LAB #10
advertisement

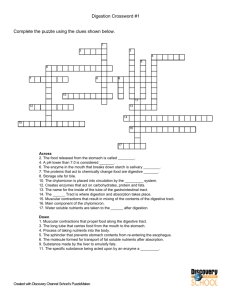
Biology 242 – Lab LAB #10 (10th/19 Lab Sessions for Winter Quarter, 2008) TOPICS TO BE COVERED: »Introduction to Structures of the Digestive System: the GI Tract and Accessory Organs »Demonstration of Dissection techniques »Use of Anatomical Models for identification of Digestive System structures DESIRED OUTCOMES: After completing the activities described for this lab session, students should: »Be able to identify all digestive system anatomy on lab models, charts, and dissection specimens. »Be able to identify the histological structuare of the various digestive organs. »Be familiar with the major layers/tissues of the digestive tract structures and these are modified in each region of the tract »Be able to tract the secretion of bile from the liver to the duodenum, naming each structure through which the bile passes on this journey. MATERIALS NEEDED: »Anatomical models including Mandibular hemisection showing dentition, Stomach, Small Intestine, Torsos and all removable parts, Stomach with Pancreas, Tooth, and various X-rays of GI series »Cats »Dissection Pans »Dissection Tools »Wall Charts of Digestive System »Skulls – with dentition intact »Photographic Atlas, Ch. 15 Activity #1: Introduction to Structures of the Digestive System The Digestive System functions in processing food into usable forms for cellular respiration. The major processes include: (1) ingestion of food into the mouth; (2) secretion of watery substances into the lumen of the tract containing acids, buffers, and enzymes; (3) mixing an propulsion of food through the digestive tract; (4) digestion of food by mechanical and enzymatic (chemical) activities; (5) absorption of nutrients into the blood; and (6) defecation (formation and elimination) of indigestible material and waste products. To accomplish these functions, the digestive system is highly specialized. Food passes through a tubular digestive tract extending from the mouth to the anus, and each organ of the tract has a specific function in the digestive process. In addition, accessory organs of digestion occur outside the digestive tract. The salivary glands, liver, gallbladder, and pancreas manufacture and squirt enzymes, hormones, and other compounds onto the inner lining of the digestive tract. See Figure 15.1 of your Photographic Atlas (Note that food does not pass through the accessory organs of the digestive system.) To begin a discussion of the anatomy of the Digestive Tract, examine the inside of your cheek with your tongue. What do you feel? The mucosal layer lining your mouth and the rest of your digestive tract is a mucous membrane that is kept wet. Glands drench the lining epithelium with enzymes, mucus, hormones, pH buffers, and other compounds to orchestrate the step-by-step breakdown of food as it passes through each region of your digestive system: mouth, pharynx, esophagus, stomach, small intestine, large intestine, and finally, rectum. Four major tissue layers compose the digestive tract: the mucosa, submucosa, muscularis, and serosa (aka adventitia). Although this basic histological structure of the tract is similar along its entire length, each region has anatomical specialization reflecting that region’s role in the digestive process. (Figures 15.40 and 15.42) Biology 251 – LAB #10 – continued Page Two The mucosa lines the digestive lumen and is in contact with the food being pushed through the tract. Three distinct mucosal layers can be identified: (1) the digestive epithelium, (2) a sheet of connective tissue called the lamina propria, and (3) a thin smooth muscle layer: the muscularis mucosae. The digestive epithelium is the only layer exposed to the lumen of the tract. From the mouth to the esophagus, the digestive epithelium is stratified squamous epithelium, protecting the muscosa from abrasion during swallowing. The stomach and small and large intestines are lined with simple columnar epithelium. Food in these regions of the tract is liquid and therefore is much less abrasive to the digestive epithelium. Beneath the digestive epithelium is the lamina propria, a layer of connective tissue that attaches the epithelium and contains blood vessels, lymphatic vessels, and nerves. A thin layer of smooth muscle, the muscularis mucosae, is the the outermost layer of the mucosa. This layer of smooth muscle creates tone and tension within the lamina propria to support the huge folding of the mucosa – as in the villi of the small intestine or the rugae of the stomach, etc. Without this tone, the folds of mucosa would collapse and the overall surface area of the inner layer of each region would be markedly diminished. Superficial to the mucosa is the submucosa, a thick layer of loose connective tissue layer containing large blood and lymphatic vessels and numerous nerve as well as the submucosal glands. Between the submucosa and the adjoining superficial layer of the muscularis (externa) is a network of the sensory and autonomic nerves, the submucosal plexus (aka plexus of Meissner), that controls the tone of the muscularis mucosae, and sends signals for glandular secretion. Surrounding the submucosa are several layers of smooth muscle tissue in the muscularis (sometimes called the muscularis externa. We will refer to it merely as the muscularis.) The inner layer is circular muscle that wraps around the digestive tract, causing the tract to narrow, or constrict its lumen, upon contraction. The outer layer is longitudinal muscle with myofibers oriented parallel to the length of the tract. (The stomach also has a third layer of smooth muscle: the middle oblique layer. It is the only region of the digestive tract whose muscularis consists of three layers of smooth muscle.) Contraction of this layer of muscle shortens the tract. Together, both layers of the muscularis contract and relax to move and process materials in the digestive tract. Between the two muscle layers, is the myenteric plexus (aka plexus of Auerbach), nerves that control the activity of the muscularis. The superficial layer of the digestive tract is the serosa (aka adventitia), a loose connective tissue overlain by a simple squamous epithelium, forming a covering that attaches and holds the tract in position as well as secreting a serous fluid that acts as a lubricant for all the “moving parts” that are packed into the peritoneal cavity. As you already know, the serosa is modified into peritoneal folds, the various mesentery. (Please review these.) The structures you’ll need to know are into grouped into upper digestive tract and lower digestive tract: A. The Upper Digestive Tract Structures: 1. The mouth, or oral cavity, is the beginning of the one-way human digestive tract. Locate these features: Lips (there are labial frenula for both the upper and lower lips) Buccinator muscle – muscle that forms most of the cheek walls Tongue – mass of skeletal muscle covered with mucous epithelium containing taste buds; the lingual frenulum is a fold of tissue anchoring its underside to the floor of the mouth. Hard palate – anterior, boney portion of the mouth’s roof Soft palate – posterior, soft portion of the mouth’s roof (it ends in the conelike, midline uvula) *Palatine tonsils – lymphatic structures on the posterior, lateral aspect of the mouth cavity (between the anterior palatoglossal arch and the posterior palatopharyngeal arch). These tonsils are rereferred to as “the tonsils” *Lingual tonsils – lymphatic structures on the posterolateral aspect of the tongue *Pharyngeal tonsils – lymphatiac structures in the midline of pharyngeal roof (behind the soft palate) These tonsils are referred to as “the adenoids”. (*Three sets of tonsils are collectively referred to as Waldeyer’s Ring, protecting the oral cavity immunologically. ) Biology 251 – LAB #10 – continued Page Three 2. The 32 teeth of the normal adult are special features of the mouth cavity. Identify these tooth types in a skull or model (each type has a representataive on each side, left and right, of each jaw, maxillary and mandibular .) Incisors – central and lateral cutting teeth Canine – tearning tooth First and Second Premolars – tearing and cutting teeth; each with two cusps (but may have three, that is why they should NOT be referred to as “bicuspids”) First, Second, and Third Molars – grinding teeth with three flattened cusps Now find each of these features on a sectioned tooth or tooth model: Crown – superior portion of the tooth covered by enamel Neck – narrow portion where the crown joins the root Root – portion of the tooth within the alveolus, or space, of the mandible/maxillae. The root is covered with cementum Pulp cavity – central space of the tooth filled with pulp, which is a specialized connective tissue with nerves and blood vessels. Dentin – hard, calcified tissue that forms the bulk of the tooth itself. Populated by living cells called odontoblasts, dentin can and does repair itself once injured. Enamel – hardest of all human substances (not truly “a tissue” since it contains no living cells; it is considered a secretory product, produced by ameloblasts (enamel cells) that die once the tooth has erupted into the oral cavity.) Enamel is a nonliving, mineralized substance that covers the dentin of the crown. Periodontal membrane – fibrous lining of the alveolar walls (Sharpey’s fibers, collectively referred to as the periodontal ligaments project from this membrane to the root of the tooth, keeping it in place.) 3. The salivary glands are exocrine glands whose ducts empty into the oral cavity. Saliva, produced by the glands is a liquid solution (referred to either as serous = watery, or mucus = more viscous) containing mucus, mineral ions, and digestive enzymes. Identify these three pairs of major salivary glands on a torso model: Parotid glands – the largest pair, just anterior to each ear, each secretes a serous (watery) solution that flows through a duct (Stensen’s duct) piercing the masseter muscle and leading to the cheek wall across from the second maxillary molar. Submandibular glands – medial to the angle of the mandible, these glands produce mostly serous fluid and some mucous fluid. Their ducts (Wharton’s duct) empty onto the floor of the mouth, just lateral to the lingual frenulum. Sublingual glands – smallest pair of salivary glands in the floor of the mouth, they produce mostly mucous fluid, which flows into the mouth through 10 or more small ducts (Bartholin’s ducts) in the floor of the mouth. There are several groups of minor salivary glands: lingual, labial, buccal, and palatine. These are microscopic aggregates of salivary acini scattered throughout the oral cavity. The ones specifically associated with the circumvallate papillae on the posterior 1/3 of the tongue are called von Ebner’s glands. 4. The pharynx, or throat, is divided into three regions: Nasopharynx – that part of the pharynx posterior to the nasal cavity; the passage from the nasal cavity into the nasopharynx is called the choanae (aka internal nares) Oropharynx – that part of the pharynx posterior to the oral cavity; the passage from the Ooal cavity into the oropharynx is called the fauces Laryngopharynx – that part of the pharynx posterior to the larynx 5. The esophagus is a long, muscular tube connecting the pharynx to the stomach. Upper and lower esophageal sphincters are represented in the models in our lab. Biology 251 – LAB #10 – continued Page Four 6. The stomach is a dilation of the digestive tract just inferior to the diaphragm, at the end of the esophagus. These are the parts of the stomach that you should identify: Cardiac region – region immediately surrounding the opening from the esophagus into the stomach Fundus – region of the stomach superior to the opening from the esophagus into the stomach; it is the “blind, cul-de-sac” portion of the stomach. Body – Main portion of the stomach, forming a greater curvature along the left border and a lesser curvature along the right border. Pyloric region – portion of the stomach near the pyloric opening into the small intestine and the pyloric sphincter that surrounds the opening. Rugae – large folds of the mucosa oriented obliquely downward which serve to increase the surface area of the stomach lining and also to channel the contents, once liquefied, down toward the pyloric antrum and pyloric sphincter. B. The Lower Digestive Tract Structures: 1. The small intestine is a long, narrow, convoluted tube whose folds fill a large portion of the abdominal cavity. Find these features of the small intestine: Duodenum – short (≈10 inches), C-chaped beginning portion of the small intestine. Jejunum – long (≈10 feet) middle portion of the small intestine. Ileum – very long (≈20 feet) terminal portion of the small intestine. Common bile duct – duct that empties into the duodenum at the major duodenal papilla. (See also: Biliary Tree discussion in #2 below.) Ileocecal junction – junction of the ileum with the large intestine, featuring an ileocecal sphincter and a one-way ileocecal valve. The Mesentery – double reflection of the serous peritoneum that suspends the convolutions of the Entire small intestine from the posterior abdominal wall (except for the middle 1/3 of the duodenum – which is retroperitoneal), allowing it to move about, but still remain “in position”. 2. The liver, a large gland in the superior right abdominal cavity which has myriad distinct functions, one of which is to produce bile that is secreted into the duodenum. Two **hepatic ducts (R + L) conduct bile from the liver and fuse to form a *common hepatic duct. The common hepatic duct joins the two-way *cystic duct from the gallbladder (just inferior to the liver) to form the *common bile duct. The common bile duct empties into the duodenum at the major duodenal papilla. (Structures preceeded by the * are collectively referred to as the Biliary Tree.) 3. The gallbladder (aka cystic gallbladder) – a small pouch, located inferior to the liver, that stores and concentrates bile and empties by means of the two-way cystic duct. 4. The pancreas is a gland cradled in the “C” of the duodenum that is both an endocrine and an exocrine organ. Its endocrine portion (1% of the mass of the pancreas – in discrete aggregates called Islets of Langerhans) produces hormones that regulate blood glucose concentrations, and glucose catabolism; its exocrine portion (99% of the mass of the pancreas) secretes digestive fluids including enzymes which aid in catabolism of all food molecules (carbohydrates, lipids, proteins, and nucleic acids), buffering ions, and other substances. Exocrine pancreatic secretions flow through the main pancreatic duct (aka Duct of Wirsung) that joins the common bile duct emptying into the middle 1/3 of the duodenum at the major duodenal papilla. (There is also an accessory pancreatic duct (aka Duct of Santorini) that opens by itself into the middle 1/3 of the duodenum. ) 5. The large intestine, or more commonly called the colon, includes these features: Cecum – a blind sac extending inferiorly from the ileocecal junction; attached to the posterior wall of the cecum is a narrow, worm-like blind sac called the vermiform appendix. (The appendix is stabilized by its own mesentery called the mesoappendix.) Biology 251 – LAB #10 – continued Page Five Ascending Colon – the portion situated in the right lateral gutter of the abdominal cavity and in whose lumen the products of digestion are being moved in an upward direction; held in place by the mesocolon. Hepatic Flexure – the genu (or turn) anteriorly and to the left that the colon makes due to encountering the mass of the liver which prevents it from going up any further. Transverse Colon – the portion which traverses from right to left across the abdominal cavity until it reaches the spleen. This section is held in place by the mesentery known as the transverse mesocolon. Splenic Flexure – the genu posteriorly and inferiorly that the colon makes due to encountering the mass of the spleen, which prevents it from travelling any farther to the left. Descending Colon – the portion situated in the left lateral gutter of the abdominal cavity and in whose lumen the products of digestion are being moved in a downward direction; this portion is held in place by the mesocolon. Sigmoid Colon – the “S” shaped portion of the colon in moving from the left lateral gutter back toward the right to align itself in the midline. Rectum – short, straight, muscular tube at the end of the sigmoid colon. Anal canal – short (≈1 inch), muscular canal at the end of the rectum that exits to the outside of the body by way of the anus; it features a smooth muscle internal anal sphincter at its superior end and a skeletal muscle external anal sphincter at its inferior end. Also of note: The longitudinal layer of the colon’s muscularis is not continuous; that is, it is interrupted into three bands of muscle called the teniae coli; the tone/tension in these cause outpouchings of the colon called haustra. The exterior aspect of the colon wall has fatty attachments called epiploic appendages. 6. The organs and inner wall of the abdominal cavity are covered with a serous membrane called the peritoneum. The reflection of this serous membrane that covers the organs is called the visceral peritoneum, and the reflection that lines the cavity walls is called the parietal peritoneum. Two (or, in one case, four) extensions of the peritoneum that are neither visceral nor parietal occur at various locations and are called mesenteries. Locate the: Greater Omentum – four layers of peritoneum that connect the stomach’s greater curvature to the transverse colon and posterior abdominal wall. It has a long, fatty, double fold that forms an apronlike pocket called the omental bursa over the front of the viscera. Lesser Omentum – two folds of peritoneum that connect between the liver (and diaphragm) and the lesser curvature of the stomach. Unlike the two folds of other mesenteries that “fuse together”, the two folds of the lesser omentum do NOT fuse together. They remain separated by the large size and number of structures that enter and exit the porta hepatis. Falciform Ligament – double fold of peritoneum that encompassed the umbilical vein fetally; but now in the adult has the ligamentum teres at its leading edge. This mesentery divides the liver into its two principal lobes – a large right lobe and a smaller left lobe; and it helps anchor the liver to the anterior abdominal wall. Activity #2: Demonstration of Dissection Techniques Since you will be viewing the structures of the Digestive System in your cat specimen, your Instructor will give you several pointers as to how best to proceed with your dissection. It is especially “tricky” to view the pancreas and its ducts, the porta hepatis with its intricate anatomy, and several other structures. Thus, be sure to pay close attention to the demonstration in today’s lab session. Biology 251 – LAB #10 – continued Page Six Activity #3: Identification of Digestive System Structures on Anatomical Models After you have visualized the structures of the Digestive System in your cat, please make use of Mr. Torso models, the stomach model, the stomach with pancreas in situ model, and all the other anatomical models on which to quiz each other about the names of the structures, their functions, and their relationships to other digestive system anatomy and physiology. Make up as many “practice practical exam” questions as you can – for your own team-members as well as for other teams.