LAB #3
advertisement
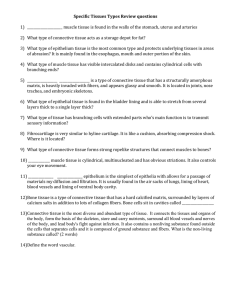
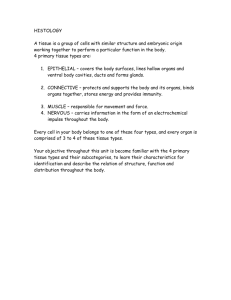
Biology 241 – Lab LAB #3 (3rd/21 Lab Sessions for Fall Quarter, 2008) TOPICS TO BE COVERED: »Microscopic examination and drawing/labeling of Simple Squamous Epithelium »A Discussion of the Classification Criteria for Connective Tissue »Microscopic examination and drawing/labeling of the following Connective Tissue sub-types: (1) Areolar Connective Tissue (2) Collagenous Connective Tissue (3) Elastic Connective Tissue (4) Reticular Connective Tissue and (5) Adipose Connective Tissue DESIRED OUTCOMES: After completing the activities described for this lab session, students should: »Be able to recognize microscopically all epithelia sub-types based upon cell layers / cell shape. »Be able to recognize microscopically certain connective tissue traits and specializations. »Have rendered drawings of the various tissue sub-types assigned, along with proper labeling of prominent features of each. »Relate tissue sub-type structural characteristics to the specific functioning of that sub-type. »Be able to give one (or more) example(s) of where in the body each sub-type is found. MATERIALS NEEDED: »Blue Box of prepared microscope slides marked: HISTOLOGY SLIDE SERIES in Lab Bench Drawer; specifically Slide #1: Simple Squamous Epithelium; Slide #7: Areolar C.T.; Slide #8: Collagenous C.T.; Slide #9: Elastic C.T.; Slide #10: Reticular C.T.; and Slide #11: Adipose C.T. »Histology Drawing Sheets, pencils, eraser, Histology Drawing Assignment as reference sheets. »Photographic Atlas, Ch. 3 Activity #1: Microscopic examination and drawing/labeling of Simple Squamous Epithelium Simple Squamous epithelium is more difficult to isolate in a specimen; and it is more difficult to draw correctly. Thus, our histology drawings started with other epithelia that are easier to “decifer”, and, at the same time, the student was sharpening his/her powers of observation and extending the “comfort zone” for using the microscope as an investigative tool. By now, however, the student is ready to find, view, draw and label Simple Squamous epithelium. Take Slide #1 from the Blue Box of prepared slides, noting that the label reads: Simple Squamous epithelium and the specimen under the cover-slip looks like a triangle. Indeed, the thin section of specimen was cut from a triangular “chunk” of kidney organ, such that the part of the triangle adjacent to the rounded-surface cor-responds to the outer zone of this organ, called the renal cortex; and the rest of the specimen reveals the inner zone of this organ, called the renal medulla. It is important to know that the kidney is composed of functional units called nephrons and MOST of each nephron is composed of convoluted or straight tubular portions whose walls are made up of Simple Cuboidal epithetlium. (Thus, unless you know where to look specifically, the general finding will be hundreds of cross-sections of renal tubules (of the nephrons) with nearly ALL simple cuboidal epithelium in the fields of view.) The only part of each nephron that is composed of Simple Squamous epithelium is a structure called the renal corpuscle. A renal corpuscle consists of two parts: (1) the Glomerulus - a tangled tuft, or rounded mass, of a specialized blood vessel that behaves like capillaries but is really a tiny arteriole; and (2) the glomerular capsule (aka Bowman’s Capsule) – a double-walled “globe-shaped” structure at the proximal end of the nephron that is then continuous with the renal tubule part of each nephron. It will be a renal corpuscle (specifically the outerwall of the glomerular capsule (Bowman’s Capsule) that you will need to find in order to view a clear and precise example of Simple Squamous epithelium. Renal corpuscles are located ONLY in the (outer) renal cortex zone of a kidney; thus you MUST be sure to stay in the region of the specimen CLOSEST to its rounded surface. Biology 241 – LAB #3 – continued Page Two PLEASE: DO NOT PROCEED WITH YOUR DRAWING UNTIL YOU HAVE HAD THE INSTRUCTOR CHECK THE FIELD OF VIEW to make sure you are focused on a glomerular capsule. This will ensure that you do not waste valuable time; and that the time you do spend can be most productively used to discern the continuous layer of very, very thin (flat) cells on its Basement Membrane (basally) and with the apical surface of these cells “touching” the lumen of the glomerular capsule. Also, you will need to understand that what “fills” the lumen of the capsule is a glomerulus – which is also composed of a Simple Squamous epithelium (called an endothelium) – but which is too tightly coiled to be drawn effectively. You may represent the glomerulus with “squiggle lines” because not a lot of detail is required. Thus, DO NOT spend your time tediously rendering detail of the blood vessel contained in the capsule; rather, expend time and artistic talent on capturing the exquisite detail of the capsule’s Simple Squamous Epithelial layer in all of its contiguous glory!! Activity #2: A Discussion of the Classification Criteria for Connective Tissue We are ready to proceed with a discussion of the second of the four basic tissue types, Connective Tissue: Connective Tissue is the single most abundant and most diverse type of tissue in the body. It has the most sub-types. In order to understand the sub-types, one must first understand the criteria for classification of connective tissues. Whereas classification of Epithelia is based upon (1) number of layers of cells and (2) cell shape; Connective Tissue classification is based upon (1) the nature of the matrix* and (2) the cell type that manufactures it. Let’s first understand a fundamental difference between cells of an epithelium and cells of a connective tissue. Remember: cells of an epithelium are packed VERY TIGHTLY together such that there are few or NO intercellular spaces. (This is referred to as “cellularity”; and since there are no “spaces” between cells, there is also no substance between epithelial cells.) Cells of connective tissues, on the other end of the extreme, are NOT packed closely together; rather they are FEW and FAR APART. Thus, the “character” of a connective tissue becomes as much a matter of what specific cell-type there is as what is the nature of all the “stuff” between the widely spaced cells. For any of the connective tissue sub-types, the “stuff” between the cells is referred to as matrix. Matrix (as referenced below) has two sub-components: Ground substance and protein fibers. BOTH OF THESE COMPONENTS (the ground substance and the protein fibers) are manufactured by the resident cells of the connective tissue. As each connective tissue cell goes through its cellular life cycle, it is busy secreting ground substance and protein fibers and becoming surrounded (above, below, on all sides) even entrapped by all this “goo”. A connective tissue cell literally can be said to “stew in its own juices” during its lifetime. How thick the “juices are” depends upon the TYPE of connective tissue cell making them, and the quantity and type of protein fibers that cell manufactures to exocytose out into the intercellular compartment; as well as how loosely or closely packed the fibers tend to get once they find themselves out in the ground substance. *Matrix: intercellular substance composed of ground substance and protein fibers. (Ground substance contains water and an assortment of large organic molecules, many of which are complex combinations of polysaccharides and proteins. The polysaccharides include hyaluronic acid, chondroitin sulfate, dermatan sulfate, and keratan sulfate; collectively referred to as glycosaminoglycans (GAGs). Except for hyaluronic acid, the GAGs are associated with proteins called proteoglycans which form a core protein around which the GAGs project like the bristles of a brush. One of the most important properties of GAGs is that they trap water, making the ground substance more jellylike. Functionally, ground substance supports cells, binds them together, stores water, and provides a medium through which substances are exchanged between the blood and cells. It plays an active role in how tissues develop, migrate, proliferate, and change shape and in how they carry out their metabolic functions. Also, taking into account the specific quantity of and type of protein fibers that become embedded in the ground substance, the entire matrix may undergo a texture change from fluid to semifluid, semisolid, gelatinous, or even calcified. Biology 241 – LAB #3 – continued Page Three The most predominant protein fibers that come to be embedded in ground substance are: Collagen fibers (composed of the protein collagen); Elastic fibers (composed of the protein elastin); and Reticular fibers (composed of the protein reticulin). Depending upon which protein fiber type predominates in the matrix, the connective tissue will bear that name: ex: Elastic C.T. has fibroblast cells which manufacture and exocytose predominately elastic fibers which come to be aligned in the matrix to give a loose, but strong and very extensible/ elastic tissue perfect for the dermis of the skin to give it its resilience! Collagenous C.T. has fibroblast cells that manufacture and exocytose predominately collagen fibers, which then pack very closely together in the matrix and give an extremely dense, non-yielding texture to the tissue; perfect for tendons and ligaments! Or, Reticular C.T. has fibroblast cells which manufacture and exocytose predominately reticular fibers which are branched and come to form a “net” or “mesh” in the matrix giving it a loose, spongy texture. Areolar C.T. has equal numbers of all protein fiber types, none of which pack closely together, so this tissue has an “airy” quality to it. Here are the names of the various TYPES of Connective Tissue cells: Fibroblasts Chondroblasts/Chondrocytes Osteoblasts/Osteocytes/Osteoclasts Adipocytes (Also, Blood cells: RBCs/ WBCs/Platelets aka Erythrocytes/Leucocytes/Thrombocytes – which are not studied histologically in Biology 240/241. We will view these in detail in Biology 250/251 ) Here are the “textures” of the matrix component of the various Connective Tissues: Soft Firm Rigid Fluid Of the Soft Connective Tissue sub-types, there are two additional categories: Embryonic and Adult (aka Mature) The two Embryonic soft connective tissue sub-types are: ▪Mesenchyme ▪Mucous C.T. (aka Wharton’s Jelly”) The Adult (Mature) soft connective tissue sub-types are: ▪Areolar (Loose) C.T. ▪Adipose C.T. ▪Reticular C.T. The Adult (Mature) soft (but dense) C.T. sub-types are: ▪Dense regular C.T. ▪Dense irregular C.T. ▪Elastic C.T. Firm Connective Tissue sub-types include the Cartilages (Cartilage is not soft, but not rigid either. It is semisolid.) The three sub-types are: ▪Hyaline Cartilage C.T. ▪Fibrocartilage C.T. ▪Elastic Cartilage C.T. Rigid (aka Hard) Connective Tissue sub-types include all the normally calcified tissues The various sub-types are : ▪Osseous C.T. ▪Cementum C.T. ▪Dentin C.T. ▪Enamel C.T. (Note: Only ▪Osseous C.T. (aka Bone C.T.) will be examined histologically in Biology 240/241. The other rigid C.T. sub-types are all dental connective tissues and are studied in the Dental Hygiene Program) Fluid Connective Tissue sub-types include ▪Blood C.T. and ▪Lymph C.T. These will not be studied histologically in Biology 240/241. We will view these connective tissue sub-types in detail in Biology 250/251. Activity #3: Microscopic examination and drawing/labeling of assigned C.T. sub-types For today, you will examine and generate labeled drawings for Slides #7 - #11 representing the following five connective tissue sub-types: Areolar C.T., Collagenous C.T. (aka Dense regular C.T.), Elastic C.T., Reticular C.T. and Adipose C.T.* *Note: Adipose C.T. is an “exception to the rule” for Connective Tissue sub-types in two ways: (1) its cells (adipocytes) are not “few and far in between”, but rather are packed very tightly together; and (2) because the cells are packed so tightly, there is little or no matrix. So, in the case of this specialized C.T., matrix considerations are not important; rather it is what these cells accumulate and store in their interior that is significant: a large, round, lipid (triglyceride) droplet. As adipocytes fill up with lipid, their cytoplasm and nucleus are pushed to the periphery of the cell, making the entire cell resemble a signet ring; hence, their nickname: “Signet cells”.