1
advertisement

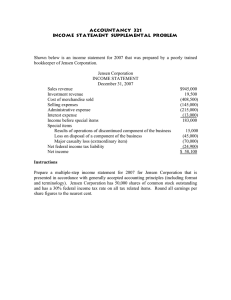
1 >> Alex Weinert: Hi, and welcome to the Microsoft Research Speaker Series. I was told to say that. I hope I said it okay. My name is Alex Weinert, and I'm here to talk a little bit to introduce Dr. Michael Jensen, who is our speaker today. That's me, and the person clinging on to me is my son, Owen, at about 9 years old, probably six months or so after he started treatment for acute lymphoblastic leukemia at Seattle Children's. Just shortly after Dr. Jensen joined the team at Seattle Children's, coming from -- I hope I get this right -- City of Hope, and that was largely made possible by the Ben Town Foundation, who did some amazing work to get him up here. And I was going to give you a quick little tour of why this talk matters a lot to me and try to put some context around it, because the science is amazing, and the technology is amazing, but it's actually a very human story at the bottom of it. So this is very much my personal story. So I want to talk to you about a period from 2009, December, to March of 2010, which I would talking from zero to 60 in four seconds if you have a good car. This is from wonderful to freak out in three months. In December, I would say everything was just great. By the end of December, there was some weird kind of frequency in the amount of colds and sinus infections and things like that that Owen was getting, but otherwise pretty well. To the point where in January, he did something -- we're into cycling in my family, and there's a mountain bike ride called the stinky spoke, and he came across the line and everybody was amazed, and he was the youngest kid to ever do that ride. Very, very strong, very fit athletic kid. Still pretty strong. He had wanted to ride a charity ride to raise money for cancer, actually, which was a 50-mile ride, so he'd been training pretty ride and he went into a ride called the Chilly Hilly which is 30 miles. But he was very weak and kind of off his game, I would say, at that time. And by March, we find out, and some of this is retroactive, that we'd learned this, but he'd been staying in from recess. He'd stopped going to lunch. He had stopped eating breakfast at home. He started losing weight. He was getting pallid. On March 21, we went out for a fun day, but he slept all the way to the park and he didn't do anything at the park and he slept all the way home. And I got really, it was like lights started coming on. 2 So I got out a grocery list piece of paper and I wrote down in pencil, and I still have this piece of paper, all the symptoms that I could think of and what I'd been seeing since about January. As I wrote the list, I got more and more kind of centered on what was probably happening. And I gave it to my wife and I said, he has to be seen tomorrow. And she called and they couldn't see him because they didn't have any schedule time. We're like, well, this has been months building up so we can go another day. That day, he was sent home from school with a fever of 102 degrees. But we had the doctor's appointment set up for the morning so we thought, well, that's all right. We went in. He slept through the night. Went in in the morning, still had the fever. She saw the list. This is Ballard pediatrics, if anybody cares, she saw the list and immediately sent him for blood tests. So here's my day, I send them off to the doctor in the morning. I good to work, and at 3:30, I think oh, I wonder how the doctor's appointment went. Are we on antibiotics now? And I got a text message from Heather in reply to my message which was no, we're still in the lab. This is 3:30. I'm going into an exec review. And I think I had this -- yeah, so I'm going into an exec review at 3:30. And I get this text, I'm starting to wonder what's going on. And the exec review ends at 5:00, and I got a schedule plus, and this is through a weirdness of the way we were communicating and her inability to reach me by phone. But the first word I got was a schedule plus saying we need to be at Hemonc at 8:00 the next morning. So I look up Hemonc, and it's hematology oncology and it basically means cancer and blood disorders. So that was how I found out. So the next morning, Owen goes in, and I want you to look at this picture. That's him healthy. That's January, late January. That's the day he was getting the blood tests. That's the next day. So the next day, we went in, and -- I'm sorry. I'm getting more emotional than I thought I would. And he was admitted, and we started chemo. And from that day to this day, he's been taking chemo. That picture on the bottom left is a picture of his weekly pill load. The picture in the middle from IT methotrexate, he was being neuro toxic, his brain was basically poisoned. He had to go in for MRIs to deal with 3 measuring the damage and addressing it and fixing it. to mitigate it. Thankfully, we were able The picture there is when he was, I believe he was hepatotoxic, which means his liver was failing, because of the chemo he was getting. You know, it's hair loss, you can see that. One of the pills I have to give him every single night has that warning label on it. It's a biohazard warning label. Okay? It says Mercaptopurine. In my family, we're really lucky. Owen is a standard risk low. He has great, what's called cytology, which means the particular mutation he got that gave him leukemia is one of the easiest ones for us to cure. He's one of the luckiest kids out there as far as pediatric cancers go. He has it really easy. That doesn't make it easy. So by the numbers, and I pulled this data, there's a cite called PAC-2. This is mostly from the organization called decog, which is a cancer oncology group. Is that right? Children's oncology group, which is I think 250 or so hospitals that collaborate with research and sharing data and treatment. And so this is relatively current data. About 13,500 kids a year are diagnosed in the U.S. About 36 a day. Mortality is about seven children a day. This is the state of treatment today. ALL is the most common by a fairly wide margin of the pediatric cancers, and then comes brain cancer. So I said, you know, this is an introduction talking about a cure, and cure with an asterisk. And so what's with the asterisk? The issue with the asterisk is when we say cure, we're talking about 80 percent of children, not 100 percent of children. Secondly, of the statistics, I won't read through them, but they have very, very significant side effects to the treatment. Not just the treatment that he went through, and the suffering that he's gone through for the last three years, but his long-term prognosis. Like 74 percent of children will have one or more serious side effects. The graph on the right is one I really want to call attention to. The top two lines are average mortality for children in the United States. The bottom two lines for female and male are for children who have been treated for cancer, who have made it through the first five years of treatment. these are what we call survivors. These are people that meet the 80 percent 4 criteria. This is what happens to them afterwards. That's the mortality. Those are side effects of treatment. Secondary cancers, chemo that gives you cancer. Radiation that gives you cancer. Chemo that gives you heart disease, all right. Chronic cognitive disorders. Chronic depression, chronic pain. Very serious things. I put a picture of a single round in a chamber there with an arrow to 0.84. That's the same statistics as Russian Roulette. Your chances of making it 25 years past treatment are worse than your chances of surviving Russian Roulette if you're a pediatric cancer survivor. There's a couple things I want to sign off with. One is a couple of good pictures. One of them was inpatient last Christmas. So we made the doctors who were rounding come in and put on reindeer. We wouldn't let them in unless they put on reindeer heads. And the person on the left, closest to us, is Dr. Rebecca Gardner, and Dr. Gardner is working with Dr. Jensen to begin the phase one trials for the work he's going to talk about to you today. And the other thing is if there's anybody who is paying attention online or in the room would like to learn how to help, one of the things we do, and I can give you lots of ideas, but one of them is that we have a cycling team, and we raised about 50,000 through Microsoft last year for this research. And then finally, if you're interested, you could go look at the link. It might be sensitive, so I'm just going to say there exists a [indiscernible], but it points, I think, very directly to the profound need to fund research. And then I'm going to sign off with something that Owen was insistent we did last night. >>: Hello, I'm Owen Weinert. I'm an 11-year-old cancer patient in treatment for acute lymphocytic leukemia. I was diagnosed in March of 2010 when I was just 8 years old, and I've been taking chemo orally through injections or through spinal tap ever since. Dr. Michael Jensen's research is a new way to program the T cells to fight back against cancer cells called blasts in the body. It's like adding a feature on the body's own defense system. And so without further ado, Dr. Michael Jensen. >> Dr. Mike Jensen: Okay. Thank you all for coming. This is a real privilege to be able to come here and tell you about our research at Seattle Children's 5 Research Institute. If I'm successful, I will hopefully open some doors for you in to the type of work and the way we think about doing our research at the institute, and also I think through this, you'll see some fairly startling parallels to maybe some of the research you do here at Microsoft, and there's potential synergies that may flow from that. I want to also begin by thanking you, Microsoft employees, because over the years through your employee giving programs, Seattle Children's has, I think, benefits as one of the top five charitable organizations to receive your help, and it's gone a long way. And we have a lot more work to do. Also, I want to point out that we have a research institute at Seattle Children's Hospital, Seattle Children's Research Institute, and this really came from the recognition by the hospital about seven or eight years ago that if we are to fully capitalize on the future well-being and health of our children and children around the world, that Seattle Children's Hospital had to engage in biomedical research to find the cures and the treatments to help kids either prevent serious illness from occurring and to safeguard their futures. So we are located, actually, in downtown Seattle. We're one of the top five NIH funded pediatric research institutes in the country. And a lot of people in the Seattle region don't know that we exist yet, and so I'm trying to spread the word. We are a serious operation in terms of biomedical research, and I'm here to tell you a little bit about our cancer research program. So I think Owen gave you a very vivid snapshot, and his father, Alex, thank you for that. And I think most people, if I were to say what is cancer in a child look like, an image just like this would come up in your minds. I think for most of you, that would be true and there's probably very few of you, and wherever you are watching this, that hasn't seen cancer play out in a loved one, whether it's a parent, grandparent, a friend, a child. This image is a lot like the image of a child with leukemia if that child were diagnosed in 1963. It hasn't changed a lot. And that's because in large part, we are still relegated to dealing with cancer with the same basic armamentarium that we've been using over decades now. Chemotherapy, radiation, surgery. Cut it out, burn it out or poison it out of the body. A lot of chemotherapy actually evolved from poisons that were developed in World War One and World War II that we learned how to give just enough to not kill the patient with the goal of killing rapidly proliferating cancer cells. 6 With kids, we have, I guess, an opportunity as pediatric cancer specialists, because kids have generally good hearts and they have good lungs, they have healthy bodies, we can give more chemotherapy in higher doses to a child than an adult could ever survive. And that's what has allowed us over the last couple of decades to move the bar such that in 2013, about 75 to 80 percent of kids can be what we call cured. That means the tumor doesn't come back within five years. And you heard about some of being cured is not -- doesn't mean that you're going to be able to have a long and uncomplicated life ahead of you. So we have a lot of work to do and when I talk about those cure rates in the '70s and '80s, that's in large part because acute lymphoblastic leukemia is very curable and that's the most common. But if you look at cure rates of the common solid tumors that we see in kids, things like neuroblastoma and brain tumors and rabdos, we're well below the 50 percent mark in 2013 with the most aggressive therapies a human body can tolerate. We have to do better. So why is it crucial for us at Seattle Children's Research Institute and other cancer research programs around the country and around the world to try to help create solutions through research for kids with cancer? One part of the story is I don't think we can rely on big pharma and the industrial complex of medical research to come to the rescue of children. That's in large part because of the numbers you saw Alex give. You add up all the kids with cancer, it's still called an orphan disease. And from a business perspective, it's a business orphan disease in terms of how many of your pills you'll be able to sell to that population. Kids' cancer is fundamentally different than adult cancers and doesn't respond the same. Nor do we do studies that test the potency or side effects in kids. When we get to use a drug that's been developed for breast cancer in a child, it's not because we know how much to give and what the side effects will be. As pediatric oncologists, we have to do that on our own. And the third component is there's a lot of emphasis now in pharmaceuticals to think of cancer as -- make cancer a chronic disease. Develop pills that a person can take every day from the time they're diagnosed to the time they pass away that will slow the tempo, put a lid on it. And that might be great if you're in your 70s and you can get another ten years of high quality life. But if you're a 3-year-old with a brain tumor and the only drugs that exist are 7 drugs that will give you another five, eight, ten years, that's an empty -that's an empty victory. So we have to do better. We have to do research that's really drilling down to try to cure the disease. And if we can do that for kids, and translate that to the common adult cancers, everybody wins. So cancer is the number one cause of death from disease in the United States in children. Of the toxicities, you've heard about, but they can be life-threatening at the time, and they can cause life-long disabilities that take away a child's future for a healthy and fulfilled life. And the treatment of cancers, you heard, greatly increases your chances of getting cancer 30 years later. Colon cancer rates in kids that were cured of pediatric cancer skyrocket. So because of the therapies that we use, we doom a lot of childhood survivors to be back in an oncology clinic again as an adult with something like colon cancer, breast cancer, kidney cancer. So our vision at Ben Towne Center For Childhood Cancer Research at Seattle Children's Research Institute is to really accelerate the timetable to do innovative translational research where all children can be cured, and we cure them with therapies that are specific enough that it doesn't harm the body along the way. So in my world, I'm trained as a molecular immunologist, and I think about how the immune system works. And in your vernacular, in some ways, immune system uses -- the immune system uses devices to get the job done, and the device I want to talk about today is a device of a white blood cell called a lymphocyte and, in particular, the T lymphocyte. The T lymphocyte is really the master regulator of the immune system. If you develop a sore throat and your lymph nodes and your throat get swollen and tender, that's because millions and millions of these T cells are going into that area to rid that area of the virus that's trying to get into your body. T cells move throughout the body, and they have sensors, they have programs and sensors that allow them to make decisions. And if a T cell that is roaming your body encounters a virus that it has a sensor for, then it can do something, a fairly typical program that it executes that goes something like this. 8 Here's a C cell. It's encountered a cell with influenza virus on the inside, the T cell is now getting signals through its sensors that activate a program that tell that T cell, drill holes in the membrane of the virally infected cell, insert packets of proteins that make the virally infected cell dissolve into a dead bit of cellular mush, if you will, and do that repetitively. Right now, the virally infected cell has been destroyed. The virus can't come out. The infection won't be propagated, and there are vacuum cleaner like cells of the immune system that come by, call macrophages, that clean up the mess. These T cells that encounter a virus when you're six years old will be in your body when you're 70 years old, waiting there to protect you if that virus were to try to come in again. If you had a polio vaccine, those same T cells are in your body protecting you from polio decades later because part of the program for the T cells to differentiate and become a memory cell that sits back and says, I've seen it before, I know what to do when I encounter it again. So how do T cells make this decision? When that T cell bumps up against a virally infected cell, it has to make a critical decision. Turn on the program, destroy that cell or back off and say that cell is a healthy cell. I don't want to do that. You think about it, the immune system and T cells have to make critical decisions every day. If the T cells are too fired up and they are not having discretion, then you get things like ought to immunity, rheumatoid arthritis, diabetes, MS. If the T cells are too wound down, they may come up against a fairly abnormal cancer cell and say, well, it's not -- that cancer cell is not really like a virally infected cell, I'm not getting all the signals that say to trigger, I'm just going to back off and leave it alone. And that's this tight rope walk that the immune system has to walk every day. So let's drill down a little bit more into the molecules that are involved in this -- you see it here, the trellis reaching out with kind of cellular hands and fingers and probes, and basically going over the surface of another cell to say are you okay? Are you a normal cell, or are you abnormal? And really what's happening there on the inside of that is a number of molecules that start to engage from the surface of the T cell to the surface of either the virally infected cell, the cancer cell or the stimulatory cell of the immune system. 9 This is a lot like the central nervous system forming synapses. In the central nervous system, the synapses are fairly stable over time, but in a T cell, this T cell is roaming around the body and doing it basically on an as-needed basis. If there is an antigen from a virus, for instance, it's going to be sitting up in this cleft here and the T cell sensors, when that triggers, will trigger the T cell to what I showed you, destroy the virally infected cell. So that's the natural biology that's been integrated into T cells over the course of evolution. >>: Can I ask one question? What are APC cells? >> Dr. Mike Jensen: APC stands for antigen presenting cells. So that's the cell that's designed to present new things to T cells when you get a vaccine or when you see a virus for the first time. So the immune system has evolved over millions of years. Cancers, when they occur in the body, come from a cell that essentially, the break is broken and the gas pedal is stuck on. The cancer cell, within the life cycle of its existence in your body, is evolving as well. And it's evolving and selecting against an immune system that wants to get rid of it. We know that if you're born with a genetic syndrome in which your immune system doesn't form naturally, you get a lot higher cancer rates than if you're otherwise healthy. So the immune system gets rid of most all the cancers that are generated in our body over time, but it's that cancer cell that makes a few extra evolutionary steps because its genome is unstable that could subvert the immune system and basically become invisible to the immune system. Then you have the diagnosis of cancer when you walk into the doctor's office, but your immune system isn't globally impaired. You can still fight infections. It's not like you have HIV virus and your immune system has been destroyed. Because tumors use very specific mechanisms in order to thwart the ability of the immune system to either know it's there or to be able to do anything about it when it encounters it. This is the problem of cancer when we, I as a doctor, see it in the clinic. The cat's kind of out of the bag. The tumor's already had a chance over the years that it has been quietly in the body developing to basically evade the immune response. 10 So what can we do about that? In your world and in the world of technology, we're in a logarithmic increases in knowledge and technology and the ability to do things, and I would say that in biomedical research, we lag behind technologies that you probably take for granted that you see the pace of in large part because we have difficulty accessing it in realtime. But having said that, can we think about a T cell as a device? It's a mobile device. And can we create apps for T cells to allow them to do something that the cancer never expected. Basically create an orthogonal immune response that the cancer never sees coming, because we are now reprogramming T cells, creating artificial intelligence for T cells when we isolate them out of the body so they can go back into the body and hunt down cancer in a way that the immune system and the rest of the body cannot do. So that's the concept. In many ways, I think about a T cell in ways in which there are similar structures and functions as a personal computer. The nucleus is essentially the hard drive. Chromosomes are depositories of large amounts of data bits. There are programs that turn on and off, based on transcriptional factors that go in and turn on gene expression. Messenger RNAs made in proteins come out that is basically the functional units. So what we're talking about is going in and putting Apps into the hard drive of T cells, into the nucleus, into the chromosomes to create new functions. You might get a little squirmish now. Amy? >>: [indiscernible]. >> Dr. Mike Jensen: >>: Yes, we have a question in the back. Could I do that at the end? Absolutely. >> Dr. Mike Jensen: That would be great. Remind me of that, okay. So for those of you who have taken some molecular biology, there is something you learned, I'm sure you remember about it and you think about it every day called the central dogma. Which is DNA begets RNA, messenger RNA, which codes for proteins and proteins do something. That's our grandparents' central dogma. Boy, that's changed, because RNA and DNA and proteins can do a whole lot more than that central dogma. 11 But for us, the issue is can we create apps that are encoded by DNA that create artificial mRNAs, that create artificial proteins and have those apps installed in T cells so those artificial proteins can allow the T cell to attack the cancer. So we're working along this line of thought. And so for us, you know, state of the art phone here, point that out. How do we do this? We make our app from recombinant DNA models that we create. We download the app into the T cell, and one of our first areas of synthetic biology is the app codes for a protein that's like a molecular velcro that's designed to be a lock and key so when now this T cell bumps up against the cancer cell, instead of the T cell saying, you're not normal, but you're not so abnormal that I'm going to trigger you, the velcro molecules look on to structures on the tumor sell, and on the inside of the velcro molecules, the whole alarm system that the T cell uses, when it's triggered by a virally infected cell. So we're creating now synthetic biology by creating artificial velcro-like receptors to express in T cells. I'm very happy to see that you have an app lab in your institution. I would recommend, this is just my bias that your app lab employees wear white, long white lab coats. It's much more impressive. Yes, sir? >>: I'm just wondering, do the T cell successful in detecting a cancer cell be consumed in the process? >> Dr. Mike Jensen: No. So just like T cells that fight infections, we know this from our lymph nodes in our neck, massive increases of a very few cells to millions or billions of cells over the course of a day or week or two, the infection and gone, and the evolutionary program for the trellis let's have 99 percent of those billion cells go die off. If we didn't do that, by the time we were 21 years old, we'd weigh about 500 pounds and about 350 pounds would be T cells, because we're always seeing infections. Our T cells are grow, they die back. And that one percent that's left over are those memory cells that will stay for the rest of your life and give you immunity. It's a very good question. So I'm going to show you the app and how it works first and then I'm going to show you under the hood how we made the app. So this is human neuroblastoma. It's one of the most lethal forms of pediatric cancer. These are living, human neuroblastoma cells. They're growing on a 12 plastic petri dish and we're imaging them through a video camera attached to a microscope. These cells will rapidly grow and take over the petri dish in a matter of 24 to 48 hours. What I'm about to do is add in human T cells that we've genetically engineered to have an app that codes for a velcro for a neuroblastoma. And to orient you right now, these little guys here, these are all the T cells that have been added. There's about one T cell for every cancer cell in the entire dish. And what I want you to notice first is how mobile these -- my kids call these the pack man cells or angry bees. You get a sense, they're swarming. They're going over the entire dish, but now something happens where now they're seeing the tumor cells, and you see that there's far fewer of these T cells that are just floating around where there's no cancer cells. They're actually coalescing around the tumor cells, even within this short part of the video, you see probably 80 percent of the cancer cells have been wiped clean off the petri dish. And you see how this plays out. The other thing I want you to see is now there's clusters of T cells. These are not tumor cells. These are now clusters of T cells. The number of T cells in the petri dish are starting to grow massively, because the T cells, through the velcro molecule, have seen the cancer cells. If we put T cells in this dish that had no velcro, there would be a few T cells that would float around, and they would die off in 12 to 24 hours. So as. A biologist and researcher, I'm like okay, how fast do these cells move? How many times can one cell kill a number of tumor cells. How many cells will come from one cell and divide and become clusters of cells. That's one part of my mind. And then the other part of my mind, I get this kind of Al Pacino voice that comes on, and it goes something like, you know, hey, neuroblastoma, let me show you my little friend, the T cells. And that's not right. I shouldn't do that. That's not a plug for the Scarface movie, but, you know, this is pretty exciting for us to see this. And now we're probably about six hours after adding the T cells. I want to point out one cell here. Your heart goes out to this guy. This is the neuroblastoma. I think it's one of the last ones in the dish. It's like I don't know what happened to those other guys, but I made it. I'm going to hang 13 out here and I'm going to grow back and take over this dish when the T cells are gone. It's a very ill advised perspective for that cell, and there you go. There are no more tumor cells. This is about six hours. Radiation and chemotherapy can't work this fast. Look at these T cells grow. So this is a very dynamic, living therapy. We're talking about taking a tube of blood from a patient, bringing it into a manufacturing environment, putting the app into the T cells, growing up several million or billion of these T cells outside the body for a week or two and then infusing that back into the patient where those living T cells that came from the patient go back in with this new program. Now, you saw how rapidly these cells start to grow, and that's a good thing, because there's a lot of tumor in the body when we treat most of our patients. There's millions, if not trillions of tumor cells. One app that I won't talk a lot about, but I think it's very important for this kind of work, because this is gene therapy or genetic engineering, is we put another app in with the velcro molecule called a suicide gene. What that means is that if we want these T cells to go away because they're getting over active or they've been around too long, we can give the patient a pill that activates the suicide gene and kills just the genetically engineered cells in the body and not the other T cells. And that's a safety feature that we put into the system. >>: Can you [indiscernible] sort of balances out only on the ones that we're working? >> Dr. Mike Jensen: That's exactly where we're going. About three slides from now, I want to show share that with you. So what's under the hood? How did we make this app happen? And what we did is conceptually, let's create what we call orthogonal function of the immune system through engineering. And the way we make these velcro molecules is we choose protein domains from monoclonal antibodies. You probably heard of Herceptin for breast cancer, or Rituxan for lymphoma therapy. There's a whole array of monoclonal antibody therapies. Most of those antibodies came genetically from mice. Now we have genetic libraries where we can make whole human libraries of antibodies and monoclonals that come from the human genome, but it's all made artificially. We cloned the 14 DNA from the antigen binding domain and we cloned the DNA from the T cell sensor, what's natively in the T cell and we fused these molecules so it looks like an antibody on the outside and it's a T cell receptor on the inside. And the tumor has no idea that this is coming, because there's no parallel in the natural immune system for this to happen. Of course, Reese's figured this out a long time ago. things and making something even better. It's bringing two great So not to alarm anyone, but in my world, in my laboratory, we work with chain reactions and HIV and all these things, and I want to put some perspective. Because in the media, when we talk about this research, the media says, oh, you work with a crippled HIV virus and it scares the bejeebers out of most people. I want to put some perspective. So we make this recombinant DNA technology possible through instruments that look the size of a toaster now. And the lab techs can put in the ingredients for making DNA and a template molecule to start with. They press a button, they go to Starbucks and have a latte. And about 90 minutes later, they come back with two to the fifth perfect copies of that DNA. So several billion copies over 30 cycles. And it's all replicas of artificial sequences that we can now make in hours. And back when I was a post-doc in the laboratory, we didn't have these machines. We had a hot water bath and a cold water bath and a stop watch and we used to do it by hand. Now these things are multiplex and they're controlled by servers and computers that will control arrays of these devices to create the building blocks. The way we get the app into the T cell is we use a remnant of the HIV virus. HIV evolved to be really effective at getting into T cells and delivering its genetic load. Yes, it's a crippled HIV virus, but it's been so -- we have so torn it apart genetically that the only thing about HIV that's left to this virus is the ability to get into the T cell and to deliver a recombinant DNA molecules into the cell hard drive by integrating into the chromosome. These viral vectors have no ability to make virus again. It's a one-way trip. Put our app into the chromosome. There's nothing left and now the T cell can go on with the only ramification of having seen that viral vector is now it has a new genome, the new app that's working. 15 So let me give you an example of how technology is changing our lives. We used to do cancer experiments in mice where the only thing we can do is measure how long a mouse lived or with calipers measure tumors under the skin. And that meant that doing mouse experiments usually took months and you had to do hundreds of mice to get the data, because you had only one outcome. Using PCR, some bright folks decided, hey, let's clone out from the firefly, the gene in the firefly tail that makes light. So it's a biological living cell that can make light. And let's PCR that up so that we can express it. Here it's expressed in bacteria. If you add in a substrate, the chemical reaction creates photons. And now living cells can make photons of light. And then some other engineer said let's take Hubble telescope liquid cooled CCD cameras instead of looking at galaxies, let's look at animals. What you get now is the ability to image in a living animal that has some sleeping medicine light coming from the tumor. And there are different enzymes now that can make different lights based on different chemical inputs. So you can input the T cells by giving the mouse one medicine and couple hours later come back, give the mouse the other medicine and image the tumor cell. This allows us to do animal experiments with just a couple mice and because we can recursively, in the same mouse, test and see what's going on over time, it's very powerful, and it speeds our work up enormously. So reprogrammed T cells can be tested in mice that have no mouse immune system. There's no rejection going on. And I told you that T cells are mobile devices. Here's an example of this technology. We've infused human T cells that have the firefly gene in a mouse that has a tumor over here. The T cells go in through the vein. They go up to the heart, and they hang out in the lung for an hour or two before they go to the rest of the body. And what we found was this is a natural aspect of T cell biology is that they'll spread out throughout the body. This is 24, 48, and about 72 hours, this is what T cells do. They home to the tumor. What we've learned is that T cells have the equivalent of a chemical nose. They can smell things. And tumors make smells that are like three day old garbage and the T cell says I've got to go to where the smell is the strongest because I have to take out the garbage. That's my goal. So it's based on the activity of a type of protein and peptide called a 16 chemokine in which cells have evolved to go either towards the highest amount of that or to the lowest amount of that. And T cells happen to respond to tumor chemokines very, very robustly. So the other thing we can do is we can test our model systems. This is where we put the firefly gene into the tumor cell. And here we're imaging human glioblastoma, the most lethal form of brain cancer that is not curable today. And here, if we put those tumor cells that make light into the mouse brain and then we come and we treat the mice, and if we treat the mice with a T cell that has a velcro that we've developed for acute lymphoblastic leukemia, the T cell interaction with the tumor is so specific because of the reprogramming, it's expected that we see this. It's as if we gave no treatment and all the tumors grow. We've designed a velcro molecule for targeting T cells to human glioblastoma, and if we give one dose of those T cells to a cohort of animals, this is about 72 hours after the T cells were given. Day 11 afterwards and for the natural life span of the mice, the tumors don't come back. And when we look at the brain, there's very little pathology. There's just a little bit of a reaction of cells in the brain to that, and the mice were functionally and behaviorally, for what mice do. You know, they run around and chase each other's tails. They were doing all of that perfectly well. So getting back to your question, we have many different apps that we're working on. So this is an app for velcro molecules so the T cell can see the tumor cells. We're making apps for T cells that allows them to grow and proliferate when they see a tumor in a place where T cells don't normally grow, such as in the brain. We're making apps for the T cells to become a biologic factory in and of itself and start secreting recombinant proteins into the tumor micro environment when they get there. And we're creating apps here, this is called an riboswitch, which is part of the mRNA of the central dogma, where you can create secondary structures such that this becomes a little sensor for a drug that the doctor gives. And if the doctor gives the drug, it will turn on the transgene and allow the cells to do their thing. And if the doctor says, well, I think you're done now, why don't you stop taking the pills, call me in the morning and we'll see if we have to turn it on or off again the next day. So we're starting to work 17 now with these technologies. And I think the potential strength of this -each one could have a role. But the potential real, I think, breakthrough strength is this idea, can we create circuitry. Can we have the different apps start organizing and making decisions based on what the other app is doing. So we're getting very interested in creating networks or synthetic biology to import into T cells for cancer therapy. And I think, you know, I'm talking about cancer therapy to you in this talk, but this could be equally true for T cells of the immune system that are the cells that say, hey, don't do anything. Those are called regulatory T cells. So for autoimmune diseases, we have the potential of engineering those T regulatory cells in patients with autoimmune disease for patients to go back in the body and turn off an autoimmune response such as one that causes MS or diabetes. So this is all happening in the labs at Ben Towne Center For Childhood Cancer Research. It's very easy to get really engrossed in this technology. I'm sure -- you know, there will be times when my wife says hello! I'm here and you have to now focus on dinner and getting the kids to sleep. But really, we are a biomedical research institute that has a very, very defined focus on bringing this to therapies that will help kids with cancer. And this is the classic conundrum for the academic researcher. You can do your mouse work and get grants and write papers and be pretty happy, or you can go off this cliff and say, how do I take this work that you've seen and turn it into a clinical trial that's supported adequately that will be approved by the FDA and you can go through all the regulatory hurdles. By the way, with absolutely zero budget, no project management, not even a secretary to answer the phones. It's a real hard job. I think Seattle Children's Research Institute has said we can't have this be the paradigm where the researcher heads back to the mice. We have to go forward and they've been very, very creative. So this is where my center exists on the corner of Olive and Bourne. I invite you all if you have a chance to come and have a tour. There's nothing like seeing the facility from the inside and seeing what's going on. I'm trying to create this academic research institute with a very strong flavor of biotech infrastructure so I actually have a preclinical development team that is to take the research from the laboratories and fast track it and do what's 18 necessary to get it to the point where the FDA can look at it and authorize a clinical trial. We also have in this building, because it was biotech company in its former life, called targeted genetics, we have clean room facilities for manufacturing cells that are at a level of purity, potency and safety that the FDA will allow us to take cells that we manufacture here and give them back to patients at Seattle Children's Hospital and FDA supervised clinical trials. So we have this and we're up and running. We built this and got it running in about 18 months. And what we're doing now is we've created now, it's one thing to make enough cells to treat a mouse. It's a whole different things to make enough cells to treat a human. It's a scalar difference and all the methodologies that are good for making a million cells fall apart when you try to make a billion at a time. So we've had to do what biotech companies do is do process development. How do we go from a tube of blood into the clean rooms to make enough cells that it will be a dose for a child on a clinical trial. And as of this August, we received the FDA's approval to move forward with our first clinical trial to treat children with acute lymphoblastic leukemia. The type of leukemia Owen has if the tumor relapses. And those are children who have very poor prognoses. Here's an example of some of the work that I did before coming back to Children's Hospital in Seattle, back at City of Hope. We were doing studies for glioblastoma multiformae, using the same app that I showed you in the mice, which patients with relapsed, unresectable tumors that have failed radiation and chemotherapy come into the trial, we give T cell doses, starting with a small dose up to higher doses and here's an example of a patient with a near complete regression of a highly refractory tumor. I think if we can start doing this in glioblastoma multiformae, things like leukemia and then neuroblastoma and sarcomas are going to be pretty straightforward. So we have a hit list. I'm about doing this to better children's outcomes in cancer. So relapsed leukemia, neuroblastoma, brain tumors, sarcomas. This causes about 80 percent of all cancer death in children. And then once we lick these, we'll get into the rare tumors. 19 I think the important part of this is what our velcro molecules target on a pediatric cancer are fairly unique, because cancer in kids evolves genetically in a very different way from adults. Adults, it's because of all your skin, your intestines, everything that interacts with planet earth on life, you're accumulating small hits, small hits, small hits. For kids, it's really more dramatic genetic changes that occur during development of the body, where you have to go from one cell to become a liver or muscle or brain, and you have to step on the gas and take off of the brake, and that's when there's a vulnerability. But having said that, that velcro molecule that we developed for neuroblastoma, if I showed you the same experiment in the petri dish with ovarian cancer, the same thing would have happened. So we're creating molecules and applications that could help in very common adult carcinomas, such as colon carcinoma, breast, prostate. And we're here to help our peers. Our process for doing, to give you the big picture, it's probably a lot like when you do with software development. It's an iterative process. So we discover in the laboratory, we take those discoveries forward to make them ready for an application. Here it would be a clinical trial. We do the clinical trial, and then we study the patients very carefully. What worked and what didn't work. Because our recombinant DNA is just like software. We can go back and adjust the code to tweak the app to do better where it needs to, or if it's too strong in another Ware, we can tune it down and then we can take it through, and take it through this iterative process to really try to evolve the therapeutic to its safest and most reliable iteration. So I think to get back to the beginning, this is where we are in 2013. I'm cautiously optimistic if we're able to push this forward that in the not-to-distant future, maybe being cured of cancer as a child may look like this, where a diagnosis happens on Wednesday. You give your blood sample on Friday, and next week, you come back for your T cells for an overnight infusion and the likes of chemotherapy and radiation are relegated to the medical history books. None of this would have been possible working in a vacuum. And here in Seattle 20 we have this incredible collaborative environment with scientists and researchers at the UW and the Fred Hutch helping us. We help them. We have an incredible support basis through Ben Towne foundation. I encourage you to go to their website and check them out. Crush Kids Cancer has come through for us and is really helping us with our leukemia trials. So it's going to take a village to get this done. I think what keeps me up at night, the hardest thing about all of this is that this is what you need in terms of financial input to cure mice of cancer and this is what you need to cure kids of cancer. The NIH, the federal government only funds this much. That's all they're going to do. Only three cents on every dollar, cancer research dollar from the NIH goes to pediatric cancer research. It's very underserved. And as you know, because of our economic situation nationally, that NIH budget, that 3 percent is getting smaller and smaller very rapidly. So that's what keeps me up at night. I want to thank you for your time and attention. And I could take questions either here or remotely as well, right, Amy? >>: Once the therapy that you're working on is under way, what is the difference in cost -- or what you would imagine the difference in cost between your therapy and traditional chemo and radiation. >> Dr. Mike Jensen: That's a good question. So right now, in the beginning, at its small scale, it's at its most expensive phase. To do our clinical trials, it's about 30 to 35 thousand dollars per product per kid. That sounds expensive. I will point out that there are a lot of drugs now on the market that you have to take every day to keep the -- that won't cure you. That will give you a couple extra years or maybe sometimes only a couple extra months. Some of those pills can cost $60,000 a year to take, and you have take it year in and year out. A bone marrow transplant costs a quarter of a million dollars. If everything goes smoothly. The lifetime cost to deal with the side effects can be millions of dollars. So this can -- if this can be a therapy that's highly effective with minimal toxicity, it will more than pay for itself. It sounds exotic and expensive now, but I think that's, you know, that's a new technology coming into an early application phenomenon. >>: [indiscernible] paid out over $2 million. I mean, $35,000 is chump 21 change. >> Dr. Mike Jensen: Leukemia therapy is pretty cheap compared to the other forms of therapy. Yeah? >>: I don't know anything about the field, really. source of funding for this research? Are insurance companies a >> Dr. Mike Jensen: No, no. So no, insurance companies don't fund the research, and for phase one studies, which we have to go through, insurance companies won't even pay the hospital bill for a bag of IV solution that's given to a patient while they're there to get the experimental therapy. We have to bootstrap this. And one of the things that, for instance, Ben Towne foundation has started is let's think about fund-raising. If we have to do a trial that the FDA says is 50 patients, let's start raising funds and say okay, we have enough for three patients, five, ten. How do we make that happen. Because we are on our own, and, you know, used to be before the recession hit, it used to be that you could get grants and make it work through grants. But now, without philanthropy, we're just going to cure mice. >>: You had mentioned high rates of evolution of cancer cells. if the cancer cell outpaces the [indiscernible]? What happens >> Dr. Mike Jensen: It's a good question. I think part of it is strategically to target the velcro to molecules that are drivers of the cancer. So there's oncogenic protein, such as receptors that sit on the surface that signal to the cancer cells, always grow, always grow. So if we can -- and there's evidence that tumors can become addicted to those oncogenic drivers. So if you hit the tumor at its Achilles heel, with a velcro, that's a good step. The other aspect of what we're working on is I showed you mono-specific velcro molecules, we're now building these so there's more than one specificity. So we could have one T cell through one molecule start seeing two to three different antigens and then the chance of a mutation occurring to have one antigen loss and a second antigen loss, it's a multiplication factor. And so that becomes much more rare. So that's a major issue for any targeted therapy for cancer, whether it's drug 22 or immunotherapy. But I think this technology platform has abilities to really address it in a meaningful way. >>: You can always update your app, right? >> Dr. Mike Jensen: Yeah, so we could have -- for individual cancers, we're probably going to have a small library of apps. Because what I see the future being is that the way cancer drugs are developed now, you develop a drug, and you give it to a thousand patients whether the drug's going to help them or not, and you ask, well, it caused the tumor to shrink in 20 percent. That's a winner. What I -- this technology is so targeted that what I see is you're going to have a biopsy of your tumor. Its genome is going to be sequenced. You going to know what's expressed and what's not expressed, and we're going to have basically a Chinese menu list of these velcro molecules. And if we have 20 different velcro molecules and your tumor has four, we're going to make your T cell product for you with those four that match the tumor that's inside your border. This kind of personalized matching up the therapy with really what's important for you to be cured of cancer, not a population of patients. >>: And you can test that, right? >> Dr. Mike Jensen: Yes. >>: So would the modified T cells or these customized T cells, is there recurrence of cancer? Because I know that's a problem with leukemia, recurrence or another occurrence of cancer. Would that then reduce that, eliminate that risk? >> Dr. Mike Jensen: Well, that's the goal that certainly one of the goals -I'm not developing this therapy and my team's not developing this therapy to just palliate, to give you a couple extra years. We want this therapy to eradicate every cancer cell that's in the body. We know from animal studies and some early clinical trials that these cells, once infused in the body, appear potentially never to go away. So they could be sitting there and if the target is absolutely tumor-specific, why not have 23 them for the rest of your life just in case. There are some targets that we might say, it's a good target to get rid of leukemia, but it will also get rid of the normal B cells, and that's the most effective form of this therapy right now. And you can do without B cells probably for months or a year or two, but without B cells in your immune system, that's going to be a problem later on, and that's where we have this concept that we'll use the suicide gene. Let's say a patient goes into remission and they're in remission three weeks or three months or three years later, then we'll say, we'll have a discussion, we're going to get rid of those cells now. We're going to let the B cells come back. But we have another vial of the T cells that we made for you in the freezer, because these cells can be put into suspended animation for decades, if not a lifetime. There is a potential, I think, if you look really forward, it's like, you know, we toss out cord blood. That's your most healthy, resilient part of your immune system when you're born. There's a lot of it in the cord blood that gets put in the trash can. Why not, you know, some day thinking big, it's just standard to have your immune cells frozen back for you from that cord blood, because the immune system does wear down. When you get your 70s, 80s and 90s, one of the major causes of end of life physiologically is the immune system basically exhausting itself and you die of an infection. And so this idea of replenishing the immune system or having it there for you, if you get cancer when you're 60, 70 or 80, which is when the cancer rates really start going up in the latter part of life. I think that should be on the table. Yeah? >>: Do you have the app to adapt this therapy from pediatric cancer to geriatric cancer and everything in between? Or is there something about pediatric cancer that makes this effective? >> Dr. Mike Jensen: No. So like at the hutch, I'm working with scientists and faculty there. And as I'm launching the leukemia trial, they're launching the adult version of it. There's a lot of back and forth, back and forth, back and forth. Some of the velcro molecules that I need to generate for pediatric cancer will never work in anything but a pediatric neuroblastoma, for instance. 24 Every now and then I'll cancer. I give the app this happen for ovarian say, oh, that does work back and forth. have a hit, neuroblastoma. Oh, it also gets ovarian to the folks at the U, I say go with it, please. Make cancer. Sometimes they'll have molecules that would for pediatric, and we're sharing it back and forth, >>: How many patients do you think have to go through your clinical trials before the FDA will approve your process? >> Dr. Mike Jensen: So typically, the very first trial of a new therapeutic is called a phase one study. A phase one study is statistically geared to show that the therapy is safe. And to determine what's called the maximal tolerated dose. Now, for a T cell, there may be no maximal tolerated dose, because it doesn't work like chemotherapy, in which we'd stop at the maximal manufacturable dose. We do those studies in cohorts. First three patients get this many cells or this much drug, higher, higher, until we start seeing side effects. Typically, that's a clinical trial. That's about 25 patients or so, just to give you a ballpark. The next type of study is a phase two study that shows, okay, in what percentage of patients at that safe dose do you get tumor responses. How effective is it? Usually, what will happen is if you have positive phase two data that, at that point, based on statutes and law, an insurance company then would be obligated to pay for the cost of us making the T cells in our facility. We can't make a profit, but the actual cost. That's a big deal. That's only happened a couple times, but that would be the paradigm. You know, Seattle's been a real driving force in curative cancer therapeutics for decades now. Bone marrow transplant was founded in Seattle and is now a life saving procedure all around the world. This would be potentially could be a similar type of deployment where centers of excellence that have these facilities, manufacturing facilities, can start making products for patients and patients come in and receive that therapy. We're also doing developments where we freeze the cells so we can FedEx them back to where the patient is. So we can become a hub and be able to supply 25 products around the country and eventually all around the world. It's a very interesting time in this field in terms of biotechnology. Ten years ago, when I talked about this stuff, folks in biotech and pharma, their eyes would glaze over. What do you mean a patient-specific product. You mean you're going to make something for each patient? Yeah, yeah. Dendrion kind of broke that glass ceiling in a way. We could talk about maybe offline their technologies and, you know, what challenges they have. But it could be that same type of phenomenon where companies can create these hubs and be able to FedEx in cells and then FedEx out products back to patients. >>: For the mice cancer cells that you worked on, what percentage -- what was your success rate of killing it, but in addition it killed the mice? >> Dr. Mike Jensen: My general philosophy is if you're working with something that can't cure 100 percent of the mice, it's not good enough for a human trial. It's a little bit of an artificial situation, because we create models that help us read out something. So they're nowhere close to being like real world. This is the same as a patient when they come in with a diagnosis of acute lymphoblastic leukemia. We rig the system in ways that we try to parse it so we ask a specific question of the model that gives us an insight into the biology of the system or different aspects of it. But it's never -- the models are never good enough to say this replicates the clinical situation. You really have to move quickly into that phase one trial. >>: So they're a little optimistic, but how good is optimistic right now? >> Dr. Mike Jensen: Well, the velcro technology, you know, I've been in this for 16 years. There's a couple other institutions in the country that have been working on this. We all collaborate and share information. But the Children's Hospital of Philadelphia was the first to treat the first three or four children, and there were children of that very first cohort that got one dose of cells in which their leukemia was most of their bone marrow that everything had failed, and about three weeks later, they go into remission. And without any chemotherapy. And some of the first kids treated are now eight months out in remission with these T cells floating around. So the ability of this therapy to cure a human, I think, is becoming quite 26 clear. How do we make this address all cancers in different patient populations become usable is a big challenge. >>: What I was getting at is I was wondering for the mice that you can freely test, if you had 90 percent success rate, once you can kill them in the dish, you can kill them in the mouse. Is it 50 percent? Because it seems like it's the same thing with the human cells without any approval, you can just test it in the dish. If you're effective there ->> Dr. Mike Jensen: The dish, if it's not effective in the dish, it won't cure a mouse. If it's effective in the dish, you can probably create a mouse model where it's 100 percent effective by how many tumor cells you put in and what the timing is. There have been situations where it looks good in the petri dish and it's a complete failure in the mouse, and that's an end of story for that version of the app. We usually go back and say, okay, we need to advance it more in the molecular side before we go back. So there's a lot of ping-pong back and forth. >>: So it's hard to say? >> Dr. Mike Jensen: Yeah. It's very empiric right now. We'd love to have molecular models based on crystal structures of these molecules and comprehensive readouts of signaling pathways that are predictive, and that's part of what I hope to do in the next year or two is what works in the petri dish, what works in the model. Give me the type of readout called mass spec, and tell me about all the signaling molecules that get turned on for the one that works, compared to the one that doesn't work. And can we then kind of high through-put the velcro molecules based on a signature that's predictive of 18 months of laboratory work. That would be a nice place to get to. I know there's a urinary biomarker question. I know so little about urinary biomarkers, that I'm -- I think I should defer. >>: There's another question about [indiscernible]. opportunities [inaudible]. >> Dr. Mike Jensen: Oh, who is that person? One was about volunteer Name the names. I think 27 that's ->>: [indiscernible]. >> Dr. Mike Jensen: It's a really good question, and we were talking about this a little bit. I think we, in biomedical -- in academic biomedical research, you would be horrified by the lack of sophistication and access to tools, even computational tools and ability to communicate and share data sets between individuals down the hall or between SCRI, where I am, and the UW and the Hutch and across the country. It's woefully under developed and under supported, and I think, you know, we are now getting into Big Data. The genomeics efforts I was saying that I'm part of a grant that seeks to link genomeics data, which is sequencing the genomes of hundreds of cancer cell lines and patient genomes and link it with what can we pull out of that computationally that will identify the target for the velcro. And I'm trying to -- we're trying to put together this organization that will span seven or eight institutions in the United States and a couple in Canada. And we're in a vacuum. So I think there's -- it's a great conversation that I would love to have with any of you offline and talk about. I think an organization like Microsoft could have incredible impact in helping academic researchers and non-for-profits be able to work faster and more efficiently. I'm a clinical oncologist by training, pediatric oncologist, and I will tell you that the main thing that families think about is time. And you walk through the waiting room, and they look up at you and say when is that breakthrough coming to save my child's life or to make it so my child doesn't need to have radiation to their brain. It's all about time and it's all about acceleration. And any assets we can bring from any, any sectors in industry or otherwise to help accelerate the process are most welcome. >>: I'll give my unsolicited pitch here. I'm part of the cancer advocacy network field. I work in research. And we support Seattle Children's Hospital, specifically Dr. Michael Jensen's work. But there are about 13 cancer research guilds that support Seattle Children's Hospital and my guild pulls them all together and has a website where you can find all kinds of activities, events, ways to volunteer, ways to donate. You've got the Ben Towne Foundation, which funds Mike Jensen as well, and then Alex here has his 28 Crush Kids Cancer, which is part of the ->> Alex Weinert: It's part of the guild. >>: So there's all kinds of ways that people can help, and we believe that the cure is in the research. >> Alex Weinert: As Dr. Jensen said, the hope is in the research. The thing that anybody in my situation up here more than anything is relapse. Owen goes off treatment in May and he's got a higher probability of relapse right after he goes off treatment. If that were to happen, those are the trials that can save Owen's life. So that hope, and I know parents who have seen that window come and go. Certainly, I'd be willing to volunteer Lisa or myself, if you want to know more about how to volunteer to help, we would be happy to be a liaison for Microsoft. So my name is on the first set of slides. Just send me an email. >>: And I'm in research. I'm Lisa Clausen. Just to mention, if anybody actually wants to come in and see Mike's lab and see the facilities, we do tours. There's contact information on some flyers that are outside as well. You can get my card as well and I can set something up for you. >> Dr. Mike Jensen: So thank you all for coming to this lecture and all of you out there in cyberspace too. It was really great to have this chance to come and tell you about our work. Thank you.