonary hemodynamics Beardsley, Scott, Ph.D. Neuroengineering, computational modeling, perceptual learning, functional imaging Gilat-Schmidt, Taly, Ph.D. Medical imaging, image processing and reconstruction, systems engineering Goldberg, Jay R., Ph.D., P.E. Director, Healthcare Technologies Management Program Harris, Gerald F., Ph.D. Quantitative assessment of neuromuscular function, human motion analysis, orthopedic biomechanics, data acquisition and control, real time analysis LaDisa, John F., Jr., Ph.D. Cardiovascular biomechanics, adult and congenital heart disease, stent design and development Jeutter, Dean C., Ph.D., P.E. Implantable transcutaneous radio frequency power transfer, biotelemetry, biomedical instrumentation, radio frequency circuit design and development Ropella, Kristina M., Ph.D Professor and OPUS Dean Signal processing, cardiac and neuro-electrophysiology, functional magnetic resonance imaging Scheidt, Robert A., Ph.D. Human motor control, systems identification, rehabilitation engineering, embedded systems, product development Schmit, Brian D., Ph.D. Spinal cord injury, human neurophysiology, neurorehabilitation, instrumentation, biomechanics Silver-Thorn, M. Barbara, Ph.D. Prosthetic limbs, soft tissue mechanics, rehabilitation engineering, orthopaedic and dental biomechanics Winters, Jack M., Ph.D. Neuromuscular control systems, movement and tissue biomechanics, rehabilitation engineering, telehealth, neurofuzzy computing Senior Design • 23 • 2014–2015 Associate Faculty Cariapa, Vikram, Ph.D. Rapid prototyping, process controls, neural networks, design of experiments Clough, Anne V., Ph.D. Mathematical and computer modelling of biomedical systems, image processing and analysis, modeling of pulmonary hemodynamics, integral equations Josse, Fabien J., Ph.D. Biochemical sensors, acoustics, acousto-electronic devices Krenz, Gary S., Ph.D. Mathematical modeling of hemodynamic properties of the lung, microangiographic measurements, pulmonary vascular morphogenesis Marklin, Richard W., Ph.D. Ergonomics in office and industrial settings, human factors, cumulative trauma disorders Nagurka, Mark L., Ph.D., P.E. Biomechanics, vehicle dynamics and controls, and control system design Voglewede, Phillip A., Ph.D. Lower limb prostheses, dynamics, kinematics OPUS COLLEGE OF ENGINEERING S ince 1908, the Marquette University Opus College of Engineering has been uniquely blending professional engineering preparation with a liberal arts education to provide the world with well-balanced leaders in their profession. Our Mission The mission of the College is to excel in four critical areas: • To prepare all students for successful careers based on a strong moral and ethical foundation • To advance the state-of-the-art in engineering • To serve our professional and technical communities • To contribute to our global society The Opus College of Engineering offers six undergraduate degrees in eleven programs/majors through four departments: Biomedical Engineering; Civil & Environmental Engineering; Electrical and Computer Engineering; and Mechanical Engineering. Marquette also offers a wide range of graduate and doctoral programs. Accreditation All undergraduate programs offered by the Marquette University Opus College of Engineering are accredited by the Engineering Accreditation Commission of ABET, 111 Market Place, Suite 1050, Baltimore, MD 21202-4012, 410-347-7700. The University Founded in 1881 in Milwaukee, Wisconsin, Marquette University has been educating people of faith to be leaders in their professional lives, their communities and in society for more than 120 years. Since the first graduating class of five men were awarded bachelor of arts degrees in the 1880s, Marquette has grown into a modern coed campus of more than 11,000 students who learn and grow through nationally admired undergraduate, graduate and professional programs. Opus College of Engineering Department of Biomedical Engineering P.O. Box 1881 Milwaukee, WI 53201-1881 www.marquette.edu/engineering/biomedical 150/TFC/07-15