-
advertisement

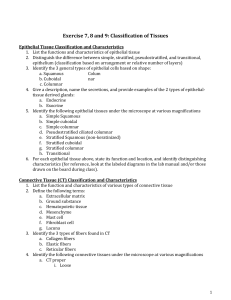
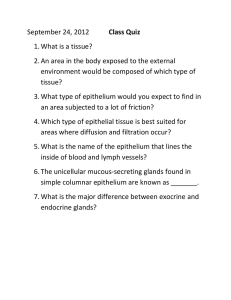
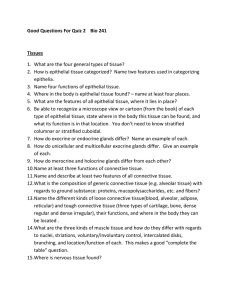
Lecture Notes: Unit I: Organization of the Human Body Chapter Four - The Tissue Level of Organization I. Introduction A. Tissues are groups of identical (or similar) cells that have formed an aggregate and have special ized for a particular function. B. Histology is the study of tissues C. Pathology is the science that recognizes when tissues are diseased and assists physicians with the diagnosis of these diseases. II. General Tissue Types A. Four principle types of tissues found in the adult human being: 1. Epithelial Tissue (Epithelia) - covers body surfaces, lines hollow organs, body cavities, and ducts and all glands are derived trom epithelial tissue. 2. Connective Tissue - connects (anchors) one tissue type to another; protects and supports the body and its organs; binds organs together, stores energy reserves as fat; and pro vides immunity. 3. Muscle Tissue - responsible for movement and generation of force via contraction 4. Nervous Tissue - initiates and transmits action potentials (nerve impulses) that help co ordinate body activities. B. Four primary germ layers of the eq1bryo give rise to adult tissues: 1. Ectoderm - outermost layer of the developing embryo which gives rise to the skin and Nervous tissue. 2. Neurectoderm - certain ectodermal cells trom the neural plate (called neural crest cells) which migrate and become specialized as melanocytes, dental tissue cells (those cells that produce enamel, dentin, cementum, and pulp), and parts of the face. 3. Mesoderm - middle layer of the developing embryo which gives rise to muscle and con nective tissues. 4. Endoderm - innermost layer of the developing embryo which gives rise to epithelium of the digestive system III. Cell junctions (points of contact between adjacent plasma membranes of most epithelial cells and amongst some muscle and nerve cells.) A. Tight junctions - form fluid-tight seals between cells such as epithelial cells lining the digestive system and the urinary bladder. B. Adherens junctions - consist of a plaque structure on the inside of plasmalemma anchored by microfilaments; transmembrane glycoproteins embed in the plaques of adjacent cells crossing the intermembrane space but not "pinching" it off. These are essentially lateral attachments that help epithelial surface cells to resist separation one from the other. C. Desmosomes - composed of plaques and are linked by transmembrane glycoproteins that cross and eliminate the intercellular gap because the adjacent cells' cytoskeletons are now aligned. These are numerous in epithelial cells of the epidermis and between cardiac muscle cells (heart). D. Hemidesmosomes - connect one cell to extracellular material such as the basement membrane. E. Gap junctions - allow cells in a tissue to rapidly communicate through connexons, transmem brane fluid-filled channels that run between adjacent cells such as are found between nerve-tonerve cells, or nerve-to-muscle cells, or nerve-to-glandular cell synapses. IV. Epithelial Tissue A. General features of all epithelial tissues 1. Arranged in "sheets" or layers of cells, either a single layer or multiple layer. 2. Consists of closely and densely packed cells with little or no extracellular substance. 3. Contains many cell junctions providing very secure attachments amongst cells. 4. Epithelial cells (and therefore epithelia) have an apical surface (free surface) and a basal surface (aattached to the basement membrane) 5. Epithelia are avascular (no blood capillaries are present); exchange of materials between epithelia and adjacent connective tissue is by diffusion. 6. Epithelia adhere firmly to adjacent connective tissue via a thin, extracellular structure, the basement membrane. (Note: the basement membrane's upper layer is secreted by the overlying epithelial cells and the basement membrane's lower layer is secreted by the underlying connective tissue cells. Although both tissue types contributeto the basement membrane. it belongs to the epithelial tissue.) 7. Epithelia have a nerve supply 8. Epithelia have a high capacity for regeneration and renewal (cells are highly mitotic) B. Classification of Epithelia is based upon two criteria: Cell Shape and Number of Layers 1. Cell shapes: a. Squamous - flat cells ("squame" is Greek for "jishscale") b. Cuboidal - cube-like cells with height, width, and depth nearly equal. c. Columnar - column-like cells (height is greater than width or depth) d. Transitional- variable shape from squamous (flat) to balloon (rounded) 2. Number oflayers: a. Simple - a single layer of cells b. Stratified - two or more layers of cells (can be up to 80 layers) a. Pseudostratified - truly only one layer of columnar cells 3. Modifications: b. Transitional - several layers of cells whose apical-most layer changes from rounded to squamous (Found only in the urinary bladder) C. Specific Types of Epithelia 1. Simple squamous epithelium: a single layer of squamous cells a. Adapted for diffusion and filtration b.Found in the body subject to little wear and tear c.Examples: Endothelium -lines the heart and all blood vessels; Mesothelium -lines the thoracic and abdominopelvic cavities and covers the organs within them 2. Simple cuboidal epithelium: a single layer of cuboidal cells a. Performs functions of secretion and absorption b. Many glandular structures are arranged into spherical units called acini. Each acinus is lined with simple cuboidal epithelial cells which due to having a larger outer perimeter than inner perimeter causes the cuboidal cells to be more pyramidal in shape. 3. Simple columnar epithelium: a single layer of columnar cells a. Non-ciliated simple columnar epithelium (1) Presence of microvilli which increases surface area for absorptioin (2) Presence of goblet cells which secrete the protein mucin in the form of mucous b. Ciliated simple columnar epithelium (1) Cilia are usually about one-third as long as the columnar cell is tall (2) Cilia move fluids and particulate matter along the epithelial surface c. Pseudostratified columnar epithelium (1) Is truly a "simple epithelial" tissue because it consists of only one layer of cells (all cells have their basal surface on the basement membrane; not all cells' apical surfaces touch the lumen (or the free edge) (2) Gives the appearance of many cell layers, since the nucleus of each cell occupies a different region of the cell than its "next-door neighbor" cell (3) There is both ciliated and non-ciliated pseudostratified columnar epithelium: (a) Ps. ciliated col. epi. secretes mucous (goblet cells do) and bear cilia that sweep away mucous and trapped foreign particles (lines airways of most of the upper respiratory tract - nose, nasal cavity, pharynx and associated str.) (b) Ps. nonciliated col. epi. lacks cilia and goblet cells (lines larger ducts of many glands~ the epididymis, and part of male urethra) 5. Stratified squamous epithelium: multiple layers of squamous epithelial cells~ only the basal-most layer touches the basement membrane~ and only the apical layer cells touch the free edge (or lumen) a. In general, the basal-most layer of cells are quite cuboidal in shape~ even some are a bit columnar b. It is the basal cells that undergo mitotic division with one daughter cell staying put on The basement membrane and the other one eventually pushing up to the apical layer c. There is keratinizing stratified squamous epi. and non-keratinizing str. sq. epi. (1) Keratinizing st. sq. epL forms the epidermis of the skin and consist of anywhere between 50 layers of cells (in thin skin) to 100 layers of cells (in thick skin) (2) The distinct zones within this keratinizing str. sq. epi. are: (a) Stratum basale - one, single layer of cuboidal-shaped cells (b) Stratum spinosum - 8-10 layers of polygonal (many-sided) cells (c) Stratum granulosum - three to five layers of flattened cells (d) Stratum lucidum - 3-5 layers of extremely flattened cells (and this layer is present only in the fingertips, palms, and soles) (e) Stratum corneum - 25-30 layers of not only flattened, but dead cells. (3) Non-keratinizing str. sq. epLlines wet surfaces such as thoses of the oral cavity (including covering the tongue) and esophagus~ parts of the epiglottis and the vaginal canal. (a) There are usually far few layers of cells in non-keratinizing str. sq. epi. (b) The first three stratification zones are the same as above; the last two zones are absent. (An interesting note is that the vermillion zone (of the lips) which is the transition region trom the keratinizing epidermis of the skin of the face and the non-keratinizing oral epithelium has FOUR strata (basale, spinosum, granulosum, and lucidum) which imparts the lips' unique color and texture compared to either of the other two areas. Lips are smoother and slicker than the skin~ but not as constantly moist as the oral epithelium. Due to the presence of the protein eleidin.) 6. Stratified cuboidal epithelium: more than one layer of cuboidal cells. a.F ound only in the ducts of adult sweat glands, in esophageal glands, and part of male urethra b. Functionally, this tissue is protective and has limited secretion and absorption capabilities 7. Stratified columnar epithelium: more than one layer of columnar cells a. Has protective and secretory functions b. Found only rarely in the body in the lining of parts of the urethra, large excretory ducts of some glands, in the anal mucous membranes, and in the conjunctiva of the eye. c.Cells in the first and second layers removed from the basement membrane may only have their nutrients provided and waste products removed by simple diffusion because remember: Epithelia are avascular tissues. This explains why stratified cuboidal and stratified columnar epithelia are rare, indeed. 7. Transitional epithelium: truly a stratified epithelium because it consists of several layers (usually 5-8 layers) of epithelial cells whose apical-most layer of cells "transition between being big and rounded ("balloon cells") and being very flat and met~ed. . a. Capable of stretching and thus permitting distention (as of the urinary bladder) b. Lines the urinary bladder and portions of the ureters and the urethra D. Glandular epithelium 1. A gland is a single cell or a mass of epithelial cells adapted for secretion. All glands derive from epithelium. 2. Endocrine glands are ductless; their secretory products (hormones) enter the extracellular fluid and then diffuse into the blood. (-crine = Greek. krinein: to secrete; endo = within 3. Exocrine glands (sudoriferous, sebaceous, ceruminous, mammary, digestive) secrete their products into ducts that empty at the surface of covering and lining epithelia or directly onto a free surface. (Exo = to the outside; crine = to secrete) 4. Structural classification of exocrine glands a. Unicellular glands are single-celled (ie: goblet cells) b. Multicellular glands are composed of cells that form distinctive microscopic structures (ie: sudoriferous, sebaceous, salivary, etc.) (1) Tubular glands (2) Acinar glands (3) Tubuloacinar glands (4) Simple glands (5) Compound glands 5. Functional classification of exocrine glands a. Merocrine glands - secretory products are discharged "cleanly" by exocytosis and no cellular debris accompanies it (salivary glands and the pancreas) b. Apocrine glands - secretory products are released when enough secretory vesicles alc cumulate at the apical portion of the cell which then "pinches oft''' dis charging not only the secretory product, but cellular membrane and debris c. Holocrine glands - secretory products are released only when the cell itself dies thus releasing all manner of cellular products. (sebaceous glands, which is why sebum is so "oily" - there is lots of phospholipids and other lipids.) V. Connective Tissues A. General features of connective tissues 1. Most abundant and widely distributed basic tissue-type in the body 2. Characterized by cells which are relatively few and far apart (sparsely distributed) with LOTS of intercellular substance between the cells. (As a point of terminology, the term -blast refers to an immature cell; -cyte refers to the mature, fully differentiated form of the cell.) 3.Cell types: a. Fibroblasts - cells that produce fibers b. Macrophages - phagocytic cells derived from monocytes of the blood with there being many specific ones: histiocytes (stationary macrophages) and wandering macrophages: Kuppfer cells, alveolar cells, etc) c. Plasma cells give rise to antibody-producing B-lymphocytes d. Mast cells produce histamine which causes vasodilation and enhances white blood cell action e. Adipocytes are fat cells which store lipids f. Chondroblasts/-cytes are cells which produce and maintain cartilage c. t. g. Osteoblasts/-cytes are cell which produce and maintain osseous C.t. (bone) h. Blood cells: Erythrocytes (red blood cells) and Leukocytes (white blood cells) and Thrombocytes (platelets) 4. Presence of matrix (matrix = ground substance plus fibers; does not include cells) a. Ground substance - non-cellular material (mostly glycoproteins and proteoglycans such as hyaluronic acid, chondroitin sulfate, dextran sulfate, etc) secreted by the conn. tissue cells (may be fluid, semifluid, gelatinous or calcified to a small are large degree. This is the basis for allowing the C.t. to be classified according to their "texture" as either (1) Soft - aerolar, reticular, elastic, collagenous, adipose, pulp (2) Firm - the cartilages (hyaline, elastic, fibro-) (3) Rigid - bone and the dental tissues (enamel, dentin, cementum) (4) Fluid - blood and lymph b. Fibers (1) Collagen fibers - composed of collagen (which then polymerizes); very tough and resistant to stretching; found in collagenous C.t. 's, bone, cartilage, tendons, and ligaments. (2) Elastic fibers - composed of elastin; provide strength and stretching capacity; found in dermis of the skin, in elastic cartilage, blood vessels, and the lungs. (3) Reticular fibers - composed of reticulin (simple collagen plus a glycoprotein), provide support in the walls of blood vessels and lymphatic organs and form a strong supporting network around collections of adipocytes, neuron processes, and muscle cells. (4) Connective tissue is not found on free surfaces (5) Highly vascular (exception is cartilage and tendons) (6) Presence of a nerve supply (exception is cartlage) C. Classification of connective tissues 1. Mesenchyme is the embryonic tissue from which all other c.t.' s eventually arise 2. Loose Connective Tissues consist of fibers, cells and a semifluid ground substance a. Areolar c.t. - ground substance allows for passage of nutrients from the blood into adja cent cells and tissues; found in subcutaneous tissue b. Adipose c.t. - composed of adipocytes; associated with areolar c.t.; supports, protects, and generates heat (brown fat is used by infants to regulate their temperature) c. Reticular c.t. (1) Consists of fine interlacing reticular fibers and reticular cells (2) Forms the stroma of certain organs (lymph nodes) (3) Helps bind together the cells of smooth muscle 3. Dense Connective Tissues a. Dense regular c.t. (collagenous c.t.) bundles of collagen fibers in a regular and orderly, parallel arrangement that confers great strength b. Dense irregular c.t. (collagenous c.t.) (1) Collagen fibers that are irregularly arranged and is found in parts of the body where tensions are exerted in various directions (2) Found in sheets (dermis of the skin, heart valves, perichondrium, periosteum) c. Elastic c.t. (1) Consists of elastic fibers and fibroblasts (2) Very strong and can recoil back to its original shape after being stretched (3) Found in lung tissue and elastic arteries 4. Cartilages a. General Characteristics (1) Composed of dense network of collagen- and elastic-fibers embedded in chondroitin sulfate. (2) Chondrocytes are found in spaces called lacunae (3) Perichondrium is the dense irregular connective tissue layer which surrounds cartilage (4) The cartilages are avascular (no blood vessels); they also lack nerves b. 3 Types of Cartilage: Hyaline cartilage; Fibrocartilage; Elastic cartilage (1) Hyaline cartilage (a) most abundant form of carilage (b) fine collagen fibers embedded in a gel-type matrix (c) weakest of the three types of cartilage (2) Fibrocartilage (a) bundles of collagen fibers in the matrix (b) no perichondrium is present - (c) strongest of the three types of cartilage (3) Elastic cartilage (a) threadlike network of elastic fibers is found in the matrix (b) perichondrium is present 5. Bone (osseousconnective tissue) a. The matrix contains mineral salts, collagenous fibers and osteocytes b. Compact bone is composed of a basic unit called the osteon or Haversian system (1) Lamella are concentric rings of matrix (2) Lacunae are small spaces between lamellae that contain osteocytes (mature bone cells) (3) Canaliculi are minute canals containing processes of osteocytes that provide routes for nutrient and waste transport (4) Central (Haversian) canal contains blood vessels and nerves c. Spongy bone has trabeculae as its functional unit (rather than osteons) d. Functions of bone (1) Supports 2 Protects 3 Helps provide movement 4 Stores minerals 15jHouses blood-forming tissue 6. Blood (vascular connective tissue) a. LiqUid matrix (plasma) and formed elements (erythrocyte~ leukocytes, thrombocytes) VI. Membranes (flat sheets of pliable tissue that cover or line a part or the body) A. Synovial membranes (not true membranes) 1. Line joint cavities and coDSiSt of only connective tissue (no epithelial layer 2. Secretes synovial fluid-used for lubrication of joints B. Mucous membranes (collectively all the mucous membranes are called: mucosae) 1. Line cavities that open to the exterior 2. Acts as a barrier to pathogens and a trapping surface for particles 3. Lamina propria is the connective tissue layer of the mucous membrane C. Serous membranes (collectively all the serous membranes are called: serosae) 1. Line body cavities that do not open directly to the exterior and covers organs that lie within the cavity (pleura, pericardium, pentoneum) 2. The membrane consists of parietal and visceral portions 3. Serous fluid is secreted to provide lubrication vn. Muscle tissue A. Muscle cells (called myofibers) are modified for contraction B. Functions: 1. Provide motion 2. Mainrenanceofposture 3. Heat production C. Types of muscle tissue: 1. Skeletal muscle a. attached to bone b. striated (light and dark banding) c. voluntary d. Multinucleated cells 2. Cardiac muscle a. Forms most of the heart wall b. Striated c. Involuntary d. Single nucleus per myofiber e Presence of intercalated discs Gunctions between myofibers) 3. Smooth muscle (visceral muscle) a. Found in walls of hollow internal structures/organs. b. Nonstriated c. Involuntary d. Single nucleus per cell VIII. NelVous tissue A. Functional nerve cells are called neurons 1. Three functional classes of neurons: motor, sensory, intemeurons. 2. The cell bodies of each of the neuron functional types are located in specific parts of the peripheral and central nelVOUS system. B. Each neuron has three distinct structural parts: 1. One soma (cell body) 2. Each neuron has only one axon (cytoplasmic extension or process along which the nelVe action potential (impulse) travels away from the cell body. 3. Neurons may have only one dendrite or may have multiple dendrites (cytoplasmic extensions or processes along which the nelVe action potentials (impulses) travel toward the cell body. 4. Neurons respond to various stimuli and conduct nelVe impulses to other neurons, to muscle cells, or to glands. C. The supporting nerve tissue cells are called neuroglia 1. Neuroglial cells are differentiated from connective tissue cells; but are now con sidered nelVe tissue cells. 2. Four types of Central NelVOUS System (CNS) neuroglia: a. Astrocytes b. Oligodendrocytes - make myelin in the CNS c. Microglia d. Ependymal cells 3. Two types of Peripheral Nervous System (PNS) neuroglia: a. Neurolemmocytes - Schwann cells - make myelin in the PNS b. Satellite cells